Building on the Evidence Base: Studies on the Effects of Medicaid Expansion, February 2020 to March 2021
Introduction
The new financial incentive for expansion in the American Rescue Plan Act (ARPA) of 2021 has reignited debate on Medicaid expansion under the Affordable Care Act (ACA) in the twelve states that have not adopted the expansion. Further, the coronavirus pandemic has adversely affected health outcomes (as evidenced by suppressed health care utilization and increased excess mortality) and economic wellbeing. While Medicaid has served as a coverage safety net during the pandemic and resulting economic crisis, coverage options for many low-income adults are limited in non-expansion states.
This literature review provides context for these expansion debates by summarizing evidence from nearly 200 studies published between February 2020 and March 2021 on the impact of state Medicaid expansions under the ACA. This review builds on an earlier report (examining over 400 studies) concluding that expansion is linked to gains in coverage; improvements in access, financial security, and some measures of health status/outcomes; and economic benefits for states and providers (see Appendix A for figures summarizing study findings from the combined 601 studies from both reviews).
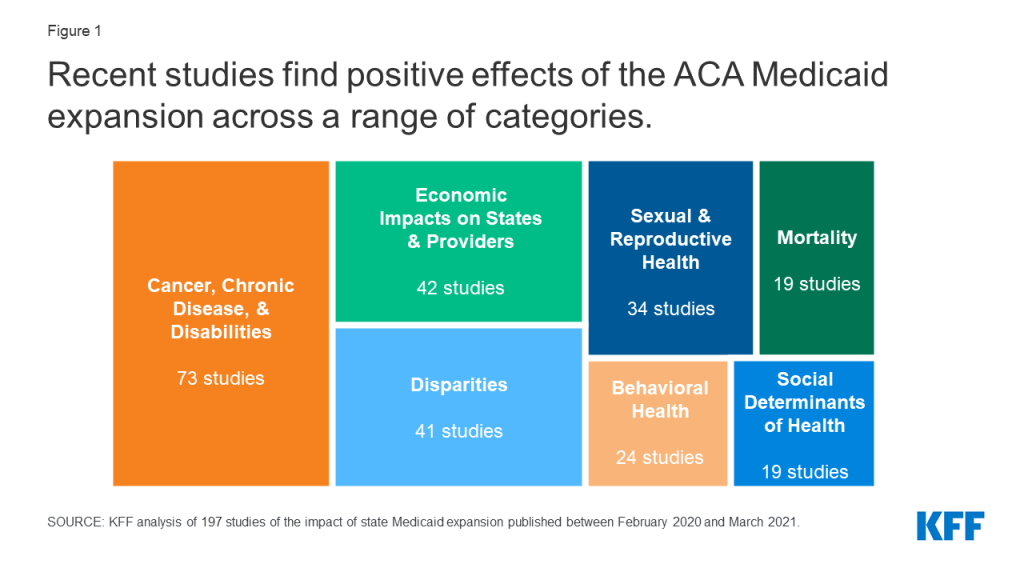
This recent body of research finds positive effects of expansion across a range of increasingly complex and specific categories. Accordingly, this report highlights study findings across multiple key themes of interest:
- Mortality, overall and associated with specific conditions.
- Cancer, chronic disease, and disabilities, including conditions considered risk factors for COVID-19.
- Sexual and reproductive health, including maternal and infant health, postpartum insurance coverage, access to contraception, and HIV/AIDS screening and outcomes.
- Behavioral health, including substance use disorder and mental health.
- Economic impacts on states and providers, including effects on state economies and on hospital financial performance.
- Disparities by race/ethnicity, socioeconomic status, and other categories.
- Social determinants of health including access for rural areas, economic and educational outcomes, and outcomes for justice-involved and homeless individuals.
Studies included in this review may include multiple findings across multiple categories. Additionally, this report does not attempt to summarize all findings across all studies but instead aims to highlight conclusions across themes. A small number of studies reviewed and included in the appendices to this review did not have findings that fall into the thematic categories and thus are not cited in the text of this report.
Methods
This literature review summarizes findings from 197 studies of the impact of state Medicaid expansions under the ACA published between February 2020 and March 2021. This report builds on an earlier literature review that includes studies on the impact of expansion published between January 2014 (when the coverage provisions of the ACA went into effect) and January 2020. While the figures in this report (Appendix A) include the full body of 601 studies published between January 2014 and March 2021, the text of this report focuses on the 197 recent studies. Because this report highlights key themes across recent studies (versus attempts to summarize all findings in all studies), some recent studies included in the figures, bibliography, and appendices may not be cited in the text of this report.
This literature review includes studies, analyses, and reports published by government, research, and policy organizations using data from 2014 or later and only includes studies that examine impacts of the Medicaid expansion in expansion states. This review excludes studies on impacts of ACA coverage expansions generally (not specific to Medicaid expansion alone), studies investigating potential effects of expansion in states that have not (or had not, at the time of the study) expanded Medicaid, and reports from advocacy organizations and media sources.
To collect relevant studies, we conducted keyword searches of PubMed and other academic health/social policy search engines as well as websites of government, research, and policy organizations that publish health policy-related research. We also used a snowballing technique of pulling additional studies from reference lists in previously pulled papers. While we tried to be as comprehensive as possible in our inclusion of studies and findings that meet our criteria, it is possible that we missed some relevant studies or findings. For each study, we read the final paper/report and summarized the population studied, data and methods used, and findings. In instances of conflicting findings within a study, or if a reviewer had questions about specific findings, multiple reviewers read and classified the study to characterize its findings. In the report text, findings are broken out by key areas of interest, and studies may be cited in multiple of these categories or in multiple places within a category.
Report
Themes in Recent Research
Several key themes emerge from recent literature investigating the effects of Medicaid expansion (Figure 1). In contrast to earlier research, which largely focused on the impacts of Medicaid expansion for the general population or for low-income populations, recent research has increasingly focused on outcomes for specific populations, such as people with cancer or behavioral health needs. Recent research has also focused on specific outcomes such as mortality and social determinants of health. Although overall findings across these themes generally show positive effects of Medicaid expansion, a smaller number of studies find no impact of expansion on specific outcomes for specific populations; however, very few studies suggest any negative effects.
Many studies published between February 2020 and March 2021 and cited throughout this report have findings across multiple of these themes and are thus cited in multiple sections. Additionally, many studies on expansion published prior to February 2020 also have findings related to these themes but are not cited in this report; however, these can be found cited in an earlier literature review and are also included in the Bibliography and Appendices to this report.
Mortality
A growing body of research finds that Medicaid expansion has improved overall mortality rates as well as mortality rates associated with some specific health conditions. These findings are consistent with earlier research identifying that expansion contributed to declines in overall and some specific mortality rates, but had no effect on mortality rates associated with other specific conditions.
- Overall mortality. A 2020 national study found that expansion was associated with a significant 3.6% decrease in all-cause mortality, the majority of which was accounted for by a significant 1.93% decrease in health care amenable mortality. Another study found that expansion was associated with reductions in health care amenable mortality and in mortality not due to drug overdose.1 ,2
- Mortality associated with specific health conditions. A larger number of studies consider the impact of expansion on mortality rates for particular populations or associated with certain health conditions:
- Studies find that expansion was associated with significant declines in mortality related to certain specific conditions, in some instances limited to certain subgroups. These findings include decreased mortality associated with different types of cancer, cardiovascular disease, and liver disease. Studies also find decreased maternal mortality, and one study found a decrease in infant mortality among Hispanics only.3 ,4 ,5 ,6 ,7 ,8 ,9 ,10
- However, other studies suggest no effect of expansion on mortality among safety-net hospital patients, individuals with glottic cancer, individuals with glioblastoma, patients undergoing hemodialysis, and overall infant mortality. One study found no significant difference between COVID-19 mortality rates in expansion versus non-expansion states, despite lower incidence rates in expansion states. One study concluded that available data was insufficient to adequately identify the impact of expansion on opioid mortality.11 ,12 ,13 ,14 ,15 ,16 ,17 ,18 ,19
Cancer, Chronic Disease, and Disabilities
Recent research finds largely positive impacts of expansion on coverage and access to care among populations with cancer, chronic disease, and/or disabilities. However, findings on utilization of care and health outcomes are more mixed, with some studies suggesting improvements and others finding no effect of expansion. These studies build on prior research indicating generally positive effects of expansion for populations with cancer and other health conditions. Recent research also provides additional evidence on expansion’s impacts across a range of chronic conditions considered by the CDC to put people at higher risk of severe illness and death from COVID-19 (such as diabetes, obesity, and lung and heart conditions).
- Cancer. A large body of recent research considers the impact of Medicaid expansion on coverage, treatment, and outcomes of people with cancer, as well as access to cancer screenings.
- Coverage of people with cancer. Studies overwhelmingly find that Medicaid expansion has increased insurance coverage rates among cancer patients and survivors. Research also finds changes in payer mix of care for patients with cancer, with declines in the proportion of uninsured patients and increases in the proportion of Medicaid-insured patients.20 ,21 ,22 ,23 ,24 ,25 ,26 ,27 ,28 ,29 ,30 ,31 ,32 ,33 ,34 ,35 ,36 ,37 ,38 ,39 ,40 ,41 ,42 ,43
- Cancer diagnosis, treatment, and outcomes. Most studies find an association between expansion and increases in early-stage diagnosis rates among cancer patients, suggesting that expansion has facilitated earlier utilization of care for these patients. Findings on utilization of cancer treatment services and on access to timely treatment are mixed, though more studies find improvements as compared to studies that find no effect of expansion. Of studies that consider cancer mortality, three suggest improvements for patients with certain types of cancer, while three suggest no effect for patients with other types of cancer.44 ,45 ,46 ,47 ,48 ,49 ,50 ,51 ,52 ,53 ,54 ,55 ,56 ,57 ,58 ,59 ,60 ,61 ,62 ,63 ,64 ,65 ,66 ,67 ,68 ,69 ,70 ,71 ,72 ,73 ,74 ,75
- Cancer screening and prevention. Several studies find that expansion increased receipt of cancer screenings such as mammograms, though a similar number of studies find no effect of expansion on screening rates for certain cancers. Two studies identified an association between expansion and increased rates of human papillomavirus (HPV) vaccines (overall and among teenagers specifically), while a third found no effect of expansion on HPV vaccination rates among female community health center patients.76 ,77 ,78 ,79 ,80 ,81 ,82 ,83 ,84
- Diabetes. Studies find that expansion increased insurance coverage rates among adults and teenagers with diabetes. Although research indicates that expansion increased affordability of health care for populations with diabetes, findings on utilization of preventive care and treatment are more mixed (between studies finding improvements and studies finding no effect). Two studies identified improvements in diabetes biomarkers among community health center patients following expansion. Two studies that considered women of reproductive age found that expansion did not affect the prevalence of diabetes prior to or during pregnancy.85 ,86 ,87 ,88 ,89 ,90 ,91 ,92 ,93 ,94 ,95 ,96
- Other chronic disease. In addition to cancer and diabetes, research also considers a range of other chronic conditions including cardiovascular and pulmonary diseases, obesity, and liver disease. Studies find that among those with chronic disease, expansion contributed to increased insurance coverage and improvements in payer mix, improved access to care, and better health outcomes including disease management and mortality. Findings on effects on treatment utilization and quality of care were mixed (between studies finding improvements and studies finding no effect). Finally, studies generally suggest that expansion increased screening for chronic conditions but did not reduce the prevalence of these conditions except for smoking.97 ,98 ,99 ,100 ,101 ,102 ,103 ,104 ,105 ,106 ,107 ,108 ,109 ,110 ,111 ,112 ,113 ,114 ,115 ,116 ,117 ,118 ,119 ,120 ,121 ,122 ,123
- People with disabilities. A small number of recent studies consider the impacts of expansion for people with disabilities. One study found increased coverage options for people with disabilities in expansion states, while other studies suggested no effect of expansion on utilization of care or employment among this population. One study found that expansion improved mental health outcomes for caregivers of people with disabilities.124 ,125 ,126 ,127 ,128
Sexual and Reproductive Health
Recent research finds that expansion has contributed to improvements in a number of outcomes related to sexual and reproductive health. This body of research includes findings related to women’s health and HIV/AIDS outcomes, both areas of health care that have faced increased challenges during the coronavirus pandemic. Building on prior research finding positive impacts among people of reproductive age, recent research indicates that expansion has improved measures including coverage rates before, during, and after pregnancy; maternal mortality and infant health outcomes; utilization of the most effective contraceptive methods; and screening for HIV/AIDS.
- Maternal and infant health outcomes. Studies find that expansion significantly increased access to and utilization of health care for pregnant women and mothers. Two studies found significant declines in maternal mortality, in contrast to one study which found no impact of expansion on certain health outcomes during pregnancy. Studies generally suggest an association between expansion and improvements in birth outcomes such as low birthweight, but find no impact on infant mortality (except for one study which found a reduction in Hispanic infant mortality only).129 ,130 ,131 ,132 ,133 ,134 ,135 ,136 ,137 ,138 ,139 ,140
- Postpartum insurance coverage. Although the American Rescue Plan Act of 2021 created a new option to expand postpartum coverage to 12 months via a State Plan Amendment, current federal statute requires that pregnancy-related Medicaid coverage continue through just 60 days. Research indicates that ACA Medicaid expansion has decreased coverage loss after this 60-day period ends: all recent studies that consider rates of insurance coverage after pregnancy find that expansion significantly increased postpartum coverage. Studies also suggest an association between expansion and increased coverage prior to and during pregnancy.141 ,142 ,143 ,144 ,145 ,146 ,147 ,148 ,149
- Access to contraception. Most studies find that expansion increased utilization of the most effective contraception methods (long-acting reversible contraception, which includes IUDs and implants); however, studies generally find no effect on overall contraception use. One study found an association between expansion and improved payer mix for contraceptive visits at safety net clinics, with a decline in the proportion of uninsured patients and an increase in the proportion of publicly-insured patients.150 ,151 ,152 ,153 ,154 ,155
- HIV/AIDS screening and outcomes. Studies suggest that expansion increased overall rates of HIV screening, including one study that found that increases in HIV test and diagnosis rates occurred despite no change in actual HIV incidence. Research also indicates higher insurance coverage rates among people with or at risk of HIV, increased utilization of Pre-Exposure Prophylaxis (PrEP) to treat HIV, and improved quality of care for patients with HIV.156 ,157 ,158 ,159 ,160 ,161 ,162 ,163 ,164 ,165 ,166 ,167
Behavioral Health
A growing body of research finds that expansion is associated with improvements in access to care and outcomes related to substance use disorder (SUD) as well as other mental health care. These findings are consistent with prior research indicating positive effects of expansion on behavioral health care access and outcomes. Recent research on SUD largely focuses on opioid use disorder (OUD) specifically, which is more prevalent among Medicaid enrollees as compared to the general population. Given the impacts of the coronavirus pandemic on mental health and substance use, Medicaid expansion coverage is likely to continue to serve as a significant source of coverage for behavioral health care.
- Access to care and outcomes for SUD. Studies find that Medicaid expansion was associated with increased insurance coverage among adults with SUD and improved payer mix of SUD-related visits (declines in uninsured patients and/or increases in Medicaid-covered patients). Studies also find that expansion increased the receipt of medication assisted treatment (MAT) prescriptions for the treatment of OUD, and that following expansion opioid treatment facilities were more likely to offer MAT and comprehensive mental health services. In contrast, a small number of studies found no effect of expansion on utilization of certain health care services for SUD. One study found no effect of expansion on drug-overdose deaths, while a second concluded that available data was insufficient to adequately identify the impact of expansion on drug-related mortality.168 ,169 ,170 ,171 ,172 ,173 ,174 ,175 ,176 ,177 ,178 ,179 ,180 ,181
- Mental health care access and outcomes. Studies find that expansion increased access to care for adults with mental health conditions such as depression, including by increasing the likelihood that mental health care providers accepted Medicaid. Findings on utilization of mental health care are more mixed, with some studies suggesting increased utilization of services such as mental health care via telehealth, and others finding no effect of expansion on other mental health services. Findings on mental health outcomes are also mixed: one study found that expansion was associated with improvements in self-reported mental health among low-income adults, while two other studies found no impact on similar measures among near-elderly adults and among women of reproductive age.182 ,183 ,184 ,185 ,186 ,187 ,188 ,189 ,190 ,191 ,192 ,193
Economic Impacts on States and Providers
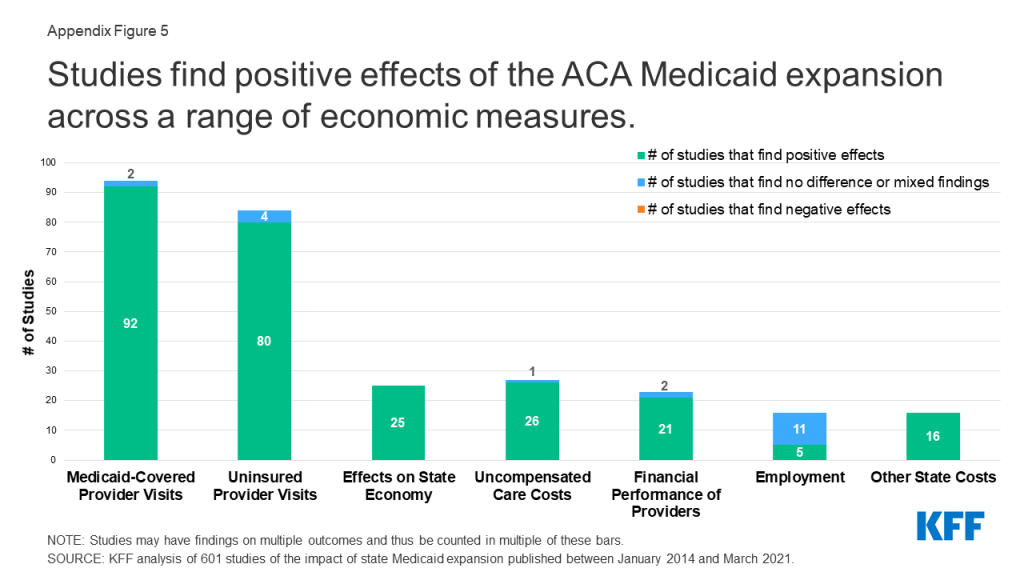
Building on prior research, recent studies identify positive financial impacts of Medicaid expansion for states, hospitals, and other providers. These studies join a body of prior research finding overwhelmingly positive effects of expansion on economic outcomes (see Appendix A, Figure 5). These economic findings are particularly relevant given fiscal stress experienced by both states and Medicaid providers during the coronavirus pandemic.
- State budgets and economies. All recent studies that consider the financial impacts of expansion for states find positive effects. Studies find that expansion states experienced increased federal Medicaid spending. One study found that through 2018, Medicaid expansion led to increased federal spending in expansion states but very small (<1%), insignificant increases in spending from state sources (including in 2017 and 2018 when states began paying 5% and 6% of expansion costs respectively, a rate that was subsequently phased to 10% in 2020 and beyond). In addition, Medicaid expansion did not crowd out other areas of state spending and states that did not expand passed up $43 billion in federal funds in 2018. Research also finds that expansion resulted in increased revenue as well as net state savings by offsetting state costs in other areas, such as state spending on substance use disorder (SUD) treatment and on the traditional Medicaid program. One study found that the mortality reductions associated with expansion resulted in between $20.97 and $101.8 billion in annual welfare gains, implying that mortality-related savings alone may offset the entire net cost of expansion.194 ,195 ,196 ,197 ,198
- Payer mix. Studies overwhelmingly find that Medicaid expansion has resulted in payer mix improvements (declines in uninsured patients and/or increases in Medicaid-covered patients). Findings include payer mix improvements for hospitalizations, emergency department visits, and visits to community health centers and other safety-net clinics. Studies identify payer mix improvements among patients hospitalized for a range of specific conditions including traumatic injuries, surgeries, and treatment for substance use disorder. In line with payer mix improvements, studies also find decreased uncompensated care costs (UCC) overall and for specific types of hospitals, including those in rural areas.199 ,200 ,201 ,202 ,203 ,204 ,205 ,206 ,207 ,208 ,209 ,210 ,211 ,212 ,213 ,214 ,215 ,216 ,217 ,218 ,219 ,220 ,221 ,222 ,223 ,224 ,225 ,226 ,227 ,228 ,229 ,230
- Financial performance of hospitals and other providers. Research finds that expansion contributed to increased hospital revenue overall and from specific services. Although studies find that expansion has improved provider operating margins and profitability, these findings vary by hospital type. For example, one study found that despite declines in UCC and increases in Medicaid revenue across all hospital types, only hospitals in non-metropolitan areas and small hospitals experienced improved profit margins; another study similarly found gains in overall revenue only for rural and small hospitals. A few studies suggest that improvements in payer mix and UCC at hospitals may have been partially offset by increases in unreimbursed Medicaid care and declines in commercial revenue. One recent study found that expansion reduced the number of annual hospital closures.231 ,232 ,233 ,234 ,235 ,236 ,237 ,238 ,239 ,240 ,241
Disparities
A growing body of research considers the impact of Medicaid expansion on disparities in different outcomes by race/ethnicity, socioeconomic status, and other categories. These studies build on an earlier literature review finding that expansion has helped to narrow racial disparities in coverage and certain health outcomes, with more limited evidence suggesting reduced racial disparities in access to and use of care. Some studies on racial/ethnic disparities cited here are also included in this earlier review, which included studies published through July 2020.
- Disparities by race/ethnicity. Findings on expansion’s impact on racial disparities in health coverage, access, and outcomes are mixed and generally mirror findings from a previous literature review, with evidence of decreased racial disparities for some populations in measures including coverage rates, affordability of care, utilization of surgery and other services, and health outcomes including maternal and infant mortality. However, similar numbers of studies identify no effect of expansion on racial disparities in these and other measures. A very small number of studies find evidence of increased racial disparities (in coverage rates for specific populations and in breast cancer mortality). Across outcomes, most research focuses on disparities for Black and Hispanic individuals, with limited findings on impacts for other groups of color.242 ,243 ,244 ,245 ,246 ,247 ,248 ,249 ,250 ,251 ,252 ,253 ,254 ,255 ,256 ,257 ,258 ,259 ,260 ,261 ,262 ,263 ,264 ,265 ,266 ,267 ,268 ,269 ,270 ,271 ,272 ,273 ,274 ,275 ,276 ,277 ,278 ,279 ,280
- Disparities by socioeconomic status (income and/or education). In contrast to research on racial disparities, recent studies that consider socioeconomic disparities all find improvements. Studies find that expansion has reduced disparities in coverage by income and/or education status, including for populations with certain cancer diagnoses. A smaller number of studies also find decreased socioeconomic disparities in utilization of care, certain health outcomes such as maternal mortality, and individual financial stability.281 ,282 ,283 ,284 ,285 ,286 ,287 ,288 ,289 ,290 ,291
- Disparities by other categories. A few recent studies identify an association between expansion and reduced coverage disparities by age, sex, and marital status, but no effect on coverage disparities by work status and obesity. One study found that expansion reduced age disparities in individual financial stability. Another study found no effect of expansion on disparities by sex in receipt of HIV tests.292 ,293 ,294 ,295 ,296 ,297 ,298
Social Determinants of Health
Recent research indicates largely positive impacts of expansion associated with different social determinants of health. These recent studies are consistent with prior research on expansion’s effect on social determinants of health and also contribute new evidence on effects for certain measures. Social determinants of health are the conditions in which people are born, grow, live, work, and age. Improvements in these measures associated with expansion could help to mitigate increased hardship due to the coronavirus pandemic.
- Access to care in rural areas. Studies find that expansion was associated with greater improvements in access to care in rural areas, including increased HIV diagnosis rates and access to mental health care. In contrast, one study found that utilization of tobacco cessation treatment remained limited in rural Appalachia even after Medicaid expansion in Kentucky. Research also suggests that rural hospitals experienced particularly substantial improvements in financial performance following expansion.299 ,300 ,301 ,302 ,303 ,304 ,305 ,306 ,307
- Impacts on economic stability, employment, and educational outcomes. Studies find that expansion decreased catastrophic health expenditures (health care spending as a percentage of family income). One study found that expansion was associated with greater increases in income among low-income individuals and contributed to decreased levels of income inequality. One study found an association between expansion and decreased odds of job loss, though two other studies found no effect of expansion on employment among people with disabilities. Finally, a national study found significant reductions in high school dropout rates in the first year of expansion implementation, which would translate to an 11.2% reduction in drop-out rates in non-expansion states if they adopted the expansion.308 ,309 ,310 ,311 ,312 ,313 ,314
- Outcomes for justice-involved and individuals experiencing homelessness. One study found that although pregnant women referred by criminal justice agencies to opioid use disorder (OUD) treatment facilities received medication as treatment at lower rates than women referred by other sources, expansion mitigated this effect by increasing receipt of medication for these women. Another study found that expansion resulted in decreased rates of recidivism in some geographic areas. A study in Arkansas found a spike in utilization of acute care among adults experiencing homelessness who gained coverage through expansion, suggesting a pent-up demand that stabilized in the years following expansion implementation.315 ,316 ,317
Looking Ahead
This literature review builds on a prior report and summarizes new evidence on more specific outcomes for certain populations. The full body of Medicaid expansion research includes over 600 studies (summarized in Appendix A) and indicates overall positive effects across a range of outcomes for patients, providers, and states. These findings suggest that Medicaid expansion could help mitigate adverse impacts of the coronavirus pandemic at the patient, provider, and state level; although research to date on Medicaid expansion and COVID-19 remains limited, future studies will likely further consider these impacts. Additionally, continued research cited in this report demonstrating positive economic impacts may help inform states still debating whether to adopt the expansion, particularly given the new ARPA financial incentive that would more than offset state expansion costs for two years (after which states would continue to bear 10% of the cost). Future policy proposals at the state and federal level could further affect Medicaid expansion coverage and options for people in the coverage gap.
The authors thank Diana Park for her assistance reviewing studies for inclusion and compiling supplemental materials.
Appendices: Appendix A
Appendix A: Summary Figures, January 2014 – March 2021
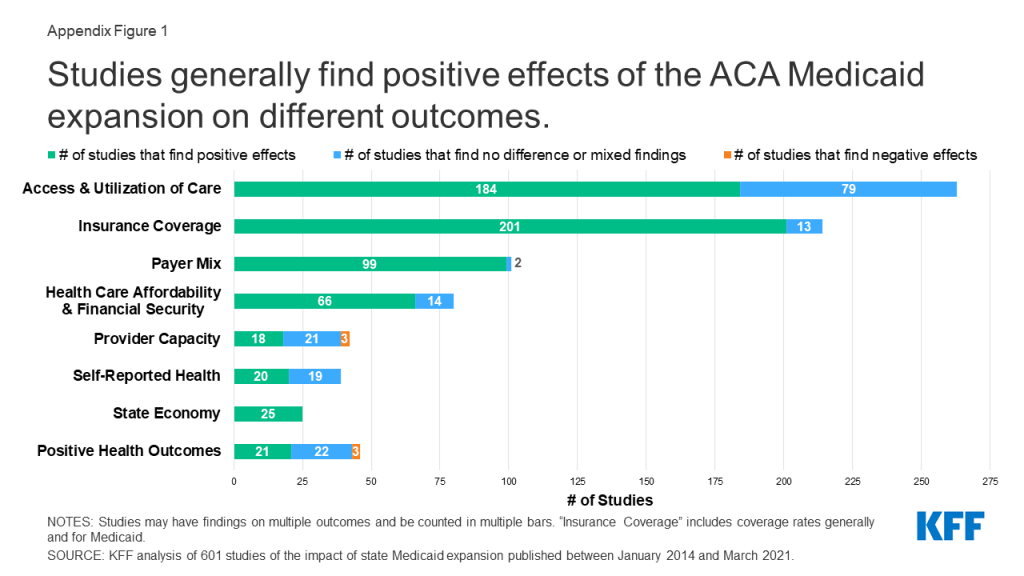
The recent studies included in this literature review build on existing research indicating that expansion is linked to gains in coverage; improvements in access, financial security, some measures of health status/outcomes; and economic benefits for states and providers (Appendix Figure 1). This appendix contains updated figures summarizing research on the effects of expansion originally published in an earlier literature review. These figures reflect all 601 included studies on the effects of ACA Medicaid expansion published between January 2014 and March 2021.
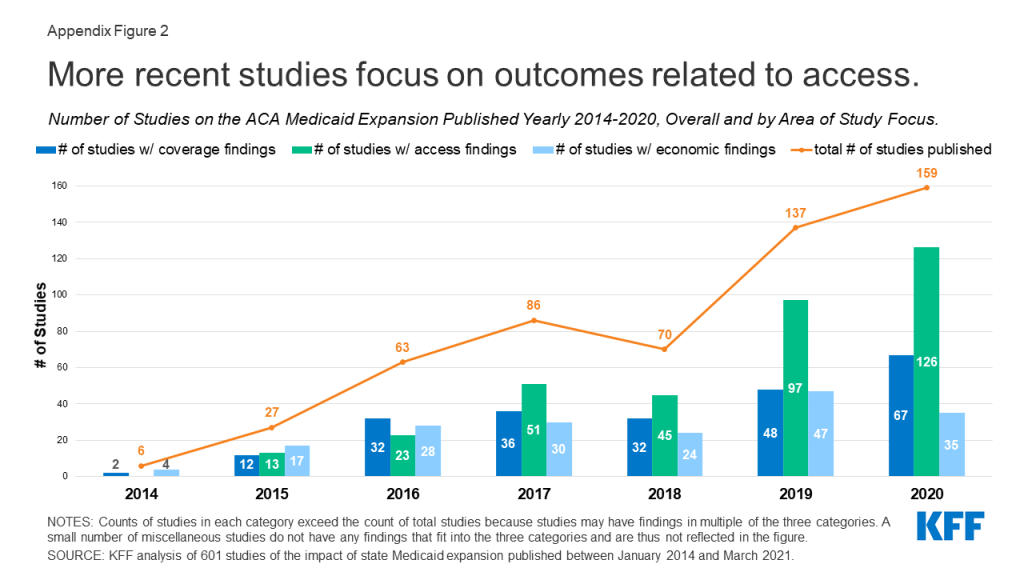
Study focus over time (Appendix Figure 2). While most early studies focused on expansion’s impact on coverage and economic measures, over time studies have increasingly focused on measures related to access to care.
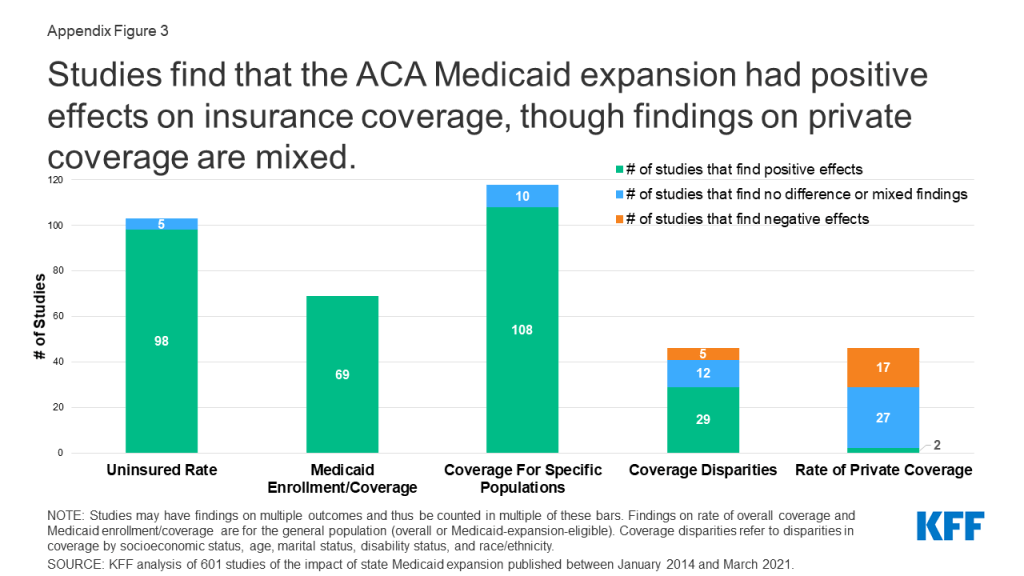
Coverage (Appendix Figure 3). The full body of research finds positive effects of Medicaid expansion on a range of outcomes related to insurance coverage, including Medicaid coverage gains and reductions in uninsured rates overall and for specific populations. Research suggests limited effects on private coverage rates. Studies also find that expansion has narrowed racial disparities in health coverage for some populations.
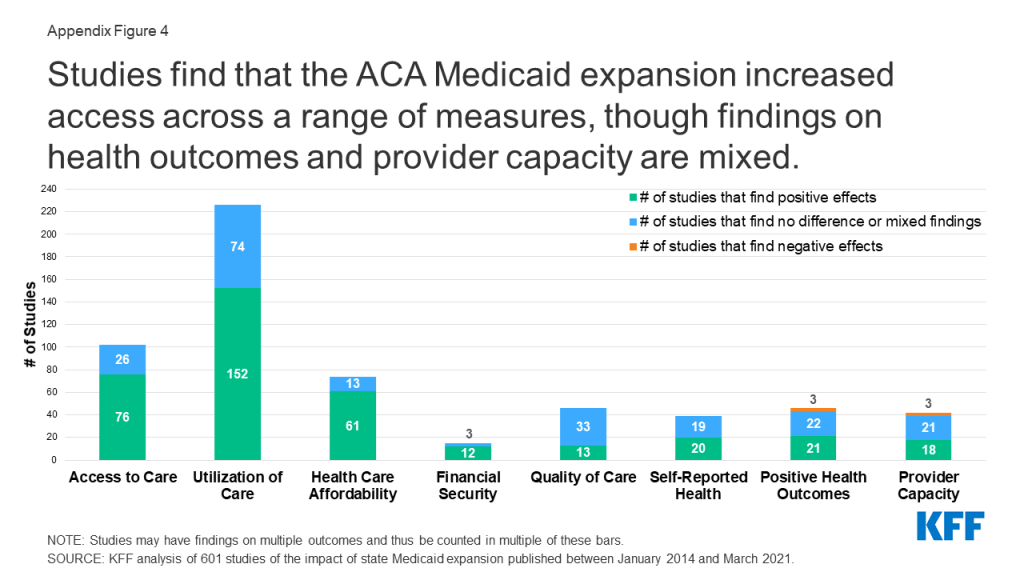
Access (Appendix Figure 4). The full body of research finds positive effects of Medicaid expansion on a range of outcomes related to access. In addition to increased access to and utilization of care, studies find that expansion has improved metrics related to quality of care, self-reported health, and health outcomes; provider capacity; and affordability and financial security.
Economic effects (Appendix Figure 5). Studies find positive effects of Medicaid expansion on a range of economic measures. Economic effects of expansion include improvements in payer mix and other impacts on hospitals and other providers and positive effects on state budgets and economies. Studies also consider Medicaid spending per enrollee, marketplace effects, and employment and labor market effects.
Appendices: Appendix B
Appendix B: Study Citations by Category of Findings and Geographic Scope, January 2014 – March 2021
DOWNLOAD APPENDIX B (.pdf)Note: This file is best viewed when downloaded and opened in Adobe Acrobat.
Bibliography
Bibliography, January 2014 – March 2021
DOWNLOAD BIBLIOGRAPHY (.pdf)Note: This file is best viewed when downloaded and opened in Adobe Acrobat.
Endnotes
- Mark Borgschulte and Jacob VoglerbaI, “Did the ACA Medicaid Expansion Save Lives?,” Journal of Health Economics 72 (July 2020), https://doi.org/10.1016/j.jhealeco.2020.102333 ↩︎
- Brandon W. Yan, Frank A. Sloan, W. John Boscardin, Felicia Guo, and R. Adams Dudley, “The Opioid Epidemic Blunted the Mortality Benefit of Medicaid Expansion,” Medical Care Research and Review Epub ahead of print (May 2020), https://journals.sagepub.com/doi/10.1177/1077558720919620 ↩︎
- Ying Liu, Graham A. Colditz, Benjamin D. Kozower, “Association of Medicaid Expansion Under the Patient Protection and Affordable Care Act With Non-Small Cell Lung Cancer Survival,” JAMA Oncology 6 no. 8 (August 2020): 1145-1308, https://jamanetwork.com/journals/jamaoncology/issue/6/8 ↩︎
- David Barrington et. al., “Where You Live Matters: A National Cancer Database Study of Medicaid Expansion and Endometrial Cancer Outcomes,” Gynecologic Oncology 158 no. 2 (August 2020): 407-414, https://doi.org/10.1016/j.ygyno.2020.05.018 ↩︎
- Miranda B. Lam, Jessica Phelan, John Orav, Ashish K. Jha, and Nancy L. Keating, “Medicaid Expansion and Mortality Among Patients With Breast, Lung, and Colorectal Cancer,” Jama Network Open 3 no. 11 (November 2020), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2772535 ↩︎
- Justin T. Moyers, Amie Patel, Wendy Shih, and Gayathri Nagaraj, “Association of Sociodemographic Factors With Immunotherapy Receipt for Metastatic Melanoma in the US,” JAMA Network Open 3 no. 9 (September 2020), https://doi.org/10.1001/jamanetworkopen.2020.15656 ↩︎
- Sadiya S. Khan, Donald M. Lloyd Jones, Mercedes Carnethon, Lindsay R. Pool, “Medicaid Expansion and State-Level Differences in Premature Cardiovascular Mortality by Subtype, 2010–2017,” Hypertension 76 (September 2020): 37-38, https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.120.15968 ↩︎
- Smriti Rajita Kumar, Sameed Ahmed M. Khatana, and David Goldberg, “Impact of Medicaid Expansion on Liver-Related Mortality,” Clinical Gastroenterology and Hepatology Epub ahead of print (December 2020), https://www.cghjournal.org/article/S1542-3565(20)31632-3/fulltext ↩︎
- Erica Eliason, “Adoption of Medicaid Expansion Is Associated with Lower Maternal Mortality,” Women’s Health Issues 30, no. 3 (May-June 2020): 147-152, https://doi.org/10.1016/j.whi.2020.01.005 ↩︎
- Alexandra Wiggins, Ibraheem M. Karaye, Jennifer A. Horney, “Medicaid Expansion and Infant Mortality, Revisited: A Difference-In-Differences Analysis,” Health Services Research 55, no. 3 (March 2020): 393-398, https://doi.org/10.1111/1475-6773.13286 ↩︎
- Paula Chatterjee, Mingyu Qi, Rachel M Werner, “Association of Medicaid Expansion With Quality in Safety-Net Hospitals,” Jama Internal Medicine Epub ahead of print (February 2021), https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2775956 ↩︎
- Bharat Akhanda Panuganti, Emelia Stuart, Philip Weissbrod, “Changes In Treatment Trends in the Early Glottic Cancer Population after the Affordable Care Act,” Journal of the Sciences and Specialties of the Head and Neck 43 no. 1 (September 2020): 137-144, https://onlinelibrary.wiley.com/doi/10.1002/hed.26463 ↩︎
- Nuriel Moghavem et al., “Impact of the Patient Protection and Affordable Care Act on 1-year Survival in Glioblastoma Patients,” Neuro-Oncology Advances 2 no. 1 (January-December 2020): 1-10, https://doi.org/10.1093/noajnl/vdaa080 ↩︎
- Scott R. Levin et al., “Association of Medicaid Expansion with Tunneled Dialysis Catheter Use at the Time of First Arteriovenous Access Creation,” Annals of Vascular Surgery Epub ahead of print (January 2021), https://www.annalsofvascularsurgery.com/article/S0890-5096(21)00082-0/fulltext ↩︎
- Amanda Cooke and Amanda Stype, “Medicaid Expansion and Infant Mortality: The (Questionable) Impact of the Affordable Care Act,” Journal of Epidemiology and Community Health 75 no. 1 (January 2021): 10-15, https://jech.bmj.com/content/75/1/10 ↩︎
- S. Marie Harvey, Lisa P. Oakley, Susannah E. Gibbs, Shyama Mahakalanda, Jeff Luck, and Jangho Yoon, “Impact of Medicaid Expansion in Oregon on Access to Prenatal Care,” Preventative Medicine 143 (February 2021), https://www.sciencedirect.com/science/article/pii/S0091743520303911?via%3Dihub ↩︎
- Jean Guglielminotti, Ruth Landau, and Guohua Li, “The 2014 New York States Medicaid Expansion and Severe Maternal Morbidity,” Anesthesia and Analgesia 10 (January 2021), https://journals.lww.com/anesthesia-analgesia/Abstract/9900/The_2014_New_York_State_Medicaid_Expansion_and.64.aspx ↩︎
- Tim F. Liao and Fernando De Maio, “Association of Social and Economic Inequality With Coronavirus Disease 2019 Incidence and Mortality Across US Counties,” JAMA Network Open 4, no.1 (January 2021), https://doi.org/10.1001/jamanetworkopen.2020.34578 ↩︎
- Rahi Abouk, Lorens Helmchen, Ali Moghtaderi, and Jesse Pines, “The ACA Medicaid Expansions and Opioid Mortality: Is There a Link?,” Medical Care Research and Review Epub ahead of print (October 2020), https://doi.org/10.1177/1077558720967227 ↩︎
- Ying Liu et al., “Association of Medicaid Expansion Under the Patient Protection and Affordable Care Act With Non-Small Cell Lung Cancer Survival,” JAMA Oncology 6 no. 8 (August 2020): 1289-1290, https://doi.org/doi:10.1001/jamaoncol.2020.1040 ↩︎
- Wen Liu, Michael Goodman, and Christopher P. Filson, “Association of State-Level Medicaid Expansion With Treatment of Patients With Higher-Risk Prostate Cancer,” Jama Open Network 3 no. 10 (October 2020), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2771396 ↩︎
- Archana Babu et al., “The Affordable Care Act: Implications for Underserved Populations with Head & Neck Cancer,” American Journal of Otolaryngology 41, no. 4 (July-August 2020), https://doi.org/10.1016/j.amjoto.2020.102464 ↩︎
- Nosayaba Osazuwa-Peters et al., “State Medicaid Expansion Status, Insurance Coverage and Stage at Diagnosis in Head and Neck Cancer Patients,” Oral Oncology 110 (November 2020), https://doi.org/10.1016/j.oraloncology.2020.104870 ↩︎
- David Barrington et. al., “Where You Live Matters: A National Cancer Database Study of Medicaid Expansion and Endometrial Cancer Outcomes,” Gynecologic Oncology 158 no. 2 (August 2020): 407-414, https://doi.org/10.1016/j.ygyno.2020.05.018 ↩︎
- Azeem Tariq Malik, John Alexander, Safdar Khan, and Thomas J. Scharschmidt, “Has the Affordable Care Act Been Associated with Increased Insurance Coverage and Early-stage Diagnoses of Bone and Soft-tissue Sarcomas in Adults?,” Clinical Orthapaedics and Related Research Epub ahead of print (March 2021), https://doi.org/10.1097/CORR.0000000000001438 ↩︎
- Ari D. Schuman et al., “Changes in Diagnosis of Thyroid Cancer Among Medicaid Beneficiaries Following Medicaid Expansion,” JAMASurgery 155 no. 11 (September 2020): 1080-1081, https://doi.org/doi:10.1001/jamasurg.2020.3290 ↩︎
- Bharat Akhanda Panuganti, Emelia Stuart, and Philip Weissbrod, “Changes In Treatment Trends in the Early Glottic Cancer Population after the Affordable Care Act,” Journal of the Sciences and Specialties of the Head and Neck 43 no. 1 (September 2020): 137-144, https://doi.org/10.1002/hed.26463 ↩︎
- Heather Angier et al., “The Affordable Care Act Improved Health Insurance Coverage and Cardiovascular-Related Screening Rates for Cancer Survivors Seen in Community Health Centers,” Cancer 126 no. 14 (July 2020): 3303-3311, https://doi.org/10.1002/cncr.32900 ↩︎
- Nuriel Moghavem et al., “Impact of the Patient Protection and Affordable Care Act on 1-year Survival in Glioblastoma Patients,” Neuro-Oncology Advances 2 no. 1 (January-December 2020): 1-10, https://doi.org/10.1093/noajnl/vdaa080 ↩︎
- Richard J. Straker et al., “Association of the Affordable Care Act’s Medicaid Expansion with the Diagnosis and Treatment of Clinically Localized Melanoma: A National Cancer Database Study” Journal of the Amerian Academy of Dermatology Epub ahead of print, (February 2021), https://www.jaad.org/article/S0190-9622(21)00308-X/pdf ↩︎
- Samuel U. Takvorian et al., “Association of Medicaid Expansion Under the Affordable Care Act With Insurance Status, Cancer Stage, and Timely Treatment Among Patients With Breast, Colon, and Lung Cancer,” Jama Network Open 3 no. 2 (February 2020), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2761262 ↩︎
- Adam B. Weiner et al., “Insurance Coverage, Stage at Diagnosis, and Time to Treatment Following Dependent Coverage and Medicaid Expansion for Men With Testicular Cancer,” PLOS ONE 15 no. 9 (September 2020), https://doi.org/10.1371/journal.pone.0238813 ↩︎
- Benjamin B. Albright et al., “Impact of Medicaid Expansion on Women with Gynecologic Cancer: a Difference-in-Difference Analysis,” American Journal of Obstetrics and Gynecology 224 no. 2 (February 2021): 1-17, https://doi.org/10.1016/j.ajog.2020.08.007 ↩︎
- Quyen D. Chu et al., “Positive Impact of the Patient Protection and Affordable Care Act Medicaid Expansion on Louisiana Women with Breast Cancer,” Cancer Epub ahead of print (November 2020), https://doi.org/10.1002/cncr.33265 ↩︎
- Jessica Limberg et al., “Association of Medicaid Expansion of the Affordable Care Act with the Stage at Diagnosis and Treatment of Papillary Thyroid Cancer: A Difference-in-Differences Analysis,” The American Journal of Surgery Epub ahead of print (January 2021), https://www.americanjournalofsurgery.com/article/S0002-9610(21)00034-9/fulltext#articleInformation ↩︎
- Richard S. Hoehn et al., “Association Between Medicaid Expansion and Diagnosis and Management of Colon Cancer,” Journal of the American College of Surgeons 232 no. 2 (February 2021), https://www.journalacs.org/article/S1072-7515(20)32462-5/fulltext ↩︎
- Justin Le Blanc, Danielle Heller, Ann Friedrich, Donald Lannin, and Tristen Park, “Association of Medicaid Expansion Under the Affordable Care Act With Breast Cancer Stage at Diagnosis,” JAMA Surgery (July 2020), https://doi.org/10.1001/jamasurg.2020.1495 ↩︎
- Adrian Diaz, Daniel Chavarin, Anghela Z. Paredes, and Timothy M. Pawlik, “Utilization of High-Volume Hospitals for High-Risk Cancer Surgery in California Following Medicaid Expansion,” Journal of Gastrointestinal Surgery Epub ahead of print (July 2020), https://link.springer.com/article/10.1007/s11605-020-04747-8 ↩︎
- Johanna Catherine Maclean, Michael T. Halpern, Steven C. Hill, and Michael F. Pesko, “The Effect of Medicaid Expansion on Prescriptions for Breast Cancer Hormonal Therapy Medications,” Health Services Research, 55 no. 3 (April 2020): 399-410, https://doi.org/10.1111/1475-6773.13289 ↩︎
- Jason Tong et al., “The Impact of the Affordable Care Act on Surgeon Selection Amongst Colorectal Surgery Patients,” The American Journal of Surgery Epub ahead of print (February 2021), https://doi.org/10.1016/j.amjsurg.2021.01.041 ↩︎
- Uriel Kim, Siran Koroukian, Abby Statler, and Johnie Rose, “The Effect of Medicaid Expansion Among Adults from Low-Income Communities on Stage at Diagnosis in Those with Screening-Amenable Cancers,” Cancer 126, no. 18 (September 2020): 4209-4219, https://doi-org.proxy.library.cornell.edu/10.1002/cncr.32895 ↩︎
- Dan Kirkpatrick, Margaret Dunn, and Rebecca Tuttle, “Breast Cancer Stage at Presentation in Ohio: The Effect of Medicaid Expansion and the Affordable Care Act,” The American surgeon 86, no. 3 (2020): 195–199, https://pubmed.ncbi.nlm.nih.gov/32223797/ ↩︎
- Anuj S. Desai et al., “Medicaid Expansion Did not Improve Time to Treatment for Young Patients With Metastatic Renal Cell Carcinoma,” Clinical Genitourinary Prostate, Kidney, & Bladder Cancer 18 no. 4 (August 2020):386-390, https://doi.org/10.1016/j.clgc.2020.01.006 ↩︎
- Ying Liu et al., “Association of Medicaid Expansion Under the Patient Protection and Affordable Care Act With Non-Small Cell Lung Cancer Survival,” JAMA Oncology 6 no. 8 (August 2020): 1289-1290, https://doi.org/doi:10.1001/jamaoncol.2020.1040 ↩︎
- Justin Le Blanc, Danielle Heller, Ann Friedrich, Donald Lannin, and Tristen Park, “Association of Medicaid Expansion Under the Affordable Care Act With Breast Cancer Stage at Diagnosis,” JAMA Surgery (July 2020), https://doi.org/10.1001/jamasurg.2020.1495 ↩︎
- Azeem Tariq Malik, John Alexander, Safdar Khan, and Thomas J. Scharschmidt, “Has the Affordable Care Act Been Associated with Increased Insurance Coverage and Early-stage Diagnoses of Bone and Soft-tissue Sarcomas in Adults?,” Clinical Orthapaedics and Related Research Epub ahead of print (March 2021), https://doi.org/10.1097/CORR.0000000000001438 ↩︎
- Bharat Akhanda Panuganti, Emelia Stuart, and Philip Weissbrod, “Changes In Treatment Trends in the Early Glottic Cancer Population after the Affordable Care Act,” Journal of the Sciences and Specialties of the Head and Neck 43 no. 1 (September 2020): 137-144, https://doi.org/10.1002/hed.26463 ↩︎
- Richard J. Straker et al., “Association of the Affordable Care Act’s Medicaid Expansion with the Diagnosis and Treatment of Clinically Localized Melanoma: A National Cancer Database Study” Journal of the Amerian Academy of Dermatology Epub ahead of print, (February 2021), https://www.jaad.org/article/S0190-9622(21)00308-X/pdf ↩︎
- Nosayaba Osazuwa-Peters et al., “State Medicaid Expansion Status, Insurance Coverage and Stage at Diagnosis in Head and Neck Cancer Patients,” Oral Oncology 110 (November 2020), https://doi.org/10.1016/j.oraloncology.2020.104870 ↩︎
- Neelima Panth et al., “Change in Stage of Presentation of Head and Neck Cancer in the United States Before and After the Affordable Care Act,” Cancer Epidemiology 67 (August 2020), https://doi.org/10.1016/j.canep.2020.101763 ↩︎
- Ari D. Schuman et al., “Changes in Diagnosis of Thyroid Cancer Among Medicaid Beneficiaries Following Medicaid Expansion,” JAMASurgery 155 no. 11 (September 2020): 1080-1081, https://doi.org/doi:10.1001/jamasurg.2020.3290 ↩︎
- Samuel U. Takvorian et al., “Association of Medicaid Expansion Under the Affordable Care Act With Insurance Status, Cancer Stage, and Timely Treatment Among Patients With Breast, Colon, and Lung Cancer,” Jama Network Open 3 no. 2 (February 2020), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2761262 ↩︎
- Michelle C. Salazar et al., “Evaluation of Cancer Care After Medicaid Expansion Under the Affordable Care Act,” JAMA Network Open 3 no. 9 (September 2020), https://doi.org/10.1001/jamanetworkopen.2020.17544 ↩︎
- Adam B. Weiner et al., “Changes in Prostate-Specific Antigen at the Time of Prostate Cancer Diagnosis After Medicaid Expansion in Young Men,” Cancer 126 no. 14 (July 2020): 3229-3236, https://doi.org/10.1002/cncr.32930 ↩︎
- Quyen D. Chu et al., “Positive Impact of the Patient Protection and Affordable Care Act Medicaid Expansion on Louisiana Women with Breast Cancer,” Cancer Epub ahead of print (November 2020), https://doi.org/10.1002/cncr.33265 ↩︎
- Richard S. Hoehn et al., “Association Between Medicaid Expansion and Diagnosis and Management of Colon Cancer,” Journal of the American College of Surgeons 232 no. 2 (February 2021), https://www.journalacs.org/article/S1072-7515(20)32462-5/fulltext ↩︎
- Uriel Kim, Siran Koroukian, Abby Statler, and Johnie Rose, “The Effect of Medicaid Expansion Among Adults from Low-Income Communities on Stage at Diagnosis in Those with Screening-Amenable Cancers,” Cancer 126, no. 18 (September 2020): 4209-4219, https://doi-org.proxy.library.cornell.edu/10.1002/cncr.32895 ↩︎
- David Barrington et. al., “Where You Live Matters: A National Cancer Database Study of Medicaid Expansion and Endometrial Cancer Outcomes,” Gynecologic Oncology 158 no. 2 (August 2020): 407-414, https://doi.org/10.1016/j.ygyno.2020.05.018 ↩︎
- Adam B. Weiner et al., “Insurance Coverage, Stage at Diagnosis, and Time to Treatment Following Dependent Coverage and Medicaid Expansion for Men With Testicular Cancer,” PLOS ONE 15 no. 9 (September 2020), https://doi.org/10.1371/journal.pone.0238813 ↩︎
- Benjamin B. Albright et al., “Impact of Medicaid Expansion on Women with Gynecologic Cancer: a Difference-in-Difference Analysis,” American Journal of Obstetrics and Gynecology 224 no. 2 (February 2021): 1-17, https://doi.org/10.1016/j.ajog.2020.08.007 ↩︎
- Jessica Limberg et al., “Association of Medicaid Expansion of the Affordable Care Act with the Stage at Diagnosis and Treatment of Papillary Thyroid Cancer: A Difference-in-Differences Analysis,” The American Journal of Surgery Epub ahead of print (January 2021), https://www.americanjournalofsurgery.com/article/S0002-9610(21)00034-9/fulltext#articleInformation ↩︎
- Lauren Lin, Aparna Soni, Lindsay M. Sabik, and Coleman Drake, “Early- and Late-Stage Cancer Diagnosis Under 3 Years of Medicaid Expansion,” American Journal of Preventative Medicine 60 no. 1 (January 2021):104-109, https://doi.org/10.1016/j.amepre.2020.06.020 ↩︎
- Dan Kirkpatrick, Margaret Dunn, and Rebecca Tuttle, “Breast Cancer Stage at Presentation in Ohio: The Effect of Medicaid Expansion and the Affordable Care Act,” The American surgeon 86, no. 3 (2020): 195–199, https://pubmed.ncbi.nlm.nih.gov/32223797/ ↩︎
- Adrian Diaz, Daniel Chavarin, Anghela Z. Paredes, and Timothy M. Pawlik, “Utilization of High-Volume Hospitals for High-Risk Cancer Surgery in California Following Medicaid Expansion,” Journal of Gastrointestinal Surgery Epub ahead of print (July 2020), https://link.springer.com/article/10.1007/s11605-020-04747-8 ↩︎
- Adam B. Weiner et al., “Insurance Coverage, Stage at Diagnosis, and Time to Treatment Following Dependent Coverage and Medicaid Expansion for Men With Testicular Cancer,” PLOS ONE 15 no. 9 (September 2020), https://doi.org/10.1371/journal.pone.0238813 ↩︎
- Neal Bhutiani et al., “Identifying Factors Influencing Delays in Breast Cancer Treatment in Kentucky Following the 2014 Medicaid Expansion,” Journal of Surgical Oncology 121 no. 8 (June 2020): 1191-1200, https://doi.org/10.1002/jso.25914 ↩︎
- Johanna Catherine Maclean, Michael T. Halpern, Steven C. Hill, and Michael F. Pesko, “The Effect of Medicaid Expansion on Prescriptions for Breast Cancer Hormonal Therapy Medications,” Health Services Research, 55 no. 3 (April 2020): 399-410, https://doi.org/10.1111/1475-6773.13289 ↩︎
- Nuriel Moghavem et al., “Impact of the Patient Protection and Affordable Care Act on 1-year Survival in Glioblastoma Patients,” Neuro-Oncology Advances 2 no. 1 (January-December 2020): 1-10, https://doi.org/10.1093/noajnl/vdaa080 ↩︎
- Justin T. Moyers, Amie Patel, Wendy Shih, and Gayathri Nagaraj, “Association of Sociodemographic Factors With Immunotherapy Receipt for Metastatic Melanoma in the US,” JAMA Network Open 3 no. 9 (September 2020), https://doi.org/10.1001/jamanetworkopen.2020.15656 ↩︎
- Anuj S. Desai et al., “Medicaid Expansion Did not Improve Time to Treatment for Young Patients With Metastatic Renal Cell Carcinoma,” Clinical Genitourinary Prostate, Kidney, & Bladder Cancer 18 no. 4 (August 2020):386-390, https://doi.org/10.1016/j.clgc.2020.01.006 ↩︎
- Wen Liu, Michael Goodman, and Christopher P. Filson, “Association of State-Level Medicaid Expansion With Treatment of Patients With Higher-Risk Prostate Cancer,” Jama Open Network 3 no. 10 (October 2020), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2771396 ↩︎
- Heather Angier et al., “The Affordable Care Act Improved Health Insurance Coverage and Cardiovascular-Related Screening Rates for Cancer Survivors Seen in Community Health Centers,” Cancer 126 no. 14 (July 2020): 3303-3311, https://doi.org/10.1002/cncr.32900 ↩︎
- Jason Tong et al., “The Impact of the Affordable Care Act on Surgeon Selection Amongst Colorectal Surgery Patients,” The American Journal of Surgery Epub ahead of print (February 2021), https://doi.org/10.1016/j.amjsurg.2021.01.041 ↩︎
- Juan Chipollini and Grant R. Pollock, “National Trends in the Management of Low-Risk Prostate Cancer: Analyzing the Impact of Medicaid Expansion in the United States,” International Urology and Nephrology 52 no. 9 (September 2020): 1611–1615, https://doi.org/10.1007/s11255-020-02463-5 ↩︎
- Miranda B. Lam, Jessica Phelan, John Orav, Ashish K. Jha, and Nancy L. Keating, “Medicaid Expansion and Mortality Among Patients With Breast, Lung, and Colorectal Cancer,” Jama Network Open 3 no. 11 (November 2020), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2772535 ↩︎
- Yoshiko Toyoda, Eun Jeong Oh, Ishani D. Premaratne, Codruta Chiuzan, and Christine H. Rohde, “Affordable Care Act State-Specific Medicaid Expansion: Impact on Health Insurance Coverage and Breast Cancer Screening Rate,” Journal of the American College of Surgeons 230 no. 5 (May 2020): 775-783, https://doi.org/10.1016/j.jamcollsurg.2020.01.031 ↩︎
- Daniel B. Nelson et al., “Changes in Coverage, Access, and Health Following Implementation of Healthy Behavior Incentive Medicaid Expansions vs. Traditional Medicaid Expansions,” Journal of General Internal Medicine 35 (September 2020): 2521–2528, https://doi.org/10.1007/s11606-020-05801-6 ↩︎
- Kirsten Y. Eoma, Marian Jarlenskia, Robert E. Schoenb, Linda Robertsonc, and Lindsay M. Sabika, “Sex Differences in the Impact of Affordable Care Act Medicaid Expansion on Colorectal Cancer Screening,” Preventive Medicine 138 (September 2020), https://doi.org/10.1016/j.ypmed.2020.106171 ↩︎
- William C. Daly et al., “National Recommendations against Prostate Specific Antigen Screening versus Statewide Medicaid Expansion Initiatives: A Battle of the Titans,” The Journal of Urology Epub ahead of print (February 2021), https://doi.org/10.1097/JU.0000000000001594 ↩︎
- Sri Lekha Tummalapalli and Salomeh Keylani, “Changes in Preventative Health Care After Medicaid Expansion,” Medical Care 58 no. 6 (June 2020): 549-556, https://doi.org/doi:10.1001/jamanetworkopen.2020.18728 ↩︎
- Aparna Soni, “The Effects of Public Health Insurance on Health Behaviors: Evidence From the Fifth Year of Medicaid Expansion,” Health Economics 29 no. 12 (December 2020): 1586-1605, https://doi.org/10.1002/hec.4155 ↩︎
- Brigit Hatch et al., “Impacts of the Affordable Care Act on Receipt of Women’s Preventive Services in Community Health Centers in Medicaid Expansion and Nonexpansion States,” Women’s Health Issues 31 no. 1 (January 2021): 9-16, https://www.whijournal.com/article/S1049-3867(20)30097-9/fulltext ↩︎
- Brandon M. Hoff, Melvin D. Livingston III, and Erika L. Thompson, “The Association Between State Medicaid Expansion and Human Papillomavirus Vaccination,” Vaccine 38 no. 38 (August 2020): 5963-5965, https://www.sciencedirect.com/science/article/pii/S0264410X20309373?via%3Dihub ↩︎
- Summer Sherburne Hawkins, Krisztina Horvath, Jessica Cohen, Lydia E. Pace, and Christopher F. Baum, “Associations Between Insurance-related Affordable Care Act Policy Changes with HPV Vaccine Completion,” BMC Public Health 21, no. 304 (Februrary 2021), https://doi.org/10.1186/s12889-021-10328-4 ↩︎
- Alisha Monnette, Charles Stoecker, Elizabeth Nauman, and Lizheng Shi, “The Impact of Medicaid Expansion on Access to Care and Preventative Care for Adults with Diabetes and Depression,” Journal of Diabetes and its Complications 34 no. 10 (October 2020), https://doi.org/10.1016/j.jdiacomp.2020.107663 ↩︎
- Dahai Yu, Yuhui Zu, Petra W. Rasmussen, James Godwin, and Ninez A. Ponce, “Coverage, Affordability, and Care for Low-Income People with Diabetes: 4 Years after the Affordable Care Act’s Medicaid Expansions,” Journal of Internal Medicine 35 (January 2020): 2222-2224, https://link.springer.com/article/10.1007/s11606-019-05614-2 ↩︎
- Lily D. Yan, Mohammed K. Ali, and Kiersten L. Strombotne,”Impact of Expanded Medicaid Eligibility on the Diabetes Continuum of Care Among Low-Income Adults: A Difference-in-Differences Analysis,” American Journal of Preventative Medicine 60 no. 2 (February 2021): 189-192, https://doi.org/10.1016/j.amepre.2020.08.013 ↩︎
- Barbara H. Braffett, “Health Care Coverage and Glycemic Control in Young Adults With Youth-Onset Type 2 Diabetes: Results From the TODAY2 Study,” Diabetes Care 43, no. 10 (October 2020): 2469-2477, https://doi.org/10.2337/dc20-0760 ↩︎
- Miguel Marino et al., “The Affordable Care Act: Effects of Insurance on Diabetes Biomarkers,” Diabetes Care, 43 no. 9 (September 2020): 2074-2081, https://doi.org/10.2337/dc19-1571 ↩︎
- Miguel Marino et al., “Disparities in Biomarkers for Patients With Diabetes After the Affordable Care Act,” Medical Care 58 (June 2020), https://doi.org/10.1097/mlr.0000000000001257 ↩︎
- Andrew Sumarsono et al., “Medicaid Expansion and Utilization of Antihyperglycemic Therapies,” Diabetes Care 43 no. 11, (November 2020): 2684-2690, https://care.diabetesjournals.org/content/43/11/2684 ↩︎
- Heather Angier et al., “New Hypertension and Diabetes Diagnoses Following the Affordable Care Act Medicaid Expansion,” Family Medicine and Community Health 8 no. 4 (December 2020), https://fmch.bmj.com/content/8/4/e000607 ↩︎
- Kenrik O. Duru et al., “Evaluation of a National Care Coordination Program to Reduce Utilization Among High-cost, High-need Medicaid Beneficiaries With Diabetes,” Medical Care 58 (June 2020): 14-21, https://journals.lww.com/lww-medicalcare/Fulltext/2020/06001/Evaluation_of_a_National_Care_Coordination_Program.5.aspx ↩︎
- Sri Lekha Tummalapalli and Salomeh Keylani, “Changes in Preventative Health Care After Medicaid Expansion,” Medical Care 58 no. 6 (June 2020): 549-556, https://doi.org/doi:10.1001/jamanetworkopen.2020.18728 ↩︎
- Claire E. Margerison, Robert Kaestner, Jiajia Chen, and Collen MacCallum-Bridges, “Impacts of Medicaid Expansion Prior to Conception on Pre-pregnancy Health, Pregnancy Health, and Outcomes,” American Journal of Epidemiology Epub ahead of print (January 2021), https://doi.org/10.1093/aje/kwaa289 ↩︎
- Rebecca Myerson, Samuel Crawford, and Laura R. Wherry, “Medicaid Expansion Increased Preconception Health Counseling, Folic Acid Intake, And Postpartum Contraception,” Health Affairs 39 no. 11 (November 2020): 1883-1890, https://doi.org/10.1377/hlthaff.2020.00106 ↩︎
- Rebecca Myerson and Samuel Crawford, “Coverage for Adults With Chronic Disease Under the First 5 Years of the Affordable Care Act,” Medical Care 58 no. 10 (October 2020): 861-866, https://doi.org/10.1097/MLR.0000000000001370 ↩︎
- Chinedum O. Ojinnaka, and Yash Suri, “Impact of Medicaid Expansion on Healthcare Access Among Individuals Living With Chronic Diseases,” American Journal of Preventative Medicine 59 no. 2 (August 2020): 149-156, https://doi.org/10.1016/j.amepre.2020.03.012 ↩︎
- Janani Rajbhandari-Thappa, Donglang Zhang, Kara E. MacLeod, Kiran Thapa, “Impact of Medicaid Expansion on Insurance Coverage Rates Among Adult Populations with Low Income and by Obesity Status” The Obesity Society 28 no. 7 (April 2020): 1219-1223, https://doi.org/10.1002/oby.22793 ↩︎
- Mariam Kayle et al., “Impact of Medicaid Expansion on Access and Healthcare Among Individuals with Sickle Cell Disease,” Pediatric Blood and Cancer 67 no. 5 (May 2020), https://onlinelibrary.wiley.com/doi/abs/10.1002/pbc.28152 ↩︎
- Erica M. Valdovinos, Matthew J. Niedzwiecki, Joanna Guo, and Renee Y. Hsia, “Effects of Medicaid Expansion on Access, Treatment and Outcomes for Patients with Acute Myocardial Infarction,” PLOS ONE 15 no. 4 (April 2020), https://doi.org/10.1371/journal.pone.0232097 ↩︎
- Erica M. Valdovinos, Matthew J. Niedzwiecki, Joanna Guo, and Renee Y. Hsia, “The Association of Medicaid Expansion and Racial/Ethnic Inequities in Access, Treatment, and Outcomes for Patients with Acute Myocardial Infarction,” PLOS ONE 15 no. 11 (November 2020), https://doi.org/10.1371/journal.pone.0241785 ↩︎
- Laurent C. Glance, Caroline P. Thirukumaran, Ernie Shippey, Stewart J. Lustik, and Andrew W. Dick, “Impact of Medicaid Expansion on Disparities in Revascularization in Patients Hospitalized with Acute Myocardial Infarction,” PLOS One Epub ahead of print (December 2020), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0243385 ↩︎
- Monique Barakat et al., “Recent Trends and the Impact of the Affordable Care Act on Emergency Department Visits and Hospitalizations for Gastrointestinal, Pancreatic, and Liver Diseases,” Journal of Clinical Gastroenterology 54 no. 3 (March 2020), https://doi.org/10.1097/MCG.0000000000001102 ↩︎
- Scott R. Levin et al., “Association of Medicaid Expansion with Tunneled Dialysis Catheter Use at the Time of First Arteriovenous Access Creation,” Annals of Vascular Surgery Epub ahead of print (January 2021), https://www.annalsofvascularsurgery.com/article/S0890-5096(21)00082-0/fulltext ↩︎
- Lauren D. Nephew et al., “Association of State Medicaid Expansion with Racial/Ethnic Disparities in Liver Transplant Wait-listing in the United States,” Jama Network Open 3 no. 10 (October 2020), https://doi.org/10.1001/jamanetworkopen.2020.19869 ↩︎
- Melissa McInerney, Ruth Winecoff, Padmaja Ayyagari, Kosali Simon, and M. Kate Bundorf, “ACA Medicaid Expansion Associated With Increased Medicaid Participation and Improved Health Among Near-Elderly: Evidence From the Health and Retirement Study,” Inquiry: The Journal of Health Care Organization, Provision, and Financing 57 (July 2020): 1-10, https://doi.org/10.1177/0046958020935229 ↩︎
- Hiroshi Gotanda, Gerald F. Kominski, David Elashoff, and Yusuke Tsugawa, “Association Between the ACA Medicaid Expansions and Changes in Cardiovascular Risk Factors Among Low-Income Individuals,” Journal of General Internal Medicine Epub ahead of print (January 2021), https://doi.org/10.1007/s11606-020-06417-6 ↩︎
- Smriti Rajita Kumar, Sameed Ahmed M. Khatana, and David Goldberg, “Impact of Medicaid Expansion on Liver-Related Mortality,” Clinical Gastroenterology and Hepatology Epub ahead of print (December 2020), https://doi.org/10.1016/j.cgh.2020.11.042 ↩︎
- Sadiya S. Khan, Donald M. Lloyd Jones, Mercedes Carnethon, Lindsay R. Pool, “Medicaid Expansion and State-Level Differences in Premature Cardiovascular Mortality by Subtype, 2010–2017,” Hypertension 76 (September 2020): 37-38, https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.120.15968 ↩︎
- Heather Angier et al., “Role of Health Insurance and Neighborhood-Level Social Deprivation on Hypertension Control Following the Affordable Care Act Health Insurance Opportunities,” Social Science & Medicine 265 Epub ahead of print (November 2020), https://doi.org/10.1016/j.socscimed.2020.113439 ↩︎
- Andrew Sumarsono et al., “Association of Medicaid Expansion with Rates of Utilization of Cardiovascular Therapies among Medicaid Beneficiaries Between 2011 and 2018,” Circulation: Cardiovascular Quality and Outcomes 14 no. 1 (January 2021), https://doi.org/10.1161/CIRCOUTCOMES.120.007492 ↩︎
- Sameed Ahmed M. Khatana et al., “Medicaid Expansion and Ventricular Assist Device Implantation,” Journal of the American College of Cardiology 76 no. 12 (September 2020):1501-1502, https://www.sciencedirect.com/science/article/abs/pii/S0735109720361064?via%3Dihub ↩︎
- Khadijah Breathett et al., “Is the Affordable Care Act Medicaid Expansion Linked to Change in Rate of Ventricular Assist Device Implantation for Blacks and Whites?” Circulation: Heart Failure 13, no. 4 (April 2020), https://doi.org/10.1161/CIRCHEARTFAILURE.119.006544 ↩︎
- Xiaowen Wang, Alina A. Luke, Justin M. Vader, Thomas M. Maddox, and Karen E. Joynt Maddox, “Disparities and Impact of Medicaid Expansion on Left Ventricular Assist Device Implantation and Outcomes,” Circulation: Cardiovascular Quality and Outcomes 13 no. 6 (June 2020), https://doi.org/10.1161/CIRCOUTCOMES.119.006284 ↩︎
- Afshin Ehsan et al., “Cardiac Surgery Utilization Across Vulnerable Persons After Medicaid Expansion,” (2020), The Annals of Thoracic Surgery Epub ahead of print (November 2020), https://doi.org/10.1016/j.athoracsur.2020.08.066 ↩︎
- Heather Angier et al., “New Hypertension and Diabetes Diagnoses Following the Affordable Care Act Medicaid Expansion,” Family Medicine and Community Health 8 no. 4 (December 2020), https://fmch.bmj.com/content/8/4/e000607 ↩︎
- Heather Angier et al., “The Affordable Care Act Improved Health Insurance Coverage and Cardiovascular-Related Screening Rates for Cancer Survivors Seen in Community Health Centers,” Cancer 126 no. 14 (July 2020): 3303-3311, https://doi.org/10.1002/cncr.32900 ↩︎
- Daniel B. Nelson et al., “Changes in Coverage, Access, and Health Following Implementation of Healthy Behavior Incentive Medicaid Expansions vs. Traditional Medicaid Expansions,” Journal of General Internal Medicine 35 (September 2020): 2521–2528, https://doi.org/10.1007/s11606-020-05801-6 ↩︎
- Sri Lekha Tummalapalli and Salomeh Keylani, “Changes in Preventative Health Care After Medicaid Expansion,” Medical Care 58 no. 6 (June 2020): 549-556, https://doi.org/doi:10.1001/jamanetworkopen.2020.18728 ↩︎
- Aparna Soni, “The Effects of Public Health Insurance on Health Behaviors: Evidence From the Fifth Year of Medicaid Expansion,” Health Economics 29 no. 12 (December 2020): 1586-1605, https://doi.org/10.1002/hec.4155 ↩︎
- Rebecca Myerson, Samuel Crawford, and Laura R. Wherry, “Medicaid Expansion Increased Preconception Health Counseling, Folic Acid Intake, And Postpartum Contraception,” Health Affairs 39 no. 11 (November 2020): 1883-1890, https://doi.org/10.1377/hlthaff.2020.00106 ↩︎
- Melissa McInerney and Mark K. Meiselbach, “Distributional Effects of Recent Health Insurance Expansions on Weight-Related Outcomes,” Economics & Human Biology 38, Epub ahead of print (August 2020), https://doi.org/10.1016/j.ehb.2020.100870 ↩︎
- Molly O’Malley Watts, MaryBeth Musumeci, and Priya Chidambaram, State Variation in Medicaid LTSS Policy Choices and Implications for Upcoming Policy Debates (Washington, DC: KFF, February 2021), https://modern.kff.org/report-section/state-variation-in-medicaid-ltss-policy-choices-and-implications-for-upcoming-policy-debates-issue-brief/ ↩︎
- Stephan Lindner, Anna Levy, and Willi Horner-Johnson, “The Medicaid Expansion Did Not Crowd Out Access for Medicaid Recipients With Disabilities in Oregon,” Disability and Health Journal (Novermber 2020), https://doi.org/10.1016/j.dhjo.2020.101010 ↩︎
- Maria E. Torres, Benjamin D. Capistrant, and Hannah Karpman, “The Effect of Medicaid Expansion on Caregiver’s Quality of Life,” Social Work in Public Health 35 no. 6 (August 2020): 473-482, https://doi.org/10.1080/19371918.2020.1798836 ↩︎
- Bradley Heim, Ithai Lurie, Kathleen J.Mullen, and Kosali Simon, “How Much Do Outside Options Matter? The Effect of Subsidized Health Insurance on Social Security Disability Insurance Benefit Receipt,” Journal of Health Economics 76 Epub ahead of print (January 2021), https://doi.org/10.1016/j.jhealeco.2021.102437 ↩︎
- Purvi Sevak and Jodi Schimmel Hyde, “The ACA Medicaid Expansions and Employment of Adults With Disabilities,” Journal of Disability Policy Studies Epub ahead of print (July 2020), https://doi.org/10.1177/1044207320943554 ↩︎
- Rebecca Myerson, Samuel Crawford, Laura R. Wherry, “Medicaid Expansion Increased Preconception Health Counseling, Folic Acid Intake, And Postpartum Contraception,” Health Affairs 39 no. 11 (November 2020): 1883-1890, https://www.healthaffairs.org/doi/10.1377/hlthaff.2020.00106 ↩︎
- Tyler N. A. Winkelman et al., “Medications for Opioid Use Disorder among Pregnant Women Referred by Criminal Justice Agencies before and after Medicaid Expansion: A Retrospective Study of Admissions to Treatment Centers in the United States,” PLOS Medicine 17 no. 5 (May 2020), https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1003119 ↩︎
- S. Marie Harvey et al., “Impact of Medicaid Expansion in Oregon on Access to Prenatal Care,” Preventative Medicine 143 (February 2021), https://www.sciencedirect.com/science/article/abs/pii/S0091743520303911?via%3Dihub ↩︎
- Makayla Palmer, “Preconception Subsidized Insurance: Prenatal Care and Birth Outcomes by Race/Ethnicity,” Health Economics 29 no. 9 (September 2020): 1013-1030, https://doi.org/10.1002/hec.4116 ↩︎
- Wei Lyu and George L. Wehby, “Heterogeneous Effects of Affordable Care Act Medicaid Expansions Among Women with Dependent Children by State-Level Pre-Expansion Eligibility,” Journal of Women’s Health Epub ahead of print (Februrary 2021), https://doi.org/10.1089/jwh.2020.8776 ↩︎
- Erica Eliason, “Adoption of Medicaid Expansion Is Associated with Lower Maternal Mortality,” Women’s Health Issues 30, no. 3 (May-June 2020): 147-152, https://doi.org/10.1016/j.whi.2020.01.005 ↩︎
- Jean Guglielminotti, Ruth Landau, and Guohua Li, “The 2014 New York States Medicaid Expansion and Severe Maternal Morbidity,” Anesthesia and Analgesia 10 (January 2021), https://journals.lww.com/anesthesia-analgesia/Abstract/9900/The_2014_New_York_State_Medicaid_Expansion_and.64.aspx ↩︎
- S. Marie Harvey, Lisa P. Oakley, Susannah E. Gibbs, Shyama Mahakalanda, Jeff Luck, and Jangho Yoon, “Impact of Medicaid Expansion in Oregon on Access to Prenatal Care,” Preventative Medicine 143 (February 2021), https://www.sciencedirect.com/science/article/pii/S0091743520303911?via%3Dihub ↩︎
- Alexandra Wiggins, Ibraheem M. Karaye, Jennifer A. Horney, “Medicaid Expansion and Infant Mortality, Revisited: A Difference-In-Differences Analysis,” Health Services Research 55, no. 3 (March 2020): 393-398, https://doi.org/10.1111/1475-6773.13286 ↩︎
- Clare Brown, Jennifer Moore, Felix Holly, Kathryn Stewart, and Mick Tilford, “County-level Variation in Low Birthweight and Preterm Birth: An Evaluation of State Medicaid Expansion Under the Affordable Care Act,” Medical Care 58, no. 6 (June 2020): 497-503, https://doi.org/10.1097/mlr.0000000000001313 ↩︎
- Amanda Cooke and Amanda Stype, “Medicaid Expansion and Infant Mortality: The (Questionable) Impact of the Affordable Care Act,” Journal of Epidemiology and Community Health 75 no. 1 (January 2021): 10-15, https://jech.bmj.com/content/75/1/10 ↩︎
- Claire E. Margerison, Robert Kestner, Jiajia Chen, Collen MacCullum-Bridges, “Impacts of Medicaid Expansion Prior to Conception on Pre-pregnancy Health, Pregnancy Health, and Outcomes,” American Journal of Epidemiology Epub ahead of print (January 2021), https://academic.oup.com/aje/advance-article/doi/10.1093/aje/kwaa289/6071895 ↩︎
- Kristen S. Marchi, Melanie S. Dove, Katherine E. Heck, Chuncui Fan, “The Affordable Care Act and Changes in Women’s Health Insurance Coverage Before, During, and After Pregnancy in California,” Public Health Reports, 136 no. 1 (October 2020): 70-78, https://journals.sagepub.com/doi/10.1177/0033354920962798#articleCitationDownloadContainer ↩︎
- Rebecca Myerson, Samuel Crawford, Laura R. Wherry, “Medicaid Expansion Increased Preconception Health Counseling, Folic Acid Intake, And Postpartum Contraception,” Health Affairs 39 no. 11 (November 2020): 1883-1890, https://www.healthaffairs.org/doi/10.1377/hlthaff.2020.00106 ↩︎
- Lucy Chen, Richard G. Frank, and Haiden A. Huskamp, “Overturning the ACA’s Medicaid Expansion Would Likely Decrease Low-Income, Reproductive-Age Women’s Healthcare Spending and Utilization,” Inquiry: The Journal of Health Care Organization, Provision, and Financing 57 (December 2020), https://journals.sagepub.com/doi/10.1177/0046958020981462 ↩︎
- Emily M. Johnston, Stacey McMorrow, Tyler Thomas, and Genevieve M. Kenney, “ACA Medicaid Expansion and Insurance Coverage among New Mothers Living in Poverty,” Pediatrics 145 no. 5 (May 2020), https://pediatrics.aappublications.org/content/145/5/e20193178 ↩︎
- Jamie R. Daw, Tyler N. A. Winkelman, Vanessa K. Dalton, Katy B. Kozhimannil, and Lindsay K. Admon, “Medicaid Expansion Improved Perinatal Insurance Continuity For Low-Income Women” Health Affairs 39 no. 9 (September 2020), https://www.healthaffairs.org/doi/10.1377/hlthaff.2019.01835 ↩︎
- Anne L. Dunlop, Peter Joski, Andrea E. Strahan, Erica Sierra, and Kathleen Adams, “Postpartum Medicaid Coverage and Contraceptive Use Before and After Ohio’s Medicaid Expansion Under the Affordable Care Act,” Women’s Health Issues 30 no. 6 (November 2020): 426–435, https://doi.org/10.1016/j.whi.2020.08.006 ↩︎
- S. Marie Harvey et al., “Impact of Medicaid Expansion in Oregon on Access to Prenatal Care,” Preventative Medicine 143 (February 2021), https://www.sciencedirect.com/science/article/abs/pii/S0091743520303911?via%3Dihub ↩︎
- Jean Guglielminotti, Ruth Landau, and Guohua Li, “The 2014 New York States Medicaid Expansion and Severe Maternal Morbidity,” Anesthesia and Analgesia 10 (January 2021), https://journals.lww.com/anesthesia-analgesia/Abstract/9900/The_2014_New_York_State_Medicaid_Expansion_and.64.aspx ↩︎
- Makayla Palmer, “Preconception Subsidized Insurance: Prenatal Care and Birth Outcomes by Race/Ethnicity,” Health Economics 29 no. 9 (September 2020): 1013-1030, https://doi.org/10.1002/hec.4116 ↩︎
- Rebecca Myerson, Samuel Crawford, Laura R. Wherry, “Medicaid Expansion Increased Preconception Health Counseling, Folic Acid Intake, And Postpartum Contraception,” Health Affairs 39 no. 11 (November 2020): 1883-1890, https://www.healthaffairs.org/doi/10.1377/hlthaff.2020.00106 ↩︎
- Blair G. Darney et al., “Evaluation of Medicaid Expansion Under the Affordable Care Act and Contraceptive Care in US Community Health Centers,” JAMA Network Open 3 no. 6 (June 2020), https://doi.org/10.1001/jamanetworkopen.2020.6874 ↩︎
- Anne L. Dunlop, Peter Joski, Andrea E. Strahan, Erica Sierra, and Kathleen Adams, “Postpartum Medicaid Coverage and Contraceptive Use Before and After Ohio’s Medicaid Expansion Under the Affordable Care Act,” Women’s Health Issues 30 no. 6 (November 2020): 426–435, https://doi.org/10.1016/j.whi.2020.08.006 ↩︎
- Andrew Sumarsono et al., “Medicaid Expansion and Provision of Prescription Contraception to Medicaid Beneficiaries,” An Internal Reproductive Health Journal: Contraception Epub ahead of print (November 2020), https://www.contraceptionjournal.org/article/S0010-7824(20)30415-7/fulltext ↩︎
- Susannah E. Gibbs, S. Marie Harvey, Annie Larson, Jangho Yoon, and Jeff Luck, “Contraceptive Services After Medicaid Expansion in a State with a Medicaid Family Planning Waiver Program,” Journal of Women’s Health Epub ahead of print (October 2020), https://doi.org/10.1089/jwh.2020.8351 ↩︎
- Blair G. Darney et al., “Payment for Contraceptive Services in Safety Net Clinics: Roles of Affordable Care Act, Title X, and State Programs,” Medical Care 58 no. 5 (May 2020): 453-460, https://doi.org/10.1097/mlr.0000000000001309 ↩︎
- Anitha Menon, Payal K. Patel, Monita Karmakar, and Renuka Tipirneni, “The Impact of the Affordable Care Act Medicaid Expansion on Racial/Ethnic and Sex Disparities in HIV Testing: National Findings fromthe Behavioral Risk Factor Surveillance System,” Journal of General Internal Medicine Epub ahead of print (January 2021), https://doi.org/10.1007/s11606-021-06590-2 ↩︎
- Sri Lekha Tummalapalli and Salomeh Keylani, “Changes in Preventative Health Care After Medicaid Expansion,” Medical Care 58 no. 6 (June 2020): 549-556, https://journals.lww.com/lww-medicalcare/Abstract/2020/06000/Changes_in_Preventative_Health_Care_After_Medicaid.8.aspx ↩︎
- Aparna Soni, “The Effects of Public Health Insurance on Health Behaviors: Evidence From the Fifth Year of Medicaid Expansion,” Health Economics 29 no. 12 (December 2020): 1586-1605, https://doi.org/10.1002/hec.4155 ↩︎
- Bita Fayaz Farkhad, David R. Holtgrave, and Dolores Albarracín, “Effect of Medicaid Expansions on HIV Diagnoses and Pre-Exposure Prophylaxis Use,” American Journal of Preventive Medicine Epub ahead of print (January 2021), https://doi.org/10.1016/j.amepre.2020.10.021 ↩︎
- Daniel B. Nelson et al., “Changes in Coverage, Access, and Health Following Implementation of Healthy Behavior Incentive Medicaid Expansions vs. Traditional Medicaid Expansions,” Journal of General Internal Medicine 35 (September 2020): 2521–2528, https://doi.org/10.1007/s11606-020-05801-6 ↩︎
- Brigit Hatch et al., “Impacts of the Affordable Care Act on Receipt of Women’s Preventive Services in Community Health Centers in Medicaid Expansion and Nonexpansion States,” Women’s Health Issues 31 no. 1 (January 2021): 9-16, https://www.whijournal.com/article/S1049-3867(20)30097-9/fulltext ↩︎
- Rashunda Lewis et al., “Healthcare Access and Utilization Among Persons Who Inject Drugs in Medicaid Expansion and Nonexpansion States: 22 United States Cities, 2018,” The Journal of Infectious Diseases 222, no. 5 (October 2020): S420–S428, https://doi.org/10.1093/infdis/jiaa337 ↩︎
- Amy R. Baugher et al., “Health Care Coverage and Preexposure Prophylaxis (PrEP) Use Among Men Who Have Sex With Men Living in 22 US Cities With vs Without Medicaid Expansion, 2017,” American Journal of Public Health Epub ahead of print (January 2021), https://doi.org/10.2105/ajph.2020.306035 ↩︎
- Kathleen A. McManus, Karishma Srikanth, Samuel D. Powers, Rebecca Dillingham, and Elizabeth T. Rogawski McQuade, “Medicaid Expansion’s Impact on Human Immunodeficiency Virus Outcomes in a Nonurban Southeastern Ryan White HIV/AIDS Program Clinic,” Open Forum Infectious Diseases 8 no. 2 (February 2021), https://doi.org/10.1093/ofid/ofaa595 ↩︎
- Dimitris Karlestos and Charles Stoecker, “Impact of Medicaid Expansion on PrEP Utilization in the US: 2012–2018” AIDS and Behavior Epub ahead of print. (October 2020), https://link.springer.com/article/10.1007/s10461-020-03070-2#citeas ↩︎
- Kathleen A. McManus, Joshua Ferey, Elizabeth Farrell, and Rebecca Dillingham, “National Survey of US HIV Clinicians: Knowledge and Attitudes About the Affordable Care Act and Opinions of its Impact on Quality of Care and Barriers to Care,” Open Forum Infectious Diseases 7, no. 7 (July 2020), https://doi.org/10.1093/ofid/ofaa225 ↩︎
- Stephen Bonett, Steven Meanley, Steven Elsesser, and José Bauermeister, “State-Level Discrimination Policies And HIV Pre-Exposure Prophylaxis Adoption Efforts In The US,” Health Affairs 39 no. 9 (September 2020): 1575-1582, https://doi.org/10.1377/hlthaff.2020.00242 ↩︎
- Mark Olfson et al., “Medicaid Expansion and Low-Income Adults with Substance Use Disorders,” The Journal of Behavioral Health Services and Research Epub ahead of print (November 2020), https://link.springer.com/article/10.1007/s11414-020-09738-w ↩︎
- Rashunda Lewis et al., “Healthcare Access and Utilization Among Persons Who Inject Drugs in Medicaid Expansion and Nonexpansion States: 22 United States Cities, 2018,” The Journal of Infectious Diseases 222, no. 5 (October 2020): S420–S428, https://doi.org/10.1093/infdis/jiaa337 ↩︎
- Minji Sohn et al., “Association Between State Medicaid Expansion Status And Naloxone Prescription Dispensing” Health Services Research 55 no. 2 (February 2020): 239-248, https://onlinelibrary.wiley.com/doi/10.1111/1475-6773.13266 ↩︎
- Brendan Saloner and Johanna Catherine Maclean, “Specialty Substance Use Disorder Treatment Admissions Steadily Increased In The Four Years After Medicaid Expansion,” Health Affairs 39 no. 3 (March 2020): 453–461, https://doi.org/10.1377/hlthaff.2019.01428 ↩︎
- Hefei Wen et. al, “Association Between Medicaid Expansion and Rates of Opioid-Related Hospital Use,” JAMA Internal Medicine 180 no. 5 (May 2020): 753-759, https://doi.org/10.1001/jamainternmed.2020.0473 ↩︎
- George Pro, Jeff Utter, Shane Haberstroh, and Julie A. Baldwin, “Dual Mental Health Diagnoses Predict the Receipt of Medication-Assisted Opioid Treatment: Associations Moderated By State Medicaid Expansion Status, Race/Ethnicity and Gender, and Year,” Drug and Alcohol Dependence 209 (April 2020), https://doi.org/10.1016/j.drugalcdep.2020.107952 ↩︎
- Iraklis Erik Tseregounis, James J. Gasper, and Stephen G. Henry, “Trends in Buprenorphine to Treat Opioid Use Disorder in California, 2012 to 2018: Medicaid Outpaces the Rest of the State,” Journal of Addiction Medicine Epub ahead of print (November 2020), https://doi.org/10.1097/ADM.0000000000000768 ↩︎
- Tyler N. A. Winkelman et al., “Medications for Opioid Use Disorder among Pregnant Women Referred by Criminal Justice Agencies before and after Medicaid Expansion: A Retrospective Study of Admissions to Treatment Centers in the United States,” PLOS Medicine 17 no. 5 (May 2020), https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1003119 ↩︎
- Mark Olfson, Victoria Shu Zhang, Marissa King, and Ramin Mojtabai, “Changes in Buprenorphine Treatment After Medicaid Expansion,” Psychiatric Services Epub ahead of print (March 2021), https://doi.org/10.1176/appi.ps.202000491 ↩︎
- Alex K. Gertner et al., “The Effect of Medicaid Expansion on Use of Opioid Agonist Treatment and the Role of Provider Capacity Constraints,” Health Services Research 55 no. 3 (June 2020): 383-392, https://doi.org/10.1111/1475-6773.13282 ↩︎
- George Pro et al., “The Role of State Medicaid Expansions in Integrating Comprehensive Mental Health Services into Opioid Treatment Programs: Differences Across the Rural/Urban Continuum,” Community Mental Health Journal Epub ahead of print (October 2020), https://doi.org/10.1007/s10597-020-00719-z ↩︎
- Amanda J. Abraham et al., “Medicaid Expansion and Availability of Opioid Medications in the Specialty Substance Use Disorder Treatment System,” Psychiatric Services 72 no. 2 (February 2021): 148-155: https://doi.org/10.1176/appi.ps.202000049 ↩︎
- Rahi Abouk, Lorens Helmchen, Ali Moghtaderi, and Jesse Pines, “The ACA Medicaid Expansions and Opioid Mortality: Is There a Link?,” Medical Care Research and Review Epub ahead of print (October 2020), https://doi.org/10.1177/1077558720967227 ↩︎
- Brandon W. Yan, Frank A. Sloan, W. John Boscardin, Felicia Guo, and R. Adams Dudley, “The Opioid Epidemic Blunted the Mortality Benefit of Medicaid Expansion,” Medical Care Research and Review Epub ahead of print (May 2020), https://journals.sagepub.com/doi/10.1177/1077558720919620 ↩︎
- Alisha Monnette, Charles Stoecker, Elizabeth Nauman, and Lizheng Shi, “The Impact of Medicaid Expansion on Access to Care and Preventative Care for Adults with Diabetes and Depression,” Journal of Diabetes and its Complications 34 no. 10 (October 2020), https://doi.org/10.1016/j.jdiacomp.2020.107663 ↩︎
- Elson Oshman Blunt, Johanna Catherine Maclean, Ioana Popovici, and Steven C. Marcus, “Public Insurance Expansions and Mental Health Care Availability,” Health Services Research 55 no. 4 (August 2020): 615-625, https://doi.org/10.1111/1475-6773.13311 ↩︎
- Amelia Harju and Jonathan Neufeld, “The Impact of Medicaid Expansion on Telemental Health Utilization in Four Midwestern States,” Telemedicine and e-Health Epub ahead of print (January 2021), https://www.liebertpub.com/doi/10.1089/tmj.2020.0476 ↩︎
- Benjamin W. Cowan and Zhuang Hao, Medicaid Expansion and the Mental Health of College Students (National Bureau of Economic Research, Working Paper No. 27306, June 2020), https://www.nber.org/papers/w27306 ↩︎
- George Pro, Jeff Utter, Shane Haberstroh, and Julie A. Baldwin, “Dual Mental Health Diagnoses Predict the Receipt of Medication-Assisted Opioid Treatment: Associations Moderated By State Medicaid Expansion Status, Race/Ethnicity and Gender, and Year,” Drug and Alcohol Dependence 209 (April 2020), https://doi.org/10.1016/j.drugalcdep.2020.107952 ↩︎
- Robert Rosales, David Takeuchi, and Rocío Calvo, “After the Affordable Care Act: the Effects of the Health Safety Net and the Medicaid Expansion on Latinxs’ Use of Behavioral Healthcare in the US,” The Journal of Behavioral Health Services & Research Epub ahead of print (June 2020), https://doi.org/10.1007/s11414-020-09715-3 ↩︎
- Joshua Breslau, Bing Han, Julie Lai, and Hao Yu, “Impact of the Affordable Care Act Medicaid Expansion on Utilization of Mental Health Care,” Medical Care 58 no. 9 (September 2020): 757-762, https://doi.org/10.1097/MLR.0000000000001373 ↩︎
- George Pro et al., “The Role of State Medicaid Expansions in Integrating Comprehensive Mental Health Services into Opioid Treatment Programs: Differences Across the Rural/Urban Continuum,” Community Mental Health Journal Epub ahead of print (October 2020), https://doi.org/10.1007/s10597-020-00719-z ↩︎
- Hefei Wen et. al, “Association Between Medicaid Expansion and Rates of Opioid-Related Hospital Use,” JAMA Internal Medicine 180 no. 5 (May 2020): 753-759, https://doi.org/10.1001/jamainternmed.2020.0473 ↩︎
- Rebecca Myerson, Samuel Crawford, Laura R. Wherry, “Medicaid Expansion Increased Preconception Health Counseling, Folic Acid Intake, And Postpartum Contraception,” Health Affairs 39 no. 11 (November 2020): 1883-1890, https://www.healthaffairs.org/doi/10.1377/hlthaff.2020.00106 ↩︎
- Melissa McInerney, Ruth Winecoff, Padmaja Ayyagari, Kosali Simon, and M. Kate Bundorf, “ACA Medicaid Expansion Associated With Increased Medicaid Participation and Improved Health Among Near-Elderly: Evidence From the Health and Retirement Study,” Inquiry: The Journal of Health Care Organization, Provision, and Financing 57 (July 2020): 1-10, https://doi.org/10.1177/0046958020935229 ↩︎
- Kevin N. Griffith and Jacob H. Bor, “Changes in Health Care Access, Behaviors, and Self-reported Health Among Low-income US Adults Through the Fourth Year of the Affordable Care Act,” Medical Care 58, no. 6 (June 2020): 574-578, https://doi.org/10.1097/MLR.0000000000001321 ↩︎
- Bryce Ward, The Impact of Medicaid Expansion on States’ Budgets (The Commonwealth Fund, May 2020), https://www.commonwealthfund.org/publications/issue-briefs/2020/may/impact-medicaid-expansion-states-budgets ↩︎
- Jonathan Gruber and Benjamin D. Sommers, Fiscal Federalism and the Budget Impacts of the Affordable Care Act’s Medicaid Expansion (National Bureau of Economic Research, Working Paper No. 26862, March 2020), https://www.nber.org/papers/w26862 ↩︎
- Madeline Guth, Bradley Corallo, Robin Rudowitz, and Rachel Garfield, Medicaid Expansion Enrollment and Spending Leading up to the COVID-19 Pandemic (Washington, DC: KFF, January 2021), https://modern.kff.org/medicaid/issue-brief/medicaid-expansion-enrollment-and-spending-leading-up-to-the-covid-19-pandemic/ ↩︎
- Brendan Saloner and Johanna Catherine Maclean, “Specialty Substance Use Disorder Treatment Admissions Steadily Increased In The Four Years After Medicaid Expansion,” Health Affairs 39 no. 3 (March 2020): 453–461, https://doi.org/10.1377/hlthaff.2019.01428 ↩︎
- Mark Borgschulte and Jacob VoglerbaI, “Did the ACA Medicaid Expansion Save Lives?,” Journal of Health Economics 72 (July 2020), https://doi.org/10.1016/j.jhealeco.2020.102333 ↩︎
- Saunders Lin, Karen J. Brasel, Ougni Chakraborty, and Sherry A. Glied, “Association Between Medicaid Expansion and the Use of Outpatient General Surgical Care Among US Adults in Multiple States,” JAMA Surgery 155 no. 11 (November 2020): 1058-1066, https://jamanetwork.com/journals/jamasurgery/article-abstract/2769588 ↩︎
- Justin Le Blanc, Danielle Heller, Ann Friedrich, Donald Lannin, and Tristen Park, “Association of Medicaid Expansion Under the Affordable Care Act With Breast Cancer Stage at Diagnosis,” JAMA Surgery (July 2020), https://doi.org/10.1001/jamasurg.2020.1495 ↩︎
- Adrian Diaz, Daniel Chavarin, Anghela Z. Paredes, and Timothy M. Pawlik, “Utilization of High-Volume Hospitals for High-Risk Cancer Surgery in California Following Medicaid Expansion,” Journal of Gastrointestinal Surgery Epub ahead of print (July 2020), https://link.springer.com/article/10.1007/s11605-020-04747-8 ↩︎
- Johanna Catherine Maclean, Michael T. Halpern, Steven C. Hill, and Michael F. Pesko, “The Effect of Medicaid Expansion on Prescriptions for Breast Cancer Hormonal Therapy Medications,” Health Services Research, 55 no. 3 (April 2020): 399-410, https://doi.org/10.1111/1475-6773.13289 ↩︎
- Tyler R. McClintock et al., “Association of Affordable Care Act-Related Medicaid Expansion with Variation in Utilization of Surgical Services,” The American Journal of Surgery, 220 no. 2 (August 2020): 441-447, https://doi.org/10.1016/j.amjsurg.2019.12.017 ↩︎
- Ali Moghtaderi et al., “The Three-Year Effect of Medicaid Expansion on Emergency Department Visits and Admissions,” Annals of Emergency Medicine An International Journal 77 no. 1, (January 2021): 76-81, https://doi.org/10.1016/j.annemergmed.2020.07.021 ↩︎
- Kathleen A. McManus, Karishma Srikanth, Samuel D. Powers, Rebecca Dillingham, and Elizabeth T. Rogawski McQuade, “Medicaid Expansion’s Impact on Human Immunodeficiency Virus Outcomes in a Nonurban Southeastern Ryan White HIV/AIDS Program Clinic,” Open Forum Infectious Diseases 8 no. 2 (February 2021), https://doi.org/10.1093/ofid/ofaa595 ↩︎
- Jamie Oh et al., “Impact of the Affordable Care Act’s Medicaid Expansion on Burn Outcomes and Disposition,” Burns 47 no. 1 (February 2021): 35-41, https://doi.org/10.1016/j.burns.2020.10.030 ↩︎
- Fredric Blavin and Christal Ramos, “Medicaid Expansion: Effects On Hospital Finances And Implications For Hospitals Facing COVID-19 Challenges,” Health Affairs 40 no. 1 (January 2021): 82-90, https://doi.org/10.1377/hlthaff.2020.00502 ↩︎
- Minji Sohn et al., “Association Between State Medicaid Expansion Status And Naloxone Prescription Dispensing” Health Services Research 55 no. 2 (February 2020): 239-248, https://doi.org/10.1111/1475-6773.13266 ↩︎
- Wafa W. Tarazi, “Associations Between Medicaid Expansion and Nurse Staffing Ratios and Hospital Readmissions,” Health Services Research 55 no. 3 (June 2020): 375-382, https://doi.org/10.1111/1475-6773.13273 ↩︎
- Brendan Saloner and Johanna Catherine Maclean, “Specialty Substance Use Disorder Treatment Admissions Steadily Increased In The Four Years After Medicaid Expansion,” Health Affairs 39 no. 3 (March 2020): 453–461, https://doi.org/10.1377/hlthaff.2019.01428 ↩︎
- Jason Tong et al., “The Impact of the Affordable Care Act on Surgeon Selection Amongst Colorectal Surgery Patients,” The American Journal of Surgery Epub ahead of print (February 2021), https://doi.org/10.1016/j.amjsurg.2021.01.041 ↩︎
- Erica M. Valdovinos, Matthew J. Niedzwiecki, Joanna Guo, and Renee Y. Hsia, “Effects of Medicaid Expansion on Access, Treatment and Outcomes for Patients with Acute Myocardial Infarction,” PLOS ONE 15 no. 4 (April 2020), https://doi.org/10.1371/journal.pone.0232097 ↩︎
- Erica M. Valdovinos, Matthew J. Niedzwiecki, Joanna Guo, and Renee Y. Hsia, “The Association of Medicaid Expansion and Racial/Ethnic Inequities in Access, Treatment, and Outcomes for Patients with Acute Myocardial Infarction,” PLOS ONE 15 no. 11 (November 2020), https://doi.org/10.1371/journal.pone.0241785 ↩︎
- Hefei Wen et. al, “Association Between Medicaid Expansion and Rates of Opioid-Related Hospital Use,” JAMA Internal Medicine 180 no. 5 (May 2020): 753-759, https://doi.org/10.1001/jamainternmed.2020.0473 ↩︎
- Monique Barakat et al., “Recent Trends and the Impact of the Affordable Care Act on Emergency Department Visits and Hospitalizations for Gastrointestinal, Pancreatic, and Liver Diseases,” Journal of Clinical Gastroenterology 54 no. 3 (March 2020), https://doi.org/10.1097/MCG.0000000000001102 ↩︎
- Ezra S. Brooks et al., “The Effects of the Affordable Care Act on Access and Outcomes of Colon Surgery,” The American Journal of Surgery Epub ahead of print (January 2021), https://doi.org/10.1016/j.amjsurg.2021.01.019 ↩︎
- Blair G. Darney et al., “Payment for Contraceptive Services in Safety Net Clinics: Roles of Affordable Care Act, Title X, and State Programs,” Medical Care 58 no. 5 (May 2020): 453-460, https://doi.org/10.1097/mlr.0000000000001309 ↩︎
- Scott R. Levin et al., “Association of Medicaid Expansion with Tunneled Dialysis Catheter Use at the Time of First Arteriovenous Access Creation,” Annals of Vascular Surgery Epub ahead of print (January 2021), https://www.annalsofvascularsurgery.com/article/S0890-5096(21)00082-0/fulltext ↩︎
- Pooja S. Yesantharao et al., “The Impact of Policy Reform on Utilization of Popular Reconstructive Procedures,” Annals of Plastic Surgery Epub ahead of print (December 2020), https://doi.org/10.1097/SAP.0000000000002608 ↩︎
- Laurent C. Glance, Caroline P. Thirukumaran, Ernie Shippey, Stewart J. Lustik, and Andrew W. Dick, “Impact of Medicaid Expansion on Disparities in Revascularization in Patients Hospitalized with Acute Myocardial Infarction,” PLOS One Epub ahead of print (December 2020), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0243385 ↩︎
- Lisa Marie Knowlton et al., “The Impact of Medicaid Expansion on Trauma-Related Emergency Department Utilization: A National Evaluation of Policy Implications,” The Journal of Trauma and Acute Care Surgery 88 no.1 (January 2020): 59-69, https://journals.lww.com/jtrauma/Abstract/2020/01000/The_impact_of_Medicaid_expansion_on_trauma_related.8.aspx ↩︎
- Uriel Kim, Siran Koroukian, Abby Statler, and Johnie Rose, “The Effect of Medicaid Expansion Among Adults from Low-Income Communities on Stage at Diagnosis in Those with Screening-Amenable Cancers,” Cancer 126, no. 18 (September 2020): 4209-4219, https://doi-org.proxy.library.cornell.edu/10.1002/cncr.32895 ↩︎
- Dan Kirkpatrick, Margaret Dunn, and Rebecca Tuttle, “Breast Cancer Stage at Presentation in Ohio: The Effect of Medicaid Expansion and the Affordable Care Act,” The American surgeon 86, no. 3 (2020): 195–199, https://pubmed.ncbi.nlm.nih.gov/32223797/ ↩︎
- Anne E.Larson, Megan Hoopes, Heather Angier, Miguel Marino, and Nathalie Huguet, “Private/marketplace Insurance in Community Health Centers 5 years Post-Affordable Care Act in Medicaid Expansion and Non-Expansion States,” Preventive Medicine 141 Epub ahead of print (December 2020), https://doi.org/10.1016/j.ypmed.2020.106271 ↩︎
- Mark Olfson, Victoria Shu Zhang, Marissa King, and Ramin Mojtabai, “Changes in Buprenorphine Treatment After Medicaid Expansion,” Psychiatric Services Epub ahead of print (March 2021), https://doi.org/10.1176/appi.ps.202000491 ↩︎
- Paula Chatterjee, Mingyu Qi, and Rachel M. Werner, “Association of Medicaid Expansion With Quality in Safety-Net Hospitals,” JAMA Internal Medicine Epub ahead of print (February 2021), https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2775956 ↩︎
- Ali Moghtaderi, Jesse Pines, Mark Zocchi, and Bernard Black, “The Effect of Affordable Care Act Medicaid Expansion on Hospital Revenue,” Health Economics 29 no. 12 (December 2020): 1682-1704, https://doi.org/10.1002/hec.4157 ↩︎
- Kevin Callison, Brigham Walker, Charles Stoecker, Jeral Self, and Mark L. Diana, “Medicaid Expansion Reduced Uncompensated Care Costs At Louisiana Hospitals; May Be A Model For Other States,” Health Affairs 40 no. 3 (March 2020): 529-535, https://doi.org/10.1377/hlthaff.2020.01677 ↩︎
- Charles Stoecker, Mollye Demosthenidy, Yixue Shao, and Hugh Long, “Association of Nonprofit Hospitals’ Charitable Activities With Unreimbursed Medicaid Care After Medicaid Expansion,” JAMA Network Open 3 no. 2 (February 2020), https://doi.org/10.1001/jamanetworkopen.2020.0012 ↩︎
- Kim Andrew and Zhao Liang, “Examining the Effects of the Medicaid Expansion on Uncompensated Care and DSH Payments,” Journal of Allied Health 49 no. 4 (Winter, 2020): 274-278, https://www.ingentaconnect.com/contentone/asahp/jah/2020/00000049/00000004/art00009?crawler=true&mimetype=application/pdf ↩︎
- Paula Chatterjee, Mingyu Qi, and Rachel M. Werner, “Association of Medicaid Expansion With Quality in Safety-Net Hospitals,” JAMA Internal Medicine Epub ahead of print (February 2021), https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2775956 ↩︎
- Lisa Marie Knowlton et al., “The Impact of Medicaid Expansion on Trauma-Related Emergency Department Utilization: A National Evaluation of Policy Implications,” The Journal of Trauma and Acute Care Surgery 88 no.1 (January 2020): 59-69, https://journals.lww.com/jtrauma/Abstract/2020/01000/The_impact_of_Medicaid_expansion_on_trauma_related.8.aspx ↩︎
- Brad Wright et al., “Iowa’s Medicaid Healthy Behaviors Program Associated With Reduced Hospital-Based Care But Higher Spending, 2012–17,” Health Affairs 39 no. 5 (May 2020), https://www.healthaffairs.org/doi/10.1377/hlthaff.2019.01145 ↩︎
- Molly O’Malley Watts, MaryBeth Musumeci, and Priya Chidambaram, State Variation in Medicaid LTSS Policy Choices and Implications for Upcoming Policy Debates (Washington, DC: KFF, February 2021), https://modern.kff.org/report-section/state-variation-in-medicaid-ltss-policy-choices-and-implications-for-upcoming-policy-debates-issue-brief/ ↩︎
- Andrew Sumarsono et al., “Medicaid Expansion and Utilization of Antihyperglycemic Therapies,” Diabetes Care 43 no. 11, (November 2020): 2684-2690, https://care.diabetesjournals.org/content/43/11/2684 ↩︎
- Genevieve P. Kanter, Bardia Nabet, Meredith Matone, and David M. Rubin, “Association of State Medicaid Expansion With Hospital Community Benefit Spending,” Jama Network Open 3 no. 5 (May 2020), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2766544 ↩︎
- Fredric Blavin and Christal Ramos, “Medicaid Expansion: Effects On Hospital Finances And Implications For Hospitals Facing COVID-19 Challenges,” Health Affairs 40 no. 1 (January 2021): 82-90, https://doi.org/10.1377/hlthaff.2020.00502 ↩︎
- Ali Moghtaderi, Jesse Pines, Mark Zocchi, and Bernard Black, “The Effect of Affordable Care Act Medicaid Expansion on Hospital Revenue,” Health Economics 29 no. 12 (December 2020): 1682-1704, https://doi.org/10.1002/hec.4157 ↩︎
- Charles Stoecker, Mollye Demosthenidy, Yixue Shao, and Hugh Long, “Association of Nonprofit Hospitals’ Charitable Activities With Unreimbursed Medicaid Care After Medicaid Expansion,” JAMA Network Open 3 no. 2 (February 2020), https://doi.org/10.1001/jamanetworkopen.2020.0012 ↩︎
- Tyler L. Malone, George H. Pink, and George M. Holmes, “Decline in Inpatient Volume at Rural Hospitals,” The Journal of Rural Health Epub ahead of print (December 2020), https://doi.org/10.1111/jrh.12553 ↩︎
- David J. Wallace et al., “Association Between State Medicaid Expansion and Emergency Access to Acute Care Hospitals in the United States,” JAMA Network Open 3 no. 11 (November 2020), https://doi.org/10.1001/jamanetworkopen.2020.25815 ↩︎
- Archana Babu et al., “The Affordable Care Act: Implications for Underserved Populations with Head & Neck Cancer,” American Journal of Otolaryngology 41, no. 4 (July-August 2020), https://doi.org/10.1016/j.amjoto.2020.102464 ↩︎
- David Barrington et. al., “Where You Live Matters: A National Cancer Database Study of Medicaid Expansion and Endometrial Cancer Outcomes,” Gynecologic Oncology 158 no. 2 (August 2020): 407-414, https://doi.org/10.1016/j.ygyno.2020.05.018 ↩︎
- Thomas Buchmueller and Helen Levy, “The ACA’s Impact On Racial And Ethnic Disparities In Health Insurance Coverage And Access To Care,” Health Affairs 39, no. 3 (March 2020): 395-402, https://doi.org/10.1377/hlthaff.2019.01394 ↩︎
- Munira Z. Gunja et al, Gap Closed: The Affordable Care Act’s Impact on Asian Americans’ Health Coverage (The Commonwealth Fund, July 2020), https://www.commonwealthfund.org/publications/issue-briefs/2020/jul/gap-closed-aca-impact-asian-american-coverage ↩︎
- Anuj Gangopadhyaya and Emily M. Johnston, Impacts of the ACA’s Medicaid Expansion on Health Insurance Coverage and Health Care Access among Young Adults (Washington, D.C: The Urban Institute, February 21, 2021), https://www.urban.org/research/publication/impacts-acas-medicaid-expansion-health-insurance-coverage-and-health-care-access-among-young-adults/view/full_report ↩︎
- Hawazin W. Elani, Benjamin D. Sommers, and Ichiro Kawachi, “Changes In Coverage And Access To Dental Care Five Years After ACA Medicaid Expansion,” Health Affairs 39 no. 11 (November 2020): 1900-1908, https://doi.org/10.1377/hlthaff.2020.00386 ↩︎
- Wei Ye, and Javier M. Rodriguez, “Highly Vulnerable Communities and the Affordable Care Act: Health Insurance Coverage Effects, 2010–2018,” Social Science and Medicine 270 (February 2021), https://doi.org/10.1016/j.socscimed.2021.113670 ↩︎
- Benjamin B. Albright et al., “Impact of Medicaid Expansion on Women with Gynecologic Cancer: a Difference-in-Difference Analysis,” American Journal of Obstetrics and Gynecology 224 no. 2 (February 2021): 1-17, https://doi.org/10.1016/j.ajog.2020.08.007 ↩︎
- Barbara H. Braffett, “Health Care Coverage and Glycemic Control in Young Adults With Youth-Onset Type 2 Diabetes: Results From the TODAY2 Study,” Diabetes Care 43, no. 10 (October 2020): 2469-2477, https://doi.org/10.2337/dc20-0760 ↩︎
- Hyungjung Lee, Dominic Hodgkin, Michael P. Johnson, and Frank P. Worell, “Medicaid Expansion and Racial and Ethnic Disparities in Access to Health Care: Applying the National Academy of Medicine Definition of Health Care Disparities,” The Journal of Healthcare Organization, Provision, and Financing Epub ahead of print. (February 2021), https://journals.sagepub.com/doi/10.1177/0046958021991293 ↩︎
- Janani Rajbhandari-Thappa, Donglang Zhang, Kara E. MacLeod, Kiran Thapa, “Impact of Medicaid Expansion on Insurance Coverage Rates Among Adult Populations with Low Income and by Obesity Status” The Obesity Society 28 no. 7 (April 2020): 1219-1223, https://doi.org/10.1002/oby.22793 ↩︎
- Hyungjung Lee, Dominic Hodgkin, Michael P. Johnson, and Frank P. Worell, “Medicaid Expansion and Racial and Ethnic Disparities in Access to Health Care: Applying the National Academy of Medicine Definition of Health Care Disparities,” The Journal of Healthcare Organization, Provision, and Financing Epub ahead of print. (February 2021), https://journals.sagepub.com/doi/10.1177/0046958021991293 ↩︎
- Nosayaba Osazuwa-Peters et al., “State Medicaid Expansion Status, Insurance Coverage and Stage at Diagnosis in Head and Neck Cancer Patients,” Oral Oncology 110 (November 2020), https://doi.org/10.1016/j.oraloncology.2020.104870 ↩︎
- Archana Babu et al., “The Affordable Care Act: Implications for Underserved Populations with Head & Neck Cancer,” American Journal of Otolaryngology 41, no. 4 (July-August 2020), https://doi.org/10.1016/j.amjoto.2020.102464 ↩︎
- Anitha Menon, Payal K. Patel, Monita Karmakar, and Renuka Tipirneni, “The Impact of the Affordable Care Act Medicaid Expansion on Racial/Ethnic and Sex Disparities in HIV Testing: National Findings fromthe Behavioral Risk Factor Surveillance System,” Journal of General Internal Medicine Epub ahead of print (January 2021), https://doi.org/10.1007/s11606-021-06590-2 ↩︎
- Laurent C. Glance, Caroline P. Thirukumaran, Ernie Shippey, Stewart J. Lustik, and Andrew W. Dick, “Impact of Medicaid Expansion on Disparities in Revascularization in Patients Hospitalized with Acute Myocardial Infarction,” PLOS One Epub ahead of print (December 2020), https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0243385 ↩︎
- Makayla Palmer, “Preconception Subsidized Insurance: Prenatal Care and Birth Outcomes by Race/Ethnicity,” Health Economics 29 no. 9 (September 2020): 1013-1030, https://doi.org/10.1002/hec.4116 ↩︎
- Scott R. Levin et al., “Association of Medicaid Expansion with Tunneled Dialysis Catheter Use at the Time of First Arteriovenous Access Creation,” Annals of Vascular Surgery Epub ahead of print (January 2021), https://www.annalsofvascularsurgery.com/article/S0890-5096(21)00082-0/fulltext ↩︎
- Erica M. Valdovinos, Matthew J. Niedzwiecki, Joanna Guo, and Renee Y. Hsia, “The Association of Medicaid Expansion and Racial/Ethnic Inequities in Access, Treatment, and Outcomes for Patients with Acute Myocardial Infarction,” PLOS ONE 15 no. 11 (November 2020), https://doi.org/10.1371/journal.pone.0241785 ↩︎
- Clare Brown, Jennifer Moore, Felix Holly, Kathryn Stewart, and Mick Tilford, “County-level Variation in Low Birthweight and Preterm Birth: An Evaluation of State Medicaid Expansion Under the Affordable Care Act,” Medical Care 58, no. 6 (June 2020): 497-503, https://doi.org/10.1097/mlr.0000000000001313 ↩︎
- Miguel Marino et al., “Disparities in Biomarkers for Patients With Diabetes After the Affordable Care Act,” Medical Care 58 (June 2020), https://doi.org/10.1097/mlr.0000000000001257 ↩︎
- Minal R. Patel et al., “Examination of Changes in Health Status Among Michigan Medicaid Expansion Enrollees From 2016 to 2017,” JAMA Network Open 3, no. 7 (July 2020), https://doi.org/10.1001/jamanetworkopen.2020.8776 ↩︎
- S. Marie Harvey et al., “Impact of Medicaid Expansion in Oregon on Access to Prenatal Care,” Preventative Medicine 143 (February 2021), https://www.sciencedirect.com/science/article/abs/pii/S0091743520303911?via%3Dihub ↩︎
- Robert Rosales, David Takeuchi, and Rocío Calvo, “After the Affordable Care Act: the Effects of the Health Safety Net and the Medicaid Expansion on Latinxs’ Use of Behavioral Healthcare in the US,” The Journal of Behavioral Health Services & Research Epub ahead of print (June 2020), https://doi.org/10.1007/s11414-020-09715-3 ↩︎
- Lauren D. Nephew et al., “Association of State Medicaid Expansion with Racial/Ethnic Disparities in Liver Transplant Wait-listing in the United States,” Jama Network Open 3 no. 10 (October 2020), https://doi.org/10.1001/jamanetworkopen.2020.19869 ↩︎
- Benjamin W. Cowan and Zhuang Hao, Medicaid Expansion and the Mental Health of College Students (National Bureau of Economic Research, Working Paper No. 27306, June 2020), https://www.nber.org/papers/w27306 ↩︎
- Khadijah Breathett et al., “Is the Affordable Care Act Medicaid Expansion Linked to Change in Rate of Ventricular Assist Device Implantation for Blacks and Whites?” Circulation: Heart Failure 13, no. 4 (April 2020), https://doi.org/10.1161/CIRCHEARTFAILURE.119.006544 ↩︎
- Lauren D. Nephew et al., “Association of State Medicaid Expansion with Racial/Ethnic Disparities in Liver Transplant Wait-listing in the United States,” Jama Network Open 3 no. 10 (October 2020), https://doi.org/10.1001/jamanetworkopen.2020.19869 ↩︎
- Afshin Ehsan et al., “Cardiac Surgery Utilization Across Vulnerable Persons After Medicaid Expansion,” (2020), The Annals of Thoracic Surgery Epub ahead of print (November 2020), https://doi.org/10.1016/j.athoracsur.2020.08.066 ↩︎
- Adrian Diaz, Daniel Chavarin, Anghela Z. Paredes, and Timothy M. Pawlik, “Utilization of High-Volume Hospitals for High-Risk Cancer Surgery in California Following Medicaid Expansion,” Journal of Gastrointestinal Surgery Epub ahead of print (July 2020), https://link.springer.com/article/10.1007/s11605-020-04747-8 ↩︎
- Saunders Lin, Karen J. Brasel, Ougni Chakraborty, and Sherry A. Glied, “Association Between Medicaid Expansion and the Use of Outpatient General Surgical Care Among US Adults in Multiple States,” JAMA Surgery 155 no. 11 (November 2020): 1058-1066, https://jamanetwork.com/journals/jamasurgery/article-abstract/2769588 ↩︎
- Adam B. Weiner et al., “Changes in Prostate-Specific Antigen at the Time of Prostate Cancer Diagnosis After Medicaid Expansion in Young Men,” Cancer 126 no. 14 (July 2020): 3229-3236, https://doi.org/10.1002/cncr.32930 ↩︎
- Justin Le Blanc, Danielle Heller, Ann Friedrich, Donald Lannin, and Tristen Park, “Association of Medicaid Expansion Under the Affordable Care Act With Breast Cancer Stage at Diagnosis,” JAMA Surgery (July 2020), https://doi.org/10.1001/jamasurg.2020.1495 ↩︎
- Erica Eliason, “Adoption of Medicaid Expansion Is Associated with Lower Maternal Mortality,” Women’s Health Issues 30, no. 3 (May-June 2020): 147-152, https://doi.org/10.1016/j.whi.2020.01.005 ↩︎
- Alexandra Wiggins, Ibraheem M. Karaye, Jennifer A. Horney, “Medicaid Expansion and Infant Mortality, Revisited: A Difference-In-Differences Analysis,” Health Services Research 55, no. 3 (March 2020): 393-398, https://doi.org/10.1111/1475-6773.13286 ↩︎
- Amanda Cooke and Amanda Stype, “Medicaid Expansion and Infant Mortality: The (Questionable) Impact of the Affordable Care Act,” Journal of Epidemiology and Community Health 75 no. 1 (January 2021): 10-15, http://dx.doi.org/10.1136/jech-2019-213666 ↩︎
- Jason Semprini, Olufunmilayo Olopade, “Evaluating the Effect of Medicaid Expansion on Black/White Breast Cancer Mortality Disparities: A Difference-in-Difference Analysis.” JCO Global Oncology no. 6, (July 2020): 1178-1183, https://doi.org/10.1200/GO.20.00068 ↩︎
- Miranda B. Lam, Jessica Phelan, John Orav, Ashish K. Jha, and Nancy L. Keating, “Medicaid Expansion and Mortality Among Patients With Breast, Lung, and Colorectal Cancer,” Jama Network Open 3 no. 11 (November 2020), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2772535 ↩︎
- Matthew Buettgens, Fredric Blavin, and Clare Pan, “The Affordable Care Act Reduced Income Inequality In The US,” Health Affairs 40 no. 1(January 2021): 121-129, https://doi.org/10.1377/hlthaff.2019.00931 ↩︎
- Benjamin W. Cowan and Zhuang Hao, Medicaid Expansion and the Mental Health of College Students (National Bureau of Economic Research, Working Paper No. 27306, June 2020), https://www.nber.org/papers/w27306 ↩︎
- Afshin Ehsan et al., “Cardiac Surgery Utilization Across Vulnerable Persons After Medicaid Expansion,” (2020), The Annals of Thoracic Surgery Epub ahead of print (November 2020), https://doi.org/10.1016/j.athoracsur.2020.08.066 ↩︎
- Matthew Buettgens, Fredric Blavin, and Clare Pan, “The Affordable Care Act Reduced Income Inequality In The US,” Health Affairs 40 no. 1(January 2021): 121-129, https://doi.org/10.1377/hlthaff.2019.00931 ↩︎
- Heather Angier et al., “Role of Health Insurance and Neighborhood-Level Social Deprivation on Hypertension Control Following the Affordable Care Act Health Insurance Opportunities,” Social Science & Medicine 265 Epub ahead of print (November 2020), https://doi.org/10.1016/j.socscimed.2020.113439 ↩︎
- Anuj Gangopadhyaya and Emily M. Johnston, Impacts of the ACA’s Medicaid Expansion on Health Insurance Coverage and Health Care Access among Young Adults (Washington, D.C: The Urban Institute, February 21, 2021), https://www.urban.org/research/publication/impacts-acas-medicaid-expansion-health-insurance-coverage-and-health-care-access-among-young-adults/view/full_report ↩︎
- Francesco Renna, Kosteas D. Vasilios, Dinkar Kuchibotla, “Inequality in Health Insurance Coverage Before and After the Affordable Care Act,” Health Economics 30 no. 2 (November 2020): 384-402, https://doi.org/10.1002/hec.4195 ↩︎
- Nosayaba Osazuwa-Peters et al., “State Medicaid Expansion Status, Insurance Coverage and Stage at Diagnosis in Head and Neck Cancer Patients,” Oral Oncology 110 (November 2020), https://doi.org/10.1016/j.oraloncology.2020.104870 ↩︎
- Benjamin B. Albright et al., “Impact of Medicaid Expansion on Women with Gynecologic Cancer: a Difference-in-Difference Analysis,” American Journal of Obstetrics and Gynecology 224 no. 2 (February 2021): 1-17, https://doi.org/10.1016/j.ajog.2020.08.007 ↩︎
- Jeffrey Clemens, Drew McNichols, and Joseph J. Sabia, The Long-Run Effects of the Affordable Care Act: A Pre-Committed Research Design Over the COVID-19 Recession and Recovery (National Bureau of Economic Research, Working Paper No. 27999, October 2020), https://www.nber.org/papers/w27999 ↩︎
- Jean Guglielminotti, Ruth Landau, and Guohua Li, “The 2014 New York States Medicaid Expansion and Severe Maternal Morbidity,” Anesthesia and Analgesia 10 (January 2021), https://journals.lww.com/anesthesia-analgesia/Abstract/9900/The_2014_New_York_State_Medicaid_Expansion_and.64.aspx ↩︎
- Janani Rajbhandari-Thappa, Donglang Zhang, Kara E. MacLeod, Kiran Thapa, “Impact of Medicaid Expansion on Insurance Coverage Rates Among Adult Populations with Low Income and by Obesity Status” The Obesity Society 28 no. 7 (April 2020): 1219-1223, https://doi.org/10.1002/oby.22793 ↩︎
- Barbara H. Braffett, “Health Care Coverage and Glycemic Control in Young Adults With Youth-Onset Type 2 Diabetes: Results From the TODAY2 Study,” Diabetes Care 43, no. 10 (October 2020): 2469-2477, https://doi.org/10.2337/dc20-0760 ↩︎
- Hawazin W. Elani, Benjamin D. Sommers, and Ichiro Kawachi, “Changes In Coverage And Access To Dental Care Five Years After ACA Medicaid Expansion,” Health Affairs 39 no. 11 (November 2020): 1900-1908, https://doi.org/10.1377/hlthaff.2020.00386 ↩︎
- Nosayaba Osazuwa-Peters et al., “State Medicaid Expansion Status, Insurance Coverage and Stage at Diagnosis in Head and Neck Cancer Patients,” Oral Oncology 110 (November 2020), https://doi.org/10.1016/j.oraloncology.2020.104870 ↩︎
- Terceira Ann Berdahl and Asako Moriya, “Insurance Coverage for Non-standard Workers: Experiences of Temporary Workers, Freelancers, and Part-time Workers in the USA, 2010-2017,” Journal of General Internal Medicine Epub ahead of print (March 2021): 1-7, https://doi.org/10.1007/s11606-021-06700-0 ↩︎
- Janani Rajbhandari-Thappa, Donglang Zhang, Kara E. MacLeod, Kiran Thapa, “Impact of Medicaid Expansion on Insurance Coverage Rates Among Adult Populations with Low Income and by Obesity Status” The Obesity Society 28 no. 7 (April 2020): 1219-1223, https://doi.org/10.1002/oby.22793 ↩︎
- Matthew Buettgens, Fredric Blavin, and Clare Pan, “The Affordable Care Act Reduced Income Inequality In The US,” Health Affairs 40 no. 1(January 2021): 121-129, https://doi.org/10.1377/hlthaff.2019.00931 ↩︎
- Anitha Menon, Payal K. Patel, Monita Karmakar, and Renuka Tipirneni, “The Impact of the Affordable Care Act Medicaid Expansion on Racial/Ethnic and Sex Disparities in HIV Testing: National Findings fromthe Behavioral Risk Factor Surveillance System,” Journal of General Internal Medicine Epub ahead of print (January 2021), https://doi.org/10.1007/s11606-021-06590-2 ↩︎
- Bita Fayaz Farkhad, David R. Holtgrave, and Dolores Albarracín, “Effect of Medicaid Expansions on HIV Diagnoses and Pre-Exposure Prophylaxis Use,” American Journal of Preventive Medicine Epub ahead of print (January 2021), https://doi.org/10.1016/j.amepre.2020.10.021 ↩︎
- George Pro et al., “The Role of State Medicaid Expansions in Integrating Comprehensive Mental Health Services into Opioid Treatment Programs: Differences Across the Rural/Urban Continuum,” Community Mental Health Journal Epub ahead of print (October 2020), https://doi.org/10.1007/s10597-020-00719-z ↩︎
- Matthew Dalstrom, Laurence G. Weinzimmer, Roopa Foulger, and Colleen J. Klein, “Medicaid Expansion and Accessibility to Healthcare: The Illinois Experience,” Public Health Nursing Epub ahead of print (March 2021), https://doi.org/10.1111/phn.12899 ↩︎
- Amie Goodin, Jeffery Talbert, Patricia R. Freeman, Ellen J. Hahn, and Amanda Fallin-Bennett, “Appalachian Disparities in Tobacco Cessation Treatment Utilization in Medicaid,” Substance Abuse Treatment, Prevention, and Policy 15, no. 5 (January 2020), https://doi.org/10.1186/s13011-020-0251-0 ↩︎
- Kevin Callison, Brigham Walker, Charles Stoecker, Jeral Self, and Mark L. Diana, “Medicaid Expansion Reduced Uncompensated Care Costs At Louisiana Hospitals; May Be A Model For Other States,” Health Affairs 40 no. 3 (March 2020): 529-535, https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2020.01677?journalCode=hlthaff ↩︎
- Ali Moghtaderi, Jesse Pines, Mark Zocchi, and Bernard Black, “The Effect of Affordable Care Act Medicaid Expansion on Hospital Revenue,” Health Economics 29 no. 12 (December 2020): 1682-1704, https://doi.org/10.1002/hec.4157 ↩︎
- Fredric Blavin and Christal Ramos, “Medicaid Expansion: Effects On Hospital Finances And Implications For Hospitals Facing COVID-19 Challenges,” Health Affairs 40 no. 1 (January 2021): 82-90, https://doi.org/10.1377/hlthaff.2020.00502 ↩︎
- Tyler L. Malone, George H. Pink, George M. Holmes, “Decline in Inpatient Volume at Rural Hospitals,” The Journal of Rural Health Epub ahead of print (December 2020), https://onlinelibrary.wiley.com/doi/10.1111/jrh.12553 ↩︎
- Genevieve P. Kanter, Bardia Nabet, Meredith Matone, and David M. Rubin, “Association of State Medicaid Expansion With Hospital Community Benefit Spending,” Jama Network Open 3 no. 5 (May 2020), https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2766544 ↩︎
- Charles Liu, Yusuke Tsugawa, and Thomas J Weiser, “Association of the US Affordable Care Act With Out-of-Pocket Spending and Catastrophic Health Expenditures Among Adult Patients With Traumatic Injury,” Jama Network Open 3 no.2 (February 2020): 1-12, https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2762020 ↩︎
- Hiroshi Gotanda, Ashish K Jha, Gerald F Kominski, and Yusuke Tsugawa, “Out-of-pocket spending and financial burden among low income adults after Medicaid expansions in the United States: quasi-experimental difference-in-difference study,” BMJ 368 (February 2020), https://doi.org/10.1136/bmj.m40 ↩︎
- Matthew Buettgens, Fredric Blavin, and Clare Pan, “The Affordable Care Act Reduced Income Inequality In The US,” Health Affairs 40 no. 1(January 2021): 121-129, https://doi.org/10.1377/hlthaff.2019.00931 ↩︎
- Michael W. Sances and Andrea Louise Campbell, “State Policy and Mental Health Outcomes under COVID-19” Journal of Health Politics, Policy, and Law Epub ahead of print (March 2021), https://doi.org/10.1215/0361678-9155991 ↩︎
- Purvi Sevak and Jodi Schimmel Hyde, “The ACA Medicaid Expansions and Employment of Adults With Disabilities,” Journal of Disability Policy Studies Epub ahead of print (July 2020), https://doi.org/10.1177/1044207320943554 ↩︎
- Bradley Heim, Ithai Lurie, Kathleen J.Mullen, and Kosali Simon, “How Much Do Outside Options Matter? The Effect of Subsidized Health Insurance on Social Security Disability Insurance Benefit Receipt,” Journal of Health Economics 76 Epub ahead of print (January 2021), https://doi.org/10.1016/j.jhealeco.2021.102437 ↩︎
- Ryan Yeung, “The Effect of the Medicaid Expansion on Dropout Rates,” Journal of School Health 90 no. 10 (August 2020): 745-753, https://onlinelibrary.wiley.com/doi/10.1111/josh.12937 ↩︎
- Tyler N. A. Winkelman et al., “Medications for Opioid Use Disorder among Pregnant Women Referred by Criminal Justice Agencies before and after Medicaid Expansion: A Retrospective Study of Admissions to Treatment Centers in the United States,” PLOS Medicine 17 no. 5 (May 2020), https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1003119 ↩︎
- Carrie E. Fry, Thomas G. McGuire, and Richard G. Frank, “Medicaid Expansion’s Spillover to the Criminal Justice System: Evidence from Six Urban Counties,” RSF: The Russell Sage Foundation Journal of the Social Sciences 6 no. 2 (July 2020): 244-263, https://www.jstor.org/stable/10.7758/rsf.2020.6.2.11 ↩︎
- Jeral Self, Kevin Callison, Anthony Goudie, Kanna Lewis, and Joseph Thompson, “Medicaid Expansion And Health Services Use For Adults Experiencing Homelessness In Arkansas,” Health Affairs 40 no. 1 (January 2021): 91-97, https://doi.org/10.1377/hlthaff.2019.01812 ↩︎