Under the Radar: States Vary in Regulating and Reporting COVID-19 in Assisted Living Facilities
Since the COVID-19 pandemic first surfaced in the United States, the number of cases and deaths in long-term care (LTC) facilities has been rising. As of June 4, 2020, over 43,000 COVID-19 related resident and staff deaths have been reported in nursing homes and other long-term care facilities, which is a conservative estimate because not all states publish these data. Among 41 states reporting COVID-19 LTC data at the state level, long-term care facility residents account for 50% or more of all COVID-19 deaths in 27 states. The increase in deaths among long-term care facility residents and staff has become an urgent concern for federal and state policymakers, the long-term care industry, family members of residents, residents themselves, and the general public.
In response to these concerns, on March 13, 2020, the Centers for Medicare & Medicaid Services (CMS) released guidance to limit the spread of the novel coronavirus to nursing home residents and staff, pertaining to visitors and staff screening. On April 2, CMS released guidance recommending universal use of facemasks by nursing home staff, and use of full Personal Protective Equipment (PPE) in facilities with known or suspected COVID-19 cases. As of May 8, nursing facilities are also required by CMS to report COVID-19 cases and deaths to the Centers for Disease Control and Prevention (CDC), and on May 18, CMS released guidance for states related to reopening nursing homes.
Notably, the CMS guidance and reporting requirements apply specifically to nursing facilities that fall under federal regulatory purview, leaving it to states to establish standards for assisted living facilities (ALFs) and other congregate living facilities. Assisted living facilities are home to over 800,000 mostly frail, elderly residents, who also face elevated risk of severe illness if they contract COVID-19, according to the CDC. While a great deal of attention has been paid to efforts to prevent and contain outbreaks of COVID-19 in nursing homes, assisted living facilities have been largely overlooked.
This analysis examines how states are regulating assisted living facilities in response to the COVID-19 pandemic, based on state-issued guidance for assisted living facilities on three key measures identified by CMS pertaining to visitors to facilities, daily staff screening, and universal use of PPE by facility staff, for each of the 50 states and DC. In addition, we tally state-level data on COVID-19 cases and deaths in assisted living facilities among states reporting such data as of June 8, 2020. The estimates reported here represent a subset of the COVID-19 cases and deaths data for long-term care facilities overall, as reported in other KFF analyses. (See Methods for details).
Key Takeaways
- Ten states impose restrictions on assisted living facilities that are identical to those established by CMS for nursing facilities, i.e., prohibit visitors, require staff screening, and require staff use of PPE.
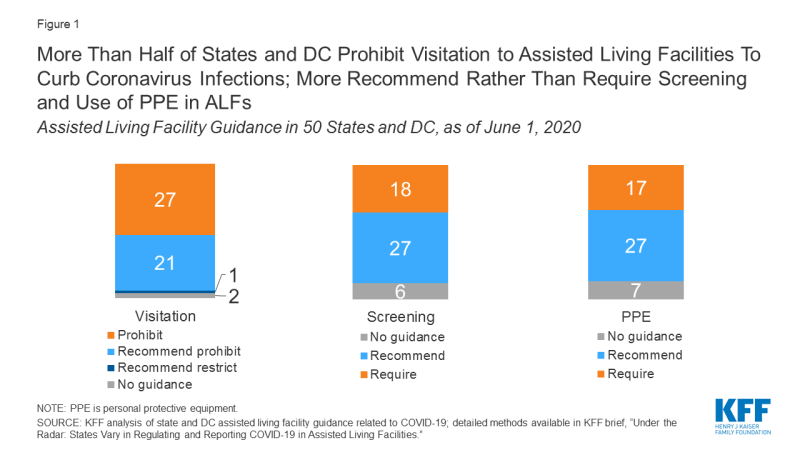
- A majority of states prohibit visits to assisted living facilities (26 states plus DC) but recommend rather than require daily staff screening (27 states) and staff use of PPE (27 states).
- Only 16 states report COVID-19 case and/or death data for assisted living facilities, either as a separate category (11 states) or combined with other long-term care facilities, other than nursing homes (5 states). Only 6 states report COVID-19 deaths occurring in assisted living facilities specifically.
- Among the 11 states reporting COVID-19 cases for assisted living facilities specifically, a total of 7,703 cases among residents and staff have been reported. Among the six states reporting COVID-19 deaths for assisted living facilities specifically, a total of 643 deaths have been reported.
Variations in guidelines for assisted living facilities across states results in a patchwork of protections against COVID-19 that is likely to result in uneven effects across the country. However, given the paucity of state-reported data on case and death numbers in assisted living facilities specifically, the picture of disease incidence and mortality in these facilities is profoundly incomplete, and undoubtedly an undercount.
Guidance for Assisted Living Facilities Related to COVID-19 Varies across States
We found significant variation in COVID-19 guidance issued to assisted living facilities across states related to visitors, staff screening, and staff use of PPE.
Ten states impose restrictions on assisted living facilities which are identical to those established by CMS for nursing facilities, while other states are mixed in whether they require or recommend adherence to the guidelines in one or more of these areas (Table 1). A handful of states have not issued any guidance in one or more of these areas as of June 1, 2020, including one state (South Dakota) with no guidance issued in any of the three areas.
- Visitors. More than half of all assisted living facilities in states and DC prohibit visitors (26 states plus DC), while 21 states recommend that assisted living facilities prohibit visitors, and two states provide no guidance on visitation to assisted living facilities (Figure 1).
- Staff screening. More states recommend than require daily screening of staff for illness in assisted living facilities: 27 states recommend, and 17 states plus DC have this requirement. Six states have not issued guidance related to staff screening.
- Use of personal protective equipment. More states recommend rather than require staff to use PPE in assisted living facilities: 27 states recommend, and 16 states plus DC require. Seven states have issued no guidance related to PPE use.
Relatively Few States Report COVID-19 Cases and Deaths Separately for Assisted Living Facilities
Our analysis shows that, as of June 8, 2020, 16 states report COVID-19 data for assisted living facilities, including 11 states that report data for assisted living facilities as its own category [CO, CT, FL, MA, MS, ND, NV, OH, RI, TX, UT] and five states that report COVID-19 data for assisted living facilities with congregate settings other than nursing homes, which are separately reported [CA, LA, NC, NY, SC]. Our analysis does not include data for the 23 states and DC that do not report COVID-19 data for assisted living facilities separately from nursing facilities; seven states that report data for nursing facilities, but not for assisted living facilities; and four states that do not report any state-level data.
COVID-19 Cases in Assisted Living Facilities
- Among the 11 states [CO, CT, FL, MA, MS, ND, NV, OH, RI, TX, UT] reporting COVID-19 cases for assisted living facilities specifically, a total of 7,703 cases among residents and staff have been reported. This total includes 3,829 cases among residents, 1,135 cases among staff, and 2,739 cases among residents and staff not separately reported in two states [MA and UT].
- Among the four states [CA, LA, NC, SC] that report COVID-19 cases occurring in a non-nursing facility category that includes, but is not limited to, assisted living facilities, a total of 3,386 COVID-19 cases have been reported among residents and staff. This includes 2,419 cases among residents and 967 cases among staff, with only three states reporting on the latter.
Covid-19 Deaths in Assisted Living Facilities
- Among the six states [CO, CT, NV, RI, TX, MS] reporting COVID-19 deaths for assisted living facilities specifically, a total of 643 deaths have been reported. This includes 642 deaths among residents and one death among staff, with only two states (CO and NV) reporting on the latter.
- Among the five states [CA, LA, NC, NY, SC] that report COVID-19 deaths in non-nursing facilities including, but not limited to, assisted living facilities, a total of 840 deaths have been reported. This includes 810 deaths among residents and 30 deaths among staff, with only three states reporting on the latter.
Discussion
With national attention focused on the rising number of COVID-19 deaths in nursing homes, this analysis takes a closer look at protections and COVID-19 cases and deaths in assisted living facilities. We found significant variation across states in assisted living facility regulations related to visitation, daily staff screening, and use of PPE, and a dearth of states reporting COVID-19 cases and deaths among residents and staff in these facilities specifically. In the majority of states, regulatory measures meant to protect assisted living facility residents and staff from COVID-19 infection are currently far less stringent than federal recommendations for nursing facilities. In the absence of uniform surveillance and reporting, little is known about the extent to which facilities are adhering to state guidelines or whether states are monitoring their enforcement.
In an effort to control outbreaks in LTC facilities, some states have instituted universal testing of nursing facility residents and staff. While some states, such as Connecticut and New York, now mandate universal testing of staff in both nursing homes and assisted living facilities, some state and national LTC associations are reporting that fewer states are testing both assisted living facilities residents and staff in addition to nursing facility residents and staff. Widespread adoption of universal testing in all LTC facilities and other congregate settings may not be possible, due to limited testing capacity nationwide. While regular screening of residents and staff for fever and respiratory symptoms is now a matter of protocol in most LTC facilities, screening only picks up symptomatic COVID-19 cases, whereas testing can identify asymptomatic carriers as well.
With many governors now moving toward relaxing restrictions that aim to slow the spread of coronavirus infections, some state guidance issued for assisted living facilities will soon expire (unless renewed). For example, executive orders issued by Michigan and Alabama will expire on June 26 and July 3, 2020, respectively. Other states, such as Arizona and North Carolina, have mandated that guidance pertaining to LTC facilities generally will expire upon termination of the state’s emergency declaration related to COVID-19. Ohio recently announced that visits to assisted living facilities will be allowed outdoors starting June 8, but visitors to nursing facilities will remain prohibited.
In terms of reporting of COVID-19 cases and deaths in long-term care facilities, the absence of uniform state reporting requirements for assisted living facilities makes it challenging to contextualize the numbers from the 16 states currently reporting such data separately from other types of long-term care facilities. For example, while CMS now reports the total number of resident beds in each nursing facility with COVID-19 cases, only three out of the 16 states reporting case and death data for assisted living facilities separate from nursing homes (Massachusetts, Connecticut, and North Dakota) also report the number of beds in each facility. This makes it challenging to examine the relationship between facility capacity and number of COVID-19 cases and deaths in assisted living facilities. Furthermore, total COVID-19 case and death counts for assisted living facilities would undoubtedly be much larger if data were released by all states, as CMS now requires for nursing homes nationwide.
This analysis confirms a patchwork state-based regulatory approach to establishing measures to limit the spread of coronavirus infection among assisted living facility residents and staff, and in reporting COVID-19 cases and deaths in assisted living facilities. This situation mirrors a larger national trend in the COVID-19 response, whereby some states have taken more aggressive actions than others and the federal government assumes a “backup” role. This state-by-state approach to the COVID-19 pandemic may result in uneven rates of illness, hospitalizations, and mortality among assisted living residents and staff across the country.