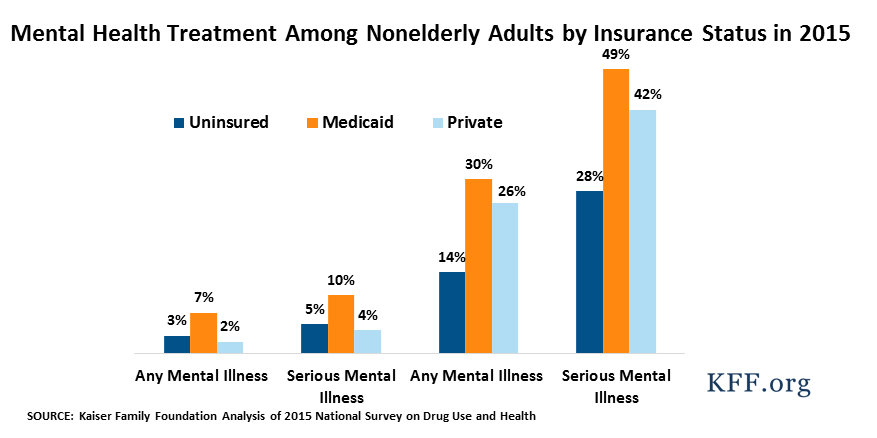
Facilitating Access to Mental Health Services: A Look at Medicaid, Private Insurance, and the Uninsured
This fact sheet provides a description of nonelderly adults with mental illness and compares receipt of mental health services among nonelderly adults with Medicaid, private insurance, and no insurance.