Community Health Centers in a Time of Change: Results from an Annual Survey
Executive Summary
With health centers playing an important role in the response to the coronavirus pandemic, findings from the KFF/Geiger Gibson 2019 Community Health Center Survey provide important information on health centers’ financial situation and their experiences in a changing policy environment. After years of growth following implementation of the Affordable Care Act (ACA), changes in Medicaid, public charge, and Title X family planning policies, among others, carry important implications for low-income patients as well as health center operations and revenue. While, overall, health center patient growth and revenue remain strong, some health centers had begun to feel the effects of these changes as they were being implemented across the nation. Federal legislation has directed additional resources to health centers in the wake of the current pandemic, but it is unclear what effect the current public health crisis will have on health centers. Findings from the survey include:
- Continuing trends following the ACA, most health centers reported patient coverage and patient care revenue remained stable or improved. One-third of health centers reported an increase in Medicaid patients, while 45% said the number had stayed the same in the past year. Similarly, three in ten health centers reported an increase in Medicaid revenue while nearly half reported no change.
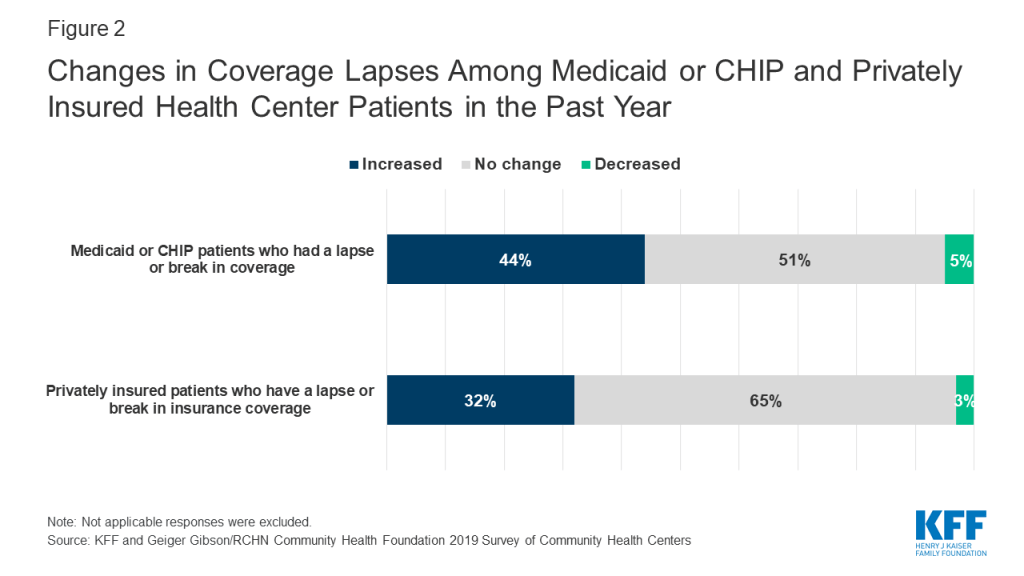
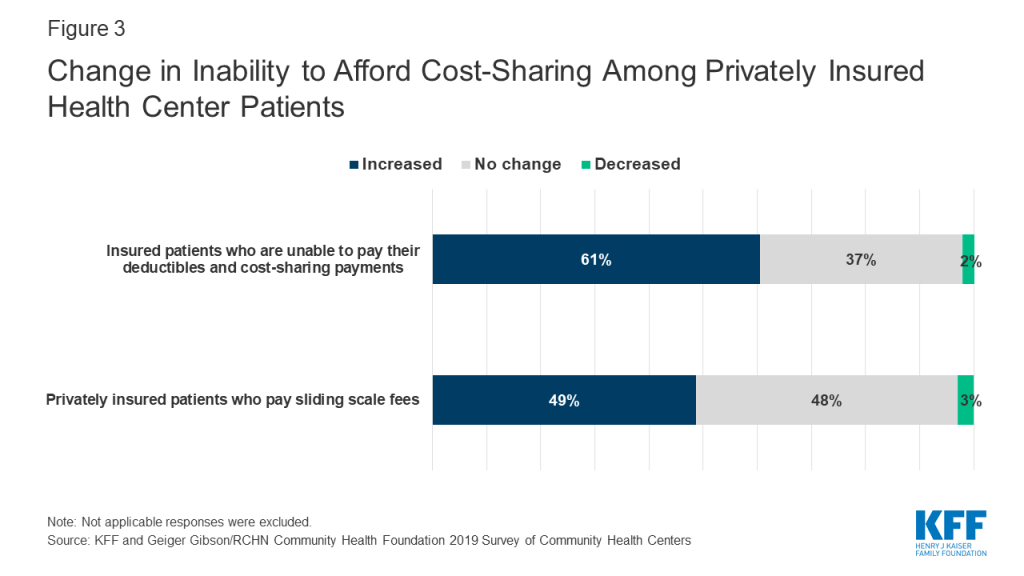
- However, a growing share of health centers reported coverage and affordability challenges for their Medicaid and privately insured patients. One in five health centers (22%) reported that the number of Medicaid patients served has declined in the past year, and 44% saw an increase in the share of Medicaid/CHIP patients with a lapse in coverage. Nearly half (49%) reported an increase in the share of privately insured patients paying sliding scale fees in the past year in lieu of deductibles and other cost sharing required by their private plan, in effect forgoing use of their insurance. Mirroring the share of health centers reporting a decline in Medicaid patients, 23% reported a Medicaid revenue decrease in the past year, up from 15% in 2018.
- There is a great deal of confusion among health center staff about the status of Medicaid work requirement waivers—most of which are on hold pending legal challenges—and health centers perceive many barriers to work and to reporting work activity for their patients. One in five respondents in states with an approved or pending waiver incorrectly identified the status of the state’s waiver or indicated that they did not know if the state had or was considering a waiver. Perceived barriers to work for patients who are not currently working included caring for family members, lack of transportation, mental health or substance use conditions, and lack of skills and education, among others.
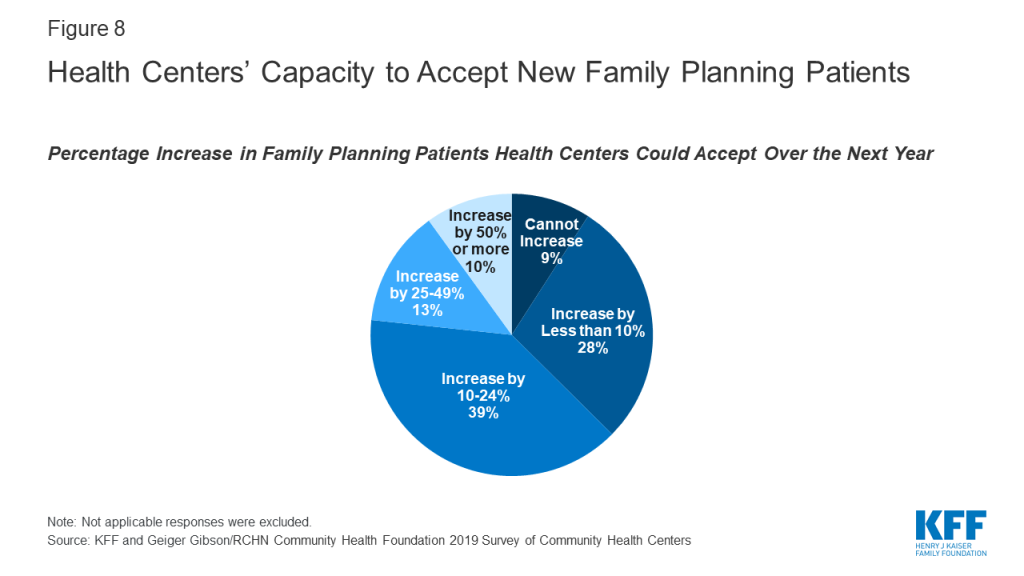
- Health centers reported limited capacity to expand family planning services as the Title X family planning program’s provider network constricts. Over three-quarters (77%) of health centers said they could increase the number of new family planning patients served by no more than 24%.
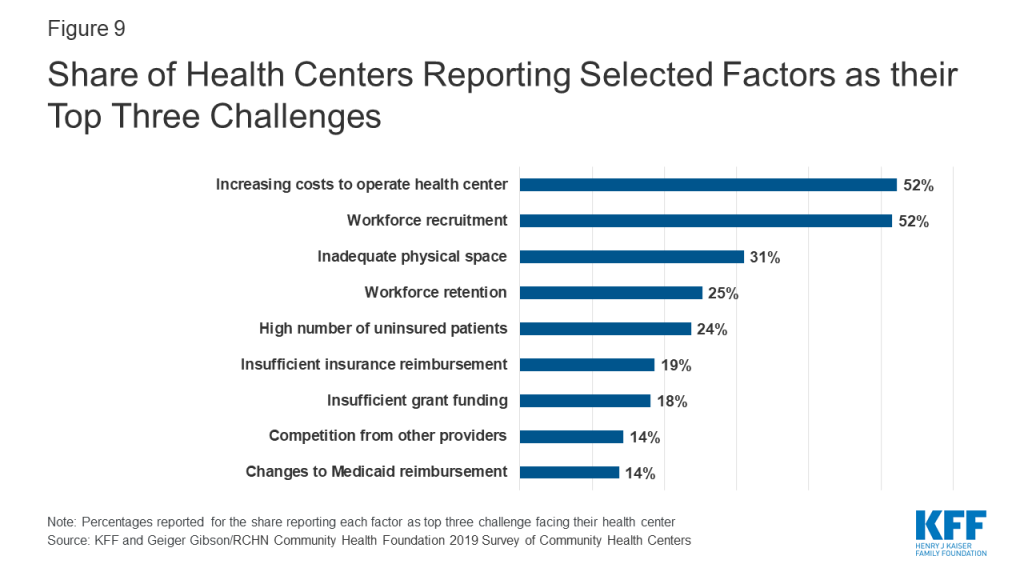
- The top three challenges facing health centers were workforce recruitment, increasing costs to operate the health center, and inadequate physical space. Health centers in non-expansion states also cited the high number of uninsured patients as a top challenge.
Introduction
Health centers are a significant source of care for low-income, medically underserved communities. They also serve as an essential part of the health care system’s response to public health emergencies and other disasters. They are playing an important role in responding to the current COVID-19 pandemic by providing COVID-19 testing as well as continuing to treat ongoing health needs of their patients. Federal legislation has provided emergency funding to support their response. Health centers experienced significant growth in service sites and patient care capacity following implementation of the ACA, which positions them well to respond to the current crisis; however, leading up to the current crisis, they had been facing more headwinds in their ability to serve patients because of recent federal policy changes.
As key providers of comprehensive primary care services in communities whose residents are more likely to experience poverty and its health effects, along with a shortage of accessible primary health care, health centers feel the effects of policies that limit benefits and services to low-income populations. As a result, changes to federal programs that provide health coverage and promote access to health care services for low-income populations can be expected to have a significant impact on health center patients and operations. Some of the policy changes that are having the biggest effects include: federal support for states interested in testing large-scale Medicaid eligibility and enrollment restrictions such as work requirements, premiums, and other policies; changes to “public charge” policies that expand the programs that can trigger public charge determinations for legal immigrants seeking to adjust to permanent legal status; and new constraints on providers that participate in the Title X family planning program.
This brief presents findings from the 2019 KFF/Geiger Gibson Community Health Center Survey on the experience of health centers in a changing policy environment. This survey was conducted before the current coronavirus crisis, and focused on changes in health center patient coverage and operations during the past year, as well as health centers’ experiences with Medicaid work requirements, and their responses to changes in the Title X program. Where appropriate, the brief also highlights differences in findings across health centers in Medicaid expansion and non-expansion states and those located in urban versus rural areas. The effects of the new public charge policy were described in an earlier brief.1 While the findings do not relate specifically to the coronavirus pandemic, they provide important context for understanding the issues facing community health centers prior to the current crisis.
Key Findings
Health coverage, affordability, and revenue
Five years following the ACA coverage expansions, most health centers reported the number of Medicaid patients had increased or stayed the same over the past year. In contrast to national trends showing Medicaid enrollment declines, one-third of health centers said the number of Medicaid patients had increased in the past year while 45% said the number had stayed the same (Figure 1). Health centers serve as an important source of care for Medicaid patients and as they continue to expand their service capacity, some are likely attracting new Medicaid patients.
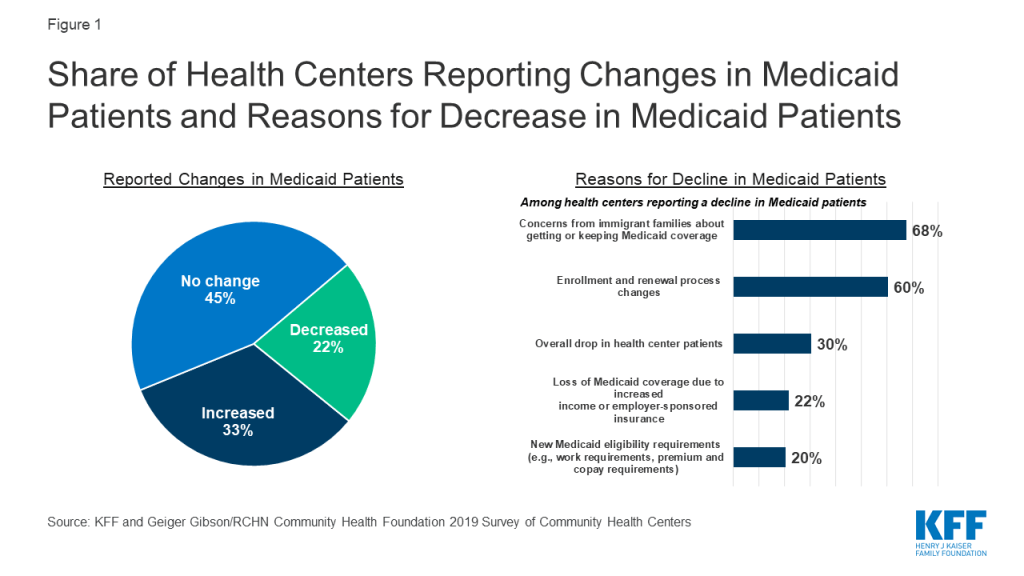
At the same time, one in five health centers said the number of Medicaid patients had declined. Health centers in non-expansion states were more likely to report their Medicaid patients had decreased (28% vs. 19% in Medicaid expansion states, data not shown). Among health centers reporting a decline, the most commonly reported reason for the decline (68%) was concerns among immigrant families about applying for or keeping Medicaid for themselves or their children. Nearly as common, six in ten health centers attributed the decline to changes in enrollment and renewal processes that make it more difficult for patients to obtain or keep Medicaid coverage, while three in ten cited an overall drop in the number of health center patients. The reasons cited for the decline differed by Medicaid expansion status and urban/rural status. Health centers in Medicaid expansion states were significantly more likely to attribute decreases in Medicaid patients to patients gaining jobs and losing Medicaid coverage due to increased income and/or employer-sponsored insurance (30% vs. 7% for non-expansion states, Appendix Table 1). Urban health centers were significantly more likely than rural health centers to report that concerns from patients in immigrant families about applying for or keeping Medicaid for themselves or their children explained the drop in Medicaid numbers (77% vs. 46%); while rural health centers were significantly more likely to cite declines in overall health center patient numbers (46% vs. 23% for urban) as a reason.
Health centers also reported an increase in coverage lapses among Medicaid and CHIP patients as well as those with private insurance. Over four in ten (44%) health centers reported an increase in coverage lapses for their Medicaid/CHIP patients, while a slightly smaller share of health centers (32%) reported coverage lapses among privately insured patients had increased (Figure 2). There are a number of reasons why people may experience a lapse or break in coverage. For Medicaid patients, the coverage lapses may stem from difficulties in renewing coverage. For privately insured patients, a break in coverage may reflect a change in employment and temporary loss of coverage or an inability to afford the monthly premium, among other reasons.
Health centers reported their privately insured patients face increasing challenges affording coverage. More than six in ten health centers (61%) reported an increase in the past year in the percentage of insured patients who are unable to pay their deductibles and cost-sharing payments, and nearly half (49%) reported an increase in privately insured patients paying sliding scale fees (Figure 3). Health center patients qualify for sliding fee scale payments based on their income. An increase in the number of patients with private insurance who pay the sliding fee scale in lieu of the health plan’s copayments or other cost sharing suggests those payments are unaffordable to the individual.
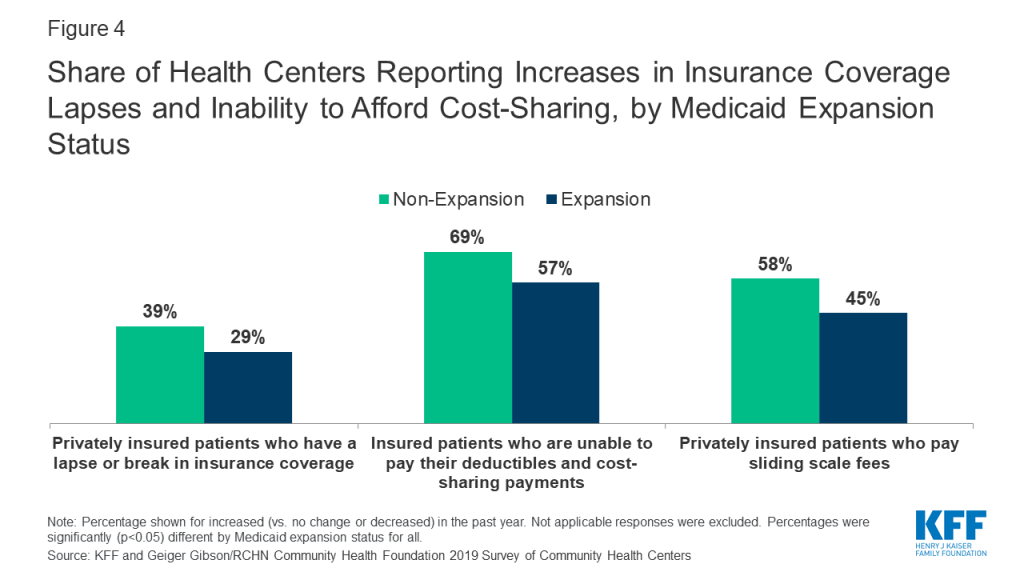
Health centers in non-expansion states were more likely to report affordability challenges for their privately insured patients. Health centers in non-expansion states were significantly more likely than health centers in Medicaid expansion states to report increases in the past year in patients’ inability to afford cost-sharing payments and in the percentage of privately insured patients paying sliding-scale fees (Figure 4). These differences may be explained, in part, by the higher rates of marketplace coverage among low-income patients in non-expansion states. In states that have not expanded Medicaid, low-income individuals with incomes above 100% of the poverty level may enroll in marketplace coverage, but will face cost sharing requirements that may be difficult for them to afford. Rural health centers were significantly more likely than urban health centers to report an increase in privately insured patients paying sliding scale fees (55% vs. 44%).
Health centers’ financial situation remains strong, with most reporting improved or stable financial factors in the past year; however, some health centers reported decreases in key revenue sources. Similar to findings on patient coverage, most health centers continue to benefit financially from the ACA coverage expansions and enhanced federal health center funding. Over half (51%) of health centers reported an increase in federal grant funding from annual appropriated funding, the Community Health Center Fund as well as from targeted grant funding, and three in ten reported an increase in Medicaid revenue (Figure 5). At the same time, a growing share of health centers reported a decrease in Medicaid revenue. In 2019, similar to the share of health centers reporting a drop in Medicaid patients, 23% of health centers reported a decline in Medicaid revenue compared to just 15% in 2018.2 As health centers’ single largest source of operating revenue (44% in 2018),3 Medicaid revenue declines may carry implications for health centers’ ability to add service sites, hire staff, and expand the scope of care they provide. Additionally, over three in ten health centers that received Title X grant funding reported a decrease in their funding in the past year.

Addressing social determinants of health
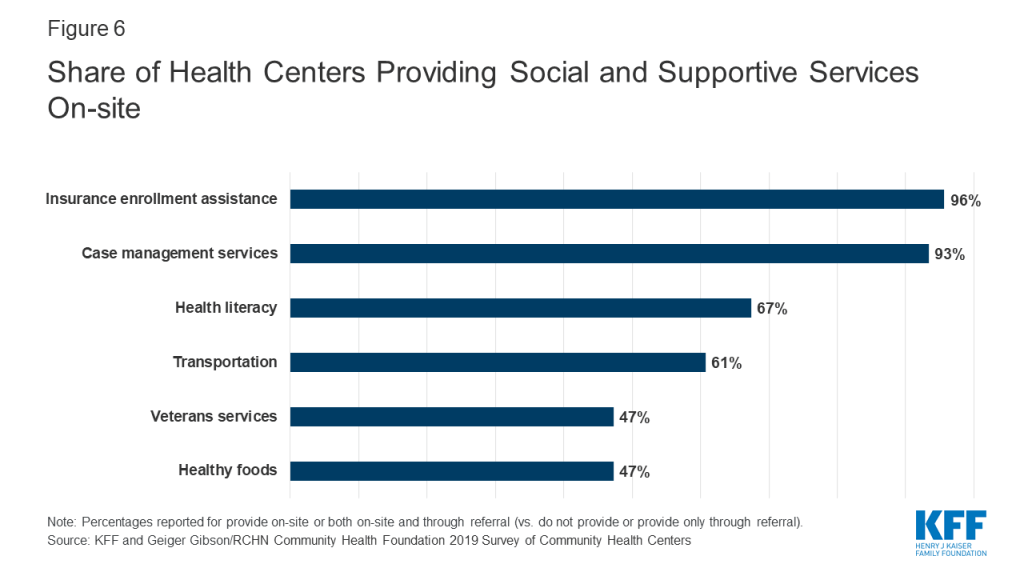
Health centers provide a range of social and supportive services aimed at addressing social determinants of health. Nearly all health centers reported providing insurance assistance services and case management services on-site (96% and 93%, respectively), and over six in ten health centers said they provided health literacy services (67%) and transportation services (61%) on-site (Figure 6). Nearly half (47%) reported providing healthy foods and veterans’ services. The provision of certain social and supportive services differed by Medicaid expansion status and between urban and rural health centers (Appendix Table 1). Health centers in non-expansion states were significantly more likely to provide veterans’, education, and agricultural worker support services on-site, while health centers in Medicaid expansion states were significantly more likely to provide insurance enrollment assistance services on-site. Urban health centers were significantly more likely to provide on-site transportation, SNAP, WIC, or other nutritional assistance, and refugee services, while rural health centers were significantly more likely to provide on-site agricultural worker support and veterans’ services (Appendix Table 1).
Potential implications of Medicaid work requirements
As of March 2020, the Centers for Medicare & Medicaid Services (CMS) had approved Medicaid Section 1115 waivers to implement work/community engagement requirements for ten states and ten state proposals are pending.4 At the same time, federal courts have set aside four approvals (Arkansas, Kentucky, Michigan, and New Hampshire) and work requirements in another four states with approved waivers—Arizona, Ohio, South Carolina, and Wisconsin—have not yet been implemented. Indiana, which has implemented work requirements, announced that it will temporarily suspend enforcement of the requirements pending the outcome of a legal challenge.5 A work demonstration was in effect and moving forward in Utah but was suspended on April 2, 2020 due to the COVID-19 pandemic.6 However, the future of these demonstrations may be in doubt following a ruling by a federal appeals court upholding a lower court’s decision striking down the work requirements in Arkansas. Before Arkansas’s work requirements program was halted by the court, over 18,000 Medicaid enrollees lost coverage; over 95% of those losing coverage either met the requirements or qualified for an exemption.7
Survey findings revealed a great deal of confusion and lack of information about the status of work requirement waivers and how those work requirements would be implemented. In states with an approved or pending waiver at the time of the survey, one in five respondents incorrectly identified the status of the state’s approved or pending waiver or indicated that they did not know if the state had or was considering a waiver. Among the survey respondents who correctly said that their state had an approved or pending waiver to implement Medicaid work/community engagement requirements or was considering developing a waiver, six in ten said their state had neither provided nor offered to provide training on the work requirements (Figure 7). Despite this lack of training from the state, nearly half (48%) of health centers reported they or their Primary Care Association (PCA) had provided or planned to provide training to their employees.
Most health centers indicated a desire to help patients with work reporting requirements and with obtaining exemptions; however, some health centers said they lacked the resources to do so. While over half (55%) of health centers in states with an approved or pending waiver said they were assisting or planned to assist patients with the new reporting requirements, more than three in ten (32%) said they were not providing or did not plan to provide the assistance (Figure 7). Most states include an exemption from work requirements for medically frail individuals; medical frailty determinations must be made by medical professionals. Although 52% of health center respondents reported state officials had not explained the process for determining patients as medically frail, 41% said they had the resources to conduct the determinations. However, reflecting the resource burden of making medical frailty determinations, six in ten (59%) said they did not have the resources or did not know if they had the resources to make these determinations.

Health centers perceive that their patients who are not currently working face many barriers to work. All health centers, regardless of their state’s waiver status, were asked about potential barriers to working among their adult, non-elderly, and non-disabled Medicaid patients who are not currently working. They reported a mix of health and mental health-related barriers as well as geographic and economic barriers to work. Over seven in ten health centers reported that many of their patients faced substance use disorders, acute or chronic mental health conditions, and acute or chronic physical health conditions (Appendix Table 1). Similar shares of health centers noted other barriers, such as child caring responsibilities, lack of transportation to jobs, or inadequate skills or education. Compared to health centers in rural areas, urban health centers were more likely to report as barriers preventing patients from working a mismatch between available jobs and patients’ skills and education and family caretaking responsibilities, while rural health centers were more likely than their urban counterparts to report a lack of jobs in the community, and the seasonal nature of many jobs.
Health centers also indicated their patients would likely face many barriers that would make it difficult for them to report work activity. In addition to confusion over reporting rules and deadlines, over half of health centers (57%) reported that lack of access to a computer would be a barrier for many patients and nearly half (47%) reported not having internet service would be a barrier for many patients, which would prevent them from being able to report work activity by phone or online, as required by several states (Appendix Table 2).
Participation in the Title X program and ability to accept new family planning patients
New rules governing the Title X family planning program went into effect on July 15, 2019, imposing new restrictions on grantee activities. These restrictions include blocking participation of program providers that also offer abortion services, barring staff from fully counseling pregnant patients about all options, and requiring mandatory referral of pregnant women for prenatal care regardless of patient choice. Before the restrictions took effect and as of June 2019, 4,008 Title X clinics were in operation. By December 20, 2019, all 410 Planned Parenthood health centers had withdrawn from the program, and an additional 631 Title X clinics, including some community health centers, were no longer participating in Title X.8 The decision to stop participating in Title X means the loss of funding to support family planning services at these clinics and health centers.
As of July 2019, a quarter of health centers reported participating in the Title X program, though that number may have changed following implementation of more restrictive rules. The share of health centers reporting receiving Title X funding was similar to the 26% who said they received Title X funding in 2017.9 Since the survey, which was conducted before the new rules went into effect, a significant number of health centers may have dropped their Title X participation, although a count is not available. Some health centers may perceive a conflict between the Title X counseling and referral ban and its physical and financial separation requirements and health centers’ patient care obligations under their funding authority (Section 330 of the Public Health Service Act).10 ,11
Health centers reported limited capacity to accept new family planning patients. With hundreds of clinics, including health centers, leaving the Title X program and their ability to serve family planning patients diminishing due to loss of funding, the need for alternative sources of care is expected to rise. Family planning services are part of the comprehensive primary care package that all health centers must furnish under Section 330.12 However, many health centers have limited capacity to expand these services. Over one-third (37%) of health centers reported either they could not expand patient load or they could expand by less than 10% with current staffing and clinic space; another 39% said they could increase the number of family planning patients by less than 25% (Figure 8). Despite limited capacity at some health centers, over one in five (23%) said they could expand capacity by 25% or more, including one in ten who said they could increase the number of family planning patients by 50% or more.
Challenges facing health centers
Despite ongoing policy challenges, health centers were more likely to report operational issues as top challenges. Over half of health centers (52%) cited workforce recruitment and increasing costs to operate their health center as top challenges, while three in ten (31%) cited inadequate physical space as a top challenge (Figure 9). A quarter of health centers reported workforce retention (25%) and high numbers of uninsured patients (24%) as major challenges. Health centers in Medicaid expansion states were more likely than health centers in non-expansion states to report workforce recruitment as a top-three challenge (55% vs. 43%), while health centers in non-expansion states were more likely than those in expansion states to report high numbers of uninsured patients as a top-three challenge (45% vs. 15%, Appendix Table 1). Rural health centers also face provider shortages and were significantly more likely to report workforce recruitment as a top-three challenge (60%) compared to urban health centers (45%). These ongoing challenges, particularly the workforce and financial challenges, are likely to be exacerbated during the current COVID-19 crisis as frontline workers get sick and others must take time off to care for children and other family members, and as health centers face potentially precipitous declines in patient care revenue.
Discussion
As federal policymakers turn to health centers during this time of crisis, they will play an important role in providing access to COVID-19 testing as well as ongoing primary care services for low-income, medically underserved communities. However, even as health centers continue their historic growth brought about by the ACA that may position them well to respond to the crisis, some have encountered limits on their ability to meet the needs of their patients because of recent policy changes, especially those that have resulted in recent declines in Medicaid coverage. While many states and the federal government have temporarily suspended some policies that create barriers to enrolling in Medicaid or to maintaining Medicaid coverage during the emergency, the reinstatement of these policies after the immediate emergency ends could make it harder for health centers to serve their communities in the longer term.
Through coronavirus response legislation, the federal government directed an initial $100 million to health centers13 and later directed over $1.3 billion in emergency grants to health centers to enable them to continue serving their patients during the crisis, and funded the Community Health Center Fund through November 2020.14 Yet, the economic upheaval from this pandemic is likely to persist long after the threat from the virus diminishes. While over half of health centers reported that federal grant funding had increased in the past year, the failure of Congress to pass a long-term extension of the Community Health Center Fund threatens to jeopardize the stable funding health centers have experienced for the past decade. The importance of stable future funding will be even greater in the aftermath of the pandemic as health centers seek to resume normal operations.
Methods
The 2019 Survey of Community Health Centers was jointly conducted by KFF and the Geiger Gibson/RCHN Community Health Foundation Research Collaborative at George Washington University’s Milken Institute School of Public Health. The survey was administered in partnership with the National Association of Community Health Centers (NACHC). The survey was fielded from May to July 2019 and was emailed to 1,342 CEOs of federally-funded health centers in the 50 states and the District of Columbia (DC) identified in the 2017 Uniform Data System (UDS). The response rate was 38%, with 511 responses from 49 states and DC.
The survey data were weighted using 2017 UDS variables for total health center patients, the percentage of patients reported as racial/ethnic minorities, and total revenue per patient. Survey findings are presented for all responding health centers and responses were analyzed using chi-squared tests to compare responses between health centers in Medicaid expansion and non-expansion states and15 health centers in rural and urban locations (based on a UDS variable).State Medicaid expansion status was assigned as of the survey fielding period.
Jessica Sharac, Anne Markus, and Sara Rosenbaum are with the Geiger Gibson Program in Community Health Policy at the George Washington University. Additional funding support for this brief was provided to the George Washington University by the RCHN Community Health Foundation.
Appendices
Appendix A
| Appendix Table 1: Health Center Responses to Specific Survey Questions by Medicaid Expansion Status and Urban/Rural Status | |||||
| All Health Centers | Medicaid expansion States | Non-expansion States | Urban | Rural | |
| Factors Accounting for Decrease in Medicaid Patients | |||||
| Concerns from immigrant families about applying for or keeping Medicaid for themselves or their children | 68% | 73% | 59% | 77% | 46%^ |
| Enrollment and renewal process changes have made it more difficult for patients to enroll in Medicaid or renew Medicaid coverage | 60% | 58% | 64% | 60% | 61% |
| Overall drop in health center patients | 30% | 28% | 35% | 23% | 46%^ |
| Patients are gaining jobs and losing Medicaid coverage due to increased income and/or employer-covered insurance | 22% | 30% | 7%* | 26% | 11% |
| New Medicaid eligibility requirements (e.g., work requirements, premium and copayment requirements) make it harder for patients to maintain Medicaid coverage | 20% | 20% | 21% | 20% | 23% |
| Significant changes in the demographic characteristics of the communities our health center serves | 15% | 14% | 16% | 13% | 18% |
| Do not contract with some or all Medicaid managed care plans that operate in our health center’s service area | 6% | 3% | 11% | 6% | 5% |
| Fewer Medicaid covered services being offered | 6% | 3% | 11% | 6% | 6% |
| All Health Centers | Medicaid expansion States | Non-expansion States | Urban | Rural | |
| Health Centers Providing Social and Support Services On-Site | |||||
| Insurance Enrollment Assistance | 96% | 97% | 92%* | 97% | 94% |
| Case Management Services | 93% | 93% | 95% | 93% | 94% |
| Health Literacy | 67% | 67% | 68% | 68% | 66% |
| Transportation | 61% | 59% | 66% | 65% | 55%^ |
| Healthy Foods | 47% | 49% | 43% | 51% | 42% |
| Veterans Services | 47% | 43% | 57%* | 42% | 54%^ |
| SNAP, WIC, or Other Nutritional Assistance Services | 40% | 41% | 39% | 47% | 31%^ |
| Physical Activity and Exercise | 40% | 40% | 39% | 40% | 41% |
| Education | 39% | 35% | 49%* | 35% | 44% |
| Domestic Violence | 31% | 33% | 27% | 34% | 28% |
| Agricultural Worker Support | 18% | 13% | 29%* | 11% | 27%^ |
| Housing (includes housing assistance and quality) | 18% | 18% | 16% | 20% | 14% |
| Refugee Services | 17% | 17% | 17% | 23% | 8%^ |
| Criminal Justice/Recidivism | 13% | 12% | 14% | 13% | 12% |
| Job Training | 12% | 12% | 11% | 11% | 12% |
| Job Search and Placement | 8% | 7% | 12% | 7% | 10% |
| Child Care/Head Start | 5% | 5% | 8% | 5% | 6% |
| All Health Centers | Medicaid expansion States | Non-expansion States | Urban | Rural | |
| Barriers to Working for Adult Health Center Medicaid Patients Who Are Not Currently Working | |||||
| Caring for children or other family members | 79% | 83% | 71%* | 83% | 73%^ |
| Lack of transportation to jobs | 78% | 78% | 80% | 78% | 79% |
| Substance use disorders | 77% | 80% | 70%* | 77% | 77% |
| Acute or chronic mental health conditions | 76% | 79% | 68%* | 78% | 72% |
| Skills and education do not meet requirements for available jobs | 76% | 79% | 69%* | 79% | 71%^ |
| Acute or chronic physical health conditions | 71% | 71% | 70% | 74% | 67% |
| Concerns about losing health coverage if they earn too much money | 56% | 57% | 53% | 57% | 54% |
| Lack of job training resources | 53% | 55% | 51% | 57% | 49% |
| Lack of jobs in the community | 45% | 45% | 46% | 40% | 53%^ |
| Many jobs in our community are seasonal | 20% | 20% | 18% | 14% | 28%^ |
| All Health Centers | Medicaid expansion States | Non-expansion States | Urban | Rural | |
| Top Three Challenges Facing Health Centers | |||||
| Increasing costs to operate health center | 52% | 55% | 46% | 54% | 49% |
| Workforce recruitment | 52% | 55% | 43%* | 45% | 60%^ |
| Inadequate physical space | 31% | 30% | 34% | 27% | 36%^ |
| Workforce retention | 25% | 27% | 21% | 27% | 24% |
| High number of uninsured patients | 24% | 15% | 45%* | 28% | 19%^ |
| Insufficient insurance reimbursement | 19% | 21% | 13% | 18% | 20% |
| Insufficient grant funding | 18% | 17% | 20% | 19% | 17% |
| Competition from other providers | 14% | 13% | 17% | 15% | 13% |
| Changes to Medicaid reimbursement | 14% | 14% | 13% | 13% | 15% |
| Changes to Medicaid eligibility criteria, including work requirements | 10% | 9% | 13% | 9% | 11% |
| Contracting with insurers | 9% | 8% | 10% | 9% | 9% |
| Efforts to integrate care provided by your health center with healthcare provided by other providers | 8% | 8% | 6% | 8% | 8% |
| Increased immigration enforcement and/or policy changes affecting immigrants | 7% | 7% | 5% | 8% | 5% |
| Patient confusion regarding eligibility for insurance programs | 6% | 6% | 4% | 5% | 6% |
| Efforts to integrate care with social services (e.g., housing, TANF, SNAP) | 4% | 5% | 2% | 5% | 4% |
| Increased demand for family planning services | 0% | 1% | 0% | 0% | 0% |
| NOTE: * Significantly different from Medicaid expansion at the <0.05 level; ^ Significantly different from Urban at p<0.05 levelSOURCE: KFF and Geiger Gibson/RCHN Community Health Foundation 2019 Survey of Community Health Centers | |||||
| Appendix Table 2: Share of Health Centers Reporting Barriers to Reporting Work/Community Engagement Activities for their Patients | |||
| Potential Barriers to Reporting Work/Community Engagement Activities | Barrier for many patients | Barrier for some patients | Not a barrier |
| Are unsure of how to request an exemption | 76% | 23% | 1% |
| Are unsure of reporting deadlines and/or how often they need to report | 70% | 28% | 2% |
| Have questions about how to report their activity | 67% | 32% | 1% |
| Are confused about whether the rules apply to them | 67% | 32% | 2% |
| Face more pressing needs | 67% | 31% | 3% |
| Have limited understanding of what they need to report | 66% | 33% | 2% |
| Do not have access to a computer | 57% | 41% | 2% |
| Lack confidence to report on their own | 49% | 49% | 2% |
| Do not have access to internet service | 47% | 51% | 2% |
| Need translation services | 32% | 57% | 11% |
| Need help because of a disability | 15% | 82% | 3% |
| Do not have access to a phone | 9% | 66% | 26% |
| NOTE: Question was asked of all health centers, so responses represent potential barriers. Don’t Know responses were excluded. Totals may not sum to 100% due to rounding. Source: KFF and Geiger Gibson/RCHN Community Health Foundation 2019 Survey of Community Health Centers | |||
Appendix B
2019 Survey of Community Health Centers(Questions 1-7 request survey respondent contact information; questions 18–26 and 28 were released separately)
Q8. Several states have received approval from the federal government to implement work/community engagement requirements in Medicaid and several others are considering such requirements. Is your health center in a state that has an approved or pending waiver or is considering developing a waiver request to require that Medicaid enrollees engage in work/community engagement activities as a condition of enrollment?
Yes, my state has an approved or pending waiver.Yes, my state is considering developing a waiver request.NoDon’t know
Q9. Have state Medicaid officials provided or offered to provide training to health center employees about the new Medicaid work/community engagement requirements?
Yes, state officials have provided the training.Yes, state officials have offered to provide training.No, state officials have not provided nor offered to provide training.Don’t know.
Q10. Has your health center or PCA provided, or does it provide, additional training to health center employees about the Medicaid work/community engagement requirements?
Yes, our health center or PCA has provided training.Yes, out health center or PCA plans to provide training.No, our health center would like to provide training but does not have the resources.No, our health center has not provided training and does not plan to provide training.Don’t know.
Q11. Is your health center assisting or does it plan to assist patients with meeting reporting requirements related to the Medicaid work/community engagement requirements, including explaining the requirements, creating online accounts, reporting monthly work/community engagement activity, or seeking and reporting exemptions?
Yes, we are currently assisting patients.Yes, we plan to assist patients.No, we would like to assist patients but do not have the resources.No, we are not assisting patients and do not plan to assist patients.Don’t know.
Q12. People deemed “medically frail” are excluded from Medicaid work/community engagement requirements. Has your state explained the process for designating patients with physical health conditions or mental health conditions/substance use disorders as medically frail?
Yes, state officials have explained the process.No, state officials have not explained the process.Don’t know.
Q13. Does your health center have the resources to complete the clinician evaluation that is required as part of the medical frailty determination for patients with physical health conditions or mental health conditions/substance use disorders?
YesNoDon’t know
Q14. If Medicaid enrollees were required to report work/community engagement activity online or by phone, please indicate whether the following factors would be a barrier for many patients, some patients, or not a barrier to meeting these reporting requirements among your Medicaid patients.
Do not have access to a computerDo not have access to internet serviceDo not have access to a phoneHave limited understanding of what they need to reportHave questions about how to report their activityAre unsure of reporting deadlines and/or how often they need to reportAre unsure of how to request an exemptionNeed translation servicesNeed help because of a disabilityLack confidence to report on their ownAre confused about whether the rules apply to themFace more pressing needsHave other barrier to reporting (specify)
Q15. Among your health center’s adult Medicaid patients who are non-elderly and non-disabled and who are not currently working, what would you identify as the barriers, if any, that prevent them from working? (Check all that apply).
No barriers (if so, please do not select other options)Acute or chronic physical health conditionsAcute or chronic mental health conditionsSubstance use disordersLack of jobs in the communityLack of job training resourcesSkills and education do not meet requirements for available jobsLack of transportation to jobsCaring for children or other family membersConcerns about losing health coverage if they earn too much moneyMany jobs in our community are seasonalDon’t know
Q16. Over the past year, has your health center noticed any of the following among your immigrant patients and their family members? Please indicate whether the following have been seen among many patients, some patients, a few patients, or no patients. Mark not applicable if these scenarios do not apply to your health center or don’t know if you are unsure.
Patients who refuse to enroll in Medicaid for themselvesPatients who refuse to enroll in Medicaid for their childrenPatients who disenroll or refuse to renew their own Medicaid coveragePatients who disenroll or refuse to renew Medicaid coverage for their childrenA reduction in the number of adult patients seeking care from the health centerA reduction in the number of patients seeking care for their children from the health center
Q17. If your health center has noticed immigrant patients and their family members choosing not to enroll in Medicaid, disenrolling from or not renewing Medicaid, or not seeking care, do you think the following federal policies or actions are a factor?
Recent proposed changes that would permit officials to consider use of Medicaid, SNAP, or other non-cash programs in public charge determinationsEnhanced immigration enforcement activityChanging federal policy limiting immigration pathways (e.g., elimination of protected status for some groups, limiting entry from certain countries, etc.)Other factor (please specify)
Q27. Please indicate whether your health center has experienced changes to the following financial factors in the past year. (Mark no change, increased, decreased, or not applicable for each option).Access to private capital
Federal grantsState and local grantsMedicaid revenuePrivate insurance revenueTitle X family planning grantsPercentage of Medicaid/CHIP patients who have a lapse or break in insurance coveragePercentage of private insurance patients who have a lapse or break in insurance coveragePercentage of insured patients who are unable to pay their deductibles and cost-sharing paymentsPercentage of privately insured patients who pay sliding scale feesFunding for community benefit activities from local hospitals and/or health plans
Q29. Over the past year, would you say the number of patients enrolled in Medicaid at your health center has increased, decreased, or stayed about the same? (If you answer increased or stayed the same, please skip to question 31).
The number of Medicaid patients has increasedThe number of Medicaid patients has stayed about the sameThe number of Medicaid patients has decreased
Q30. What would you say are the factors that likely account for the decrease in Medicaid patients at your health center? (Check all that apply).
Overall drop in health center patientsDo not contract with some or all Medicaid managed care plans that operate in our health center’s service areaSignificant changes in the demographic characteristics of the communities our health center servesPatients are gaining jobs and losing Medicaid coverage due to increased income and/or employer-covered insuranceConcerns from immigrant families about applying for or keeping Medicaid for themselves or their childrenEnrollment and renewal process changes have made it more difficult for patients to enroll in Medicaid or renew Medicaid coverageNew Medicaid eligibility requirements (e.g., work requirements, premium and copayment requirements) make it harder for patients to maintain Medicaid coverageFewer Medicaid covered services being offered
Q31. Does your health center currently receive funding from the Title X Family Planning Program?
YesNoDon’t know
Q32. In the next year, what it the estimated percentage increase in new family planning patients your health center could accept with current staffing and clinic space?
Not applicable, we do not currently have any family planning patientsNoneLess than 10%10-24%25-49%50-74%75-99%100% or more
Q33. How do patients at your health center receive prescription medications? (Check all that apply).
Dispensed by providerThrough an on-site pharmacy (either in-house or contract pharmacy)Through an off-site contract pharmacyThrough an off-site, non-contract pharmacyDon’t know
Q34. Which of the following types of social or support services does your health center provide on-site and/or through referrals to local organizations (Mark provide on-site, provide through referral, provide both on-site and through referral, or do not provide)?
Agricultural worker supportChild care/Head startCriminal justice/recidivismDomestic violenceEducationJob trainingJob search and placementHealthy foodsSNAP, WIC, or other nutritional assistance servicesHousing (includes housing assistance and quality)Health literacyInsurance enrollment assistancePhysical activity and exerciseRefugee servicesTransportationVeterans servicesCase management services
Q35. Please identify the top 3 challenges facing your health center.
Patient confusion regarding eligibility for insurance programsChanges to Medicaid reimbursementChanges to Medicaid eligibility criteria, including work requirementsInsufficient grant fundingInsufficient insurance reimbursementContracting with insurersWorkforce recruitmentWorkforce retentionHigh number of uninsured patientsCompetition from other providersEfforts to integrate care provided by your health center with healthcare provided by other providersEfforts to integrate care with social services (e.g., housing, TANF, SNAP)Increased immigration enforcement and/or policy changes affecting immigrantsIncreased demand for family planning servicesInadequate physical spaceIncreasing costs to operate health centerOther challenge (please specify)
Endnotes
- Tolbert, J., Artiga, S., & Pham, O. (2019). Impact of Shifting Immigration Policy on Medicaid Enrollment and Utilization of Care among Health Center Patients. Kaiser Family Foundation, https://modern.kff.org/report-section/impact-of-shifting-immigration-policy-on-medicaid-enrollment-and-utilization-of-care-among-health-center-patients-issue-brief/ ↩︎
- Markus, A., Sharac, J., Tolbert, J., Rosenbaum, S., & Zur, J. (2018). Community Health Centers’ Experiences in a More Mature ACA Market. Kaiser Family Foundation. https://modern.kff.org/medicaid/issue-brief/community-health-centers-experiences-in-a-more-mature-aca-market/ ↩︎
- Sharac, J., Shin, P., Rosenbaum, S., & Handarov, T. (2019). Community health centers continue steady growth, but challenges loom. Geiger Gibson/RCHN Community Health Foundation Research Collaborative, George Washington University. Policy Research Brief No. 60. https://www.rchnfoundation.org/?p=8436 ↩︎
- Kaiser Family Foundation. (March 10, 2020). Medicaid Waiver Tracker: Approved and Pending Section 1115 Waivers by State. https://modern.kff.org/medicaid/issue-brief/medicaid-waiver-tracker-approved-and-pending-section-1115-waivers-by-state/ ↩︎
- Indiana Family and Social Services Administration. (October 31, 2019). Pending resolution of federal lawsuit, FSSA will temporarily suspend Gateway to Work reporting requirements. https://www.in.gov/fssa/files/Gateway_to_Work_suspension_announcement.pdf ↩︎
- Utah Department of Health. (April 3, 2020). Medicaid Expansion Community Engagement Requirement Suspended. https://medicaid.utah.gov/Documents/pdfs/4.3.20_NR_CEsuspension.pdf ↩︎
- Sommers, B. D., Goldman, A. L., Blendon, R. J., Orav, E. J., & Epstein, A. M. (2019). Medicaid Work Requirements—Results from the First Year in Arkansas. New England Journal of Medicine, 381: 1073-1082. ↩︎
- Kaiser Family Foundation. (December 20, 2019). The Status of Participation in the Title X Federal Family Planning Program. https://modern.kff.org/interactive/the-status-of-participation-in-the-title-x-federal-family-planning-program/ ↩︎
- Wood, S.F., et. al. (2018). Community Health Centers and Family Planning in an Era of Policy Uncertainty. KFF. https://modern.kff.org/womens-health-policy/report/community-health-centers-and-family-planning-in-an-era-of-policy-uncertainty/ ↩︎
- Rosenbaum, S., Wood, S.F., Strasser, J., Sharac, J., Wylie, J., Tran, T.C. (2018). The Title X Family Planning Proposed Rule: What’s at Stake for Community Health Centers? Health Affairs blog. https://www.healthaffairs.org/do/10.1377/hblog20180621.675764/full/ ↩︎
- Sobel, L., Salganicoff, A., and Frederiksen, B. (2019). New Title X Regulations: Implications for Women and Family Planning Providers, Kaiser Family Foundation. https://modern.kff.org/womens-health-policy/issue-brief/new-title-x-regulations-implications-for-women-and-family-planning-providers/ ↩︎
- https://uscode.house.gov/view.xhtml?req=granuleid:USC-prelim-title42-section254b&num=0&edition=prelim ↩︎
- Department of Health and Human Services. (March 24, 2020). HHS Awards $100 Million to Health Centers for COVID-19 Response. https://www.hhs.gov/about/news/2020/03/24/hhs-awards-100-million-to-health-centers-for-covid-19-response.html ↩︎
- National Association of Community Health Centers. (2020). Summary of Key CHC Provisions in the Coronavirus Aid, Relief, and Economic Security (CARES) Act as signed into law on March 27, 2020. https://wsd-nachc-sparkinfluence.s3.amazonaws.com/uploads/2020/03/CARES-Act-Summary-for-Health-Centers.pdf ↩︎
- Medicaid expansion status was as of the time of the survey fielding period. Note that Utah and Idaho, which implemented the Medicaid expansion on January 1, 2020, and Nebraska, which has adopted but not yet implemented the expansion, were categorized as non-expansion states in this analysis. ↩︎