The Status of Funding for Zika: Comparing the President’s Request and Congressional Proposals
Zika, a mosquito-transmitted infection that in pregnant women can cause microcephaly as well as other serious birth defects, has recently become a global challenge, and with the first cases of local transmission now reported in the U.S., a domestic one as well. No new funding for Zika has yet been appropriated by Congress. While the President requested emergency funding from Congress to address Zika last February, it has yet to approve any funding and its own proposals differ significantly from the President’s. As lawmakers return from summer recess and consider funding for the Zika virus again, a new issue brief from the Kaiser Family Foundation provides a landscape of where the debate stands and compares the President’s emergency Zika request to Congressional proposals thus far.
The brief highlights that the President’s emergency request to Congress is significantly above the amount proposed in three Congressional bills. The proposals also differ by whether the funding would be “new” appropriations or entirely offset by changes to prior appropriations, the period of time for which funds would be available, the activities supported, and restrictions on how the funding would be utilized. In all proposals, the Department of Health and Human Services would receive the majority of resources, while the State Department and U.S. Agency for International Development would receive the remaining funding.
Key Implementers of U.S. Global Health Efforts
Summary
To carry out global health efforts around the world, the U.S. government (USG) funds a wide range of implementing entities, including non-governmental organizations (NGOs), multilateral/international organizations, private sector organizations, educational institutions, and other governments. This brief provides an analysis of the implementing organizations that received U.S. global health funding from the U.S. Agency for International Development (USAID) in FY 2015. It helps to provide a more complete picture of key implementers of U.S. government global health efforts, building on earlier KFF analyses that focused on NGOs only.1 It finds that:
- In FY 2015, 773 organizations received $6.65 billion to implement global health programs in 90 countries around the world.
- Funded activities spanned all 9 major program areas of the U.S. global health portfolio, including HIV, tuberculosis, and family planning/reproductive health (FP/RH).
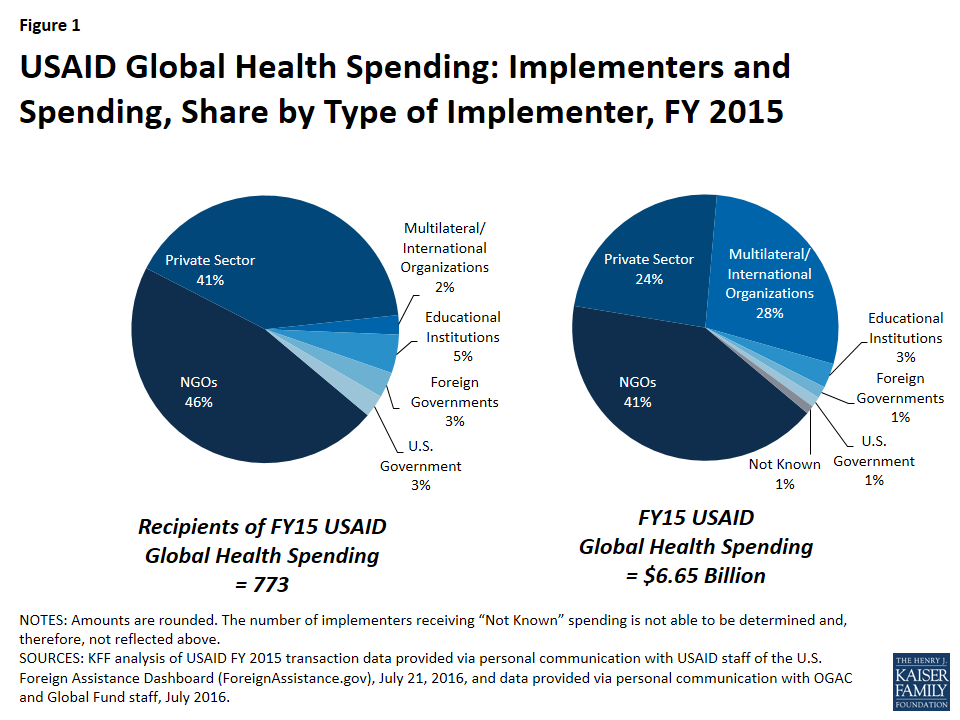
- Most implementing organizations were NGOs (46%), followed by private sector organizations (41%). The largest share of funding (41%) was directed to NGOs; private sector organizations received about a quarter of funding (24%). While multilateral/international organizations made up only 2% of implementing organizations, they received more than a quarter of funding (28%). Foreign governments received only a small share of funding directly (1%).
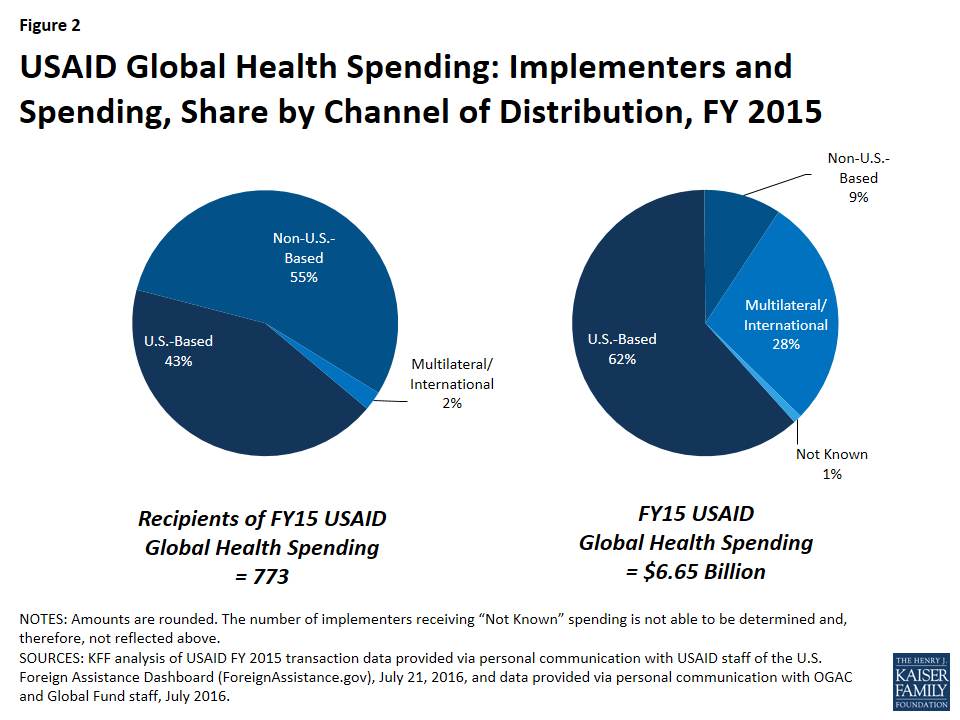
- While most implementing organizations were based outside the U.S. (55%), most funding was provided to U.S.-based organizations (62%); non-U.S.-based organizations, including local NGOs, received just 9% of funding.
- The majority of funding (56%) was provided to just 10 organizations, most of which (7) were U.S.-based; none were local NGOs.
- The greatest proportion of funding was provided to organizations working on HIV (54%), followed by maternal and child health (MCH) (13%), malaria (10%), and FP/RH (10%).
Issue Brief
Introduction
To carry out global health efforts around the world, the U.S. government (USG) funds a wide range of implementing entities, including non-governmental organizations (NGOs), multilateral/international organizations, private sector organizations, educational institutions, and other governments.
This brief provides an overview of the implementing organizations that received U.S. global health funding from the U.S. Agency for International Development (USAID) in FY 2015.2 It is based on analysis of data on USAID spending by implementing entity.3 Such spending includes funding received by USAID directly from Congress as well as through interagency transfers (primarily from the Department of State but also from the U.S. Department of Agriculture), which together account for the majority of U.S. global health spending.4 See Appendix A for a detailed methodology.
Findings
Overview
In FY 2015, 773 organizations5 received $6.65 billion in U.S. global health funding (see Table 1) to carry out global health activities in 90 countries,6 as follows:
- Six main types of organizations received funding: NGOs,7 multilateral/international organizations, private sector organizations,8 educational institutions, foreign governments, and USG agencies and departments.
- Most implementing organizations were NGOs (46%), followed by private sector organizations (41%). Multilateral/international organizations made up only 2% of implementing organizations. See Table 1 and Figure 1.
- The largest share of U.S. global health funding went to NGOs (41%). Multilateral/international organizations received more than a quarter of funding (28%), while private sector organizations only received less than a quarter of funding (24%), followed by educational institutions (3%). Only a small share went to foreign governments (1%) or to USG agencies (1%). See Table 1 and Figure 1.
| Table 1: USAID Global Health Spending – Number of Implementers and Spending, by Type of Implementer, FY 2015 | ||
| Type of Implementer | Number of Implementers | Spending($ millions) |
| Total | 773 | 6,650 |
| NGOs | 359 | 2,760* |
| Multilateral/International Organizations | 18 | 1,864* |
| Private Sector | 315 | 1,581* |
| Educational Institutions | 36 | 197 |
| Foreign Governments | 24 | 96 |
| U.S. Government | 21+ | 84 |
| Not Known | n/a | 68 |
| NOTES: Amounts are rounded. In the data, organizations are identified by implementer type; inaccurate categorizations appearing in the data would affect the totals above. * indicates a small amount of funding was “unattributed” to an implementing organization. + indicates the number of organizations/entities reflects entities, departments, operating divisions, etc., that were individually reflected in the data. n/a indicates the number of organizations could not be accurately determined because of redacted data. | ||
- Most implementing organizations were based outside the U.S. (55%); the rest were U.S.-based (43%) or multilateral/international organizations (2%). See Table 2 and Figure 2.
- On the other hand, most funding went to U.S.-based organizations, which accounted for $6 of every $10 (62%). The rest was provided through multilateral and international channels (28%) and to organizations that were based outside the U.S. (9%). See Table 2 and Figure 2.
| Table 2: USAID Global Health Spending – Number of Implementers and Spending, by Channel of Distribution, FY 2015 | ||
| Channel of Distribution | Number of Implementers | Spending($ millions) |
| Total | 773 | 6,650 |
| U.S.-Based | 332 | 4,093 |
| Non-U.S.-Based | 423 | 626 |
| Multilateral/International | 18 | 1,864 |
| Not Known | — | 68 |
| NOTES: Amounts are rounded. In the data, organizations are identified by implementer type and country of origin; inaccurate categorizations appearing in the data would affect the totals above. — indicates the number of organizations could not be accurately determined because of redacted data. | ||
- The majority of funding was provided to just 10 organizations (56%, $3.757 billion); of these, 3 were U.S.-based private sector organizations, 4 were U.S.-based NGOs, and 3 were multilateral/international organizations. None were local NGOs. See Table 3.
| Table 3: Top 10 Recipients of USAID Global Health Spending, FY 2015 | ||
| Implementer | Spending($ millions) | Type of Implementer |
| Global Fund to Fight AIDS, Tuberculosis and Malaria | 1,267 | Multilateral/Int’l |
| John Snow, Inc.* | 583 | Private Sector |
| Partnership for Supply Chain Management~ | 552 | NGO |
| FHI Development 360 | 297 | NGO |
| Abt Associates | 226 | Private Sector |
| Jhpiego | 207 | NGO |
| Management Sciences for Health (MSH) | 175 | NGO |
| Gavi, the Vaccine Alliance | 175 | Multilateral/Int’l |
| Chemonics | 149 | Private Sector |
| World Bank | 124 | Multilateral/Int’l |
| NOTES: Reflects organizations that received funding spent by USAID for USG global health efforts. Amounts are rounded. Multilateral/Int’l means Multilateral/International Organization. * indicates company also has a non-profit arm that is counted separately as an NGO (JSI’s non-profit arm is JSI Research & Training Institute). ~ indicates NGO is a separate legal entity established by JSI Research & Training Institute and MSH to implement specific work. | ||
- Organizations received funding in all 9 major program areas of the U.S. global health portfolio: HIV; tuberculosis (TB); malaria; maternal and child health (MCH); nutrition; family planning/reproductive health (FP/RH); other public health threats, including neglected tropical diseases (NTDs); pandemic influenza and other emerging threats (PIOET); and water supply and sanitation. Most funding went to HIV (54%, $3.615 billion), followed by MCH (13%, $833 million) and malaria (10%, $674 million). See Figure 3.
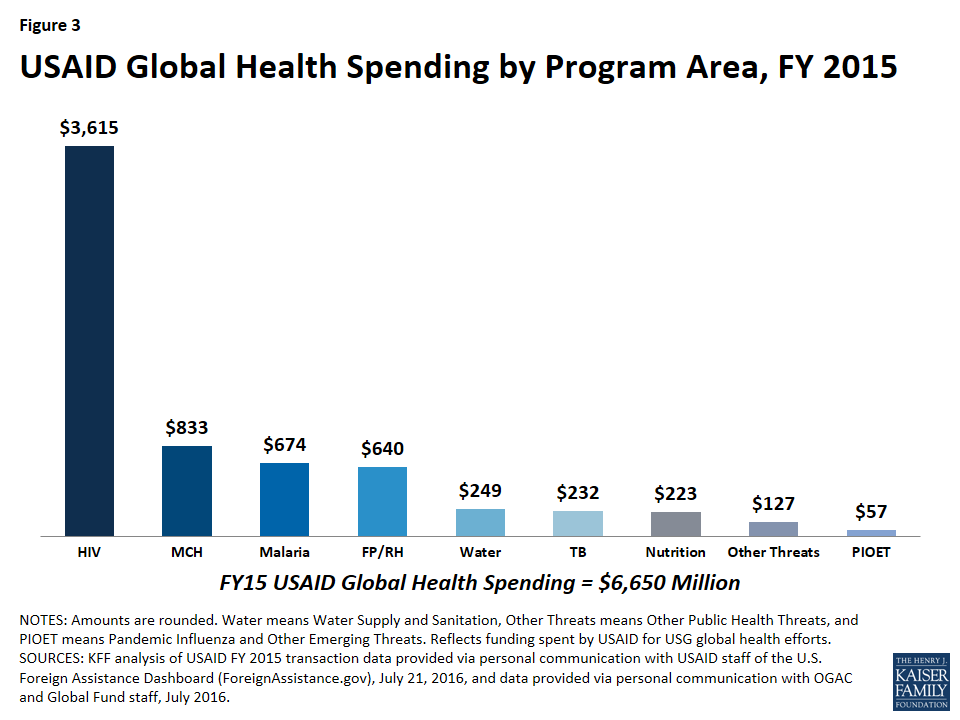
- The major types of implementer varied by program area. For example, TB funding mostly went to NGOs (48%, $110 million), followed by multilateral/international organizations (30%, $70 million), while malaria funding mostly went to the private sector (67%, $451 million), followed by NGOs (21%, $140 million). See Table 4.
- NGOs received the most funding in five program areas (HIV, FP/RH, TB, nutrition, and other public health threats); private sector organizations received most in two program areas (malaria, and water supply and sanitation); multilateral/international organizations received most in one program area (MCH); and educational institutions received most in one program area (PIOET). See Table 4.
| Table 4: USAID Global Health Spending – Spending by Program Area, FY 2015 | ||||||||
| Program Area | Share of Spending by Type of Implementer(%) | Spending($ millions) | ||||||
| NGOs | Multilateral/International | Private Sector | Educational Institutions | Foreign Governments | U.S. Government | Not Known | ||
| HIV | 42 | 38 | 15 | 2 | <1 | 1 | 1 | 3,615 |
| MCH | 36 | 38 | 17 | 2 | 6 | <1 | <1 | 833 |
| Malaria | 21 | 5 | 67 | 3 | 1 | 3 | <1 | 674 |
| FP/RH | 48 | 3 | 39 | 5 | 3 | <1 | <1 | 640 |
| Water* | 35 | 5 | 53 | 4 | 3 | <1 | <1 | 249 |
| TB | 48 | 30 | 19 | <1 | <1 | 1 | <1 | 232 |
| Nutrition | 85 | 7 | 5 | 2 | <1 | <1 | <1 | 223 |
| Other Threats^ | 73 | 12 | 6 | 3 | 2 | 3 | <1 | 127 |
| PIOET | 14 | 24 | 16 | 31 | <1 | 11 | 5 | 57 |
| NOTES: Percentages and $ amounts are rounded, except <1 shows those percentages under 1%. Percentages may not sum to 100%. Abbreviations mean: Multilateral/International means Multilateral/International Organizations, MCH – Maternal and Child Health, FP/RH – Family Planning and Reproductive Health, TB – Tuberculosis, PIOET – Pandemic Influenza and Other Emerging Threats. * means Water Supply and Sanitation. ^ means Other Public Health Threats, which includes NTDs. + indicates that funding for the Global Fund is attributed by USAID in the data to HIV only rather than to HIV, TB, and malaria. | ||||||||
Implementers by Type
Non-Governmental Organizations (NGOs)
As mentioned above, NGOs9 received the largest share of U.S. global health funding in FY 2015 (41%, $2.76 billion). The vast majority of this funding went to U.S.-based NGOs (85%), versus NGOs based outside the U.S. (15%). On the other hand, less than half of the NGOs who received funding were U.S.-based (41%, 148); most were based outside the U.S. (59%, 211). Additionally:
- About half (49%, $1.346 billion) of this funding went to the top 5 highest-funded NGOs, which were all U.S.-based; see Table 5.
- The majority of funding provided to NGOs was for activities related to HIV (55%), followed by FP/RH (11%) and MCH (11%); see Table 7.
| Table 5: Top 5 Recipients of USAID Global Health Spending, FY 2015 – NGOs and Multilateral/International Organizations | |
| Implementer | Spending($ millions) |
| NGOs | |
| Partnership for Supply Chain Management ~ | 552 |
| FHI Development 360 | 297 |
| Jhpiego | 207 |
| Management Sciences for Health (MSH) | 175 |
| Catholic Relief Services (CRS) | 114 |
| Multilateral/International Organizations | |
| Global Fund to Fight AIDS, Tuberculosis and Malaria | 1,267 |
| Gavi, the Vaccine Alliance | 175 |
| World Bank | 124 |
| World Health Organization (WHO) | 107 |
| United Nations Children’s Fund (UNICEF) | 70 |
| NOTES: Reflects organizations across selected implementer types that received funding spent by USAID for USG global health efforts. Amounts are rounded. ~ indicates NGO is a separate legal entity established by JSI Research & Training Institute and MSH to implement specific work. | |
Multilateral/International Organizations10
Nearly 20 multilateral/international organizations received more than a quarter of U.S. global health funding – the second largest share – in FY 2015 (28%, $1.864 billion). Additionally:
- The vast majority (94%, $1.743 billion) of this funding went to the top 5 highest-funded multilateral/international organizations; see Table 5. The Global Fund to Fight AIDS, Tuberculosis and Malaria (the Global Fund; an independent, international financing institution established in 2001 that provides grants to countries to address HIV, TB, and malaria)11 alone accounts for more than two-thirds of this funding (68%, $1.267 billion)12 and is the largest organizational recipient of U.S. global health funding.13
- Nearly three quarters of funding provided to multilateral/international organizations was for activities related to HIV (73%).14 See Table 7.
Private Sector
Private sector organizations received less than a quarter of U.S. global health funding in FY 2015 (24%, $1.581 billion). Nearly all funding went to U.S.-based private sector organizations (93%), versus those based outside the U.S. (7%). On the other hand, less than half of the private sector organizations that received funding were U.S.-based (44%, 139); more than half were based outside the U.S. (56%, 176). Additionally:
- Nearly three quarters (72%, $1.131 billion) of this funding went to the top 5 highest-funded private sector organizations, which were all U.S.-based; see Table 6.
- A third of funding provided to the private sector was for activities related to HIV (34%), followed by malaria (29%) and FP/RH (16%); see Table 7.
| Table 6: Top 5 Recipients of USAID Global Health Spending, FY 2015 – Private Sector, Educational Institutions, Foreign Governments, and U.S. Government Entities | |
| Implementer | Spending($ millions) |
| Private Sector | |
| John Snow, Inc.* | 583 |
| Abt Associates | 226 |
| Chemonics | 149 |
| University Research Co., LLC* | 120 |
| Futures Group International+ | 53 |
| Educational Institutions | |
| Johns Hopkins University | 75 |
| University of North Carolina at Chapel Hill | 35 |
| Eastern Virginia Medical School | 27 |
| University of California | 14 |
| Florida International University | 9 |
| Foreign Governments | |
| Afghanistan | 46 |
| Liberia | 18 |
| Egypt | 7 |
| Pakistan | 6 |
| Tanzania | 5 |
| U.S. Government/Other Agencies | |
| Centers for Disease Control and Prevention (CDC) | 35 |
| Department of State | 8 |
| U.S. Census Bureau | 4 |
| General Services Administration (GSA) | 4 |
| Naval Medical Research Center (NMRC) | 1 |
| NOTES: Reflects organizations across selected implementer types that received funding spent by USAID for USG global health efforts. Amounts are rounded. * indicates company also has a non-profit arm that is counted separately as an NGO. For example, URC’s non-profit arm is The Center for Human Services. + indicates now known as Palladium. | |
Educational Institutions
Educational institutions received a small share of U.S. global health funding in FY 2015 (3%, $197 million). Nearly all of this funding went to U.S.-based institutions (97%), versus those based outside the U.S. (3%). Two-thirds of the educational institutions were U.S.-based (67%, 24); the rest were based outside the U.S. (33%, 12). Additionally:
- The vast majority (81%, $160 million) of this funding went to the top 5 highest-funded institutions, which were all U.S.-based; see Table 6.
- Nearly half of funding provided to educational institutions was for activities related to HIV (45%), followed by FP/RH (18%); see Table 7.
Foreign Governments
Foreign governments received a very small share of U.S. global health funding in FY 2015 (1%, $96 million). This funding went to the governments of 24 countries, which is about a quarter of the overall number of countries reached by U.S. global health funding in FY 2015. Additionally:
- Five foreign governments accounted for the vast majority (85%, $81 million) of this funding; see Table 6.
- Almost half of funding provided to foreign governments was for activities related to MCH (48%), followed by FP/RH (22%) and water (9%); see Table 7.
U.S. Government
USAID also provided approximately 1% ($84 million) of funding for global health to USG agencies:
- Five other USG agencies/departments accounted for more than half (61%, $52 million) of this funding; see Table 6. The Centers for Disease Control and Prevention (CDC) was the largest recipient ($35 million).
- Nearly half of funding transferred to USG entities was for activities related to HIV (47%), followed by malaria (24%); see Table 7.
| Table 7: USAID Global Health Spending – Spending by Type of Implementer, FY 2015 | ||||||||||
| Type of Implementer | Share of Spending by Program Area(%) | Spending($ millions) | ||||||||
| HIV | MCH | Malaria | FP/RH | Water* | TB | Nutrition | Other Threats^ | PIOET | ||
| NGOs | 55 | 11 | 5 | 11 | 3 | 4 | 7 | 3 | <1 | 2,760 |
| Multilateral/International | 73+ | 17 | 2 | <1 | <1 | 4 | <1 | <1 | <1 | 1,864 |
| Private Sector | 34 | 9 | 29 | 16 | 8 | 3 | <1 | <1 | <1 | 1,581 |
| Educational Institutions | 45 | 9 | 9 | 18 | 5 | 1 | 2 | 2 | 9 | 197 |
| Foreign Governments | 7 | 48 | 8 | 22 | 9 | 2 | <1 | 3 | <1 | 96 |
| U.S. Government | 47 | 6 | 24 | 6 | 1 | 3 | <1 | 5 | 7 | 84 |
| Not Known | 78 | 5 | 3 | 6 | <1 | 1 | <1 | 2 | 4 | 68 |
| NOTES: Percentages and $ amounts are rounded, except <1 shows those percentages under 1%. Percentages may not sum to 100%. Abbreviations mean: Multilateral/International means Multilateral/International Organizations, MCH – Maternal and Child Health, FP/RH – Family Planning and Reproductive Health, TB – Tuberculosis, PIOET – Pandemic Influenza and Other Emerging Threats. * means Water Supply and Sanitation. ^ means Other Public Health Threats, which includes NTDs. + indicates that funding for the Global Fund is attributed in the data to HIV only rather than to HIV, TB, and malaria. | ||||||||||
Conclusion
To carry out its global health programs, the U.S. government funds a wide range of implementing organizations. In an effort to shed light on this landscape, this brief provides an analysis of the implementing organizations that received U.S. global health funding from USAID during FY 2015. As it finds, NGOs represent the largest group of implementers and receive the greatest share of U.S. global health funding. In addition, most implementers are based outside of the U.S. However, the analysis also finds that most funding is concentrated among a subset of implementers and is directed to U.S.-based organizations, which may have implications for longer term sustainability and country ownership. Taken together, these findings provide new information on the types of implementing organizations funded to carry out U.S. global health efforts around the world and point toward areas for further research.
Appendix
Appendix A: Detailed Methodology
This report is based on Kaiser Family Foundation analysis of USAID global health funding data for FY 2015, which were provided to KFF on request by USAID staff working on the U.S. Foreign Assistance Dashboard website and by OGAC and Global Fund staff, and additional research on some of the funded organizations.
The analysis uses transaction-level data on funding disbursed by USAID to organizations for global health activities as well as the reported U.S. contribution to the Global Fund.15 Data include funding that was appropriated by Congress to USAID for global health activities and then disbursed to organizations, as well as funding that was appropriated to other agencies for global health efforts, transferred to USAID, and then disbursed to organizations.16 It does not include funding that was directly disbursed by other USG departments/agencies, such as the Department of State or the Centers for Disease Control and Prevention, to organizations.
Funding totals are likely under-estimates, because some USAID spending has not been categorized into a specific category of activity (e.g., health, environment, economic development, etc.) in the transaction data and may include health funding.
Additionally, note:
-
Organizations were classified by implementer type based on existing categories in the data, specifically non-profit organization (referred to as NGOs in the analysis17 ), for-profit (referred to as private sector in the analysis), educational institution, government, redacted (referred to as “not known” in the analysis, and public international organization (referred to as multilateral/international organizations in the analysis). The only exception to this were entries in the “not known” type that included the name of an implementing organization: six of these organizations appeared under a specific implementer type elsewhere in the data and were re-categorized accordingly, while eight of these organizations did not appear elsewhere in the data and were re-categorized using standard conventions. Five entries that included the name of an individual (which is usually redacted in this dataset) under the “not known” type were not re-categorized and were not counted as implementing organizations.
It is possible that implementer type misclassifications by USAID are present in the data, meaning that one or more organizations may have been classified as a certain implementer type by USAID in the data when another type would have been more appropriate.
Funding totals shown in this report represent net disbursements, which include positive and negative disbursed funding amounts as well as zero-dollar disbursed funding amounts. For zero-dollar transactions, we included only transactions we could verify as no-cost extensions.18
The numbers of organizations reflected under each type were calculated based on available data, reflecting how each organization/entity appears in the data, where possible. It was not possible to calculate the number of organizations receiving funding included under the “not known” implementer type, due to redacted data on the implementing organization. Similarly, it was also not possible to precisely calculate the number of organizations receiving funding included under the non-profit organizations, private sector, and multilateral/international organizations types, due to redacted data on the implementing organization – resulting in small amounts of unattributed funding.
Funding totals in this brief should not be compared with earlier KFF analyses of USAID global health spending via NGOs, due to several differences between the datasets examined (including the availability of data on transferred funding to USAID from the U.S. Department of Agriculture, which was ultimately disbursed by USAID, in the dataset used for this analysis) as well as minor differences in methodology (including NGOs and other non-profit organizations not being delineated into distinct categories in this analysis, versus the prior analyses).
Endnotes
- Figures in this analysis should not to be compared to earlier KFF analyses of USAID spending to NGOs due to data and methodology differences. See Appendix A for more information. Earlier reports include KFF: The Role of NGOs in the U.S. Global Health Response, July 2015; Foreign NGO Engagement in U.S. Global Health Efforts: Foreign NGOs Receiving USG Support Through USAID, May 2015; NGO Engagement in U.S. Global Health Efforts: U.S.-Based NGOs Receiving USG Support Through USAID, Dec. 2014. ↩︎
- Figures in this analysis should not to be compared to earlier KFF analyses of USAID spending to NGOs due to data and methodology differences. See Appendix A for more information. Earlier reports include KFF: The Role of NGOs in the U.S. Global Health Response, July 2015; Foreign NGO Engagement in U.S. Global Health Efforts: Foreign NGOs Receiving USG Support Through USAID, May 2015; NGO Engagement in U.S. Global Health Efforts: U.S.-Based NGOs Receiving USG Support Through USAID, Dec. 2014. ↩︎
- KFF analysis of USAID FY 2015 transaction data provided via personal communication with USAID staff of the U.S. Foreign Assistance Dashboard, ForeignAssistance.gov, July 21, 2016; and KFF personal communication with OGAC and the Global Fund, July 2016. ↩︎
- Based on KFF analysis of USAID FY 2015 transaction data provided via personal communication with USAID staff of the U.S. Foreign Assistance Dashboard, ForeignAssistance.gov, July 21, 2016; FY 2015 transaction data from the U.S. Foreign Assistance Dashboard website, ForeignAssistance.gov, downloaded July 14, 2016; and data from the Office of Management and Budget, Agency Congressional Budget Justifications, and Congressional Appropriations Bills, and the U.S. Foreign Assistance Dashboard website, ForeignAssistance.gov. ↩︎
- Some recipients were not identified in the data, i.e., the information was redacted, most likely for privacy reasons because the recipient was an individual. ↩︎
- Funding through U.S.- and non-U.S.-based channels directly supported activities in 90 countries; some of this funding supported “worldwide” activities and regional activities spanning five regions (Africa, Asia, Europe & Eurasia, Latin America & the Caribbean, and the Middle East) and may have reached additional countries. Additionally, funding through multilateral and international channels indirectly supported activities that may have reached additional countries/regions as well. ↩︎
- Our earlier analyses of FY 2013 and FY 2014 health spending by USAID focused specifically on NGOs and include a definition of NGOs. This category also includes other non-profit organizations, which would include those that were not identified in the data as PIOs nor, in earlier analyses, by KFF as NGOs (e.g., hospitals, educational institutions, organizations with ties to government(s), and foundations supporting these) as well as recipients that were redacted in the data but were categorized as non-profit organizations in the data. In this report, we did not categorize non-profit organizations as NGOs and other non-profits specifically and, therefore, did not delineate between them, but many of the NGOs and other non-profits identified in our earlier analyses also appear in the FY 2015 USAID health spending data. Earlier analyses demonstrated that nearly all support for non-profits went to NGOs. See KFF: The Role of NGOs in the U.S. Global Health Response, July 2015; Foreign NGO Engagement in U.S. Global Health Efforts: Foreign NGOs Receiving USG Support Through USAID, May 2015; NGO Engagement in U.S. Global Health Efforts: U.S.-Based NGOs Receiving USG Support Through USAID, Dec. 2014. ↩︎
- For-profit organizations. ↩︎
- This also includes other non-profit organizations, which are organizations identified in the data as non-profits that were neither identified as public international organizations in the data, nor would they classified as NGOs (see KFF definition of NGOs used in earlier analyses); they might include hospitals, educational institutions (specifically, those not classified separately as such in the data), organizations with ties to government(s), and foundations supporting these. See KFF: The Role of NGOs in the U.S. Global Health Response, July 2015; Foreign NGO Engagement in U.S. Global Health Efforts: Foreign NGOs Receiving USG Support Through USAID, May 2015; NGO Engagement in U.S. Global Health Efforts: U.S.-Based NGOs Receiving USG Support Through USAID, Dec. 2014. ↩︎
- Referred to in the data as Public International Organizations (PIOs), which are defined in USAID, ADS Chapter 308: Awards to Public International Organizations, April 3, 2014, as “an international organization composed principally of countries or such other organization as designated pursuant to” a section therein, and also in USAID, ADS Glossary, April 30, 2014, as “an organization in which the U.S. participates composed principally of governments.” ↩︎
- For more information on the Global Fund, see KFF, “The U.S. & The Global Fund to Fight AIDS, Tuberculosis and Malaria,” fact sheet. ↩︎
- This is the amount of funding that the U.S. government and the Global Fund reported as the U.S. contribution for FY 2015, although a portion of it was disbursed in FY 2016 due to congressional requirements on the overall level of U.S. funding for the Global Fund. KFF personal communication with OGAC and the Global Fund, July 2016. ↩︎
- This funding is provided by Congress to the Department of State, which in turn provides it as a pass-through to USAID. KFF personal communication with OGAC, March 2016; CRS, U.S. Agency for International Development: Background, Operations, and Issues, July 21, 2015, R44117. ↩︎
- Funding for the Global Fund is attributed by USAID in the data to HIV only rather than to HIV, malaria, and TB. ↩︎
- This is the amount of funding that the U.S. government and the Global Fund reported as the U.S. contribution for FY 2015, although a portion of it was disbursed in FY 2016 due to congressional requirements on the overall level of U.S. funding for the Global Fund. KFF personal communication with OGAC and the Global Fund, July 2016. ↩︎
- For example, USAID transaction data analyzed for this report include funds transferred from the Department of State to USAID for HIV efforts, which were then obligated and eventually disbursed to various implementing organizations. ↩︎
- Our earlier analyses of FY 2013 and FY 2014 health spending by USAID focused specifically on NGOs and include a definition of NGOs. Other non-profit organizations would include those that were not identified in the data as PIOs, nor would they classified as NGOs (see KFF definition of NGOs used in earlier analyses); they might include hospitals, educational institutions (specifically, those not classified separately as such in the data), organizations with ties to government(s), and foundations supporting these. See KFF: The Role of NGOs in the U.S. Global Health Response, July 2015; Foreign NGO Engagement in U.S. Global Health Efforts: Foreign NGOs Receiving USG Support Through USAID, May 2015; NGO Engagement in U.S. Global Health Efforts: U.S.-Based NGOs Receiving USG Support Through USAID, Dec. 2014. ↩︎
- Positive and negative disbursements along with zero-dollar disbursements that are no-cost extensions are each closely linked to the recent completion or ongoing execution of global health activities, providing the best approximation available for showing where work is being done. ↩︎
Kaiser Health Tracking Poll: August 2016
Findings
KEY FINDINGS:
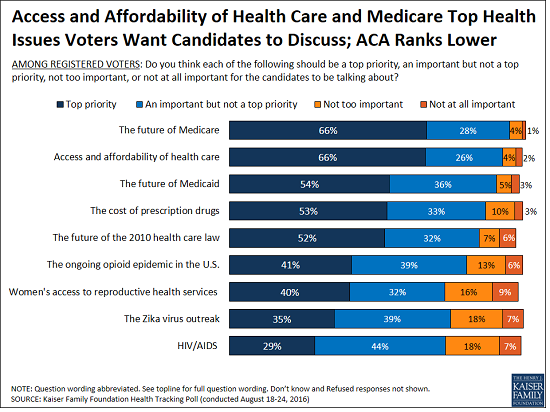
- Two-thirds of voters say the future of Medicare and access and affordability of health care are top priorities for the candidates to be talking about during the 2016 presidential campaign.
- More voters trust Hillary Clinton to do a better job dealing with health care issues than trust Donald Trump, although few believe their own ability to access affordable health care would get better regardless of which candidate is elected. Voters, age 65 and older, are split between which candidate they trust to do a better job dealing with the future of Medicare with a similar share saying they trust Trump (44 percent) as say they trust Clinton (47 percent).
- Almost all Americans have heard or read about the Zika virus (92 percent), and one-third (36 percent) say that passing new funding to deal with the outbreak in the U.S. should be a top priority for Congress, with an additional 40 percent saying it should be an important but not a top priority. A large majority of all partisans say that new Congressional funding should be at least an important priority for Congress.
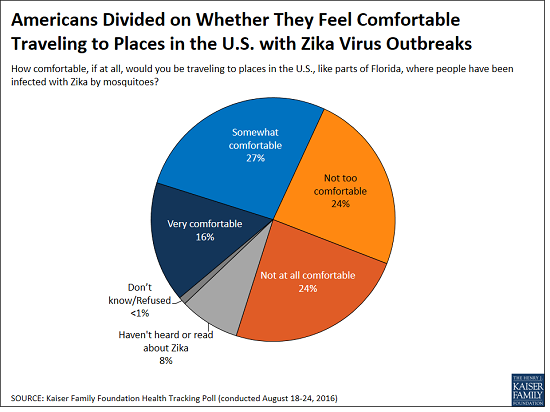
- About half of the public says they would not feel comfortable traveling to places like parts of Florida where people have been infected with the Zika virus by mosquitoes. In addition, three-fourths (77 percent) say these places are generally unsafe for pregnant women. The Kaiser Family Foundation has been tracking public opinion on Zika since February 2016; for more poll results, visit the up-to-date Zika slideshow.
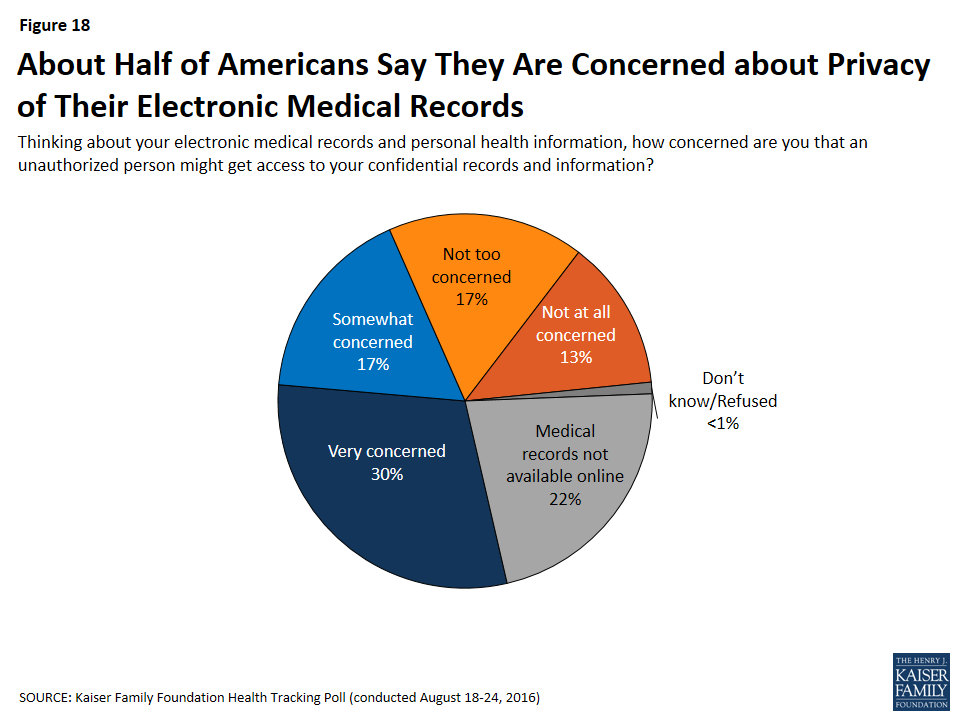
- About half of Americans are concerned that an unauthorized person might get access to their confidential records and information; despite this, 80 percent say it is important that their doctors use online medical records.
- Americans’ opinion of the health care law remains split, with 40 percent saying they have a favorable view and 42 percent saying they have an unfavorable view.
Voters and the 2016 Presidential Campaign
There are less than 10 weeks until the 2016 general election and no shortage of issues for the presidential candidates to discuss on the campaign trail and in upcoming debates. While health care has generally taken a backseat so far in the 2016 presidential election,1 during the past month, there have been several health policy stories garnering media attention including the Zika virus outbreak, prescription drug costs, health insurers leaving ACA marketplaces, and the ongoing opioid epidemic. These are in addition to other health policy issues the next president will almost certainly have to address.
When asked which health issues the presidential candidates should prioritize discussing during the 2016 presidential campaign, two-thirds of voters say the future of Medicare and access and affordability of health care are top priorities for the candidates to be talking about. About half of voters also say the future of Medicaid (54 percent), the cost of prescription drugs (53 percent), and the future of the health care law (52 percent) are top priorities. Fewer than half say the ongoing opioid epidemic (41 percent) and women’s access to reproductive health services (40 percent) are top priorities, with 35 percent saying the same about the Zika virus outbreak and 29 percent saying the same about HIV/AIDS. While the Zika virus outbreak is not viewed by the majority of voters as a top priority for candidates to discuss during the campaign, it is the most closely followed health policy news story during August.

Partisans hold differing opinions on which health issues are a “top priority” for the presidential candidates to be talking about during the presidential campaign. Three-fourths (77 percent) of Democratic voters say access and affordability of health care is a top priority; however, this opinion is shared by a smaller majority of independent voters (62 percent) and Republican voters (55 percent). Six in ten Republican voters say the future of Medicare is a top priority for the candidates to be talking about, which is equal to the share of independent voters who say the same, and lower than the share of Democratic voters (73 percent) who say the same.
A smaller share of Republican voters than Democratic voters say that each health issue should be a top priority for the presidential candidates to discuss during the presidential campaign, with one notable exception — the future of the 2010 health care law. Similar shares of Republican voters (55 percent) and Democratic voters (59 percent) say the health care law should be a top priority for the candidates to be talking about, compared to a smaller share (44 percent) of independent voters.
| Table 1: Top Health Priorities for the Candidates to Discuss During the 2016 Presidential Election | ||||
| The percent who said the following should be a “top priority” for the presidential candidates to be talking about during the 2016 presidential campaign | All Registered Voters | RepublicanVoters | DemocraticVoters | IndependentVoters |
| Access and affordability of health care | 66% | 55% | 77% | 62% |
| The future of Medicare | 66 | 60 | 73 | 60 |
| The future of Medicaid | 54 | 43 | 64 | 50 |
| The cost of prescription drugs | 53 | 47 | 63 | 48 |
| The future of the 2010 health care law | 52 | 55 | 59 | 44 |
| The ongoing heroin and prescription painkiller addiction epidemic in the U.S. | 41 | 34 | 51 | 35 |
| Women’s access to reproductive health services | 40 | 21 | 59 | 37 |
| The Zika virus outbreak | 35 | 30 | 44 | 30 |
| HIV/AIDS | 29 | 18 | 38 | 28 |
Who Do the Voters Trust On Health Issues?
When it comes to dealing with health issues facing the country, a larger share of voters say they trust Hillary Clinton to do a better job than say they trust Donald Trump to a better job. In fact, across all of the health issues included in this survey, at least half of voters say they trust Clinton to do a better job, and on the majority of the health issues, she has a double digit percentage point advantage over Trump. The largest difference between the two presidential candidates is on women’s access to reproductive health services; 64 percent of voters say they trust Clinton to do a better job dealing with this compared to 28 percent of voters who say they trust Trump to do a better job, giving Clinton a 36 percentage point advantage. A majority of female voters (71 percent) say they trust Clinton to do a better job on women’s access to reproductive health services compared to one in five (20 percent) who say they trust Trump. The smallest difference is on the future of the 2010 health care law, on which Clinton has a 9 percentage point advantage over Trump (50 percent compared to 41 percent). Voters, age 65 and older, are split between which candidate they trust to do a better job dealing with the future of Medicare with a similar share saying they trust Trump (44 percent) as say they trust Clinton (47 percent).

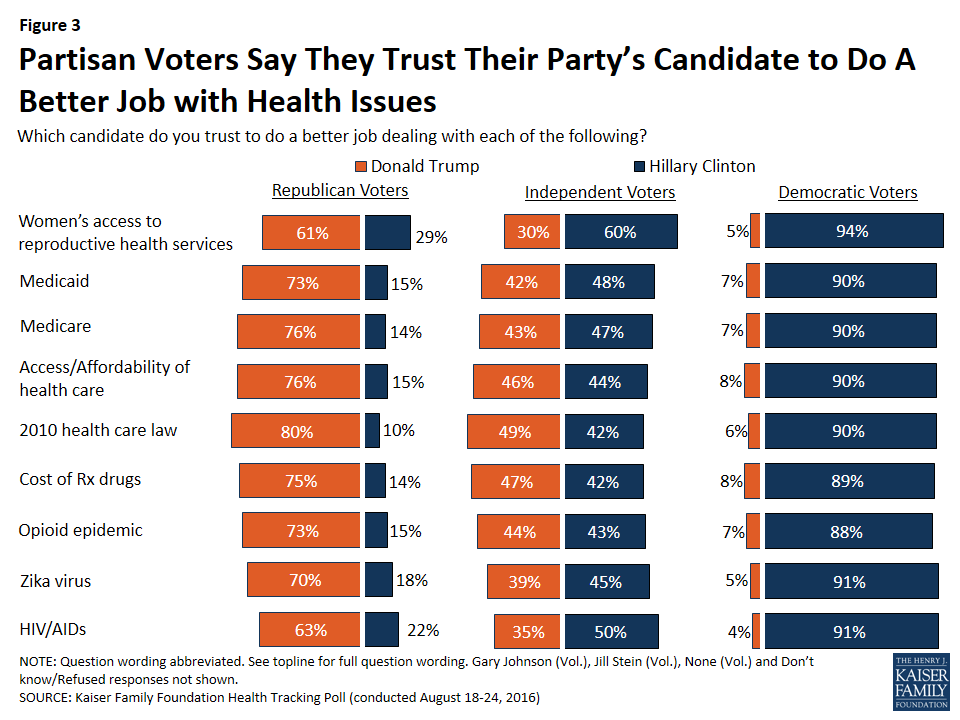
Majorities of voters from each political party say they trust their party’s candidate to do a better job dealing with each of the health issues compared to the other party’s candidate. Across all health issues, about nine out of ten Democratic voters say they trust Clinton to do a better job while a smaller share, yet still a majority, of Republican voters say they trust Trump to do a better job. Independent voters are more divided on all of these health care issues.
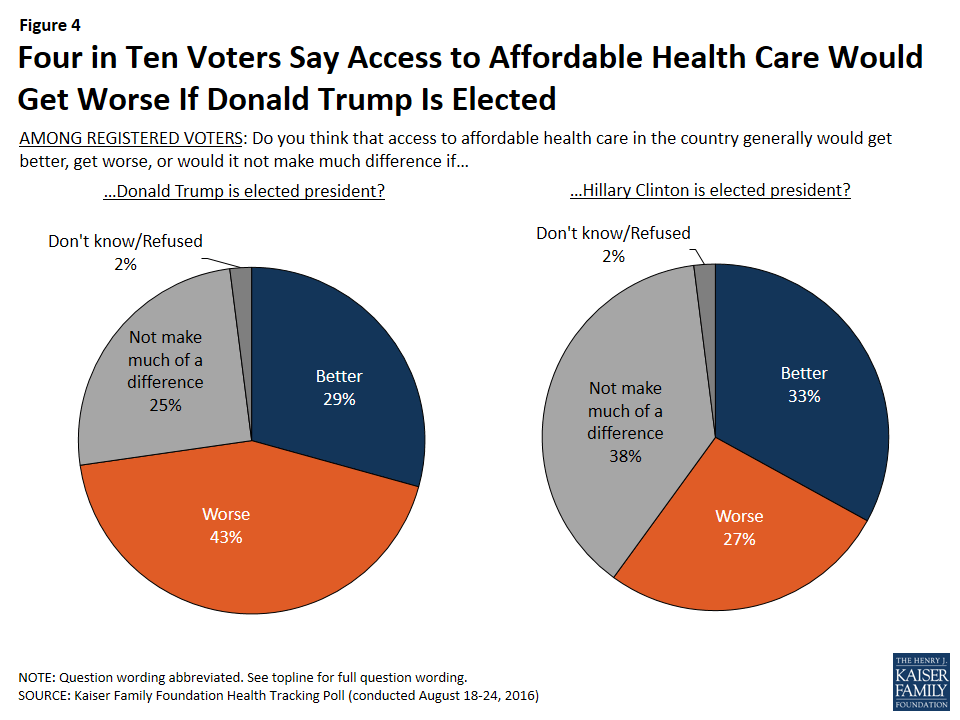
Access and Affordability of Health Care
When asked about how access to affordable health care in the country would change if Trump were elected, four in ten voters (43 percent) say that it would get worse, three in ten (29 percent) say it would get better, and one-fourth say it would not make much of a difference. When asked the same about if Clinton were elected president, 27 percent of voters say access to affordable health care in the country generally would get worse, one-third say it would get better, and four in ten (38 percent) say it would not make much of a difference.
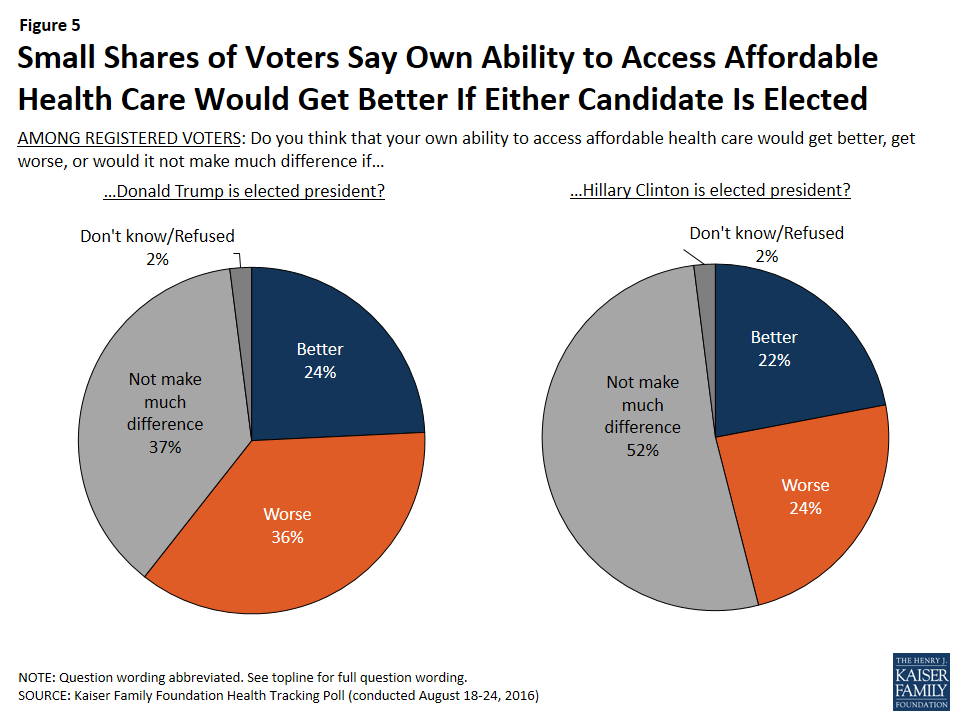
When asked how a Trump or Clinton presidency would affect their own ability to access affordable health care, half of voters (52 percent) say if Clinton is elected president it would not make much of a difference, while similar shares say it would get better (22 percent) as say it would get worse (24 percent). This is compared to 37 percent of voters who say that if Trump is elected, it would not make much of a difference in their own ability to access affordable health care, 36 percent who say it would make their own ability to access affordable health care get worse, and 24 percent who say it would get better.
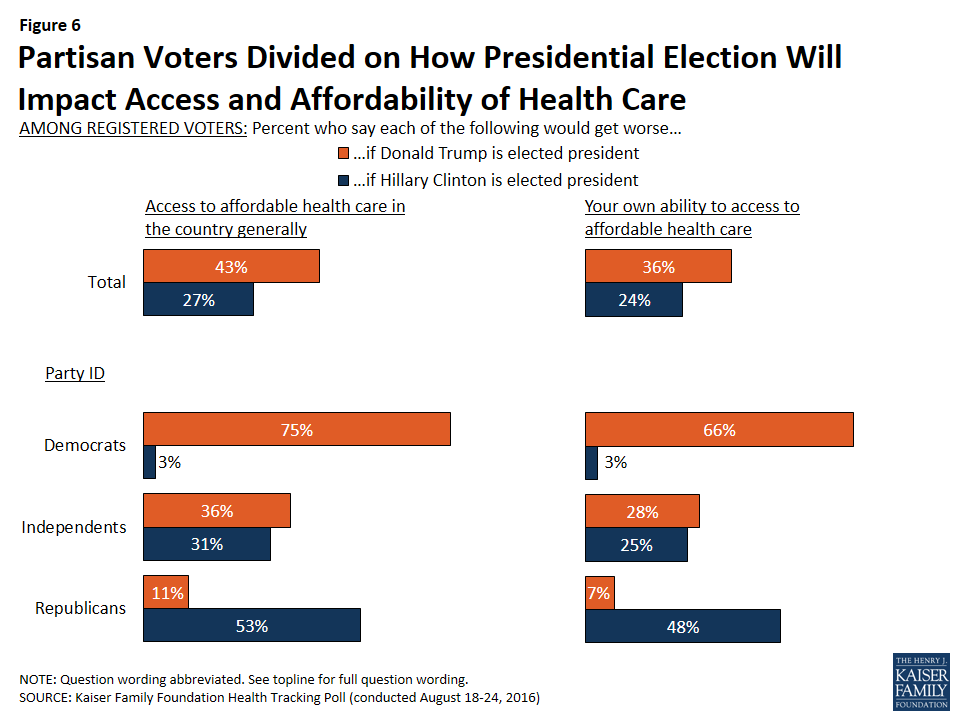
Partisan voters are divided on how access to affordable health care would change, both in the country generally and for them personally, under a Trump or Clinton presidency. Three-fourths of Democratic voters say that if Donald Trump were elected president, access to affordable health care in the country generally would get worse (compared to 11 percent of Republican voters); two-thirds of Democratic voters say their own ability to access affordable health care would get worse if Trump were elected (compared to 7 percent of Republican voters). On the other hand, if Hillary Clinton were elected president, 53 percent of Republican voters say access to affordable health care in the country generally would get worse (compared to 3 percent of Democratic voters), and 48 percent say their own ability to access affordable health care would get worse (compared to 3 percent of Democratic voters). Independent voters are split on what would happen if Trump or Clinton is elected, with about one-fourth saying their own ability to access affordable health care would get worse if either candidate was elected.
Americans’ Opinions of the Affordable Care Act
Americans’ opinion of the health care law remains divided, with 40 percent saying they have a favorable view and 42 percent saying they have an unfavorable view.
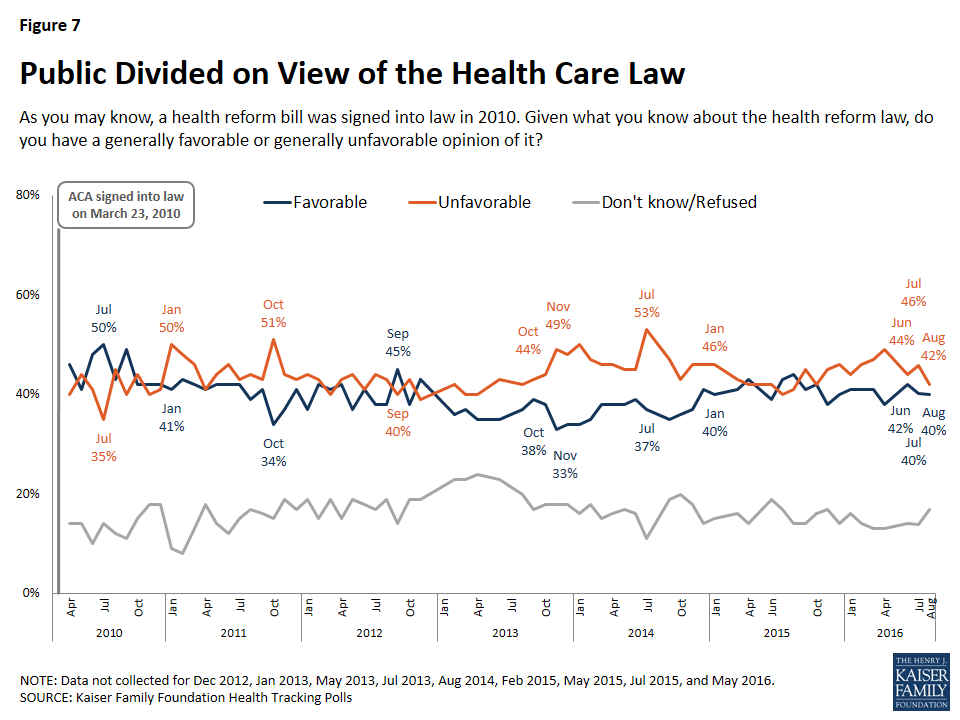
Furthermore, partisans continue to hold widely differing views; two-thirds of Democrats (67 percent) report a favorable view, while three-fourths of Republicans (76 percent) report an unfavorable view and independents tilt negative, with 37 percent saying they have a favorable opinion and 47 percent saying they have an unfavorable opinion.
When asked about the news media’s coverage of the health reform law, four in ten say that the coverage is mostly balanced while 27 percent say it is biased in favor of the law and 21 percent say it is biased against the law. About half (47 percent) of Republicans say the news media coverage of the health reform law is biased in favor of the law while half of Democrats and 43 percent of independents say the news coverage is mostly balanced.

The Zika Virus Outbreak
The Zika virus outbreak continues to be the health policy story most followed by Americans. In July, health officials confirmed the first cases of individuals being infected by mosquitoes in the U.S. in a Miami, Florida neighborhood, and a subsequent travel advisory recommended that pregnant women stay away from the area.2
The August tracking poll takes a look at the public’s knowledge of these recent developments, their attitudes about travel to – and safety of – areas affected by Zika, and their views on the importance of Congressional funding to deal with the outbreak in the United States. The Kaiser Family Foundation has been tracking public opinion on Zika since February 2016; for more poll results, visit the up-to-date Zika slideshow.
Knowledge of Local Transmission and Domestic Travel Warnings
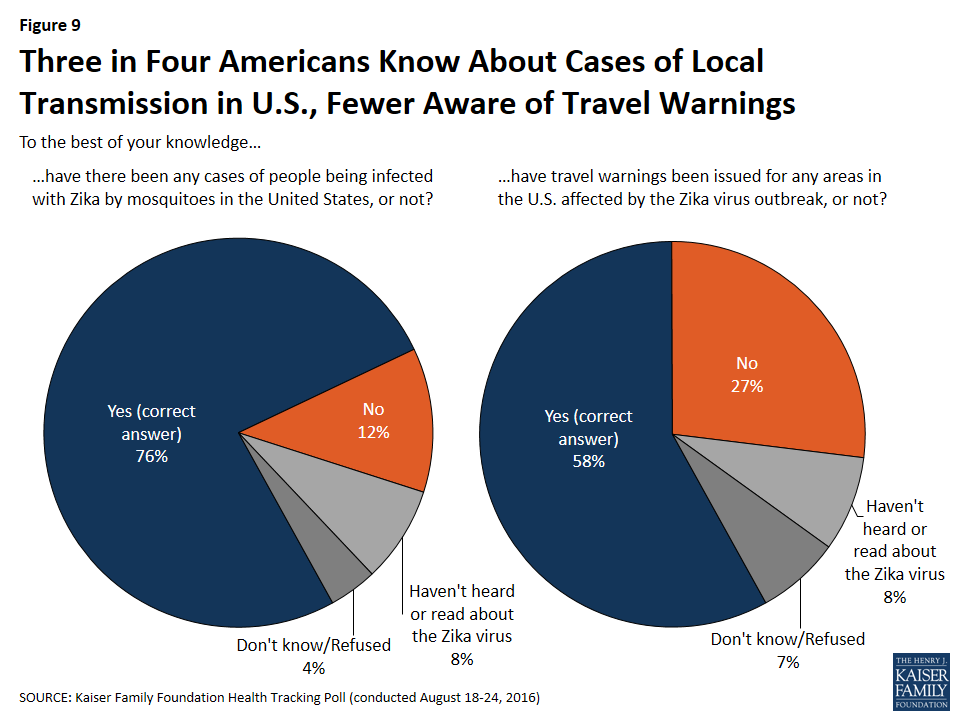
Three-fourths of the public (76 percent) are aware that there are cases of local transmission in the country – that is, cases where people are being infected with the Zika virus by mosquitoes. A smaller share, but still a majority, report being aware of travel warnings issued for areas in the United States affected by the outbreak (58 percent).
Attitudes Toward Traveling to Places Affected by Zika
About half of the public (48 percent) say that they would be “not too” or “not at all” comfortable traveling to places in the U.S., like parts of Florida, where people have been infected with Zika by mosquitoes. In contrast, six in ten say they would be not be comfortable traveling to U.S. territories like Puerto Rice where people have become infected (59 percent) or to places outside the U.S. where people have become infected (61 percent).
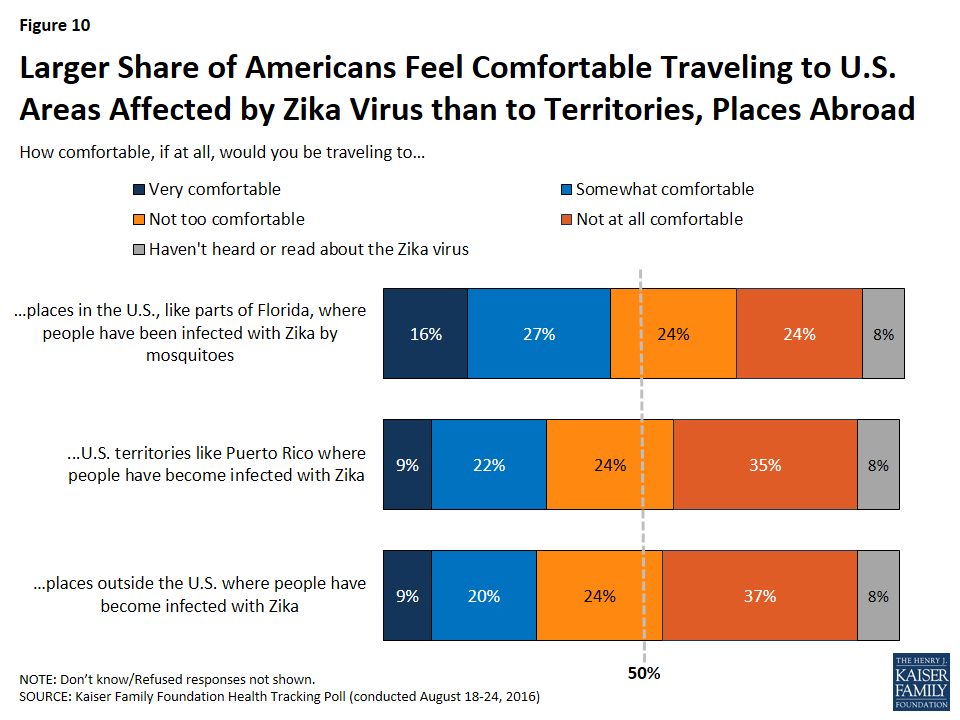
Individuals who report being aware of travel warnings for areas in the U.S. affected by Zika are more likely to say they are not comfortable traveling to places affected by the virus. For example, when asked about traveling to places in the U.S. like Florida where people have been infected by mosquitoes, 59 percent of individuals aware of travel warnings say that they would not be comfortable, compared to 39 percent of those who thought travel warnings had not been issued. In addition, women are not as comfortable traveling to places affected by Zika than men. Fifty-three percent of women, compared to 43 percent of men, report being not comfortable traveling to places in the U.S. where people have been infected by mosquitoes.
Evaluations of Safety for Pregnant Women
A large majority – 77 percent – of the public say they think areas in the U.S. where people have been infected by mosquitoes are generally unsafe for pregnant women. A small share appears concerned about the safety of these places for themselves, with half saying that areas in the U.S. where people have been infected with Zika by mosquitoes are generally safe for them, personally and 39 percent saying they are generally unsafe.
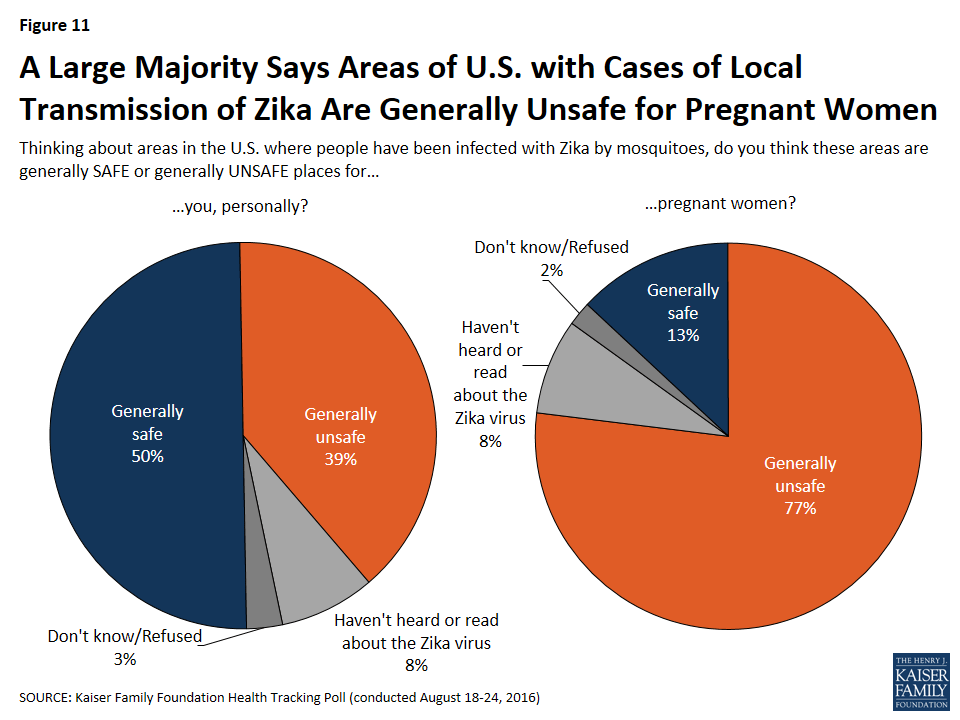
Individuals aware of the travel warnings issued for places in the U.S. affected by Zika are more likely to say that places with local transmission are generally unsafe for pregnant women (89 percent v. 77 percent of those who thought travel warnings had not been issued). They are also more likely to say that such places are generally unsafe for them, personally (47 percent v. 32 percent). Furthermore, women are more likely than men to say that places with local transmission are generally unsafe for pregnant women (81 percent v. 74 percent) and to say they are generally unsafe for themselves, personally (43 percent v. 35 percent).
Most See Congressional Funding to Deal with the Virus as an Important Priority
Despite President Obama’s February request for almost $1.9 billion to deal with the Zika virus outbreak,3 U.S. Congress has not passed any additional funding. Thirty-six percent of the public say that passing new funding to deal with the outbreak in the U.S. should be a top priority, with an additional 40 percent saying it should be an important but not a top priority. Nine percent think passing new funding is not too important, and 5 percent say that new funding should not be passed at all.
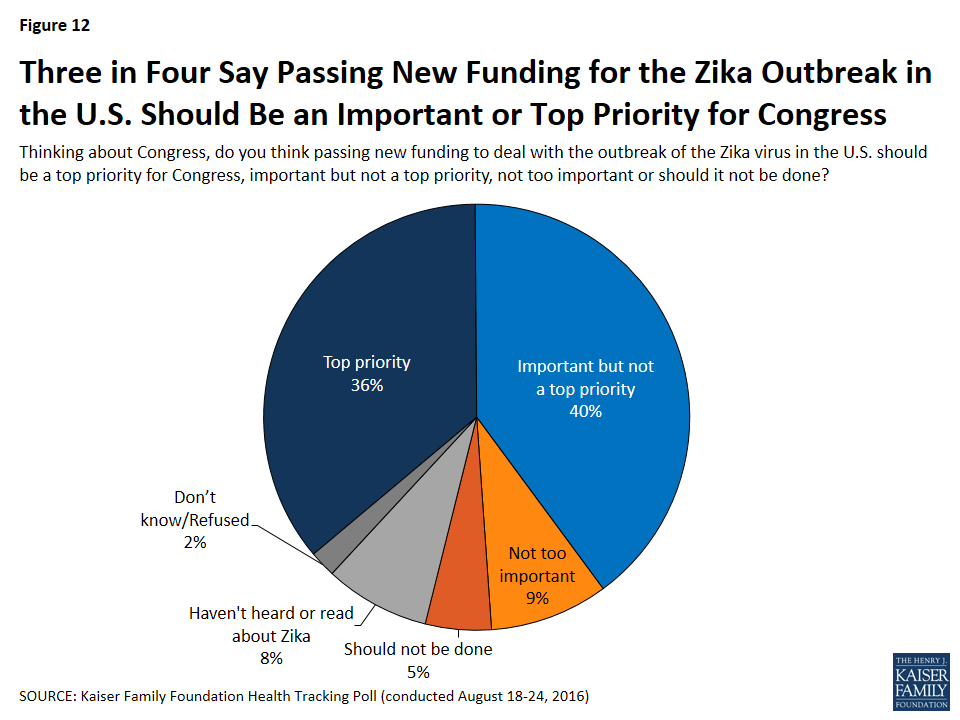
There are partisan differences in these findings, with a larger share of Democrats than independents or Republicans saying Congressional funding to deal with the Zika virus outbreak should be a top priority (46 percent v. 34 percent and 27 percent). However, a large majority of all partisans say that new Congressional funding should be at least an important priority of Congress.
| Table 2: Majorities of Democrats, Independents, and Republicans Say New Funding to Deal with Zikafrom Congress Should at Least Be an Important Priority | ||||
| Percent who say new Congressional funding to deal with the Zika virusoutbreak in the U.S. should… | Total | Democrats | Independents | Republicans |
| Be a top priority | 36% | 46% | 34% | 27% |
| Be an important but not top priority | 40 | 36 | 41 | 46 |
| Be not too important | 9 | 6 | 12 | 10 |
| Not be done | 5 | 2 | 5 | 8 |
Electronic Health Records
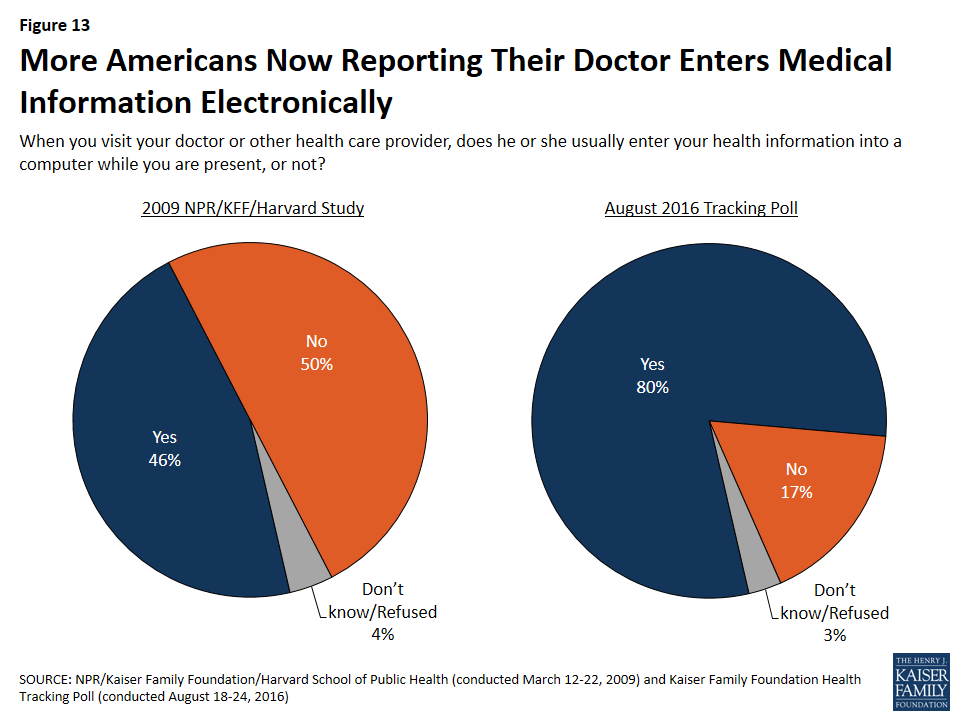
In 2009, the federal government passed the Health Information Technology for Economic and Clinical Health (HITECH) Act which allocated $27 billion for an incentive program encouraging health care providers to adopt electronic health records systems (EHR).4 In a 2009 poll5 conducted by the Kaiser Family Foundation, NPR, and the Harvard School of Public Health, about half of the public (46 percent) reported that their doctor entered their health information into a computer during a visit. In the most recent survey, eight in ten Americans say their doctor or health care provider enters their health information into a computer during a visit.
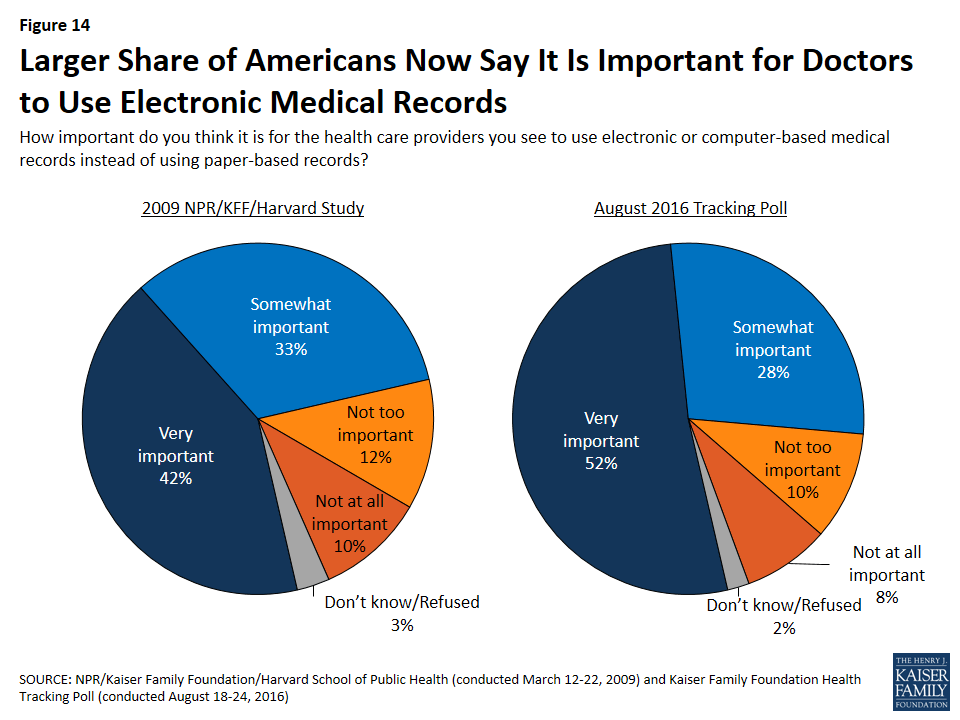
In addition, half (52 percent) of Americans say it is “very important” for their health care provider to use electronic or computer-based medical records instead of using paper-based records, up from 42 percent in 2009.
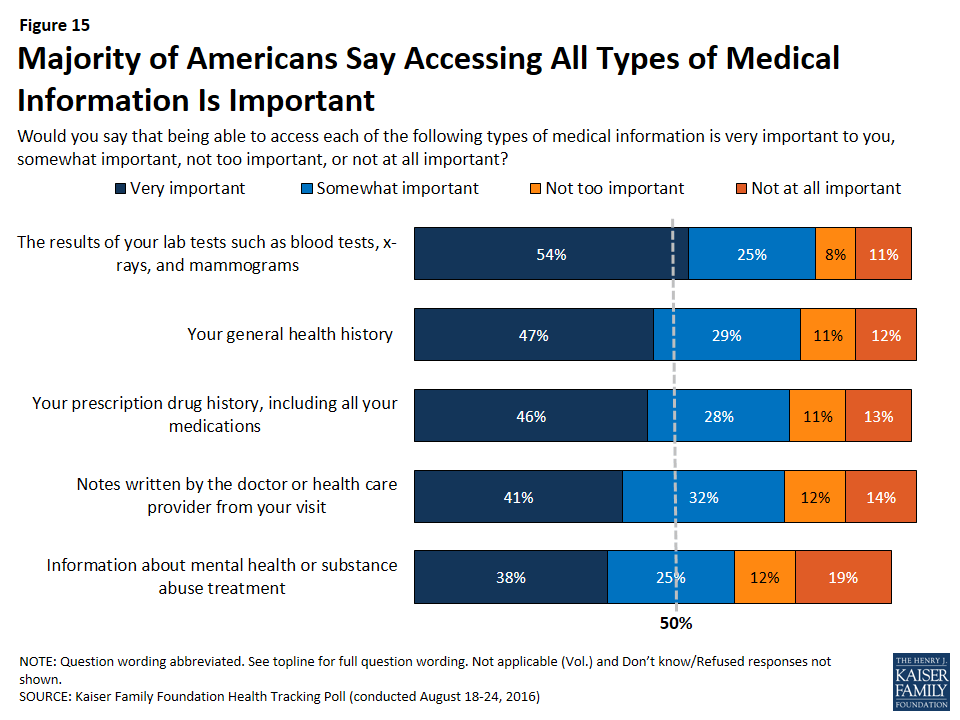
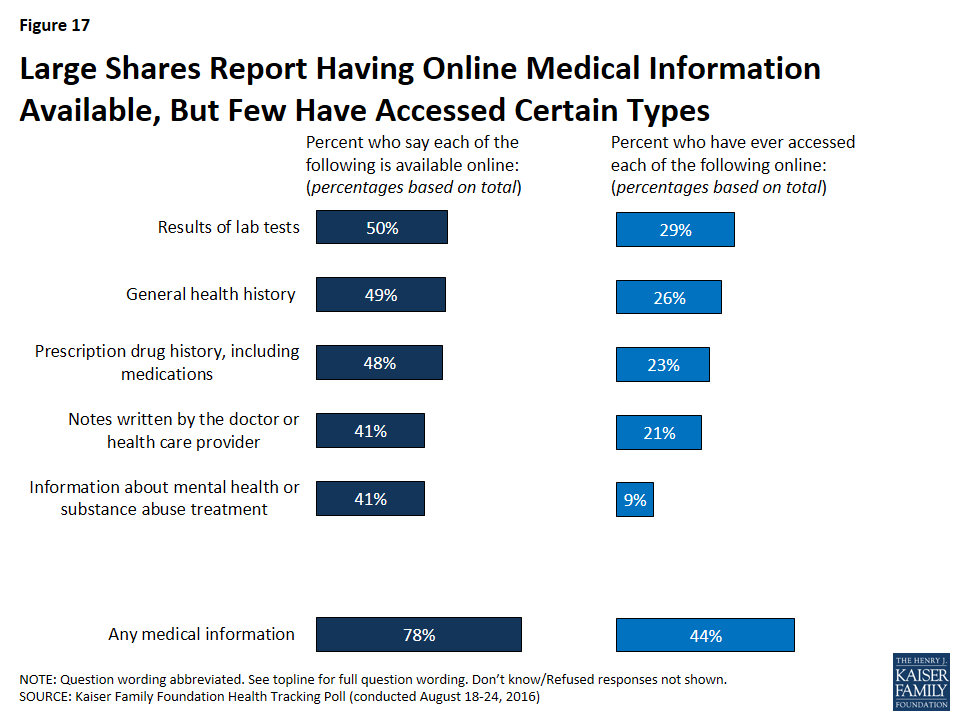
When asked about what type of medical information is important to be able to access, the majority of the public say each type of information included in the survey is at least “somewhat” important. Eight in ten (79 percent) say being able to access the results of their lab tests is at least somewhat important. This is followed by about three-fourths who say the same about being able to access their general health history (75 percent), their prescription drug history (74 percent), and the notes written by their doctor of health care provider from their visit (73 percent). A smaller share (63 percent) say accessing information about their mental health or substance abuse treatment is at least somewhat important.
Some Availability But Limited Accessing of EHRs
While the vast majority of Americans say it is important for their health care provider to use electronic medical records and most say that being able to access different types of medical information is important, a large share currently say their medical information is not available online. Across all the different types of health information, about a third say these types of information are not currently available to them online, with a slightly larger share (41 percent) saying the notes written by their doctor or health provider are not available.
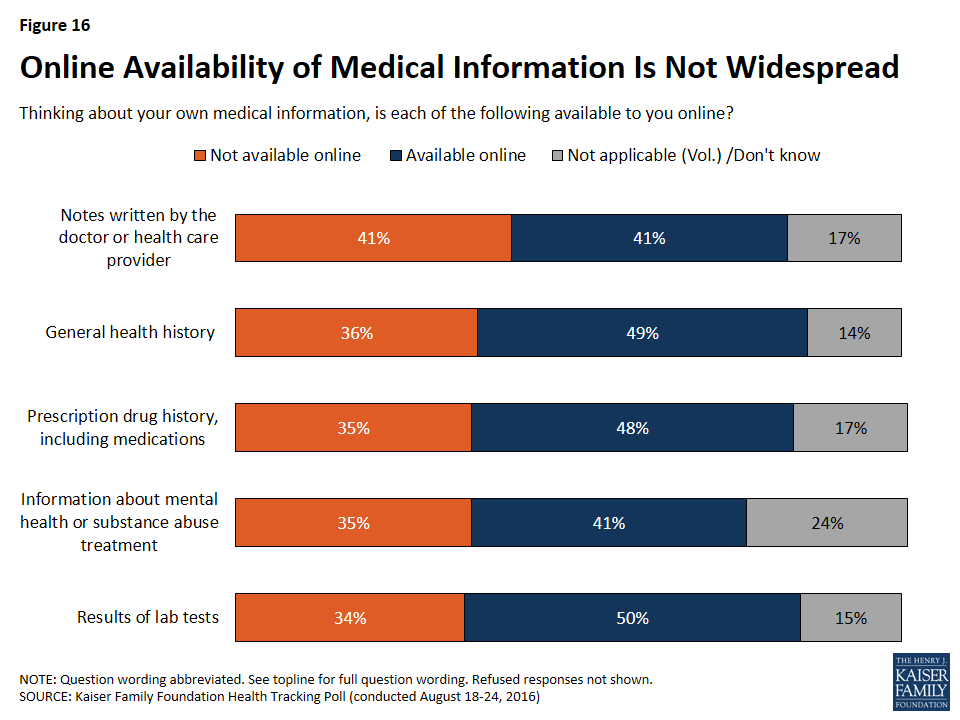
While 78 percent of Americans report that at least some of their medical information is available online, much smaller shares report accessing this information. Less than half of Americans report having accessed any type of medical information online. When they do access medical information, 29 percent say they have accessed the results of lab tests, such as blood tests, x-rays, and mammograms, 26 percent say they have accessed general health history, 23 percent say they have accessed prescription drug history, and 21 percent say they have accessed notes written by their doctor or health care provider. A much smaller share report accessing information about mental health or substance abuse treatment (9 percent).
Majority of Americans Have Security or Privacy Concerns Regarding Online Medical Records
About eight in ten (78 percent) Americans have at least some medical records and personal health information available online. Of these, 60 percent (47 percent of total population) say they are either “very” or “somewhat” concerned that an unauthorized person might get access to their confidential records and information. Larger shares of Hispanic individuals (58 percent of total) and Blacks (56 percent of total) report having privacy concerns than Whites (42 percent of total).
Why Some Americans Still Don’t Access Online Medical Records
One-third of Americans report that they have the ability to access their medical records or personal health information online but have not done so. The main reason given is that they did not have a need to access the information (49 percent), followed by not having access to the internet (15 percent), not knowing how to access the information (13 percent), and being concerned about privacy or security (11 percent).

In addition, accessing online medical records or health information is seemingly dependent on education level and income, but noticeably, not on age. Almost half of individuals who have not accessed their own medical records have a high school diploma or less (49 percent) or earn less than $40,00 a year (47 percent).
| Table 3: Demographics of Those Who Have and Have Not Accessed Their Own Medical Records or Personal Health Information Online | |||
| Have Accessed | Have Not Accessed | Total | |
| Education | |||
| High school or less | 31% | 49% | 40% |
| Some college | 30 | 31 | 30 |
| College+ | 39 | 20 | 29 |
| Income | |||
| <$40K | 34 | 47 | 40 |
| $40K to less than $90K | 29 | 31 | 30 |
| >$90K | 26 | 12 | 20 |
| Age | |||
| 18-29 | 19 | 21 | 20 |
| 30-49 | 35 | 30 | 32 |
| 50-64 | 29 | 28 | 29 |
| 65+ | 17 | 20 | 19 |
Kaiser Health Policy News Index: August 2016
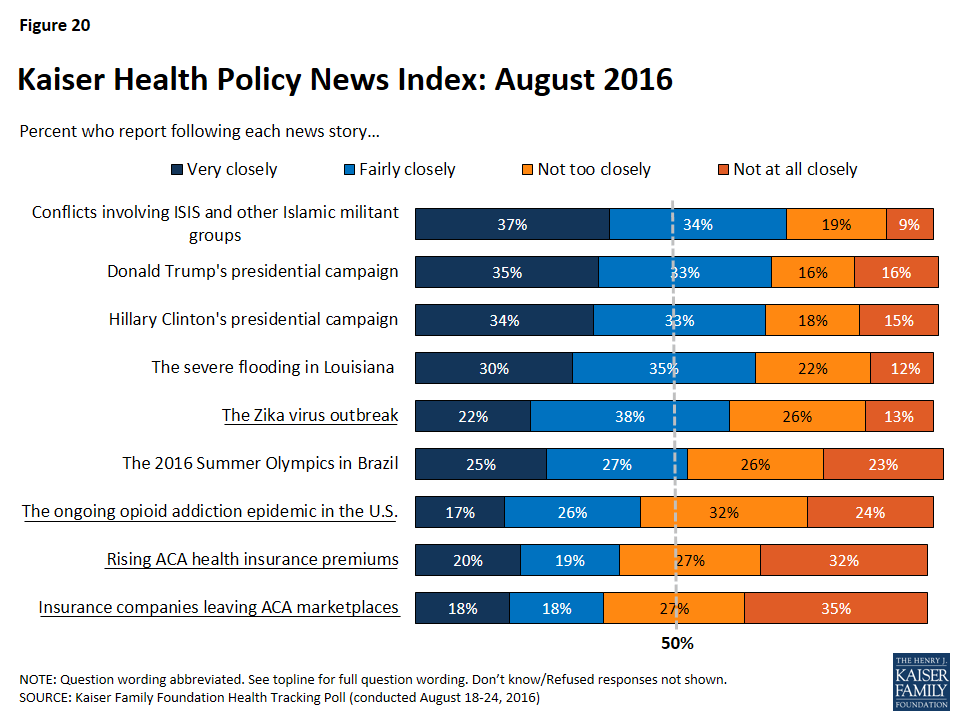
The August Kaiser Health Tracking Poll finds that the majority of Americans (71 percent) are following stories about conflicts involving ISIS and other Islamic militant groups as well as both Donald Trump’s presidential campaign (68 percent) and Hillary Clinton’s presidential campaign (67 percent). Other stories that capture the attention of Americans this month include the severe flooding in Louisiana (65 percent) and the Zika virus outbreak (60 percent). About half of Americans say they have been following stories about the 2016 Summer Olympics, which took place in Brazil from August 5th to 21st. While a majority of the public say they follow news about the Zika virus outbreak, fewer Americans report following three additional health policy stories: the ongoing heroin and prescription painkiller addiction epidemic in the U.S. (43 percent), reports about rising ACA health insurance premiums (39 percent), and news of health insurance companies leaving ACA marketplaces (36 percent).
Methodology
This Kaiser Health Tracking Poll was designed and analyzed by public opinion researchers at the Kaiser Family Foundation (KFF). The survey was conducted August 18-24, 2016, among a nationally representative random digit dial telephone sample of 1,211 adults ages 18 and older, living in the United States, including Alaska and Hawaii (note: persons without a telephone could not be included in the random selection process). Computer-assisted telephone interviews conducted by landline (423) and cell phone (788, including 473 who had no landline telephone) were carried out in English and Spanish by Princeton Data Source under the direction of Princeton Survey Research Associates International (PSRAI). Both the random digit dial landline and cell phone samples were provided by Survey Sampling International, LLC. For the landline sample, respondents were selected by asking for the youngest adult male or female currently at home based on a random rotation. If no one of that gender was available, interviewers asked to speak with the youngest adult of the opposite gender. For the cell phone sample, interviews were conducted with the adult who answered the phone. KFF paid for all costs associated with the survey.
The combined landline and cell phone sample was weighted to balance the sample demographics to match estimates for the national population using data from the Census Bureau’s 2014 American Community Survey (ACS) on sex, age, education, race, Hispanic origin, and region along with data from the 2010 Census on population density. The sample was also weighted to match current patterns of telephone use using data from the July-December 2015 National Health Interview Survey. The weight takes into account the fact that respondents with both a landline and cell phone have a higher probability of selection in the combined sample and also adjusts for the household size for the landline sample. All statistical tests of significance account for the effect of weighting.
The margin of sampling error including the design effect for the full sample is plus or minus 3 percentage points. Numbers of respondents and margins of sampling error for key subgroups are shown in the table below. For results based on other subgroups, the margin of sampling error may be higher. Sample sizes and margins of sampling error for other subgroups are available by request. Note that sampling error is only one of many potential sources of error in this or any other public opinion poll. Kaiser Family Foundation public opinion and survey research is a charter member of the Transparency Initiative of the American Association for Public Opinion Research.
| Group | N (unweighted) | M.O.S.E. |
| Total | 1211 | ±3 percentage points |
| Registered Voters | ||
| Total RV | 1020 | ±4 percentage points |
| Democratic RV | 340 | ±6 percentage points |
| Republican RV | 256 | ±7 percentage points |
| Independent RV | 340 | ±6 percentage points |
| Party Identification | ||
| Democrats | 381 | ±6 percentage points |
| Republicans | 286 | ±7 percentage points |
| Independents | 404 | ±6 percentage points |
| Gender | ||
| Men | 630 | ±5 percentage points |
| Women | 581 | ±5 percentage points |
| Zika Travel Warnings | ||
| Aware of domestic travel warnings related to Zika | 742 | ±4 percentage points |
| Say there aren’t domestic travel warnings related to Zika | 308 | ±6 percentage points |
Endnotes
- See previous KFF Health Tracking Polls including the July 2016 Tracking Poll which found that about one-third of voters say health care is “extremely important” to their vote for president this year, https://modern.kff.org/health-costs/poll-finding/kaiser-health-tracking-poll-july-2016/. ↩︎
- https://www.washingtonpost.com/news/to-your-health/wp/2016/08/01/florida-announces-10-new-zika-cases-a-travel-advisory-is-expected/ The Centers for Disease Control has since expanded their warning after new cases of local transmission were confirmed in another neighborhood. ↩︎
- https://www.washingtonpost.com/opinions/zika-is-spreading-in-florida-but-congress-still-hasnt-approved-cash-to-fight-it/2016/08/23/cafe91e2-6966-11e6-99bf-f0cf3a6449a6_story.html?utm_term=.e96a1d4a23ea ↩︎
- https://www.healthit.gov/policy-researchers-implementers/health-it-legislation ↩︎
- https://modern.kff.org/health-reform/poll-finding/the-public-and-the-health-care-delivery-2/ ↩︎
Campaign 2016: Voters Give Clinton Wide Edge Over Trump on Trust to Handle Health Care Issues; ACA Ranks Lower Among Health Issues Voters Want Discussed
Zika Outbreak: Half of Public Would Be Uncomfortable Visiting Affected Parts of Florida; Large Majority Says New Zika Funding Is a Top or Important Priority for Congress
Electronic Medical Records: Eight in 10 Americans Say It Is Important for Providers to Computerize Records, But Half Worry About Unauthorized Access to Online Information
With the 2016 elections just 10 weeks away, voters give Democratic presidential nominee Hillary Clinton a substantial advantage over Republican nominee Donald Trump on a wide array of health care issues, the latest Kaiser Health Tracking Poll finds.
Two thirds of voters (66%), including large shares of Democrats, Republicans, and independents, identify access and affordability of health care and the future of Medicare, an issue not being widely discussed on the campaign trail, as top priorities for the presidential candidates to talk about during the campaign. Smaller majorities of voters say the same about Medicaid’s future (54%), prescription drug costs (53%), and the future of the 2010 health care law (52%).
On each of those issues and several other health policy issues, more voters say they trust Clinton to do a better job than say they trust Trump, the poll finds. For example, Clinton leads Trump on Medicare’s future (53% compared to 38%), access and affordability to health care (52% to 39%), Medicaid’s future (54% to 37%), prescription drug costs (51% to 39%), and the Zika virus outbreak (54% to 34%). Among the nine issues asked about, Clinton’s largest lead is 36 percentage points on women’s access to reproductive health care (64% to 28%), while her smallest lead is on the future of the 2010 Affordable Care Act (50% to 41%).
A majority of female voters (71%) say they trust Clinton to do a better job on women’s access to reproductive health services compared to one in five (20%) who say they trust Trump. Voters, age 65 and older, are split between which candidate they trust to do a better job dealing with the future of Medicare with a similar share saying they trust Trump (44%) as saying they trust Clinton (47%).
In spite of Clinton’s edge with voters on these issues, most voters don’t expect much improvement in access to affordable care regardless of who wins the election. A third (33%) of voters say access to affordable care would get better across the country generally if Clinton wins; a similar share (29%) say so if Trump were to win. The poll also shows few voters expect their own ability to access affordable care to improve under either candidate. On each question, more voters say they expect the situation to get worse if Trump were elected than if Clinton were elected.
KFF has been tracking public opinion on the Zika virus outbreak since February 2016, and this month’s survey finds three quarters (76%) of the public are aware that people in the United States have become infected from the bite of mosquitoes locally. A smaller majority (58%) is aware that travel warnings have been issued for areas in the United States affected by the outbreak.
About half of the public (48%) say that they would not be comfortable traveling to places in the United States, like parts of Florida, where people have been infected by mosquitoes. Slightly more say the same about traveling to U.S. territories like Puerto Rico or to places outside the United States where people have become infected (59% and 61%, respectively).
With Congress set to return from its August recess after Labor Day, the poll finds a third (36%) of the public views passing new funding to combat Zika as a top priority for Congress. An additional 40 percent say it is an important, but not top, priority. Democrats are more likely than Republicans or independents to view Zika as a top Congressional priority, though large majorities within each group consider it at least an important priority.
The survey also probes the public’s experience and views with electronic medical records. Today, 80 percent of the public says their doctor or other healthcare provider usually enters their health information into a computer while they are present – up sharply since 2009, when an earlier KFF poll found 46 percent said this usually happened. Half (52%) now say it is “very important” for their providers to use electronic medical records, up from 42 percent in 2009.
About eight in ten (78%) Americans say they have at least some medical records and personal health information available online. Of these, 60 percent (47% of total population) say they are either “very” or “somewhat” concerned that an unauthorized person might get access to their confidential records and information.
Other poll findings include:
- Americans’ opinion of the health care law remains split with 40 percent saying they have a favorable view and 42 percent saying they have an unfavorable view.
- When asked about the news media’s coverage of the health reform law, four in ten say that the coverage is mostly balanced while 27 percent say it is biased in favor of the law and 21 percent say it is biased against the law. About half (47 percent) of Republicans say the news media coverage of the health reform law is biased in favor of the law while half of Democrats and 43 percent of independents say the news coverage is mostly balanced.
Designed and analyzed by public opinion researchers at the Kaiser Family Foundation, the poll was conducted from August 18-24 among a nationally representative random digit dial telephone sample of 1,211 adults. Interviews were conducted in English and Spanish by landline (423) and cell phone (788). The margin of sampling error is plus or minus 3 percentage points for the full sample. For results based on subgroups, the margin of sampling error may be higher.
Preliminary Data on Insurer Exits and Entrants in 2017 Affordable Care Act Marketplaces
In October 2016, the Foundation issued a updated version of this analysis with a new county-level interactive map and slideshow
The following charts provide a preliminary picture of the potential effect insurer exits and entrants may have on competition and consumer choice in the Affordable Care Act (ACA) marketplaces. This analysis was done at the request of the Wall Street Journal. Our earlier analysis found that UnitedHealth’s absence from these markets would leave many parts of the country with fewer marketplace insurers, and that the number of counties with a single insurer would likely increase substantially if there were no new entrants. Similarly, our July analysis of insurer participation in 17 states with detailed, publicly available premium and participation data found that on average there would be fewer insurers participating in 2017 in these states than there had been in 2016 or 2015.
Since the time of our earlier analyses, more details have emerged on the degree to which some insurance companies, most recently Aetna and Oscar, are planning to scale back or withdrawing their participation on the marketplaces. Meanwhile other insurers, including Cigna, have noted their intent to enter into new markets or expand their offerings in their 2017 rate filings to state regulators.
Despite these new details, much is still unknown and the majority of states’ 2017 filings are either redacted or unavailable publicly. Because only premium changes, and not new entrant premiums, are posted on Healthcare.gov’s rate review site, it is also likely that more is known at this time of market exits than is known of entrants. Complete information on insurer participation and premiums across all states does not typically become public until shortly before the beginning of the open enrollment season. It is therefore likely that the complete picture of how entrants and exits are shaping these markets in 2017 will not come into focus for two more months.
Given these limitations, it is too soon to say with certainty how many marketplace insurers enrollees will have available to them when they go to shop for coverage in November. In this analysis, we start with insurers’ participation in 2016 and make adjustments for reported entrants, exits, scale-backs, and expansions. More information on our methods and limitations can be found below. We intend to update this analysis when more complete data are available.
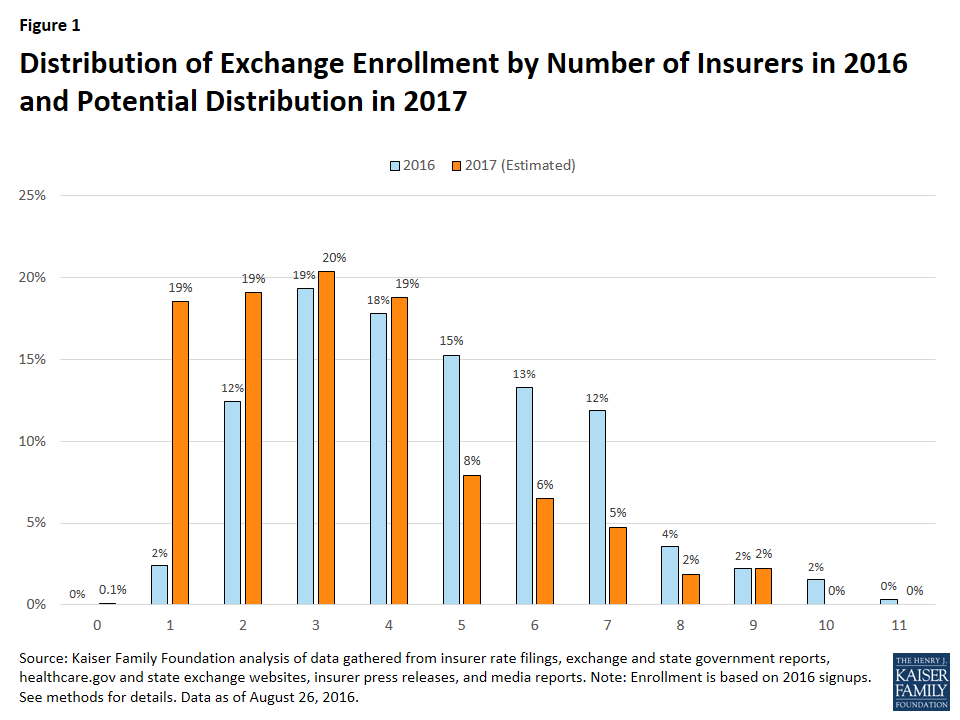
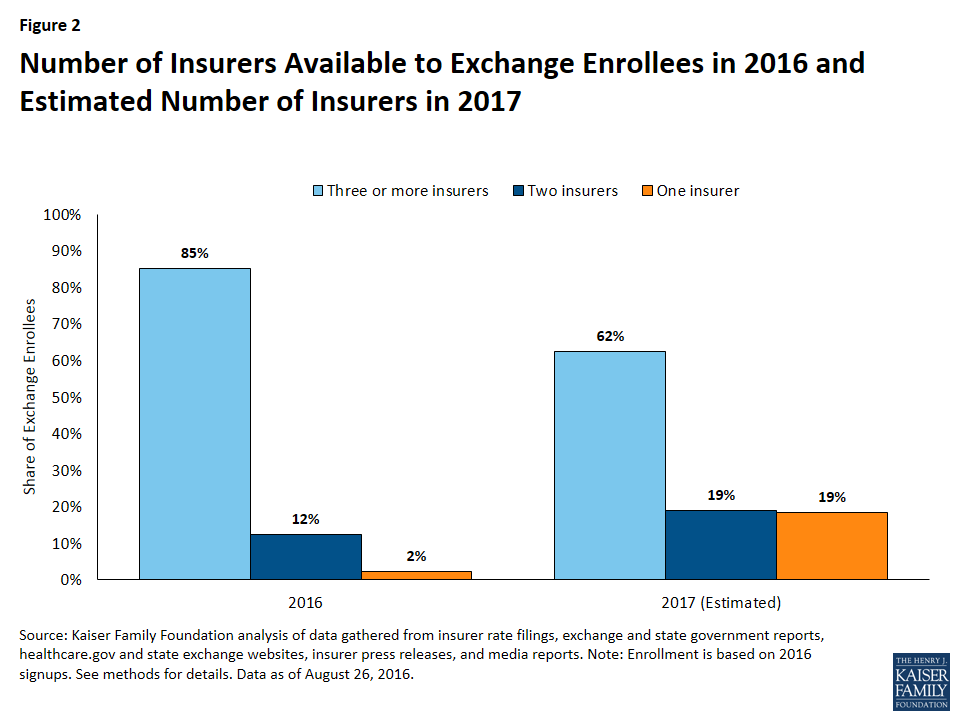
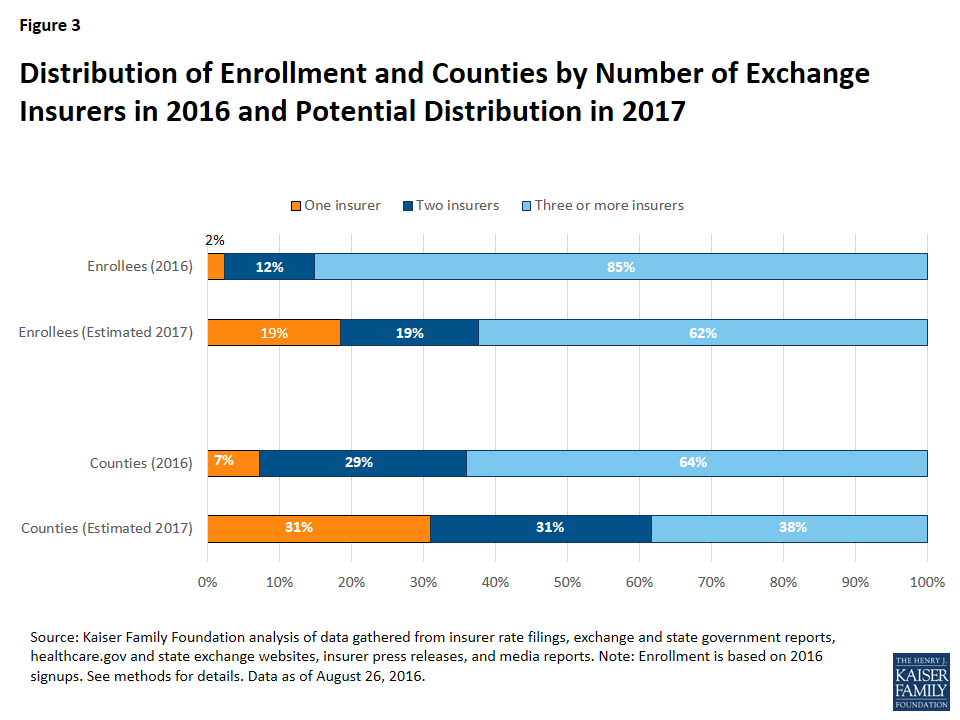
We find that most marketplace enrollees will likely continue to have a choice of three or more plans in 2017, based on what is currently known of marketplace insurer participation and changes next year. However, assuming county-level enrollment holds steady from 2016 to 2017, a smaller share of enrollees will likely have a choice of three or more insurers in 2017 than in previous years. We estimate that 62% of enrollees in 2017 will have a choice of three or more insurers, compared to 85% of enrollees in 2016.
We estimate that 2.3 million marketplace enrollees, or 19% of all enrollees, could have a choice of a single insurer in 2017, which is an increase of 2 million people compared to 2016. Going into marketplace open enrollment in 2016, about 303,000 enrollees (2%) had a single insurer option.
Similarly, we estimate that the number of counties with a single marketplace insurer is likely to increase, from 225 (7% of counties) in 2016 to 974 (31% of counties) in 2017. Approximately 6 in 10 counties could have 2 or fewer marketplace insurers in 2017. The bulk of the increase in single-insurer counties is a result of the UnitedHealth exit, as the company was often the second insurer in rural areas.
In 2016, counties with a single marketplace insurer are concentrated in a handful of states, particularly rural ones: Wyoming (where 100% of counties have one insurer), West Virginia (82%), Utah (69%), South Carolina (63%), and Nevada (59%).
Given what is known at this time of entrants and exits, four additional states are likely to have a single marketplace insurer in all counties: Alabama, Alaska, Oklahoma, and South Carolina, for a total of five states (including Wyoming, which already had one insurer in the state). Other states with significantly more single-insurer counties in 2017 will likely include Arizona (87% of counties in 2017, compared to none in 2016), Mississippi (80% vs. 0%), Missouri (85% vs. 2%), Florida (73% vs. 0%), North Carolina (90% vs. 23%), and Tennessee (60% vs. 0%). With the exception of Alaska, the states left with the most limited exchange participation as a result of 2017 market exits are likely to be in the south.
One county, Pinal County in Arizona, could be at risk of having no insurer options on the marketplace, given what is currently known of exits in the state. However, this could change as another plan that offers elsewhere in the state could expand its service area. In the figures cited in the paragraph above, Pinal County is grouped with single-insurer counties in Arizona.
Rural areas have historically had lower insurer participation, so even one exit can have a significant effect on consumer choice. About 629,000 marketplace enrollees who live in primarily rural counties will likely have a single insurer in 2017, representing 41% of all marketplace enrollees living in mostly rural counties (up from 7% in 2016). Marketplace enrollees living in some urban areas will also have less choice as a result of the exits. As many as 1.7 million enrollees who live in primarily urban counties could have a single marketplace insurer in 2017, representing 15% of all enrollees living in mostly urban counties (up from 2% in 2016).
About 7.9 million enrollees are likely to have three or more choices of marketplace insures in 2017, based on information currently available on entrants and exits. Of these enrollees with at least three choices, the vast majority (7.4 million) live in counties that are primarily urban, while 504,000 live in counties that are primarily rural. Our analysis of information currently available finds that about two out of every three enrollees in primarily urban counties (66%) will likely have a choice of at least three marketplace insurers in 2017, while one in three enrollees in primarily rural counties (33%) are likely to have a choice of three or more insurers.
The map below shows counties where we estimate there could be one or two marketplace insurers in 2017, and the 50-state tables show changes in the number of counties with one insurer from 2016 to 2017 in each state.
| Table 1: Distribution of Counties by Number of Exchange Insurers in 2016 and Potential Distribution in 2017 | ||||||||
| State | 2016 | 2017 (Estimated) | ||||||
| No Insurer | 1 Insurer | 2 Insurer | 3+ Insurer | No Insurer | 1 Insurer | 2 Insurer | 3+ Insurer | |
| AL | – | – | 60 (90%) | 7 (10%) | – | 67 (100%) | – | – |
| AK | – | – | 30 (100%) | – | – | 30 (100%) | – | – |
| AZ | – | – | 8 (53%) | 7 (47%) | 1 (7%) | 12 (80%) | 2 (13%) | – |
| AR | – | – | – | 75 (100%) | – | – | – | 75 (100%) |
| CA | – | – | 1 (2%) | 57 (98%) | – | – | 27 (47%) | 31 (53%) |
| CO | – | – | 4 (6%) | 60 (94%) | – | – | 47 (73%) | 17 (27%) |
| CT | – | – | – | 8 (100%) | – | – | 8 (100%) | – |
| DE | – | – | 3 (100%) | – | – | – | 3 (100%) | – |
| DC | – | – | 1 (100%) | – | – | – | 1 (100%) | – |
| FL | – | – | 44 (66%) | 23 (34%) | – | 49 (73%) | 8 (12%) | 10 (15%) |
| GA | – | – | 30 (19%) | 129 (81%) | – | 77 (48%) | 49 (31%) | 33 (21%) |
| HI | – | – | 5 (100%) | – | – | – | 5 (100%) | – |
| ID | – | – | – | 44 (100%) | – | – | – | 44 (100%) |
| IL | – | – | – | 102 (100%) | – | 8 (8%) | 69 (68%) | 25 (25%) |
| IN | – | – | – | 92 (100%) | – | – | 27 (29%) | 65 (71%) |
| IA | – | – | 21 (21%) | 78 (79%) | – | – | 49 (49%) | 50 (51%) |
| KS | – | – | 105 (100%) | – | – | – | 105 (100%) | – |
| KY | – | – | 66 (55%) | 54 (45%) | – | 54 (45%) | 48 (40%) | 18 (15%) |
| LA | – | – | – | 64 (100%) | – | – | 59 (92%) | 5 (8%) |
| ME | – | – | – | 16 (100%) | – | – | – | 16 (100%) |
| MD | – | – | – | 24 (100%) | – | – | – | 24 (100%) |
| MA | – | – | – | 14 (100%) | – | – | – | 14 (100%) |
| MI | – | 14 (17%) | 24 (29%) | 45 (54%) | – | 14 (17%) | 27 (33%) | 42 (51%) |
| MN | – | – | – | 87 (100%) | – | – | 26 (30%) | 61 (70%) |
| MS | – | – | 50 (61%) | 32 (39%) | – | 66 (80%) | 16 (20%) | – |
| MO | – | – | 2 (2%) | 113 (98%) | – | 98 (85%) | 13 (11%) | 4 (3%) |
| MT | – | – | – | 56 (100%) | – | – | – | 56 (100%) |
| NE | – | – | – | 93 (100%) | – | – | 2 (2%) | 91 (98%) |
| NV | – | 10 (59%) | 4 (24%) | 3 (18%) | – | 10 (59%) | 4 (24%) | 3 (18%) |
| NH | – | – | – | 10 (100%) | – | – | – | 10 (100%) |
| NJ | – | – | – | 21 (100%) | – | – | – | 21 (100%) |
| NM | – | – | – | 33 (100%) | – | – | – | 33 (100%) |
| NY | – | – | 3 (5%) | 59 (95%) | – | – | 3 (5%) | 59 (95%) |
| NC | – | 23 (23%) | 38 (38%) | 39 (39%) | – | 90 (90%) | 10 (10%) | – |
| ND | – | – | 4 (8%) | 49 (92%) | – | – | 4 (8%) | 49 (92%) |
| OH | – | – | – | 88 (100%) | – | – | 5 (6%) | 83 (94%) |
| OK | – | – | 77 (100%) | – | – | 77 (100%) | – | – |
| OR | – | – | – | 36 (100%) | – | – | – | 36 (100%) |
| PA | – | – | – | 67 (100%) | – | 5 (7%) | 34 (51%) | 28 (42%) |
| RI | – | – | – | 5 (100%) | – | – | 5 (100%) | – |
| SC | – | 29 (63%) | 15 (33%) | 2 (4%) | – | 46 (100%) | – | – |
| SD | – | – | 66 (100%) | – | – | – | 66 (100%) | – |
| TN | – | – | 57 (60%) | 38 (40%) | – | 57 (60%) | 24 (25%) | 14 (15%) |
| TX | – | 58 (23%) | 110 (43%) | 86 (34%) | – | 88 (35%) | 129 (51%) | 37 (15%) |
| UT | – | 20 (69%) | 3 (10%) | 6 (21%) | – | 20 (69%) | 2 (7%) | 7 (24%) |
| VT | – | – | 14 (100%) | – | – | – | 14 (100%) | – |
| VA | – | – | 37 (28%) | 97 (72%) | – | 29 (22%) | 38 (28%) | 67 (50%) |
| WA | – | – | 6 (15%) | 33 (85%) | – | 5 (13%) | 11 (28%) | 23 (59%) |
| WV | – | 45 (82%) | 10 (18%) | – | – | 45 (82%) | 10 (18%) | – |
| WI | – | 3 (4%) | 7 (10%) | 62 (86%) | – | 4 (6%) | 13 (18%) | 55 (76%) |
| WY | – | 23 (100%) | – | – | – | 23 (100%) | – | – |
| US | – | 225 (7%) | 905 (29%) | 2,014 (64%) | 1 (0%) | 974 (31%) | 963 (31%) | 1,206 (38%) |
| Source: Kaiser Family Foundation analysis as of August 26, 2016. | ||||||||
| Table 2: Distribution of Enrollees by Number of Exchange Insurers in 2016 and Potential Distribution in 2017 | ||||||||
| State | 2016 | 2017 (Estimated) | ||||||
| No Insurer | 1 Insurer | 2 Insurer | 3+ Insurer | No Insurer | 1 Insurer | 2 Insurer | 3+ Insurer | |
| AL | – | – | 130,000 (67%) | 65,000 (33%) | – | 195,000 (100%) | – | – |
| AK | – | – | 23,000 (100%) | – | – | 23,000 (100%) | – | – |
| AZ | – | – | 31,000 (15%) | 172,000 (85%) | 10,000 (5%) | 36,000 (18%) | 157,000 (78%) | – |
| AR | – | – | – | 74,000 (100%) | – | – | – | 74,000 (100%) |
| CA | – | – | 1,000 (0%) | 1,575,000 (100%) | – | – | 86,000 (5%) | 1,489,000 (95%) |
| CO | – | – | 8,000 (5%) | 143,000 (95%) | – | – | 30,000 (20%) | 120,000 (80%) |
| CT | – | – | – | 116,000 (100%) | – | – | 116,000 (100%) | – |
| DE | – | – | 28,000 (100%) | – | – | – | 28,000 (100%) | – |
| DC | – | – | 23,000 (100%) | – | – | – | 23,000 (100%) | – |
| FL | – | – | 268,000 (15%) | 1,475,000 (85%) | – | 352,000 (20%) | 258,000 (15%) | 1,133,000 (65%) |
| GA | – | – | 20,000 (3%) | 568,000 (97%) | – | 81,000 (14%) | 83,000 (14%) | 424,000 (72%) |
| HI | – | – | 15,000 (100%) | – | – | – | 15,000 (100%) | – |
| ID | – | – | – | 101,000 (100%) | – | – | – | 101,000 (100%) |
| IL | – | – | – | 388,000 (100%) | – | 56,000 (14%) | 99,000 (26%) | 233,000 (60%) |
| IN | – | – | – | 196,000 (100%) | – | – | 24,000 (12%) | 172,000 (88%) |
| IA | – | – | 5,000 (10%) | 50,000 (90%) | – | – | 17,000 (31%) | 38,000 (69%) |
| KS | – | – | 102,000 (100%) | – | – | – | 102,000 (100%) | – |
| KY | – | – | 31,000 (33%) | 63,000 (67%) | – | 26,000 (28%) | 32,000 (35%) | 35,000 (38%) |
| LA | – | – | – | 214,000 (100%) | – | – | 131,000 (61%) | 83,000 (39%) |
| ME | – | – | – | 84,000 (100%) | – | – | – | 84,000 (100%) |
| MD | – | – | – | 162,000 (100%) | – | – | – | 162,000 (100%) |
| MA | – | – | – | 214,000 (100%) | – | – | – | 214,000 (100%) |
| MI | – | 13,000 (4%) | 57,000 (17%) | 276,000 (80%) | – | 13,000 (4%) | 59,000 (17%) | 274,000 (79%) |
| MN | – | – | – | 84,000 (100%) | – | – | 13,000 (16%) | 70,000 (84%) |
| MS | – | – | 47,000 (43%) | 62,000 (57%) | – | 63,000 (58%) | 46,000 (42%) | – |
| MO | – | – | 4,000 (1%) | 286,000 (99%) | – | 101,000 (35%) | 136,000 (47%) | 53,000 (18%) |
| MT | – | – | – | 58,000 (100%) | – | – | – | 58,000 (100%) |
| NE | – | – | – | 88,000 (100%) | – | – | 1,000 (1%) | 87,000 (99%) |
| NV | – | 3,000 (3%) | 6,000 (7%) | 79,000 (90%) | – | 3,000 (3%) | 6,000 (7%) | 79,000 (90%) |
| NH | – | – | – | 55,000 (100%) | – | – | – | 55,000 (100%) |
| NJ | – | – | – | 289,000 (100%) | – | – | – | 289,000 (100%) |
| NM | – | – | – | 55,000 (100%) | – | – | – | 55,000 (100%) |
| NY | – | – | 2,000 (1%) | 269,000 (99%) | – | – | 2,000 (1%) | 269,000 (99%) |
| NC | – | 50,000 (8%) | 155,000 (25%) | 409,000 (67%) | – | 490,000 (80%) | 123,000 (20%) | – |
| ND | – | – | 1,000 (3%) | 21,000 (97%) | – | – | 1,000 (3%) | 21,000 (97%) |
| OH | – | – | – | 244,000 (100%) | – | – | 3,000 (1%) | 241,000 (99%) |
| OK | – | – | 145,000 (100%) | – | – | 145,000 (100%) | – | – |
| OR | – | – | – | 147,000 (100%) | – | – | – | 147,000 (100%) |
| PA | – | – | – | 439,000 (100%) | – | 173,000 (39%) | 143,000 (33%) | 124,000 (28%) |
| RI | – | – | – | 35,000 (100%) | – | – | 35,000 (100%) | – |
| SC | – | 91,000 (39%) | 116,000 (50%) | 25,000 (11%) | – | 232,000 (100%) | – | – |
| SD | – | – | 26,000 (100%) | – | – | – | 26,000 (100%) | – |
| TN | – | – | 79,000 (29%) | 190,000 (71%) | – | 79,000 (29%) | 69,000 (26%) | 121,000 (45%) |
| TX | – | 55,000 (4%) | 123,000 (9%) | 1,128,000 (86%) | – | 162,000 (12%) | 383,000 (29%) | 761,000 (58%) |
| UT | – | 34,000 (19%) | 6,000 (3%) | 136,000 (77%) | – | 34,000 (19%) | 3,000 (2%) | 139,000 (79%) |
| VT | – | – | 29,000 (100%) | – | – | – | 29,000 (100%) | – |
| VA | – | – | 73,000 (17%) | 349,000 (83%) | – | 21,000 (5%) | 91,000 (22%) | 309,000 (73%) |
| WA | – | – | 7,000 (3%) | 194,000 (97%) | – | 7,000 (3%) | 22,000 (11%) | 172,000 (86%) |
| WV | – | 26,000 (70%) | 11,000 (30%) | – | – | 26,000 (70%) | 11,000 (30%) | – |
| WI | – | 7,000 (3%) | 7,000 (3%) | 225,000 (94%) | – | 8,000 (3%) | 12,000 (5%) | 219,000 (92%) |
| WY | – | 24,000 (100%) | – | – | – | 24,000 (100%) | – | – |
| US | – | 303,000 (2%) | 1,578,000 (12%) | 10,801,000 (85%) | 10,000 (0%) | 2,349,000 (19%) | 2,417,000 (19%) | 7,906,000 (62%) |
| Source: Kaiser Family Foundation analysis as of August 26, 2016. | ||||||||
Methods and Limitations
As complete insurer participation data are not yet available for the 2017 marketplaces, we began our analysis with data on participation in 2016. We gathered these data from healthcare.gov for states with a federally run, partnership, and facilitated marketplaces. For states that run their own exchanges, we compiled 2016 insurer participation data by reviewing rate filings to state regulators and reports released by some states. We then verified county-level data in these states by searching state plan shopping tools. We grouped insurers by parent company or group affiliation, which we obtained from HHS Medical Loss Ratio public use files and supplemented with additional research. We then analyzed, at the county level, how many parent companies participate in these Marketplaces.
Using this data on 2016 insurer participation, we made adjustments based on information we could find on 2017 entrants, exits, scale-backs, and expansions. In total, we made over 600 changes at both the state and county levels. We took two different approaches, depending on the amount of information that is available in a given state:
- In the 17 states included in our 2017 premium and participation analysis published in July, 2016 we are able to account for changes in participation, including new entrants and service area expansions based on rate filings to state regulators. For example, in California, the start-up insurer Oscar had already participated in 2016 and is planning to expand to other parts of the state in 2017, according to a report by the exchange. In the 17 states in our premium analysis where detailed information is available, we also compared insurer participation in 2016 and 2017 to account for any scale-backs. For example, we found that Sentara (Optima) is scaling back its participation in many Virginia counties, while remaining in some counties. We then supplemented rate filing data with media reports when necessary. For example, Aetna had submitted filings to enter into the Indiana exchange, but reportedly no longer intends to expand into new states, so we do not include the company as a new entrant.–
- In other states not included in our July analysis, we also account for new entrants, scale-backs, and expansions where we could find this information through news coverage and press releases, and attempted to verify these reports against redacted rate filings available on Healthcare.gov. For all reported new entrants in our analysis, we attempt to verify the counties and/or regions they would service rather than assuming state-wide entry. For example, a press release indicates that Medica is entering the entire state of Kansas, while Wellcare is entering 47 counties in Iowa. In cases where a new entrant is reported to offer in a specific metro area, but where counties are not specified and no detailed filing is available, for example in the case of Cigna reportedly entering into Raleigh, NC and other cities, we treat the company as if it is entering the rating area that includes the major city.–We also attempt to account for reported scale-backs, or insurers continuing to offer in states but with a more limited service area, when information is available. In these states where detailed filings are not publicly available, we rely on what is known of insurers’ current participation and what has been reported of their future participation. For example, in Georgia, UnitedHealth Group will no longer offer plans under its subsidiary United Healthcare but reportedly will continue to offer through another subsidiary, Harken Health. Therefore, we treat UnitedHealth Group as exiting all counties in Georgia with the exception of those counties where Harken Health branded plans are currently offered.
To the extent possible, we have attempted to account for any reported entrant, exit, scale-back, or expansion in our analysis, but are limited in our ability to do so because the market is undergoing changes, data are limited, and we may not be aware of all developments even if they have been reported. The information we gathered for this analysis is still preliminary and will continue to evolve over the coming months as more information becomes public. We intend to update this analysis when more complete data are available for 2017 exchange insurer participation.–Enrollment numbers in this analysis are based on 2016 exchange signups as of the end of open enrollment (February 2016). In states using Healthcare.gov, county level enrollment is made available by The U.S. Department of Health and Human Services. In states that run their own exchanges, county-level enrollment is estimated by distributing total state enrollment by county population using data from the Missouri Census Data Center. All estimates relating to 2017 enrollment assume that enrollment at the county level holds steady from 2016 to 2017, but total enrollment will likely change as will the distribution of enrollment across counties. The percent of county population residing in rural areas was obtained from the Missouri Census Data Center. Counties where more than 50% of the population lives in rural areas are considered primarily rural and other counties are considered primarily urban.
A Final Look: California’s Previously Uninsured after the ACA’s Third Open Enrollment Period
Executive Summary
The Kaiser Family Foundation California Longitudinal Panel Survey is a series of surveys that, over time, tracked the experiences and views of a representative, randomly selected sample of Californians who were uninsured prior to the major coverage expansions under the Affordable Care Act (ACA). The initial baseline survey was conducted with a representative sample of 2,001 nonelderly uninsured Californian adults in summer 2013, prior to the ACA’s initial open enrollment period.
After each enrollment period concluded, a survey was conducted of the same group of previously uninsured Californians who participated in the baseline (a longitudinal panel survey). The fourth and final survey in the series, and the focus of this report, followed up with them after the third open enrollment period in spring 2016 to find out whether more have gained coverage, lost coverage, or remained uninsured, what barriers to coverage remain, how those who now have insurance view their coverage, and to assess the impacts that gaining health insurance may have had on financial security and access to care. The surveys were designed and analyzed by researchers at KFF and the fieldwork costs associated with the spring 2014, spring 2015, and spring 2016 surveys were paid for by The California Endowment.
This longitudinal panel study allows us to follow a large group of randomly selected uninsured Californians and assess how their insurance status changed over time to learn more about why those changes did or did not occur, and what gaining health insurance means for their daily lives without having to rely on respondents’ ability to report and recall details from months or years ago. By tracking a scientifically representative panel, we can quantify how widespread or limited certain problems or changes that may have been reported anecdotally actually were. Statistically representative narratives and stories from individuals’ actual experiences can then be drawn from the sample to illuminate more accurately how the uninsured fare as the law is implemented in California.
Key Findings
Coverage Among Key Groups
After three rounds of open enrollment under the Affordable Care Act, 72 percent of Californians who were uninsured prior to the first open enrollment period now report that they have health insurance (including 78 percent of all eligible individuals). This is similar to the share who reported having insurance last year, after the second open enrollment period (68 percent). The largest share of California’s previously uninsured, one-third, say they have coverage through the state’s Medicaid program, Medi-Cal, while 21 percent say they have insurance through an employer, about one in ten (11 percent) say they have a plan through Covered California — the state’s health insurance marketplace where people can shop for and compare health insurance plans and access federal subsidies for coverage — and another 8 percent say they have non-group coverage or insurance through some other source.
By tracking the insurance status of these individuals over a period of four years, it is clear that the majority of individuals who get health insurance coverage keep some form of coverage. Sixty-three percent of habitual survey respondents report having had health insurance for a period of at least one year, including 48 percent who have had coverage for at least two years. In fact, 14 percent of the habitual respondents have unstable health insurance status, meaning that they have gained health insurance in the past two years and have subsequently lost their coverage. Of the individuals with unstable health insurance status, 5 percent gained coverage again but 9 percent remain without health insurance coverage.
Gains In Financial Security and Health Needs Being Met For Recently Insured
Overall, Californians who recently obtained health insurance are more likely to report that their health needs are being met today than they were in 2013. About three-fourths (77 percent) of those who report now having coverage after the third open enrollment period say their health needs are being met either “very” or “somewhat” well today, while half of them (49 percent) said the same thing when they were uninsured in summer 2013, prior to the first open enrollment period. This is compared to the remaining uninsured, among whom a similar share say their health needs are being met well today as did in 2013 (62 percent compared to 59 percent). In addition, 60 percent of insured Californians currently say it is difficult for them to afford health care. While this is still more than half, it is considerably smaller than the 85 percent of these individuals who reported the same in 2013. And while half (53 percent) of California’s recently insured are still “very worried” that they would not be able to pay medical bills in the event of a serious illness or accident, this is a smaller share than the percent of these who reported being “very worried” in 2013 (80 percent) and smaller than the share of the remaining uninsured who now report being “very worried” (72 percent).
Most Rate Plan Favorably, But Some Report Access Challenges
The majority of the recently insured say their experiences with their current health insurance plan have been positive. About one-third (31 percent) say their experiences have been very positive with an additional 48 percent saying their experiences have been somewhat positive. Only 15 percent say their experiences have been negative. Despite this, one-fifth of the recently insured report forgoing needed medical care in the past year due to cost. But this share is smaller than the share of those remaining without insurance (32 percent) who report not getting medical care due to costs. The share of those with insurance who have foregone medical care due to costs is similar across insurance type, with about one in five of those with Medi-Cal, Covered California, and employer-sponsored insurance saying they have not gotten care due to costs. In addition, some of the recently insured report problems accessing medical care. One-fourth of the recently insured say they have had to wait longer than a reasonable time to get an appointment for medical care and about one in ten (12 percent) say they have been told by a doctor’s office or clinic in the past 12 months that they would not be accepted as a new patient.
Remaining Uninsured Are Largely Long-Term Uninsured, Cite Costs As Reason For Not Getting Insurance
Although many previously uninsured Californians gained coverage since the health care law went into effect, 27 percent report that they do not currently have health insurance. Many of these remaining uninsured had little interaction with the health insurance system in the years prior to the ACA implementation. Nearly four in ten of the remaining uninsured reported in the baseline survey that they had been without health insurance for two or more years. When asked to say in their own words the main reason why they do not currently have health insurance, 47 percent of California’s remaining uninsured say it is because health insurance is too expensive and they can’t afford it. This is in spite of the fact that many of the remaining uninsured report a family income that makes them likely eligible for Medi-Cal (27 percent) or for financial assistance through Covered California (30 percent).
Hispanics Lag in Coverage
One-third of the Hispanic individuals included in the panel still do not have insurance. A significant portion of these uninsured Hispanics may not have insurance due to the fact that they are not eligible for coverage because of their immigration status. Of all eligible Hispanics in this survey, three-fourths (76 percent) report having health insurance, which is similar to the share of non-Hispanic whites who report having health insurance (80 percent).
Most Know About Health Care Law Fines, Fewer Know About Provisions
A large share (83 percent) of the remaining uninsured in California are aware of the health care law’s requirement that most Americans have health insurance or pay a fine, and most (54 percent) think that the requirement applies to them. Smaller shares of the remaining uninsured are aware of provisions of the health care law, beyond the requirement to have coverage, intended to expand coverage to the uninsured and those with lower-incomes. Just over half know that the law allowed for the expansion of the Medi-Cal program to cover more low-income Californians (54 percent), and half (49 percent) know that the law provides financial help to low- and moderate-income people to help them purchase health insurance coverage.
Introduction
This report is the fourth, and final, in the California Longitudinal Panel Survey series examining how previously uninsured Californians navigate the health care system as the Affordable Care Act (ACA) goes into effect. Prior to the enactment of the health care law, California had the largest nonelderly uninsured adult population in the nation, at nearly 6 million.1 The state eagerly adopted options under the ACA to expand coverage to more low- and moderate-income people, primarily through the development of Covered California, the state’s marketplace where people can shop for and compare health plans and access financial help to purchase insurance, and by expanding eligibility for Medi-Cal, the state’s Medicaid program, to include parents and adults without dependent children earning 138% of the federal poverty level (FPL) or less (about $33,534 annually for a family of 4 in 2016). As an early adopter with large numbers of uninsured, California is a particularly valuable place to track how the rollout of the health care law has impacted the state’s uninsured, and its progress and challenges can help inform future enrollment efforts state-wide and nationally.
To track the experiences and perceptions of California’s uninsured as the ACA is implemented, the Kaiser Family Foundation conducted the California Longitudinal Panel Survey series, following the same group of randomly selected Californians over time who were uninsured prior to the major coverage expansions under the ACA. The initial baseline survey was conducted with a representative sample of 2,001 nonelderly uninsured Californian adults in summer 2013, prior to the ACA’s initial open enrollment period.2 It found most of the state’s uninsured said they wanted insurance but that most didn’t think they could afford it, as the vast majority reported family incomes under 400% FPL (about $94,000 a year for a family of 4 in 2013). At that time, the first open enrollment period under the ACA was just a couple months away, and many of California’s uninsured were unaware of the upcoming coverage expansion opportunities and were unsure of how the law would impact them.
After the first open enrollment concluded in spring 2014, the second survey in the series followed up with the same group of previously uninsured Californians to find out whether they gained coverage or remained uninsured, how they felt about and interacted with the new coverage options, and what barriers to getting insurance remained.3 Many (58 percent) of California’s previously uninsured reported having health insurance at the close of the first open enrollment period. Most reported that shopping for coverage went smoothly; however, some expressed difficulty affording the cost of coverage. Still, about four in ten remained uninsured, despite the fact that many reported incomes that put them in the group likely eligible for Medi-Cal or for financial assistance through Covered California. The third survey in the series found recently insured residents reported very different experiences than they did in 2013 when they were uninsured, but many still reported problems paying for and accessing care.4
While the surveys are generally timed around the ACA’s open enrollment periods, it is important to note that eligible individuals are able to enroll in Medi-Cal year round. California has made considerable strides in enrolling eligible low- and moderate-income people in new coverage options under the ACA. By following a representative group of Californians who were uninsured prior to the ACA’s coverage expansions, a key target of the ACA, we can better understand how these new coverage opportunities have impacted this group’s ability to access coverage and gain insight into their interactions with these new pathways to coverage.
While the ACA makes it easier for some people to get and keep coverage, other people will move in and out of coverage due to job status changes, shifts in income that change their eligibility for public subsidies or coverage, or missed deadlines for enrollment. While many previously uninsured Californians now have insurance, other Californians who had insurance prior to the ACA’s coverage expansions may now be uninsured, a group whose experiences and movements within the health care system are not captured in this series of surveys. As a result, this survey does not estimate the overall change in the number of uninsured Californians since the start of open enrollment but instead estimates the share of previously uninsured who gained coverage.
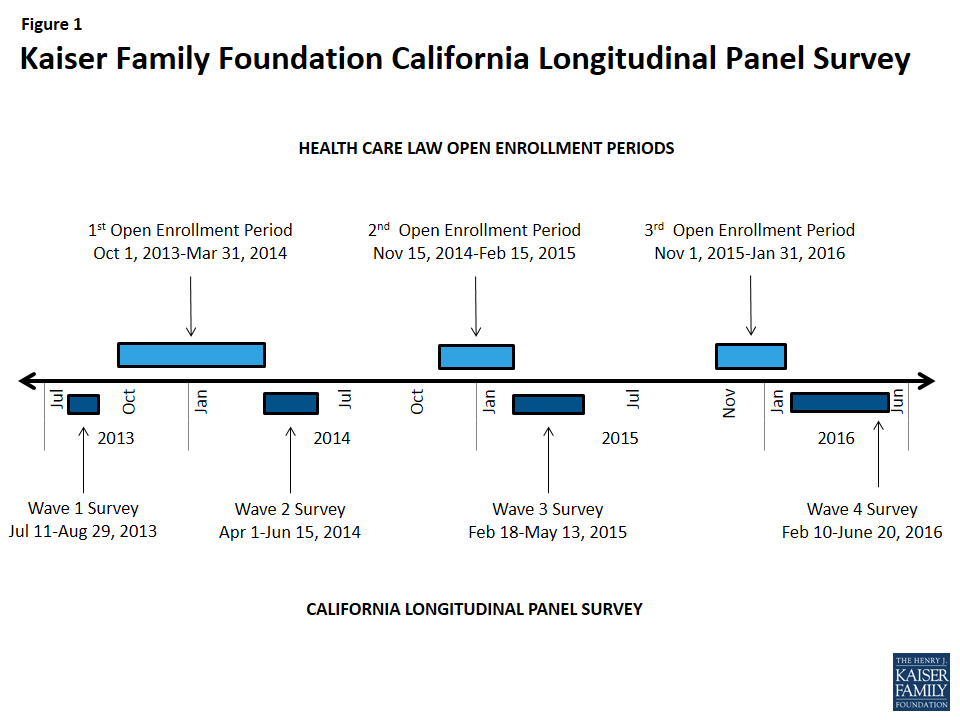
Section 1: Coverage Among The Previously Uninsured
Enrolling in Health Care Coverage
After three rounds of open enrollment under the Affordable Care Act, 72 percent of Californians who were uninsured prior to the first open enrollment period now report that they have health insurance. This is similar to the share who were insured after the second open enrollment period (68 percent), which may indicate a stabilizing of health insurance coverage. About one-fourth (27 percent) report being currently uninsured, a group referred to throughout this report as the “remaining uninsured.” Excluding those who are likely ineligible for coverage under the ACA due to their immigration status,5 78 percent of California’s eligible uninsured now report having coverage.
For the purposes of this report, the “eligible uninsured’” are California residents who said they had been uninsured for at least two months in the baseline survey and would be eligible for participation in the ACA coverage expansion based on their self-reported status as a citizen, permanent resident, or lawfully present immigrant.6
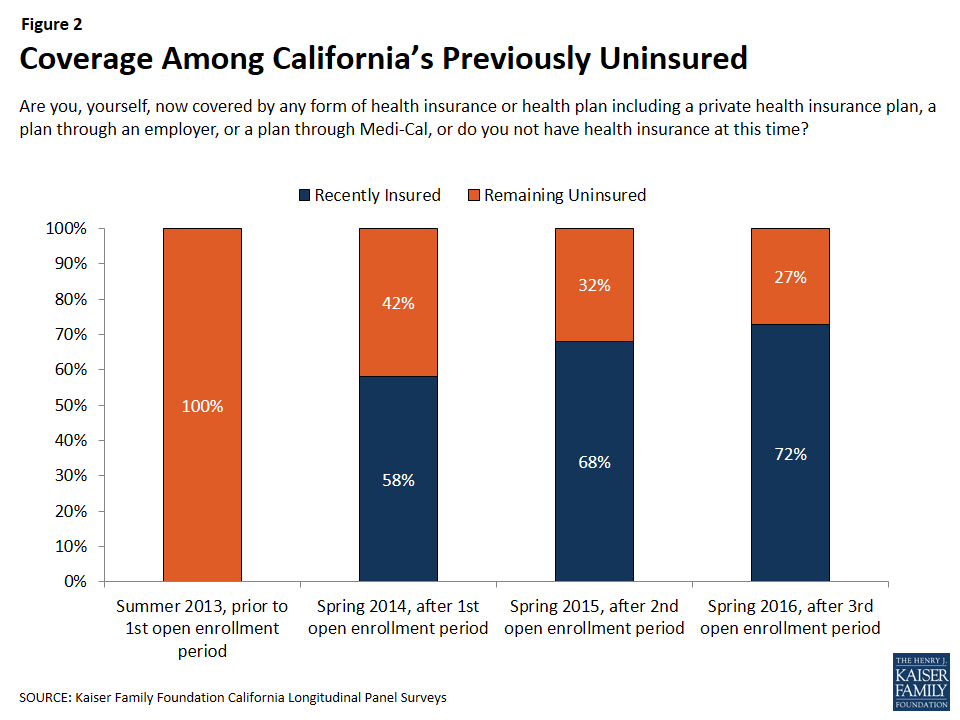
Those previously uninsured Californians who report after the third open enrollment period that they have health insurance (72 percent), referred to throughout this report as “California’s recently insured,” say they gained coverage from several different sources. The largest share of California’s previously uninsured (33 percent) say they have coverage through the state’s Medicaid program, Medi-Cal, which is similar to the share reported in 2015 (34 percent). One in five say they have insurance through an employer, up from 14 percent in 2015. About one in ten (11 percent) say they have a plan through Covered California, the state’s health insurance marketplace where people can shop for and compare health insurance plans and access federal subsidies for coverage, and another 8 percent say they have non-group coverage or insurance through some other source.7
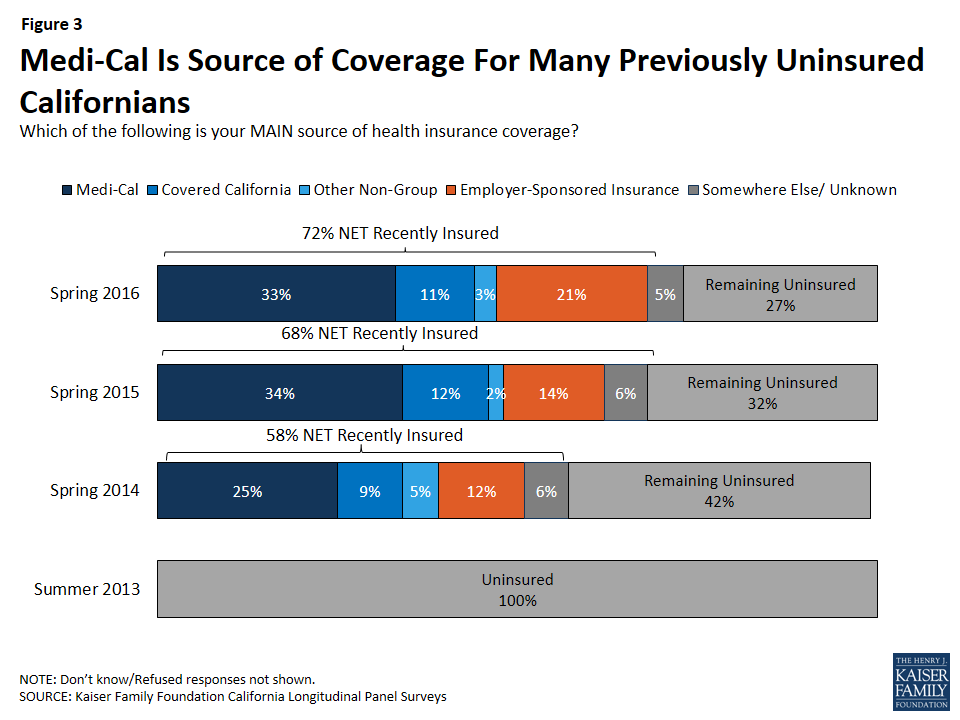
Who Now Has Coverage?
Similar shares of many demographic groups now report having coverage, such as men and women, people of different ages, and people of different employment status, with one notable exception: Hispanic individuals. One-third of previously uninsured Hispanic individuals still do not have insurance, with individuals who may not be eligible for insurance comprising nearly half of this group. This subgroup is examined in more depth in Section 3.
There are some factors that contribute to now being insured. Over half (62 percent) of those who said in 2013 that they had spent their lifetime without insurance now report having coverage while nearly eight in ten of the individuals who reported in 2013 that they had health insurance less than a year earlier report now being insured. Previously uninsured people who report being in good health are slightly less likely to say they have coverage than those who report being in fair or poor health (69 percent v. 78 percent). In addition, those who report having a debilitating chronic disease that keeps them from fully participating in work or other activities are more likely to say they have coverage now than those without significant chronic disease (85 percent vs. 70 percent).
| Table 1: Percentage Of Each Group Of Previously Uninsured Reporting That They Are Recently Insured Or Remain Uninsured | |||||||
| TOTAL RECENTLY INSUREDIN 2016 | COVERAGE TYPE IN 2016 | TOTALREMAININGUNINSUREDIN 2016 | |||||
| Medi-Cal | Covered California | Other Non-Group | Employer-Sponsored Insurance | ||||
| TOTAL | 72% | 33% | 11% | 3% | 21% | 27% | |
| AGE | 19-34 | 70% | 30% | 8% | 1% | 28% | 29% |
| 35-49 | 65% | 28% | 8% | 6% | 20% | 35% | |
| 50-64 | 81% | 42% | 18% | 3% | 14% | 19% | |
| RACE | White non-Hispanic | 80% | 33% | 15% | 6% | 21% | 18% |
| Hispanic (NET) | 67% | 32% | 8% | 2% | 21% | 33% | |
| Hispanic, Eligible | 76% | 37% | 11% | 3% | 22% | 24% | |
| GENDER | Male | 72% | 30% | 10% | 2% | 24% | 27% |
| Female | 73% | 38% | 11% | 5% | 17% | 27% | |
| LENGTH OF TIME UNINSURED PRIOR TO ACA | 2mo – <1 year | 81% | 32% | 10% | 5% | 32% | 19% |
| 1 year to <2 years | 75% | 33% | 7% | 3% | 26% | 25% | |
| 2 or more years | 77% | 35% | 14% | 3% | 19% | 23% | |
| Never had insurance | 62% | 32% | 7% | 3% | 16% | 37% | |
| EMPLOYMENT | Employed | 75% | 27% | 13% | 2% | 31% | 25% |
| Unemployed | 60% | 44% | 8% | 3% | 4% | 38% | |
| A student, retired, on disability, or stay at home parent | 72% | 44% | 7% | 6% | 4% | 28% | |
| EDUCATION | High school or less | 65% | 35% | 6% | 3% | 18% | 34% |
| Some college | 79% | 35% | 15% | 4% | 21% | 21% | |
| College or more | 88% | 22% | 21% | 3% | 36% | 12% | |
| HEALTH STATUS | Excellent/ Very good/ Good | 69% | 30% | 12% | 4% | 20% | 30% |
| Fair/ Poor | 78% | 39% | 8% | 2% | 22% | 22% | |
| MARITAL STATUS | Married | 71% | 27% | 12% | 4% | 23% | 29% |
| Not married | 73% | 37% | 10% | 3% | 20% | 26% | |
| FAMILY INCOME | Less than 138% FPL | 71% | 49% | 4% | 4% | 11% | 29% |
| Between 138% – 400% FPL | 73% | 18% | 17% | 2% | 30% | 27% | |
| DEBILITATING CHRONIC CONDITION | Yes | 85% | 44% | 15% | 3% | 12% | 15% |
| No | 70% | 31% | 10% | 4% | 22% | 30% | |
The Enrollment/Renewal Process
Being contacted by phone, email or a door-to-door visit about signing up for health insurance appears to have played a role in some of California’s previously uninsured gaining or keeping coverage. A large majority (85 percent) of those who say they were personally contacted since November 1st say they now have coverage, compared to 68 percent of those who report that they were not contacted.
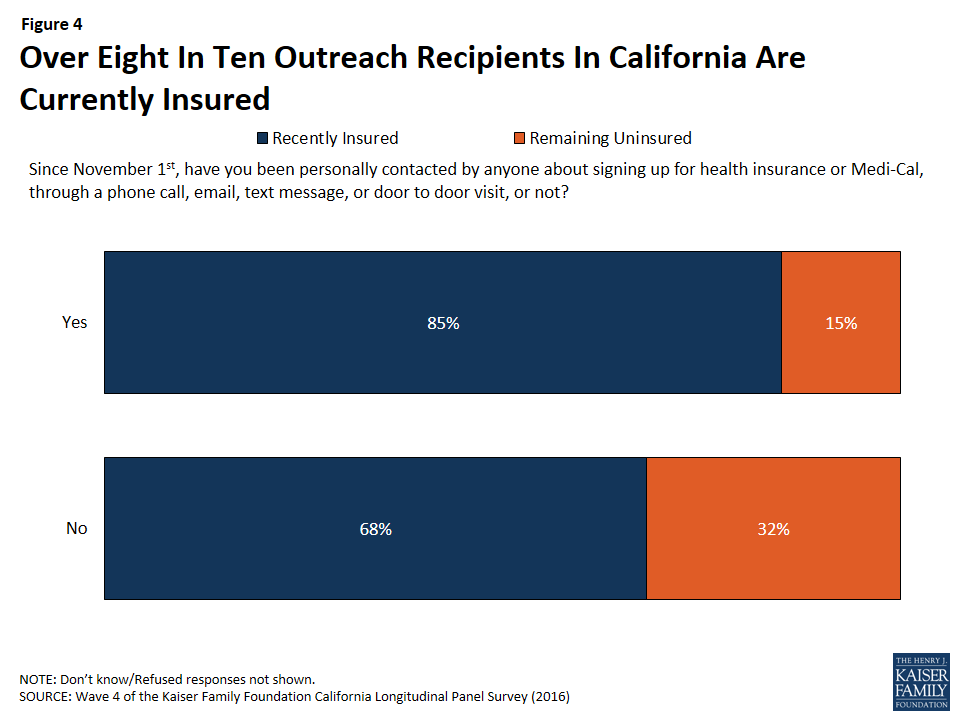
In addition, of the recently insured individuals whose main source of health insurance is not an employer-sponsored plan, 43 percent say that someone either helped them complete the enrollment/renewal process or someone else did the entire thing. This share includes 14 percent who report that a Covered California representative helped them enroll or renew, which is slightly higher than the share (8 percent) who say a community or county health worker helped them or who say a health plan representative helped them. Five percent of recently insured individuals without employer-sponsored coverage say a family member or friend helped them enroll or renew.
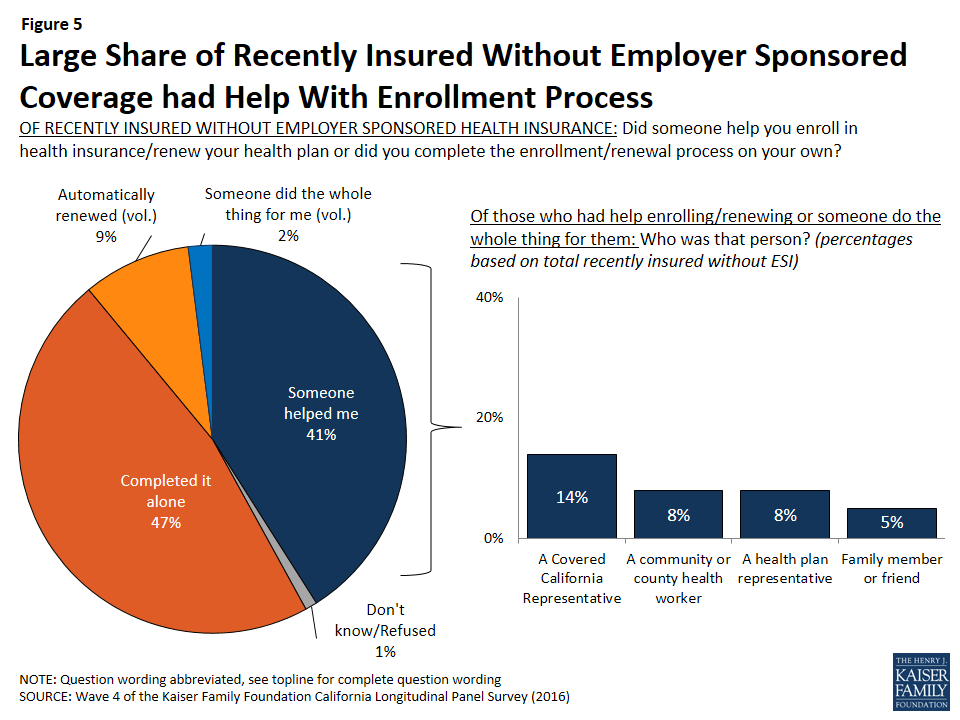
The majority of California’s recently insured (70 percent) have the same plan in 2016 that they did in 2015 while one-fourth say they changed to a different plan and 5 percent were uninsured last year. This is also true of only those who got health insurance through Covered California. Of individuals who currently have health insurance coverage through Covered California, 68 percent say they have the same health insurance plan as they had last year in 2015, one-fourth say they changed to a different plan, and 7 percent were uninsured in 2015.
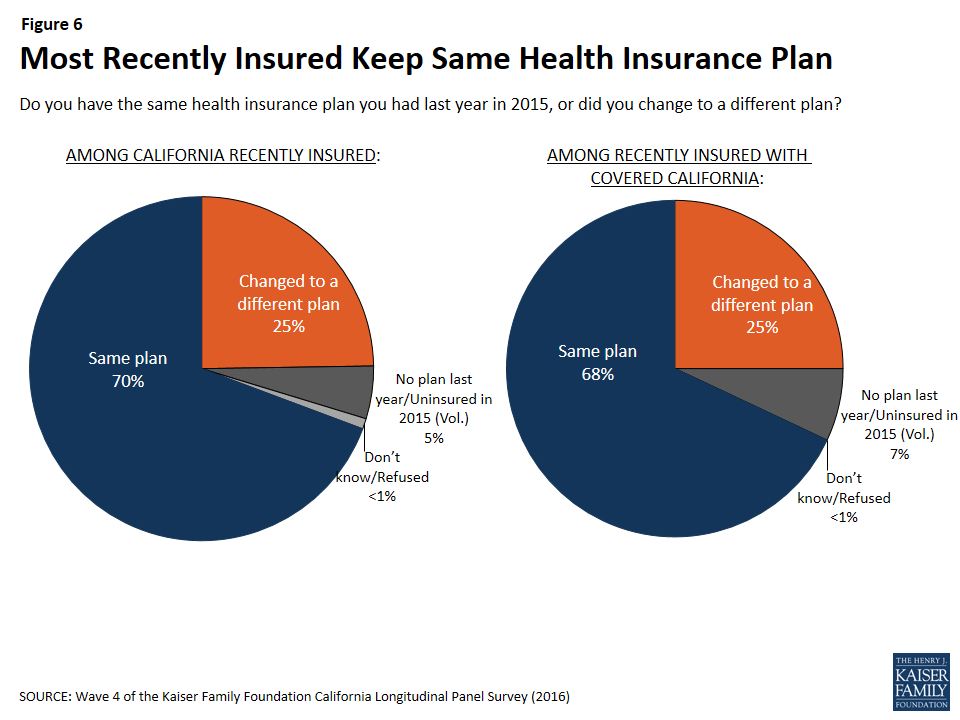
For most recently insured, re-enrolling was automatic, with two-thirds saying they were re-enrolled in the same health plan without having to take any action while one-third say they took action to re-enroll in their same health plan. Only 15 percent of those who kept the same plan as they had last year shopped around for another health plan (9 percent of total insured).
Changing Health Insurance Plans
Of the one-fourth of California’s recently insured who did change health insurance plans, about three-fourths (77 percent) found the process either “very easy” or “somewhat easy” while 22 percent say the process was either “somewhat” or “very” difficult.
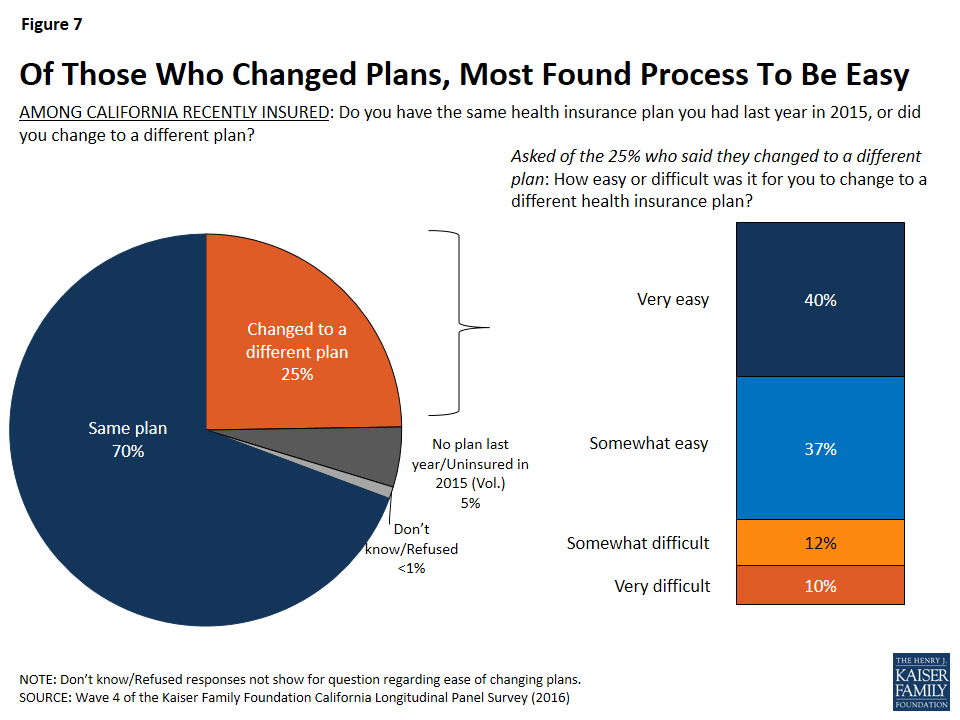
When those who had changed plans in the past year were asked their reasoning for switching to a different health plan, more than half (56 percent) say it was because their income changed. This was followed by half (49 percent) who say it was because they were able to enroll in an employer-sponsored plan, 31 percent who found a plan with a lower monthly premium, 28 percent who wanted a plan with more choice in providers, 27 percent who wanted a plan with a lower annual deductible, and 22 percent who said their or their family’s health needs changed. Only 5 percent say they changed health plans because they wanted to be eligible for government financial help.8
Dynamics In Enrollment And Coverage
People tend to move in and out of coverage as their income, employment status and other life factors change, particularly those with lower incomes or recent experience being uninsured. Many (57 percent) Californians who reported being uninsured in 2013, prior to the ACA’s first open enrollment period, reported gaining insurance in the spring 2014 or the second open enrollment period (spring 2015), and now report still having insurance coverage after the third open enrollment period (spring 2016). These individuals are referred to here as those “still insured.”9 While these people may have fluctuated in and out of coverage or changed plans over the course of the past two years, they are not new to health insurance. Another 15 percent of California’s previously uninsured are more likely to be new to their coverage because they reported being uninsured in the survey they most recently completed (whether it was Wave 3 or Wave 2). This group is referred to here as the “newly insured.”10 In addition, 22 percent of people reported being uninsured after three open enrollment periods and another 5 percent said they had coverage in the most recent survey they completed (either Wave 3 or Wave 2) but now say they are without health insurance. These groups combined are referred to here as the “remaining uninsured.” To see a demographic profile of each of these groups, see Appendix A.
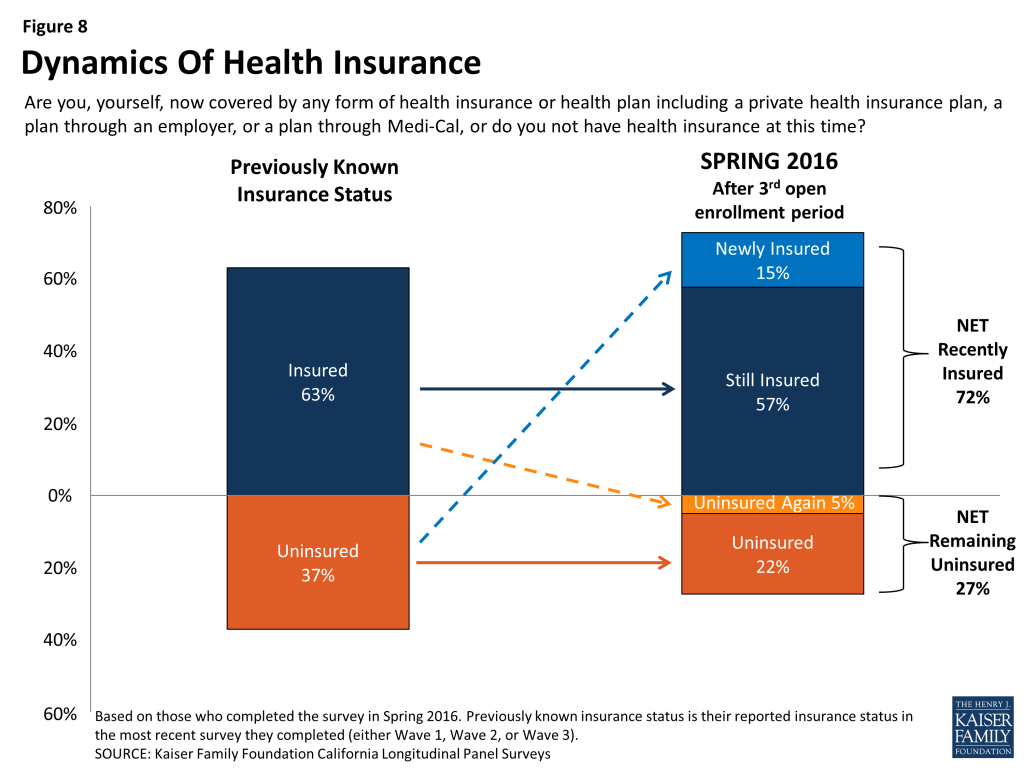
Getting Health Insurance Coverage and Keeping Coverage
By tracking the insurance status of these individuals over a period of four years, it is clear that the majority of individuals who get health insurance coverage keep some form of coverage. Individuals who completed all four waves of interviews are known as “habitual respondents.” In the first survey, conducted in 2013, 70 percent of the habitual respondents reported not having health insurance for a period of at least 2 years. Now, after collecting the insurance status of these individuals over the past three years, we can report that 63 percent of these individuals have reported having health insurance for at least one year, including 48 percent who have had coverage for at least two years. In addition, 14 percent of the habitual respondents have unstable health insurance status meaning that they have gotten health insurance in the past two years and have subsequently lost their coverage. Of the individuals with unstable health insurance status, 5 percent gained coverage again but 9 percent remain without health insurance coverage.
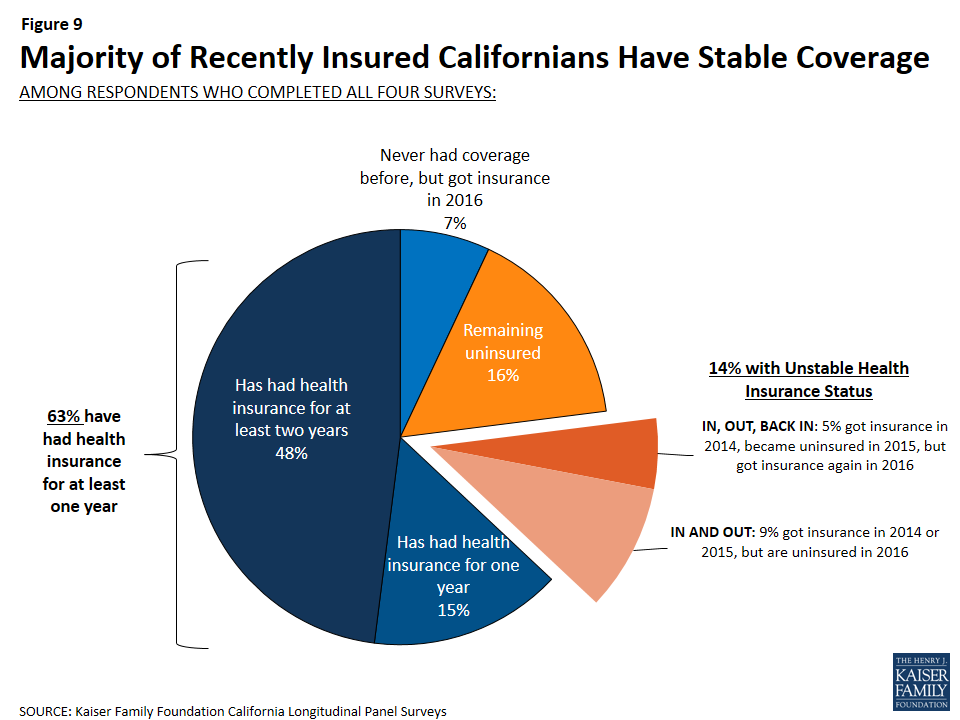
Section 2: Financial Security, Health-related Worries, Accessing Care, And Evaluations Of Insurance Plans
By repeatedly contacting individuals who participated in a baseline survey, one of the strengths of the California Longitudinal Panel Survey is to track the experiences and perceptions of these individuals over time, while comparing their current experiences to previous experiences. One of the ways this is best illustrated is by comparing the change over time between individuals who recently got health insurance and those who remain uninsured.
Overall, Californians who recently got health insurance are more likely to report that their health needs are being met today than in the past. About three-fourths (77 percent) of those who report now having coverage after the third open enrollment period say their health needs are being met either “very” or “somewhat” well today, while only half of them (49 percent) said the same thing when they were uninsured in summer 2013, prior to the first open enrollment period. This is compared to the remaining uninsured, in which a similar share say their health needs are being met well today as did in 2013 (62 percent compared to 59 percent).
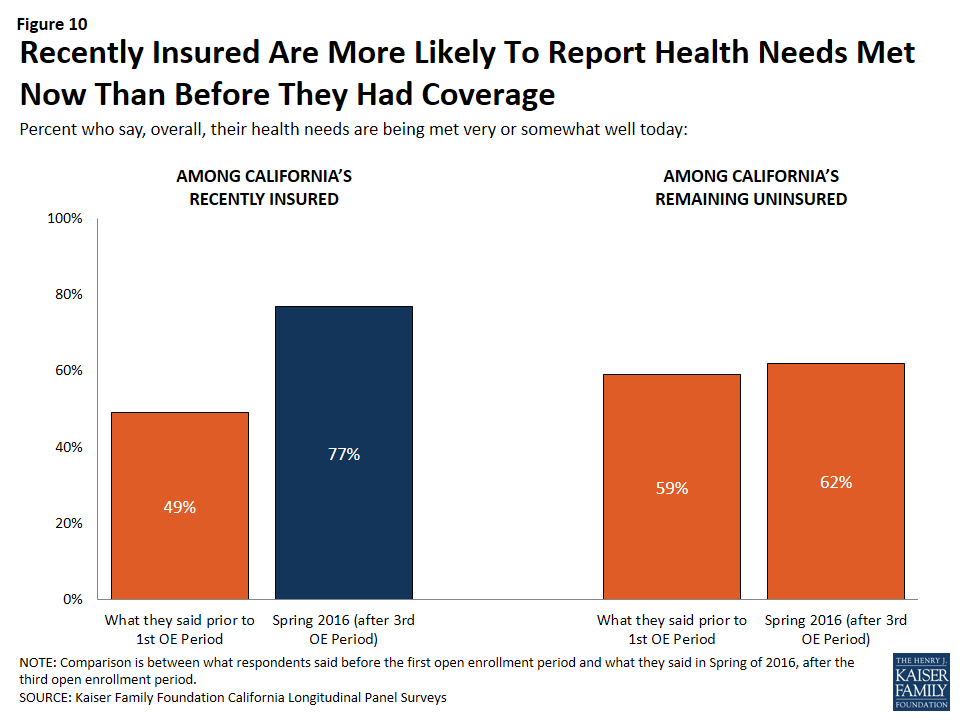
Californians who recently got health insurance are also less likely to report having difficulty affording a variety of household expenses, including health care, in 2016 than they did in 2013.
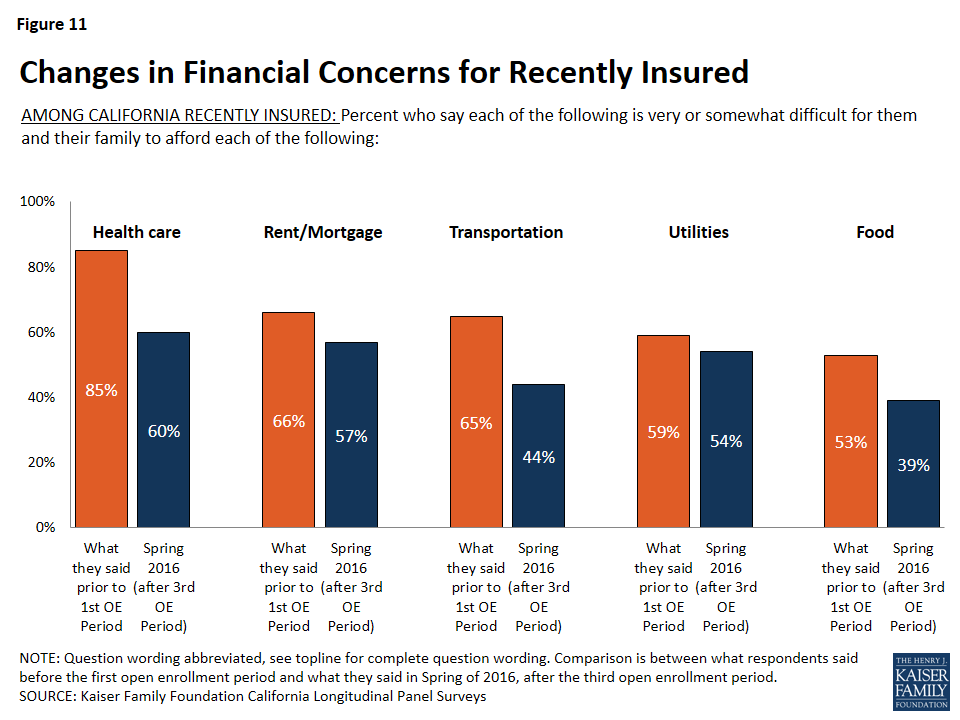
In 2016, 60 percent of California’s recently insured say it is difficult for them to afford health care. While this is still a majority, it is considerably less than the share of these individuals who reported the same in 2013 (85 percent). In comparison, of the remaining uninsured, the percent who say it is difficult for them to afford health care has remained stable (80 percent in 2016 v. 84 percent in 2013). For those who report having health insurance in spring 2016 after the third open enrollment period, affording health care falls among one of several household expenses people say they have difficulty affording. But, for those who remain uninsured, health care is by far the most frequently cited burdensome household expense, with eight in ten saying it is at least somewhat difficult to afford.
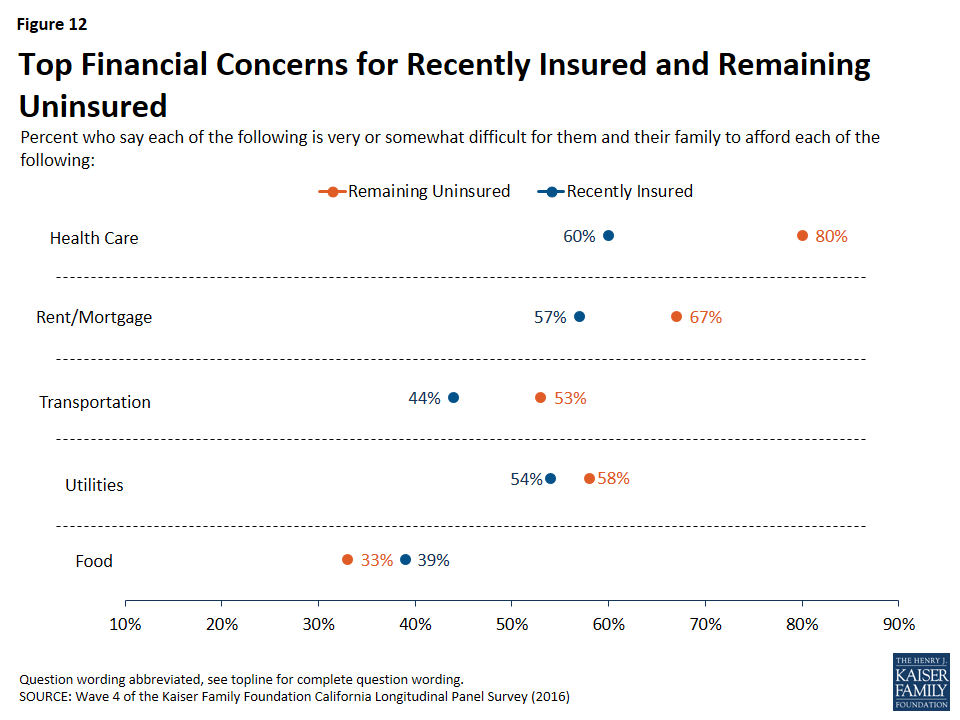
Financial Security
Even with some saying coverage is difficult to afford, overall, about half (46 percent) of previously uninsured Californians who have recently gained coverage say that having health insurance makes them feel more financially secure. About four in ten (41 percent) say it doesn’t make a difference, and a smaller share (11 percent) say it makes them feel less financially secure. In addition, most (58 percent) of those now with insurance say they feel well-protected by their health insurance, but 40 percent say they feel vulnerable to medical bills. The share of the insured who say they feel vulnerable to medical bills has increased slightly since 2015 (33 percent).
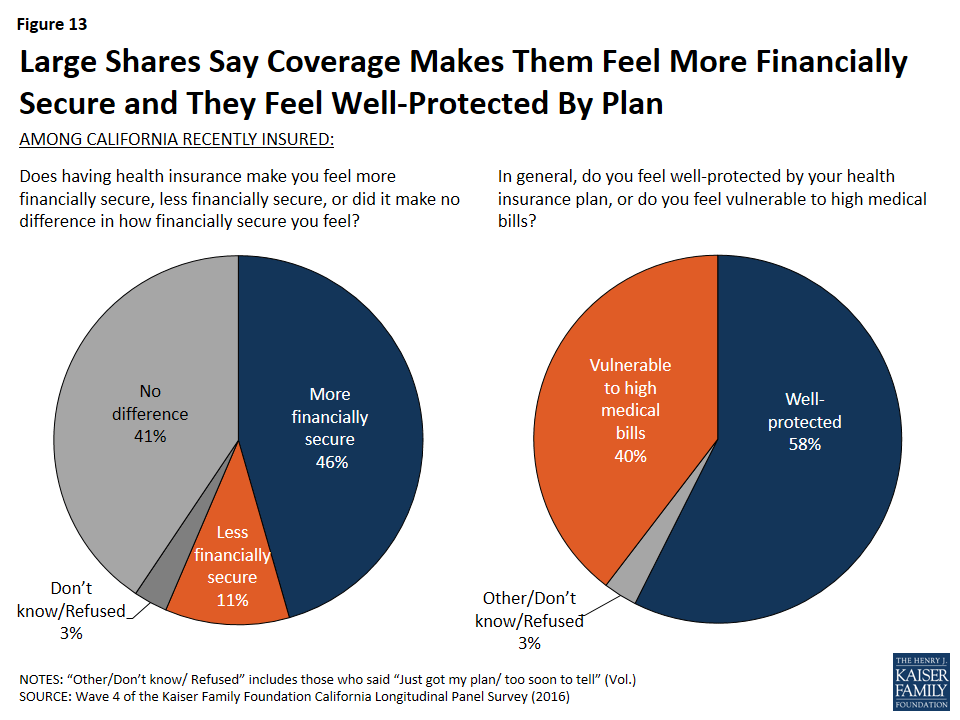
Among the recently insured, a larger share (52 percent) of individuals who have Medi-Cal report that getting insured made them feel more financially secure compared to those with Covered California (42 percent) and those with employer-sponsored insurance (40 percent).
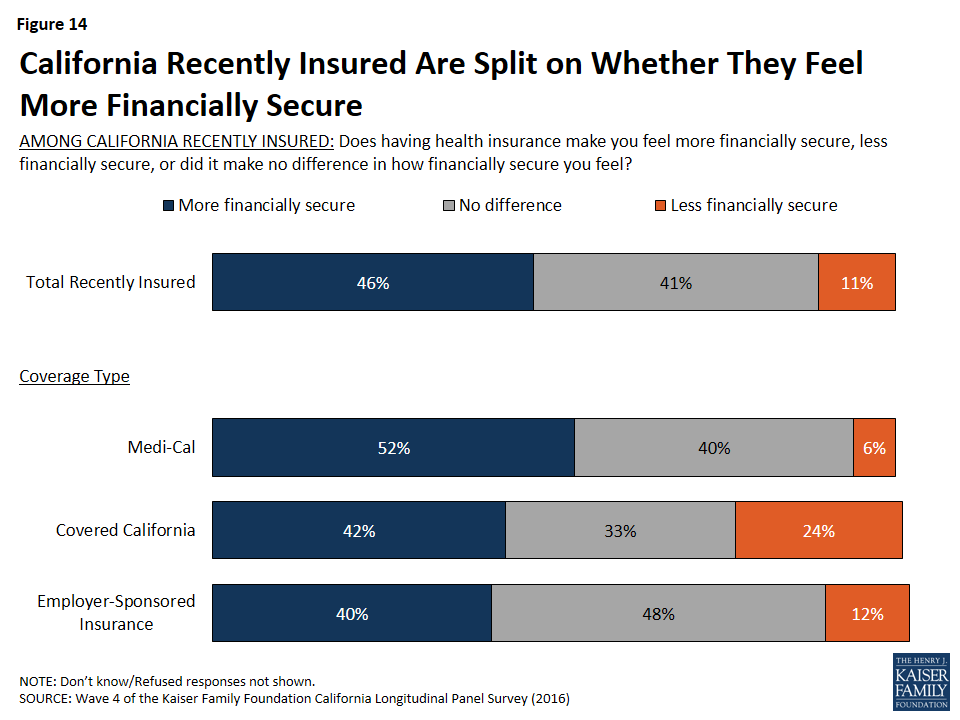
Similarly, a larger share of individuals with Medi-Cal feel well protected by their health insurance plan from high medical bills than those with Covered California and those with employer-sponsored insurance (62 percent compared to 50 percent and 53 percent, respectively). This is likely due to lower cost sharing for those with Medi-Cal.
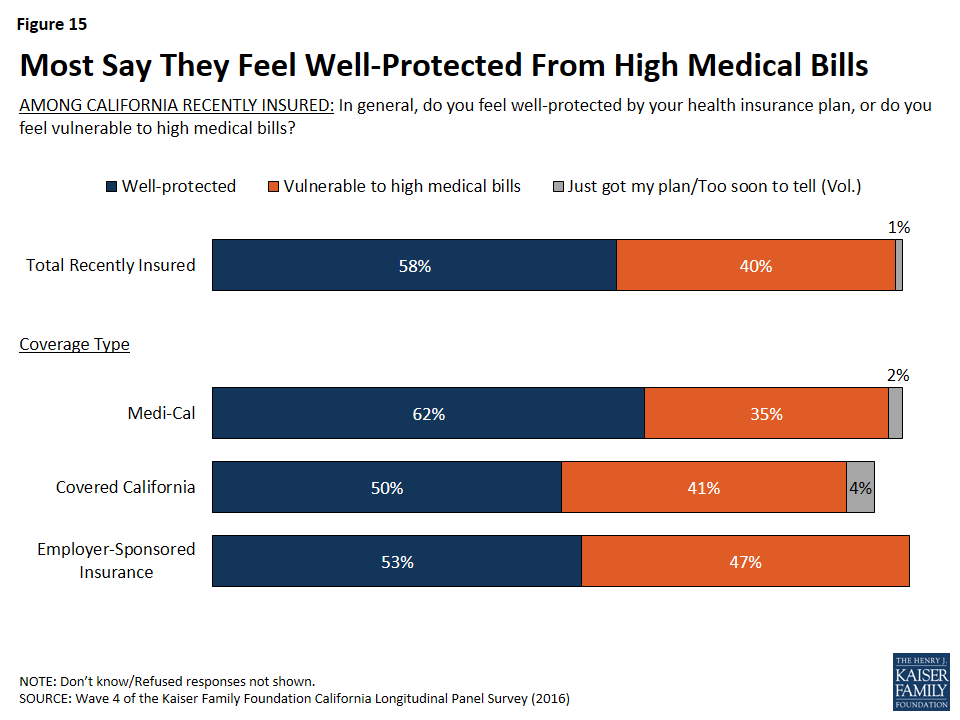
For Some, Health Care-Related Worries Persist
While many who have recently gained insurance report feeling more financially secure as a result of their coverage, one-fifth of the recently insured report forgoing needed medical care in the past year due to cost. But this share is smaller than the share of those remaining without insurance (32 percent) who report not getting medical care due to costs. The share of those with insurance who have foregone medical care due to costs is similar across insurance type, with about one in five of those with Medi-Cal (17 percent), and about one in four with those with Covered California (23 percent) and employer-sponsored insurance (24 percent) saying they have not gotten care due to costs.
| Table 2: Likelihood Of Forgoing Medical Care and Worries About Health Costs | |||||
| REMAINING UNINSURED | RECENTLY INSURED | ||||
| Total Recently Insured | Medi-Cal | Covered California | Employer-Sponsored Insurance | ||
| Was there a time over the past twelve months when you needed medical care, but did not get it because of the cost, or not? | |||||
| YES | 32% | 20% | 17% | 23% | 24% |
| NO | 68 | 79 | 82 | 77 | 76 |
| Percent who say they are very worried about not being able to do the following: | |||||
| Pay medical bills for health care services | 55 | 39 | 47 | 29 | 28 |
| Pay medical bills in the event of a serious illness or accident | 72 | 53 | 61 | 44 | 47 |
| Find a doctor or health professional who will treat you | 44 | 35 | 42 | 23 | 30 |
Having health insurance also leads to lower rates of reporting being worried about a series of health-care related concerns. Forty-four percent of California’s remaining uninsured saying they are “very worried” they will not be able to find a doctor or health professional to treat them, 55 percent are “very worried” they won’t be able to pay medical bills for health care services, and 72 percent are “very worried” they won’t be able to pay medical bills in the event of a serious illness or accident. This is compared to smaller shares of recently insured individuals who report being “very worried” about all of these health-related concerns. In addition, California’s recently insured now report a lower rate of being “very worried” about being able to pay medical bills for routine health care services than they did in 2013 (39 percent in 2016 compared to 52 percent in 2013), while the share of the remaining uninsured who are very worried has not changed and is 55 percent now compared to 57 percent in 2013.
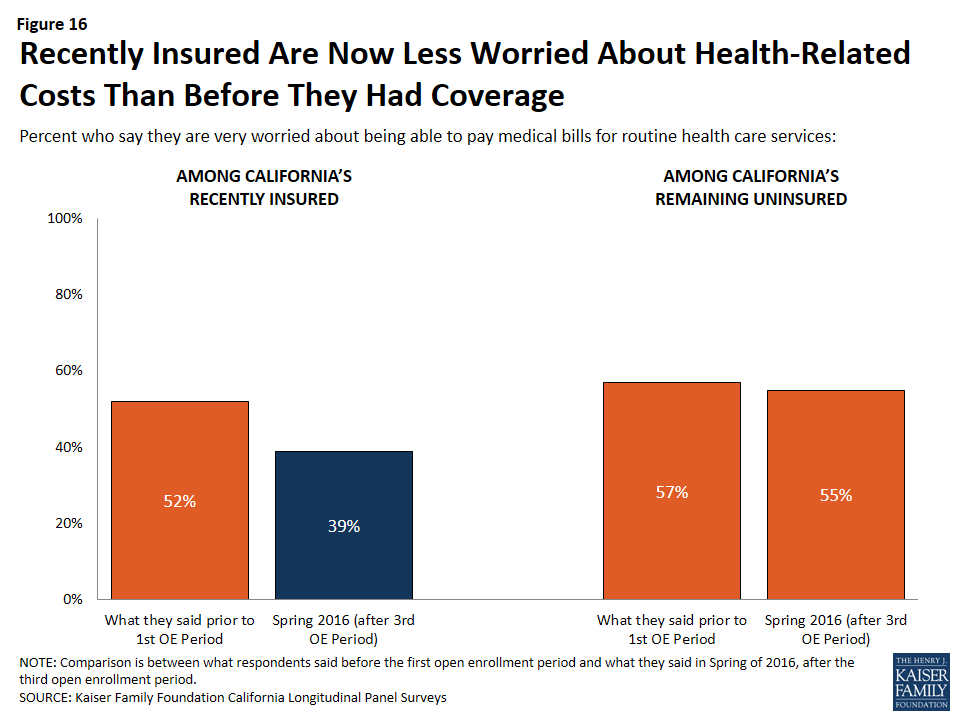
While half (53 percent) of California’s recently insured are still “very worried” that they would not be able to pay medical bills in the event of a serious illness or accident, this is a smaller share than the percent of these people who reported being “very worried” in 2013 (80 percent) and smaller than the share of the remaining uninsured who now report being “very worried” (72 percent). A larger share of individuals with Medi-Cal coverage (61 percent) say they are “very worried” about medical expenses for a serious illness compared to 47 percent of those with employer-sponsored coverage and 44 percent of individuals with Covered California health insurance coverage.
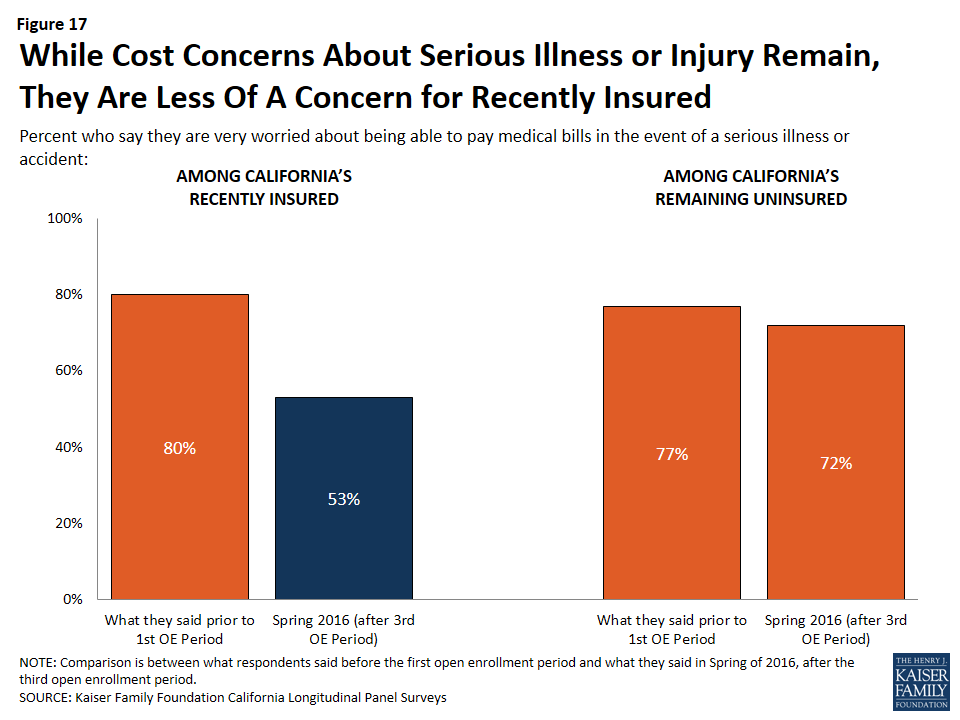
Accessing Health Care
Three-fourths of California’s recently insured have visited a doctor or health clinic in the past 12 months compared to 40 percent of California’s remaining uninsured.
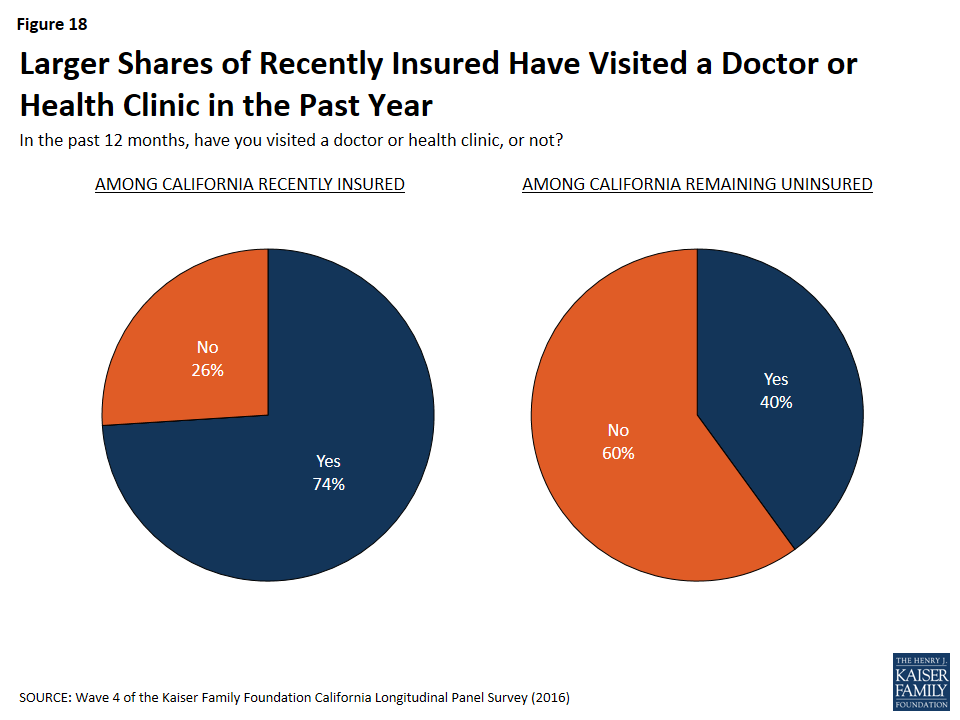
Among California’s recently insured, 57 percent say they have a usual source of care outside of the hospital emergency room, which is slightly higher than the share of these individuals who reported having a usual source of care outside of the hospital emergency room in 2013 (48 percent).
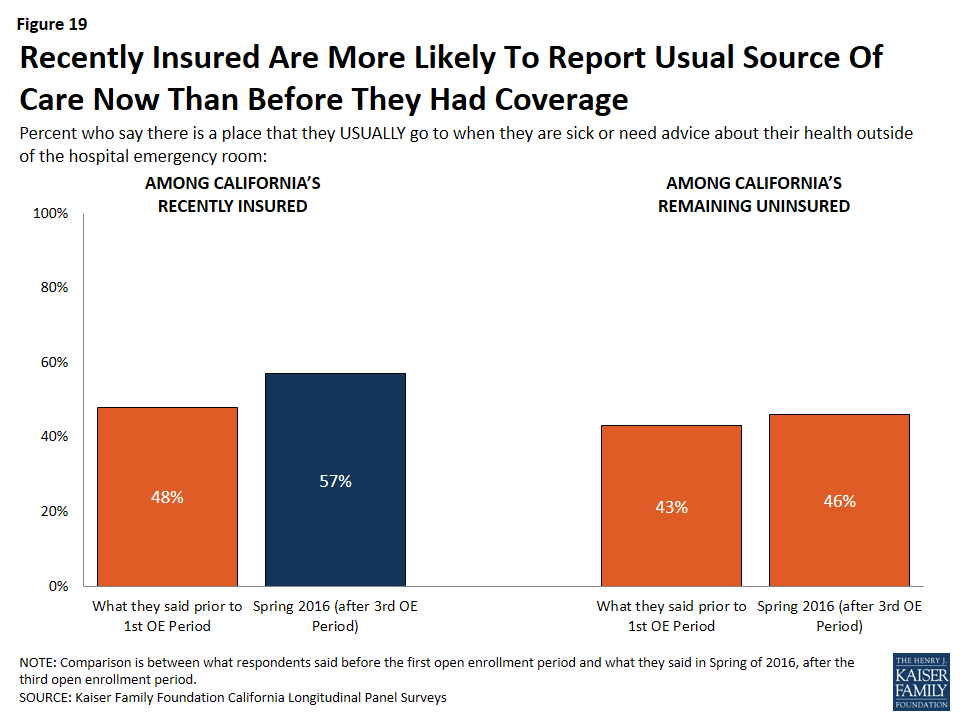
A larger share of California’s recently insured now report there is a place they usually go to, outside of the hospital emergency room, when they are sick or need advice about their health. In 2016, nearly six in ten (57 percent) of the recently insured report a usual source of care outside of the emergency room. In 2013, 48 percent of these individuals reported the same.
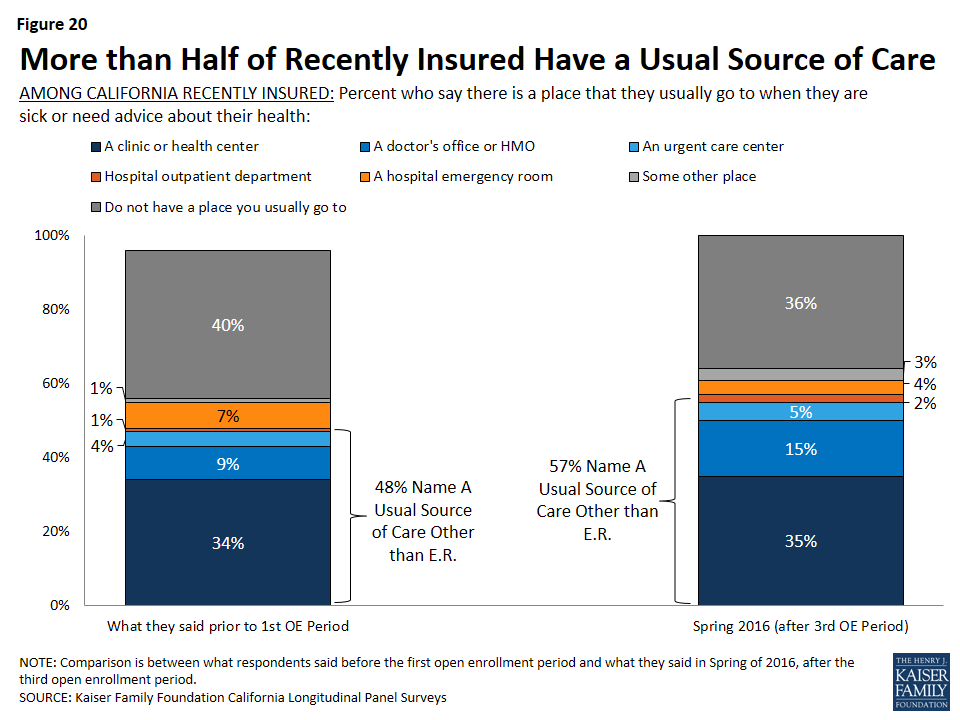
Problems Accessing Medical Care Among Recently Insured
Yet, for some of the recently insured, some problems accessing medical care remain. One-fourth of the recently insured say they have had to wait longer than a reasonable time to get an appointment for medical care and about one in ten (12 percent) say they have been told by a doctor’s office or clinic in the past 12 months that they would not be accepted as a new patient.
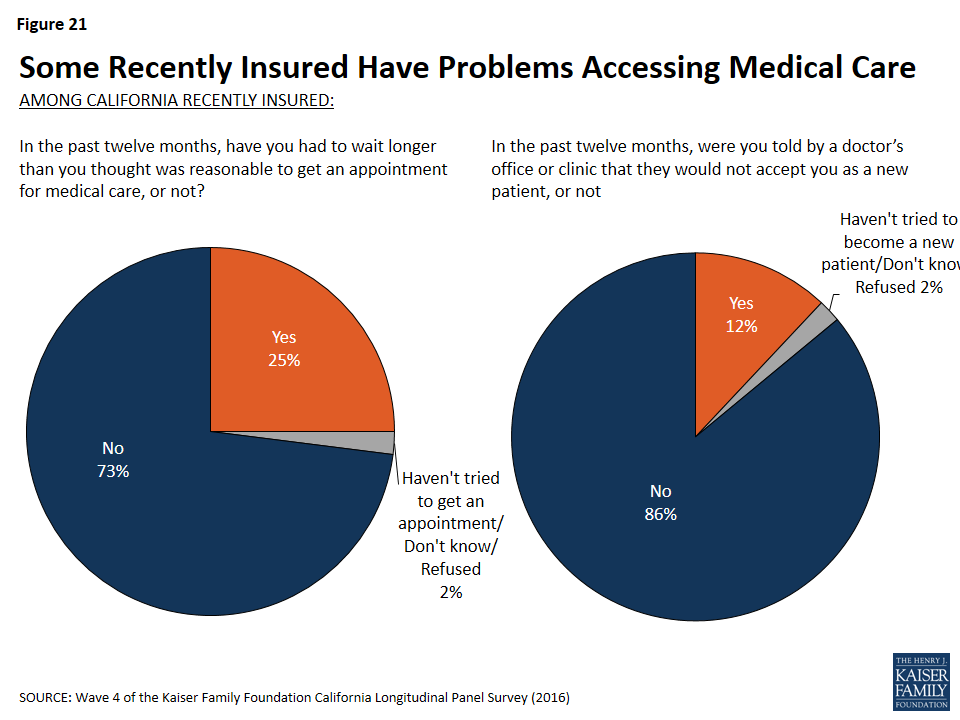
Evaluations of Health Insurance
Sixty-five percent of California’s recently insured say health insurance is worth the money that it costs. This is slightly larger than the share in 2013, in which 58 percent of these individuals reported that health insurance is worth the money that it costs. Among the remaining uninsured, 56 percent say health insurance is worth the money it costs.
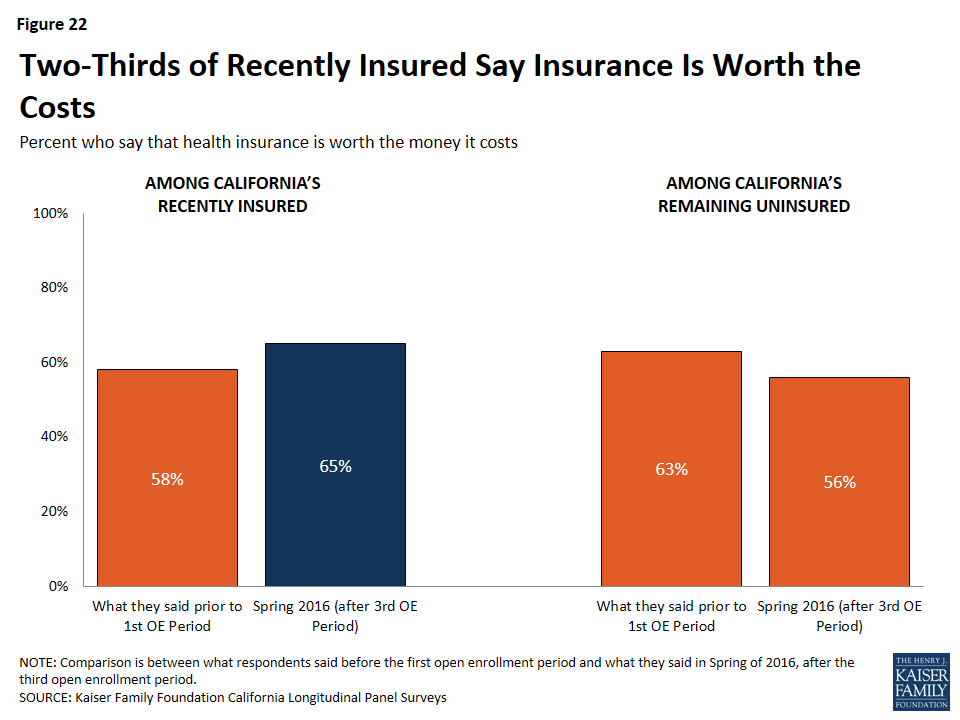
In addition, 85 percent of California’s recently insured say health insurance is something they need compared to 75 percent of those who remain uninsured. There are differences by gender within insurance status. Of the men who were recently insured, eight in ten say health insurance is something they need compared to 69 percent of men who remain uninsured. More than eight in ten women, regardless of insurance status, say health insurance is something they need.
| Table 3: Gender Differences in Perceptions of Whether Health Insurance is Needed | ||||||
| RECENTLY INSURED | REMAINING UNINSURED | |||||
| Total | Men | Women | Total | Men | Women | |
| Health insurance is something I need | 85% | 80% | 90% | 75% | 69% | 82% |
| I’m healthy enough that I don’t really need health insurance | 14 | 20 | 8 | 22 | 28 | 15 |
Satisfaction with Current Health Insurance Plan
Of the recently insured, the majority say their experiences with their current health insurance plan have been positive. About one-third (31 percent) say their experiences have been “very positive” with an additional 48 percent saying their experiences have been “somewhat positive.” Only 15 percent say their experiences have been negative: 10 percent say “somewhat negative” and 5 percent “very negative.” When looking at differences among coverage type, slightly larger shares of recently insured individuals with Medi-Cal say their experiences have been either very or somewhat positive (85 percent), compared to about three-fourths of those with employer-sponsored insurance and 70 percent of those with Covered California.
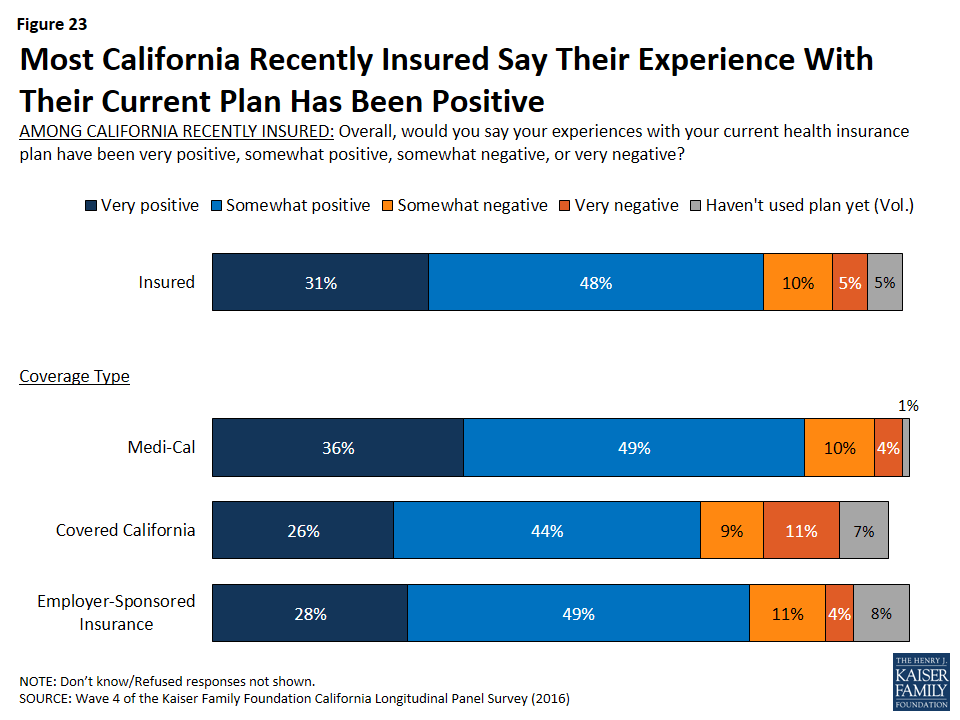
In addition, the majority of the recently insured report that they are either “very satisfied’ or “somewhat satisfied” with various aspects of their current plan including their choice of hospital (80 percent), their choice of primary doctors (76 percent), and their choice of specialists (68 percent).
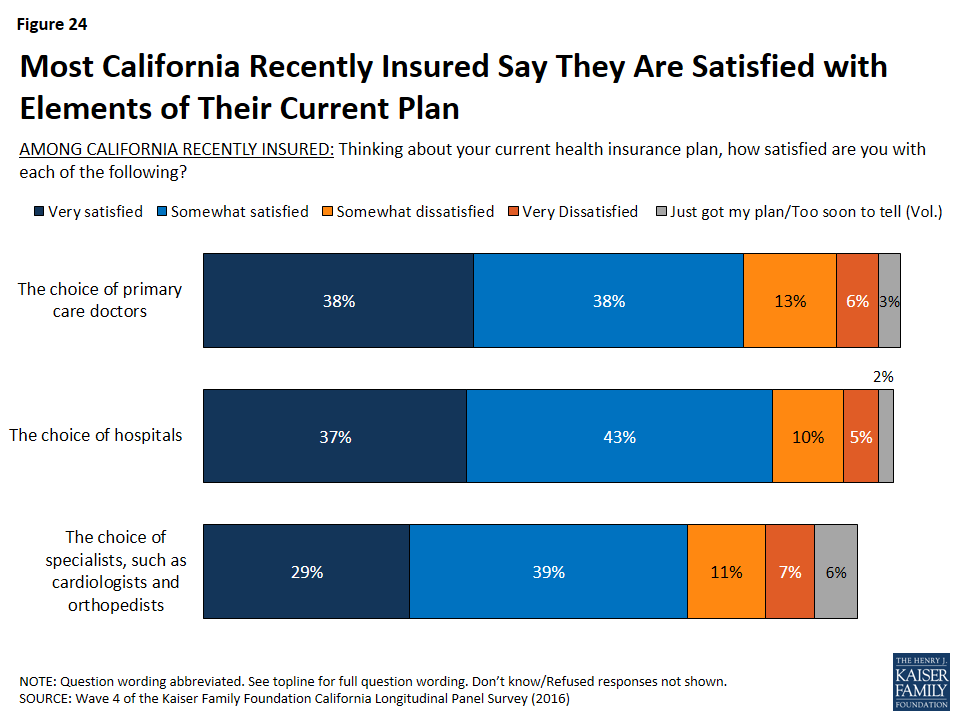
Section 3: The Remaining Uninsured
Who are the Remaining Uninsured?
Although many previously uninsured Californians gained coverage since the health care law went into effect, 27 percent report that they do not currently have health insurance. Many of these remaining uninsured had little interaction with the health insurance system in the years prior to the ACA implementation. Nearly four in ten of the remaining uninsured reported in the baseline survey that they had been without health insurance for two or more years (39 percent), and an additional 41 percent said they have never had insurance. Seventeen percent of the remaining uninsured are between the ages of 19 and 26 and therefore may be eligible to be covered through a parent or guardian’s health plan — if their parents have health insurance. However, the largest share are individuals between the ages of 30 and 39 (33 percent), followed by those between the ages of 40 and 49 (22 percent). Hispanics make up two-thirds of the remaining uninsured. Though half of them (33 percent of all remaining uninsured) are likely undocumented immigrants who are not eligible for Medi-Cal or assistance through Covered California. Many report a family income that makes them likely eligible for Medi-Cal (27 percent) or for financial assistance through Covered California (30 percent), while 41 percent are likely undocumented and therefore are ineligible.11
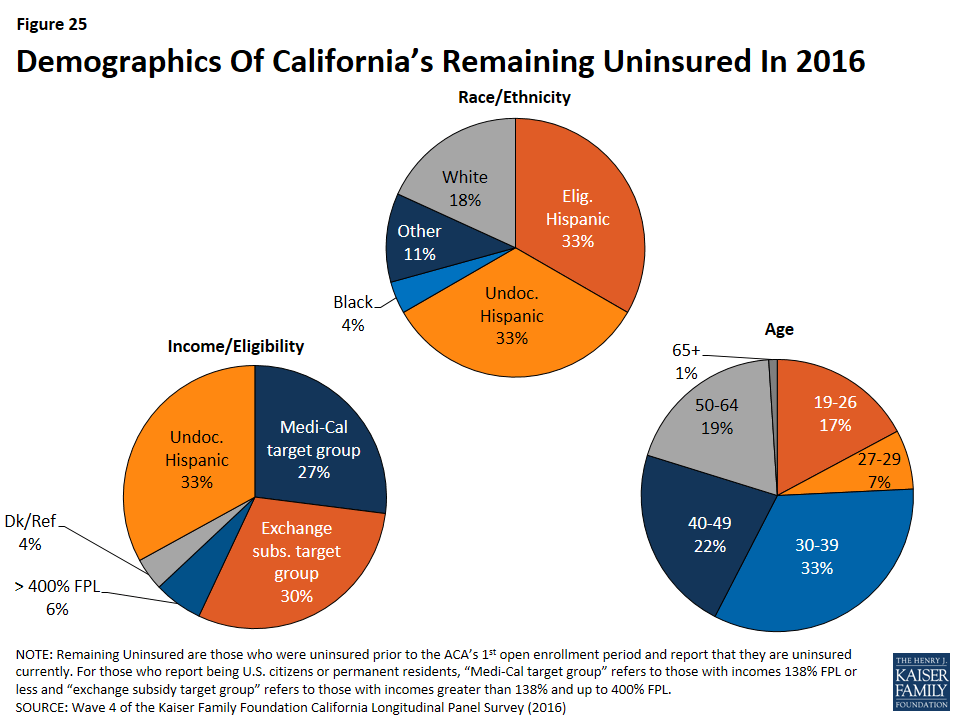
Why Don’t They Have Insurance?
When asked to say in their own words the main reason why they do not currently have health insurance, 47 percent of California’s remaining uninsured say it is because health insurance is too expensive or they can’t afford it. Affordability is by far the most common reason named for lacking health insurance, followed by eligibility reasons (19 percent), such as immigration concerns (10 percent) or the fact that they believe they are ineligible for Medi-Cal or government help (4 percent). One in ten say they haven’t tried to get insurance, they don’t need insurance, or they just haven’t gotten around to it, and about one in ten (9 percent) name application-process-related issues as the main reason. Small shares say other reasons such as unavailability (2 percent) — including that their employer doesn’t offer coverage (1 percent), unemployment (2 percent), and opposition to the health care law (2 percent).
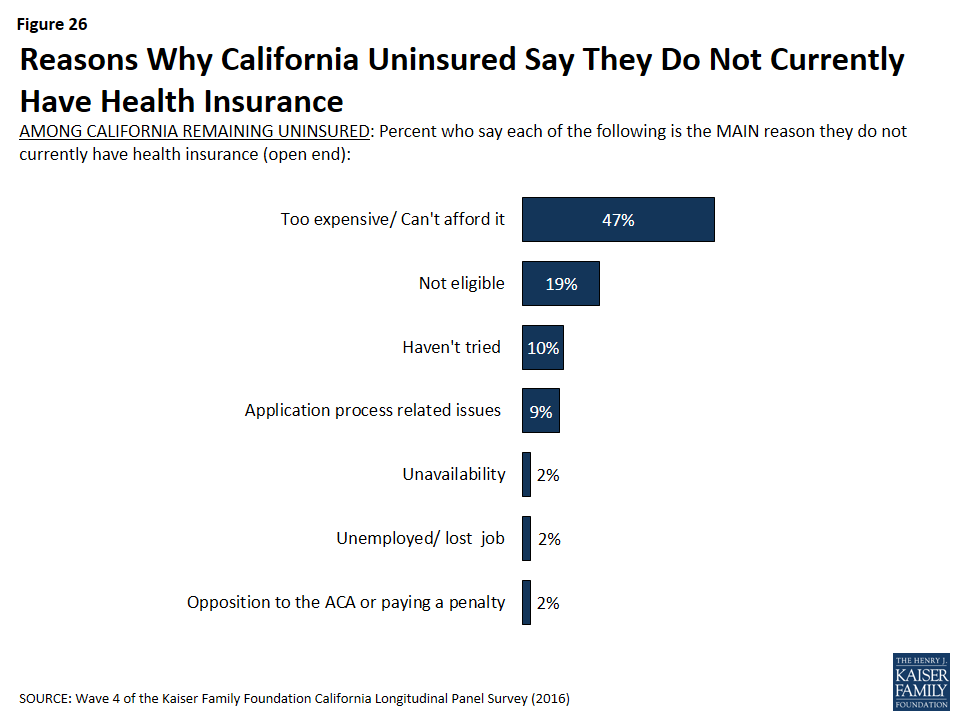
Did They Try To Get Insurance?
Slightly more than one-third (36 percent) of California’s remaining uninsured say they tried to get health insurance in the past 6 months. Those who tried but did not gain health insurance point to cost as a main reason they were unsuccessful. About a quarter (27 percent) of California’s remaining uninsured say they tried but didn’t get insurance because it was too expensive, including 19 percent who say they shopped for health insurance and 7 percent who say they didn’t bother shopping because they didn’t think they could afford it. Another 15 percent say they weren’t eligible for coverage, and less than one in ten (7 percent) say they were not able to complete the application process.
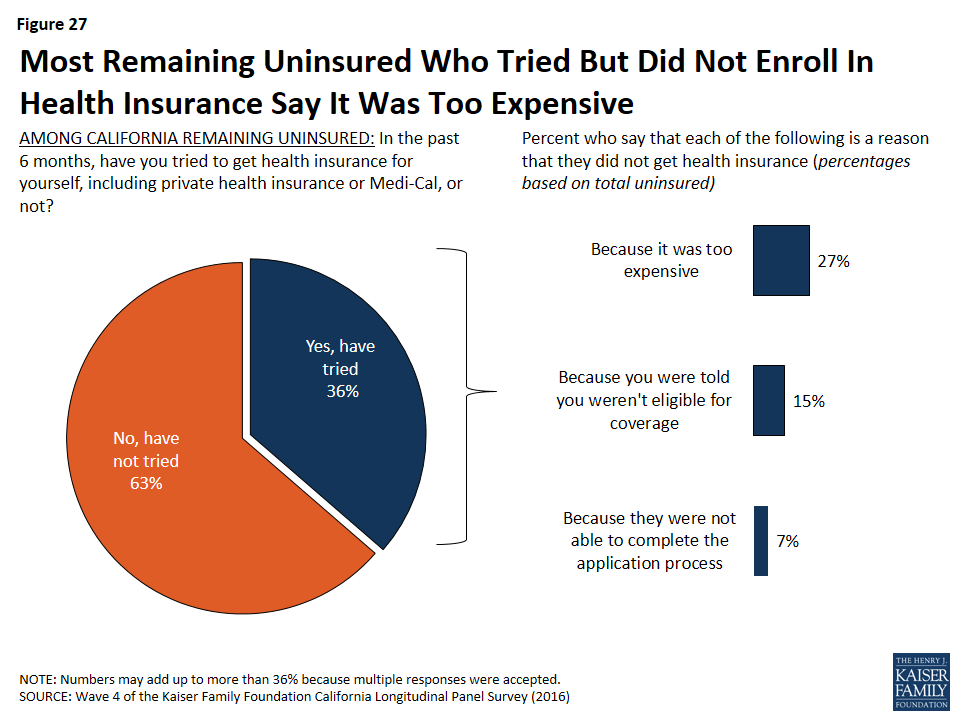
While a large share of California’s remaining uninsured say they did not get insurance because it was too expensive, there is little consensus on how much they would be willing to pay each month for health insurance or how much they think it will cost for them to buy health insurance. About half of the remaining uninsured say they are willing to pay up to $99. However, only 20 percent say they think it will cost them that much per month. About one-third (35 percent) of the remaining uninsured is unsure how much it would cost them each month to buy health insurance for themselves.
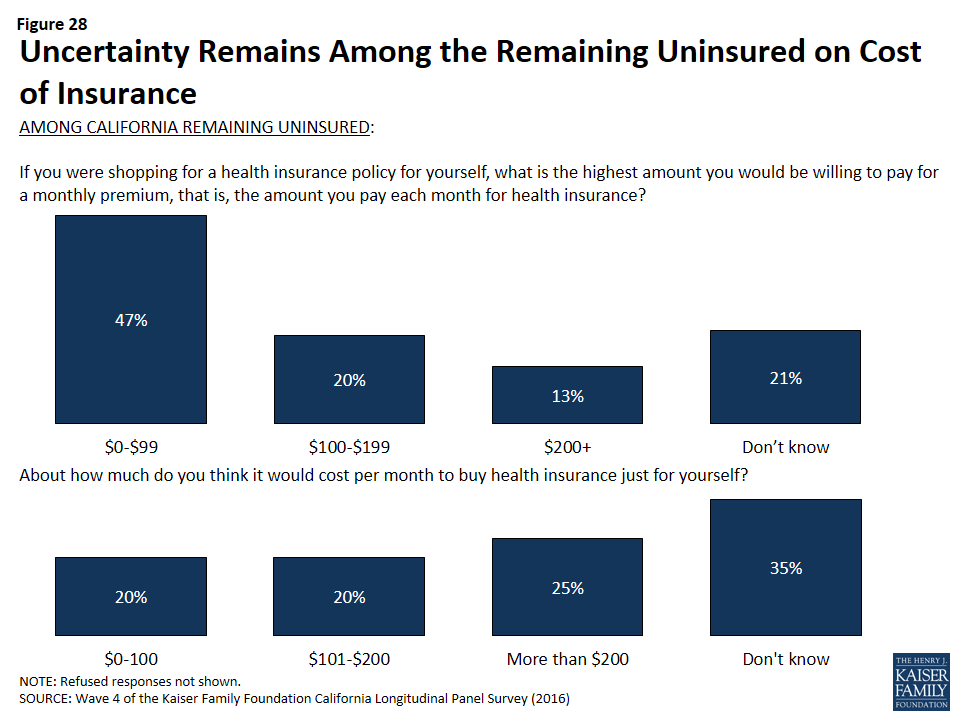
In addition, getting health insurance for free and buying health insurance for less than they thought are two of the many factors that could influence the remaining uninsured to get coverage. In fact, more than half of the remaining uninsured say they would be likely to get health insurance in the future if they had time to explore their options, they could get health insurance for free, they had more time to understand how to sign up, they could buy health insurance for less than they thought, the fine for not getting health insurance is higher this year, they or their spouse’s employer offered health insurance coverage, or if they had to pay a fine for not having health insurance.
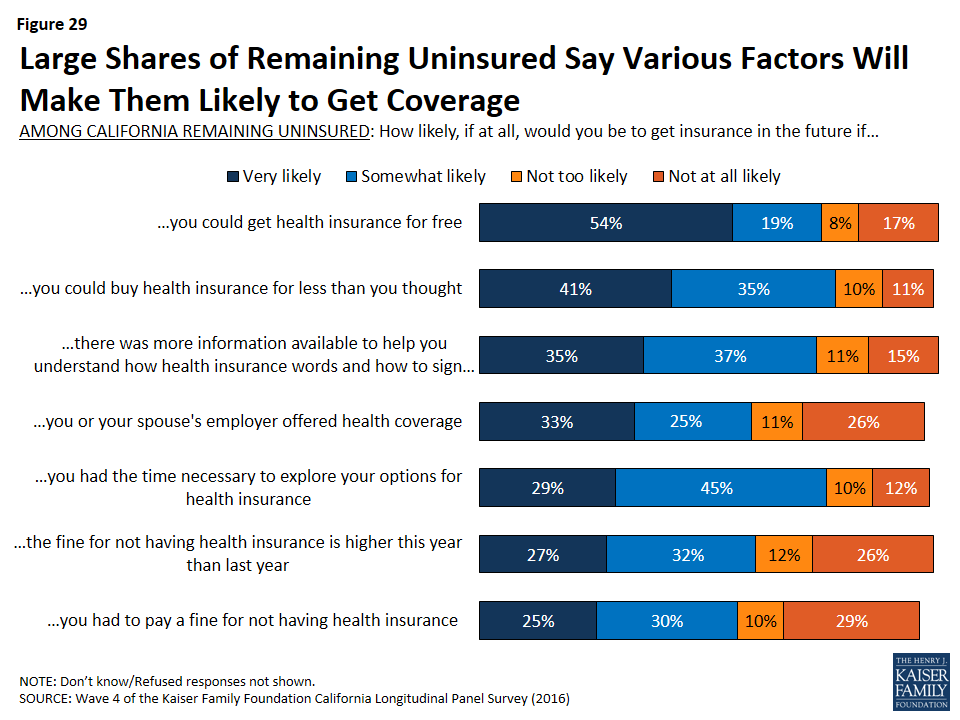
Knowledge About Health Care Law Fines and Provisions
A large share (83 percent) of the remaining uninsured in California are aware of the health care law’s requirement that most Americans have health insurance or pay a fine, and most (54 percent) think that the requirement applies to them but more than one-third (37 percent) say the requirement does not apply to them.
In fact, nearly equal shares of the uninsured think they will have to pay a fine for not having health insurance (45 percent) as think they will not have to pay a fine (40 percent), with the remaining 15 percent unsure of whether or not they will have to pay a fine. It is important to note that many may in fact be exempt from the requirement due to financial hardship or other exceptions under the law, including exceptions for undocumented immigrants.
Smaller shares of the remaining uninsured are aware of provisions of the health care law, beyond the requirement to have coverage, intended to expand coverage to the uninsured and those with lower incomes. Just over half know that the law allowed for the expansion of the Medi-Cal program to cover more low-income Californians (54 percent), and half (49 percent) know that the law provides financial help to low- and moderate-income people to help them purchase health insurance coverage.
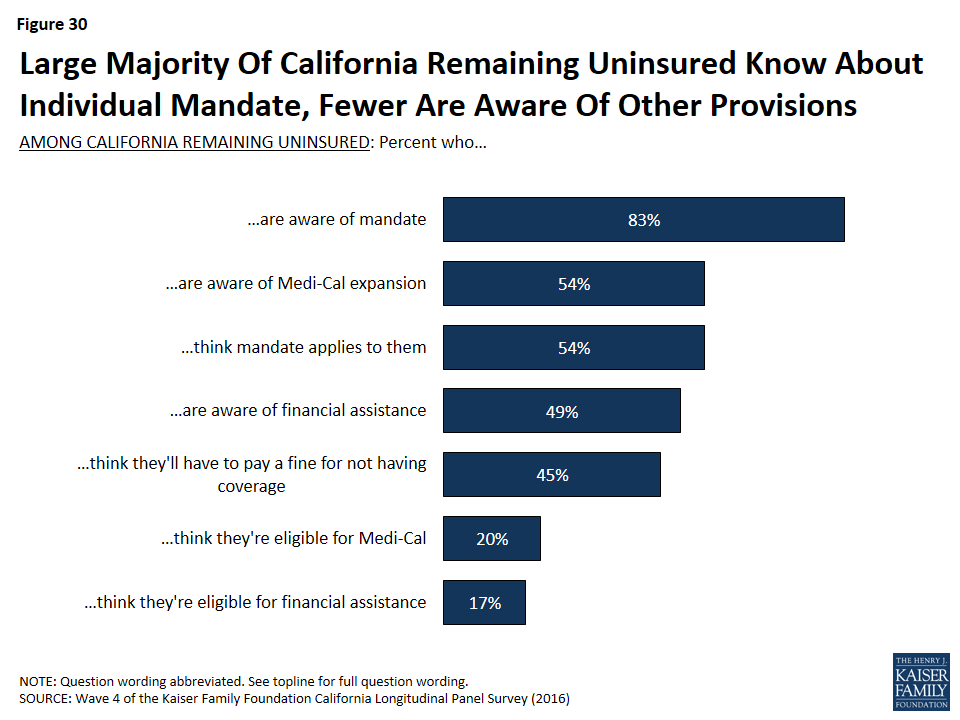
California’s Remaining Uninsured Immigrants
The Hispanic population is particularly important in California because Latinos make up the largest racial or ethnic group in the state, accounting for 39 percent of the population,12 and about seven in ten of the remaining uninsured are Hispanic (67 percent). Overall, one-third of California’s Hispanics remain uninsured. A significant portion of these uninsured Hispanics may not have insurance due to the fact that they are not eligible for coverage because of their immigration status. Of the total Hispanic population, about one-third (32 percent) are likely not eligible for health insurance coverage. Of all eligible Hispanics in this survey, three-fourths report having health insurance leaving one-fourth (24 percent) eligible for, but without health insurance coverage. This is compared to about one in five of white non-Hispanics who do not have health insurance coverage.
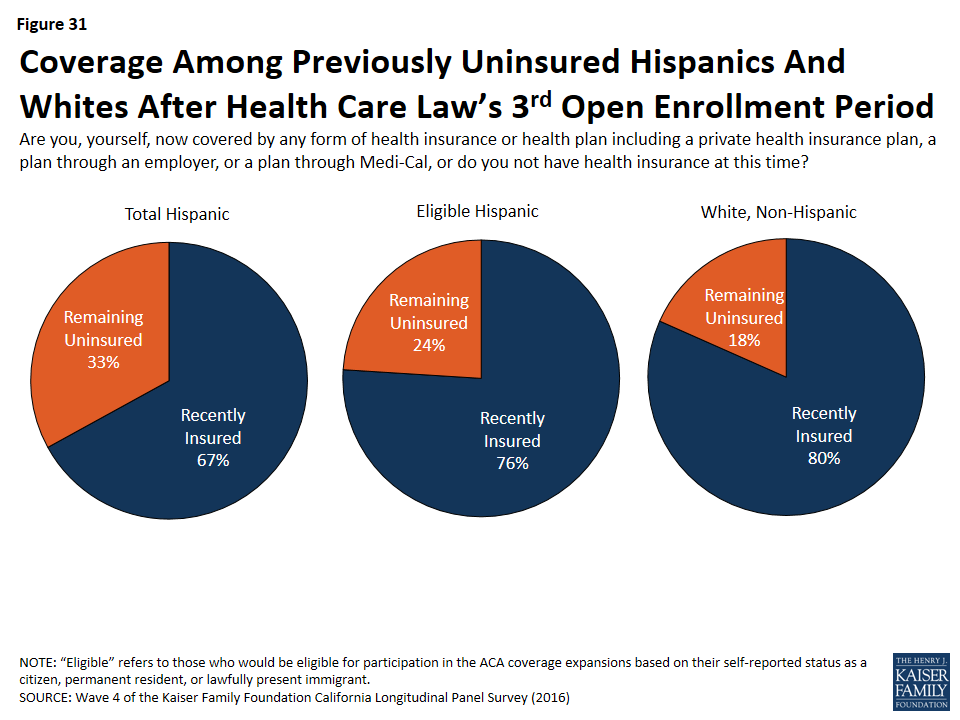
Half (55 percent) of uninsured Hispanics and two-thirds of uninsured Hispanics who completed the survey in Spanish say they are very or somewhat worried that if they sign up for health insurance, it will draw attention to their immigration status or that of a family member.
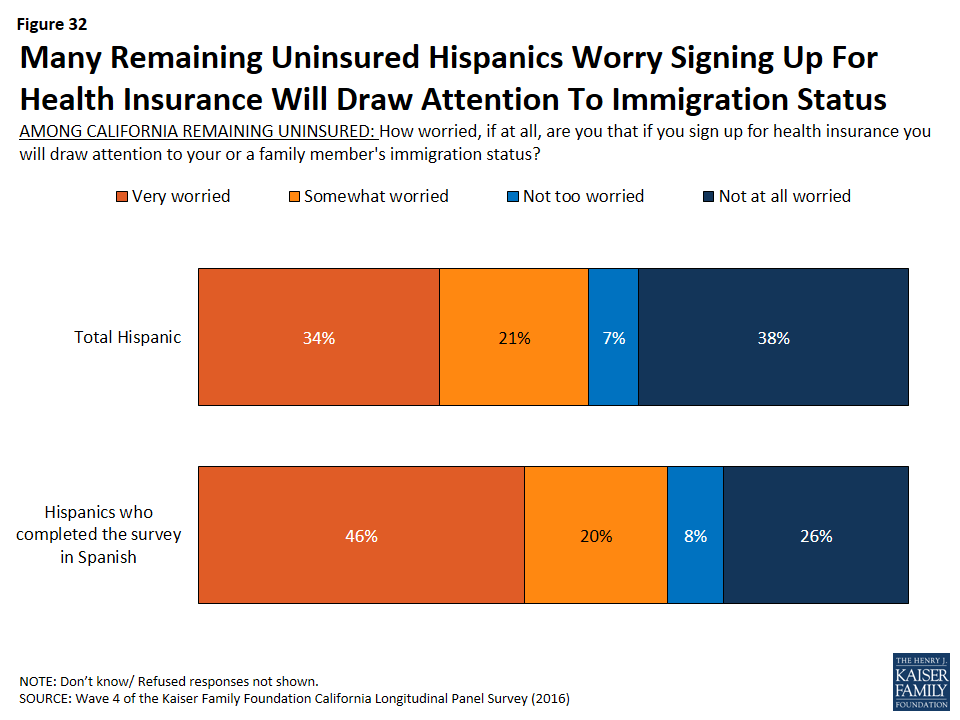
In fact, concerns about immigration status exist for all California’s remaining uninsured who were born in another country — both Hispanics and non-Hispanics. One-fourth (27 percent) of California’s remaining uninsured worry that they or a family member could be deported if they sign up for health insurance. In addition, 50 percent of all uninsured who were born in another country worry that signing up for health insurance could hurt their ability to become a U.S. citizen.
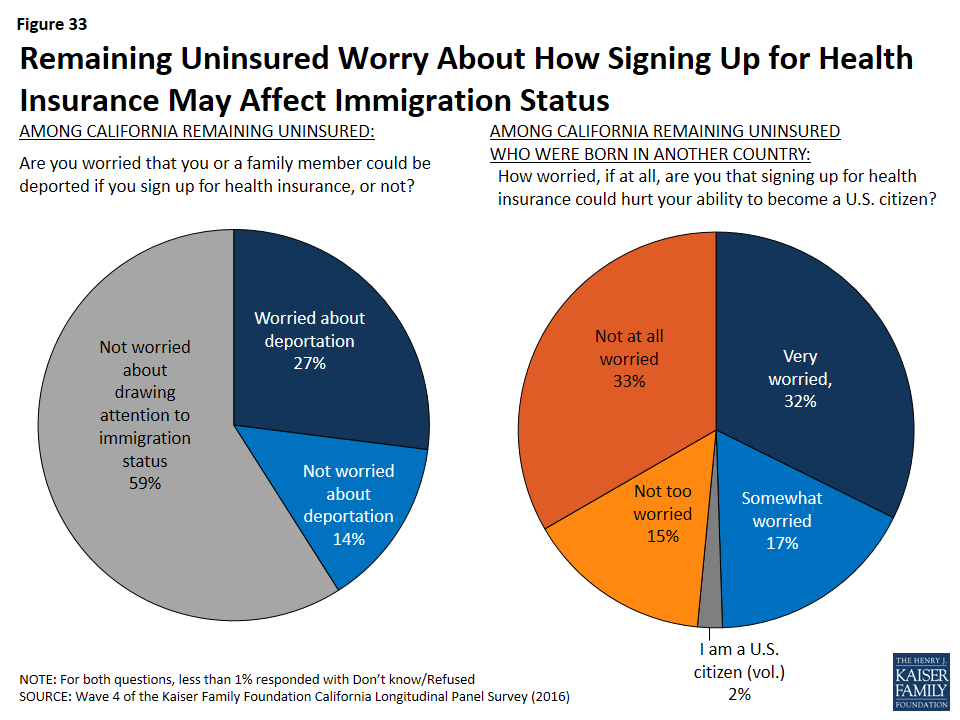
Spanish Language Assistance
Navigating health insurance options and health care jargon can be confusing, and adding language differences to the equation has the potential to be an even bigger barrier to enrollment. However, Californians currently without health insurance who prefer to communicate in Spanish give largely positive feedback when asked how much information is available in Spanish and whether there are people in their community trained to help them sign up for insurance in Spanish. Most (65 percent) remaining uninsured Spanish speakers say that, in their experience, there is at least some information about signing up for insurance available in Spanish – about four in ten (39 percent) say there is a lot of information available and another 26 percent say there is some information available. There is still room for improvement though, as a third of Spanish-speaking remaining uninsured Californians report that there is only a little information available in Spanish (24 percent) or say that there is none available at all (7 percent). Six in ten Spanish-speaking uninsured report there are people in their community trained to help them sign up (compared to 72 percent in 2015), while one-third (35 percent) say that there are not people in their community trained to help and 6 percent say they do not know.
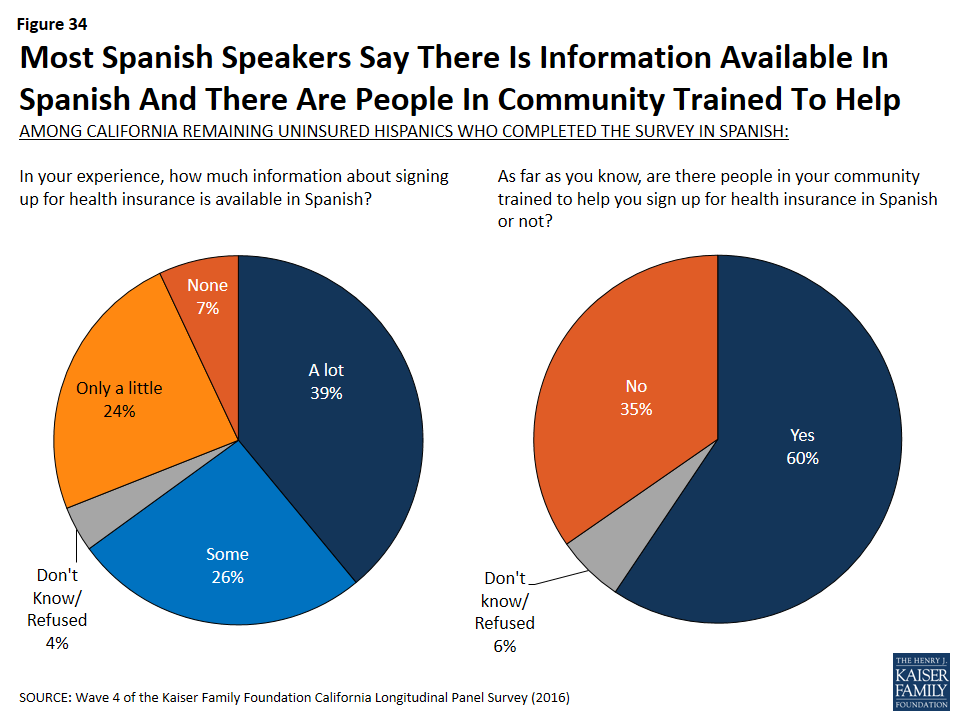
Conclusion: Conclusion
The Kaiser Family Foundation California Longitudinal Panel Survey provides unique insights into the experiences and views of a representative, randomly selected sample of Californians who were uninsured prior to the major coverage expansions under the Affordable Care Act (ACA). The initial baseline survey was conducted with a representative sample of 2,001 nonelderly uninsured Californian adults in summer 2013, prior to the ACA’s initial open enrollment period. Because the same group of previously uninsured people has been followed over time, the survey is able to explore the dynamics of health insurance and track how many people have moved in to or back out of coverage since the baseline survey in 2013.
After three rounds of open enrollment under the Affordable Care Act, nearly three-fourths (72 percent) of Californians who were uninsured prior to the first open enrollment period now report that they have health insurance. This share is similar to the 68 percent who said they were insured after the second open enrollment period in the spring of 2015, and is an increase from 58 percent after the first open enrollment period in the spring of 2014. This indicates that the percent of Californians with health insurance may have reached a relatively steady rate, with less fluctuation in the market as individuals gain and keep coverage.
Most of California’s previously uninsured who reported having coverage after the first open enrollment period continued to report having coverage, but some have since become uninsured, while some others who reported being uninsured after the first open enrollment period or the second enrollment period now report having coverage. These dynamics indicate the potential challenges of getting and keeping coverage for the previously uninsured as well as potential opportunities for new enrollment gains among those who have potentially missed chances to enroll in the past. Future gains in coverage may be moderate, however, with the remaining shares of California’s previously uninsured consisting largely of harder-to-reach groups: those who are undocumented immigrants and therefore ineligible for coverage through the ACA and those who reported as of the baseline survey that they had been without coverage for two or more years or had never had health insurance. There is some lack of knowledge of the assistance that is currently available, which indicates that there is potential for outreach to make a difference.
Among the recently insured, there have been considerable gains in access and affordability compared to what they said in the baseline survey, but concerns about health care costs remain. The final fourth wave of the Kaiser Family Foundation California Longitudinal Panel Survey illustrates that while more individuals are gaining access to health insurance coverage, challenges still exist for both the remaining uninsured and those who now have health insurance coverage.
Conclusion: About The Terms Used In This Report
This report primarily uses the following definitions for key groups examined in the survey:
The overall group of Californians who were uninsured prior to the ACA’s first open enrollment period, most often referred to as “California’s previously uninsured.”
- The subgroup of previously uninsured Californians who currently report that they are uninsured, referred to as “California’s remaining uninsured.” This group includes some who reported having coverage in 2014 or 2015, some who reported not having coverage in 2014 or 2015, and some whose 2014 coverage status or 2015 coverage status is unknown because they were unable to be contacted during those years.
- The subgroup of previously uninsured Californians who now report that they have health insurance, referred to as “California’s recently insured.” Two subgroups within California’s recently insured are:
- Those who reported that they were uninsured in the summer of 2013 and either said in spring 2014 or spring 2015 that they did not have coverage or were unable to be contacted, but now report having health insurance, referred to as “California’s newly insured,” and
- Those who reported that they were uninsured in the summer of 2013, reported gaining insurance sometime in the past two years and say they still have coverage in spring 2016, referred to as “California’s still insured.”
And, as noted in the Survey Methodology Section, only those uninsured for at least two months were included in the baseline survey. Other terms used occasionally throughout the report are defined below.
- Eligible Previously Uninsured Californians: Because the coverage expansions under the ACA do not extend to undocumented immigrants, some of the analyses focuses on those who reported being U.S. citizens or permanent residents in the baseline survey, described in shorthand as those who are ‘eligible’ for the ACA’s coverage expansions.
- Undocumented Previously Uninsured Californians: For the purposes of this report, undocumented immigrants are defined as those who reported in the baseline survey that a) they were not born in the United States or Puerto Rico, b) they came to this country without a green card, and c) they have not received a green card or become a permanent resident since arriving. There are several ways that this definition, while workable for the purposes of a broad analysis of this sort, falls short of the complexity of real life. First, it relies on self-reporting, and since respondents have an incentive not to reveal unlawful immigration status, it is undoubtedly a somewhat imperfect measure. Second, those that did not answer all three in the series of immigration status items in the baseline survey were not able to be categorized. Third, by necessity of time and efficiency, the survey did not allow for a full exploration of the many nuances inherent in the U.S. immigration system. For example, this category may actually include a small number of individuals in California as refugees, asylees or other humanitarian immigrants who might better be placed among the ‘eligible uninsured’. The survey, unfortunately, does not allow this level of detailed sorting. Since estimated immigration status is based on individuals’ responses to the baseline survey, it is possible that some small share of those thought to be undocumented immigrants have now become permanent residents or received a green card.
- Income categories: Because eligibility for two of the law’s main components – the Medi-Cal expansion and the tax credits being made available to purchase insurance on the new exchanges – is based on an individual’s family income relative to the federal poverty level (FPL), in some cases we report survey results by FPL categories. Eligible previously uninsured Californians with incomes 138% FPL or less (roughly $33,000 a year for a family of 4 in 2015) are eligible for Medi-Cal coverage, while those with incomes greater than 138% and up to 400% FPL (roughly $33,000-$97,000 for a family of 4 in 2015), are eligible for subsidies to purchase insurance through Covered California Marketplace. Those with incomes above 400% FPL are allowed to buy insurance through Covered California but are not eligible for subsidy assistance. For convenience, we sometimes refer to the eligible group with incomes 138% FPL or less as the “Medi-Cal target group”, and those greater than 138% and up to 400% FPL as the “exchange subsidy target group”. These obviously are approximations that do not allow for every real world exception to be taken into account. For example, lawfully present immigrants may remain subject to a five year wait before they may enroll in Medi-Cal, but for the purposes of this analysis they are included in the Medi-Cal target group if they meet the income criteria. Similarly, some of those in the exchange subsidy target group may not be eligible for marketplace subsidies if they have access to affordable employer coverage, a situation difficult to ascertain in a phone survey.
Methodology
Survey Methodology
This is the fourth in a series of surveys by the Kaiser Family Foundation (KFF) tracking the views and experiences of a group of Californians who were uninsured in the summer of 2013, prior to implementation of the ACA’s insurance market reforms and coverage expansions through Covered California and Medi-Cal. The first survey (Wave 1) was conducted from July 11-August 29, 2013, with a randomly selected group of individuals who were uninsured at the time of the interview, and was paid for entirely by KFF. The second survey (Wave 2) was conducted from April 1-June 15, 2014. The third survey (Wave 3) was conducted from February 18-May 13, 2015, and the current survey (wave 4) was conducted from February 10-June 20, 2016, with the same longitudinal panel of respondents, whether they obtained coverage or remained uninsured. All four surveys were designed and analyzed by researchers at KFF. Social Science Research Solutions collaborated with KFF researchers on sample design, weighting, and supervised fieldwork. Fieldwork costs associated with Waves 2, 3, and 4 of the survey were paid for by The California Endowment.
The Wave 1 survey was conducted among a representative random sample of 2,001 adults ages 19-64 living in California who reported having been without health insurance for at least two months at the time of the interview13 (NOTE: persons without a telephone could not be included in the random selection process). Computer-assisted telephone interviews conducted by landline (990) and cell phone (1,011, including 660 who had no landline telephone) were carried out in English and Spanish by SSRS. To increase efficiency in reaching this low-incidence, hard-to-reach group, both the landline and cell phone sampling frames oversampled areas with a lower-income population (since being uninsured is negatively correlated with income). The landline sample frame also oversampled households whose phone numbers were matched with directory listings indicating the presence of at least one person age 19-64 and a household income of less than $25,000. Additionally, 230 interviews (130 landline, 100 cell phone) were conducted with respondents who previously completed recent national SSRS omnibus surveys of the general public and indicated they were ages 19-64 and uninsured. These previous surveys were conducted with nationally representative, random-digit-dial landline and cell phone samples. Waves 2, 3, and 4 also consisted of computer-assisted telephone interviews conducted in English and Spanish by landline and cell phone, including those who had no landline phone.
| Table 4: Comparing Respondent Contact Mode Across Waves | ||||
| Total | Landline | Cell phone (no landline) | Web | |
| Wave 1 (July 11-August 29, 2013) | 2,001 | 990 | 1,011 (660) | Not applicable |
| Wave 2 (April 1-June 15, 2014) | 1,219 | 623 | 545 (327) | 51 |
| Wave 3 (February 18-May 13, 2015) | 1,105 | 555 | 463 (317) | 87 |
| Wave 4 (February 10-June 20, 2016) | 1001 | 484 | 404 (240) | 113 |
In order to re-connect with respondents who may be more willing to complete the survey online, an abbreviated web version was introduced for Waves 2, 3, and 4 after attempts had been made to reach respondents by phone. The online questionnaire was offered in English and Spanish and was limited to key questions about insurance status, type of coverage, and reasons for obtaining coverage or remaining uninsured. A total of 51 respondents in Wave 2, 87 respondents in Wave 3, and 113 in Wave 4 completed the online version of the survey.
Screening for Waves 2, 3, and 4 involved verifying that the respondent had participated in Wave 1. Multiple attempts were made to reach every respondent from Wave 1 and encourage participation in later waves. Efforts included multiple dialing at various times of day and throughout the week, mailings and emails to those who provided such contact information, repeated dialing of non-working numbers, and attempts to find alternative phone numbers for non-working numbers.
A multi-stage weighting design was applied to ensure accurate representation of California’s nonelderly adult uninsured population prior to the ACA’s coverage expansions. The weighting process for Waves 2, 3, and 4 involved corrections for sample design, as well as sample weighting to match the weighted Wave 2 sample, weighted Wave 3 sample, and weighted Wave 4 sample to Wave 1 responses along demographic characteristics. As it did for Wave 1, the base weight for Waves 2, 3, and 4 accounted for the oversamples used in the sample design, as well as the likelihood of non-response for the sample from earlier omnibus surveys, number of eligible household members for the landline sample, and a correction to account for the fact that respondents with both a landline and cell phone have a higher probability of selection. Demographic weighting parameters for Waves 2, 3, and 4 were based on Wave 1 weighted demographics, which were adjusted for age, education, race/ethnicity, nativity (for Hispanics only), Hispanics by gender, presence of own child in household, marital status, California region, poverty level, and phone usage. For more information on weighting and data sources, see the Wave 1 methodology. All differences referred to in the report are statistically significant. Statistical tests of significance account for the effect of weighting, and, for trend analysis, testing takes into account the survey’s panel design.
A unique consideration for panel surveys such as the Kaiser Family Foundation California Longitudinal Panel Survey, is whether those who participate in subsequent waves are different in terms of their attitudes or demographics than those who refuse to participate again or were unable to be re-contacted. Of the total 2,001 respondents who completed Wave 1, 1,219 participated in Wave 2, 1,105 completed Wave 3, and 1001 completed Wave 4. These completion rates are within an expected range given that the uninsured are already an often a difficult to reach population since many are lower income, younger, undocumented immigrants, and members of racial/ethnic minority groups, and may change phone numbers or move more often than the public at large. After data collection was complete, data from Wave 1 and Wave 4 were compared to evaluate the impact of some respondents not completing Wave 4, referred to as attrition. While there are some differences in the unweighted demographics of those who completed Wave 4 and the full Wave 1 sample, these observable differences are corrected for by weighting. As shown in the table below the total weighted distributions are similar for Wave 1 and Wave 4 for age, gender, race/ethnicity, party identification, education and income. See the Wave 4 Attrition Appendix for more information on attrition.
| Table 5: Comparing Respondent Demographics | ||||||||
| Unweighted | Weighted | |||||||
| Wave 1 (n=2001) | Completed Wave 4 (n=1001) | Completed all 4 Waves (n=764) | Percentage PointDifference(W1 – W4 Total) | Wave 1 | Completed Wave 4 | Completed all 4 Waves | Percentage PointDifference(W1 – W4 Total) | |
| Gender | ||||||||
| Male | 48% | 43% | 41% | 5 | 54% | 53% | 50% | 1 |
| Female | 52% | 57% | 59% | -5 | 46% | 47% | 50% | -1 |
| Race/ethnicity | ||||||||
| White | 27% | 33% | 36% | -6 | 26% | 27% | 28% | -1 |
| Black | 7% | 8% | 8% | -1 | 5% | 5% | 5% | 0 |
| Hispanic | 58% | 51% | 50% | 7 | 56% | 55% | 54% | 1 |
| Other Race | 8% | 8% | 7% | 0 | 13% | 12% | 13% | 1 |
| Age | ||||||||
| 18 to 29 | 23% | 19% | 17% | 4 | 33% | 31% | 28% | 2 |
| 30 to 39 | 21% | 19% | 19% | 2 | 24% | 23% | 24% | 1 |
| 40 to 49 | 22% | 20% | 19% | 2 | 21% | 22% | 23% | -1 |
| 50 to 64 | 35% | 43% | 45% | -8 | 22% | 24% | 25% | -2 |
| Education | ||||||||
| HS or less | 57% | 49% | 47% | 8 | 58% | 57% | 57% | 1 |
| Some college | 28% | 33% | 34% | -5 | 29% | 29% | 29% | 0 |
| College Grad+ | 15% | 17% | 18% | -2 | 12% | 13% | 14% | -1 |
| Phone status | ||||||||
| Landline | 49% | 55% | 56% | -6 | 42% | 45% | 48% | -3 |
| Cell | 51% | 45% | 44% | 6 | 58% | 55% | 52% | 3 |
| Marital status | ||||||||
| Married | 33% | 34% | 33% | -1 | 37% | 38% | 37% | -1 |
| Not Married | 67% | 65% | 67% | 2 | 62% | 62% | 63% | 0 |
| Family income | ||||||||
| <138% FPL | 60% | 57% | 57% | 3 | 52% | 53% | 55% | -1 |
| 138%-400% FPL | 30% | 33% | 33% | -3 | 36% | 34% | 33% | 2 |
| 400%+ | 5% | 6% | 6% | -1 | 7% | 7% | 6% | 0 |
| Language of interview | ||||||||
| English | 63% | 70% | 72% | -7 | 65% | 66% | 64% | -1 |
| Spanish | 37% | 30% | 28% | 7 | 35% | 34% | 34% | 1 |
| Resident Status | ||||||||
| Citizen/ legal immigrant | 79% | 85% | 86% | -6 | 78% | 81% | 81% | -3 |
| Undocumented immigrant | 20% | 14% | 13% | 6 | 21% | 18% | 18% | 3 |
| Party Identification | ||||||||
| Republican | 11% | 13% | 13% | -2 | 11% | 11% | 12% | 0 |
| Democrat | 35% | 39% | 39% | -4 | 32% | 34% | 34% | -2 |
| Independent | 35% | 32% | 32% | 3 | 37% | 36% | 35% | 1 |
| Other | 9% | 8% | 8% | 1 | 9% | 9% | 9% | 0 |
Another consideration for panel surveys is the potential for “sensitization effects,” that is, what effect returning to the same people about the same topics has on their experiences or views. For example, after taking the baseline survey that covered many aspects of the coverage expansions under the ACA, were people more likely to seek out information about health insurance and enroll than they would have been otherwise? While there is no direct way to measure this effect on this survey, other analyses have found that these effects are minimal and short-lived,14 and we do not believe they would have had a substantial impact on results presented here, particularly given all the other media coverage, advertising, and outreach targeted at this population during the fall and winter of 2013, 2014, and 2015.
The margin of sampling error including the design effect for the full sample is plus or minus 5 percentage points. For the recently insured, it is plus or minus 5 percentage points and for the remaining uninsured it is plus or minus 9 percentage points. Numbers of respondents and margin of sampling error for key subgroups are shown in the table below.
| Table 6: Margin of Sampling Errors Across Subgroups | |||||
| Group | N | MOSE | |||
| Total Wave 4 | 1001 | +/- 5 percentage points | |||
| Recently Insured | 781 | +/- 5 percentage points | |||
| Recently insured by Medi-Cal | 393 | +/- 7 percentage points | |||
| Recently insured by non-group plan | 147 | +/- 11 percentage points | |||
| Recently insured through Covered California | 121 | +/- 12 percentage points | |||
| Recently insured through an employer | 180 | +/- 10 percentage points | |||
| Recently insured Hispanics | 366 | +/- 7 percentage points | |||
| Remaining Uninsured | 218 | +/- 9 percentage points | |||
| Remaining uninsured Hispanics | 143 | +/- 11 percentage points | |||
For results based on other subgroups, the margin of sampling error may be higher. Sample sizes and margin of sampling errors for other subgroups are available by request. Note that sampling error is only one of many potential sources of error in this or any other public opinion poll.
Some demographic measures referred to in the report were only asked during the baseline survey, such as questions about educational attainment, debilitating chronic condition, length of time uninsured, resident status, and race/ethnicity. For more information on the first and second waves of the Kaiser Family Foundation California Longitudinal Panel Survey visit:
Wave 1: https://www.kff.org/health-reform/report/californias-uninsured-on-the-eve-of-aca-open-enrollment/
Appendices
Findings Appendix
| Table A1: Demographic Profiles Of Each Group Of Newly Insured, Still Insured, and Remaining Uninsured Californians | ||||
| NEWLY INSURED IN 2016 (15%) | STILL INSURED IN 2016 (57%) | REMAINING UNINSURED IN 2016 (28%) | ||
| AGE | 19-29 | 32% | 21% | 24% |
| 30-49 | 35% | 42% | 55% | |
| 50-64 | 32% | 31% | 19% | |
| 65+ | 2% | 6% | 1% | |
| RACE | White non-Hispanic | 19% | 33% | 18% |
| Black non-Hispanic | 8% | 5% | 4% | |
| Other non-Hispanic | 26% | 13% | 9% | |
| Hispanic | 59% | 48% | 67% | |
| Hispanic, eligible | 30% | 40% | 33% | |
| GENDER | Male | 57% | 51% | 53% |
| Female | 43% | 49% | 47% | |
| LENGTH OF TIME UNINSURED PRIOR TO ACA | 2 months to less than a year | 6% | 15% | 8% |
| 1 year to less than 2 years | 6% | 16% | 12% | |
| 2 years or more | 43% | 49% | 39% | |
| Never had insurance | 45% | 21% | 41% | |
| EMPLOYMENT | Employed | 58% | 67% | 57% |
| Unemployed | 14% | 11% | 19% | |
| A student, retired, on disability, or stay at home parent | 26% | 21% | 24% | |
| EDUCATION | High school or less | 52% | 51% | 72% |
| Some college | 31% | 32% | 22% | |
| College or more | 13% | 16% | 6% | |
| HEALTH STATUS | Excellent/ Very good/ Good | 61% | 59% | 70% |
| Fair/ Poor | 39% | 41% | 30% | |
| MARITAL STATUS | Married | 22% | 42% | 42% |
| Not married | 77% | 57% | 58% | |
| FAMILY INCOME | Less than 138% FPL | 56% | 51% | 56% |
| Between 138% – 400% FPL | 41% | 37% | 37% | |
| Over 400% FPL | 3% | 11% | 6% | |
| DEBILITATING CHRONIC CONDITION | Yes | 12% | 20% | 8% |
| No | 87% | 79% | 92% | |
| PERSONALLY CONTACTED | Yes, been contacted | 30% | 32% | 15% |
| No, have not been contacted | 70% | 67% | 84% | |
Wave 4 Attrition Appendix
A unique consideration for panel surveys such as the Kaiser Family Foundation California Longitudinal Panel Survey is whether those who participate in subsequent waves are different in terms of their attitudes or demographics than those who refuse to participate again or were unable to be re-contacted. Of the total 2,001 respondents who completed Wave 1, 1,219 participated in Wave 2, 1,105 completed Wave 3, and 1,001 completed Wave 4. These completion rates are within an expected range given that the uninsured are already a difficult to reach population since many are lower income, younger, undocumented immigrants, and members of racial/ethnic minority groups, and may change phone numbers or move more often than the public at large. After data collection was complete, data from Wave 1 and Wave 4 were compared to evaluate the impact of some respondents not completing Wave 4, referred to as attrition. Wave 4 respondents included those who completed all four waves (n=764) as well as those who completed Waves 1 and 4 only (n=52), those who completed Waves 1, 2, and 4 (n=87), and those who completed Waves 1, 3, and 4 (n=98). The analysis was designed to assess whether: (1) The makeup of respondents differed systematically between the waves; and (2) whether these differences correspond with bias as far as the study’s substantive questions.
As detailed below in Table A1, we compared Wave 1 question responses for the total Wave 1 and Wave 4 samples to assess whether Wave 4 consists of respondents who answered Wave 1 differently than the full Wave 1 sample. The table also includes comparisons for the subsample of Wave 4 respondents who have completed all four waves. The weighted columns indicate whether any differences in sample characteristics and substantive responses were minimized through Wave 4 weighting. The comparison indicates that the greatest difference between the complete Wave 1 sample and the Wave 4 sample centers on respondents with lower educational attainment (8 percentage points less in Wave 4), Spanish speaking (7 percentage points less in Wave 4), undocumented respondents (6 percentage points less in Wave 4), male respondents (5 percentage points less in Wave 4), cell phone respondents (6 percentage points less in Wave 4), and respondents under age 30 (4 percentage points less in Wave 4), along with an increase in the share of white respondents as well as a decrease in the share of Hispanic respondents (6 and 7 percentage points, respectively). This seems to indicate that the harder-to-reach (namely undocumented), more transient (cell phone), and younger respondents were slightly less likely to be reached and to complete the Wave 4 interview. These differences are similar to the differences among those who completed all four waves of the survey. However, these demographic differences between the samples did not translate into meaningful differences on the questions of self-reported party identification, self-reported health status, or whether respondents reported having a usual source of care at Wave 1. Furthermore, once the sample was weighted as it would be in any case, only slight demographic differences remained. The variables not included in the weighting were hardly affected by weighting, or became more similar to Wave 1 (Table A2). Overall, this analysis finds fairly small observable differences between Wave 4 respondents and the full Wave 1 sample as far as Wave 1 responses. Attrition does not appear to introduce significant bias, and most differences are addressed by weighting (that was specifically designed to match the Wave 1 sample, adding parameters such as language of interview and income relative to the federal poverty level (FPL)).
| Table A2: Wave 1 To Wave 4 Sample Comparisons For Wave 1 Questions (Weighted And Unweighted) | ||||||||
| Unweighted | Weighted | |||||||
| Wave 1(n=2001) | Completed Wave 4(n=1001) | Completed all 4 Waves (n=764) | Percentage PointDifference(W1 – W4 Total) | Wave 1 | Completed Wave 4 | Completed all 4 Waves | Percentage PointDifference(W1 – W4 Total) | |
| Gender | ||||||||
| Male | 48% | 43% | 41% | 5 | 54% | 53% | 50% | 1 |
| Female | 52% | 57% | 59% | -5 | 46% | 47% | 50% | -1 |
| Race/ Ethnicity | ||||||||
| White | 27% | 33% | 36% | -6 | 26% | 27% | 28% | -1 |
| Black | 7% | 8% | 8% | -1 | 5% | 5% | 5% | 0 |
| Hispanic | 58% | 51% | 48% | 7 | 56% | 55% | 54% | 1 |
| Other Race | 8% | 8% | 8% | 0 | 13% | 12% | 13% | 1 |
| Age | ||||||||
| 19 to 29 | 23% | 19% | 17% | 4 | 33% | 31% | 28% | 2 |
| 30 to 39 | 21% | 19% | 19% | 2 | 24% | 23% | 24% | 1 |
| 40 to 49 | 22% | 20% | 19% | 2 | 21% | 22% | 23% | -1 |
| 50 to 64 | 35% | 43% | 45% | -8 | 22% | 24% | 25% | -2 |
| Education | ||||||||
| HS or less | 57% | 49% | 47% | 8 | 58% | 57% | 57% | 1 |
| Some college | 28% | 33% | 34% | -5 | 29% | 29% | 29% | 0 |
| College Grad+ | 15% | 17% | 18% | -2 | 12% | 13% | 14% | -1 |
| Phone status | ||||||||
| Landline | 49% | 55% | 56% | -6 | 42% | 45% | 48% | -3 |
| Cell | 51% | 45% | 44% | 6 | 58% | 55% | 52% | 3 |
| Marital status | ||||||||
| Married | 33% | 34% | 33% | -1 | 37% | 38% | 37% | -1 |
| Not Married | 67% | 65% | 67% | 2 | 62% | 62% | 63% | 0 |
| Family income | ||||||||
| <138% FPL | 60% | 57% | 57% | 3 | 52% | 53% | 55% | -1 |
| 138%-400% FPL | 30% | 33% | 33% | -3 | 36% | 34% | 33% | 2 |
| 400%+ FPL | 5% | 6% | 6% | -1 | 7% | 7% | 6% | 0 |
| Language of interview | ||||||||
| English | 63% | 70% | 72% | -7 | 65% | 66% | 64% | -1 |
| Spanish | 37% | 30% | 28% | 7 | 35% | 34% | 34% | 1 |
| Table A3: Wave 1 And Wave 4 Sample Comparisons For Wave 1 Questions Not Used In Weighting (Weighted And Unweighted) | ||||||||
| Unweighted | Weighted | |||||||
| Wave 1(n=2001) | Completed Wave 4(n=1001) | Completed all 4 Waves (n=764) | Percentage PointDifference(W1 – W4 Total) | Wave 1 | Completed Wave 4 | Completed all 4 Waves | Percentage PointDifference(W1 – W4 Total) | |
| Resident Status | ||||||||
| Citizen/ legal immigrant | 79% | 85% | 86% | -6 | 78% | 81% | 81% | -3 |
| Undocumented immigrant | 20% | 14% | 13% | 6 | 21% | 18% | 18% | 3 |
| Party Identification | ||||||||
| Republican | 11% | 13% | 13% | -2 | 11% | 11% | 12% | 0 |
| Democrat | 35% | 39% | 39% | -4 | 32% | 34% | 34% | -2 |
| Independent | 35% | 32% | 32% | 3 | 37% | 36% | 35% | 1 |
| Other | 9% | 8% | 8% | 1 | 9% | 9% | 9% | 0 |
| Length of time uninsured prior to ACA | ||||||||
| 2 months to less than a year | 12% | 11% | 11% | 1 | 13% | 11% | 11% | 2 |
| 1 year to less than 2 years | 12% | 12% | 13% | 0 | 14% | 13% | 15% | 1 |
| 2 years or more | 48% | 53% | 55% | -5 | 44% | 45% | 45% | -1 |
| Never insured | 28% | 23% | 21% | 5 | 29% | 30% | 30% | -1 |
| Self-reported health status | ||||||||
| Excellent/Very good/Good | 59% | 60% | 60% | -1 | 62% | 62% | 64% | 0 |
| Fair/Poor | 41% | 40% | 40% | 1 | 38% | 37% | 36% | -1 |
| Debilitating Chronic Condition | ||||||||
| Yes | 16% | 19% | 21% | -3 | 13% | 15% | 15% | -2 |
| No | 84% | 81% | 79% | 3 | 87% | 84% | 85% | 3 |
| Usual place for care | ||||||||
| Yes | 61% | 63% | 63% | -2 | 56% | 57% | 57% | -1 |
| No | 39% | 36% | 37% | 3 | 43% | 42% | 43% | 1 |
An indicator consistent with this observation is the mean Wave 1 Weight of the Wave 4 sample. This value, 0.979 (SE=0.031), indicates that the measure to which Wave 4 respondents further accentuated Wave 1 non-response patterns (corresponding with smaller weights) was relatively small, about 2%. For those who responded to all four waves, this value was slightly smaller (0.973; SE=0.036), but still indicative of overall similarity between responders and non-responders.
We also compared the unweighted demographics for those who completed Wave 4 with those who didn’t (a typical nonresponse analysis) and there are some differences between these two groups. Those who did not participate in Wave 4 were somewhat more likely to be younger, male, Hispanic, undocumented, have lower levels of education, report never having had health insurance, or prefer taking the survey in Spanish. In order to further isolate the demographic factors associated with completing the Wave 4 survey or not, we conducted a logistic regression analysis. After controlling for demographic characteristics such as income, race/ethnicity, and party identification, the factors associated with completing Wave 4 include being interviewed on a landline telephone, being older, having a disability, and having higher levels of education. The factors associated with not completing Wave 4 are being male and being Hispanic as well as being undocumented. This pattern is similar when looking at those who completed all 4 waves as well as those who have not participated since taking the initial baseline survey. As noted above, weighting corrects for some of these differences.
Endnotes
- Kaiser Family Foundation analysis of 2013 ASEC Supplement to the Current Population Survey. ↩︎
- Kaiser Family Foundation, California’s Uninsured On The Eve Of ACA Open Enrollment, September 2013, https://modern.kff.org/health-reform/report/californias-uninsured-on-the-eve-of-aca-open-enrollment/. ↩︎
- Kaiser Family Foundation, Where Are California’s Uninsured Now? Wave 2 Of The Kaiser Family Foundation California Longitudinal Panel Survey, July 2014, https://modern.kff.org/health-reform/report/where-are-californias-uninsured-now-wave-2-of-the-kaiser-family-foundation-california-longitudinal-panel-survey/. ↩︎
- Kaiser Family Foundation, California’s Previously Uninsured After The ACA’s Second Open Enrollment Period, July 2015, https://modern.kff.org/health-reform/report/californias-previously-uninsured-after-the-acas-second-open-enrollment-period/. ↩︎
- For the purposes of this report, the ‘eligible uninsured’ are California residents who said they had been uninsured for at least two months in the baseline survey and would be eligible for participation in the ACA coverage expansion based on their self-reported status as a citizen, permanent resident, or lawfully present immigrant. See the “About The Terms In This Report” Section for more details. ↩︎
- See the “About The Terms In This Report” Section for more details. ↩︎
- The total share with non-group coverage, including those in Covered California, remained stable in the past three waves. ↩︎
- It is important to note that among individuals with health insurance through Covered California, the most common reason for changing health insurance plans was that they found a plan with a lower monthly premium, however, the number of individuals in this group is too small to report. ↩︎
- The analysis of the dynamics of health insurance includes those who were unable to be contacted in spring 2014 or spring 2015. For instances of missing data from the most recent survey, their previous insurance status is reported. The only criteria for being included in this group is completing either Wave 2 or Wave 3 and completing both Wave 1 and Wave 4 surveys. ↩︎
- As previously mentioned, the analysis of the dynamics of health insurance includes those who were unable to be contacted in spring 2014 or spring 2015. For instances of missing data from the most recent survey, their previous insurance status is reported. The only criteria for being included in this group is either reporting being uninsured in Wave 2, not completing Wave 3, and reporting being insured in Wave 4; or not completing Wave 2, reporting being uninsured in Wave 3, and reporting being insured in Wave 4. ↩︎
- See the “About The Terms In This Report” Section for more details. ↩︎
- US Census Bureau, California State & County QuickFacts http://quickfacts.census.gov/qfd/states/06000.html ↩︎
- Those who had been uninsured for less than two months were excluded from the survey since they may be experiencing a short period of uninsurance (i.e. someone who is between jobs), and the goal of the survey was to capture the experiences and views of those who have been without insurance for a longer period of time and are poised to experience the new coverage provisions of the ACA. ↩︎
- M. Brodie, “Sensitization Effects in a Study of the Impact of a Nationally Broadcast Special on Health Care Reform,” in Doctoral Thesis: Political Institutions, Participation, and Media Evaluations— Influences on Health Care Policy (Boston, Mass.: Harvard University, 1995). ↩︎
New Survey Finds 72% of Previously Uninsured Californians Now Have Coverage, Including 78% of Those Eligible for New Affordable Care Act Options
Recently Insured Residents Report Greater Health and Financial Security, Though Worries about Health Care Costs and Access Persist for Some
For Remaining Uninsured Residents, Cost and Immigration Status Are Main Obstacles
Three years after the Affordable Care Act’s coverage expansions were fully implemented in California, nearly three quarters (72%) of the state’s previously uninsured residents now have health coverage, finds the fourth Kaiser Family Foundation Longitudinal Panel Survey, which is tracking the experiences of a randomly selected group of Californian adults who were uninsured in 2013. This is similar to the share who reported having insurance last year (68%).
The share with coverage is even higher (78%) among those likely eligible for Medi-Cal and private insurance purchased through Covered California, but unchanged from last year. Undocumented immigrants are not eligible to sign up for either type of coverage.
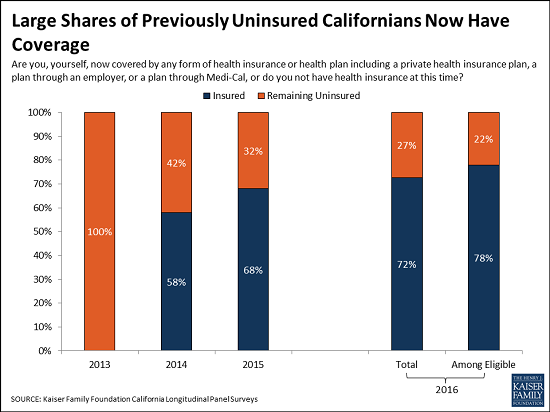
The four waves of the survey provide a detailed look at how the health and financial security of previously uninsured residents have changed in a state that fully embraced the Affordable Care Act’s opportunities to expand coverage, including creating the Covered California insurance marketplace and expanding its Medi-Cal program.
Reflecting the low incomes reported by many previously uninsured California, the largest share of recently insured residents are covered through Medi-Cal (33%), the state’s Medicaid program. The state’s marketplace, Covered California, covers about one in 10 (11%), a fifth (21%) now report employer coverage, and the rest report other sources of coverage. This new coverage likely reflects a variety of factors, including: the impact of the ACA’s new coverage options and requirements for individuals to obtain coverage and for large employer to offer it or pay penalties; a growing economy; and the regular churn of people in and out of coverage.
Overall, recently insured Californians are more likely to report that their health needs are being met today than when they were uninsured in 2013 (77% now versus 49% in 2013) and less likely to say they are very worried about paying medical bills. Californians who remain uninsured show less improvement on these and other measures of financial security and are worse off than the recently insured.
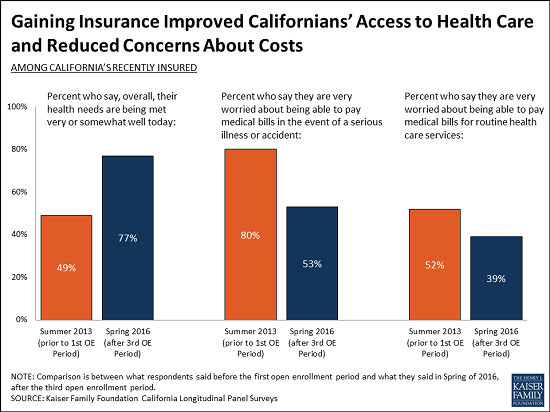
Of the recently insured, eight in 10 (79%) say their experiences with their current health insurance plan have been positive, including nearly a third (31%) who say their experiences have been very positive. Far fewer (15%) say their experiences have been negative, including just 5 percent who say very negative. Most of the recently insured also report that they are either very or somewhat satisfied with their plan’s choice of hospitals (81%), primary care doctors (76%), and specialists (68%).
At the same time, the survey finds that some recently insured Californians continue to worry about health care costs and access. For instance, one in five (20%) say they did not get medical care at some point in the past year due to cost, and more than half (53%) say they are very worried about paying medical bills in the event of a serious illness or accident, which is similar to the shares in other Foundation surveys of people with insurance nationally.
Similarly, one quarter (25%) of the recently insured say they have had to wait longer than a reasonable time to get an appointment for medical care, and 12 percent say they have been told by a doctor’s office or clinic in the past 12 months that they would not be accepted as a new patient.
While seven in 10 of California’s previously uninsured residents had gone at least two years without coverage prior to 2013, the majority now report stable coverage with nearly two thirds (63%) reporting having coverage for at least a year, including nearly half (48%) who report coverage for two or three years. Far fewer (14%) have unstable coverage, gaining it at some point, then losing it, and in some cases gaining it again.
In spite of the gains in coverage, the survey finds slightly more than a quarter (27%) of previously uninsured Californians are still without coverage. This includes 10 percent who are likely undocumented immigrants and ineligible for Medi-Cal or Covered California, leaving 17 percent who could potentially be helped by the law’s coverage expansions.
Hispanics make up two thirds (67%) of the remaining uninsured, though half of them (33% of all remaining uninsured) are likely undocumented immigrants who are not eligible for Medi-Cal or to enroll in Covered California. (Eligible Hispanics obtained coverage at rates similar to whites.)
When asked to say in their own words the main reason why they do not currently have health insurance, nearly half of the remaining uninsured (47%) say it is because health insurance is too expensive and they can’t afford it. Fewer cite eligibility issues (19%), including immigration concerns (10%). Just 2 percent cite opposition to the health care law as their main reason they don’t have coverage.
About The Survey
The survey is the fourth in a series based on the Kaiser Family Foundation California Longitudinal Panel Survey Project. It was designed and analyzed by researchers at the Foundation. The fourth and final wave of the survey was conducted primarily by telephone from February 10-June 20, 2016, among 1,001 individuals who had participated in the baseline survey. The baseline survey was conducted from July 11-August 29, 2013 with a representative sample of 2,001 adults ages 19 to 64 living in California who reported having been without health insurance for at least two months at the time of the survey. Interviews were carried out in English and Spanish by SSRS, an independent research company. The panel survey estimates the percentage of the previously uninsured who gained coverage and does not estimate the overall change in the number of uninsured Californians because it does not include anyone who may have been insured prior to open enrollment but is now uninsured. The margin of sampling error including the design effect is plus or minus 5 percentage points for results based on the full sample and for recently insured Californians, and 9 percentage points for those Californians who remain uninsured. For other subgroups, the margin of sampling error may be higher. Fieldwork for the panel survey is supported by a grant from The California Endowment.
Explaining Health Care Reform: Risk Adjustment, Reinsurance, and Risk Corridors
As of January 1, 2014, insurers are no longer able to deny coverage or charge higher premiums based on preexisting conditions (under rules referred to as guaranteed issue and modified community rating, respectively). These aspects of the Affordable Care Act (ACA) – along with tax credits for low and middle income people buying insurance on their own in new health insurance marketplaces – make it easier for people with preexisting conditions to gain insurance coverage. However, if not accompanied by other regulatory measures, these provisions could have unintended consequences for the insurance market. Namely, insurers may try to compete by avoiding sicker enrollees rather than by providing the best value to consumers. In addition, in the early years of market reform insurers faced uncertainty as to how to price coverage as new people (including those previously considered “uninsurable”) gained coverage, potentially leading to premium volatility. This brief explains three provisions of the ACA – risk adjustment, reinsurance, and risk corridors – that were intended to promote insurer competition on the basis of quality and value and promote insurance market stability, particularly in the early years of reform.
Background: Adverse Selection & Risk Selection
One concern with the guaranteed availability of insurance is that consumers who are most in need of health care may be more likely to purchase insurance. This phenomenon, known as adverse selection, can lead to higher average premiums, thereby disrupting the insurance market and undermining the goals of reform. Uncertainty about the health status of enrollees could also make insurers cautious about offering plans in a reformed individual market or cause them to be overly conservative in setting premiums. To discourage behavior that could lead to adverse selection, the ACA makes it difficult for people to wait until they are sick to purchase insurance (i.e. by limiting open enrollment periods, requiring most people to have insurance coverage or pay a penalty, and providing subsidies to help with the cost of insurance).
Risk selection is a related concern, which occurs when insurers have an incentive to avoid enrolling people who are in worse health and likely to require costly medical care. Under the ACA, insurers are no longer permitted to deny coverage or charge higher premiums on the basis of health status. However, insurers may still try to attract healthier clients by making their products unattractive to people with expensive health conditions (e.g., in what benefits they cover or through their drug formularies). Or, certain products (e.g., ones with higher deductibles and lower premiums) may be inherently more attractive to healthier individuals. This type of risk selection has the potential to make the market less efficient because insurers may compete on the basis of attracting healthier people to enroll, as opposed to competing by providing the most value to consumers.
The ACA’s risk adjustment, reinsurance, and risk corridors programs were intended to protect against the negative effects of adverse selection and risk selection, and also work to stabilize premiums, particularly during the initial years of ACA implementation.
Each program varies by the types of plans that participate, the level of government responsible for oversight, the criteria for charges and payments, the sources of funds, and the duration of the program. The table below outlines the basic characteristics of each program.
| Table 1: Summary of Risk and Market Stabilization Programs in the Affordable Care Act | |||
| Risk Adjustment | Reinsurance | Risk Corridors | |
| What the program does | Redistributes funds from plans with lower-risk enrollees to plans with higher-risk enrollees | Provides payment to plans that enroll higher-cost individuals | Limits losses and gains beyond an allowable range |
| Why it was enacted | Protects against adverse selection and risk selection in the individual and small group markets, inside and outside the exchanges by spreading financial risk across the markets | Protects against premium increases in the individual market by offsetting the expenses of high-cost individuals | Stabilizes premiums and protects against inaccurate premium setting during initial years of the reform |
| Who participates | Non-grandfathered individual and small group market plans, both inside and outside of the exchanges | All health insurance issuers and self-insured plans contribute funds; individual market plans subject to new market rules (both inside and outside the exchange) are eligible for payment | Qualified Health Plans (QHPs), which are plans qualified to be offered on a health insurance marketplace (also called exchange) |
| How it works | Plans’ average actuarial risk will be determined based on enrollees’ individual risk scores. Plans with lower actuarial risk will make payments to higher risk plans. Payments net to zero. | If an enrollee’s costs exceed a certain threshold (called an attachment point), the plan is eligible for payment (up to the reinsurance cap). Payments net to zero. | HHS collects funds from plans with lower than expected claims and makes payments to plans with higher than expected claims. Plans with actual claims less than 97% of target amounts pay into the program and plans with claims greater than 103% of target amounts receive funds. Payments net to zero. |
| When it goes into effect | 2014, onward (Permanent) | 2014 – 2016 (Temporary – 3 years) | 2014 – 2016(Temporary – 3 years) |
Risk Adjustment
The ACA’s risk adjustment program is intended to reinforce market rules that prohibit risk selection by insurers. Risk adjustment accomplishes this by transferring funds from plans with lower-risk enrollees to plans with higher-risk enrollees. The goal of the risk adjustment program is to encourage insurers to compete based on the value and efficiency of their plans rather than by attracting healthier enrollees. To the extent that risk selecting behavior by insurers – or decisions made by enrollees – drive up costs in the health insurance marketplaces (for example, if insurers selling outside the Exchange try to keep premiums low by steering sick applicants to Exchange coverage), risk adjustment also works to stabilize premiums and the cost of tax credit subsidies to the federal government.
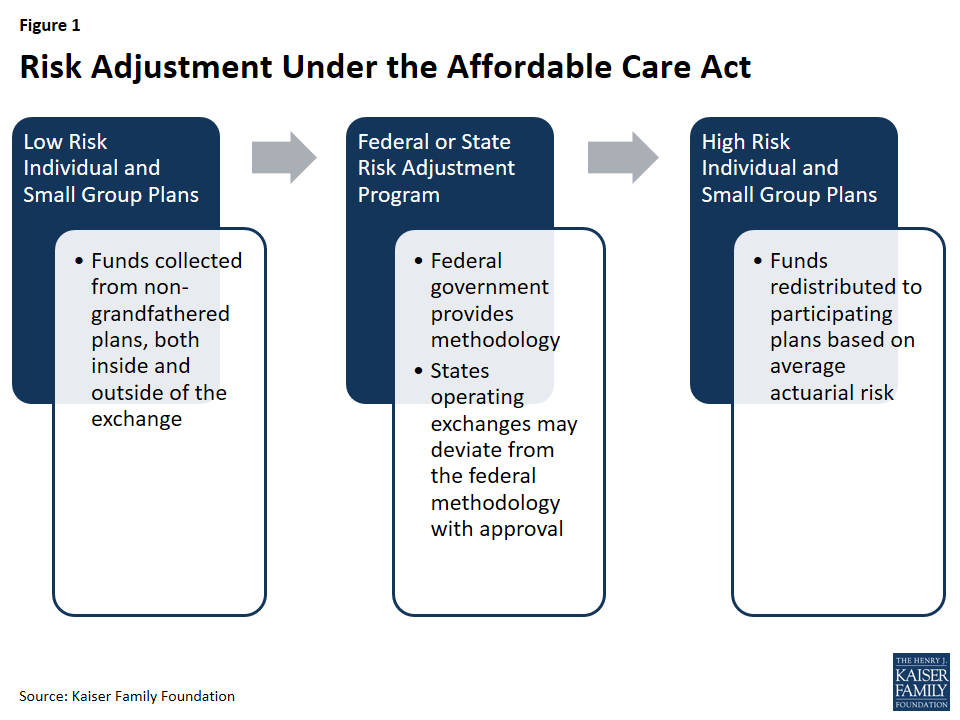
Program Participation
The risk adjustment program applies to non-grandfathered plans in the individual and small group insurance markets, both inside and outside of the exchanges, with some exceptions. Plans in existence at the time the ACA was enacted in March 2010 were grandfathered under the law and are subject to fewer requirements. Plans lose their grandfathered status if they make significant changes (such as significantly increasing cost-sharing or imposing new annual benefit limits). Plans that were renewed prior to January 1, 2014, and are therefore not subject to most ACA requirements, are not part of the risk adjustment system. Multi-state plans and Consumer Operated and Oriented Plans (COOP) are subject to risk adjustment. Unless a state chooses to combine its individual and small group markets, separate risk adjustment systems operate in each market.
Government Oversight
States operating an exchange have the option to either establish their own state-run risk adjustment program or allow the federal government to run the program. States choosing not to operate an exchange or marketplace (and thus utilizing the federally-run exchange, called the Health Insurance Marketplace) do not have the option to run their own risk adjustment programs and must use the federal model. In states for which HHS operates risk adjustment, issuers are charged a fee to cover the costs of administering the program.
HHS developed a federally-certified risk adjustment methodology to be used by states or by HHS on behalf of states. States electing to use an alternative model must first seek federal approval and must submit yearly reports to HHS. States electing to run their own risk adjustment program must publish a notice of benefit and payment parameters by March 1 of the year prior to the benefit year; otherwise they will forgo the option to deviate from the federal methodology. Once a state’s alternative methodology is approved, it becomes federally-certified and can be used by other states. Massachusetts, the only state so far to operate its own risk adjustment program, will end is program in 2017. In 2017, HHS will operate risk adjustment programs in all states.
Calculation of Payments & Charges
Under risk adjustment, eligible insurers are compared based on the average financial risk of their enrollees. The HHS methodology estimates financial risk using enrollee demographics and claims for specified medical diagnoses. It then compares plans in each geographic area and market segment based on the average risk of their enrollees, in order to assess which plans will be charged and which will be issued payments.
Under HHS’s methodology, individual risk scores – based on each individual’s age, sex, and diagnoses – are assigned to each enrollee. Diagnoses are grouped into a Hierarchical Condition Category (HCC) and assigned a numeric value that represents the relative expenditures a plan is likely to incur for an enrollee with a given category of medical diagnosis. If an enrollee has multiple, unrelated diagnoses (such as prostate cancer and arthritis), both HCC values are used in calculating the individual risk score. Additionally, if an adult enrollee has certain combinations of illnesses (such as a severe illness and an opportunistic infection), an interaction factor is added to the person’s individual risk score. Finally, if the enrollee is receiving subsidies to reduce their cost-sharing, an induced utilization factor is applied to account for induced demand. Plans with enrollees that receive cost-sharing reductions under the ACA receive an adjustment because cost-sharing reductions may induce demand for health care and are not otherwise accounted for in the other premium stabilization programs. Once individual risk scores are calculated for all enrollees in the plan, these values are averaged across the plan to arrive at the plan’s average risk score. The average risk score, which is a weighted average of all enrollees’ individual risk scores, represents the plan’s predicted expenses. Under the HHS methodology, adjustments are made for a variety of factors, including actuarial value (i.e., the extent of patient cost-sharing in the plan), allowable rating variation, and geographic cost variation. Under risk adjustment, plans with a relatively low average risk score make payments into the system, while plans with relatively high average risk scores receive payments.
Transfers (both payments and charges) are calculated by comparing each plan’s average risk score to a baseline premium (the average premium in the state). Transfers are calculated for each geographic rating area, such that insurers offering coverage in multiple rating areas in a given state have multiple transfer amounts that are grouped into a single invoice. Transfers within a given state net to zero.
On March 25, 2016, CMS hosted a public conference and released a white paper to review risk adjustment methodology and build on the first several years of experience. The white paper examined proposals to account for partial year enrollees and prescription drug use in the risk adjustment model. CMS intends to propose that the risk adjustment model begin to account for partial year enrollees in the 2017 benefit year, and begin to account for prescription drug utilization in the 2018 benefit year. Beginning in 2017, HHS will also begin to incorporate preventive services into their simulation of plan liability, and will incorporate different trend factors for traditional drugs, specialty drugs, and medical and surgical expenditures. This is intended to better reflect the growth of prescription drug expenditures compared to other medical expenditures. The risk adjustment model will be recalibrated using the most recent claims data from the Truven Health Analytics 2012, 2013, and 2014 MarketScan Commercial Claims and Encounters database (MarketScan). In response to issuer feedback from the 2014 benefit year of the risk adjustment program, CMS will also begin providing insurers with early estimates of health plan specific risk adjustment calculations. This is intended to give plans more timely information in order to set premiums. In addition, CMS has indicated that it is exploring other options to modify the permanent risk adjustment program to better adjust for higher-cost enrollees, as the temporary reinsurance program phases out in 2016.
Data Collection & Privacy
Under the federal risk adjustment program, to protect consumer privacy and confidentiality, insurers are responsible for providing HHS with de-identified data, including enrollees’ individual risk scores. States are not required to use this model of data collection, but are required to only collect information reasonably necessary to operate the risk adjustment program and are prohibited from collecting personally identifiable information. Insurers may require providers and suppliers to submit the appropriate data needed for risk adjustment calculations.
For each benefit year, an issuer of a risk adjustment covered plan or a reinsurance-eligible plan must establish a dedicated data environment (i.e. an EDGE server) and provide data access to HHS, in a timeframe specified by HHS, to be eligible for risk adjustment and/or reinsurance payments. CMS released guidance for EDGE Data submissions for the 2015 benefit year.
To ensure accurate reporting, HHS recommends that insurers first validate their data through an independent audit and then submit the data to HHS for a second audit. For the first two benefit years (2014 and 2015) no adjustments to payments or charges were made as HHS optimized the data validation process. In 2016 and onward, if an issuer fails to establish a dedicated distributed data environment, fails to submit risk adjustment data, or if any errors are found through these audits, the insurer’s average actuarial risk will be adjusted, along with any payments or charges. Because the audit process is expected to take more than one year to complete, the first adjustments to payments (for the 2016 benefit year) will be issued in 2018. Any issuer that fails to provide HHS access to EDGE server data in time to assess payments will be assessed a default risk adjustment charge. In 2015, 817 of 821 issuers participating in the risk adjustment program submitted the EDGE server data necessary to calculate risk adjustment transfers and 4 issuers were assessed the default charge.
Payments for the 2014 and 2015 Benefit Years
On Oct 1, 2015, HHS announced the results of the reinsurance, risk adjustment, and risk corridors programs for the first benefit year, 2014. For the 2014 benefit year of the risk adjustment program, $4.6 billion was transferred among insurers, and 758 total issuers participated in the program. An independent analysis found that the relative health of enrollees was the main determinant of whether an issuer received a risk adjustment payment. CMS reports that this is a sign that the risk adjustment formula is working as intended in transferring payments from plans with healthier enrollees to plans with sicker enrollees.
On June 30, 2016, HHS released a summary report on the results of the reinsurance and risk adjustment programs for the 2015 benefit year. For the 2015 benefit year of the risk adjustment program, risk adjustment transfers averaged 10% of premiums in the individual market and 6% of premiums in the small group market, similar to 2014. 821 issuers participated in the risk adjustment program. HHS also made available to each issuer of a risk adjustment covered plan a report that includes the issuer’s risk adjustment payment or charge.
Risk adjustment payments to issuers for benefit year 2015 will be sequestered at a rate of 7%, per government sequestration requirements for fiscal year 2016. HHS has suggested that risk adjustment payments sequestered in fiscal year 2016 will become available for payment to issuers in fiscal year 2017 without further Congressional action.
Reinsurance
The goal of the ACA’s temporary reinsurance program was to stabilize individual market premiums during the early years of new market reforms (e.g. guaranteed issue). The temporary program is in place from 2014 through 2016. The program transfers funds to individual market insurance plans with higher-cost enrollees in order to reduce the incentive for insurers to charge higher premiums due to new market reforms that guarantee the availability of coverage regardless of health status.
Reinsurance differs from risk adjustment in that reinsurance is meant to stabilize premiums by reducing the incentive for insurers to charge higher premiums due to concerns about higher-risk people enrolling early in the program, whereas risk adjustment is meant to stabilize premiums by mitigating the effects of risk selection across plans. Thus, reinsurance payments are only made to individual market plans that are subject to new market rules (e.g., guaranteed issue), whereas risk adjustment payments are made to both individual and small group plans. Additionally, reinsurance payments are based on actual costs, whereas risk adjustment payments are based on expected costs. As reinsurance is based on actual rather than predicted costs, reinsurance payments will also account for low-risk individuals who may have unexpectedly high costs (such as costs incurred due to an accident or sudden onset of an illness). Under reinsurance, some plans may receive payments for high-cost/high-risk enrollees, and still be eligible for payment for those enrollees under risk adjustment.
While risk adjustment payments net to zero within the individual and small group markets, reinsurance payments represent a net flow of dollars into the individual market, in effect subsidizing premiums in that market for a period of time. To cover the costs of reinsurance payments and administering the program, funds are collected from all health insurance issuers and third party administrators (including those in the individual and group markets). HHS issues reinsurance payments to plans based on need, rather than issuing payments proportional to the amount of contributions from each state.
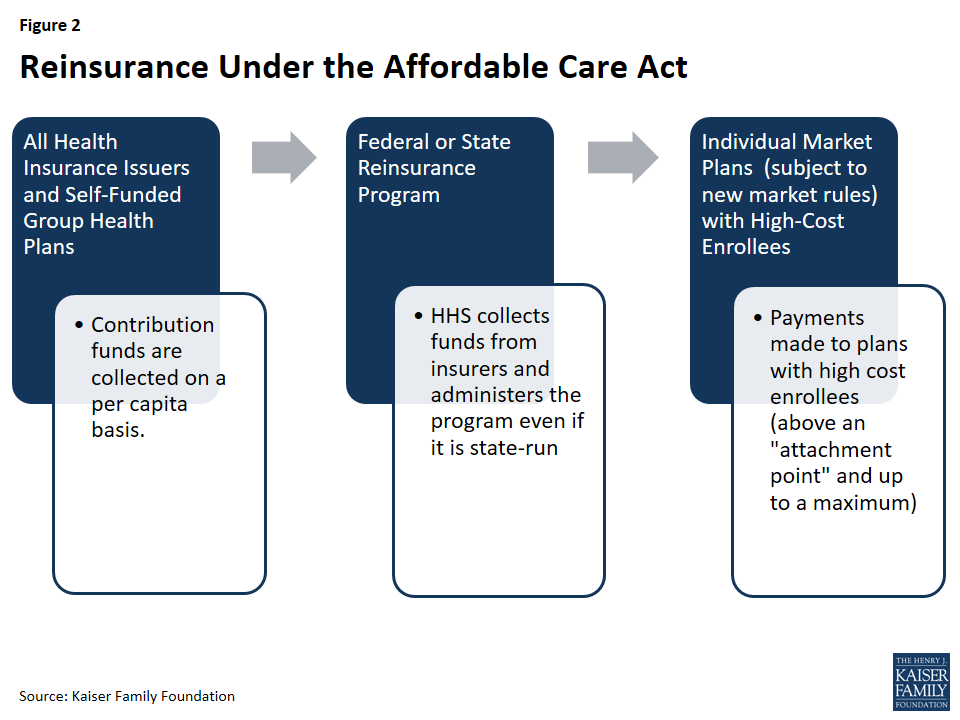
Program Participation
All individual, small group, and large group market issuers of fully-insured major medical products, as well as self-funded plans, contribute funds to the reinsurance program. Reinsurance payments are made to individual market issuers that cover high-cost individuals (and are subject to the ACA’s market rules). State high risk pools are excluded from the program.
Government Oversight
States have the option to operate their own reinsurance program or allow HHS to run one for the state. For states that choose to operate their own reinsurance program, there is no formal HHS approval process. However, states’ ability to deviate from the HHS guidelines is limited: HHS collects all reinsurance contributions – even if the program is state-run – and all states must follow a national payment schedule. Additionally, states that wish to modify data requirements must publish a notice of benefit and payment parameters. States may collect additional funds if they believe the cost of reinsurance payments and program administration will exceed the amount specified at the national level. States wishing to continue reinsurance programs after 2016 may do so, but they may not continue to use funds collected as part of the ACA’s reinsurance program after the year 2018. Connecticut was the only state to operate its own reinsurance program for benefit years 2014 and 2015. In July 2016, Alaska signed into law a two-year reinsurance program that recreates Alaska’s high-risk pool as a reinsurance fund. Alaska’s reinsurance program will cover claims for 2015 and 2016 benefit years.
Calculation of Payments and Charges
The ACA set national levels for reinsurance funds at $10 billion in 2014, $6 billion in 2015, and $4 billion in 2016. Based on estimates of the number of enrollees, HHS set a uniform reinsurance contribution rate of $63 per person in 2014, $44 per person in 2015, and $27 per person in 2016.
Eligible insurance plans received reinsurance payments when the plan’s cost for an enrollee crossed a certain threshold, called an attachment point. HHS set the attachment point (a dollar amount of insurer costs, above which the insurer is eligible for reinsurance payments) at $45,000 in 2014 and 2015. Given the smaller reinsurance payments pool for 2016, HHS raised the attachment point to $90,000 for the 2016 benefit year. HHS also set a reinsurance cap (a dollar-amount threshold, above which the insurer is no longer eligible for reinsurance) at $250,000 in 2014, 2015, and 2016. HHS initially set the coinsurance rate (the percentage of the costs above an attachment point and below the reinsurance cap that were reimbursed through the reinsurance program) at 80 percent in 2014 and 50 percent in 2015 and 2016. If reinsurance contributions exceeded the amount of payments requested, then that year’s reinsurance payments to insurers were increased proportionately (i.e. the coinsurance rate increased up to 100%). For example, in 2014, HHS was ultimately able to pay out 100 percent of claims rather than 80 percent, and in 2015 HHS raised the coinsurance rate to 55.1 percent. If surplus reinsurance funds remained available, they were rolled forward to the next benefit year. For example, $1.7 billion in surplus reinsurance funds collected for the 2014 benefit year were rolled forward to the 2015 benefit year. Similarly, if reinsurance contributions had fallen short of the amount requested for payments, then that year’s reinsurance payments would have decreased proportionately. Overall, total payments could not exceed the amount collected through contributions by insurers and third-party administrators.
States opting to raise additional reinsurance funds may do so by decreasing the attachment point, increasing the reinsurance cap, and/or increasing the coinsurance rate. States may not make changes to the national attachment point, reinsurance cap, or coinsurance rate that would result in lower reinsurance payments.
Data Collection & Privacy
Payment amounts made to eligible individual market insurers were based on medical cost data (to identify high-cost enrollees, for which plans receive reinsurance payment). Therefore, in order to calculate reinsurance payments, HHS or state reinsurance entities must either collect or be allowed access to claims data as well as data on cost-sharing reductions (because reinsurance payments were not made for costs that have already been reimbursed through cost sharing subsidies). In states for which HHS ran the reinsurance program, HHS used the same distributed data collection approach used for the risk adjustment program (i.e. an EDGE server) and similarly ensured that the collection of personally identifiable information was limited to that necessary to calculate payments. HHS proposed to conduct audits of participating insurers as well as states conducting their own reinsurance programs.
For the first two benefit years (2014 and 2015) no adjustments to reinsurance payments were made as HHS optimized the data validation process. In 2016, if an issuer fails to establish a dedicated distributed data environment or fails to adhere to reinsurance data submission requirements, the insurer may forfeit reinsurance payments. In 2015, 574 of 575 issuers participating in the reinsurance program submitted the EDGE server data necessary to calculate reinsurance payments.
Payments for the 2014 and 2015 Benefit Years
In June 2015, CMS announced the results of the reinsurance program for the first benefit year, 2014. In 2014, reinsurance contributions ($9.7 billion) exceeded requests for payments ($7.9 billion) and CMS was able to payout 100 percent of eligible claims rather than 80 percent – this amounted to $7.9 billion in reinsurance payments made to 437 issuers nationwide. Following these payments, approximately $1.7 billion in surplus reinsurance funds from the 2014 benefit year remained available, and were rolled forward to the 2015 benefit year.
CMS used this surplus of $1.7 billion, combined with additional collections of reinsurance contributions for the 2015 benefit year, to make an early partial reinsurance payment to issuers for the 2015 benefit year in March and April 2016. CMS calculated this early payment based on accepted enrollment and claims data as of February 1, 2016, at a coinsurance rate of 25%. CMS stated that reinsurance funds not paid out through this early payment will be paid out in late 2016, as part of the standard reinsurance payment process.
On June 30, 2016, CMS announced the results of the reinsurance program for the second benefit year, 2015. In 2015, estimated reinsurance contributions ($6.5 billion) were smaller than requests for payments ($14.3 billion). CMS estimates it will make $7.8 billion in reinsurance payments to 497 of the 575 participating issuers nationwide at a coinsurance rate of 55.1%.
CMS has collected approximately $5.5 billion in reinsurance contributions for 2015, with approximately $1 billion more scheduled to be collected on or before November 15, 2016. Any reinsurance contribution amounts collected above $6 billion for the 2015 benefit year are required to be allocated to the U.S. Treasury on a pro rata basis as an operating expense of the program. Combined with the surplus of $1.7 billion from 2014, CMS estimates it will have approximately $7.8 billion in reinsurance contributions available to be distributed as payments to issuers for the 2015 benefit year. On June 30, 2016 HHS made available to each issuer of a reinsurance-eligible plan a report that includes the issuer’s initial, estimated reinsurance payment for the 2015 benefit year. On August 11, 2016, CMS released an analysis based on reinsurance payments that suggests per-enrollee costs in the individual market were essentially unchanged between 2014 and 2015.
Reinsurance payments to issuers for benefit year 2015 will be sequestered at a rate of 6.8% per government sequestration requirements for fiscal year 2016. HHS has suggested that risk adjustment payments sequestered in fiscal year 2016 will become available for payment to issuers in fiscal year 2017 without further Congressional action.
Risk Corridors
The ACA’s temporary risk corridor program was intended to promote accurate premiums in the early years of the exchanges (2014 through 2016) by discouraging insurers from setting premiums high in response to uncertainty about who will enroll and what they will cost. The program worked by cushioning insurers participating in exchanges and marketplaces from extreme gains and losses.
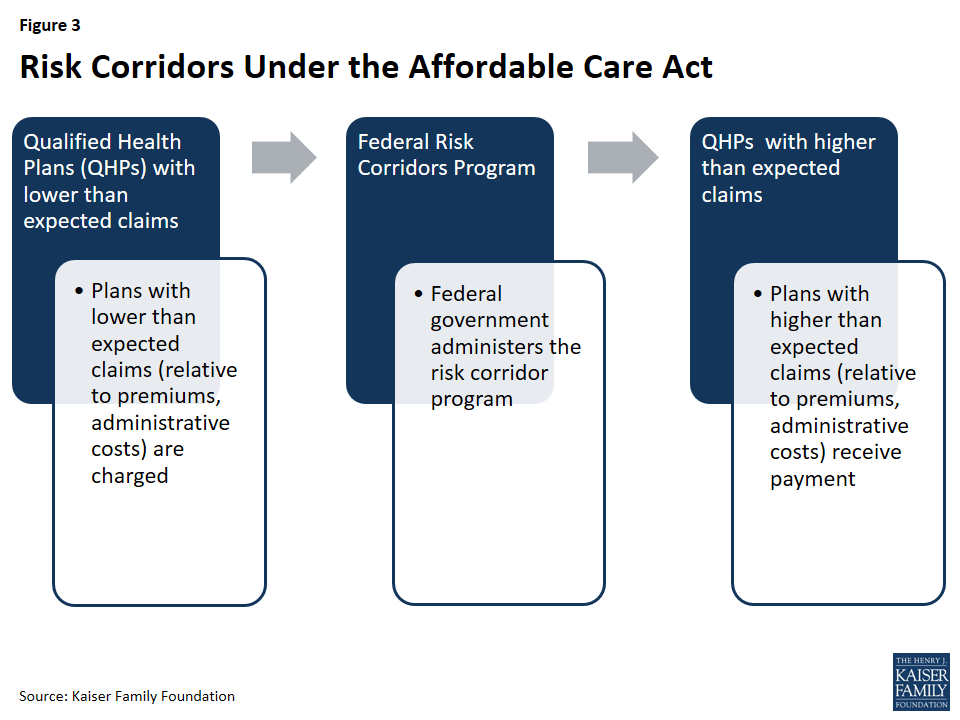
The Risk Corridors program set a target for exchange participating insurers to spend 80% of premium dollars on health care and quality improvement. Insurers with costs less than 3% of the target amount must pay into the risk corridors program; the funds collected were used to reimburse plans with costs that exceed 3% of the target amount.
This program was intended to work in conjunction with the ACA’s medical loss ratio (MLR) provision, which requires most individual and small group insurers to spend at least 80% of premium dollars on enrollee’s medical care and quality improvement expenses, or else issue a refund to enrollees.
Program Participation
All Qualified Health Plans (or QHPs, plans qualified to participate in the exchanges) were subject to the risk corridor program. Only those plans with expenses falling outside of allowable ranges made payments to the program (or qualified to receive payments). Qualified Health Plan (QHP) issuers may also offer QHPs outside of the exchange, in which case the QHP outside of the exchange were also subject to the risk corridors program.
Government Oversight
The risk corridor program was federally administered. HHS charged plans with larger than expected gains and made payments to plans with larger than expected losses.
Calculation of Payments and Charges
Each year, each Qualified Health Plan was assigned a target amount for what are called allowable costs (expenditures on medical care for enrollees and quality improvement activities) based on its premiums. Allowable costs included medical claims and costs associated with quality improvement efforts, as defined in the ACA’s medical loss ratio (MLR) calculations. Insurers must also account for any cost-sharing reductions received from HHS by reducing their allowable costs by this amount. If an insurer’s actual claims fell within plus or minus three percent of the target amount (i.e. premiums less allowable costs), it made no payments into the risk corridor program and received no payments from it. In other words, the plan was fully at risk for any loss or gain. QHPs with lower than expected claims paid into the risk corridor program:
- A QHP with claims falling below its target amount by 3% – 8% paid HHS in the amount of 50% of the difference between its actual claims and 97% of its target amount.
- A QHP with claims falling below its target amount by more than 8% paid 2.5 percent of the target amount plus 80% of the difference between their actual claims and 92% of its target.
HHS provides an example of an insurer with a $10 million target amount and actual claims of $8.8 million (or 88% of the target amount). The insurer would have to pay $570,000 to the risk corridors program because (2.5%*$10 million) + (80%*((92%*10 million)-8.8 million) = 570,000.
Conversely, HHS reimbursed plans with higher than expected costs:
- A QHP with actual claims that exceeded its target amount by 3% to 8% received a payment in the amount of 50% of the amount in excess of 103% of the target.
- A QHP with claims that exceed its target amount by more than 8% received payment in the amount of 2.5% of the target amount plus 80% of the amount in excess of 108% of the target.
In response to reports of individual market plan cancelations in November 2013, HHS instituted a transitional policy allowing certain plans to be reinstated if state regulators agree to adopt a similar transitional policy. As this policy change affected the composition of the exchange risk pool, HHS modified the risk corridors program in 2015 to change the way allowable costs are calculated (i.e., by increasing the ceiling on administrative costs and the profit margin floor by 2 percent).
In the original statute, risk corridor payments were not required to net to zero, meaning that the federal government could experience an increase in revenues or an increase in costs under the program. However, in the 2015 and 2016 appropriations bills, Congress specified that payments under the risk corridor program made to insurers in 2015 could not exceed collections from that year, and that CMS cannot transfer funds from other accounts to pay for the risk corridors program. This made the risk corridors program revenue neutral –meaning that only contributions collected from insurers could be used to fund payments for the risk corridor program. In the event that claims exceeded funds collected in a given year, CMS paid out claims pro rata and carried over deficiencies to be paid in the following year before any other claims are paid in that year. If the three-year risk corridors program ends with outstanding claims, HHS has stated it will work with Congress to secure funding for outstanding risk corridors payments, subject to the availability of appropriations.
Data Collection & Privacy
In order to calculate payments and charges for the risk corridors program, QHPs were required to submit financial data to HHS, including the actual amount of premiums earned as well as any cost-sharing reductions received. To reduce the administrative burden on insurers, HHS tied the data collection and validation requirements for the risk corridors to that of the Medical Loss Ratio (MLR) provision of the ACA. HHS will also conduct audits for the risk corridors program in conjunction with audits for the reinsurance and risk corridors program to minimize the burden on insurers.
Payments for the 2014 Benefit Year
On October 1, 2015, CMS announced that total risk corridors claims for 2014 amounted to $2.87 billion, and that insurer risk corridor contributions totaled $362 million. As a result, risk corridor payments for 2014 claims were paid out at 12.6% of claims. CMS anticipates that the remaining claims for 2014 will be paid out from 2015 risk corridor collections, and any shortfalls from 2015 claims will be covered by 2016 collections in 2017. If there are still outstanding claims when the risk corridors program ends in 2017, HHS has stated it will work with Congress to explore other sources of funding for risk corridor payments, subject to availability of appropriations.
Conclusion
The Affordable Care Act’s risk adjustment, reinsurance, and risk corridors programs were designed to work together to mitigate the potential effects of adverse selection and risk selection. All three programs aimed to provide stability in the early years of a reformed health insurance market, with risk adjustment continuing over the long-term. Many health insurance plans are subject to more than one premium stabilization program, and while the programs have similar goals, they are designed to be complementary. Specifically, risk adjustment is designed to mitigate any incentives for plans to attract healthier individuals and compensate those that enroll a disproportionately sick population. Risk corridors were intended to reduce overall financial uncertainty for insurers, though they largely did not fulfill that goal following congressional changes to the program. Reinsurance compensated plans for their high-cost enrollees, and by the nature of its financing provided a subsidy for individual market premiums generally over a three-year period. Premium increases are expected to be higher in 2017 in part due to the end of the reinsurance program.
Improving Access to Oral Health Care for Adults in Medicaid: Key Themes from a Policy Roundtable
Executive Summary
State Medicaid and CHIP programs have made significant strides in improving low-income children’s access to and use of dental care, but access to dental care for low-income adults lags far behind. To probe current opportunities, challenges, and strategies related to expanding access to oral health care for adults in Medicaid, the Kaiser Commission on Medicaid and the Uninsured convened a group of experts and stakeholders in Spring 2016 to discuss the issues. Several key themes emerged from the conversation:
- Oral disease affects overall health and well-being and also bears on other major national concerns. Poor oral health has adverse impacts on overall health and well-being. The detrimental effects of poor oral health and lack of access to services among low-income adults also ramify to employability, opiate abuse, emergency department use, and health disparities.
- Good oral health among low-income adults is an achievable goal. The science of dental caries is understood and dentistry possesses the clinical tools to prevent and manage it. Emphasizing that this capability exists and raising awareness about the burden and impact of oral disease on low-income adults could increase support and political will to expand Medicaid dental coverage for adults.
- States have levers in Medicaid to improve access to dental care for adults. States can expand Medicaid to low-income adults, expand dental benefits, ease administrative burdens that dampen dentist participation, improve provider payment, and make strategic use of incentives to improve access to and utilization of dental care.
- Innovative workforce approaches can help maximize current oral health resources and expand access. Elimination of scope-of-practice restrictions, new provider types, teledentistry, and health center expansion can increase the supply and availability of oral health care to address the growing demand for care among low-income adults as coverage expands.
- Experts say that ending the oral health crisis will not be possible without transforming the oral health care system. Ending the epidemic of poor oral health among poor populations will require an oral health system centered on prevention and evidence-based care, not driven by an invariable set of covered benefits; integration of oral and primary care; and community-based models of care.
Report
Introduction
A little over 15 years ago, Oral Health in America: A Report of the Surgeon General documented a “silent epidemic” of dental and oral diseases among poor Americans and people of color. Through concerted efforts by the Centers for Medicare and Medicaid Services (CMS) and the states in recent years, the share of low-income children enrolled in Medicaid and the Children’s Health Insurance Program (CHIP) who receive preventive dental care and treatment services has been growing, although continued efforts are needed to further reduce income- and insurance-related disparities in children’s utilization of dental services. Compared to children, access to oral health care for low-income adults has lagged far behind, for two main reasons. First, historically, Medicaid eligibility for non-elderly adults has been very restrictive, leaving many uninsured. Second, while states must provide dental benefits for children in Medicaid and CHIP, adult dental benefits are a state option.
The environment for efforts to increase access to dental care for low-income adults is favorable. Millions of previously uninsured adults have gained coverage under the Affordable Care Act’s (ACA) expansion of Medicaid to non-elderly adults with income up to 138% of the federal poverty level. Growing awareness of the importance of oral health to overall health and well-being, the movement toward more integrated care, and improving state economies have all brought the issue of strengthening adult dental benefits in Medicaid into sharper focus. A major infusion of federal funding has enabled health centers, a key source of dental care in underserved communities, to expand their service capacity. And new workforce and care delivery models designed to increase access to dental care are spreading.
To probe current opportunities, challenges, and strategies associated with improving access to oral health care for adults in Medicaid, the Kaiser Commission on Medicaid and the Uninsured convened a diverse group of experts and stakeholders in Spring 2016 for a roundtable discussion of the issues. Participants included federal and state Medicaid officials, dental providers, a large health center and large Medicaid health plan, leading clinical experts, and policy researchers, who brought a range of expertise and perspectives to the discussion. This report summarizes key themes that emerged from the conversation. A related brief provides key data and information about low-income adults’ oral health status, their access to dental care, and coverage of adult dental benefits in Medicaid.
Key Themes
Good oral health among low-income adults is an achievable goal.
Good oral health is integral to overall health and well-being.
As one roundtable participant put the point: “The mouth is part of the body.” Discussants cited associations between oral infection and chronic diseases prevalent among low-income adults, such as diabetes, and poor birth outcomes. They also stressed the broader impacts of oral health problems on individual well-being, including pain and suffering and potential adverse implications of bad or missing teeth for nutrition, employability, and self-esteem.
The capability to prevent dental disease exists.
It was noted emphatically that dental caries (tooth decay) – in sharp distinction to many other health conditions – is well-understood scientifically, and dentistry possesses the clinical know-how and technology to prevent and manage it. However, federal and state policy decisions have led to limited public spending for oral health coverage and care. Discussants suggested that messaging to policymakers and the public that emphasizes that we have capability to solve this problem, but are under-spending, could build more pressure to increase funding for adult dental coverage and services.
Failure to address the oral health needs of low-income adults affects other national priorities as well; connecting the dots could impel more action.
Roundtable participants underscored that poor access to oral health care among low-income adults stands in the way of national goals to improve population health and health equity. They also pointed out that, in addition to its adverse impact on adult oral health itself, lack of access to dental care is also a factor in both high rates of preventable emergency departments (ED) use and the opioid abuse epidemic. Individuals who lack dental coverage and care often have no alternative but to seek care in a hospital ED when they have oral pain and, since EDs do not generally provide dental services, prescription pain relief medication and a referral slip for dental care is often all they can offer. Discussants also observed that poor teeth can jeopardize job prospects among low-income adults. Interconnections were drawn between oral health problems, drug use, unemployment and economic marginalization, and incarceration, and between these risk factors and persistent social and economic disparities. Attendees suggested that, in framing initiatives to expand Medicaid adult dental coverage, articulating these connections might help broaden the constituency and strengthen the case for federal and state policy action.
A federal initiative to improve access to oral health care for adults would bring focus and resources to the issue and help drive state action.
Reflecting on the CMS Oral Health Initiative focused on children in Medicaid and CHIP, launched in 2010, and the important gains in low-income children’s utilization of dental care that have been achieved since then, discussants proposed that a similar federal initiative directed toward adults in Medicaid that sets goals for improvement, provides technical assistance to states, increases reporting, and establishes dental quality metrics, would sharpen states’ attention to this issue and increase its traction as a policy and financing priority among state decision-makers. CMS could help guide states that are interested in moving forward by providing a model Medicaid adult dental benefit and tools for estimating the cost of adding dental benefits.
More work is needed to improve oral health literacy.
Discussants highlighted the need for increased outreach and education to improve public awareness regarding the importance of oral health. One official from a state with a robust adult dental benefit in Medicaid reported that only about one-third of adults had used the benefit, and he cited low oral health literacy and patient navigation challenges as key causes of under-utilization. While Medicaid coverage of dental services removes financial barriers to access for low-income adults, overcoming these less obvious barriers, too, is necessary to convert coverage to consumer understanding of the value of dental care and the actual receipt of care. There was also discussion of the need for more education and engagement of primary care providers regarding adult oral health, generally, but also especially in light of the risks poor oral health poses to pregnancy outcomes and the management of diabetes and other chronic conditions prevalent among low-income adults.
Addressing barriers within Medicaid could improve low-income adults’ access to oral health care.
Because adult dental benefits are a state option in Medicaid, establishing, sustaining, or improving them can be challenging.
In Medicaid expansion states, millions of previously uninsured low-income adults now have health coverage. However, adult dental services are an optional benefit in Medicaid and most states cover limited or emergency-only services.1 Even in states with extensive benefits, caps on per-enrollee dental spending may constrain access for adults with high needs. State dental officials indicated that, especially in tight budget environments, prioritizing funding for Medicaid adult dental benefits is an uphill battle even when internal support for them is strong. They said that just maintaining benefits year to year can be a struggle because adult dental coverage is often seen as “low-hanging fruit” by policymakers seeking to cut spending. They added that, after new benefits are introduced, states must simultaneously implement them and think about how to keep them. Some state dental officials said that they had been able to identify temporary revenue sources to finance dental benefits, such as an unclaimed property trust fund, but sustainability remains a challenge. Limited and unstable benefits hinder access to dental care for Medicaid adults and deter dentists from seeing Medicaid patients because of uncertainty about whether services will be covered.
Dentists in many states face Medicaid policies that may discourage participation.
The roundtable discussion affirmed that low Medicaid fees and high administrative barriers dampen dentist participation in Medicaid. Managed care organizations (MCOs) often set payment rates for dentists by discounting already low Medicaid fee-for-service (FFS) rates. Onerous provider enrollment processes and prior authorization systems also deter participation, and discussants mentioned that the ACA requirement for revalidation of providers every five years has also led to some loss of dentists from the program. Government audits are often perceived as adversarial. Other barriers were cited, too. Small dental offices lack the expertise and resources to analyze and compare managed care plans’ coverage policies and payment rates. They also find it burdensome to file applications with multiple plans to participate in their networks and to deal with plans’ different credentialing processes. Medicaid coverage that pays for extractions but limits or does not pay for services that can save patients’ teeth (e.g., root canals, crowns) frustrate dentists, as do policies that thwart continuity of care, such as loss of maternal dental benefits following pregnancy in some states. One participant indicated that dental practices that serve primarily low-income patients can find it harder to get bank loans or face higher interest rates to borrow.
- Dental benefits. Recognizing the extensive unmet need for oral health care among poor adults, some states are taking steps to expand dental benefits and dentist participation in Medicaid. Participants stated that, with millions of low-income working-age adults entering the Medicaid program, awareness of the urgent need for dental care in this population has sharpened. In recent years, a number of states have restored adult dental benefits that were previously cut, introduced an adult dental benefit, or added new benefits, such as preventive dental services. The point was made that the adult Medicaid population is not monolithic and that there is need to think about subgroups with special oral health needs, including pregnant women, individuals with disabilities, and people with diabetes. Some states with limited adult dental benefits have taken steps to provide more expansive access to services for selected groups. For example, one state with caps on covered services instituted a “benefit limit exceptions” process to permit additional services, including dentures, crowns, and endodontic and periodontic care, for pregnant women as well as adults with a serious chronic or other condition when certain criteria are met. Other states provide a more robust dental benefit package for pregnant women. It was suggested that, in states where a more meaningful adult dental benefit is not possible, even paying for toothbrushes and toothpaste in Medicaid could improve prevention and self-care among adult enrollees. One participant proposed that a 90% federal match rate, as now applies to family planning services in Medicaid, would go a long way to secure a sound dental benefit for adults.
- Dental payment rates and participation. State dental officials mentioned several tacks that states are taking to improve dentist participation in Medicaid. Increased Medicaid payment rates for dentists and/or targeted increases to sustain or boost dentist participation in rural or other underserved areas are one lever states can use; one discussant noted that even small rate increases are important because they are a legislative “foot in the door.” A couple of states have instituted incentives to dental providers to participate. Under a time-limited program in one state at the table, dentists and dental hygienists enrolled in Medicaid receive an incentive payment if they take five additional Medicaid patients (and provide two visits to each), and additional incentive payments for larger increases in their Medicaid patient panels. Along similar lines, under the Dental Transformation Initiative in California’s section 1115 waiver, the state will pilot incentive payments to Medi-Cal FFS dental providers (including safety-net clinics) based on year-on-year continuity in the provider and location of the annual dental exam received by a child.2
- Medicaid delivery system choices. State policy choices regarding how dental benefits are delivered can also impact dentist participation in Medicaid and Medicaid enrollees’ access to dental care. One state Medicaid official emphasized that when his state introduced an adult dental benefit in 2014, it decided to administer the benefit itself, using an Administrative Services Only contract rather than contracting with managed care organizations (MCOs) on a capitation basis. This approach kept the state in control of credentialing, network development, and pricing, which addressed the dental community’s apprehension about managed care and reimbursement. Many states see managed care as a better means to deliver the dental benefit and ensure access to care for Medicaid enrollees. Contracts with MCOs give states leverage to establish network adequacy standards and performance requirements and hold plans accountable, and capitation payment provides plans with flexibility and incentives to organize and pay for services in innovative ways. Discussants suggested that administrative barriers to dentist participation in Medicaid could be lowered if plans within a state had uniform credentialing and other processes.
Leadership, stakeholder engagement, and being ready matter.
Roundtable participants cited the critical role of leadership and advocacy by the Governor, legislative champions, state oral health coalitions, and the state dental association in the success of state effort to strengthen Medicaid adult dental benefits. Broad stakeholder engagement and an inclusive, deliberative planning process also emerged as important factors. Discussants identified turnover in state legislatures and term limits as a challenge to gaining policymakers’ attention and commitment and legislative traction. At the same time, there can be a sudden but fleeting opportunity to advance an initiative, so having a well-developed proposal ready to go is strategically important.
Innovative workforce and service delivery models have potential to expand access to oral health care, within and beyond Medicaid.
We have not maximized the potential of our current health care workforce to supply oral health services.
Roundtable participants observed that, while more dentists and other dental professionals are likely needed to meet increasing demand for services as insurance coverage expands, it is possible to increase the supply of care available with today’s workforce. There was wide agreement that enabling dental hygienists to work “at the top of their license” by eliminating state scope-of-practice restrictions would enlarge the supply of care, especially in areas underserved areas, where dental hygienists are more willing to work and dentists are scarce. Primary care providers can also be trained and paid to furnish basic preventive services, and new provider types such as dental therapists can expand existing oral health care capacity and access. Another point discussants raised is that states may have leverage to work with dental schools – most of which are public institutions – to bring more dentists to disadvantaged and underserved communities.
Health centers remain a cornerstone of access to dental care for low-income adults.
Discussants emphasized the crucial role of health centers as a source of dental care for both Medicaid enrollees and other low-income adults, including uninsured individuals as well as QHP enrollees, many of whom lack dental coverage and qualify for health centers’ sliding fees. Most health centers have dental clinics onsite, and the large ACA investment in health centers over a 5-year period and further extended by Congress has enabled health centers to expand the oral health services they provide and increase the number of patients they serve.
It is important that strategies to provide integrated, whole-person care incorporate oral health care.
Citing the widespread efforts to integrate behavioral and physical health care in Medicaid, discussants expressed the importance of including oral health in integrated care approaches as well. They explicitly recognized health centers as leaders in the integrated delivery of oral and primary care. Discussants also highlighted the increasing number of states that previously “carved out” dental benefits from their MCO contracts but are now carving them in, holding medical directors responsible for oral health as well. The MCO executive at the table expressed strong support for integration, but observed that oral health care is not a core competency of most MCOs, so, for the near-term, many may need to pass the risk for these services to other entities. Turning to the data needs for truly integrated care, participants identified how integrated patient health records and clinical decision-support tools can improve patient care – for example, prompting dental providers when their patients are due for a cancer screen, or generating oral health messages to physicians for their patients with diabetes. Discussants suggested that other approaches to integrated care at the provider level, such as having dentists screen for hypertension and physicians screen for oral disease, could also improve patient care.
Experts said that it will not be possible to grow our way out of the oral health crisis among low-income adults without reforming the current care delivery paradigm.
Clinical experts at the table stressed that high rates of oral disease among adults in Medicaid are unlikely to change in the years ahead without fundamental reorientation of our oral health care system. The prevailing structure of dental coverage is provider-driven, based on a more or less uniform set of services and periodicity
schedules regardless of individual risk factors, and on FFS payment. Even as states move to risk contracting, the capitation rates they set assume FFS fee levels and utilization experience. Discussants urged the need to move to evidence-based models of coverage and care that emphasize prevention, early intervention, and caries risk management, and to payment models like pay-for-performance, bundled payments, and other approaches that incentivize the provision of preventive care and reward improvement in outcomes rather than simply reimburse for utilization. While stressing that a transformed system that revolves around prevention is imperative if we are to get ahead of the epidemic of oral disease among low-income adults, roundtable participants stated that, for the foreseeable future, capacity for “rescue operations” performed by dentists must also be maintained or even expanded to deal with the current burden of disease and new demand for services as coverage expands.
New models to increase access to oral health care in underserved communities and populations show promise.
A thread running through the discussion was the need to rethink how services are delivered. The vast majority of dental visits take place in dentist offices today, but new models are bringing oral health care to people where they live, go to school, and work. The discussion highlighted the “virtual dental home” demonstration in California. In this technology-facilitated model, specially licensed dental practitioners provide preventive and simple restorative care in community settings including Head Start sites, residential facilities for people with disabilities, and long-term care facilities. These providers are equipped with portable imaging and other equipment and a web-based dental record system, which enables them to exchange patient information with a collaborating dentist. The dentist reviews the information and creates a treatment plan, and the community-based providers furnish the services they can in their setting and refer patients to dentists for more complex care. It was noted that this model involved state legislation both to expand the scope of practice for allied health personnel and to require California’s Medicaid program to pay for teledentistry services. Another model, known as “hub-and-spoke,” connects dentists in their main practice locations (hubs) to settings in nearby communities (spokes) where the dentist or a dental hygienist provides dental care on scheduled days.
Data needs
Quality measures for adult oral health are needed.
Discussants suggested that prioritizing adult oral health is made more challenging by the absence of commonly accepted adult dental quality measures. Such measures would help convey the scope and scale of the problem, identify key gaps (e.g., by state or poverty level), and provide benchmarks against which performance and improvement can be assessed – data that are needed to guide Medicaid and other health policy. One policy expert noted that the American Dental Association’s Dental Quality Alliance is developing and testing several adult as well as pediatric measures, but added that only pediatric measures had been at all embraced by states, consistent with the CMS Oral Health Initiative’s tight focus on low-income children’s oral health and the much more limited coverage of adults and adult dental services in Medicaid.
Monitoring the impact of adding adult dental coverage in Medicaid may require a phased approach.
One state official emphasized that the impacts of a newly established adult dental benefit emerge over time as implementation is solidified, changes in access to care and utilization occur, and outcomes potentially improve,and that state monitoring strategies should be structured to take this reality into account. This discussant’s state adopted a multi-year monitoring plan when it launched an adult dental benefit in Medicaid. Reflecting expectations about the early impacts of the benefit, state monitoring in Year 1 focused modestly on increases in dentist participation in Medicaid, and monitoring in Year 2 focused on reductions in ED visits for non-emergency dental care. Over time, the state will focus its monitoring on measures tied more closely to long-term goals for improved oral health outcomes.
Determining the return on investment (ROI) from covering dental benefits for adults in Medicaid is challenging.
While being able to demonstrate ROI from adult dental coverage, or provide a cost-benefit analysis, could enhance efforts to stabilize and expand these benefits, the discussion highlighted several issues that present challenges. Fundamentally, costs tend to be easier to quantify than benefits. In addition, benefits often taken longer to materialize. Oral health outcomes, in particular, are lagging indicators and measurable gains may not occur in the budget or election or term-limit timeframe relevant to policymakers. Offsets or savings within Medicaid, for example, from reduced ED visits or hospital uncompensated care, can be difficult to attribute directly to expanded adult dental coverage and to quantify. Further, as new low-income adults continually cycle into Medicaid, their oral disease burden can conceal or wash out improvements in utilization, spending, and outcomes in the underlying Medicaid population. Identifying and quantifying returns to adult dental benefits beyond the Medicaid program (e.g., improved diabetes control and lower health spending, ability to work, social integration) is even more difficult analytically.
Technical assistance could help states move forward on Medicaid adult dental coverage.
Participants agreed that the availability of tools to estimate the cost of adding adult dental benefits would help states, advocates, and others begin to formulate proposals and model different alternatives. Other technical assistance from CMS and mechanisms to facilitate sharing of state experience and best practices, such as learning collaboratives, could also provide support to states considering dental benefit expansions and help guide their planning and implementation. In addition, discussants said, demonstration funding for innovative oral health care models and their evaluation could help identify promising delivery and payment system reforms and advance their diffusion.
Conclusion
The roundtable discussion on improving access to oral health care for low-income adults, drawing on the wide-ranging perspectives and expertise of the participants, yielded important themes and observations. Overarching all of them was a collective emphasis on the importance of prioritizing access to oral health care as part of the health care policy agenda. Medicaid’s growing role in covering low-income adults, combined with the large infusion of federal dollars for Medicaid expansion and health center growth, provides an opportunity to address the high rates of oral disease and unmet dental need among low-income adults by expanding adult access to dental care in Medicaid. The ramifications of poor oral health among low-income adults, which extend beyond health to employment, drug use and incarceration, social isolation, and wide-ranging disparities, enlarge the context for considering action on this issue. As a
growing number of states are demonstrating with their own initiatives, states have important levers to expand both adult coverage and the availability of dental providers in Medicaid; health plans, health centers, and provider practices are a locus of innovation as well. Federal leadership focused on measuring and improving access to dental care among adults in Medicaid could accelerate progress, and broader efforts to address workforce shortages, oral health literacy, and other factors will also be important. But ultimately, leading experts agree, ending the epidemic of oral disease among poor populations will depend on greater integration of oral and primary care and a transformed oral health system defined by an emphasis on prevention, patient risk assessment and evidence-based care, and community-based models of service delivery.
Endnotes
- Medicaid Adult Dental Benefits: An Overview, Center for Health Care Strategies, July 2016. Available at: http://www.chcs.org/resource/medicaid-adult-dental-benefits-overview/. ↩︎
- Dental Transformation Initiative (DTI), Medi-Cal 2020 Waiver, California Department of Health Care Services. Available at: http://www.dhcs.ca.gov/provgovpart/Pages/DTI.aspx. ↩︎