Exploring the Rise in Mental Health Care Use by Demographics and Insurance Status
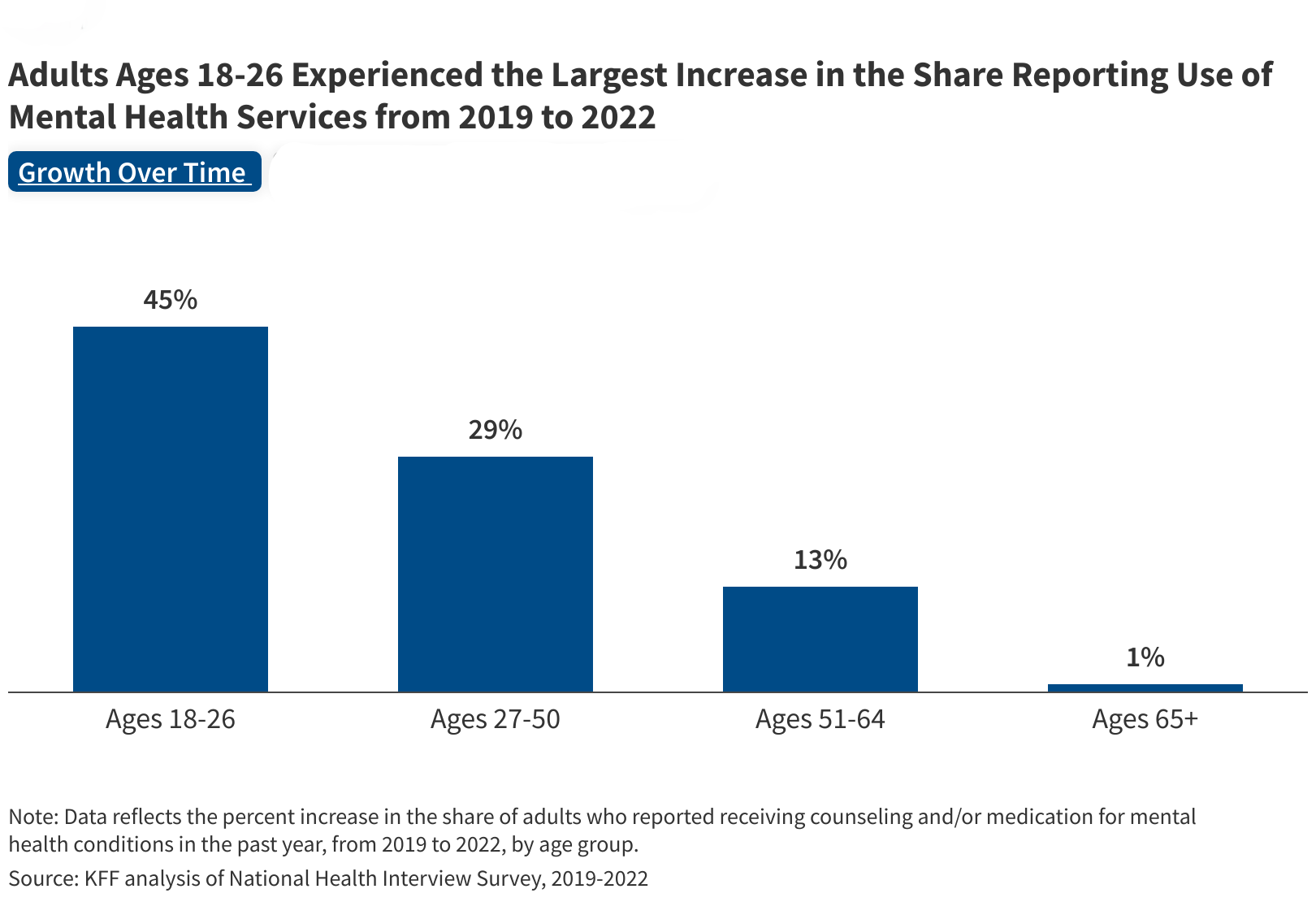
Many people experience mental health conditions, which raises questions about mental health service utilization patterns and what barriers exist with connecting people to services. This analysis explores the latest trends in utilization of mental health services and how it differs by demographics and insured status. It finds that the share of adults receiving mental health treatment has increased, particularly among young adults.