This brief provides five key facts on Medicaid and immigrants as context for understanding the potential impacts of policy changes under the Trump administration.
This brief explains the role of Medicaid for hospitals, including how much spending on hospital care comes from Medicaid, the share of births covered by the program, and how Medicaid expansion has impacted hospital finances.
As the largest public payer for family planning services in the US, changes to Medicaid could have a large impact on access to contraception and other family planning care for low-income individuals.
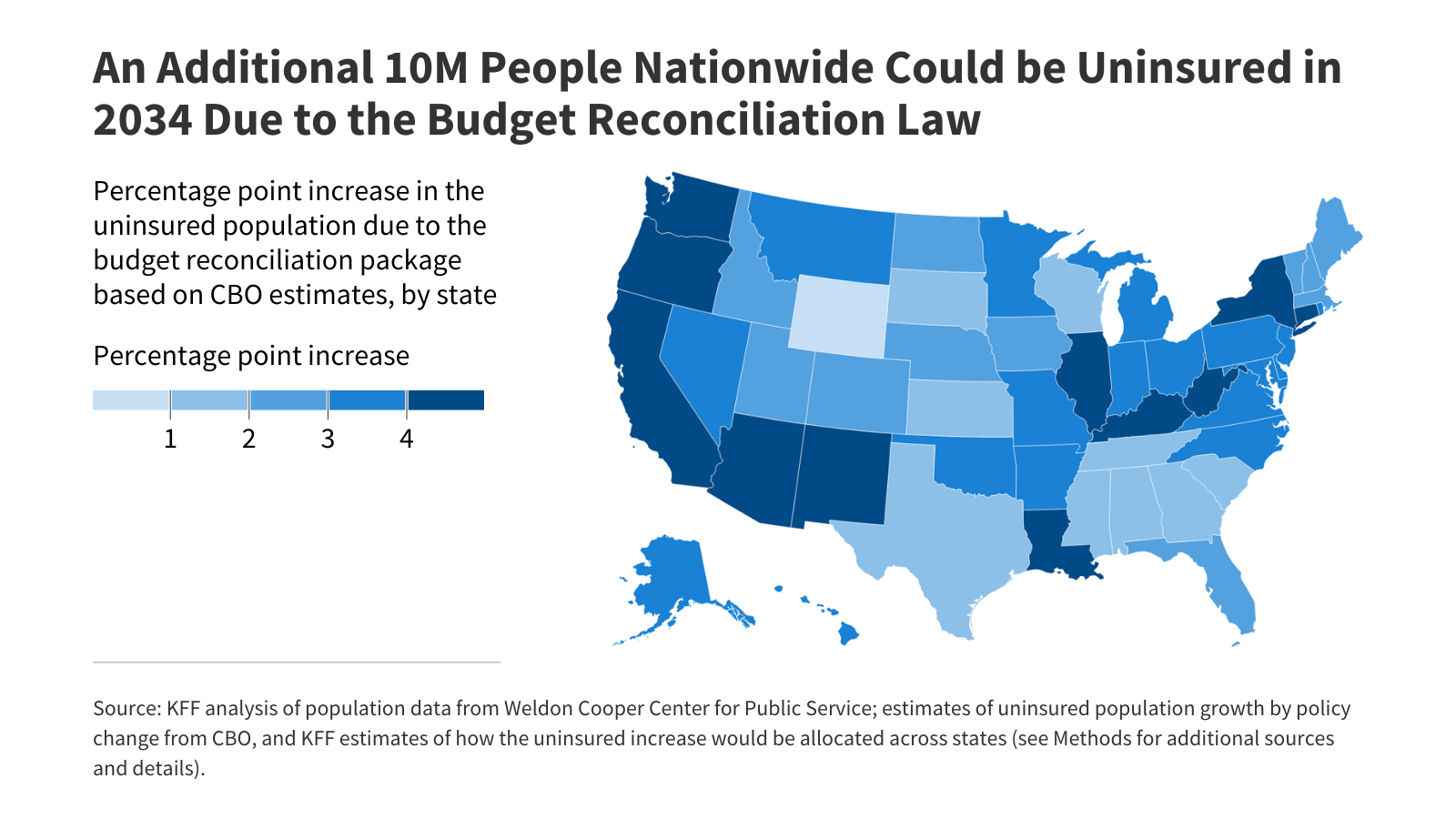
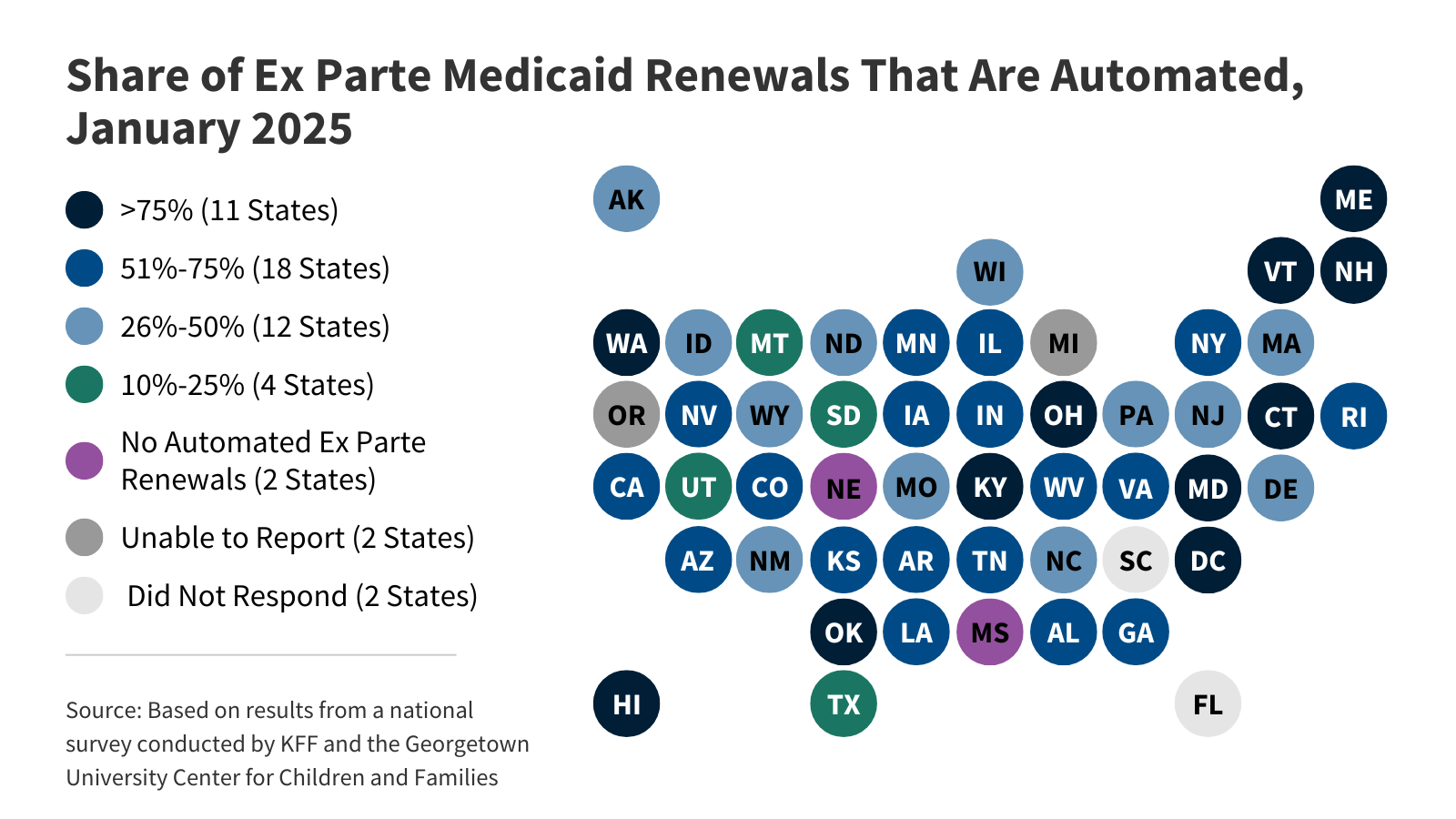
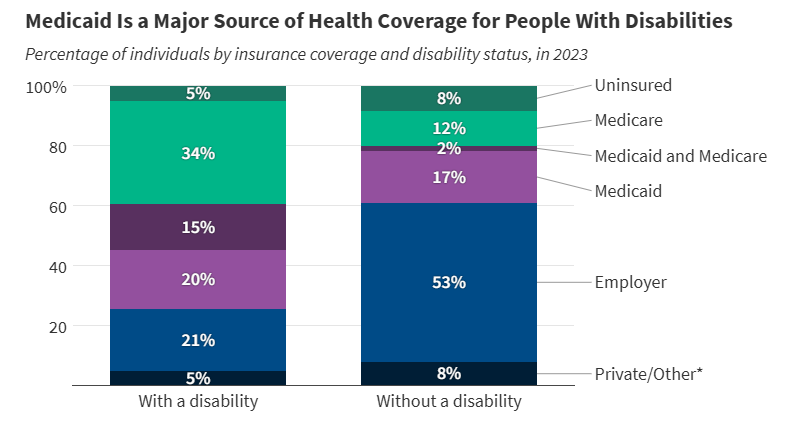
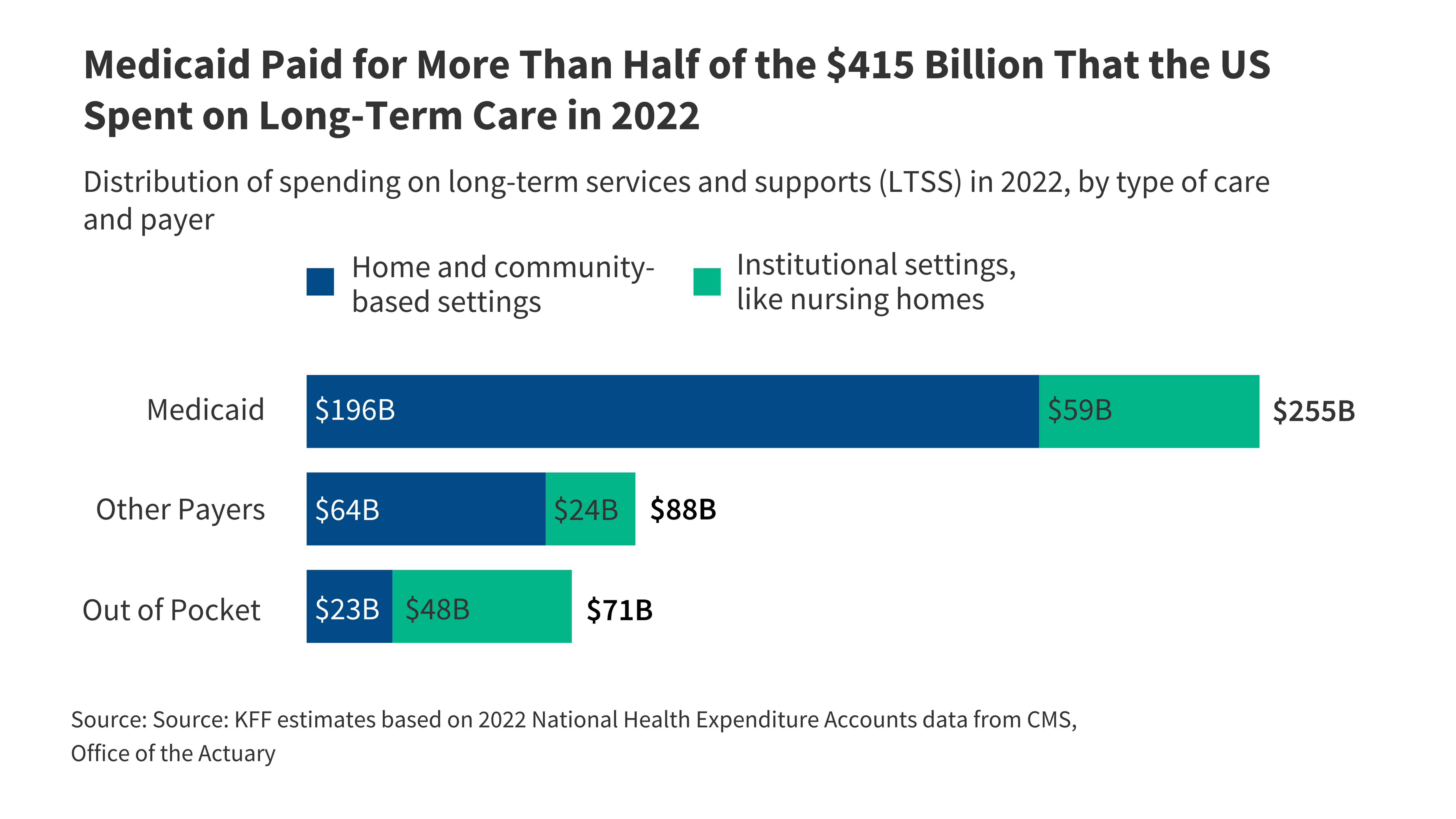
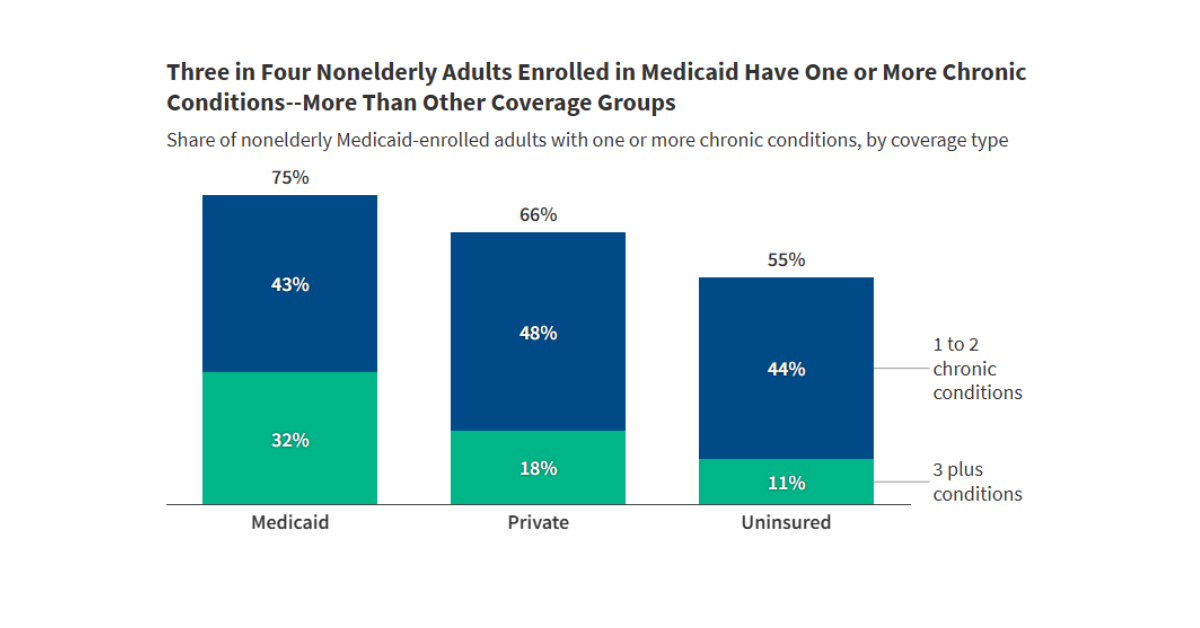
The budget reconciliation bill that includes significant changes to the Medicaid program. Many of the reductions in coverage will be among the 22 million Medicaid enrollees ages 50 and older.
The substantial Medicaid savings in the reconciliation bill could have major implications for nearly 15,000 federally certified nursing facilities and the 1.2 million people living in them.