Medicaid
The Essentials
5 Facts: Medicaid and Provider Taxes
As Congress weighs potential cuts in federal Medicaid spending, one option under consideration is to limit the use of state taxes on providers. This brief describe states’ current provider taxes and the federal rules governing them.5 Facts: Medicaid Work Requirements
This brief highlights five key facts about Medicaid work requirements, including the share of Medicaid enrollees who currently work, what research shows about the impact of work requirements, and the administrative burdens associated with implementing them.Implementing National Work Requirements
Federal Medicaid work requirements raise many operational and implementation questions, particularly considering the experience of Arkansas and Georgia with implementing work requirements through waivers.Medicaid Financing: The Basics
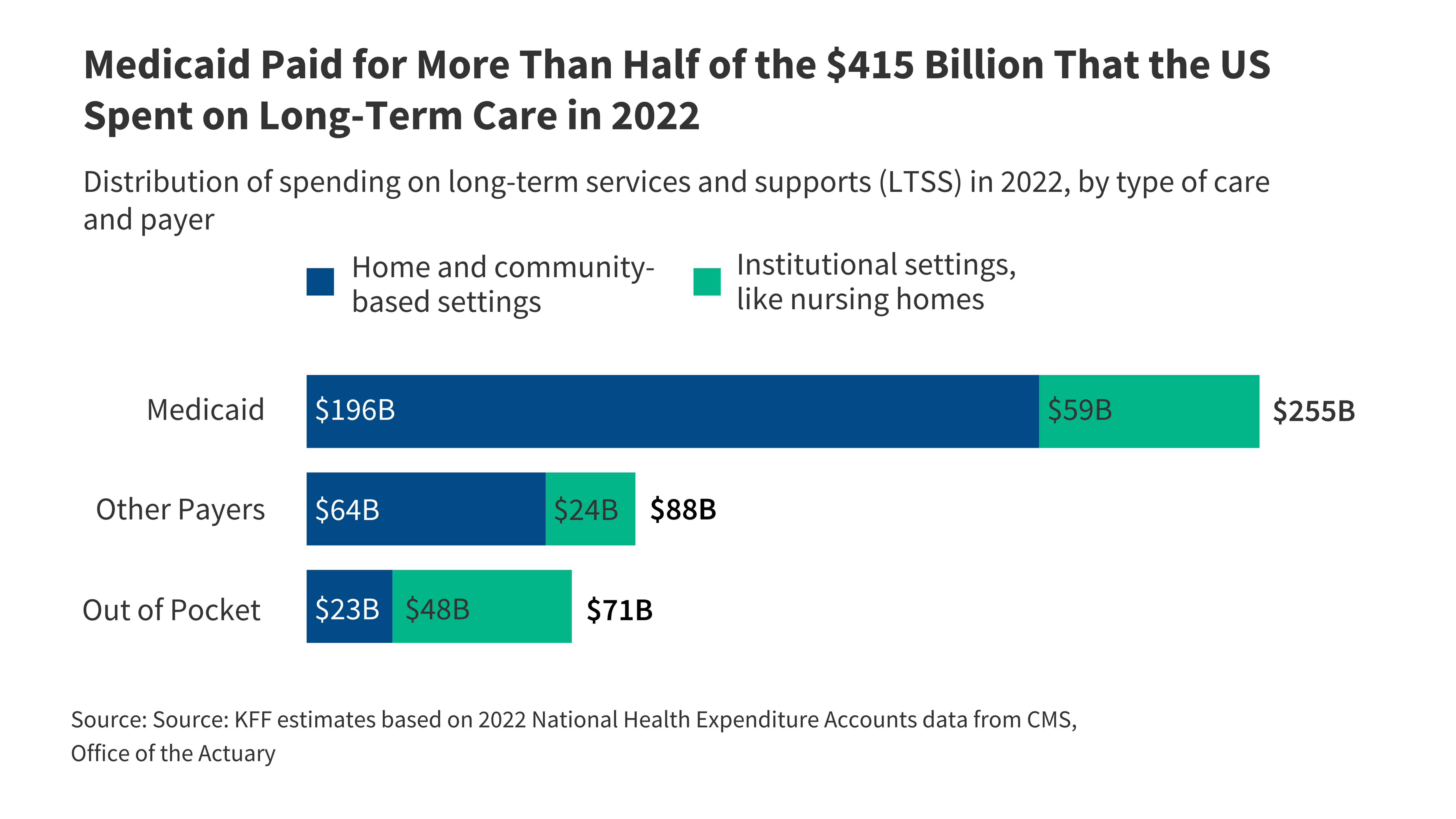
Medicaid represents $1 out of $6 spent on health care in the U.S. and is the major source of financing for state health coverage and long-term services and supports for low-income residents.
Eligibility and coverage
Eligibility, Enrollment, and Renewal Policies
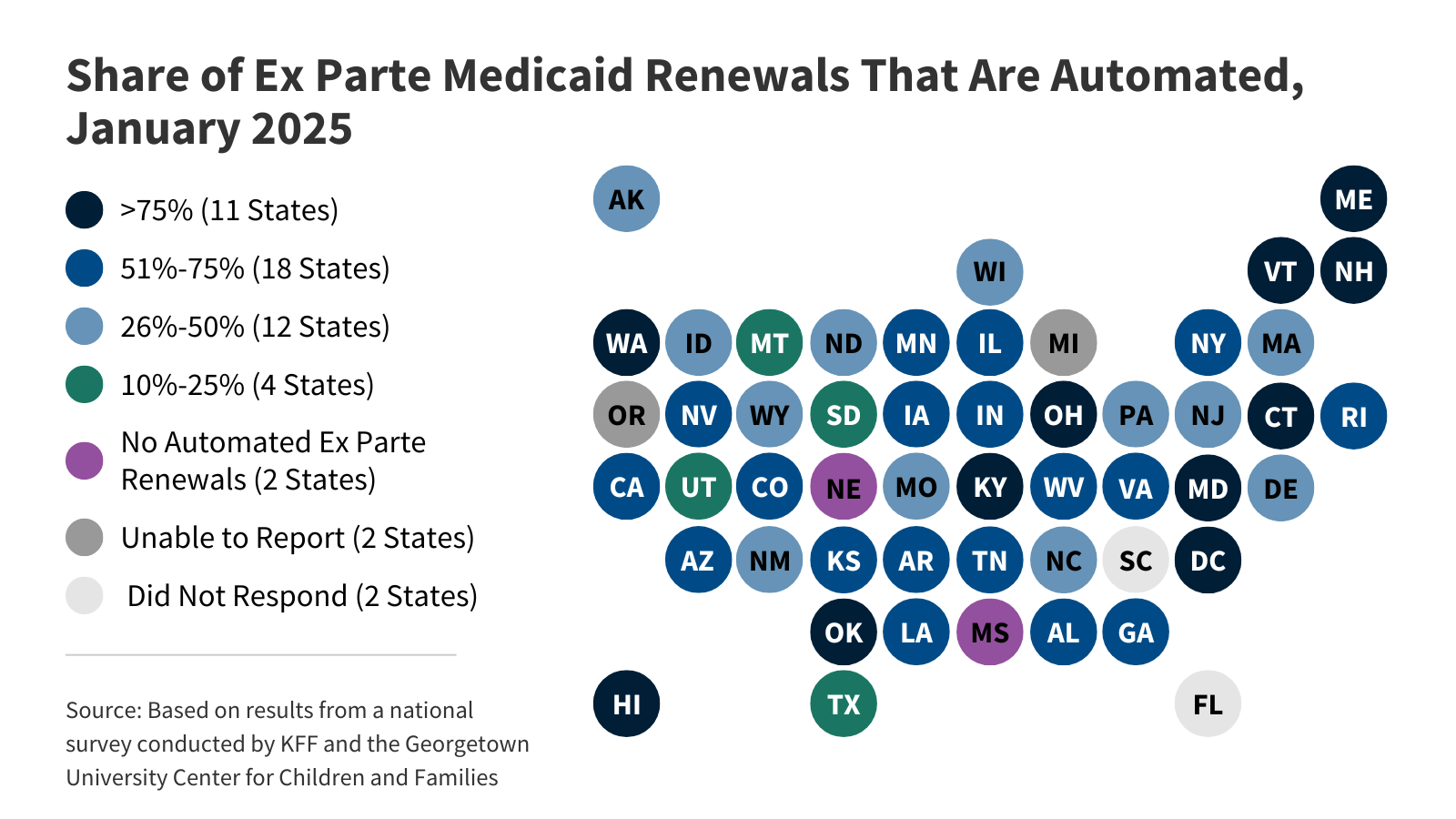 KFF's survey findings capture state actions that seek to improve the accuracy and efficiency of Medicaid and CHIP enrollment and renewal processes, as of January 2025.
KFF's survey findings capture state actions that seek to improve the accuracy and efficiency of Medicaid and CHIP enrollment and renewal processes, as of January 2025.Seniors and People with Disabilities
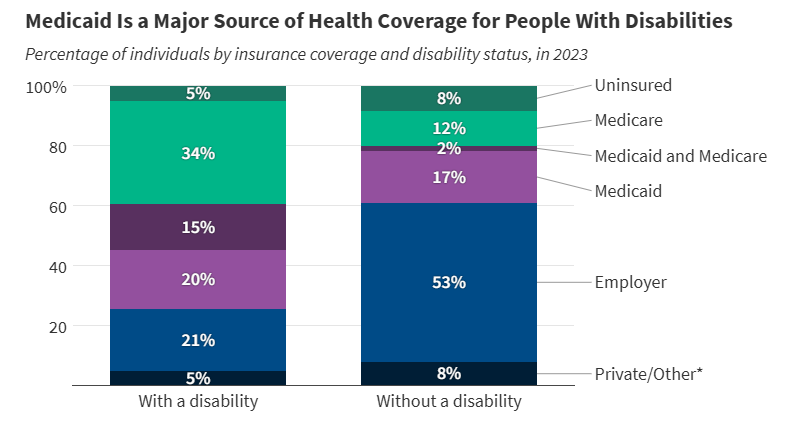 More than 1 in 3 people with disabilities (15 million) have Medicaid (35%). In comparison, only 19% of people without disabilities have Medicaid.
More than 1 in 3 people with disabilities (15 million) have Medicaid (35%). In comparison, only 19% of people without disabilities have Medicaid.Children with Special Needs
 Amid debates about proposed cuts to federal Medicaid spending, this brief analyzes key characteristics of children with special health care needs and explores how Medicaid provides them with coverage.
Amid debates about proposed cuts to federal Medicaid spending, this brief analyzes key characteristics of children with special health care needs and explores how Medicaid provides them with coverage.Adults with Mental Illness
 Options under consideration in Congress to significantly reduce Medicaid spending could have major implications for adults who live with mental illness.
Options under consideration in Congress to significantly reduce Medicaid spending could have major implications for adults who live with mental illness.Adults with Chronic Conditions
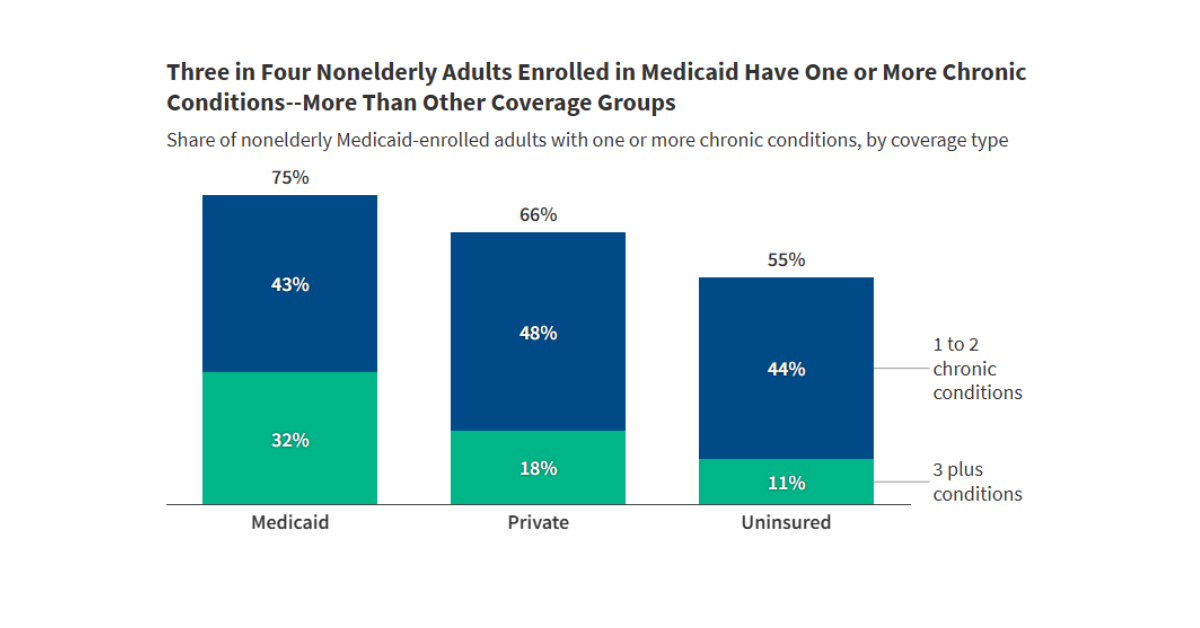 Among working age adults enrolled in Medicaid, approximately three quarters have one or more chronic conditions, and nearly one-third have three or more.
Among working age adults enrolled in Medicaid, approximately three quarters have one or more chronic conditions, and nearly one-third have three or more.
key facts about medicaid
5 Facts: Immigrants and Medicaid
This brief provides five key facts on Medicaid and immigrants as context for understanding the potential impacts of policy changes under the Trump administration.5 Facts: Medicaid and Hospitals
This brief explains the role of Medicaid for hospitals, including how much spending on hospital care comes from Medicaid, the share of births covered by the program, and how Medicaid expansion has impacted hospital finances.5 Facts: Medicaid and Family Planning
As the largest public payer for family planning services in the US, changes to Medicaid could have a large impact on access to contraception and other family planning care for low-income individuals.5 Facts: Medicaid for People 50 and Older
The budget reconciliation bill that includes significant changes to the Medicaid program. Many of the reductions in coverage will be among the 22 million Medicaid enrollees ages 50 and older.5 Facts: Medicaid and Nursing Facilities
The substantial Medicaid savings in the reconciliation bill could have major implications for nearly 15,000 federally certified nursing facilities and the 1.2 million people living in them.
Latest News
-

Native Americans Want To Avoid Past Medicaid Enrollment Snafus as Work Requirements Loom
-
KFF Health News' 'What the Health?': Happy 60th, Medicare and Medicaid!
-

Health Care Groups Aim To Counter Growing ‘National Scandal’ of Elder Homelessness
-

CDC Staff Tell Journalist They Felt Targeted Even Before Atlanta Campus Shooting
Subscribe to KFF Emails
Choose which emails are best for you.
Sign up here