Medicaid
new and noteworthy
Medicaid: What to Watch in 2026
In this brief, KFF explores how state fiscal pressures are likely to converge with the implementation of the 2025 reconciliation law to affect Medicaid coverage, financing, and access to care over the next year, especially leading up to the midterm elections.
Medicaid and work
Challenges with Implementing Work Requirements: Findings from a Survey of State Medicaid Programs
To better understand how states are preparing for Medicaid work requirements, states were asked to discuss anticipated challenges to implementing work requirements by the end of 2026, including related system changes and data matching.
understanding medicaid
5 Facts: Provider Taxes
All states except Alaska cover some state Medicaid costs with taxes on health care providers. This brief uses data from KFF’s 2024-2025 survey of Medicaid directors to describe current practices and the federal rules governing them.
5 Facts: Medicaid and Hospitals
Absorbing reductions in Medicaid spending could be challenging for hospitals, particularly for those that are financially vulnerable. This brief provides data on the reach of Medicaid across hospitals, patients, and charity care.
5 Facts: Medicaid and Rural Areas
Approximately 66 million people live in rural areas – about 20% of the U.S. population. Nearly 1 in 4 of them have Medicaid, a higher share than in urban areas (24% vs 21%).
5 Facts: Nursing Facilities
The substantial Medicaid savings in the reconciliation bill that has been passed by the House could have major implications for nearly 15,000 federally certified nursing facilities and the 1.2 million people living in them.
2025 Medicaid Home Care survey
Eligibility, Enrollment, and Renewal Policies
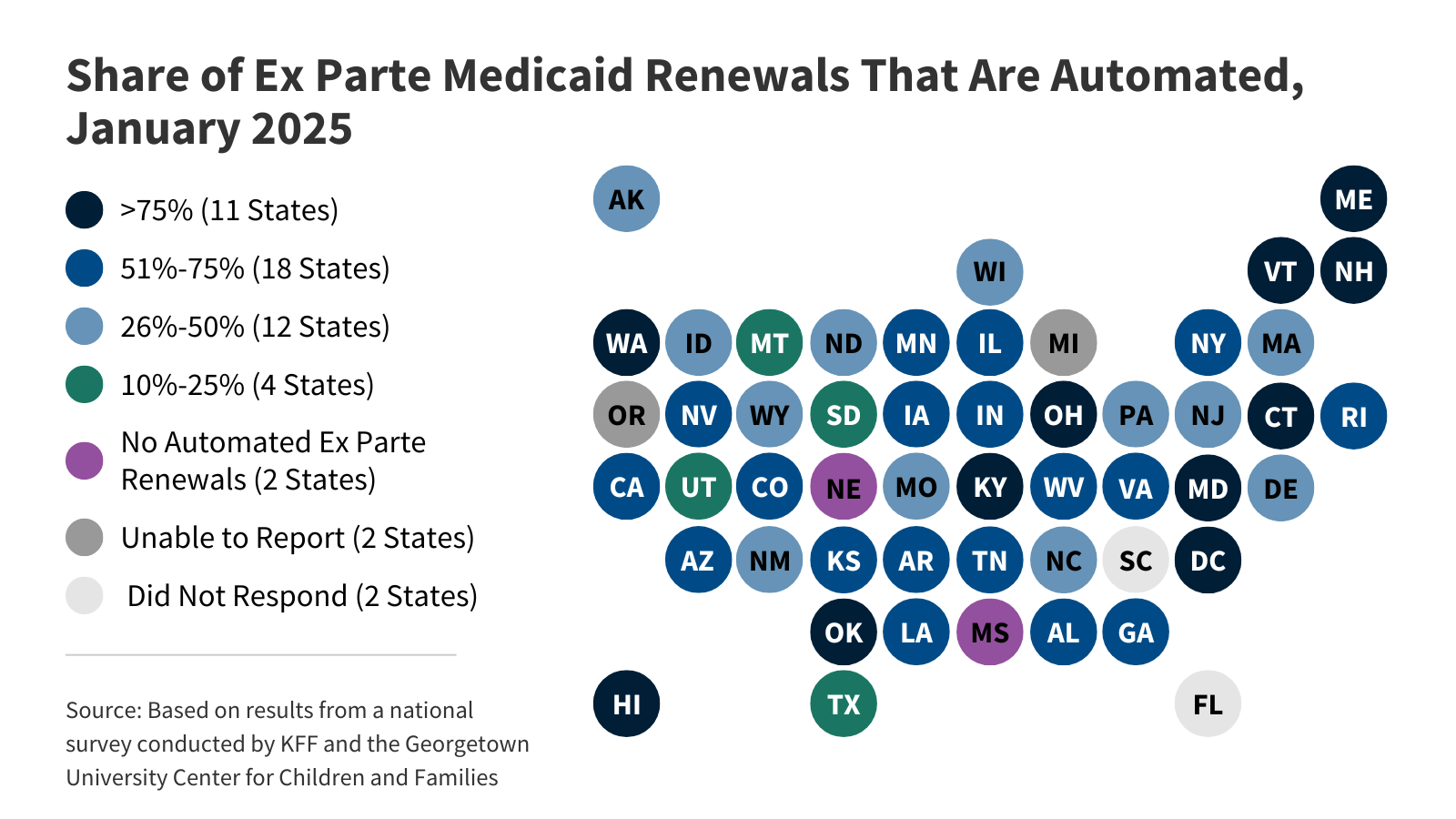 KFF's survey findings capture state actions that seek to improve the accuracy and efficiency of Medicaid and CHIP enrollment and renewal processes, as of January 2025.
KFF's survey findings capture state actions that seek to improve the accuracy and efficiency of Medicaid and CHIP enrollment and renewal processes, as of January 2025.Seniors and People with Disabilities
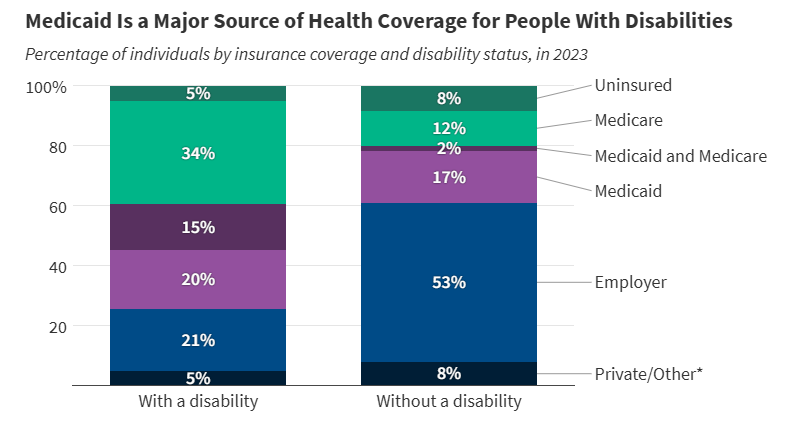 More than 1 in 3 people with disabilities (15 million) have Medicaid (35%). In comparison, only 19% of people without disabilities have Medicaid.
More than 1 in 3 people with disabilities (15 million) have Medicaid (35%). In comparison, only 19% of people without disabilities have Medicaid.Children with Special Needs
 Amid debates about proposed cuts to federal Medicaid spending, this brief analyzes key characteristics of children with special health care needs and explores how Medicaid provides them with coverage.
Amid debates about proposed cuts to federal Medicaid spending, this brief analyzes key characteristics of children with special health care needs and explores how Medicaid provides them with coverage.People With Intellectual and Developmental Disabilities
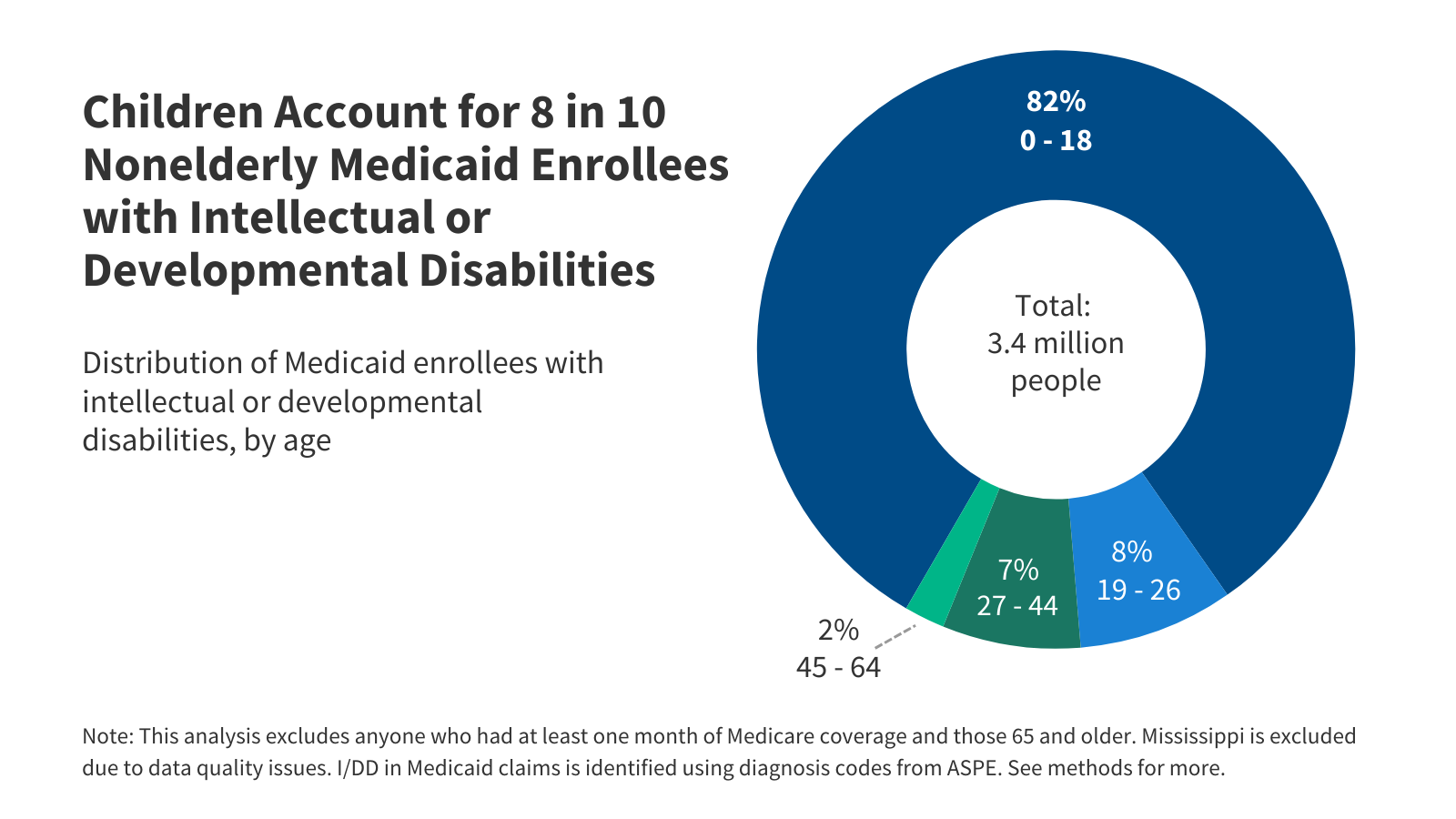 Among the estimated 8 million people with intellectual and developmental disabilities (I/DD), over three million have Medicaid coverage.
Among the estimated 8 million people with intellectual and developmental disabilities (I/DD), over three million have Medicaid coverage.Adults with Chronic Conditions
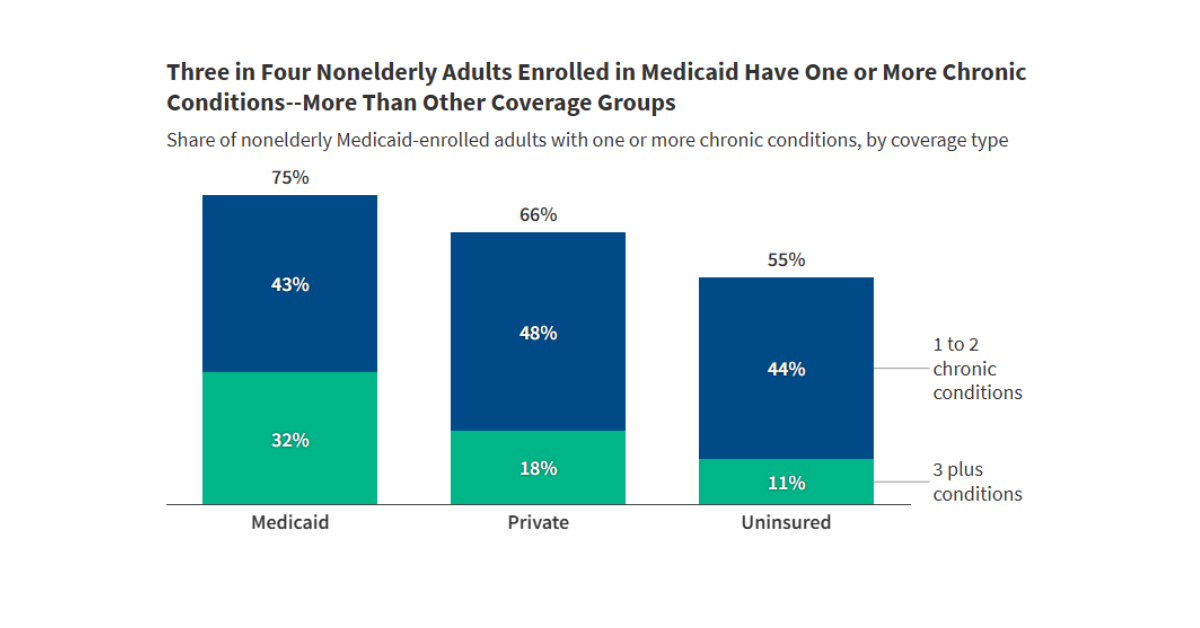 Among working age adults enrolled in Medicaid, approximately three quarters have one or more chronic conditions, and nearly one-third have three or more.
Among working age adults enrolled in Medicaid, approximately three quarters have one or more chronic conditions, and nearly one-third have three or more.
Latest News
-

When It Comes to Health Insurance, Federal Dollars Support More Than ACA Plans
-
Trump Required Hospitals To Post Their Prices for Patients. Mostly It’s the Industry Using the Data.
-

Nuevas reglas de trabajo de Medicaid podrían impactar más fuerte en adultos de mediana edad
-

New Medicaid Work Rules Likely To Hit Middle-Aged Adults Hard
Subscribe to KFF Emails
Choose which emails are best for you.
Sign up here