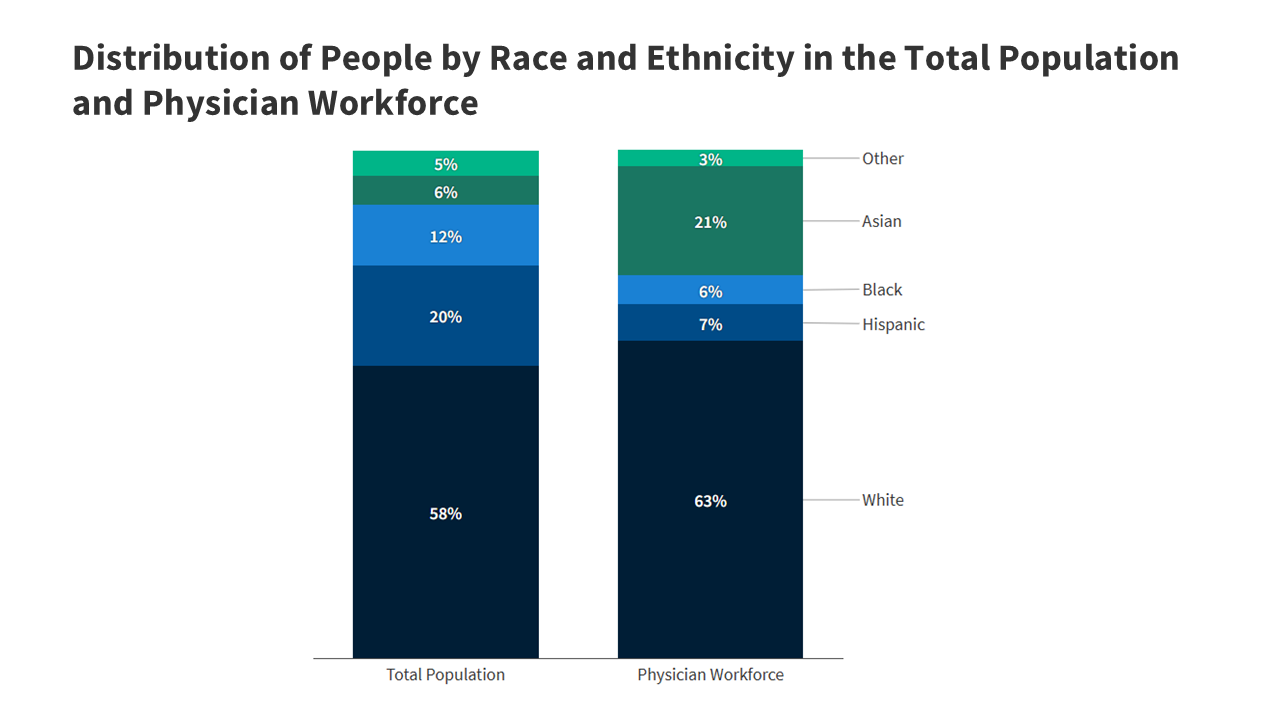
This brief provides an introduction to what health and health care disparities are, why it is important to address them, what the status of disparities is today, recent federal actions to address disparities, and key issues related to addressing disparities in the future.
This timeline offers a historical view of significant U.S. federal policies and events spanning the early 1800s to today that have influenced present-day health disparities.
Addressing persistent racial and ethnic disparities in health and health care is important for improving the nation’s health and economic prosperity. KFF explains such disparities and the factors that drive them, examines the actions to address them, and outlines future considerations.
Racial and ethnic disparities in health and health care remain a persistent challenge in the United States. An updated KFF resource examines how people of color fare compared to White people across 64 measures of health, health care, and social determinants of health.