Medicaid Retroactive Coverage Waivers: Implications for Beneficiaries, Providers, and States
Issue Brief
On October 26, 2017, the Centers for Medicare and Medicaid Services (CMS) approved an amendment to Iowa’s Section 1115 demonstration waiver eliminating 3-month retroactive coverage for nearly all new Medicaid applicants as of November 1, 2017.1 Populations affected by Iowa’s waiver include low-income parents, children over age 1, Affordable Care Act (ACA) expansion adults, seniors, and people with disabilities. Retroactive coverage waivers have been approved in a limited number of other states with certain conditions. This issue brief answers key questions about Medicaid retroactive coverage, describes Iowa’s recent waiver amendment, considers the policy implications of retroactive coverage waivers, and identifies issues to watch.
What is Medicaid retroactive coverage and why is it part of Medicaid?
Unlike private insurance, Medicaid covers vulnerable populations, such as seniors, people with disabilities, low-income children and their parents, and other low-income adults. Medicaid is a safety net program that provides services that private insurance typically does not, such as long-term care, and protects enrollees from unpaid medical bills that they cannot afford. It also ensures that providers are paid for services they offer to Medicaid-eligible people and helps encourage providers to participate in the program. Retroactive coverage is one of the long-standing safeguards built into the program for low-income Medicaid beneficiaries and their healthcare providers. Federal law directs state Medicaid programs to cover (and provides federal matching funds for) medical bills incurred up to 3 months prior to a beneficiary’s application date.2 To qualify for retroactive coverage, a Medicaid beneficiary must have been eligible for coverage during the 3 months prior to application when the bill was incurred, and the services must be those that Medicaid covers.
Some people may not become eligible for Medicaid until after they experience a traumatic event, such as a stroke that requires hospitalization and ongoing long-term care needs or a motorcycle accident resulting in a traumatic brain injury. In addition, many people mistakenly think that Medicare covers long-term care and often do not learn about Medicaid until their health deteriorates to the point that they seek a nursing home placement or other long-term care services; these events often are precipitated by a crisis, such as a fall, that cause seniors and their families to seek out services and supports. When sudden health care needs arise, the initial focus often is on stabilizing the person’s medical condition. If a traumatic event occurs toward the end of a calendar month, it may take several days or weeks for the patient and their family and providers to navigate complex medical issues before they turn to considering payment, including Medicaid eligibility. During this time, sizeable medical bills can accrue. Retroactive coverage protects patients and providers by ensuring that medical bills are paid even if a Medicaid application is not filed until the calendar month following a traumatic event.
Federal Medicaid law allows some providers, like hospitals, to determine certain people “presumptively eligible” for Medicaid. Presumptive eligibility allows providers to offer (and get reimbursed for) needed health services right away to adults and children who appear to be eligible for Medicaid based on their low incomes, while a full Medicaid application is pending. However, presumptive eligibility is not available for seniors and people with disabilities who may have long-term care needs.
What was approved in Iowa’s Retroactive Coverage Waiver?
Section 1115 of the Social Security Act authorizes the Health and Human Services (HHS) Secretary to waive state compliance with certain provisions of federal Medicaid law to allow states to engage in experimental, pilot, or demonstration projects that, in the Secretary’s judgment, further Medicaid program objectives. Iowa’s Section 1115 demonstration waiver, known as the “Iowa Health and Wellness Plan,” initially was limited to adults newly eligible under the ACA and did not apply to traditional Medicaid populations.3 However, on October 26, 2017, CMS approved an amendment to Iowa’s eliminating 3-month retroactive coverage for nearly all new Medicaid applicants as of November 1, 2017.4 While pregnant women and infants under age 1 still qualify for retroactive coverage in Iowa, the new retroactive coverage waiver applies to all other state plan populations, including low-income parents, children over age 1, ACA expansion adults, seniors, and people with disabilities. Coverage for people affected by Iowa’s waiver will now begin no earlier than the first day of the application month.
What are the expected implications for beneficiaries in Iowa?
In approving Iowa’s retroactive coverage waiver, CMS concluded that Medicaid program objectives are furthered “by encouraging beneficiaries to obtain and maintain health coverage, even when healthy.”5 For seniors and people with disabilities seeking long-term care coverage, CMS states that “this waiver will encourage beneficiaries to apply for Medicaid expeditiously when they believe they meet the criteria for eligibility to ensure primary or secondary coverage through Medicaid to receive these services if the need arises.”6 Eligibility criteria for long-term care services include both financial criteria (people must have low incomes and limited assets) and functional criteria (people must qualify for an “institutional level of care” or meet other disability-related criteria). These rules are often complicated and only available in state policy manuals. Even if people know about the rules, it can be challenging for a lay person to determine whether their situation qualifies. In Iowa’s waiver, the state “assures [CMS] that it will provide outreach and education about how to apply for and receive Medicaid coverage to the public and to Medicaid providers, particularly those who serve vulnerable populations that may be impacted by this change.”7 The terms and conditions do not provide additional detail about these efforts, although the waiver went into effect less than a week after approval.
Iowa’s waiver amendment submission to CMS acknowledged that the “majority of the [public] comments received were opposed to the elimination” of 3-month retroactive coverage.”8 For example, “[c]ommenters felt that the proposed change will place unnecessary financial burdens on patients/family members. . . , particularly those who seek services during the last few days of a month and may not apply until the following month. . . , those in rural locations. . . , or those who seek facility placement.”9 In addition, “commenters noted concerns with the potential health impacts of the amendment, indicating that future enrollees may either delay or forego needed care or be placed in inappropriate or unsafe environments.”10 However, the state indicated that it was unable to make any changes to its request in response to public comments as the waiver application was submitted pursuant to state legislation that directed the state to seek the waiver.11
What is the fiscal impact of eliminating retroactive coverage in Iowa?
Iowa’s waiver amendment submission to CMS indicated that “this change is being made to reduce program costs” and estimated that the “[e]limination of retroactive coverage is expected to reduce monthly enrollment by 3,344 enrollees and reduce annual [federal and state] Medicaid spending by $36.8 million [$9.7 million state share].”12 Specifically, the state estimated that average monthly Medicaid enrollment will decrease by 1,384 expansion adults, 1,129 children, 668 low-income parents, 157 people with disabilities, 6 seniors, and 1 breast/cervical cancer treatment enrollee as a result of the elimination of retroactive coverage.13
Have other waivers of retroactive coverage been approved?
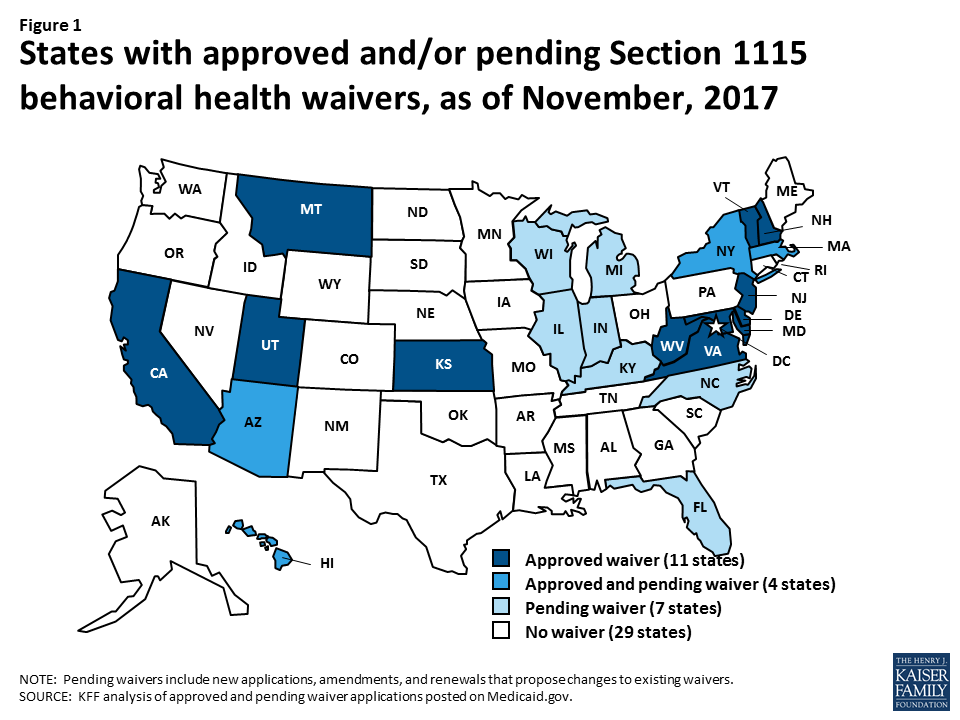
Prior to Iowa’s waiver, CMS (under the Obama Administration) waived retroactive eligibility for certain populations as part of 3 other ACA expansion waivers provided that certain conditions to safeguard beneficiaries were met. Unlike Iowa, these waivers do not apply to seniors and people with disabilities:
- New Hampshire’s retroactive coverage waiver for ACA expansion adults was to be implemented only after CMS determined that retroactive coverage is unnecessary, based on state data showing no gaps in coverage for newly eligible adults prior to their Medicaid application date and upon renewal.14
- Arkansas’s retroactive coverage waiver for ACA expansion adults was conditioned on the state meeting 3 criteria: completing an eligibility determination mitigation plan and timely eligibility determinations, providing benefits during a reasonable opportunity period for otherwise eligible individuals who attest to immigration status, and implementing a hospital presumptive eligibility program. (Arkansas has a pending waiver amending seeking to eliminate the 3 conditional criteria.)15
- Indiana’s ACA expansion waiver eliminates 3-month retroactive coverage for adults newly eligible under the ACA as well as some traditional populations, such as low-income parents, 19- and 20-year olds, and people moving from TANF to work and receiving Transitional Medical Assistance.16
A handful of other states have retroactive coverage waivers that pre-date the ACA and may have been associated with achieving the budgetary savings necessary to expand coverage before federal law authorized the use of Medicaid funds for childless adults. Some of these waivers apply to limited populations, and most have exceptions for seniors and people with disabilities:
- Delaware, which had a pre-ACA waiver expanding coverage to nearly all adults up to 100% of the federal poverty level, waives retroactive eligibility for most populations, except for people in institutions and the buy-in for working people with disabilities.17
- Massachusetts’ waiver, which also had a pre-ACA coverage expansion, limits retroactive coverage to 10 days prior to the application date for most populations, with exceptions for Katie Beckett children with significant disabilities, people with disabilities eligible under home and community-based services waivers, seniors, and people with long-term hospital or nursing home stays.18
- Maryland has a retroactive coverage waiver for certain optional targeted low-income children.19
- Tennessee has a retroactive coverage waiver that applies to state plan populations.20
- Utah waives retroactive coverage for its limited coverage expansion to parents and childless adults with income above Medicaid state plan limits up to 100% FPL.21
What do we know about the effects of retroactive coverage waivers?
Despite requirements that Section 1115 waivers serve an experimental, pilot, or demonstration purpose and have an evaluation component, little is known about the impact of retroactive coverage waivers on beneficiaries and providers. In Iowa’s submission to CMS, the “State [did] not propose any modifications to the current evaluation plan as a result of [the retroactive coverage waiver] amendment,”22 and CMS did not require any changes to the waiver terms and conditions regarding evaluation when approving the amendment. As a result, it is unclear whether Iowa’s waiver evaluation will encompass the effects of the retroactive coverage waiver. Some data is available from Indiana’s prior claims payment program that CMS required as a safeguard against unpaid medical bills for traditional populations subject to its retroactive coverage waiver. The prior claims payment program requires Indiana to reimburse providers for services received up to 90 days prior to the effective Medicaid coverage date for low-income parents who were not determined presumptively eligible. When denying Indiana’s request to discontinue the program in July, 2016, CMS noted that 13.9% of beneficiaries were eligible for the program and had incurred costs averaging $1,561 per person.23
What are the issues to Watch in the future?
Key issues to watch in retroactive coverage waivers include the following:
- Will Other States Seek Retroactive Coverage Waivers? CMS’s recent approval of Iowa’s retroactive coverage waiver may lead other states to consider similar proposals. Kentucky’s pending waiver application includes a retroactive coverage waiver for most populations (except pregnant women and children under age 1). The ACA’s waiver transparency rules, including public notice and comment periods at the state and federal levels, help stakeholders learn about state proposals and provide input.
- What Beneficiary Safeguards Will be Included in Retroactive Coverage Waivers? The steps that states take to encourage eligible people to enroll in Medicaid and prevent delays in effectuating coverage that can lead to unpaid medical bills will be an important area to watch, as will the impact of potential decisions to remove conditions on existing retroactive coverage waivers that sought to protect beneficiaries from incurring unpaid medical bills. Navigating the Medicaid application process can be confusing, particularly for seniors and people with disabilities who are seeking long-term care coverage, and eliminating retroactive coverage means that the ability to apply as quickly as possible takes on new importance to minimize unpaid bills. People who enter nursing homes initially paying out-of-pocket before they “spend down” to Medicaid eligibility might have staff familiar with the program rules to help them apply as soon as they are eligible. (Applying for coverage too soon, before eligibility criteria are met, will result in a denial.) Other people, such as those who seek long-term care services in the community or those who only become eligible after a traumatic event may not know about Medicaid eligibility until after some time has passed or may not have the bandwidth to devote to the complex long-term care application while in the midst of a health crisis.
- How Do Retroactive Coverage Waivers Affect Access to Care? Evaluations can provide information about the impact of retroactive coverage waivers on beneficiaries and providers and whether these waivers help promote or hinder access to coverage and care. Before formal waiver evaluations are completed, stakeholders also will be interested in data that states can make available sooner, through quarterly or annual waiver reports, including the impact of retroactive coverage waivers on different populations, such as seniors, people with disabilities, those with long-term care needs, children, and adults, and on providers’ uncompensated care costs.
Endnotes
- CMS, Special Terms and Conditions, Iowa Wellness Plan, #11-W-00289/5 (Jan. 1, 2017-Dec. 31, 2019, amended Oct. 26, 2017), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ia/ia-wellness-plan-ca.pdf. ↩︎
- 42 U.S.C. § 1396a (a) (34) (“A State plan for medical assistance must provide that in the case of any individual who has been determined to be eligible for medical assistance under the plan, such assistance will be made available to him for care and services included under the plan and furnished in or after the third month before the month in which he made application (or application was made on his behalf in the case of a deceased individual) for such assistance if such individual was (or upon application would have been) eligible for such assistance at the time such care and services were furnished.”) ↩︎
- The original waiver was approved in December, 2013 to implement Iowa’s ACA expansion. The waiver provisions for ACA expansion adults have been amended several times, and in July 2017, the waiver’s dental program (including tiered benefits, premiums, and healthy behavior incentives) was expanded to include all Medicaid adults. ↩︎
- CMS Special Terms and Conditions, Iowa Wellness Plan, #11-W-00289/5 (Jan. 1, 2017-Dec. 31, 2019, amended Oct. 26, 2017), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ia/ia-wellness-plan-ca.pdf. ↩︎
- CMS Letter from Brian Neale, Director, Center for Medicaid and CHIP Services to Mikki Stier, Medicaid Director, Iowa Dep’t of Human Services (Oct. 27, 2017), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ia/ia-wellness-plan-ca.pdf. ↩︎
- Id. ↩︎
- CMS Special Terms and Conditions, Iowa Wellness Plan, #11-W-00289/5 (Jan. 1, 2017-Dec. 31, 2019, amended Oct. 26, 2017), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ia/ia-wellness-plan-ca.pdf. ↩︎
- State of Iowa, Dep’t of Human Services, Iowa Wellness Plan, Project #11-W-00289/5, Section 1115 Demonstration at 5 (Aug. 2, 2017), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ia/ia-wellness-plan-pa4.pdf. ↩︎
- Id. at 7. ↩︎
- Id. ↩︎
- Id. at 6; see also Iowa House File 653, https://www.legis.iowa.gov/docs/publications/LGE/87/HF653.pdf. ↩︎
- State of Iowa, Dep’t of Human Services, Iowa Wellness Plan, Project #11-W-00289/5, Section 1115 Demonstration Amendment, Attachment A – Public Notice at 2 (Aug. 2, 2017), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ia/ia-wellness-plan-pa4.pdf. ↩︎
- Id. ↩︎
- Kaiser Family Foundation, Section 1115 Medicaid Expansion Waivers: A Look at Key Themes and State Specific Waiver Provisions (Aug. 16, 2017), https://modern.kff.org/medicaid/issue-brief/section-1115-medicaid-expansion-waivers-a-look-at-key-themes-and-state-specific-waiver-provisions/. ↩︎
- Id. ↩︎
- Kaiser Family Foundation, An Early Look at Medicaid Expansion Waiver Implementation in Michigan and Indiana (Jan. 2017), https://modern.kff.org/medicaid/issue-brief/an-early-look-at-medicaid-expansion-waiver-implementation-in-michigan-and-indiana/. ↩︎
- CMS Special Terms and Conditions, Delaware Diamond State Health Plan, #11-W-00036/4 (Sept. 30, 2013-Dec. 31, 2018), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/de/de-dshp-ca.pdf. ↩︎
- CMS Special Terms and Conditions, MassHealth Medicaid Section 1115 Demonstration, #11-W-00030/1 (July 1, 2017-June 30, 2022), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ma/ma-masshealth-ca.pdf; see also M.G.L. ch. 118E, § 9A (6), https://malegislature.gov/Laws/GeneralLaws/PartI/TitleXVII/Chapter118E/Section9A. ↩︎
- CMS Special Terms and Conditions, Maryland HealthChoice Medicaid Section 1115 Demonstration, #11-W-00099/3 (Jan. 1, 2017-Dec. 31, 2021), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/md/md-healthchoice-ca.pdf. ↩︎
- CMS Special Terms and Conditions, TennCare II, #11-W-00151/4 (Nov. 16, 2016-June 30, 2021), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/tn/tn-tenncare-ii-ca.pdf. ↩︎
- CMS Special Terms and Conditions, Utah Primary Care Network #11-W-00145/8 (Nov. 1, 2017-June 30, 2022), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ut/ut-primary-care-network-ca.pdf. ↩︎
- State of Iowa, Dep’t of Human Services, Iowa Wellness Plan, Project #11-W-00289/5, Section 1115 Demonstration Amendment (Aug. 2, 2017), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/ia/ia-wellness-plan-pa4.pdf. ↩︎
- CMS letter from Vikki Wachino, Director, Center for Medicaid and CHIP Services to Tyler Ann McGuffee, Insurance and Healthcare Policy Director, Office of Governor Michael R. Pence (July 29, 2016), https://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Waivers/1115/downloads/in/Healthy-Indiana-Plan-2/in-healthy-indiana-plan-support-20-lockouts-redetermination-07292016.pdf. ↩︎