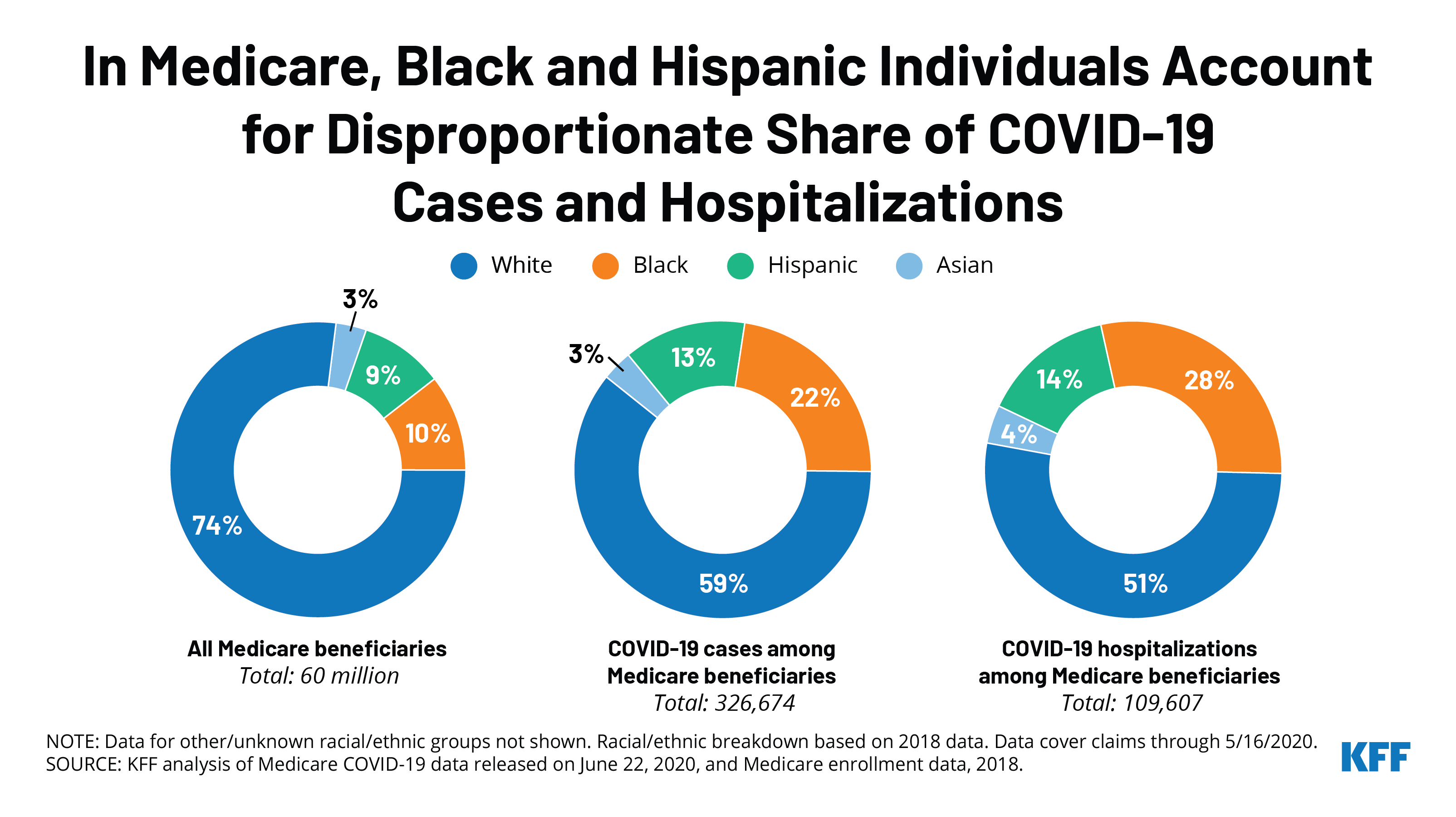
In Medicare, Black and Hispanic Individuals Account for Disproportionate Share of COVID-19 Cases and Hospitalizations
The independent source for health policy research, polling, and news.
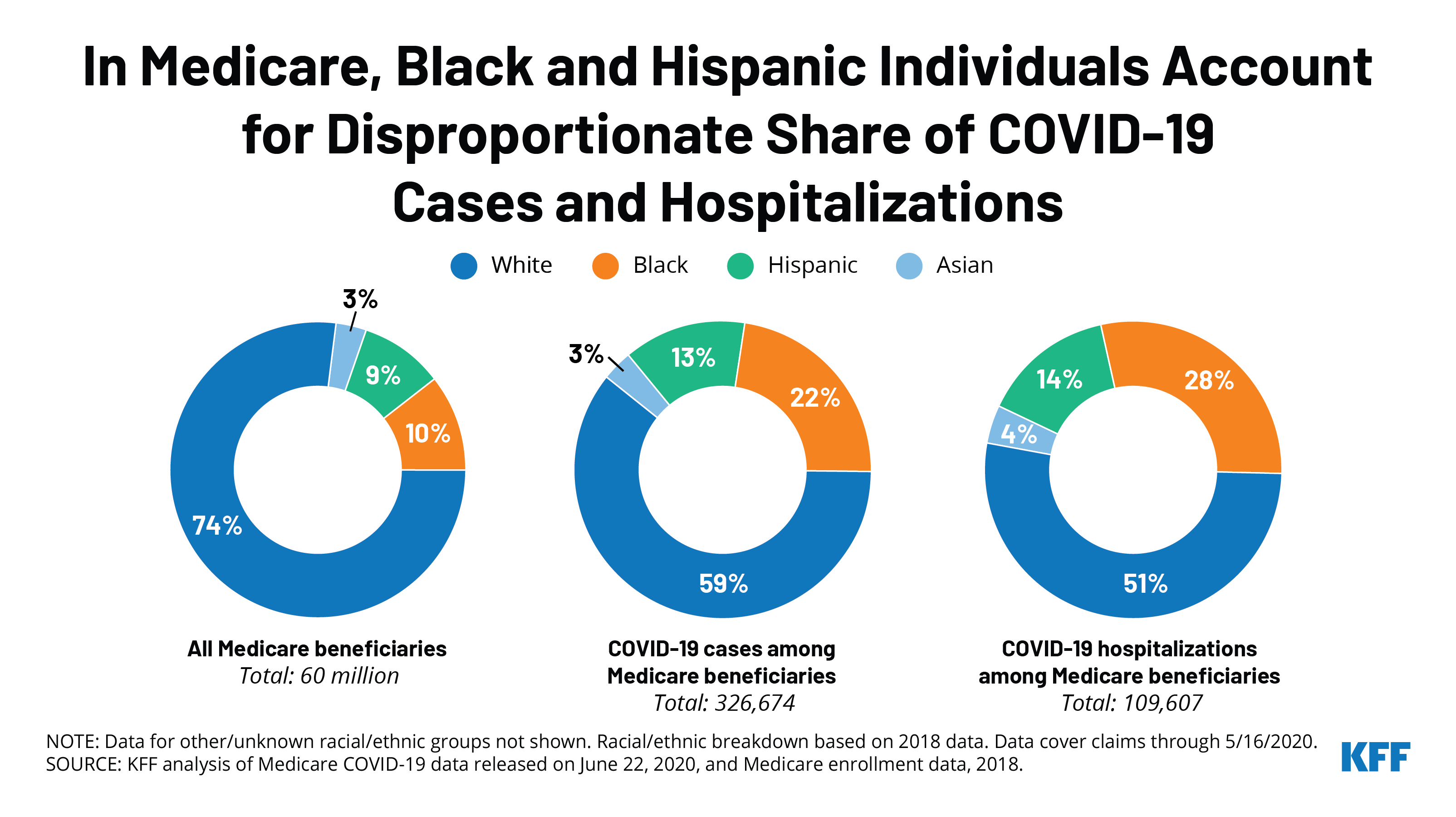
As states continue to ease social distancing restrictions, Americans are leaving their homes more often to shop, visit close family and friends and go to work than they did in April in spite of their concerns about contracting coronavirus, the latest KFF tracking poll finds.
The poll finds 9 in 10 (89%) adults say they left their home to shop for food, medicine, or essential household items in the past week, including 61% who say they did this multiple times – up from 44% in April.
Just over half (54%) say they left home to visit close friends or family in the past week, up from 30% in April. Less than half (45%) say they went to work in the past week, up from 33% in April. About three in ten (29%) report dining at a restaurant in the past week, while few (7%) rode on public transportation.
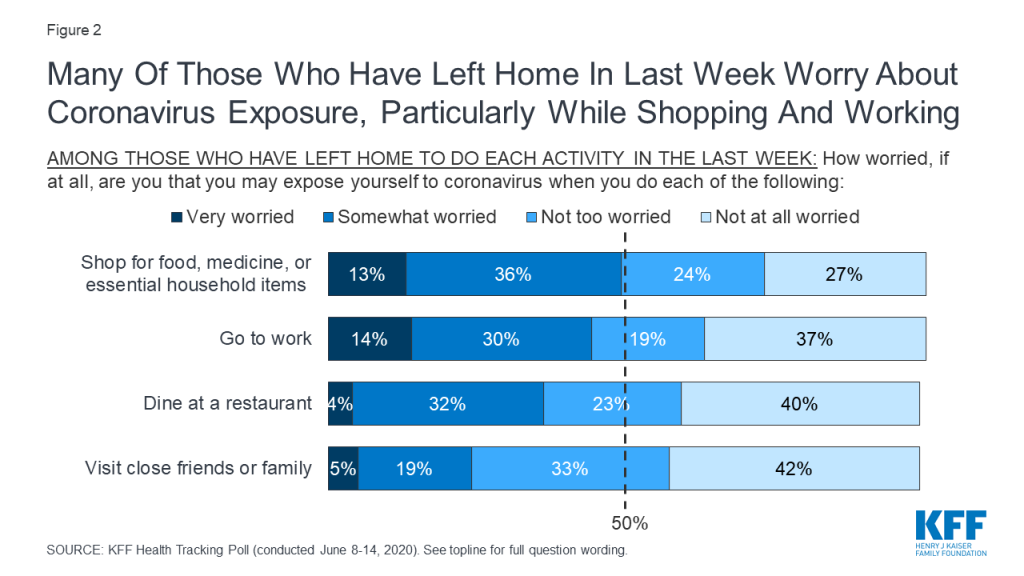
Many of those who report leaving their homes to engage in these activities are at least somewhat worried that they may expose themselves to coronavirus in the process. For example, almost half of those who went shopping (48%) and nearly as many (44%) who went to work say they are worried about exposure to the virus.
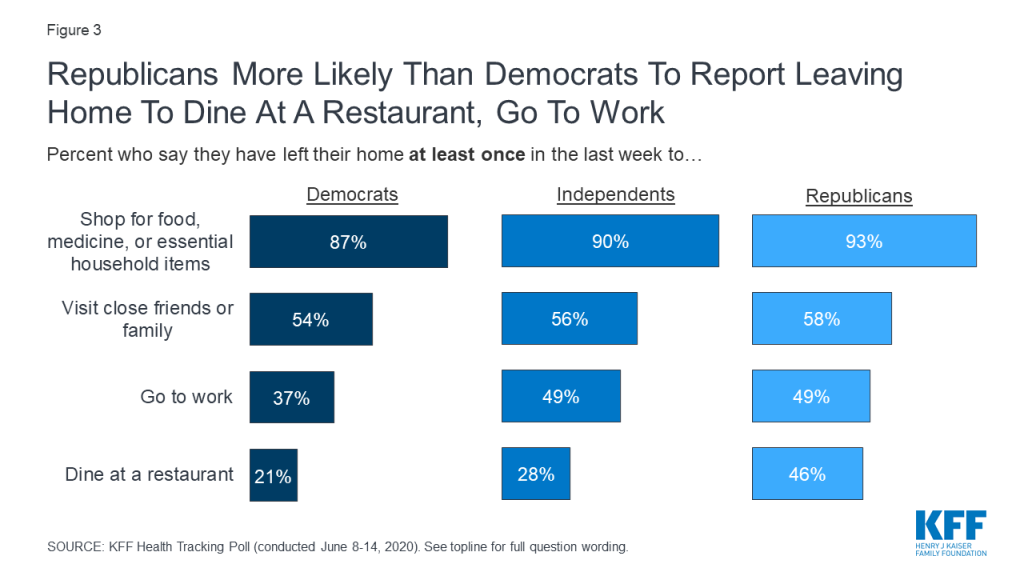
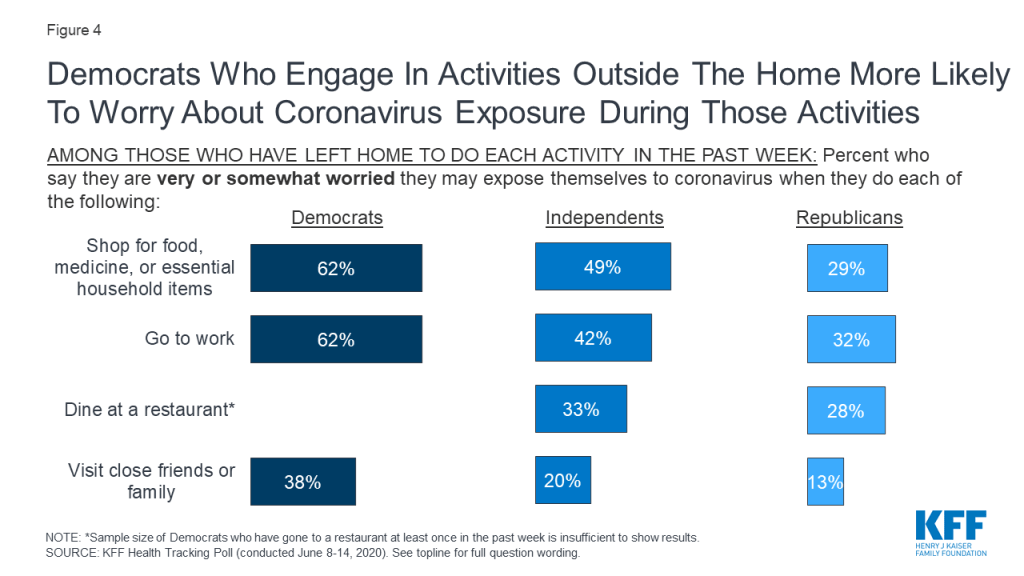
The poll continues to find partisan differences in how Americans are reacting the coronavirus pandemic. Republicans are more likely than Democrats to leave their homes to engage in some of these activities, while Democrats are more likely to worry about exposure to the virus while doing so.
For example, Republicans are more likely to report leaving their homes to go to work in the past week (49%, compared to 37% of Democrats). Among those who went to work, Democrats are more likely to say they are worried about coronavirus exposure (62%, compared to 42% of independents and 32% of Republicans).
Republicans also are twice as likely to say they ate at a restaurant at least once in the past week (46%, compared to 21% of Democrats).
The poll also probes into how the pandemic is affecting Americans’ use of medical and dental services. The share of the public who say they or a family member has skipped or delayed care in the past month has not changed much since our May poll. Half (52%) of the public says they or someone in their family has skipped or delayed getting medical or dental care because of coronavirus this month – similar to the share who said so last month (48%).
The types of care most often put off include dental check-ups and procedures (37% of all adults) and regular check-ups or physical exams (30% of all adults). Fewer report skipping or postponing doctor visits for symptoms they were experiencing (15% of all adults), doctor visits for chronic conditions (13%) or preventive screenings (12%).
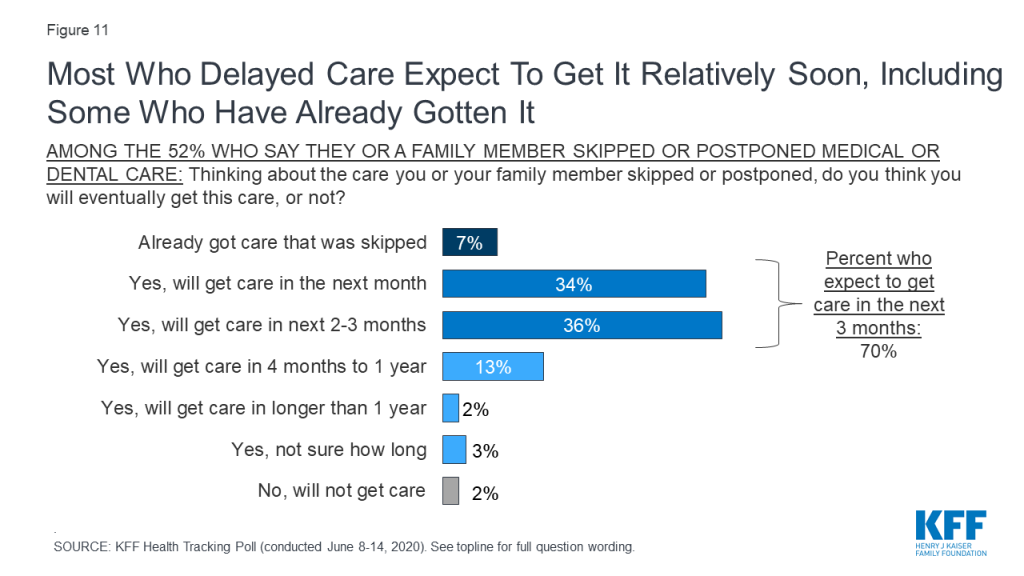
There are some signs that people are beginning to catch up on their care skipped because of coronavirus, including 7% who say they or their family member have already gotten the care they initially delayed. An additional 70% say they expect to catch up on the missed care within three months, including a third (34%) who expect to get the care within a month. Very few (2%) say they don’t expect to get the care that was skipped or postponed.
When asked why the coronavirus pandemic led them to skip or postpone care, people most often say that the doctor’s office or facility was closed or offering limited appointments (43% of all adults). Many (27% of all adults) say that they felt unsafe visiting a doctor’s office or other medical facility during the outbreak.
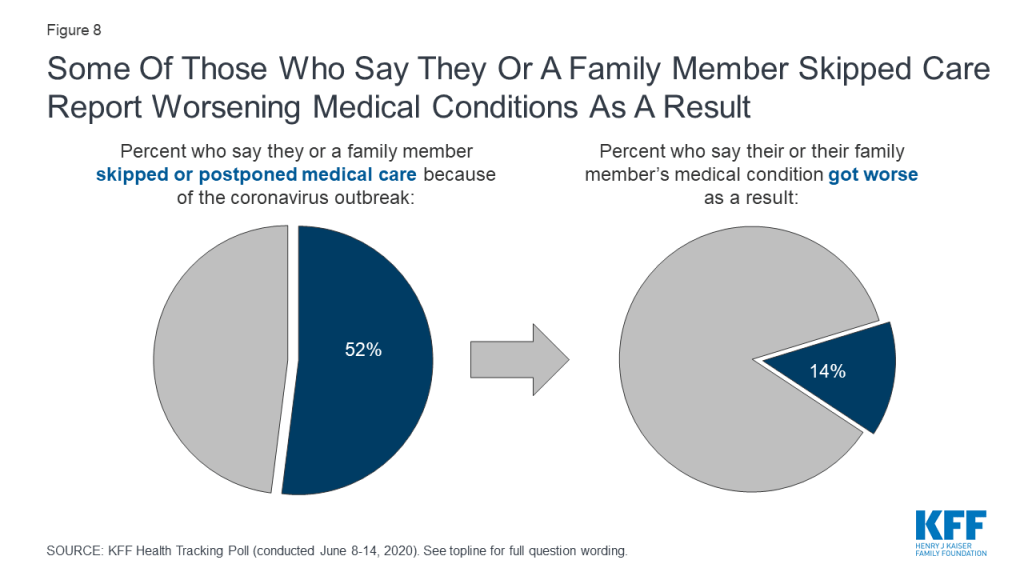
More than a quarter of those who say they or a family member skipped or postponed care because of coronavirus (27%, or 14% of all adults) say their or their family member’s condition worsened as a result.
The poll looks ahead to the presidential election in November and examines how voters view the biggest problems facing the country, and which presidential candidate they trust most to handle them.
When asked about who they most trust on various issues, more voters say presumptive Democratic presidential nominee Joe Biden than President Donald Trump on health care (53% vs. 38%) and coronavirus (50% vs. 41%). President Trump holds a narrow trust edge on the economy (49% vs. 44%), while former Vice President Biden leads on other issues including maintaining law and order (51% vs. 41%), police violence (55% vs. 36%), and race relations (58% vs. 34%).
Designed and analyzed by public opinion researchers at KFF, the poll was conducted June 8-14 among a nationally representative random digit dial telephone sample of 1,296 adults. Interviews were conducted in English and Spanish by landline (297) and cell phone (999). The margin of sampling error is plus or minus 3 percentage points for the full sample. For results based on subgroups, the margin of sampling error may be higher.
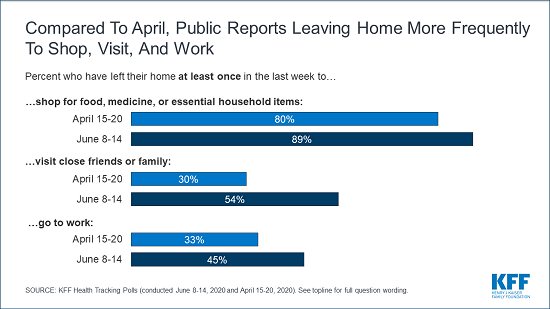
At a time when protests across the country are highlighting issues of structural racism and discrimination, 63% of Black adults and nearly half (45%) of Hispanic adults say they have been treated unfairly in a variety of situations in the past 12 months because of their race or ethnicity. Most commonly, about four in ten Black adults and about a quarter of Hispanic adults say they have been treated unfairly due to their racial or ethnic background when they were shopping (44% and 28%, respectively) or when they were at a restaurant, bar, theater, or other entertainment place (41% and 25%). Black adults (30%) are nearly three times as likely as Hispanic adults (11%) — and ten times as likely as White adults (3%) to say they have been treated unfairly in dealings with the police due to their race. About one in five Black and Hispanic adults say they have experienced unfair treatment due to their race at work (20% and 18%, respectively) and about one in six say they have been experienced unfair treatment while getting health care (17% and 14%, respectively). Very small shares of White adults say they have experienced any of these types of unfair treatment due to their racial or ethnic background.
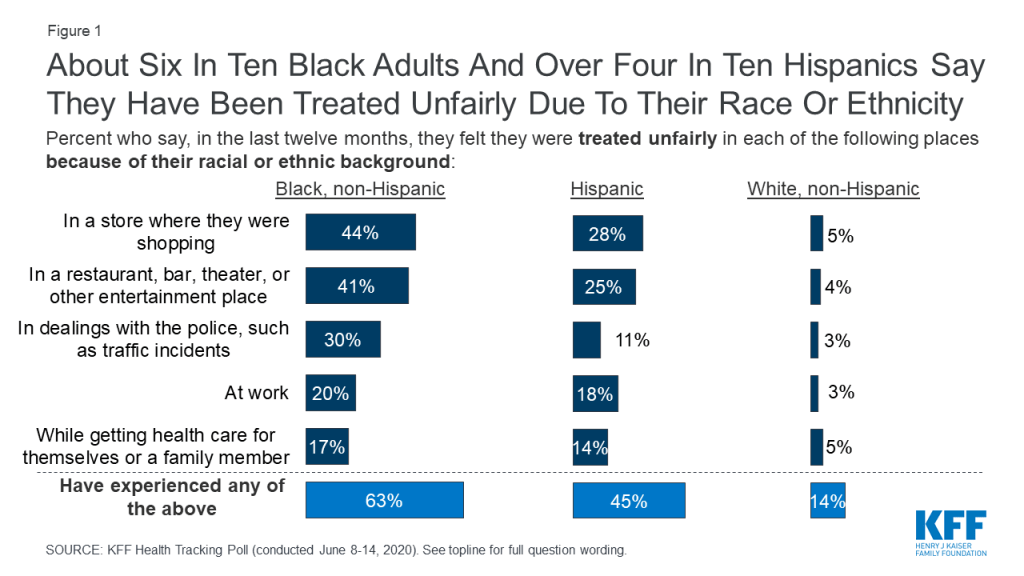
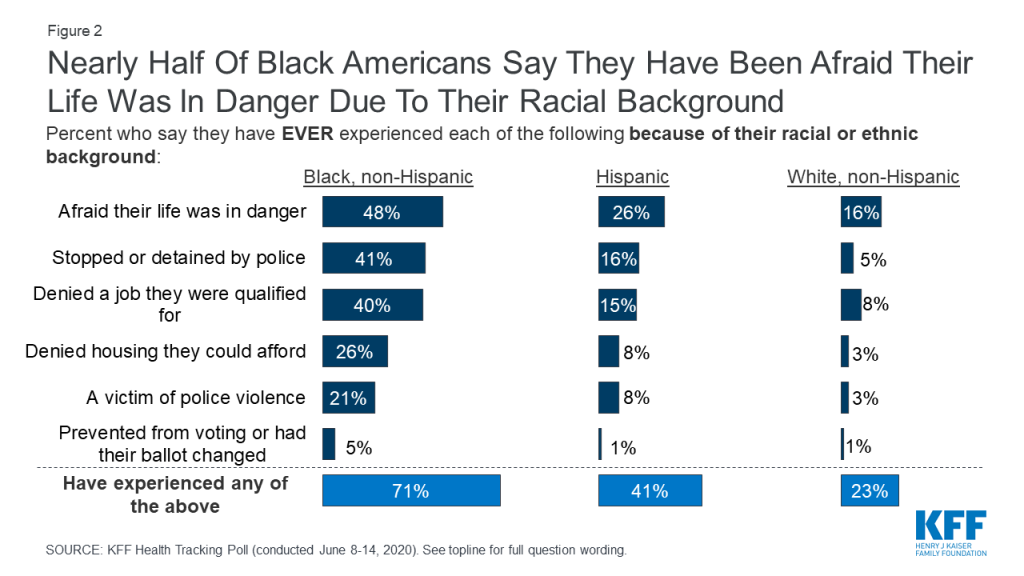
When asked about more specific experiences of discrimination or violence due to their race or ethnicity, the disparities are no less stark. About half of Black adults (48%), including 60% of Black men and 38% of Black women, say they have ever been afraid their life was in danger because of their race. This compares to about a quarter (26%) of Hispanic adults and 16% of White adults. Black adults are also much more likely than Hispanic or White adults to say they have been denied a job for which they were qualified (40%, 15%, and 8%, respectively) or denied housing they could afford due to their race (26%, 8%, and 3%). When it comes to interactions with police, Black adults are more than twice as likely as Hispanic adults and eight times as likely as White adults to say they have been stopped or detained by police because of their racial or ethnic background (41%, 16%, and 5%, respectively). Moreover, about one in five Black adults (21%) – including 30% of Black men – say they have been a victim of police violence due to their racial background. Overall, seven in ten Black adults (71%) say they have ever experienced at least one of these more specific instances of discrimination due to their race or ethnicity, compared with four in ten Hispanics (41%) and a quarter of Whites (24%).
In recent weeks following the death of George Floyd and ensuing nationwide protests, a number of reforms have been proposed to address police violence and excessive use of force. New York and Iowa have recently banned police from using chokeholds or strangleholds, Congressional Democrats have introduced a police reform bill to address racism and excessive force by police, and U.S. Representatives Justin Amash and Ayanna Pressley have introduced a bill to end qualified immunity for police officers, which would make it easier for victims of police misconduct to successfully sue officers in civil court.1 ,2
When asked about a number of proposals aimed at reducing excessive use of force by police officers, majorities of the public express support. Americans overwhelmingly support requiring police to intervene and stop excessive force used by other officers and report these incidents (95%) and requiring police to give a verbal warning, when possible, before shooting a civilian (89%). About three in four support requiring states to publicly release disciplinary records for law enforcement officers (76%) and allowing individuals to sue police officers if they feel they were subjected to excessive force (73%). Two-thirds support banning police from using chokeholds and strangleholds (68%) and about half (52%) support banning no-knock warrants that allow police to enter a person’s residence unannounced.
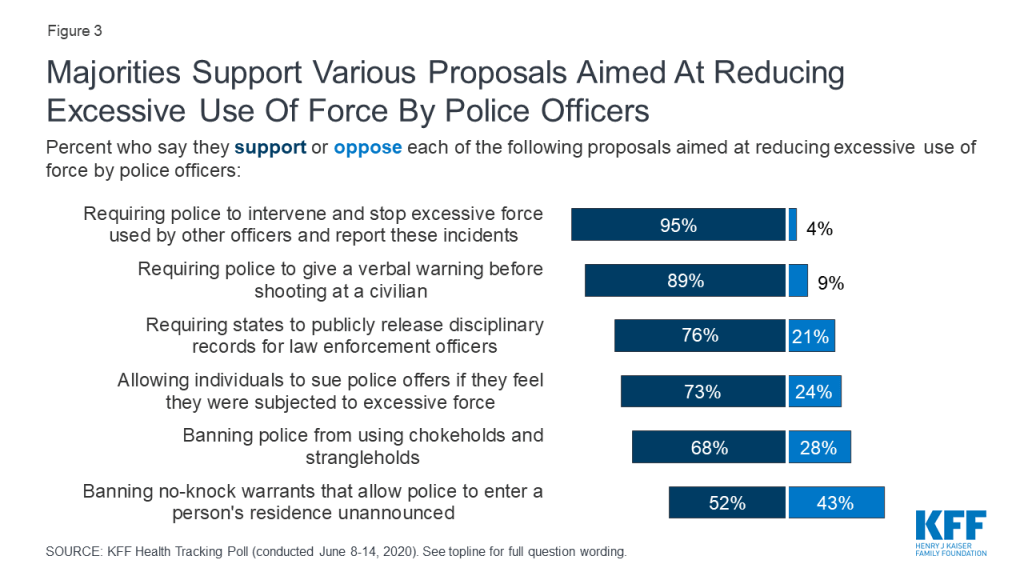
There is bipartisan support for many proposals aimed at reducing police violence, including requiring officers to intervene to stop the excessive use of force by other officers, requiring verbal warnings before shooting, mandatory public release of disciplinary records, and allowing individuals to sue police officers if they feel they were subjected to excessive force. When it comes to banning police from using chokeholds and strangleholds, large majorities of Democrats (82%) and independents (70%) are in support, compared with a bare majority (52%) of Republicans. And while majorities of Democrats and independents support banning no-knock warrants, only about a third of Republicans (34%) support this proposal.
| Table 1: There is bipartisan support for many policies aimed at reducing police violence. | |||
| Percent who support each of the following proposals: | Democrats | Independents | Republicans |
| Requiring police to intervene and stop excessive force used by other officers and report these incidents | 97% | 96% | 95% |
| Requiring police to give a verbal warning before shooting at a civilian | 95 | 90 | 83 |
| Requiring states to publicly release disciplinary records for law enforcement officers | 89 | 75 | 62 |
| Allowing individuals to sue police officers if they feel they were subjected to excessive force | 85 | 74 | 55 |
| Banning police from using chokeholds and strangleholds | 82 | 70 | 52 |
| Banning no-knock warrants that allow police to enter a person’s residence unannounced | 65 | 56 | 34 |
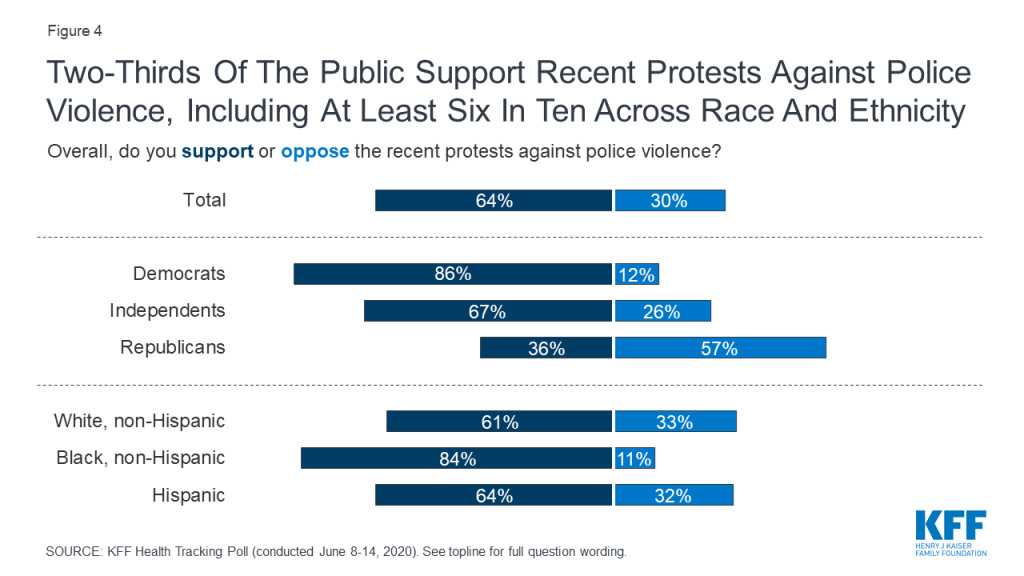
About two in three Americans (64%) support the recent protests against police violence while three in ten oppose the protests (30%). There are sharp partisan divisions on the recent protests with an overwhelming majority of Democrats (86%) and two in three independents (67%) saying they support the protests while about six in ten Republicans (57%) oppose. Majorities across racial/ethnic groups support the protests including about eight in ten Black Americans (84%) and about six in ten White Americans (61%) and Hispanics (64%).
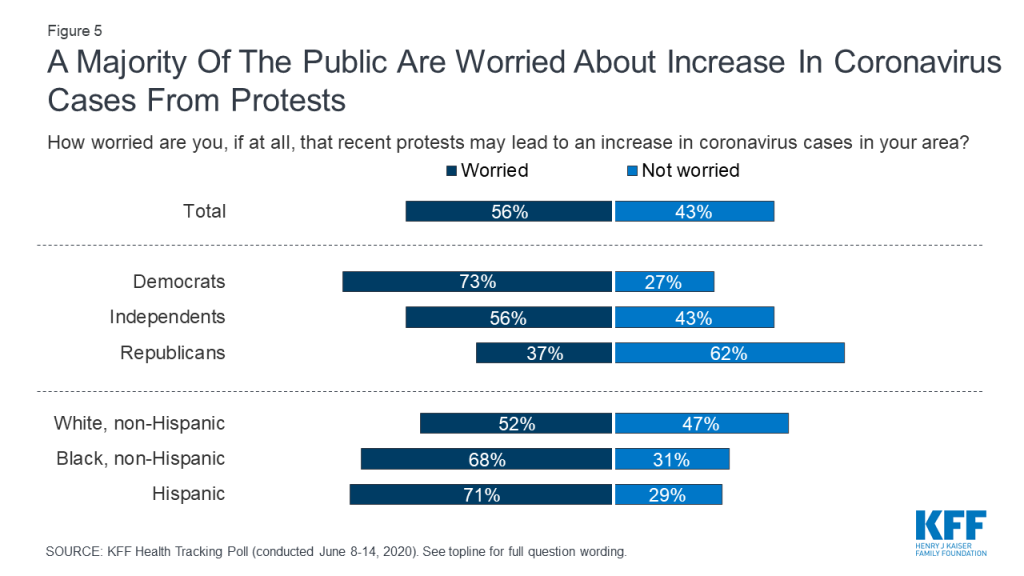
At the same time that a majority of the public supports the recent protests, more than half (56%) say they are very or somewhat worried that protests may lead to an increase in coronavirus cases in their area. Notably, Democrats and Black adults – groups that are most likely to support the protests – are also among the most likely to say they are worried about the protests leading to an increase in coronavirus cases (73% and 68% respectively).
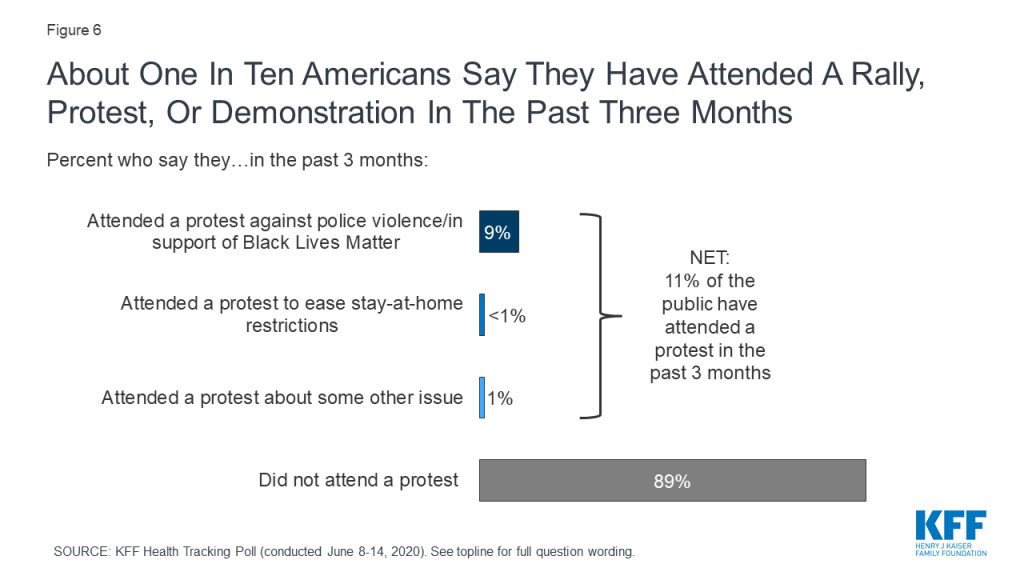
Eleven percent of adults say they have attended a protest, march, or demonstration in the last three months, including 9% who say they attended an event to protest police violence or in support of Black Lives Matter or other anti-racist causes (less than 1% of adults say they attended a protest to ease stay-at-home restrictions implemented due to coronavirus in the past three months). While a majority of Americans are worried that recent protests may lead to an increase in coronavirus cases in their area, most of those who say they attended a protest or demonstration in the last 3 months say they are not too worried (29%) or not at all worried (49%) that they may have exposed themselves to coronavirus when attending such an event.
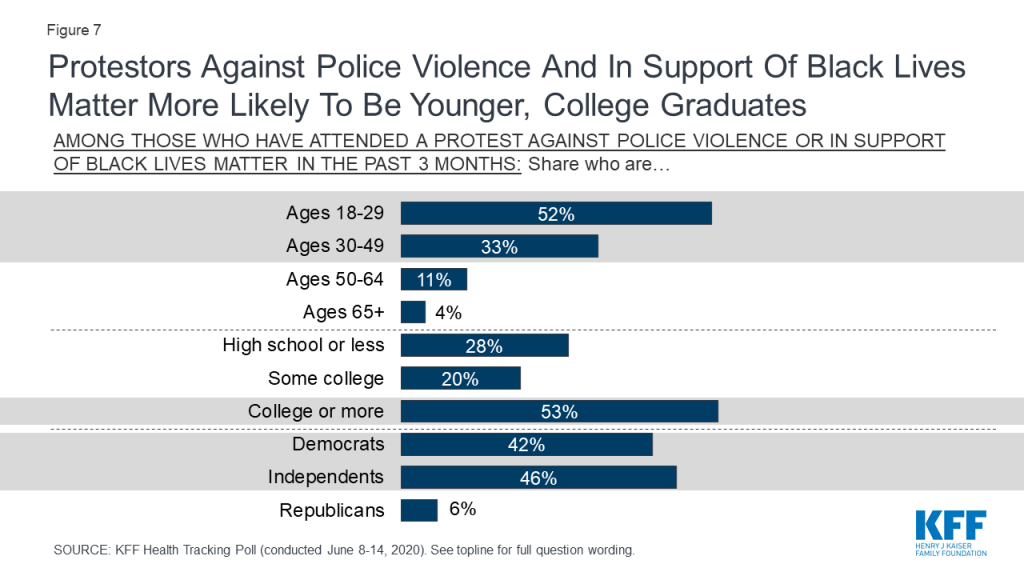
Who are the 9% of Americans who have been protesting police violence and racism in the past few months? Recent protesters are likely to be younger adults, with more than eight in ten being under 50 years old, including half (52%) who are between the ages of 18 to 29. Most of those who report attending recent protests against police violence and racism are college graduates (53%). These protesters are likely to be Democrats (42%) or independents (46%) with just 6% of protesters identifying as Republicans.
Large shares of Americans view racism, police violence, and violence caused by protesters as at least somewhat of a problem in the U.S. today. About six in ten (58%) say racism is a “big problem,” while about four in ten say the same about police violence against the public (42%) and violence caused by protesters (38%).
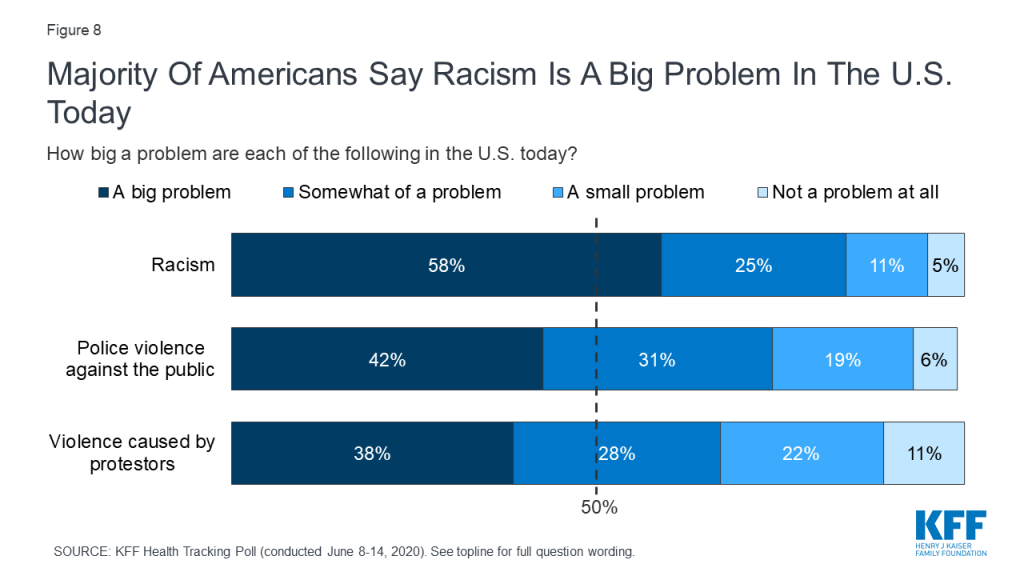
While majorities across racial and ethnic groups view racism as a big problem in the U.S., the share is largest among Black adults (85%) compared with those who are Hispanic (62%) or White (53%). Racial and ethnic divisions are deeper when it comes to perceptions of the problem of police violence – 77% of Black adults say police violence against the public is a big problem, compared with just under half (47%) of Hispanic adults and about a third (34%) of White adults.
Partisan divisions in perceptions of these problems run deep. Eight in ten Democrats (82%) and a majority of independents (59%) say racism is a big problem in the U.S. today, compared with 25% of Republicans who say the same. Democrats are much more likely to say police violence is a big problem (65%) than violence caused by protesters (24%). Conversely, Republicans are much more likely to say violence caused by protesters is a big problem (62%) than to say the same of police violence against the public (14%).
| Table 2: Black adults, Democrats are more likely to say police violence is a “big problem” | ||||||
| Percent who say each of the following is a “big problem” in the U.S. today: | Party ID | Race/Ethnicity | ||||
| Democrats | Independents | Republicans | White | Black | Hispanic | |
| Racism | 82% | 59% | 25% | 53% | 85% | 62% |
| Police violence against the public | 65 | 41 | 14 | 34 | 77 | 47 |
| Violence caused by protesters | 24 | 36 | 62 | 39 | 27 | 45 |
Overall, many adults in the U.S. recognize the disparities faced by Black and Hispanic people when it comes to health care and interactions with the police. Seven in ten adults (69%) think Black Americans are more likely than White Americans to experience police violence and a majority (56%) think Hispanic Americans are more likely than White Americans to experience police violence. A KFF analysis has shown that early data suggest coronavirus is disproportionately affecting communities of color.3 Half of the public (50%) recognize that Black Americans are more likely to get sick or die from coronavirus while fewer (36%) are aware of the disproportionate impact of coronavirus on Hispanics.4 About four in ten Americans think Black adults and Hispanic adults are more likely than their White counterparts to receive poor quality health care (42% and 38%, respectively) and to lose their job or income as a result of coronavirus (40% and 44%, respectively). More than four in ten think Black and Hispanic adults are less likely to be able to access the health care they need (44% and 45%, respectively) or to be covered by health insurance (45% and 49%, respectively).
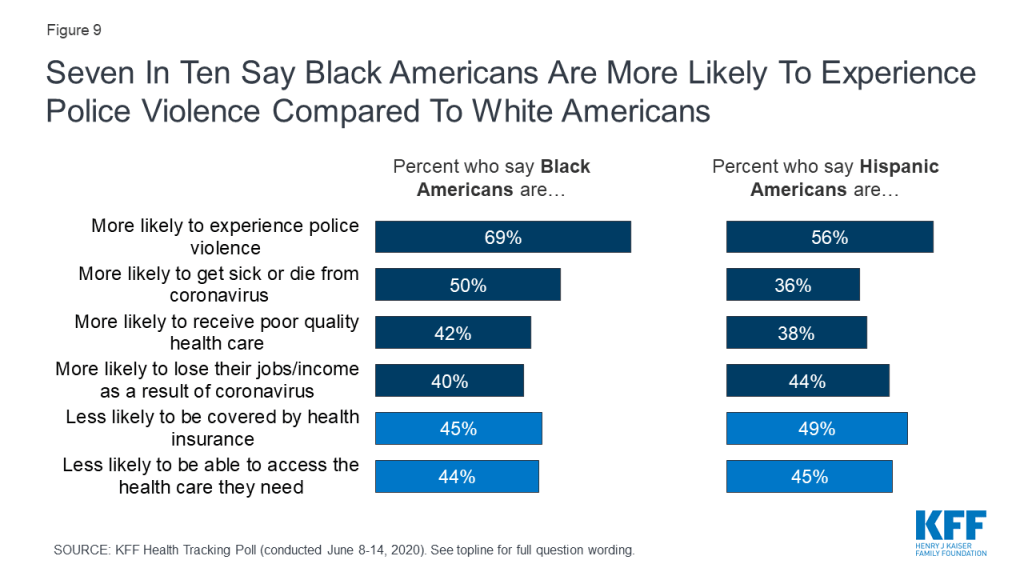
There are partisan differences in perceptions and knowledge of disparities faced by Black and Hispanic adults when it comes to health care and experiences with police. Democrats are twice as likely as Republicans to know that Black Americans are more likely than White Americans to get sick or die from coronavirus (69% vs. 34%). Similarly, 64% of Democrats know that Black Americans are less likely than White Americans to be covered by health insurance, while most Republicans (70%) say there is no difference. Nearly nine in ten Democrats (87%) know that Black Americans are more likely than White Americans to experience police violence, while 52% of Republicans say there is no difference.
| Table 3: Democrats and independents are more likely than Republicans to recognize disparities faced by Black and Hispanic Americans | ||||||
| Compared to White Americans, do you think Black Americans are more or less likely to… | Compared to White Americans, do you think Hispanic Americans are more or less likely to… | |||||
| Democrats | Independents | Republicans | Democrats | Independents | Republicans | |
| …experience police violence | ||||||
| More likely | 87% | 73% | 38% | 77% | 59% | 25% |
| Less likely | 2 | 4 | 7 | 2 | 3 | 3 |
| No difference | 11 | 21 | 52 | 20 | 36 | 71 |
| …get sick or die from coronavirus | ||||||
| More likely | 69 | 47 | 34 | 57 | 36 | 15 |
| Less likely | 1 | 3 | 2 | 3 | 4 | 2 |
| No difference | 29 | 46 | 62 | 36 | 56 | 81 |
| …be covered by health insurance | ||||||
| More likely | 5 | 6 | 10 | 8 | 7 | 8 |
| Less likely | 64 | 48 | 18 | 64 | 51 | 29 |
| No difference | 26 | 42 | 70 | 24 | 39 | 63 |
As most states move to ease social distancing restrictions, the latest KFF Health Tracking Poll finds that U.S. adults report venturing out of their homes to go to work, shop, or visit friends and family more frequently than they did in April, though few say they have eaten at a restaurant or used public transit in the past week. Nine in ten (89%) say they have left their home to shop for food, medicine, or essential household items in the past week, including 61% who say they’ve done this at least twice (up from 44% in late April). Just over half (54%) say they have left home to visit close friends or family in the last week, up from 30% in April, and the share who report going to work at least once in the last week has increased from 33% to 45%. About three in ten (29%) report dining at a restaurant in the past week, but just 7% say they’ve ridden public transit (not asked in April).

Many of those who report leaving their homes to engage in various activities are doing so with some trepidation. Among those who’ve left their homes to shop in the past week, about half (48%) say they are at least somewhat worried that they may expose themselves to coronavirus when doing so. Similarly, more than four in ten (44%) of those who’ve worked outside their home say they are at least somewhat worried about exposure to the virus at work, while just over half (56%) say they are not too worried or not at all worried. Among those who report dining out or visiting friends or family in the past week, most say they are not worried about exposure during these activities (63% and 75%, respectively).
There are some partisan differences, both in engaging in activities outside their home, and how much they worry about exposing themselves to coronavirus when they do so. For example, Republicans are more than twice as likely as Democrats to say they have left home to dine at a restaurant at least once in the past week (46% vs. 21%). Even when looking at only those counties with more than 25 deaths attributed to coronavirus, this partisan difference remains with Republicans in those counties more likely than their Democratic counterparts to report leaving the house to dine at a restaurant (45% vs. 20%).
Among those who have engaged in each of these activities at least once in the past week, most Republicans say they’re not too worried about exposing themselves to coronavirus while shopping, going to work, dining out, or visiting friends and family. Among Democrats, most of those who’ve left their house to shop or go to work in the past week are at least somewhat worried about virus exposure (62% for each).
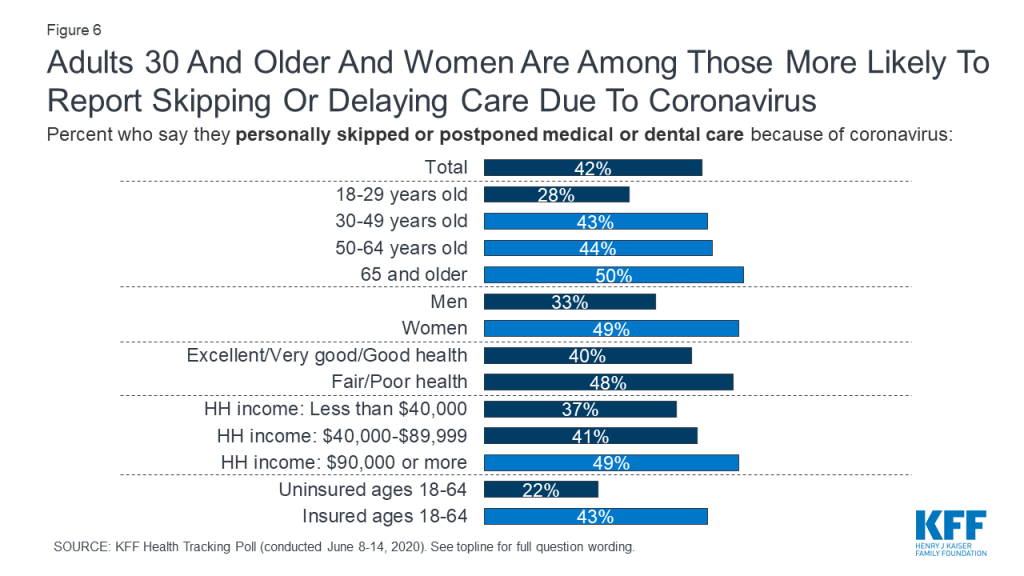
While many Americans report resuming some of their regular activities in recent weeks, many report putting off certain types of medical and dental care. About half of adults (52%) say that they or another family member living in their household skipped or postponed some type of medical or dental care in the past 3 months because of coronavirus. This includes 42% who say they personally skipped or postponed care.
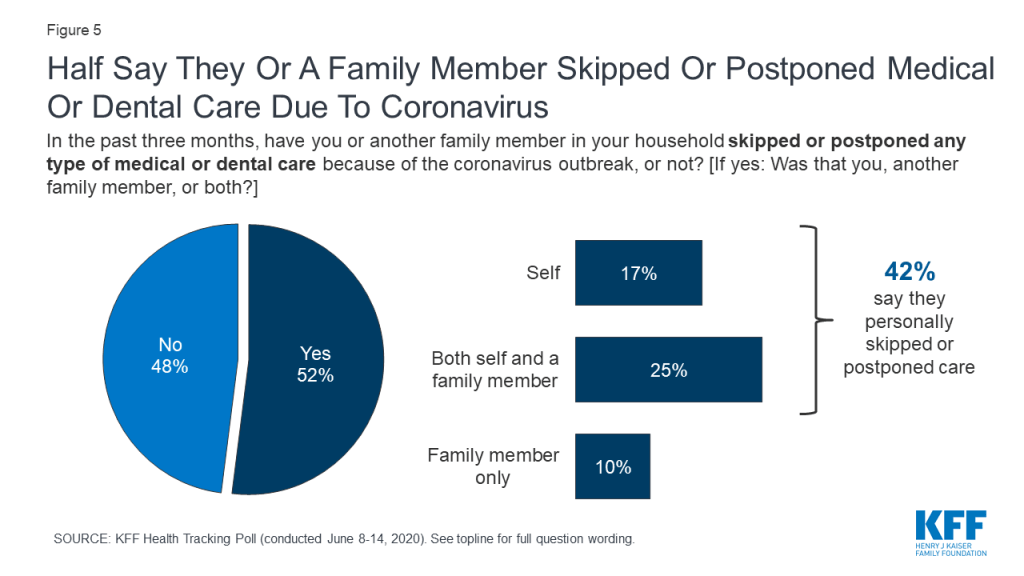
Women and older adults are more likely than their counterparts to say they personally skipped or postponed care. Those with higher incomes are also somewhat more likely than those with lower incomes to report postponing care, as are those with health insurance compared to the uninsured. This latter finding may reflect the fact that those with lower incomes or without insurance may use less care under normal circumstances, and so are less likely to report skipping or postponing visits due to coronavirus. Notably, the March 2019 KFF Health Tracking Poll found that about half of adults (51%) said they or a family member had skipped or postponed health care due to cost in the past year, with uninsured adults under age 65 (76%) and those with lower household income (62%) more likely than their counterparts to say they had skipped or postponed care.
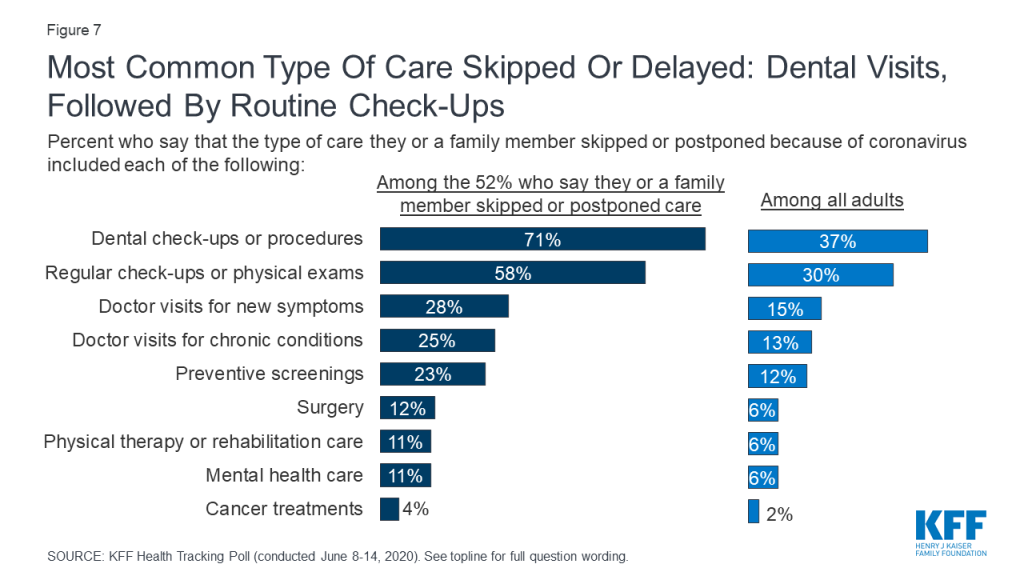
Among those who say someone in their household skipped or delayed care, the most common types of care missed are dental check-ups or procedures (71% of those who skipped or postponed care, or 37% of all adults) and regular check-ups or physical exams (58%, 30% of all). This is followed by about a quarter who say they or a family member skipped or postponed doctor visits for symptoms they were experiencing (28% of those who skipped/postponed care, or 15% of all adults), doctor visits for chronic conditions (25%, 13% of all), and preventive screenings (23%, 12% of all).
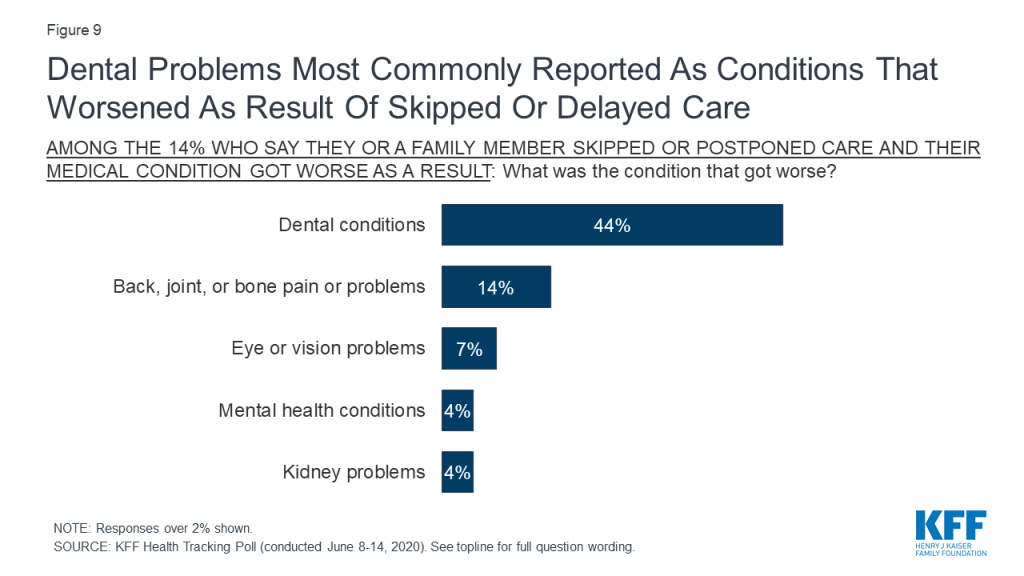
Overall, 27% of those who say they or a family member skipped or postponed care (14% of all adults) say that either they or their family member experienced a worsening medical condition as a result. When asked to name the condition that got worse, responses reflect the type of care that people report skipping or postponing, with by far the most common response being dental problems, named by 44% of those who say their own or a family member’s condition got worse after skipping care. Other responses include back, joint, or bone pain or problems (mentioned by 14% of those who say a condition got worse), eye or vision problems (7%), mental health conditions (4%), and kidney problems (4%). Since much of the care that people report skipping or delaying is in the form of routine check-ups and preventive screenings, it may be several months before the effects are recognized in terms of delayed diagnoses or missed opportunities for early treatment of cancers or other conditions.
When asked about the details behind their reasons for skipping or postponing care amid the coronavirus pandemic, large shares report that the doctor’s office or facility was closed or offering limited appointments (82% of those who say they or a family member missed out on care, or 43% of all adults). About half (53%) of those who say they or a household member skipped care due to coronavirus (27% of all adults) say that they felt unsafe vising a doctor’s office or other medical facility during the outbreak. Far fewer (11% of those who say they or a family member missed care due to coronavirus, or 6% of all adults) cite cost or affordability concerns as a driving factor. While this question was asked specifically of those who said they skipped or delayed care because of the coronavirus, previous KFF surveys have found that prior to the pandemic, about half of adults said that they or a household family member had put off or skipped some sort of health care or dental care in the past year because of the cost.

Similar to results from the May 2020 KFF Health Tracking Poll, most of those who say they or a family member skipped or postponed care due to the pandemic say they expect to get the care relatively soon, with seven in ten saying they expect to get the care within the next 3 months. Indeed, with many states easing social distancing restrictions, a third (34%) of those who say they or a family member skipped or delayed care due to coronavirus expect to get care in the next month and 7% say they have already gotten the care that was delayed. Very few (2%) say they don’t expect to get the care that was skipped or postponed.
In the midst of the coronavirus pandemic, an economic downturn, and weeks of protests against racism and police brutality, the latest KFF Tracking Poll looks ahead to the presidential election in November and examines how voters view the biggest problems facing the country, and which presidential candidate they trust most to handle them. Partisanship has a heavy hand in voters’ views when asked to say in their own words what they think is the biggest problem facing the country, with responses like “President Trump” (named by 17% of registered voters, including 31% of Democrats and 18% of independents), “political polarization” (named by 8% of voters), and “Democrats/liberals/the political left” (named by 7% of voters, including 19% of Republicans and 5% of independents) appearing among top responses to an open-ended question. Several of the issues driving recent news also appear among voters’ list of top problems, including racism and race relations (12% of voters, 20% of Democrats), coronavirus (7%), and the economy and unemployment (5%).
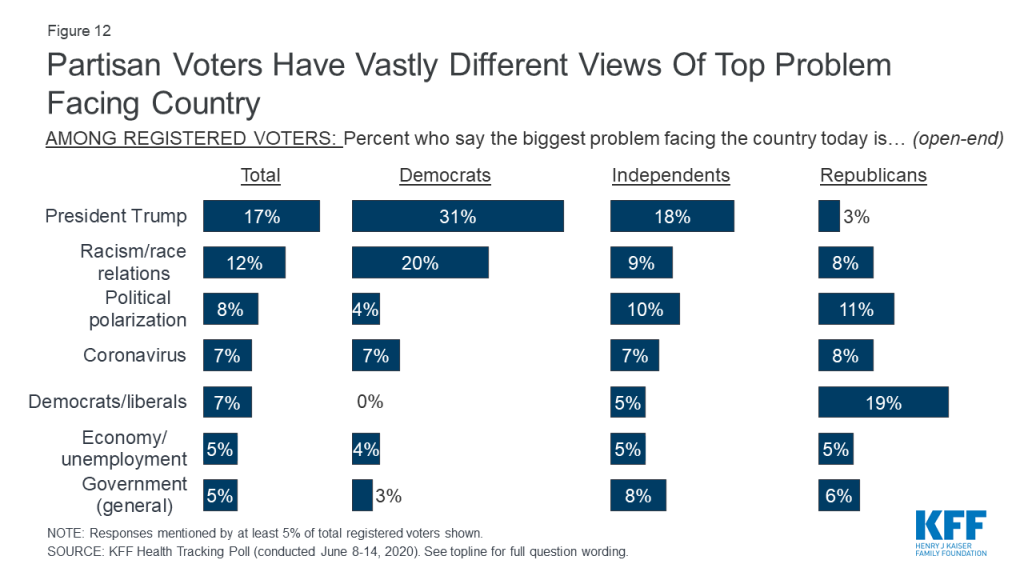
This month’s poll also takes a look at the critical group of swing voters who have not yet made up their minds about their vote for president in November. At least one in ten swing voters offer racism and race relations (15%), President Trump (10%), and political polarization (10%) as the biggest problems facing the country.
Defining Swing Voters
In this month’s poll, 30% of registered voters say they are “definitely going to vote for President Trump” and 37% say they are “definitely going to vote for Joe Biden.” Overall, 29% are defined as “swing voters,” including those who say they are undecided in their 2020 vote choice (7%) or are “probably” going to vote for President Trump (8%) or Democratic nominee Joe Biden (14%) but have not made up their minds yet.

When asked which candidate they trust to do a better job of dealing with various issues, more voters say they trust Joe Biden than Donald Trump in a variety of areas. This includes a roughly ten percentage point gap in favor of Biden on which candidate they trust to do a better job maintaining law and order (51% trust Biden vs. 41% trust Trump) and the coronavirus outbreak (50% vs. 41%). There are even larger gaps in favor of Biden on issues including health care (53% vs. 38%), police violence (55% vs. 36%), and race relations (58% vs. 34%). When it comes to handling the economy, similar shares of voters trust President Trump (49%) as trust Biden (45%).
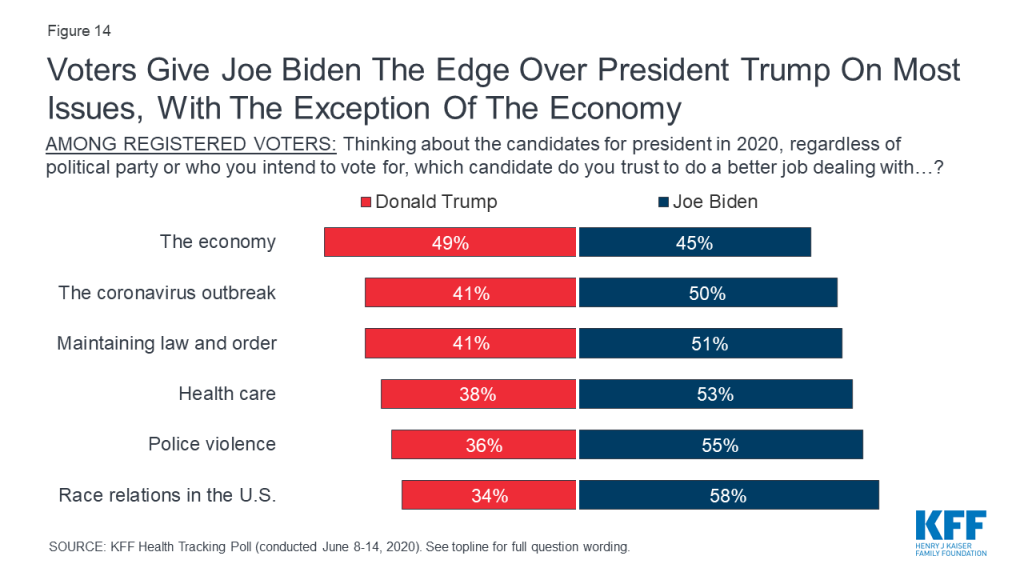
Not surprisingly, large majorities of voters from each political party say they trust their own party’s candidate to do a better job dealing with each of the issues tested in the poll. Among independent voters, Joe Biden has the clear edge over President Trump on trust to handle race relations (58% vs. 31%), police violence (54% vs. 35%), and health care (54% vs. 37%). Independent voters are more divided on which candidate they trust to do a better job on the economy (51% trust President Trump compared to 40% who trust Joe Biden) and to handle maintaining law and order (46% trust Joe Biden and 42% trust President Trump).
| Table 1: Among voters, partisans trust their party’s candidate to do a better job dealing with each of the issues compared to the other party’s candidate. | |||
| Percent of registered voters who trust each candidate to a better job dealing with each of the following: | Democratic voters | Independent voters | Republican voters |
| The economy | |||
| Donald Trump | 14% | 51% | 90% |
| Joe Biden | 81 | 42 | 8 |
| Maintaining law and order | |||
| Donald Trump | 6 | 42 | 87 |
| Joe Biden | 91 | 46 | 9 |
| The coronavirus outbreak | |||
| Donald Trump | 8 | 41 | 84 |
| Joe Biden | 86 | 49 | 10 |
| Health care | |||
| Donald Trump | 5 | 37 | 84 |
| Joe Biden | 91 | 54 | 11 |
| Police violence | |||
| Donald Trump | 4 | 35 | 76 |
| Joe Biden | 91 | 54 | 15 |
| Race relations in the U.S. | |||
| Donald Trump | 5 | 31 | 74 |
| Joe Biden | 91 | 58 | 18 |
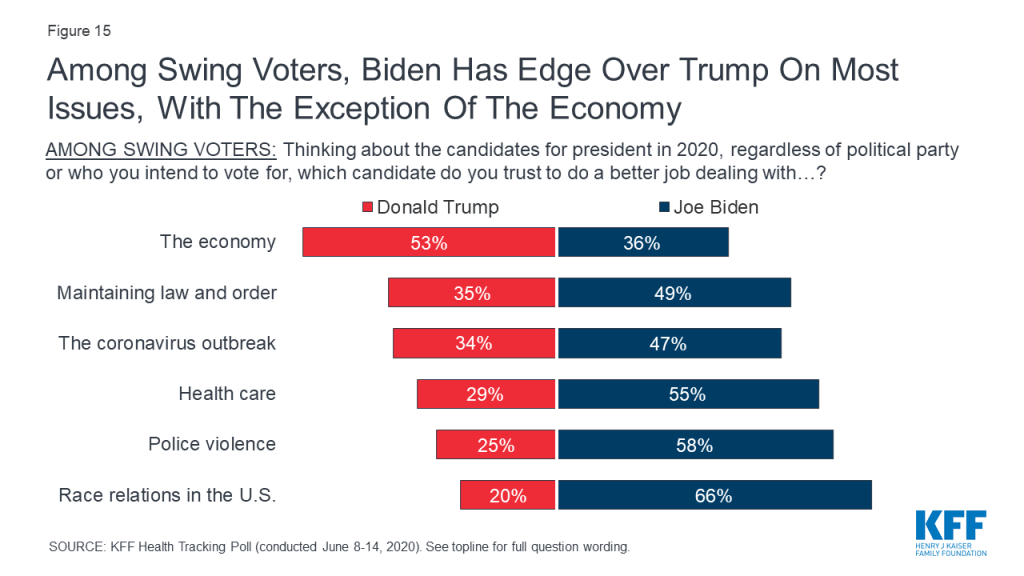
Among swing voters who are yet to make up their minds, a slight majority (53%) trust Donald Trump to do a better job dealing with the economy (compared to 36% who trust Joe Biden). However, they are more likely to trust Joe Biden than to trust Donald Trump to do a better job dealing with all other issues tested, including majorities who prefer Joe Biden to better deal with race relations (66% vs. 20%), police violence (58% vs. 25%), health care (55% vs. 29%).
This KFF Health Tracking Poll was designed and analyzed by public opinion researchers at the Kaiser Family Foundation (KFF). The survey was conducted June 8th-14th, 2020, among a nationally representative random digit dial telephone sample of 1,296 adults ages 18 and older, living in the United States, including Alaska and Hawaii (note: persons without a telephone could not be included in the random selection process). The sample included 291 respondents reached by calling back respondents that had previously completed an interview on the KFF Tracking poll at least nine months ago. Computer-assisted telephone interviews conducted by landline (297) and cell phone (999, including 719 who had no landline telephone) were carried out in English and Spanish by SSRS of Glen Mills, PA. To efficiently obtain a sample of lower-income and non-White respondents, the sample also included an oversample of prepaid (pay-as-you-go) telephone numbers (25% of the cell phone sample consisted of prepaid numbers) as well as a subsample of African American respondents who had previously completed interviews on the SSRS Omnibus poll (n=86). Both the random digit dial landline and cell phone samples were provided by Marketing Systems Group (MSG). For the landline sample, respondents were selected by asking for the youngest adult male or female currently at home based on a random rotation. If no one of that gender was available, interviewers asked to speak with the youngest adult of the opposite gender. For the cell phone sample, interviews were conducted with the adult who answered the phone. KFF paid for all costs associated with the survey.
The combined landline and cell phone sample was weighted to balance the sample demographics to match estimates for the national population using data from the Census Bureau’s 2018 American Community Survey (ACS) on sex, age, education, race, Hispanic origin, and region along with data from the 2010 Census on population density. The sample was also weighted to match current patterns of telephone use using data from the January- June 2019 National Health Interview Survey. The weight takes into account the fact that respondents with both a landline and cell phone have a higher probability of selection in the combined sample and also adjusts for the household size for the landline sample, and design modifications, namely, the oversampling of prepaid cell phones and likelihood of non-response for the re-contacted sample. All statistical tests of significance account for the effect of weighting.
The margin of sampling error including the design effect for the full sample is plus or minus 3 percentage points. Numbers of respondents and margins of sampling error for key subgroups are shown in the table below. For results based on other subgroups, the margin of sampling error may be higher. Sample sizes and margins of sampling error for other subgroups are available by request. Note that sampling error is only one of many potential sources of error in this or any other public opinion poll. Aduts of all racial and ethnic groups, including Asian, Pacific Islander, Native American, are included in the total, however only groups with sufficient numbers of responses to ensure statistical validity are broken out for individual analysis. Due to an inadvertent rounding error, an earlier version of this topline initially reported the net percentage of adults who attended a protest against police violence/in support of Black Lives Matter in Q14b/Q15 Combo Table as 10%. Kaiser Family Foundation public opinion and survey research is a charter member of the Transparency Initiative of the American Association for Public Opinion Research.
| Group | N (unweighted) | M.O.S.E. |
| Total | 1,296 | ± 3 percentage points |
| Registered voters | 1,094 | ± 4 percentage points |
| Party Identification | ||
| Democrats | 405 | ± 6 percentage points |
| Republicans | 305 | ± 7 percentage points |
| Independents | 465 | ± 5 percentage points |
| Race/Ethnicity | ||
| White | 811 | ± 4 percentage points |
| Black | 211 | ± 9 percentage points |
| Hispanic | 177 | ± 8 percentage points |
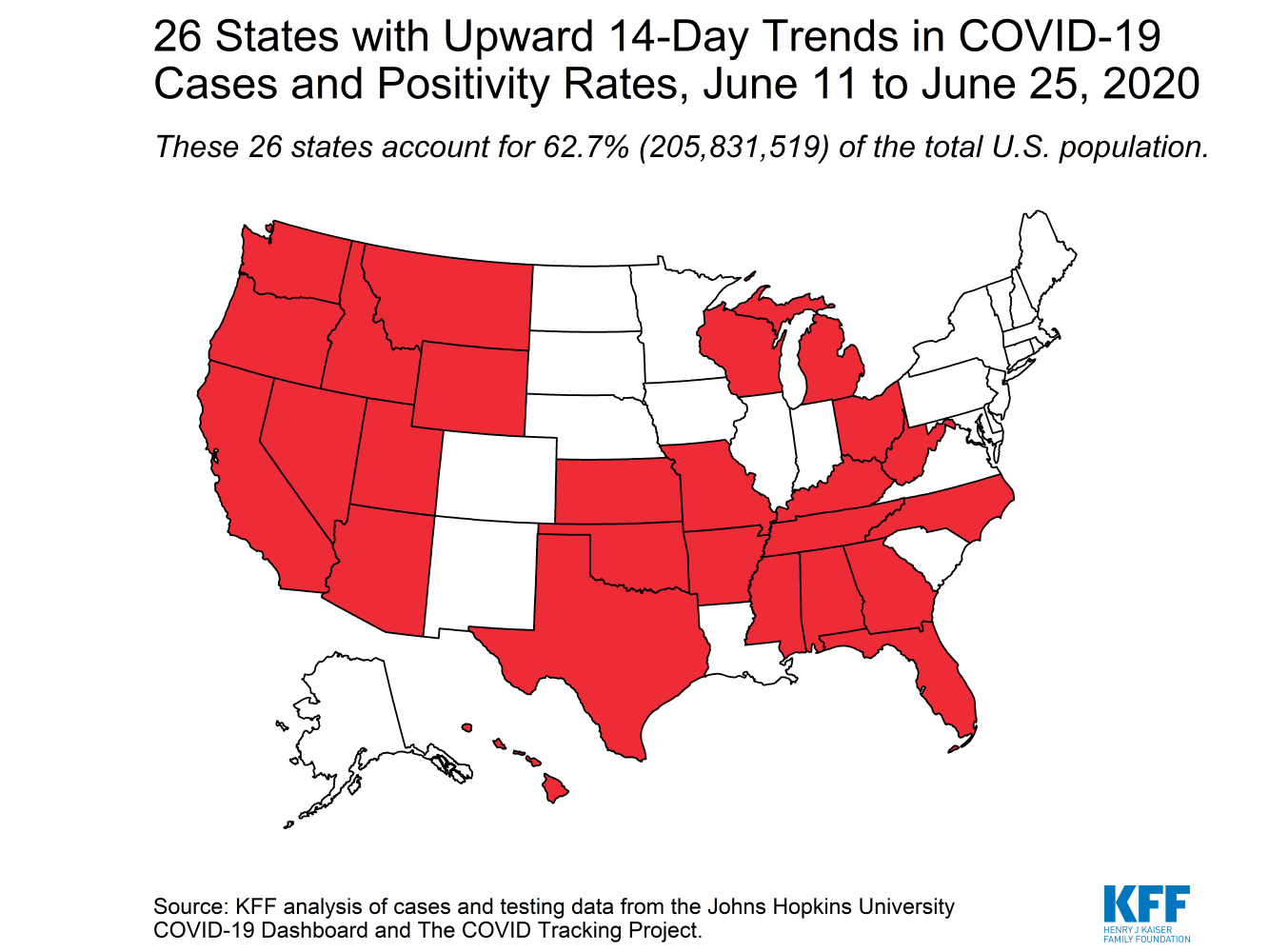
KFF analysis of cases and testing data from the Johns Hopkins University COVID-19 Dashboard and The COVID Tracking Project.
About 4.7 million uninsured adults could gain eligibility for Medicaid by 2021 if the 14 remaining non-expansion states were to expand Medicaid under the Affordable Care Act, a new KFF analysis finds.
That figure includes an estimated 2.8 million adults who already were uninsured prior to the coronavirus pandemic and would fall in the “coverage gap” – meaning they have incomes too high to qualify for Medicaid but too low for ACA marketplace subsidies – as well as 1.9 million more people who are at risk of losing health insurance due to job loss during the pandemic and otherwise would end up in the coverage gap.
An additional 3.3 million adults could become newly eligible for Medicaid coverage instead of ACA marketplace coverage if the remaining 14 states expanded Medicaid. Medicaid is more comprehensive than marketplace coverage and the federal government would pay ninety percent of the bill but that would require additional state expenditures.
Even prior to the pandemic, the potential for covering millions of uninsured people had become the focus of political debate in a number of non-expansion states, including ballot initiatives in Missouri and Oklahoma as well as debate in North Carolina and Kansas. The COVID-19 crisis highlights the implications for the uninsured in states that have not expanded. That is partly due to increased health risks, but also because some people who lose income, jobs and potentially employer-sponsored health insurance amid the pandemic may lack an affordable coverage option that protects against catastrophic health costs and facilitates access to care.
The current economic downturn is the first during which the ACA, including the Medicaid expansion, will be in place as a safety net for people losing their jobs and health insurance. Without it, many more people would likely end up uninsured as the U.S. moves through a recession.

San Francisco, CA, June 25, 2020 – With in-person health services limited due to COVID-19, Greater Than AIDS, a public information initiative of KFF, and Walgreens today announced a new program to provide 10,000 OraQuick® In-Home HIV Test kits to support expanded testing options in high-need areas. Local health agencies and community-based organizations will distribute the FDA-approved, self-administered tests at no cost to those unable to get tested in person.
Just ahead of the 25th anniversary of National HIV Testing Day (June 27), the announcement comes at a critical time with the Centers for Disease Control and Prevention (CDC) estimating that HIV testing is down 50 to 70 percent since February.
“As COVID-19 continues, we are seeing how it threatens other health responses,” said Tina Hoff, a senior vice president at KFF, which directs Greater Than AIDS. “This program aims to support frontline HIV service organizations as they transition to new ways of providing care during these difficult times.”
Walgreens is providing a donation for the purchase of 9,000 OraQuick HIV test kits with an additional 1,000 donated by OraSure Technologies, Inc., the manufacturer of the rapid oral swab HIV self-tests. KFF, through Greater Than AIDS, is managing distribution of the test kits to community partners.
“While HIV testing efforts may look different than in years past, we’re honored to collaborate with Greater Than AIDS in our 10th year of working together to highlight the critical role testing plays in prevention and care,” said Luke Sauter, vice president, specialty pharmacy, Walgreens. “Walgreens continues to advocate for HIV testing, education and care in the communities we serve with over 3,000 HIV-trained specialists in our stores.”
A record 325+ community partners, including health departments and HIV service organizations, in 215 cities in 47 states had signed on to provide free HIV testing in Walgreens stores across the country as part of the 2020 Greater Than AIDS/Walgreens National HIV Community Partnership when the in-store activation was put on hold due to COVID-19. These community partners — including those in the 48 counties in the Federal Ending the HIV Epidemic: A Plan for America — will be prioritized to receive the free HIV self-tests through this program.
The Food and Drug Administration (FDA) recently issued new information about the OraQuick In-Home HIV Test to support wider use, and a Dear Colleague Letter from the CDC in May encourages offering HIV self-testing to PrEP clients during COVID-19. Quarterly HIV testing is required as part of the prescribing protocols for PrEP, the HIV prevention pill.
“When it comes to eradicating HIV, the first step is to know your HIV status. On this year’s National HIV Testing Day, we are honored to work with Greater Than AIDS and Walgreens to provide OraQuick In-Home HIV Tests to allow testing at home or wherever is convenient,” said Stephen S. Tang, President and Chief Executive Officer of OraSure Technologies. “COVID-19 has interrupted so much of ‘normal’ life. Let’s make sure it doesn’t halt the fight against HIV/AIDS.”
Greater Than AIDS and Walgreens will also provide community partners with informational materials and digital promotions to support awareness and outreach.
For more about the Greater Than AIDS/Walgreens National HIV Community Partnership and other efforts to expand HIV testing, go to: greaterthan.org/walgreens.
About Greater Than AIDS
Greater Than AIDS is a leading national public information response from KFF focused on communities most affected in the U.S. Through targeted media messages and community outreach, Greater Than AIDS and its partners works to increase knowledge, reduce stigma and promote actions to stem the spread of the disease.
Since 2011, the Greater Than AIDS/Walgreens National HIV Community Partnership has joined with health departments and HIV service organizations across the country to provide more than 57,000 free HIV tests in Walgreens stores in support of National HIV Testing Day (NHTD). In 2019, the Partnership accounted for more than three quarters of NHTD events reported by the CDC.
Filling the need for trusted information on national health issues. KFF (Kaiser Family Foundation) is a nonprofit organization based in San Francisco, California (not affiliated with Kaiser Permanente). KFF develops and runs its own policy analysis, journalism and communications programs, sometimes in partnership with major news organizations.
About Walgreens
Walgreens (walgreens.com), one of the nation’s largest drugstore chains, is included in the Retail Pharmacy USA Division of Walgreens Boots Alliance, Inc. (Nasdaq: WBA), a global leader in retail and wholesale pharmacy. Walgreens is proud to be a neighborhood health, beauty and retail destination supporting communities across the country, and was named to FORTUNE* magazine’s 2019 Companies that Change the World list. Approximately 8 million customers interact with Walgreens in stores and online each day. As of August 31, 2019, Walgreens operates 9,277 drugstores with a presence in all 50 states, the District of Columbia, Puerto Rico and the U.S. Virgin Islands, along with its omnichannel business, Walgreens.com. Walgreens also provides specialty pharmacy and mail services and offers in-store clinics and other health care services throughout the United States, most of which are operated by our health care strategic partners.
About OraSure Technologies
OraSure Technologies, Inc. (NASDAQ: OSUR) empowers the global community to improve health and wellness by providing access to accurate, essential information. Together with its wholly-owned subsidiaries, DNA Genotek, Diversigen, CoreBiome (now operating under the Diversigen brand) and Novosanis, OraSure provides its customers with end-to-end solutions that encompass tools, services and diagnostics. The OraSure family of companies is a leader in the development, manufacture, and distribution of rapid diagnostic tests, sample collection and stabilization devices, and molecular services solutions designed to discover and detect critical medical conditions. OraSure’s portfolio of products is sold globally to clinical laboratories, hospitals, physician’s offices, clinics, public health and community-based organizations, research institutions, government agencies, pharma, commercial entities and direct to consumers.
As the country grapples with the public health and economic consequences of the coronavirus pandemic, there has been a renewed focus on coverage options that may be available to individuals who lose income, jobs and potentially employer sponsored insurance (ESI). The Affordable Care Act (ACA) established new coverage options through Medicaid or subsidized coverage through ACA marketplaces. Millions of people are enrolled in or eligible for coverage through these new pathways. However, in states that do not expand Medicaid, many adults, including almost all childless adults, fall into a “coverage gap” because their incomes are above Medicaid eligibility limits but below the poverty level, which is the lower limit for Marketplace premium tax credits. As more people lose their jobs and accompanying ESI, more may fall into the coverage gap, particularly starting in 2021 after unemployment benefits expire for many who have lost their jobs and incomes are likely to drop below the minimum threshold for marketplace subsidies. This analysis estimates how many uninsured adults—including those uninsured even before the pandemic and those who could become uninsured as a result of it— could become eligible for Medicaid if states that have not yet expanded the program do so. Methods underlying the analysis are detailed in the methods section at the end of the brief. Key findings include the following:
In states that have not expanded Medicaid, many uninsured adults below poverty, including most childless adults, fall into a “coverage gap.” Under the ACA, Medicaid eligibility is extended to nearly all low-income individuals with incomes at or below 138 percent of poverty ($17,609 for an individual in 2020). While the Medicaid expansion was intended to be national, the June 2012 Supreme Court ruling essentially made it optional for states. As of May 2020, 14 states had not expanded their programs. Medicaid eligibility for adults in states that did not expand their programs is quite limited: the median income limit for parents in these states is just 41% of poverty, or an annual income of $8,905 for a family of three in 2020, and in nearly all states not expanding, childless adults remain ineligible. Further, because the ACA envisioned low-income people receiving coverage through Medicaid, it does not provide financial assistance to people below poverty for other coverage options. As a result, in states that do not expand Medicaid, many adults, including all childless adults, fall into a “coverage gap” of having incomes above Medicaid eligibility limits but below the poverty level, which is the lower limit for Marketplace premium tax credits.
Among adults uninsured even before the pandemic, an estimated 2.8 million poor uninsured adults would fall into the “coverage gap” that results from state decisions not to expand Medicaid by 2021. This number includes the 2.3 million in the coverage gap without accounting for the effects of the pandemic and an additional half a million individuals in non-expansion states who did not have insurance in early 2020 and are estimated to lose Marketplace eligibility by 2021 due to job losses. Individuals in the gap have income that is above current Medicaid eligibility but below the lower limit for Marketplace premium tax credits. Reflecting limits on Medicaid eligibility outside ACA pathways, most people in the coverage gap (81%) are adults without dependent children. Adults left in the coverage gap by 2021 are concentrated in the South, which accounts for 9 out of 14 states that have not expanded. Of those in the gap, one-third live in Texas, 18 percent in Florida, 12 percent in Georgia, and eight percent in North Carolina. There are no uninsured adults in the coverage gap in Wisconsin because the state is providing Medicaid eligibility to adults up to the poverty level under a Medicaid waiver.
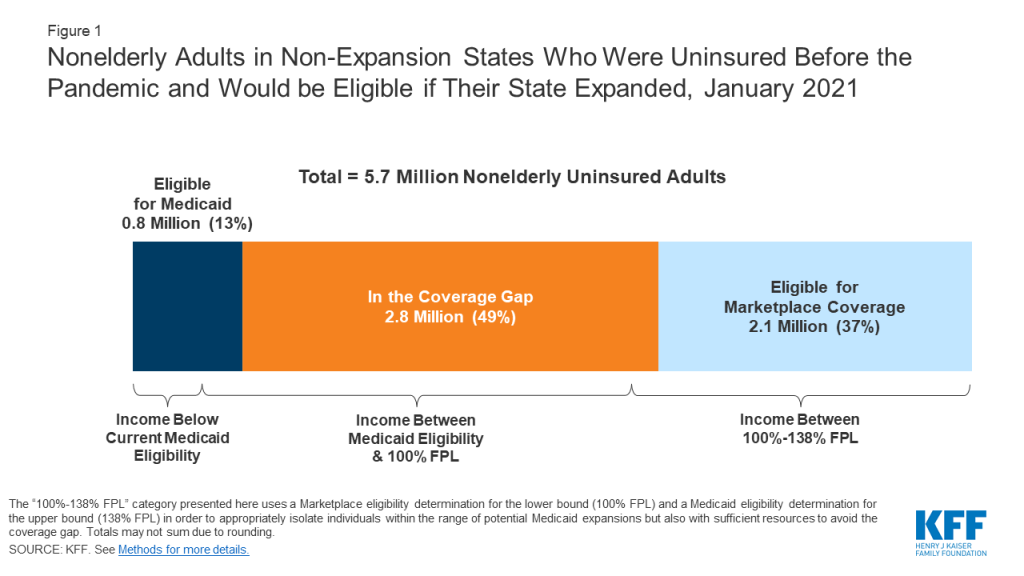
If states that are currently not expanding their programs adopt the Medicaid expansion, all of the 2.8 million adults in the coverage gap would gain Medicaid eligibility (Table 1 and Figure 1). In addition, 2.1 million uninsured adults with incomes between 100 and 138% of poverty (most of whom are currently eligible for Marketplace coverage) would also gain Medicaid eligibility, substantially lowering the out-of-pocket costs for premiums and cost-sharing they would otherwise face. A smaller number (about 757,000) of uninsured adults in non-expansion states are already eligible for Medicaid under eligibility pathways in place before the ACA. If all states expanded Medicaid, those in the coverage gap and those who are instead eligible for Marketplace coverage would bring the number of nonelderly uninsured adults eligible for Medicaid to about 5.7 million people in the fourteen current non-expansion states. The potential scope of Medicaid varies by state.
The economic consequences of the coronavirus pandemic have led to historic level of job loss in the United States. Social distancing policies required to address the crisis have led many businesses to cut hours, cease operations, or close altogether. Between March 1st and May 2nd, 2020, more than 31 million people filed for unemployment insurance and an estimated nearly 78 million people lived in a family in which someone lost a job. Most people in these families (61%, or 47.5 million) were covered by ESI prior to job loss. Previous KFF estimates showed that nearly 27 million people could lose ESI and became uninsured following job loss. In some cases, employers may be continuing health benefits for furloughed or laid off workers, but that will likely end if unemployment remains high. Some people in this group can elect to continue ESI for a period by paying the full premium (called COBRA continuation) or may become eligible for Medicaid or subsidized coverage through the ACA marketplaces. While the state unemployment insurance benefit payments and federal supplement available to most people mean few will fall into the coverage gap immediately, a larger number could find themselves in the gap after these benefits expire.
Nationally, coverage losses among people who previously had ESI and lost their jobs could lead an additional 1.9 million adults to fall into the coverage gap by January 2021. Recent analysis shows that by January 2021, when unemployment insurance (UI) benefits cease for most people, an estimated 1.9 million could fall into the coverage gap. People who lose ESI and find themselves in the coverage gap by January 2021 are concentrated in Georgia (21%), Texas (20%), and Florida (18%).
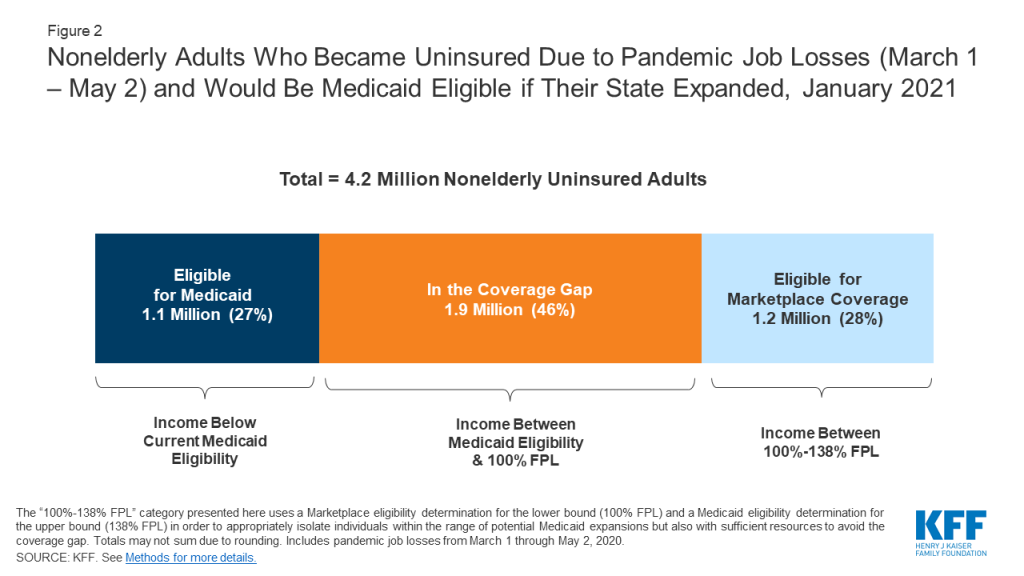
If all states adopted the expansion, 1.9 million newly uninsured adults who otherwise would fall into the coverage gap would instead be eligible for Medicaid (Figure 2 and Table 2). If all states adopted the expansion, these individuals would be eligible for Medicaid. In addition, an estimated 1.2 million individuals with incomes between 100-138% FPL who otherwise would be eligible for marketplace subsidies would also become eligible for Medicaid if all states expanded. Counting the 1.1 million adults in non-expansion states who are already eligible for Medicaid even without expansion (and whose eligibility would not change), the total number of newly-uninsured adults who could be eligible for Medicaid in non-expansion states would be 4.2 million.
In total, if non-expansion states expanded Medicaid under the ACA, about 4.7 million adults who would otherwise fall into the coverage gap by 2021 would gain eligibility (Table 3). An additional 3.3 million adults would become newly eligible for Medicaid coverage instead of marketplace coverage. Including the small number of currently eligible non-elderly adults in these states, the total reach of Medicaid among uninsured nonelderly adults in non-expansion states could be nearly 10 million.
Given the health risks facing all Americans right now, access to health coverage after loss of employment provides important protection against catastrophic health costs and facilitates access to care. This is the first economic downturn during which the ACA will be in place as a safety net for people losing their jobs and health insurance. Without it, many more people would likely end up uninsured as the U.S. heads into a recession. However, if all states adopted the expansion, more people would have options for affordable coverage and not fall into the coverage gap. These estimates show increases in eligibility but do not account for take-up or enrollment in coverage. Individuals currently in the coverage gap as well as those who may be newly eligible for coverage due to job loss may not know they are eligible for ACA coverage or may need assistance in applying to enroll in coverage. The federal government covers 90% of the cost of coverage for Medicaid expansion enrollees, leaving states with 10% of the expense, an amount that could grow if job losses increase. However, some research that pre-dates the pandemic shows that states may experience net budget savings following Medicaid expansion after accounting for resulting reductions in the cost of other state programs.
Methods
This analysis draws on KFF’s estimates of the number of adults that fall into the Medicaid coverage gap as well as ACA eligibility among people losing employer-sponsored insurance (ESI) due to the coronavirus pandemic. Detailed methods underlying both those analyses, both of which are based on the 2018 American Community Survey, are available via the links above. Notably, in contrast to previous coverage gap estimates, the estimates in this brief are based on estimated 2020 population. In order to estimate the 2020 population within each state, we linearly extrapolated 2020 state population estimates based on 2018 and 2019 population estimates from the U.S. Census Bureau to determine a population increase factor between 2018 and 2020 within each state. We then applied this multiplier to the weight of each individual in the microdata to approximate state population sizes in mid-2020 rather than mid-2018. Coverage gap numbers in this analysis also differ from previous KFF estimates in that they include people who, absent the pandemic and estimated related job loss/loss of income, were uninsured but eligible for marketplace premium subsidies; with the loss of jobs and income, they instead fall into the coverage gap.
Robin Rudowitz and Rachel Garfield are with KFF. Anthony Damico is an independent consultant.
| Table 1: Nonelderly Adults in Non-Expansion States Who Were Uninsured Before the Pandemic and Would be Medicaid Eligibleif Their State Expanded, January 2021 | ||||
| Newly Eligible for Medicaid if State Expands | ||||
| State | Total | Eligible for Medicaid under non-ACA Pathway | In the Coverage Gap(<100% FPL) | Eligible for Marketplace Coverage(100%-138% FPL**) |
| All Non-Expansion States | 5,679,000 | 757,000 | 2,802,000 | 2,119,000 |
| Alabama | 275,000 | 32,000 | 155,000 | 88,000 |
| Florida | 1,022,000 | 96,000 | 491,000 | 435,000 |
| Georgia | 656,000 | 105,000 | 342,000 | 208,000 |
| Kansas | 97,000 | 12,000 | 47,000 | 38,000 |
| Mississippi | 203,000 | 25,000 | 114,000 | 65,000 |
| Missouri | 255,000 | 27,000 | 134,000 | 94,000 |
| North Carolina | 457,000 | 56,000 | 234,000 | 167,000 |
| Oklahoma | 232,000 | 34,000 | 117,000 | 82,000 |
| South Carolina | 250,000 | 30,000 | 127,000 | 93,000 |
| South Dakota | 37,000 | 6,000 | 16,000 | 16,000 |
| Tennessee | 292,000 | 50,000 | 138,000 | 104,000 |
| Texas | 1,772,000 | 195,000 | 878,000 | 699,000 |
| Wisconsin* | 109,000 | 87,000 | – | 22,000 |
| Wyoming | 21,000 | N/A | 10,000 | 8,000 |
| NOTES: * Wisconsin provides Medicaid eligibility to adults up the poverty level under a Medicaid waiver. As a result, there is no one in the coverage gap in Wisconsin. ** The “100%-138% FPL” category presented here uses a Marketplace eligibility determination for the lower bound (100% FPL) and a Medicaid eligibility determination for the upper bound (138% FPL) in order to appropriately isolate individuals within the range of potential Medicaid expansions but also with sufficient resources to avoid the coverage gap. Totals may not sum due to rounding. N/A: Sample size too small for reliable estimate.SOURCE: KFF. See Methods for more details. | ||||
| Table 2: Nonelderly Adults in Non-Expansion States Who Became Uninsured Due to Pandemic Job Losses (March 1st thru May 2nd) and Would Be Medicaid Eligible if Their State Expanded, January 2021 | ||||
| Newly Eligible for Medicaid if State Expands | ||||
| State | Total | Eligible for Medicaid under Non-ACA Pathway | In the Coverage Gap(<100% FPL) | Eligible for Marketplace Coverage(100%-138% FPL**) |
| All Non-Expansion States | 4,225,000 | 1,127,000 | 1,924,000 | 1,174,000 |
| Alabama | 225,000 | 53,000 | 115,000 | 57,000 |
| Florida | 741,000 | 149,000 | 351,000 | 241,000 |
| Georgia | 802,000 | 209,000 | 398,000 | 195,000 |
| Kansas | 112,000 | 29,000 | 52,000 | 31,000 |
| Mississippi | 113,000 | 29,000 | 58,000 | 27,000 |
| Missouri | 242,000 | 50,000 | 119,000 | 73,000 |
| North Carolina | 367,000 | 86,000 | 178,000 | 104,000 |
| Oklahoma | 163,000 | 43,000 | 74,000 | 46,000 |
| South Carolina | 211,000 | 52,000 | 99,000 | 61,000 |
| South Dakota | 15,000 | N/A | 7,000 | 5,000 |
| Tennessee | 206,000 | 57,000 | 86,000 | 63,000 |
| Texas | 798,000 | 173,000 | 382,000 | 243,000 |
| Wisconsin* | 213,000 | 189,000 | – | 24,000 |
| Wyoming | 16,000 | N/A | N/A | N/A |
| NOTES: * Wisconsin provides Medicaid eligibility to adults up the poverty level under a Medicaid waiver. As a result, there is no one in the coverage gap in Wisconsin. ** The “100%-138% FPL” category presented here uses a Marketplace eligibility determination for the lower bound (100% FPL) and a Medicaid eligibility determination for the upper bound (138% FPL) in order to appropriately isolate individuals within the range of potential Medicaid expansions but also with sufficient resources to avoid the coverage gap. Totals may not sum due to rounding. N/A: Sample size too small for reliable estimate.SOURCE: KFF. See Methods for more details. | ||||
| Table 3: Nonelderly Adults in Non-Expansion States Who Were Uninsured Before the Pandemic or Lost ESI due to Pandemic and Would be Medicaid Eligible if Their State Expanded, January 2021 | ||||
| Newly Eligible for Medicaid if State Expands | ||||
| State | Total | Eligible for Medicaidunder Non-ACA Pathway | In the Coverage Gap(<100% FPL) | Eligible for Marketplace Coverage(100%-138% FPL**) |
| All Non-Expansion States | 9,904,000 | 1,884,000 | 4,727,000 | 3,293,000 |
| Alabama | 500,000 | 85,000 | 270,000 | 145,000 |
| Florida | 1,764,000 | 245,000 | 842,000 | 676,000 |
| Georgia | 1,458,000 | 315,000 | 740,000 | 403,000 |
| Kansas | 209,000 | 41,000 | 99,000 | 69,000 |
| Mississippi | 317,000 | 53,000 | 171,000 | 92,000 |
| Missouri | 497,000 | 77,000 | 253,000 | 167,000 |
| North Carolina | 825,000 | 142,000 | 411,000 | 271,000 |
| Oklahoma | 395,000 | 77,000 | 190,000 | 128,000 |
| South Carolina | 461,000 | 82,000 | 226,000 | 153,000 |
| South Dakota | 52,000 | 9,000 | 23,000 | 20,000 |
| Tennessee | 499,000 | 107,000 | 224,000 | 167,000 |
| Texas | 2,570,000 | 368,000 | 1,260,000 | 942,000 |
| Wisconsin* | 322,000 | 276,000 | – | 46,000 |
| Wyoming | 37,000 | 7,000 | 17,000 | 13,000 |
| NOTES: * Wisconsin provides Medicaid eligibility to adults up the poverty level under a Medicaid waiver. As a result, there is no one in the coverage gap in Wisconsin. ** The “100%-138% FPL” category presented here uses a Marketplace eligibility determination for the lower bound (100% FPL) and a Medicaid eligibility determination for the upper bound (138% FPL) in order to appropriately isolate individuals within the range of potential Medicaid expansions but also with sufficient resources to avoid the coverage gap. Totals may not sum due to rounding. N/A: Sample size too small for reliable estimate.SOURCE: KFF. See Methods for more details. | ||||
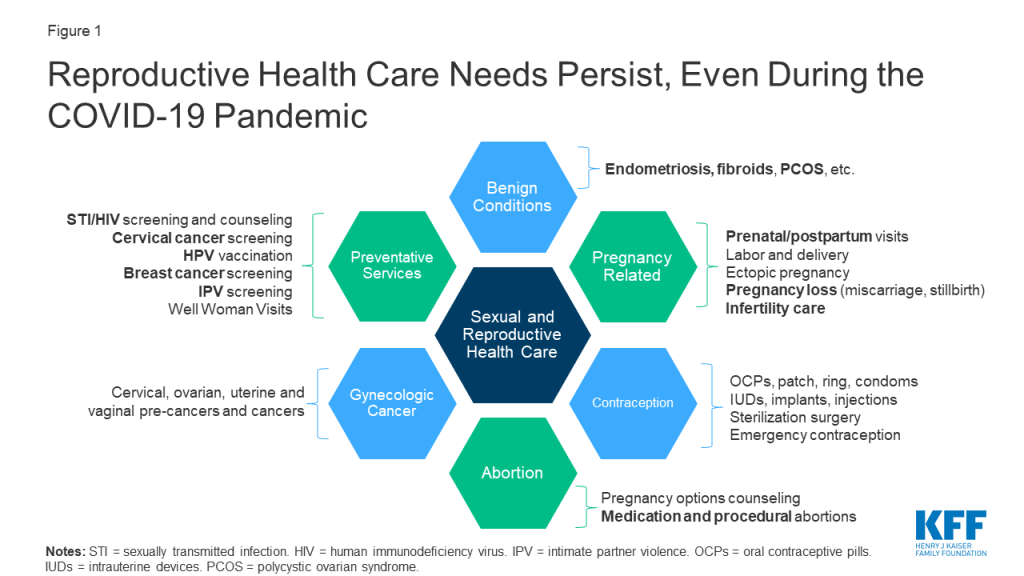
A new KFF brief outlines the potential impacts of delaying reproductive health care during the COVID-19 pandemic.
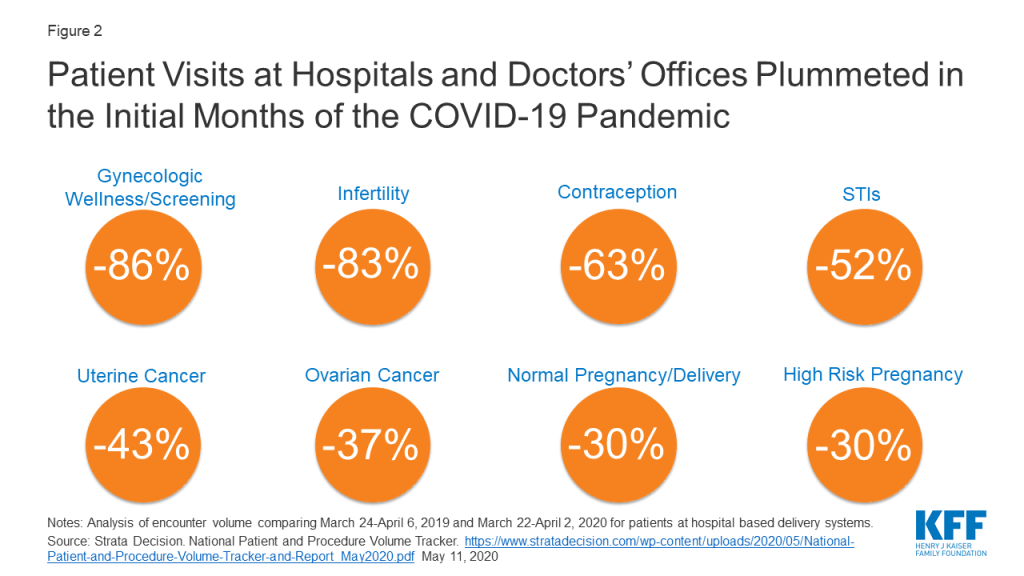
In order to reduce the risk of coronavirus exposure and preserve personal protective equipment, government agencies and professional health societies were tasked with providing guidance on which health care services to consider “essential” and which to consider “elective” and postpone. As a result, large declines in patient encounters have been observed within reproductive health care, particularly for preventive health services (e.g. cancer screening), infertility care, contraception and sexually transmitted infections. While many of the conditions deemed “non-essential” are not life-threatening, they can result in significant morbidity and poor quality of life if delayed.
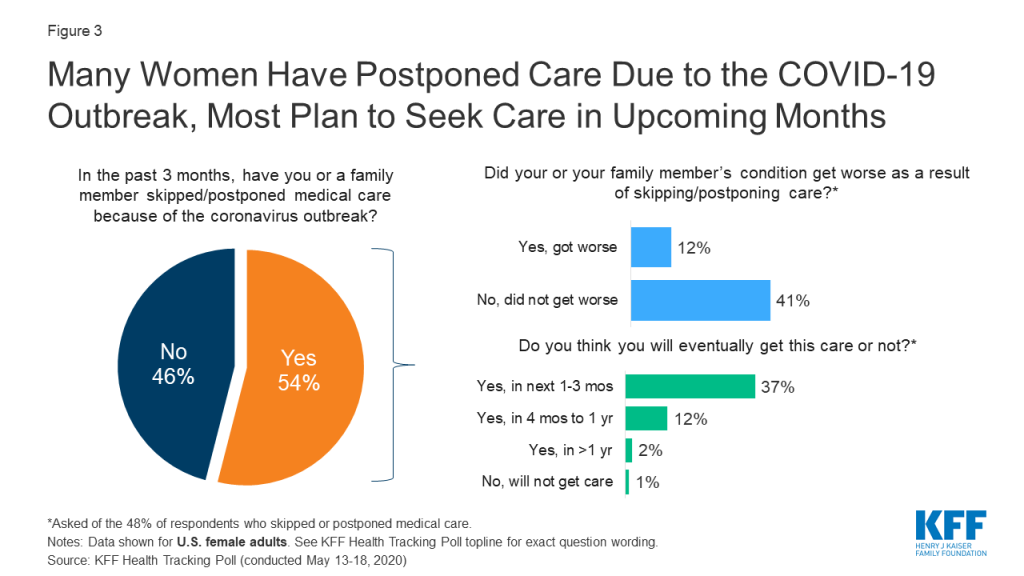
Recent KFF polling data finds that more than half (54%) of US women reported they or a family member have skipped or postponed medical care due to the coronavirus outbreak. As states begin to reopen and health systems resume more in-person care, many women said they plan to seek care in the next one to three months. However, policymakers and providers may have to again contend with deciding which services can be delayed in the event of future surges of COVID-19 cases.
Key Takeaways
Amidst the current COVID-19 public health emergency, patients continue to face many of the same sexual and reproductive health issues they always have (Figure 1). Each year in the U.S. there are nearly 47 million women using contraception, 20 million new cases of sexually transmitted infections (STIs), 3.8 million births, 1 million pregnancy losses, 6.5 million women with endometriosis, 862,000 abortions, and 94,000 women newly diagnosed with gynecologic cancer. This is not to mention the millions of patients each year who access preventive services for reproductive health (e.g. STI and cancer screenings, HPV vaccinations). The difference now, however, is that much of this care is being delayed due to the COVID-19 emergency.
After decades of public health initiatives urging people to not delay or forgo many types of care, we are now experiencing a paradigm shift in response to COVID-19. Facing extraordinary circumstances, the U.S. government, states, health centers and providers have been tasked with determining which health care services are “essential,” and which are “elective,” or “non-urgent” thereby influencing what care is available to patients at this time. Beginning in March 2020, guidance from the CDC urged providers to postpone non-urgent outpatient visits and preventive health care, if it was not able to be performed via telehealth. Additionally, both the CDC and CMS recommended postponing “elective” and “non-essential” surgeries and procedures, using a tiered framework that balanced how severe and time-sensitive a patient’s needs were, with the tradeoffs associated with in-person care (e.g. coronavirus exposure, depletion of PPE). As of May 21, 2020, the CDC removed said language regarding delaying non-urgent visits and “elective” procedures from their published guidance. During that time however, dramatic decreases were seen in patients seeking reproductive health care, and health care more generally.
A study by Strata Decision Technology of 228 hospitals across 40 states found patient encounters for various reproductive health services showed large decreases compared to the year prior (Figure 2). The largest drops in patient volume were seen for preventive health services, infertility care, and contraception, with smaller, but still sizable decreases in encounters for gynecologic cancer and pregnancy. A study by IQVIA similarly showed an 83% decline in the number of pap smears in April compared to February 2020.
Various medical societies have issued guidance to help providers decide which reproductive health services necessitate prompt, in-person care, which may be suitable for telehealth, and which may be delayed altogether (Appendix). In general, most pregnancy-related services have been considered essential (prenatal care, labor and delivery, ectopic pregnancies, pregnancy loss, abortions), as well as most treatments for gynecologic cancer. Meanwhile, some methods of contraception that require in-person care (e.g. sterilization, IUD removal), as well as most preventive health care (e.g. STI and cervical cancer screening, HPV vaccines) have been recommended to be postponed. The Society for Family Planning’s guidelines emphasize use of telehealth to assess if an in person visit is required, or if contraception can be provided and managed through a virtual visit. That said, recommendations for care have been changing rapidly during the course of the COVID-19 emergency; for example, as of March 2020, the American Society for Reproductive Medicine recommended cancelling all new infertility treatments and diagnostic procedures, but relaxed these recommendations as of May 2020.
Some states have specifically deemed certain reproductive health services essential or non-essential. This is most common when it comes to abortion services. At least 12 states (AK, AL, AR, IA LA, MI, OH, OK, TN, TX, WV) issued policies to suspend abortion during the COVID-19 emergency; most bans are not in effect however due to ongoing or resolved litigation, or states lifting restrictions on “non-essential” services. Meanwhile, 5 states (MA, NJ, NM, VA, WA) included language in their executive orders or public health guidance to clarify that abortion is considered essential, or to explicitly protect the “full suite of family planning services.”
For pregnancy-related care, New Mexico and Tennessee have specifically excluded pregnancy-related visits or procedures from their definition of “non-essential” care. Regarding gynecologic cancer, a handful of states clarify that postponement of elective procedures does not apply if there is a risk of cancer advancing or spreading (AR, IA) or if the treatment is to remove a cancerous tumor (FL, NM, TN, WA). Meanwhile, Massachusetts specifically included colposcopy (to detect cervical cancer) and endometrial biopsies (to detect uterine cancer) as examples of “nonessential, elective” procedures.
More commonly however, states have not specified certain procedures or diagnoses in their executive orders regarding COVID-19. Rather, states more broadly defined “non-essential” procedures as those which can be safely postponed for a certain amount of time without risking serious harm to the patient. As of mid-April 2020, 32 states had issued formal orders to postpone so-called “elective” and “non-essential” surgeries and procedures, but by mid-May 2020, the majority had rolled back these restrictions to allow some procedures to continue, under certain conditions. At the federal level, in June 2020 CMS recommended that patients should not further delay preventive care such as cancer screenings and vaccinations. As the COVID-19 pandemic evolves in the months to come, some regions with recurrent outbreaks of SARS CoV2 will likely have to consider reinstating restrictions on “non-essential” services.
For years, public health officials and providers have urged the public to actively seek reproductive health care, as we know the negative health consequences that may result from not doing so. We know that limited access to contraception puts women at risk for unintended pregnancies, while undetected and untreated STIs can lead to complications like infertility, pelvic inflammatory disease and ectopic pregnancies. We know that forgoing prenatal care may result in poor maternal and infant outcomes, and that halting time-sensitive fertility care may reduce the chance for family building for the 10-15% of couples with infertility. Meanwhile, untreated conditions like endometriosis and fibroids can result in significant morbidity, and delays in gynecologic cancer diagnosis and treatment could mean cancer progression and increased mortality. We also know that even when reproductive health conditions are not life-threatening, they threaten to reduce one’s quality of life and overall wellbeing, and therefore warrant care and attention.
Health systems and providers have been forced to adapt to the evolving landscape of the coronavirus pandemic, and most have quickly adopted telehealth solutions in order to continue to see patients; many reproductive health care services can be delivered via telehealth, including prescription of hormonal contraception and many prenatal/postpartum visits. There have also been innovations during the pandemic in using telehealth for medication abortion, and to assist patients in IUD self-removal and self-administered Depo-Provera injections. That said, several services still require in-person care, including several of the most effective methods of contraception (e.g. sterilization, IUD and implant placement), several preventive services (e.g. HPV vaccination, cervical cancer screening), procedural abortions, and the host of procedures and surgeries used to diagnose and treat many gynecologic conditions (e.g. infertility, endometriosis, gynecologic cancers). These services requiring in-person attention are at risk of delay during the COVID-19 pandemic.
Data from the KFF May 2020 Health Tracking Poll reveal more than half of US women reported they or a family member have skipped or postponed medical care due to the coronavirus outbreak. A majority of those who delayed care also reported the condition did not get worse in that time, and that they planned to seek care within the next 1 to 3 months (Figure 3). Therefore, it seems as if most plan to return to care in the near future. That said, many people also remain fearful of accessing in-person health services; a Gallup poll (conducted March 28 to April 2, 2020) showed 88% of US women reported being very or moderately concerned about being exposed to the novel coronavirus at a doctor’s office or hospital; this dropped to 70% when the poll was conducted again from May 14 to 24, 2020. Patients may also forgo care due to cost, as over half of the workforce has lost their jobs or wages, and some may have subsequently lost their health insurance.
When and if patients decide to seek in-person care, it is important to note that providers may be functioning at reduced clinic capacity as compared to before the coronavirus outbreak. A survey of primary care providers from 48 states (conducted May 22-26, 2020) revealed that many practices are struggling financially; 14% of provider’s practices were still temporarily closed, and 77% reported net-negative revenues in April 2020. Many have had to furlough or layoff staff, and were uncertain if they would remain open in the weeks to come. It remains to be seen if the financial impact to medical practices will still allow these sites to function at pre-COVID-19 patient volumes in the months to come. This may be particularly difficult for publicly-funded family planning clinics, given existing funding challenges related to changes in Title X.
Even amidst the coronavirus pandemic, millions of patients continue to need quality sexual and reproductive health care in the U.S. While most providers have shifted to telehealth in an attempt to maintain care, many reproductive health conditions that have been deemed “non-essential” require in-person evaluation and treatment, and therefore patients have experienced delays in this care. As the U.S. looks to move into the next phase of the COVID-19 emergency, states and health systems are deciding when it is appropriate to resume provision of these in-person, “non-essential” health care services. While many have loosened restrictions, a second wave of the pandemic or infection hotspots may force providers again to restrict in-person care. As public leaders and officials monitor the capacity of our health systems to respond patient needs during the COVID-19 pandemic, they will also continue to be faced with difficult decisions regarding whether again to delay many reproductive health care services that are critical to women’s health.
| What services have been deemed essential by leading medical societies? | |
| Health Care Need | Statements by leading medical societies |
| Pregnancy | Prenatal care: considered essential, but may consolidate number of visits (ACOG). Prenatal ultrasound and fetal surveillance should continue as medically indicated, but consider postponing/canceling some testing or examinations if risk outweighs benefits. (ACOG) Amniocentesis may be delayed a few weeks (ACS) |
| Cesarean sections: emergent, do not delay (ACS) | |
| Postpartum care: consider expediting discharge after delivery (ACOG) | |
| Ectopic pregnancy: emergent, do not delay (ACS) | |
| Contraception | Contraception considered essential health care (ACOG, SFP) |
| Prescription methods: use telehealth to conduct visits and prescribe (AOCG) | |
| IUDs and Implants: continue to offer in-person insertion when possible, postpone removals (ACOG) | |
| Sterilization: Procedures can be delayed several months (ACS). Considered elective, unless done during a cesarean section (ACOG) | |
| Emergency contraception: continue to provide prescriptions and counseling on over-the-counter methods (ACOG) | |
| Abortion | ACOG opposes COVID-19 responses that cancel or delay abortion procedures. Delaying abortions may cause significant harm (ACS). |
| Infertility | Infertility procedures can be delayed several months (ACS) Initial recommendation to suspend new fertility treatment/diagnostic procedures, unless treatment cycle already started. Some care now resuming (ASRM Update 1, Update 4) |
| Pregnancy Loss | Emergent, do not delay (ACS) |
| Gynecologic Cancer | Most gynecologic cancer procedures considered non-elective (SGO) Surgery for gynecologic cancer delay may cause significant harm (ACS). |
| Diagnostic evaluations for uterine/cervical cancer may be delayed a few weeks to months (ACS, ASCCP) | |
| Benign Gynecologic Conditions | Surgeries for fibroids, endometriosis, pelvic pain, and benign ovarian masses can be delayed several months (ACS) |
| Recommended Preventative Care | (e.g. STI and cervical cancer screenings, HPV vaccination)Potentially defer until after COVID-19 outbreak (ACOG). Reduce or postpone visits for preventative services (AAFP) |
| Notes: Info current as of 5/13/2020. Recommendations may change as COVID-19 emergency evolves.ACOG = American College of Obstetricians and Gynecologists; ASRM = American Society for Reproductive Medicine; ACS = American College of Surgeons; AAFP = American Academy for Family Medicine (AAFP); SGO = Society of Gynecologic Oncology; SFP = Society of Family Planning. | |