Women’s Sexual and Reproductive Health Services: Key Findings from the 2017 Kaiser Women’s Health Survey
Issue Brief
Introduction
Reproductive and sexual health is an integral component of women’s general health and well-being. The ACA has afforded more women the opportunity to seek and obtain reproductive health care by expanding access to Medicaid and affordable coverage. In addition, the law requires than plans cover a broad range of recommended preventive services including contraceptive care and STI screening services without cost sharing, critical elements of women’s health care. Plans were required to offer no-cost coverage for prescription contraceptives to women with private insurance starting in August 2012. Coverage for other preventive services, such as counseling and testing for STIs, are also now required benefits in private insurance plans and covered by Medicaid in most states. Women have a choice of providers, and while most seek care at private doctors’ offices, a substantial share go to clinics that are Medicaid participating providers such as community health centers and Planned Parenthood clinics for their reproductive and sexual health care.
This brief presents selected findings from the 2017 Kaiser Women’s Health Survey, a nationally representative survey of women conducted in the summer and fall of 2017. The survey also covered a wide range of topics related to women’s coverage, use, access, and experiences with the health care system. This brief presents survey findings on coverage and use of reproductive and sexual health services among women ages 18 to 44 years old. The data presented is from the newest 2017 survey, but some findings presented in this brief include trends from earlier surveys that the Kaiser Family Foundation conducted in 2004, 2008, and 2013.
Use of Contraceptives
Nearly one in five sexually active women of reproductive age report that they are not using contraception, despite reporting that they do not want to become pregnant.
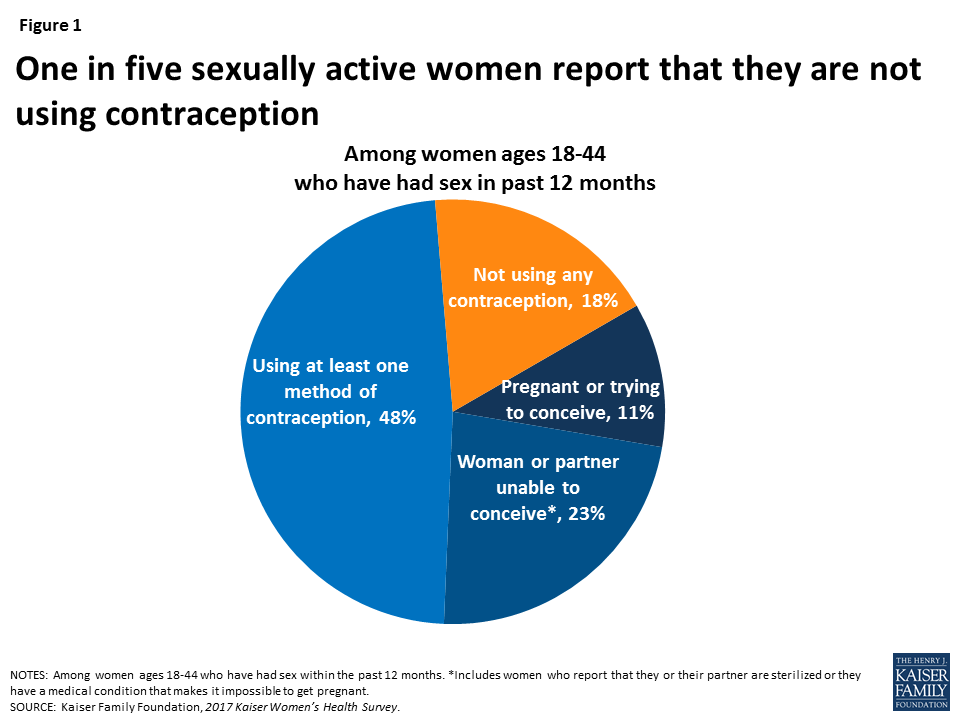
For women with reproductive capacity, but who want to avoid an unintended pregnancy, contraception is an essential health service. An estimated 18% of sexually active women ages 18 to 44, however, are not using contraception and are at high risk for unintended pregnancy (Figure 1). Among reproductive-age women who have had sex in the past year, half (48%) report that they or their partners used at least one reversible contraceptive method. One in ten (11%) are pregnant or trying to conceive, and nearly a quarter (23%) of women report that they or their partners have had a sterilization procedure or cannot become pregnant.
Women who do not use contraception are more likely to be low-income than women who use contraception.
Among sexually active women who are not pregnant or actively trying to conceive, almost half (46%) are low-income, compared to about a third (34%) of women who do use contraception or have had a sterilization (Table 1). However, in some ways, women at risk for unintended pregnancy are similar to women who do use contraception. There are no significant differences in age composition, insurance coverage, or race/ethnicity between the two groups.
| Table 1: Characteristics of sexually active women who use contraception compared to those who do not use contraception and do not want to be pregnant | ||
| Use Contraceptives (woman or partner used contraceptives) | Do not use contraceptives (at high risk for unintended pregnancy) | |
| Characteristics: | ||
| Age Group | ||
| 18-24 years | 18% | 24% |
| 25-44 years | 82% | 76% |
| Race/Ethnicity | ||
| White | 57% | 53% |
| Black | 12% | 16% |
| Latina | 22% | 21% |
| Insurance Type | ||
| Private | 65% | 62% |
| Medicaid | 16% | 15% |
| Uninsured | 12% | 15% |
| Poverty Level | ||
| <200% FPL | 34% | 46%* |
| >200% FPL | 66% | 54%* |
| NOTES: Among women ages 18-44 who were sexually active in past year and say they were not pregnant or trying to get pregnant. Race/Ethnicity and Insurance columns do not sum to 100% because respondents identifying as “Other Non-Hispanic” or stating “Other Public” coverage not shown. The Federal Poverty Level (FPL) was $20,420 for a family of three in 2017. *Indicates a statistically significant difference from Use Contraceptives; p<.05.SOURCE: Kaiser Family Foundation, 2017 Kaiser Women’s Health Survey. | ||
Condoms and oral contraceptives are the most commonly used forms of contraception.
While all forms of FDA approved contraception can reduce the risk of unintended pregnancy when used correctly, they vary in their use and effectiveness. Women are encouraged to consider a range of issues when choosing a contraceptive method in order to find the one that is most effective but also fits best within their beliefs and lifestyle. Condoms can protect against STIs and are widely available through many outlets without a prescription. Oral contraceptives, often referred to as the Pill, require prescriptions and are hormonal, and therefore cannot be used or tolerated by all women. Other methods include injectables, implants, patches, and the vaginal ring, which deliver different doses of hormones. Intrauterine Devices (IUD) are devices that are inserted into a woman’s uterus by a provider and some types also include hormones. They can last up to 5 years or longer and are among the most effective methods of reversible contraception. Under the ACA’s preventive services provision, most private plans are required to cover each of the 18 FDA-approved methods of contraception as prescribed for women without cost sharing. Medicaid also prohibits cost-sharing for all family planning services.
Among sexually active women who use contraception, just over half (57%) rely on one method and just under half (42%) use more than one method. Women most frequently report that they have used condoms or birth control pills in the past year, a rate that has remained consistent since 2013. Nearly six in ten (59%) sexually active women who have used contraceptives in the past year report using male condoms, four in ten (40%) have used oral contraceptive pills, and about one in five (24%) used an IUD (Table 2). Younger women ages 18-24 rely on the pill (60%) or condoms (79%) at greater rates than those who are 25 and older.
| Table 2: Types of contraceptives women report they or partners used in past 12 months, by age | ||||
| All Women | Age Group | |||
| Types of contraception used within the past 12 months | 18-24 | 25-34 | 35-44 | |
| Male condoms | 59% | 79% | 56%* | 48%* |
| Oral contraceptives | 40% | 60% | 34%* | 34%* |
| IUD | 24% | 16% | 27% | 25% |
| Injectables | 9% | 13% | 9% | 5% |
| Implants | 8% | 14% | 7% | 4% |
| Other | 10% | 13% | 11% | 8% |
| NOTES: Among women ages 18-44 who were sexually active in past year and used contraceptives in past year. Women may use more than one form of contraception. Oral contraceptives include birth control pills. IUD is an intrauterine device such as Mirena, Skyla, or Paragard. Injectables include Depo-Provera. Implants include Implanon or tubes in arm. Other methods include vaginal ring and the topical patch. *Indicates a statistically significant difference from 18-24; p<.05.SOURCE: Kaiser Family Foundation, 2017 Kaiser Women’s Health Survey. | ||||
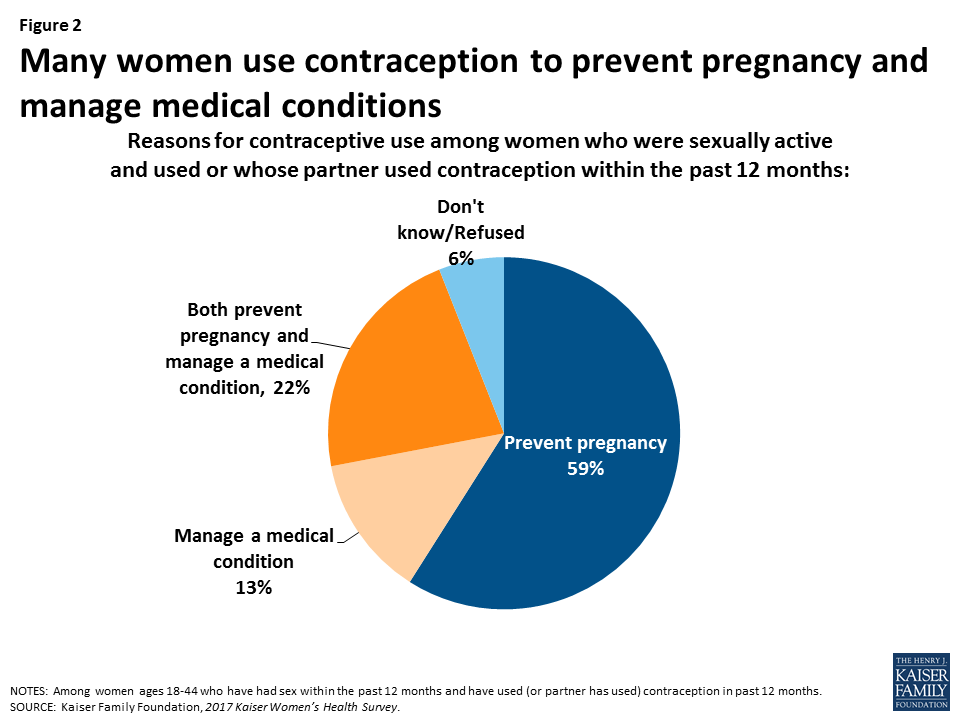
Preventing pregnancy is the leading reason for contraceptive use, but more than one-third of women also use them to manage a medical condition.
The majority of women ages 18-44 use contraception to prevent pregnancy (59%), but 13% use it to manage a medical condition, and 22% use it both to prevent pregnancy and to manage a medical condition (Figure 2). Some women use hormonal contraceptives to manage other conditions, such as acne, irregular menstrual cycle, and endometriosis. This likely affects women’s choices in the types of contraceptives they select. There have been a number of efforts to establish new avenues for obtaining prescription contraceptives, such as from online apps or pharmacists who are now able to prescribe certain contraceptives in some states. However, when asked how they obtained oral contraceptives and the patch, almost all women (95%) stated they obtained these methods from a doctor or clinic prescription rather than directly from pharmacy or from an online app.
Contraceptive Coverage
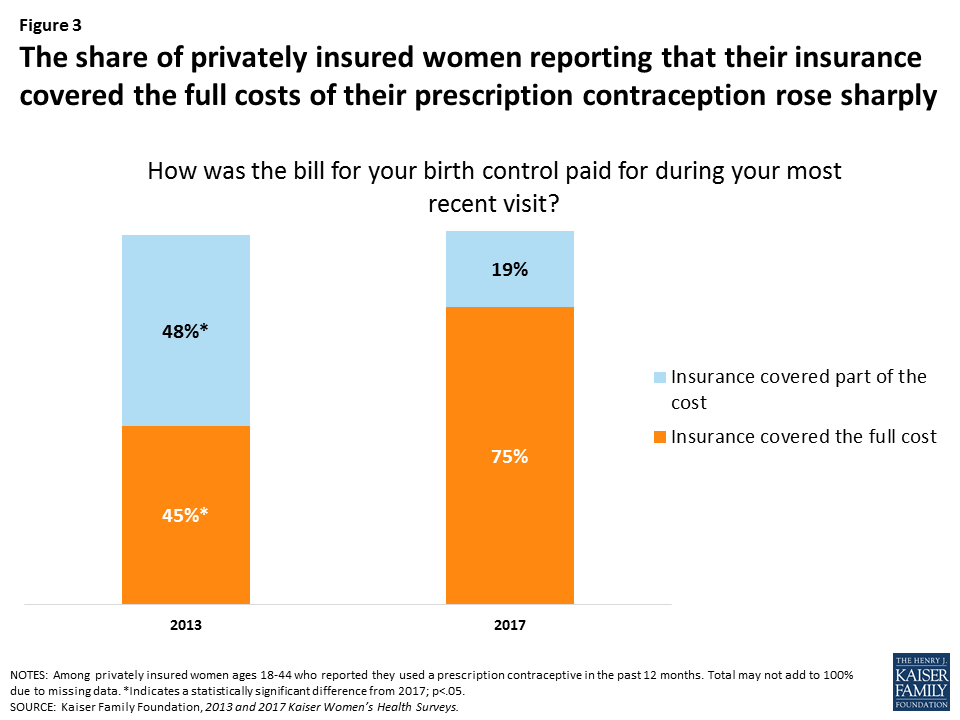
Three-fourths of privately insured women who used contraception in the past year say they had full contraceptive coverage, a sharp rise since 2013.
In 2012, the Affordable Care Act (ACA) required all new private plans to cover, without cost sharing, the full range of contraceptives and services approved by the Food and Drug Administration (FDA) as prescribed for women. In 2017, approximately three-fourths (75%) of privately insured women ages 18-44 who use contraception reported that their insurance fully covered the cost of contraceptives (Figure 3). Another 19% said their insurance paid for part of the costs. Partial coverage could represent women who are enrolled in an older private plan that is still “grandfathered” from the ACA requirements, who used a particular contraceptive that is not covered by the requirement (such as a brand name drug), or who obtained care outside of the plan’s network. Most (92%) women with private insurance stated they did not have any trouble getting insurance to pay for prescribed contraceptives. Only 5% reported that they had problems getting their insurance to pay.
The share of privately insured women with full contraceptive coverage has sharply increased since 2013 when 45% of insured women who used prescription contraception reported their insurance paid the full cost and almost half had only partial coverage.
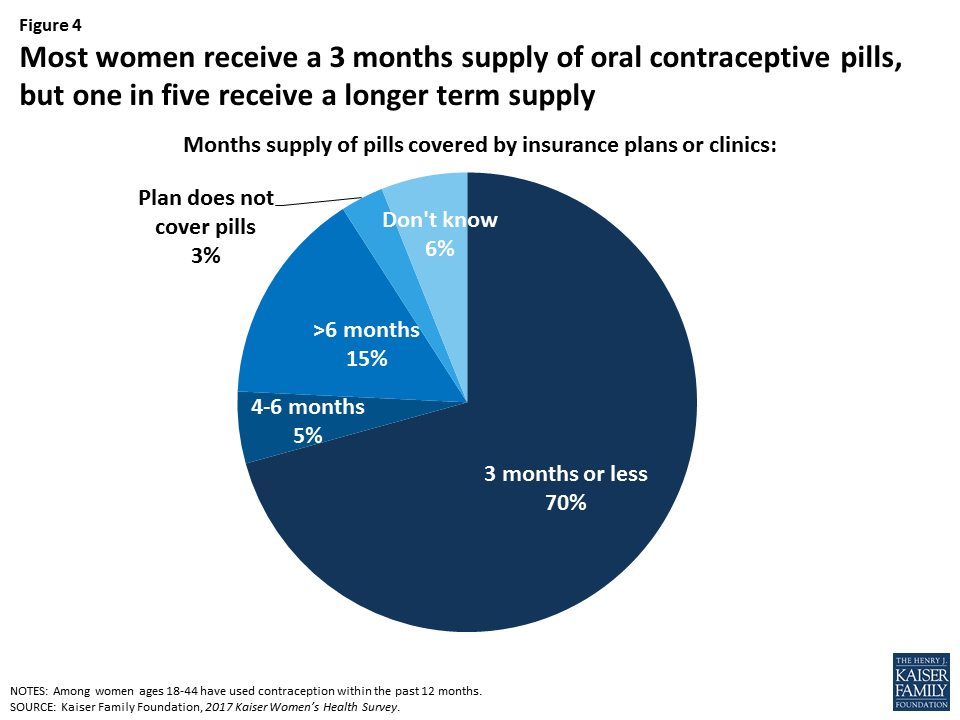
Among women who use oral contraceptives, most typically receive 3 months’ supply at a time.
Women who use oral contraceptives must take a pill every day; therefore having an adequate supply is important for consistent and effective use. One quarter (25%) of women reported that they have missed a pill because they were not able to get their next pack in time. Among women who have used oral contraceptives in the past year, most (70%) report their insurance plan or clinic allows them only to receive three months or less at a time (Figure 4). However, 15% of women reported their plan allows them to get a supply that lasts six months or longer. This has been an area of public policy activity in recent years, with several states now requiring private plans and Medicaid to provide women up to 12 months’ supply.
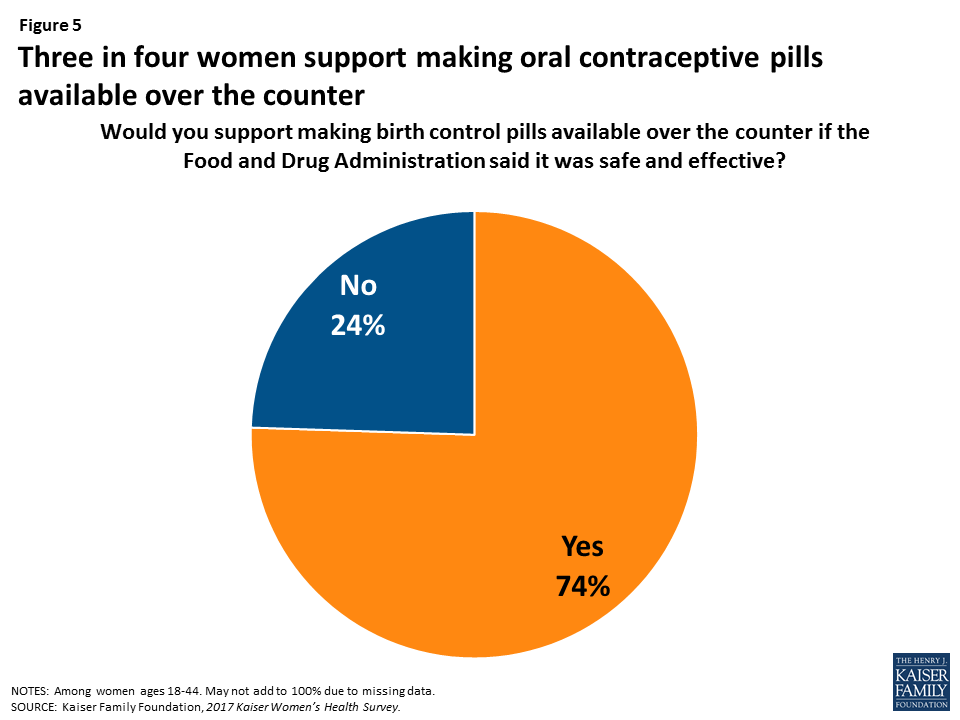
The vast majority of women support making oral contraceptives available over the counter (OTC).
Research suggests that OTC access to oral contraceptives would increase the use of contraception and facilitate continuity of use; however currently, oral contraceptives are only available by prescription, usually from a doctor’s office. Among women of reproductive age, three-fourths (74%) support making oral contraceptives available over the counter if the FDA said it was safe and effective (Figure 5). Support remains at this level across age, race, income, and insurance type subgroups.
Because the federal contraceptive coverage requirement applies only to prescription methods, new federal legislation or administrative changes to the ACA’s preventive services policy would be needed to include over the counter contraceptives as a no cost benefit.
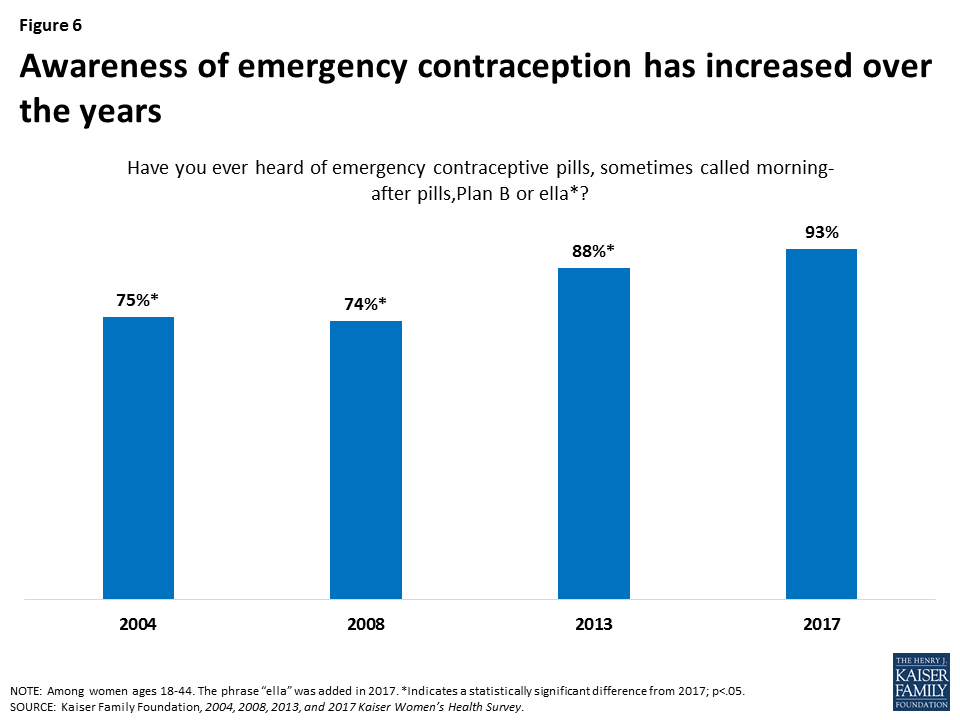
Awareness about emergency contraception has been rising over the past decade.
Emergency contraception (EC), which is contraception that can be used after sex to prevent pregnancy, has been available in the U.S. since 1999. There are multiple forms, including the copper IUD, Plan B® pills (levonorgestrel), and another pill, known by the brand name ella® (ulipristal acetate). Copper IUDs and ella® both require a prescription, but Plan B® is available over the counter and has generic equivalents. As with other contraceptives, most private plans are required to cover prescriptions for EC without cost sharing under the ACA’s preventive services policy.
There has been growing awareness about EC pills over the past decade (Figure 6). In 2004, three-quarters of reproductive-age women reported they had heard of EC pills, and that share has now climbed to more than nine in ten women (93%). Among this group, about one in ten (8%) report they bought or used EC pills in the prior year. Use is highest among women in their late teens or early twenties, Latina women, and women living in urban areas (Table 3).
| Table 3: Emergency contraception, use and awareness | |||||||||||
| All Women | Age Group | Race/Ethnicity | Location | Poverty Level | |||||||
| 18-24 | 25-34 | 35-44 | White | Black | Latina | Urban | Rural | <200%FPL | ≥200%FPL | ||
| Have heard of emergency contraception (EC) | 93% | 92% | 93% | 94% | 97% | 94% | 91%* | 94% | 93% | 90%* | 97% |
| Have taken or bought EC in the past year^ | 8% | 14%* | 10%* | 2% | 5% | 5% | 12%* | 11% | 4%* | 7% | 8% |
| NOTES: ^Among women ages 18-44 who had heard of emergency contraception. Emergency contraception, sometimes called morning-after pills, include Plan B or Ella. The Federal Poverty Level (FPL) was $20,420 for a family of three in 2017. *Indicates a statistically significant difference from 35-44, White, urban, ≥200% FPL; p<.05SOURCE: Kaiser Family Foundation, 2017 Kaiser Women’s Health Survey. | |||||||||||
A small share of women with employer-sponsored insurance are in plans sponsored by faith-based organizations.
The ACA requires that all private plans, including employer-sponsored plans, cover the full cost of prescription contraceptives for women. This policy has been challenged in the courts since it was put in place as some employers with religious or moral objections to contraception claim that the policy violates their religious rights. In October 2017 the Trump Administration greatly broadened the exemption from this requirement that was available for any employer that objects to contraceptive coverage for religious or moral reasons. While currently blocked from implementation, if this policy is ultimately adopted, it has the potential for very large impact, given that employer-based plans cover the majority of women. In the Kaiser Women’s Health Survey, 6% of women with employer-sponsored insurance say that the employer is faith-based or affiliated with a faith-based organization. These employers and other employers who object to contraception for other reasons could qualify for an exemption if the October 2017 regulations are implemented.
Site of Care for Sexual Health Services
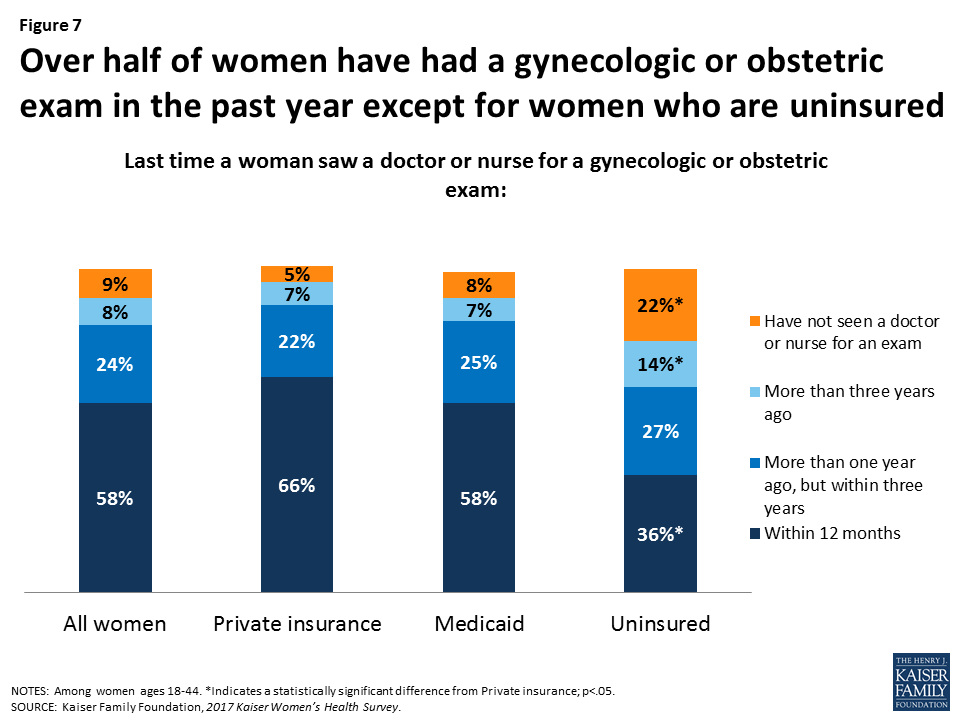
Six in ten reproductive-age women have had a gynecologic or obstetric visit in the past year.
Most women ages 18-44 (58%) report seeing a provider for a gynecologic or obstetric visit in the past year (Figure 7). This rate is higher among women with private insurance (66%) and Medicaid (58%) and far lower among uninsured women (36%). One in seven (14%) uninsured women reported that their last visit was more than 3 years ago, twice the rate of women with private insurance (7%) and Medicaid (7%). Just 9% of women ages 18-44 reported they had never seen a provider for gynecologic or obstetric care. However, 22% of uninsured women reported they had never seen one, almost three times the rate of women with Medicaid (8%) and more than four times the rate of women with private insurance (5%).
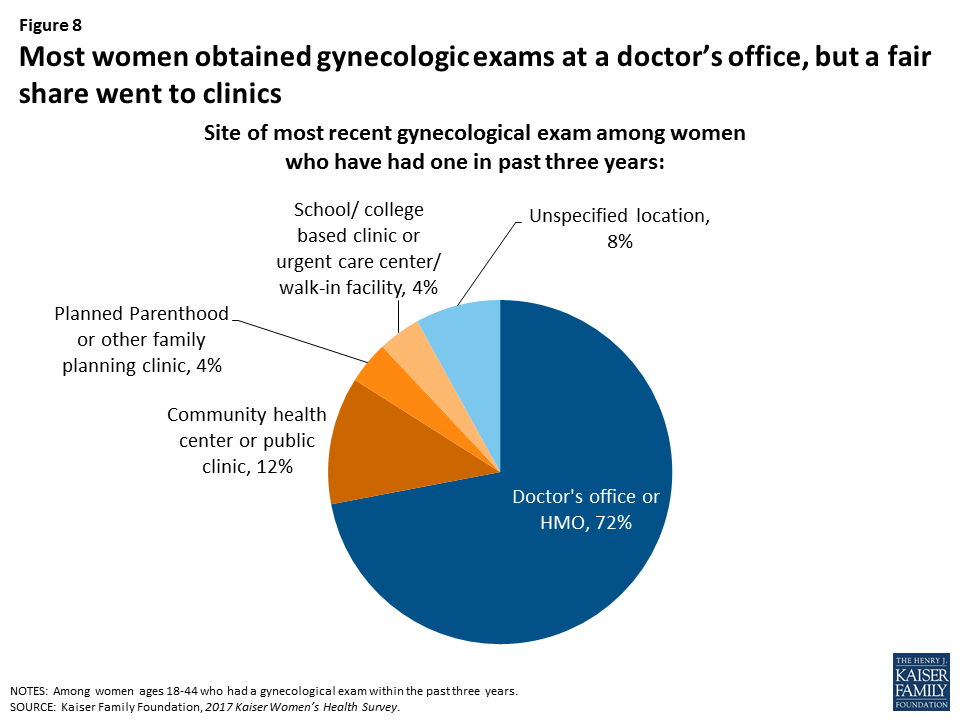
The majority of women get their gynecologic care in private doctors’ offices or HMOs, but clinics play an important role for certain groups of women.
Most women (83%) report that their last reproductive health visit was for gynecologic care or a check-up and 16% report it was for prenatal or pregnancy care. Among the women who report they have had a gynecologic exam in the past three years, 72% report that their most recent exam took place at a doctor’s office or HMO. Roughly one in ten (12%) women report that they went to a public health clinic or community health center (Figure 8). However, this rate is higher among some groups – 30% of Latinas, 23% of rural women, 34% of uninsured women, and 19% of women who have Medicaid reported going to these clinics for their most recent exam (Table 4).
| Table 4: Site of most recent gynecologic exam among women, by selected characteristics | |||||||||||||
| Age Group | Insurance Type | Race/Ethnicity | Location | Poverty Level | |||||||||
| Site of most recent visit | 18-44 | 18-24 | 25-44 | Private | Medicaid | Uninsured | White | Black | Latina | Urban | Rural | <200% FPL | ≥200% FPL |
| Doctor’s office or HMO | 72% | 59% | 75%* | 81% | 59%* | 46%* | 81% | 71% | 53%* | 73% | 64% | 58%* | 82% |
| Community health center or public clinic | 12% | 14% | 12% | 8% | 19%* | 34%* | 5% | 13%* | 30%* | 13% | 23%* | 23%* | 5% |
| Other place | 15% | 27% | 13%* | 12% | 22%* | 21% | 13% | 16% | 17% | 15% | 13% | 19% | 13% |
| NOTES: Among women ages 18-44 who have had an exam in the past three years. Other place includes other types of clinics such as Planned Parenthood centers, school-based clinics, and other locations such as emergency departments. Columns may not sum to 100% due to rounding. The Federal Poverty Level (FPL) was $20,420 for a family of three in 2017. *Indicates a statistically significant difference from ages 18-24; Private, White, Urban, ≥200% FPL; p<.05.SOURCE: Kaiser Family Foundation, 2017 Kaiser Women’s Health Survey. | |||||||||||||
There are differences in the patient populations that seek gynecologic care at doctors’ offices compared to clinics.
Community health centers and other publicly funded clinics have a commitment to delivering care to underserved communities, and this is reflected in their patient population. More than half (56%) of women who obtained gynecologic exams at community health centers are low-income, compared to about a quarter (28%) of women at private doctors’ offices (Table 5). Latina and Black women accounted for 48% of clinic patients, while making up less than a third (31%) at doctors’ offices. Coverage patterns also differ. Private insurance is the leading payer at both sites, but less than half of women at clinics (46%) are privately insured compared to 72% of women at doctors’ offices. Medicaid covers nearly a quarter (24%) of women at clinics, and one in five are uninsured (19%).
| Table 5: Characteristics of women who obtained a gynecologic exam in prior three years | ||
| Characteristics: | Doctor’s Office | Clinic or Health Center |
| Age Group | ||
| 18-24 | 15% | 29%* |
| 25-34 | 40% | 40% |
| 35-44 | 45% | 31%* |
| Race/Ethnicity | ||
| White | 61% | 36%* |
| Black | 16% | 16% |
| Latina | 15% | 32%* |
| Other | 8% | 16%* |
| Poverty Level | ||
| <200% FPL | 28% | 56%* |
| ≥200% FPL | 72% | 44%* |
| Insurance Type | ||
| Private | 72% | 46%* |
| Medicaid | 14% | 24%* |
| Uninsured | 6% | 19%* |
| NOTES: Among women ages 18-44 who have had a gynecologic exam in the past three years. The Federal Poverty Level (FPL) was $20,420 for a family of three in 2017. *Indicates a statistically significant difference from doctor’s office; p<.05.SOURCE: Kaiser Family Foundation, 2017 Kaiser Women’s Health Survey. | ||
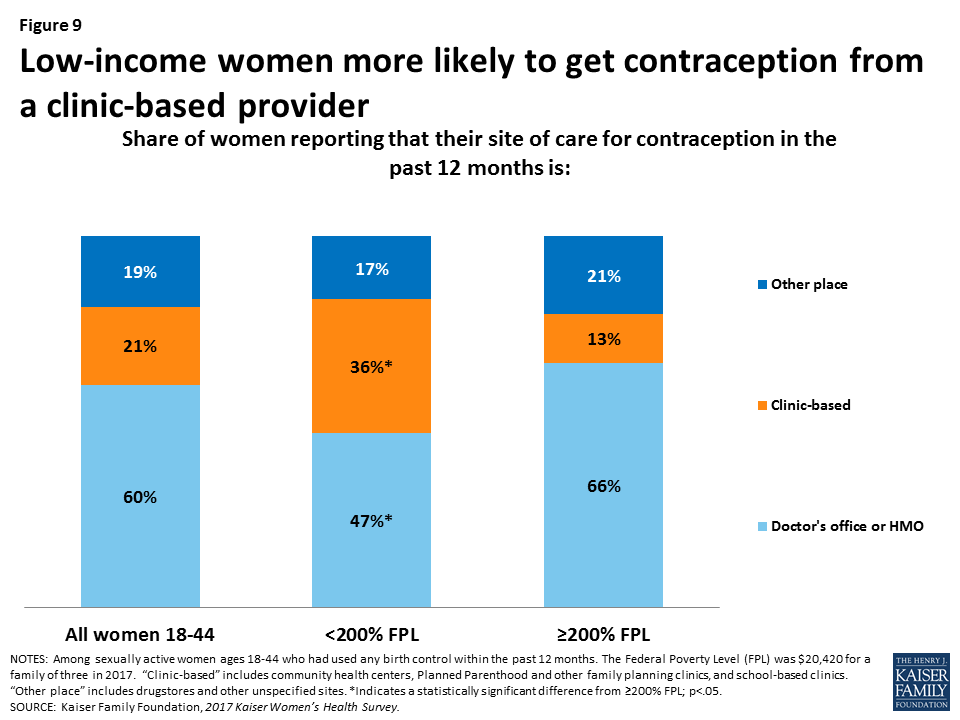
Most women go to a doctor’s office or HMO for contraception care; however, among low-income women, over one-third get their contraceptives from a clinic-based provider.
As with gynecologic care, most women obtain contraception at private doctors’ offices but there are differences between subgroups. Overall, more than half (60%) of women got their birth control care from a doctor or HMO, 21% from a clinic-based provider such as a community health center, Planned Parenthood clinic or other family planning clinic. A large share of women (19%) also report going to some other place for their contraception, which includes drugstores and clinics in retail outlets. Among low-income women however, roughly one in three (36%) get contraception at a clinic based-provider. Comparatively, among women who are at or above 200% FPL, only 13% get their contraceptives from a clinic-based provider (Figure 9). The outcome of current debates about the future of federal financing of family planning services, including Medicaid reimbursements to Planned Parenthood clinics, will have a disproportionate impact on low-income women’s access to contraception.
A third of reproductive-age women report that they have ever visited a Planned Parenthood clinic for health care services.
One in three women ages 18-44 report having ever visited a Planned Parenthood clinic for health care services (Figure 10). This is higher among women in fair or poor health, with almost one half (45%) reporting they have ever visited a Planned Parenthood clinic, compared to 32% of women in good, very good or excellent health. Rates do not differ significantly by race/ethnicity or type of insurance.

Counseling and Screening
A higher share of women report provider counseling for contraception than for sexual history, sexually transmitted infections (STIs), and HIV.
An important element of reproductive and sexual health care is the counseling and education that health care clinicians can offer patients. Counseling allows clinicians to provide patient education, screen for high-risk behaviors, social determinants that could affect health outcomes, and identify the need for additional testing or treatment. Some factors that are associated with poor reproductive and sexual health outcomes are preventable or avoidable. It is estimated that nearly half of all pregnancies in the U.S. are unintended. In addition, there are approximately 20 million new cases annually of STIs, such as chlamydia, gonorrhea, and HPV, and many reached record-breaking levels in 2016. Most Medicaid programs and private plans include coverage for provider counseling on a wide range of sexual health topics, including STIs, contraception use, and partner violence.
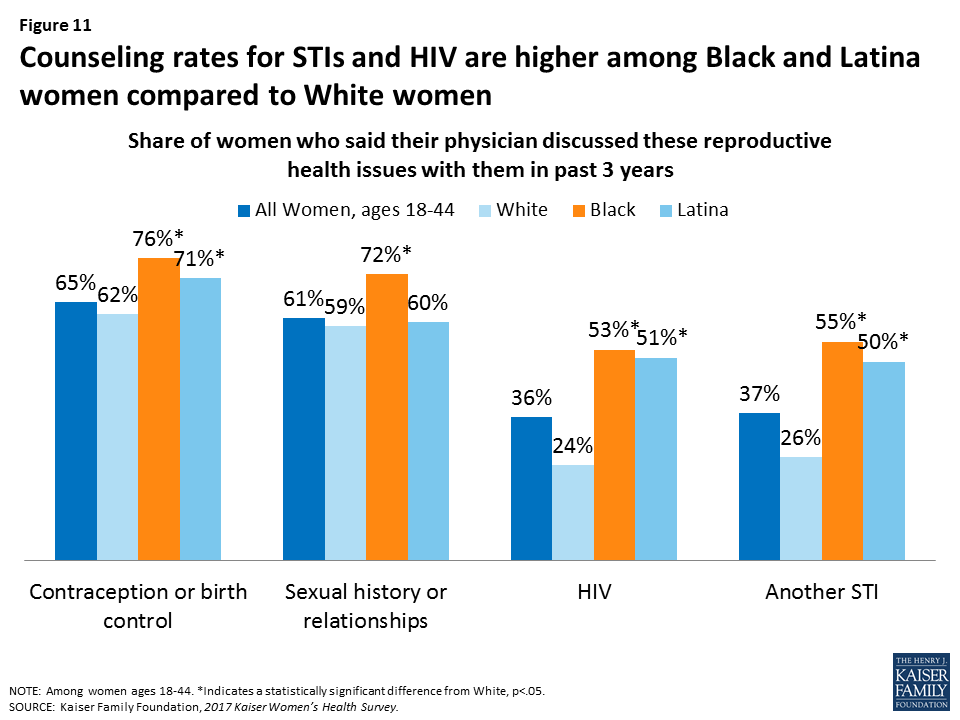
Despite these public health challenges and the recommendations of professional groups, counseling on many of these topics is not routine among women of reproductive age. While most reproductive-age women report having had a recent conversation with a provider about contraception (65%) and sexual history (61%), fewer report having discussed HIV (36%) and other STIs (37%). Overall, counseling rates are higher among Black and Latina women (Figure 11). While women who have private insurance report the highest rates of counseling on contraception and sexual history, women covered by Medicaid report significantly higher rates of counseling on HIV and other STIs (Table 6). Lower-income women and those who live in urban settings report higher rates of discussion on HIV and STIs. Only one-third of women between the ages of 40-64 said a clinician had discussed symptoms of menopause with them in the past three years.
| Table 6: Share of women who said their physician discussed these reproductive health issues with them in past three years, by selected characteristics | |||||||||||
| All Women | Insurance Type | Poverty Level | Age Group | Location | |||||||
| Reported having discussed in past 3 years | Private | Medicaid | Uninsured | ≥200% FPL | <200% FPL | 18-24 | 25-34 | 35-44 | Urban | Rural | |
| Contraception or birth control | 65% | 70% | 61% | 55%* | 69% | 62% | 69%* | 74%* | 54% | 66% | 60% |
| Sexual history or relationships | 61% | 63% | 60% | 50%* | 61% | 63% | 70%* | 68%* | 48% | 62% | 55% |
| HIV | 36% | 29% | 50%* | 38% | 30% | 43%* | 42%* | 37% | 30% | 41% | 27%* |
| Another STI | 37% | 34% | 48%* | 36% | 32% | 46%* | 48%* | 40%* | 28% | 43% | 32%* |
| Menopause^ | 34% | 33% | 37% | 34% | 33% | 37% | – | – | 34% | 32% | 46% |
| NOTES: ^All topics are among women ages 18-44, except Menopause, which is among women, ages 40-64. The Federal Poverty Level (FPL) was $20,420 for a family of three in 2017. *Indicates a statistically significant difference from Private, ≥200% FPL, Ages 35-44, Urban; p<.05. – indicates data not available.SOURCE: Kaiser Family Foundation, 2017 Kaiser Women’s Health Survey. | |||||||||||
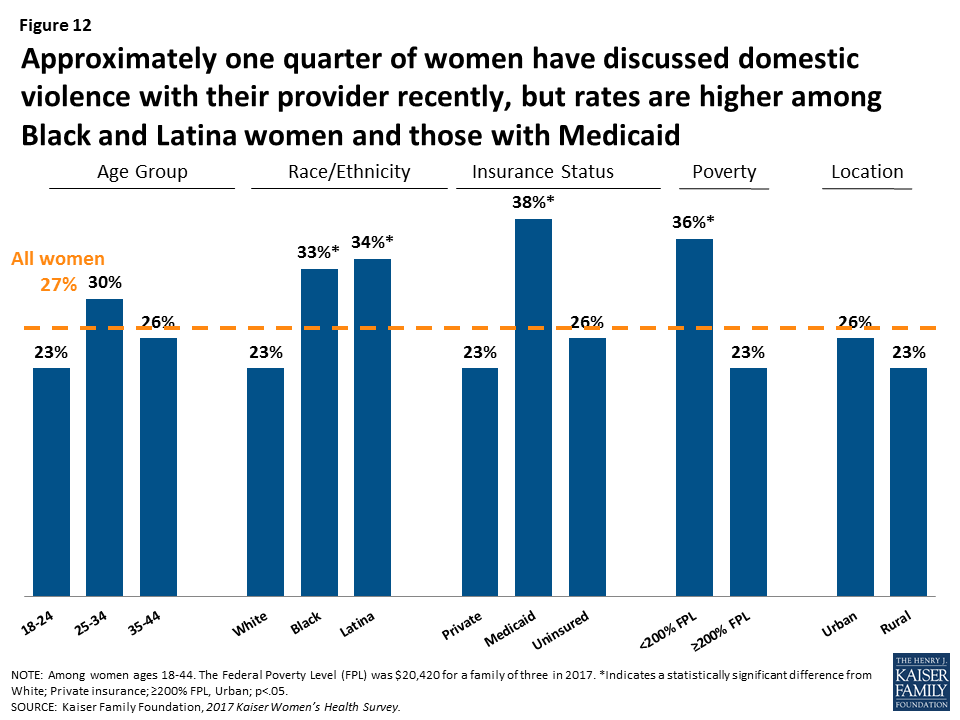
Despite the high rate of sexual violence on women in the U.S., few women report they have talked with a provider about intimate partner violence.
More than 1 in 3 adult women in the United States (36%) have experienced rape, physical violence, and/or stalking by an intimate partner in their lifetime. Intimate partner violence (IPV), also called domestic or dating violence, can affect women at any point in their lives, but rates are highest among women in their reproductive years.
It has long been recognized that clinicians can play an important role in the identification and treatment of women who have suffered from violence, and one of the preventive services that the ACA covers without cost sharing is provider counseling on IPV. While there have been advances in the health care system’s handling of IPV and newly developed screening tools for providers to use, it is still far from routine for providers to raise the issue of violence with women. A little more than a quarter (27%) of women say they have discussed domestic or dating violence in the past three years with their provider (Figure 12). Counseling rates are higher among women of color, low-income women, and those covered by Medicaid.
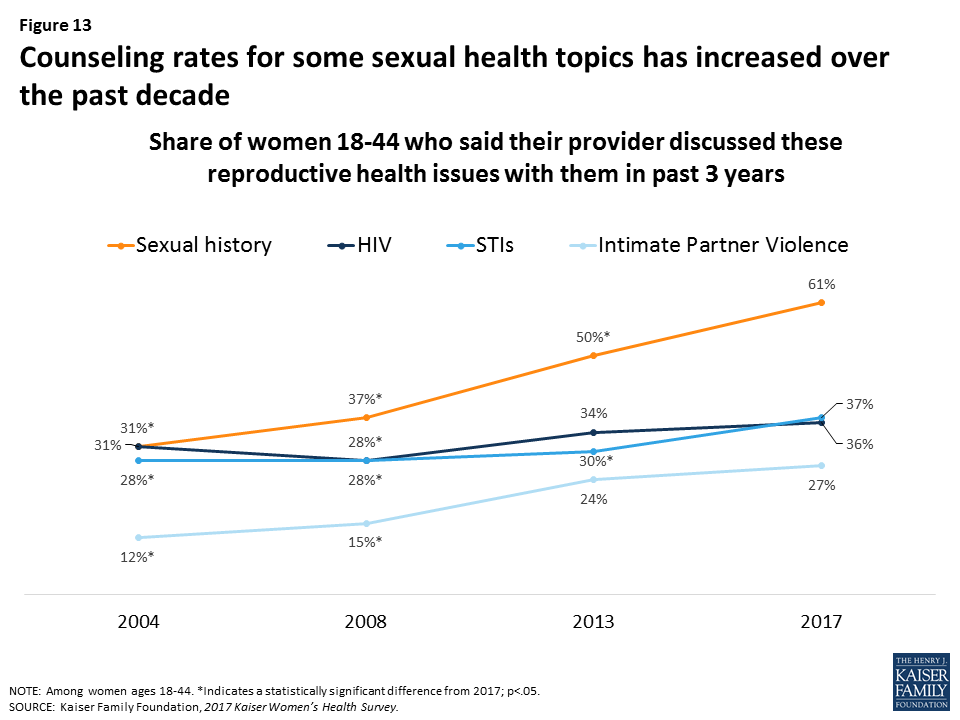
Provider counseling rates on many sexual health topics are on the rise.
There has been a rise in counseling rates on some sexual health topics over the past decade, particularly sexual history and intimate partner violence (Figure 13). In 2004, less than a third of women reported recently speaking with a provider about their sexual history, but this has risen sharply to six in ten women (61%) in 2017. Provider counseling on violence remains relatively low at 27%, but this is up from 12% in 2004. Counseling rates on HIV and STIs have risen more modestly.
Approximately four in ten women report recent screenings for HIV and other STIs, but many incorrectly assume they are being tested.
Along with counseling, several professional groups and government agencies, including the USPSTF, the Institute of Medicine, and the Centers for Disease Control and Prevention, recommend that women in their reproductive years be tested for STIs such as chlamydia, gonorrhea and HIV. Knowing one’s status is important to receive early treatment and prevent transmission to sexual partners. STI and HIV tests are covered without cost sharing in new private plans under the ACA’s preventive services coverage requirements and are typically covered by most Medicaid programs.
Approximately four in ten women report that they have had a test for HIV (42%) or other STIs (42%) in the past two years; however, roughly half (49%) of these women assumed this test was a routine part of an examination—which is often not the case (Figure 14). Therefore, the actual screening rate is likely lower than the share of women who report being tested. This may cause women to believe they do not have an STI when in fact they have not actually been tested.
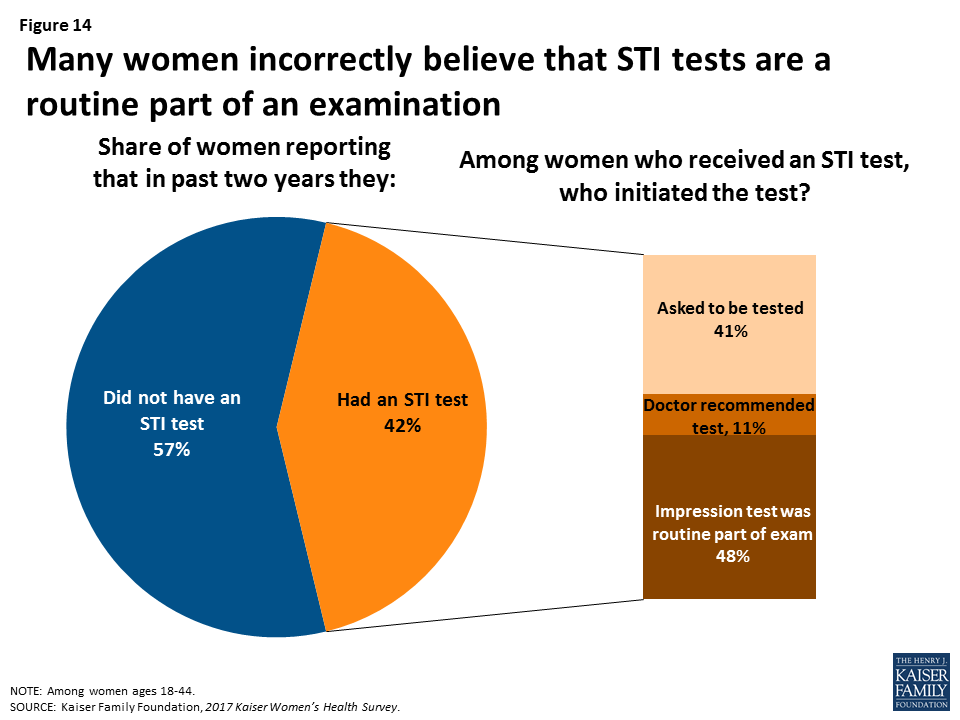
Screening rates for HIV and other STIs were higher among women of color, women covered by Medicaid, and women living in urban areas (Table 7). Black women reported asking to be tested for HIV and other STIs at higher rates, whereas Latina and White women were more likely to have the impression it was a routine part of the exam.
| Table 7: Receipt of sexual health screening tests, by race/ethnicity, insurance status, poverty level | |||||||||
| All Women | Race/Ethnicity | Insurance Type | Poverty Level | ||||||
| Reported having test in past 2 years | White | Black | Latina | Private | Medicaid | Uninsured | <200%FPL | ≥200%FPL | |
| HIV Test | 42% | 33% | 66%* | 51%* | 38% | 58%* | 39% | 54%* | 36% |
| Thought test was routine part of exam | 49% | 52% | 35%* | 60%* | 50% | 47% | 48% | 47% | 49% |
| Doctor recommended test | 11% | 9% | 11% | 10% | 12% | 6% | 12% | 11% | 11% |
| Asked to be tested | 40% | 38% | 54%* | 29% | 38% | 47% | 40% | 42% | 39% |
| STI Tests | 42% | 37% | 63%* | 45% | 41% | 54%* | 31% | 50%* | 39% |
| Thought test was routine part of exam | 48% | 50% | 31%* | 66%* | 47% | 48% | 59% | 42% | 52% |
| Doctor recommended test | 11% | 9% | 12% | 8% | 10% | 9% | 6% | 10% | 11% |
| Asked to be tested | 41% | 41% | 57%* | 26%* | 42% | 43% | 34% | 47% | 37% |
| NOTES: Among women ages 18-44. The Federal Poverty Level (FPL) was $20,420 for a family of three in 2017. *Indicates a statistically significant difference from White; Private insurance; ≥200% FPL, p<.05.SOURCE: Kaiser Family Foundation, 2017 Kaiser Women’s Health Survey. | |||||||||
Conclusion
This survey finds that a sizeable share of sexually active women are not using any contraception and are at greater risk for unintended pregnancy. Provider counseling rates on many topics such as a woman’s sexual history and STIs, have increased over time, but many women still report that their provider has not spoken with them about important issues, such as intimate partner violence. Publicly supported clinics, including community health centers and Planned Parenthood sites, play an important role in providing reproductive and family planning care for uninsured women and women of color. The ACA’s requirement for contraceptive coverage without cost sharing has reached a large swath of women, who now do not pay any out of pocket costs for contraception.
However, the Trump Administration’s health policy agenda proposes many changes that would affect women’s access to reproductive health care. The Administration has proposed new regulations that would extend the number of employers who may be exempted from the contraceptive coverage requirement because of religious or moral objections. The Administration has also expressed support for withdrawing federal reimbursements for services that Planned Parenthood provides to low-income women including Medicaid and Title X family planning funds. These policies would cripple the ability of Planned Parenthood to continue to provide care that women need and use, and would disproportionately limit access to low-income and minority women.
This brief was prepared by Caroline Rosenzweig, Usha Ranji, and Alina Salganicoff of the Kaiser Family Foundation.
The authors would like to thank Anthony Damico, an independent consultant, for his assistance with survey analysis.
