2025 Employer Health Benefits Survey
Overview
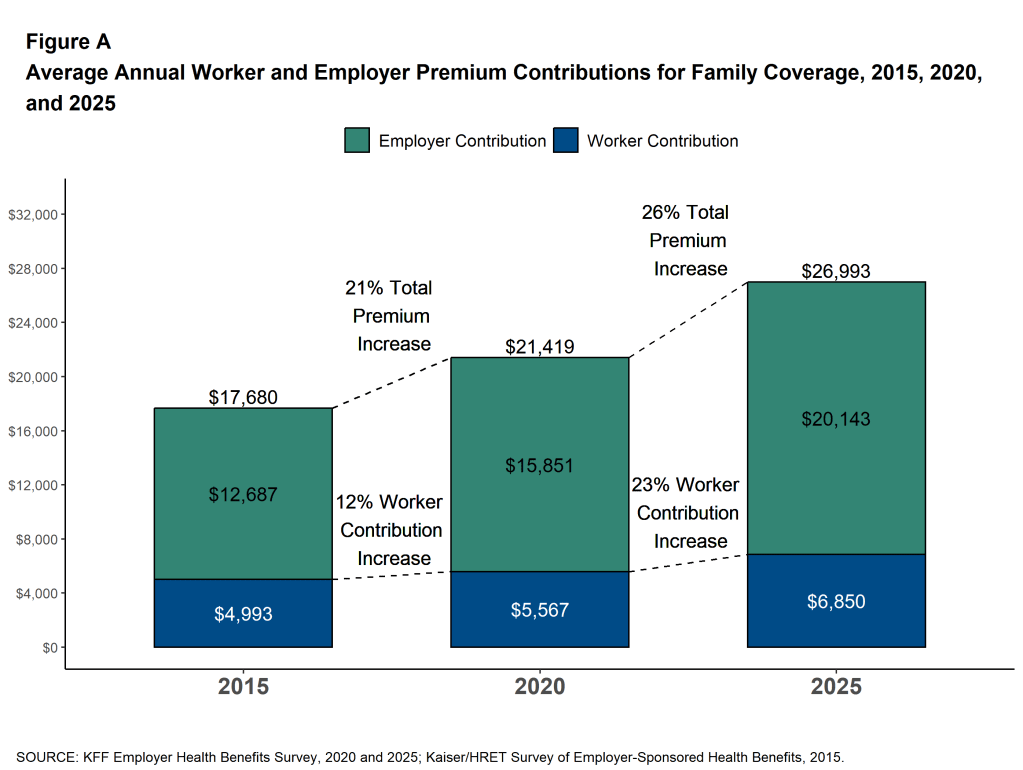
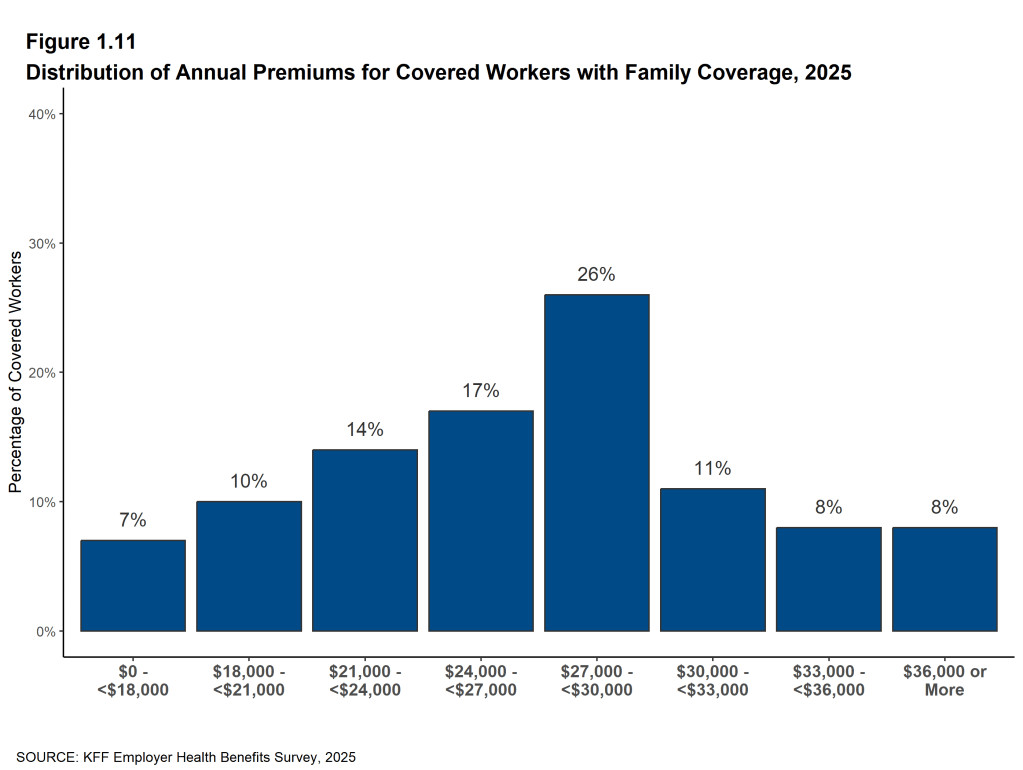
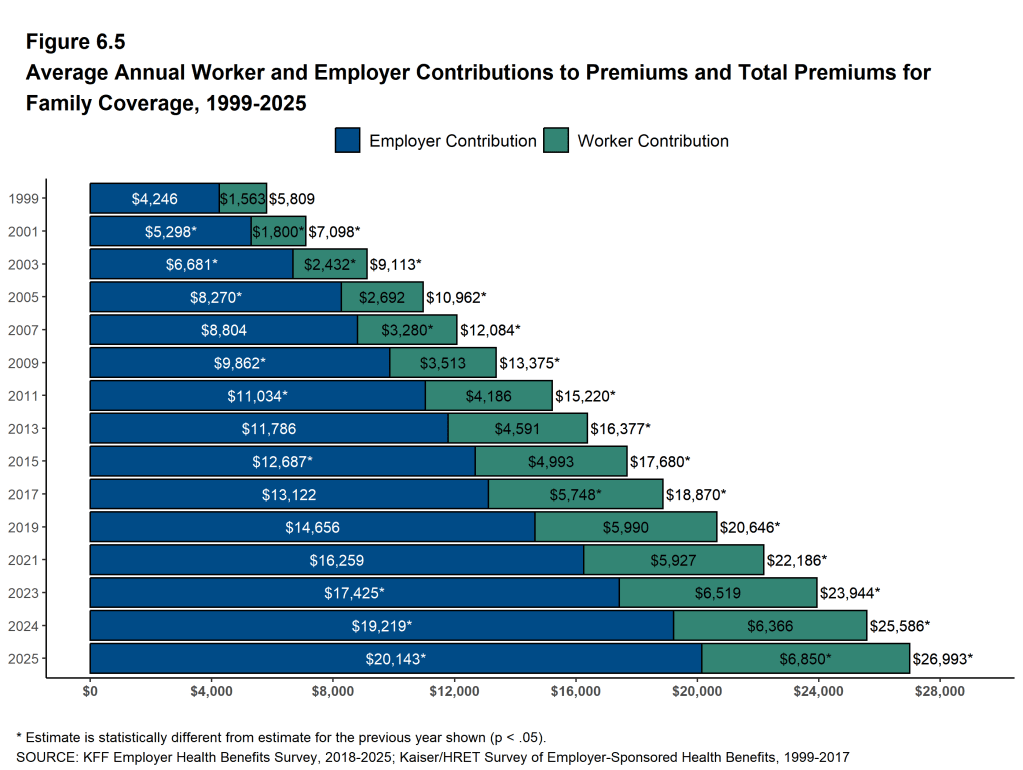
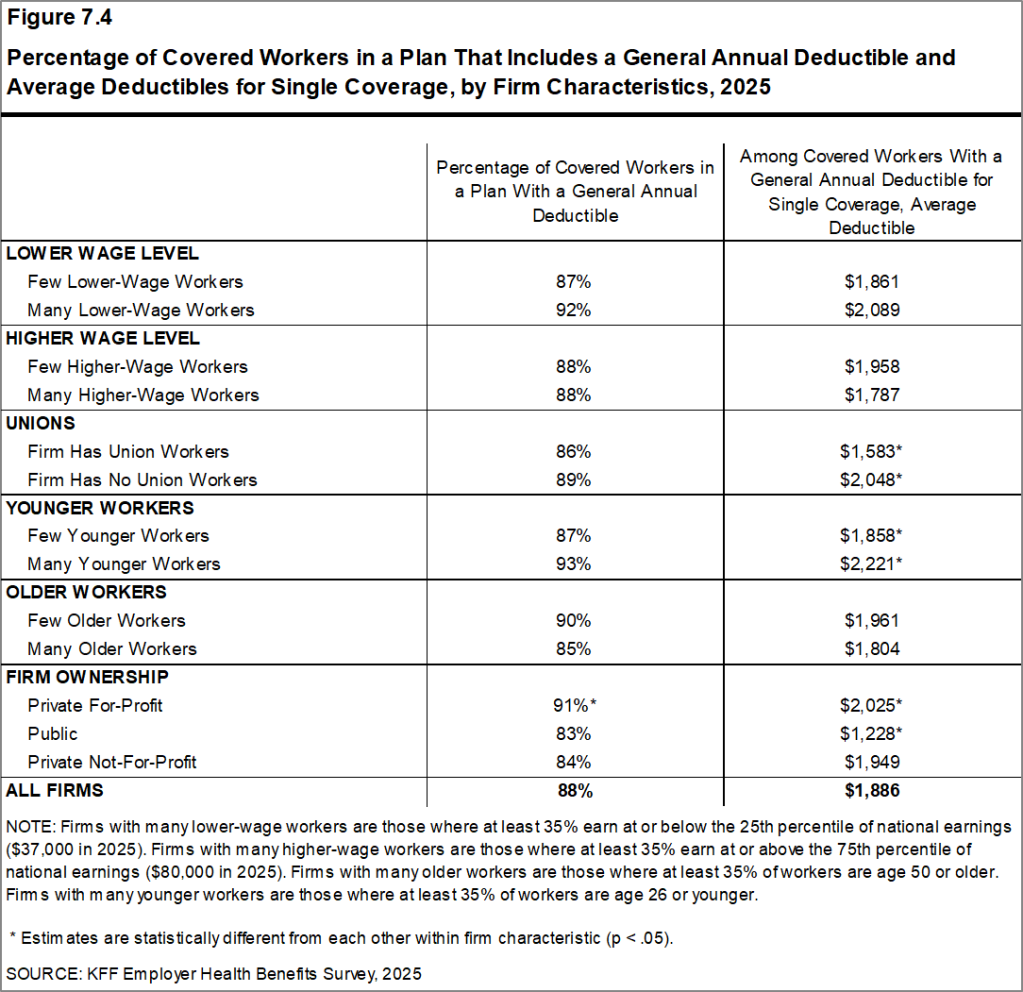
Annual premiums for employer-sponsored family health coverage reached $26,993 this year, 6% higher than in 2024. On average, workers contributed $6,850 toward the cost of family coverage. The average deductible among covered workers in a plan with a general annual deductible was $1,886 for single coverage.
Survey results are released in several formats, including a full report with downloadable tables on a variety of topics, a summary of findings, and an article published in the journal Health Affairs.
NEWS RELEASE
- A news release announcing the publication of the Employer Health Benefits Survey is available.
SUMMARY OF FINDINGS
- The Summary of Findings provides an overview of the survey results and is available under the Summary of Findings.
FULL REPORT
- The complete Employer Health Benefits Survey report includes over 200 exhibits and is available under the Report. The “Report” contains 13 separate sections. Users can view each section separately or download the section exhibits from the links below.
HEALTH AFFAIRS
- The peer-reviewed journal Health Affairs has published an article with key findings from the survey (subscription required): Health Benefits In 2025: Premiums Rise 6 Percent, Larger Employers Increase Coverage of GLP-1 Drugs For Weight Loss
INTERACTIVE GRAPHIC
- This graphing tool allows users to look at changes in premiums and worker contributions for covered workers at different types of firms over time: Premiums and Worker Contributions Among Workers Covered by Employer-Sponsored Coverage, 1999-2025.
CHARTPACK
- Key slides from the 2025 Employer Health Benefits Survey are here.
2025 TABLES BY SECTION
ADDITIONAL RESOURCES
Employer Health Benefits Surveys from 1998–2024 are available here. Please note that historic survey reports have not been revised with methodological changes.
Researchers may request a public use dataset by completing a data use agreement (available here).
Summary of Findings
Employer-sponsored insurance covers 154 million people under the age of 651. To provide a current snapshot of employer-sponsored health benefits, KFF conducts an annual survey of private and non-federal public employers with ten or more workers. This is the 27th Employer Health Benefits Survey (EHBS) and reflects employer-sponsored health benefits in 2025.
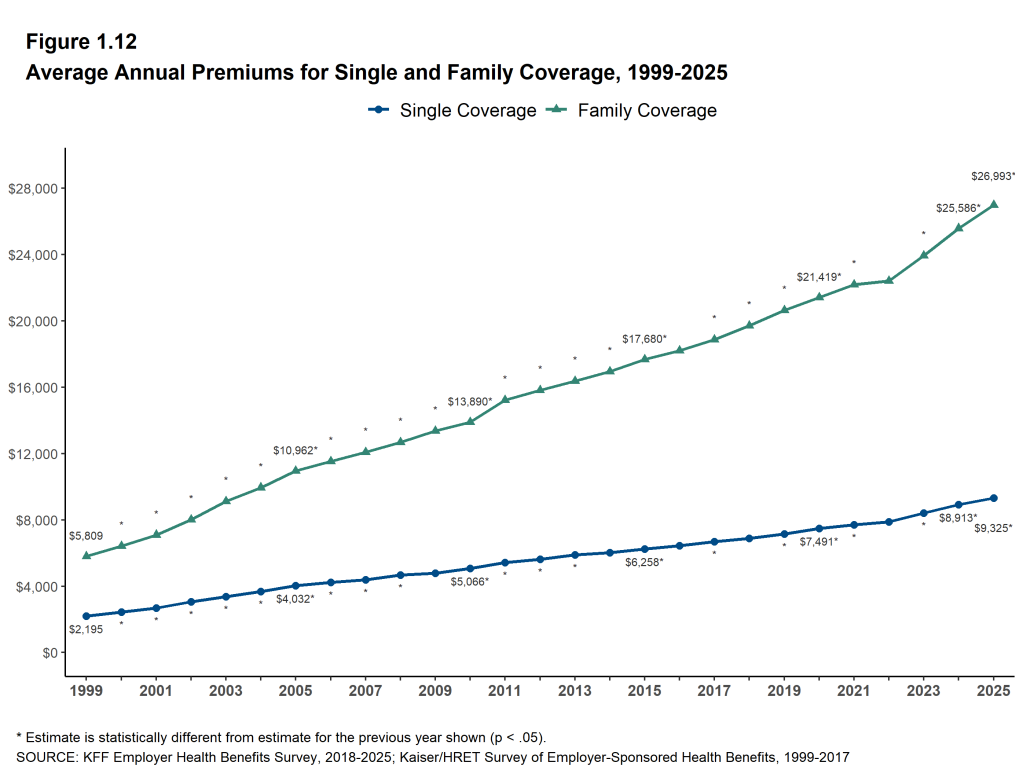
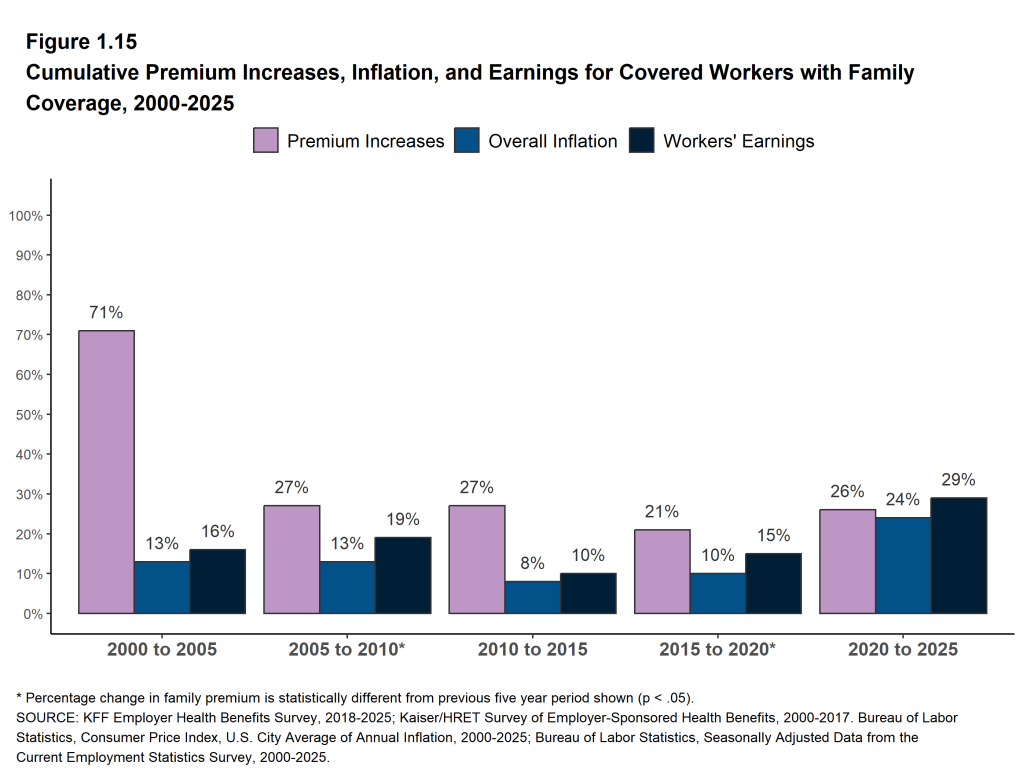
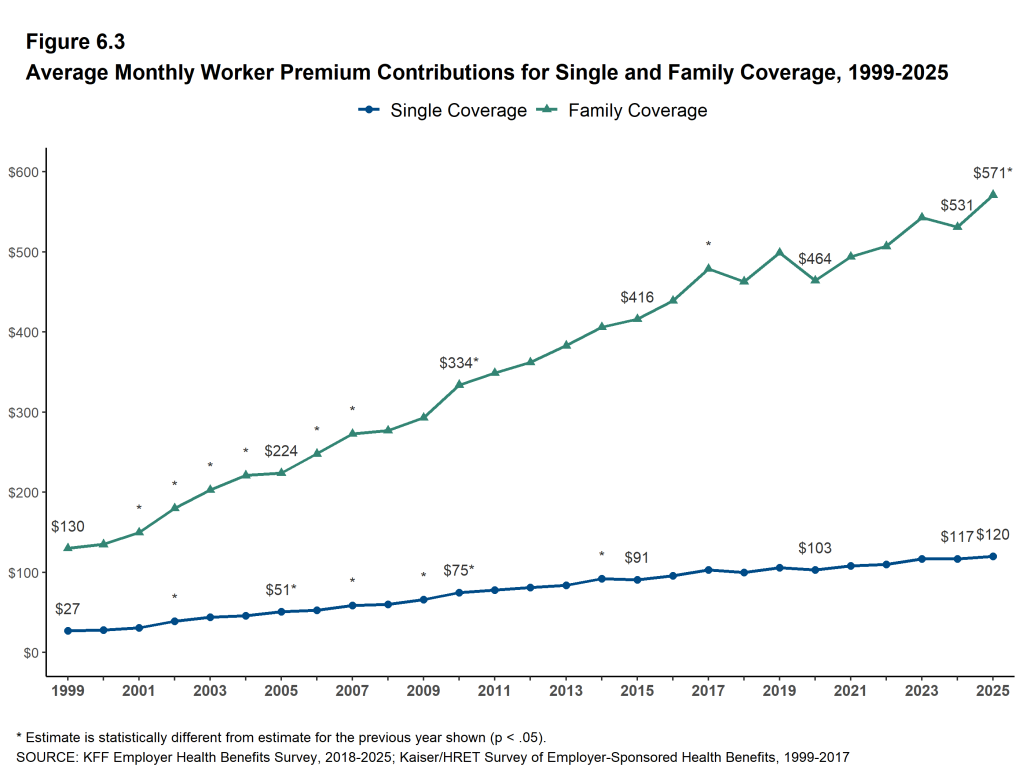
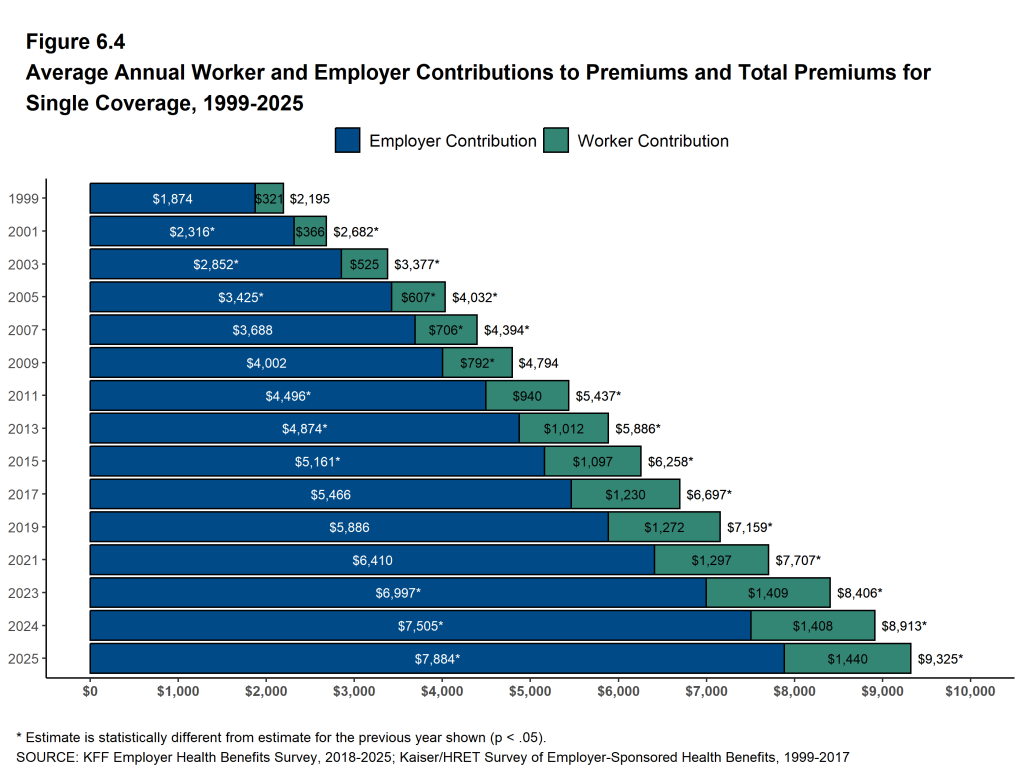
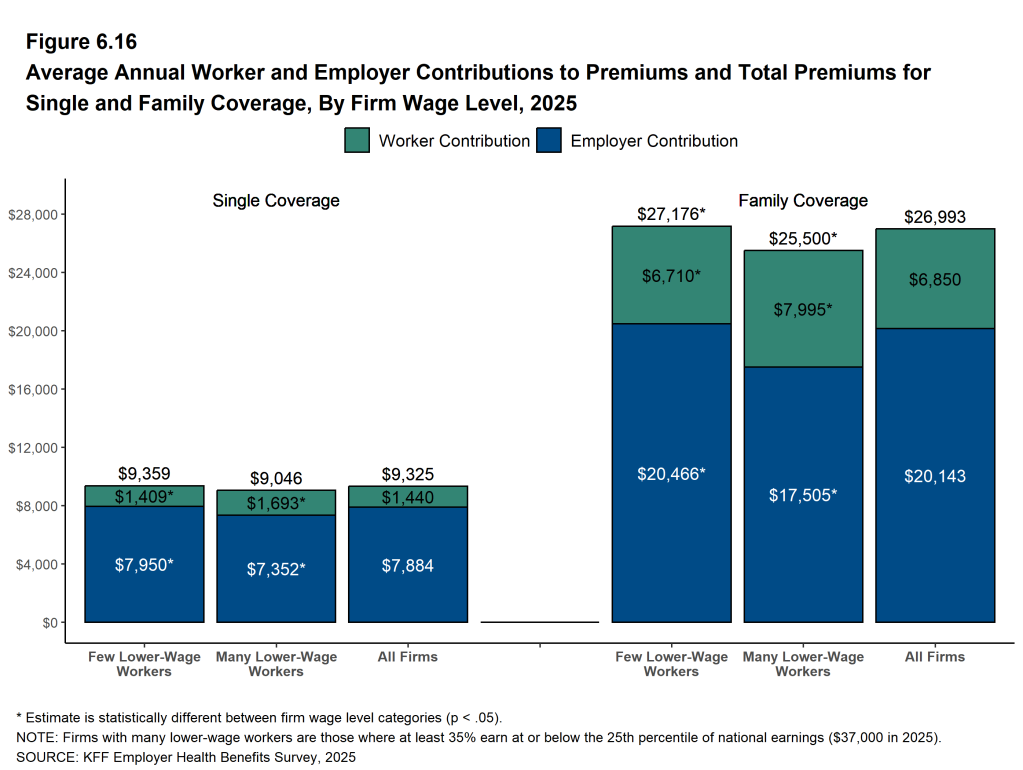
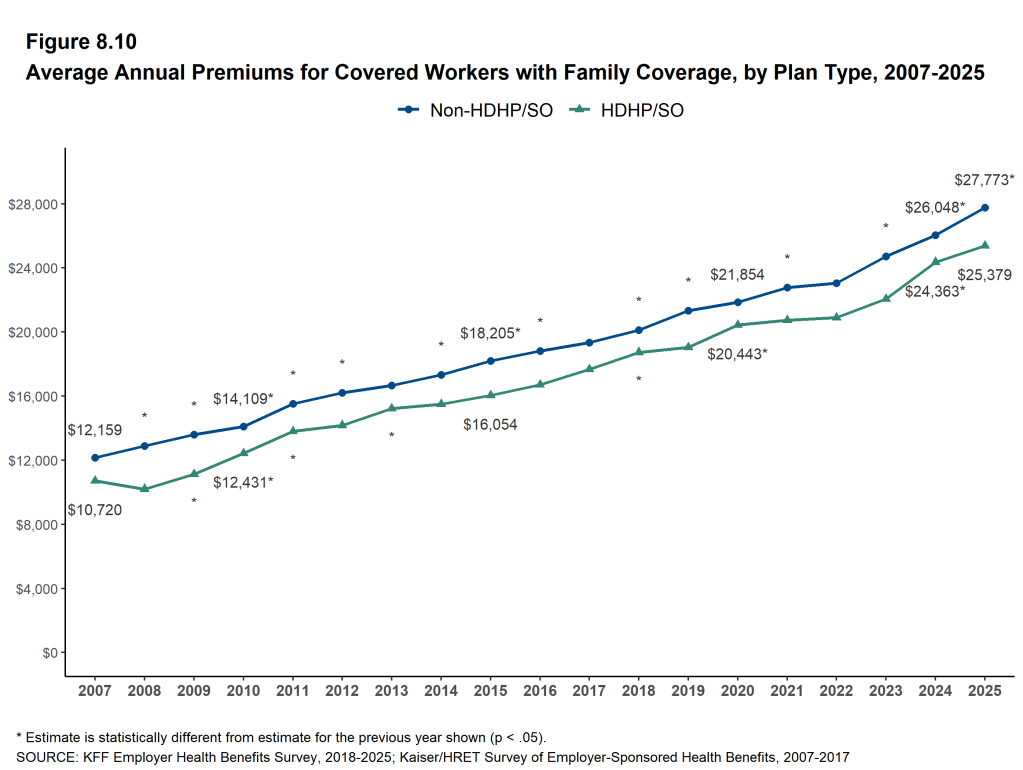
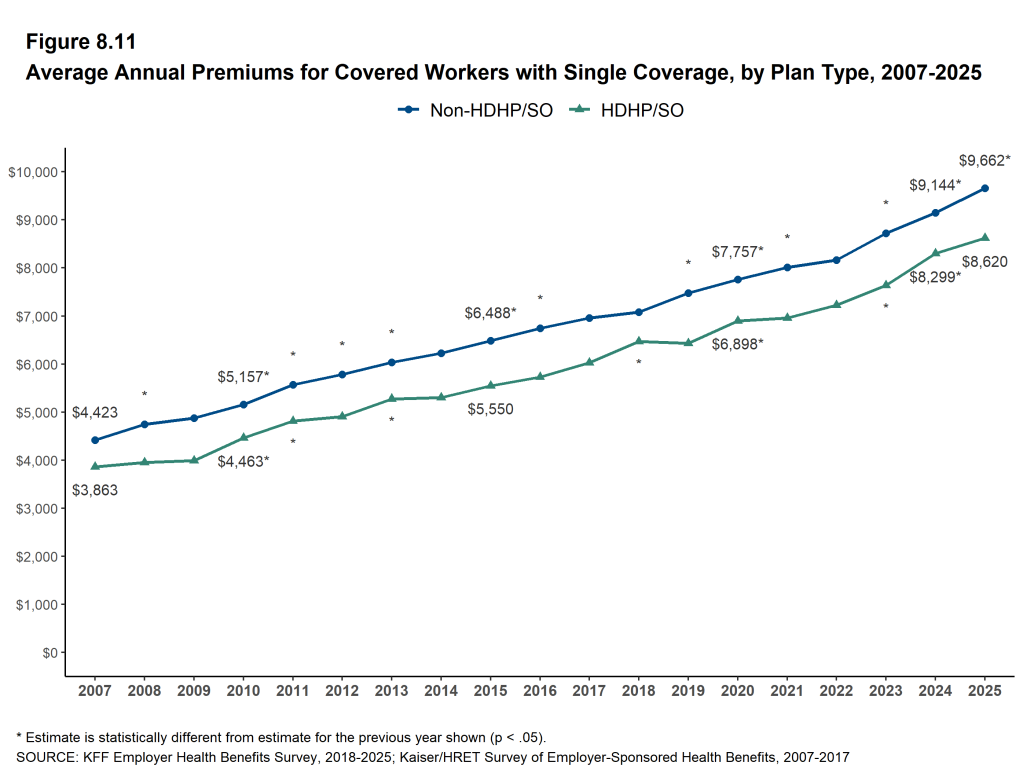
HEALTH INSURANCE PREMIUMS AND WORKER CONTRIBUTIONS
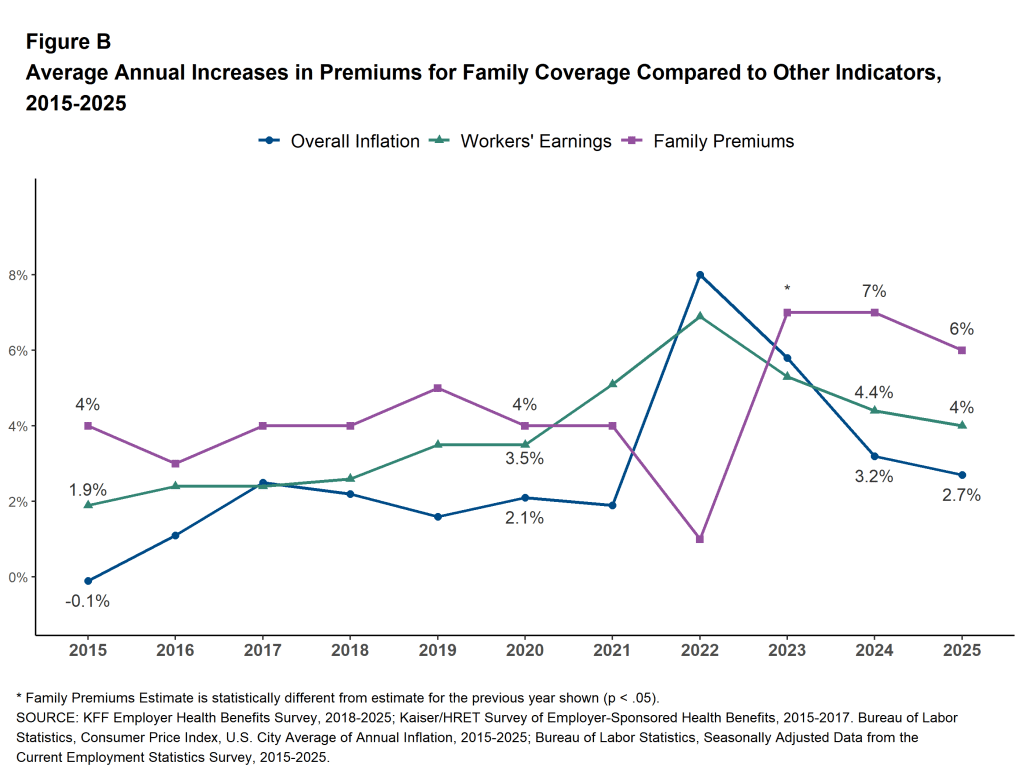
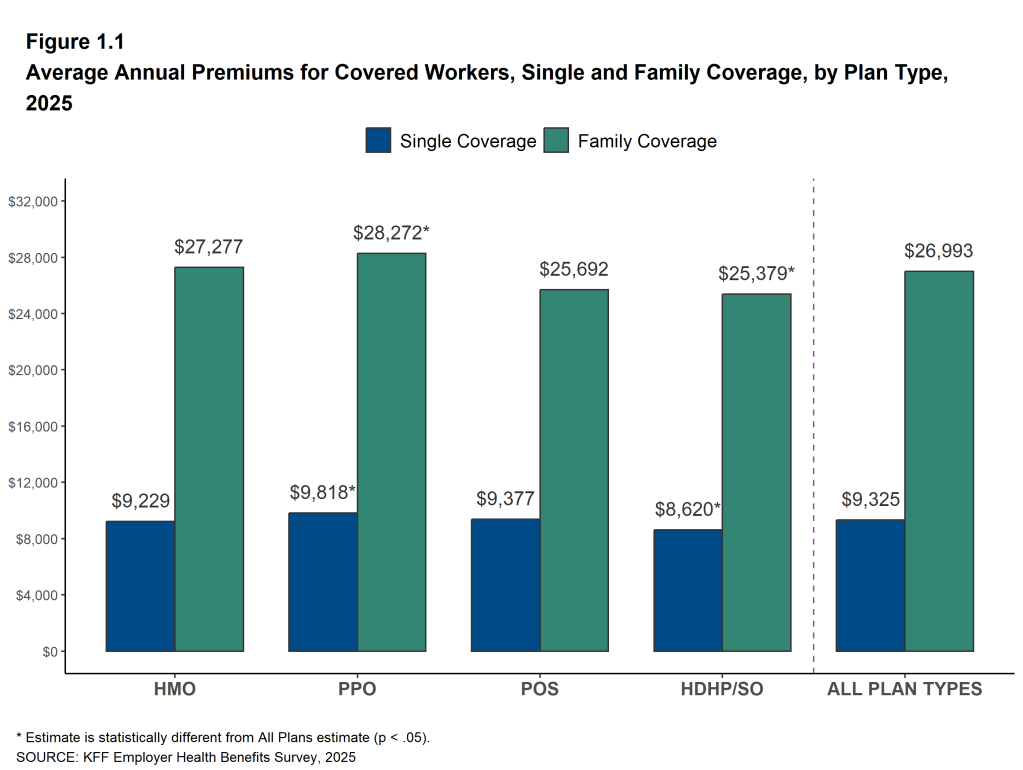
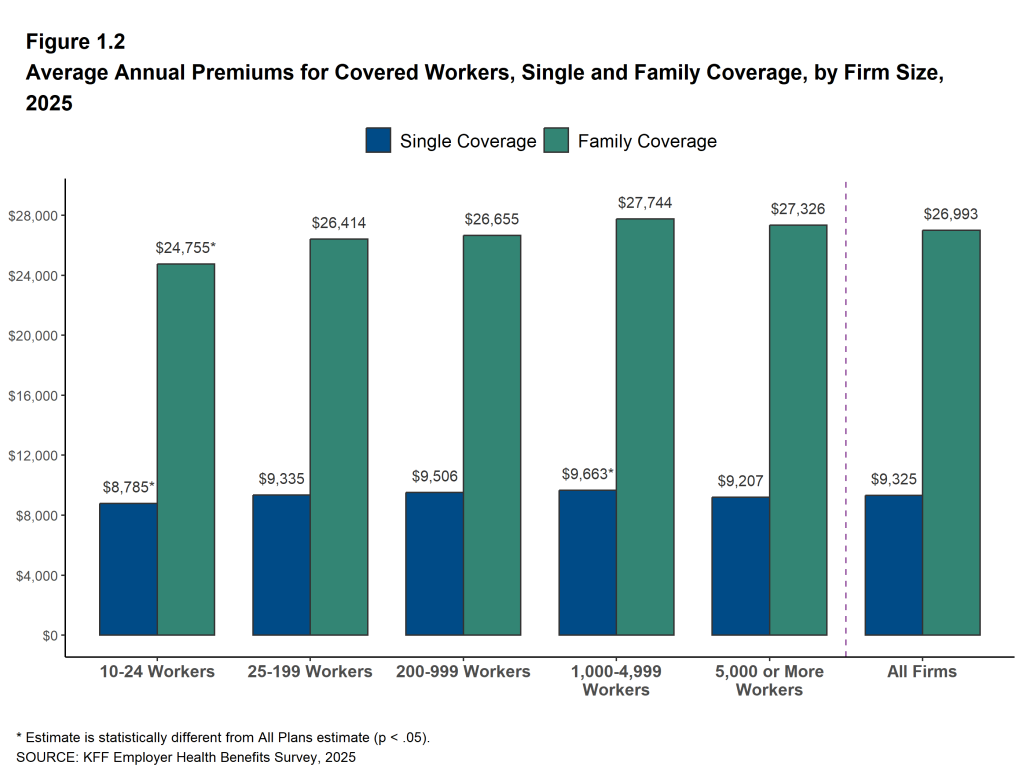
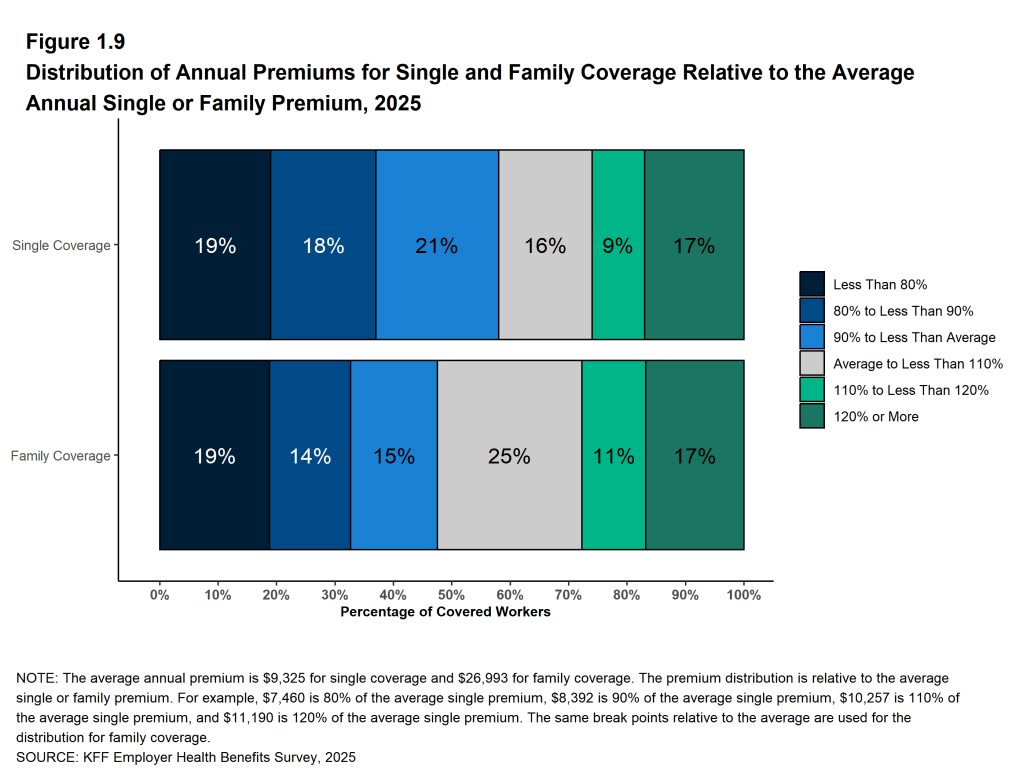
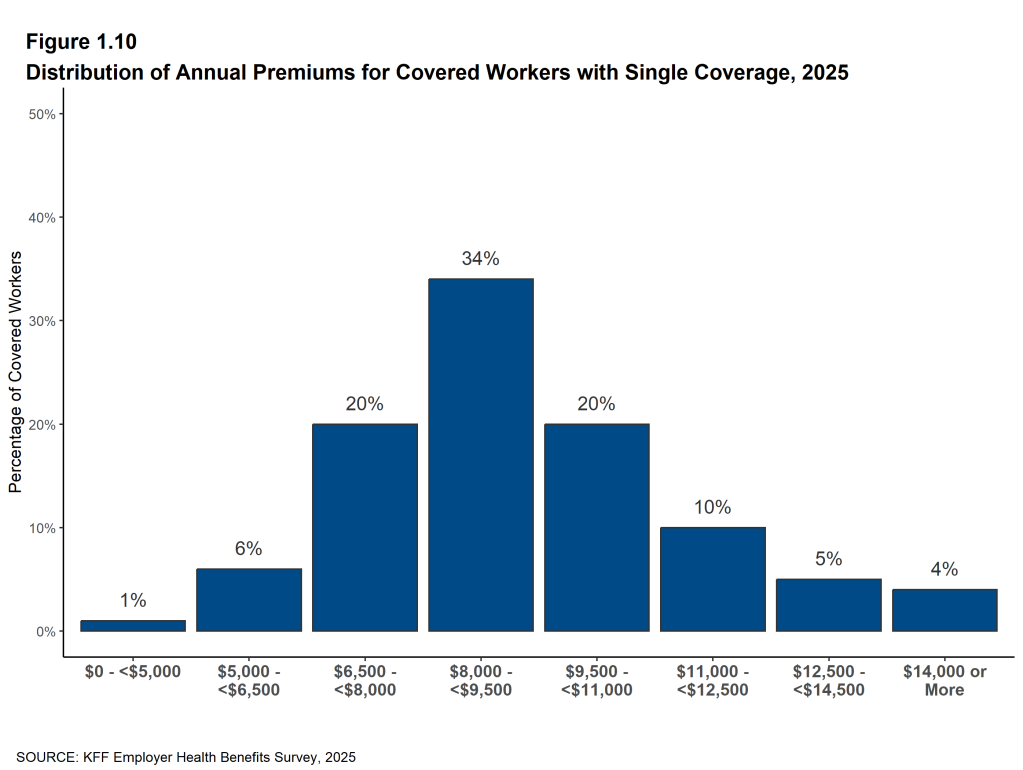
The average annual premiums for employer-sponsored health insurance in 2025 are $9,325 for single coverage and $26,993 for family coverage. Over the last year, the average single premium increased by 5% and the average family premium increased by 6%. Comparatively, there was an increase of 4% in workers’ wages and inflation of 2.7%2 3. Over the last five years, the average premium for family coverage has increased by 26%, compared to a 28.6% increase in workers’ wages and inflation of 23.5% [Figure A, Figure B].
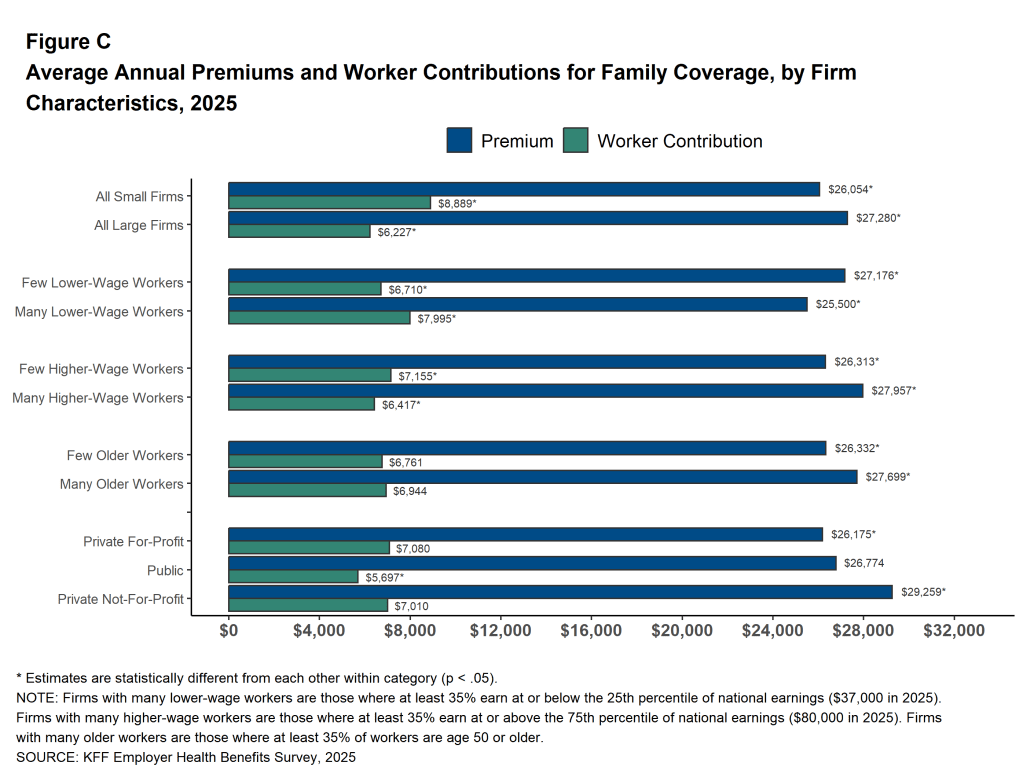
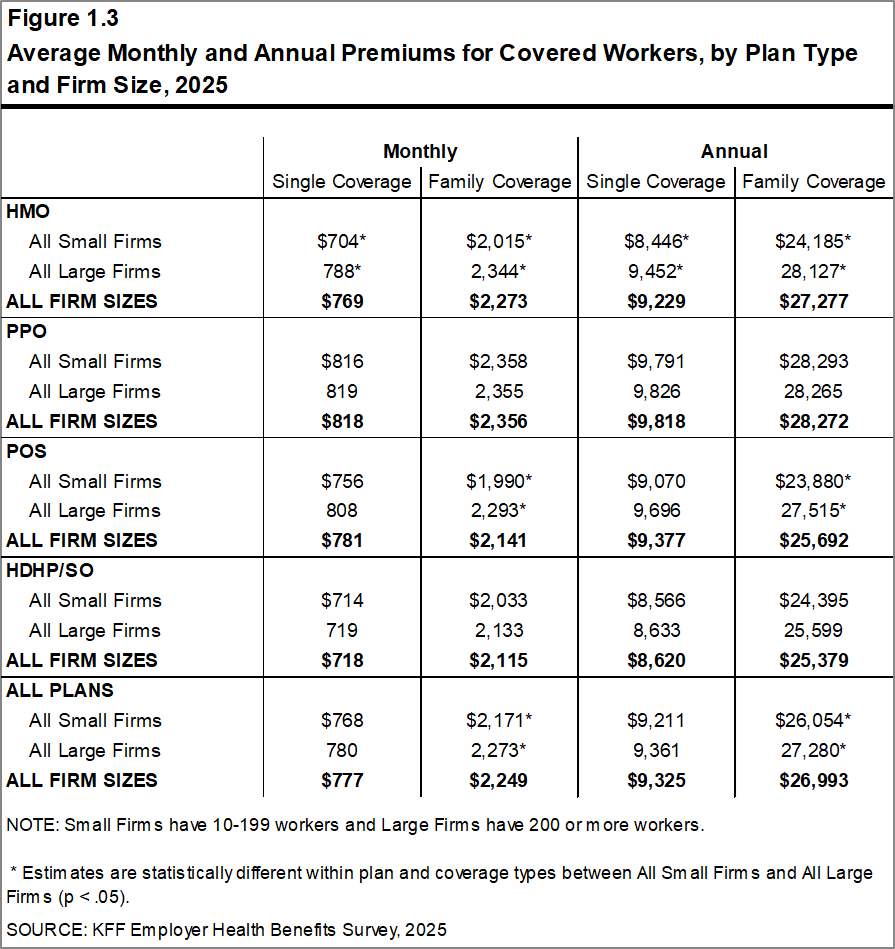
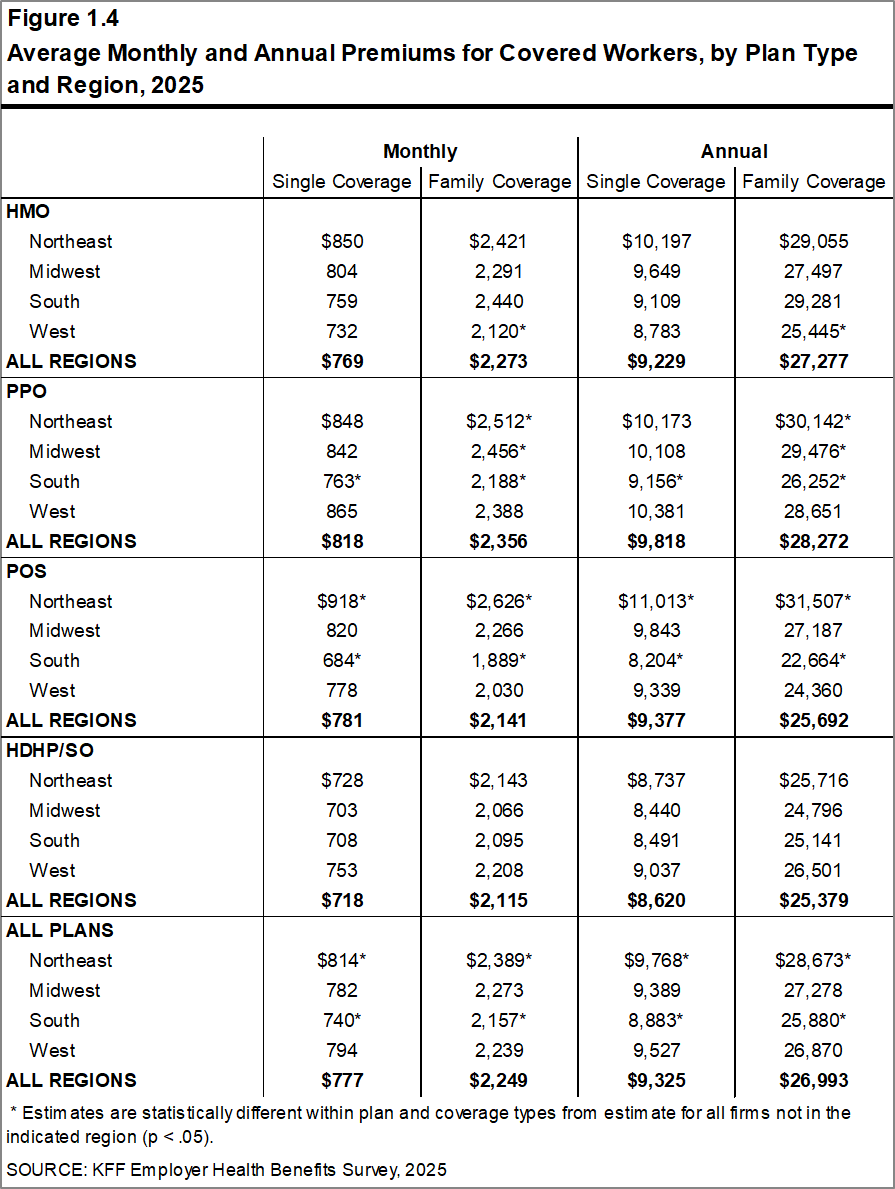
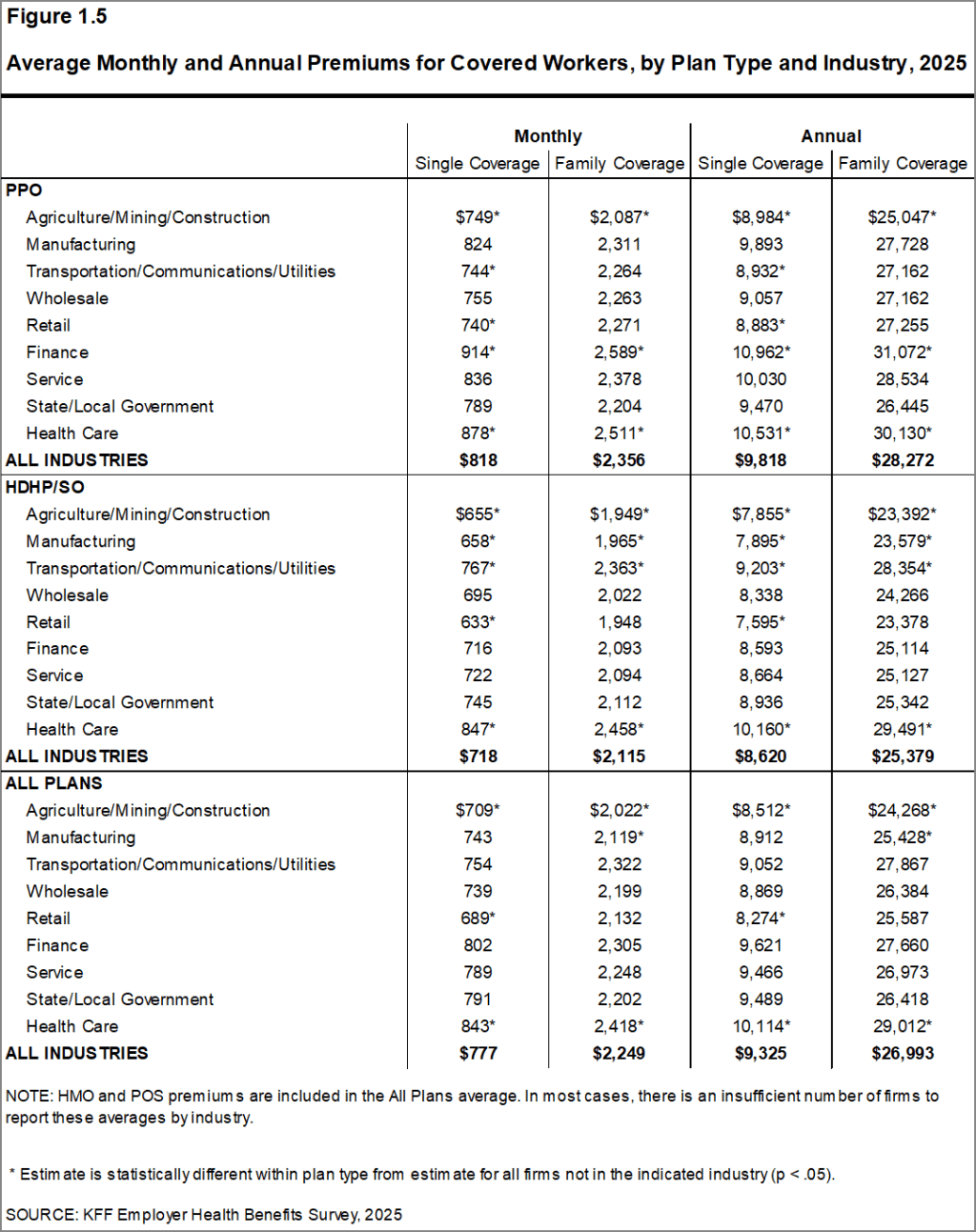
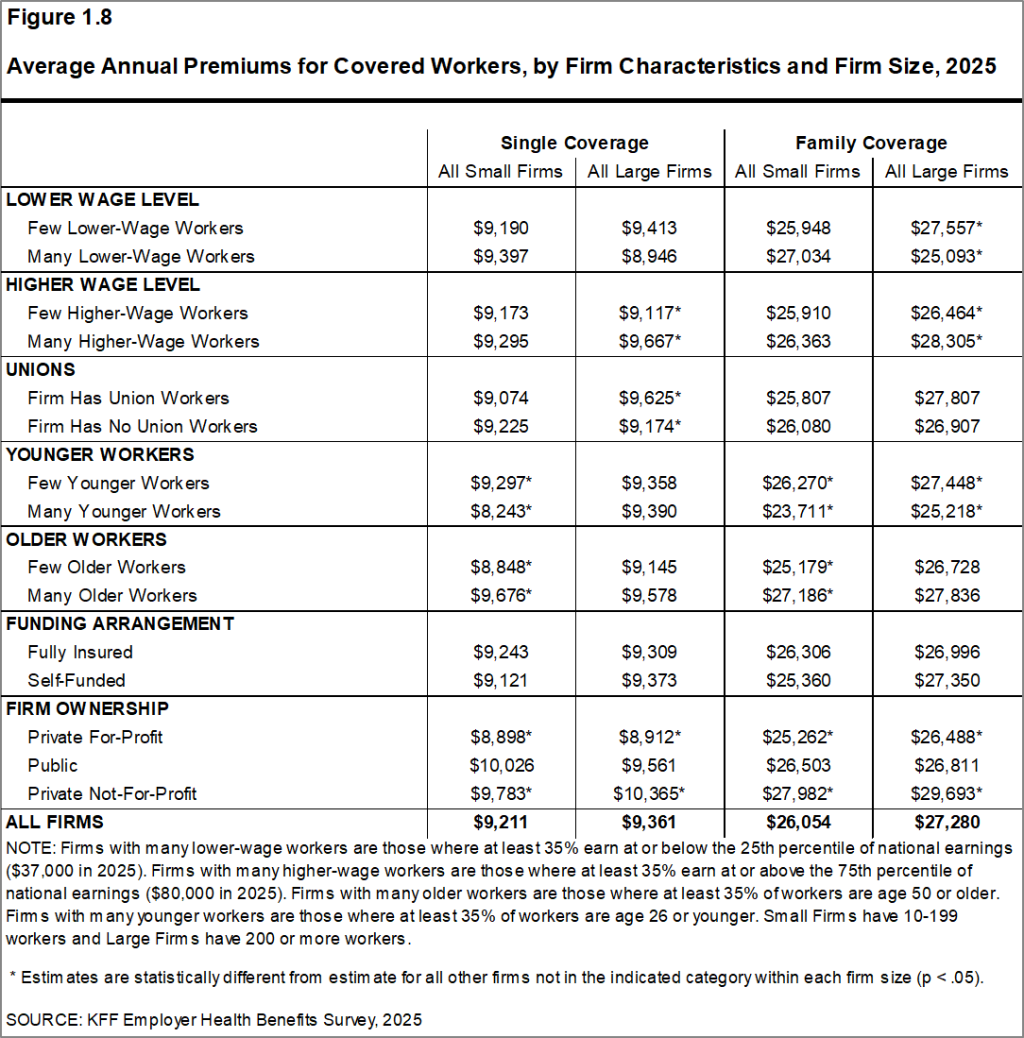
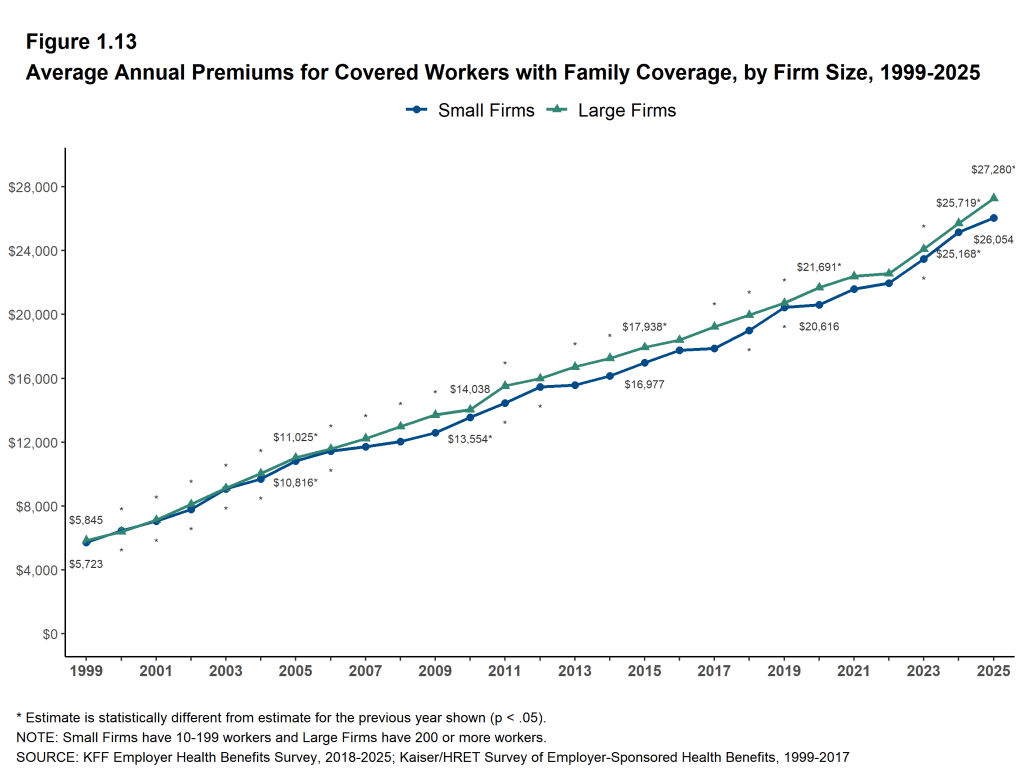
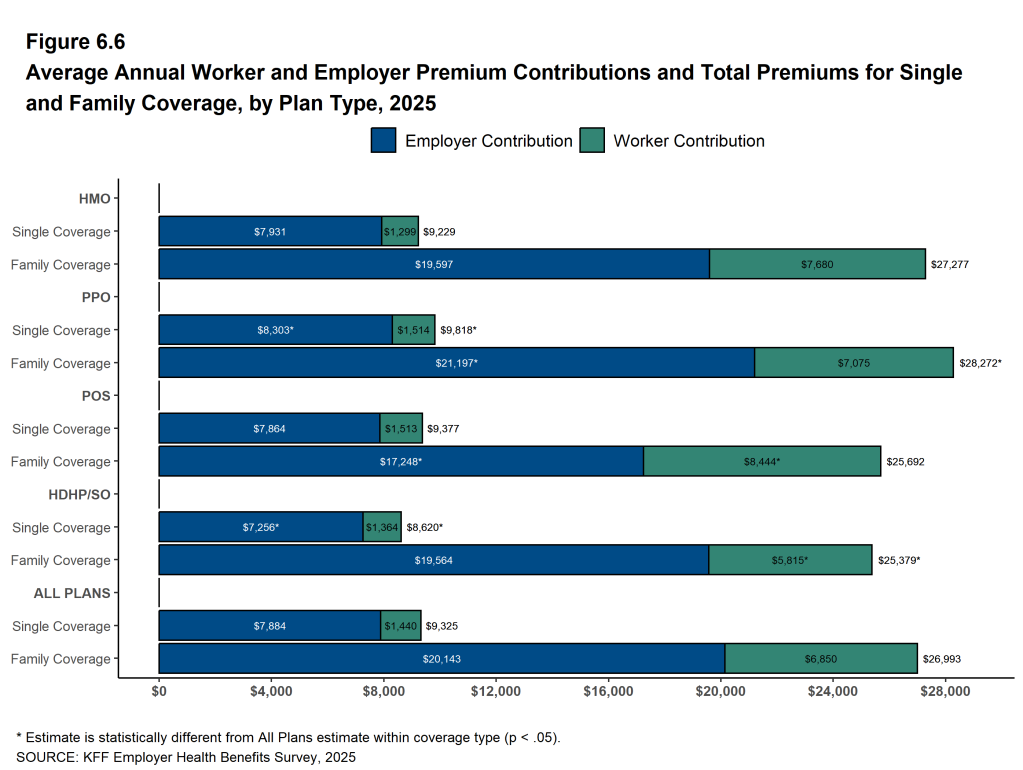
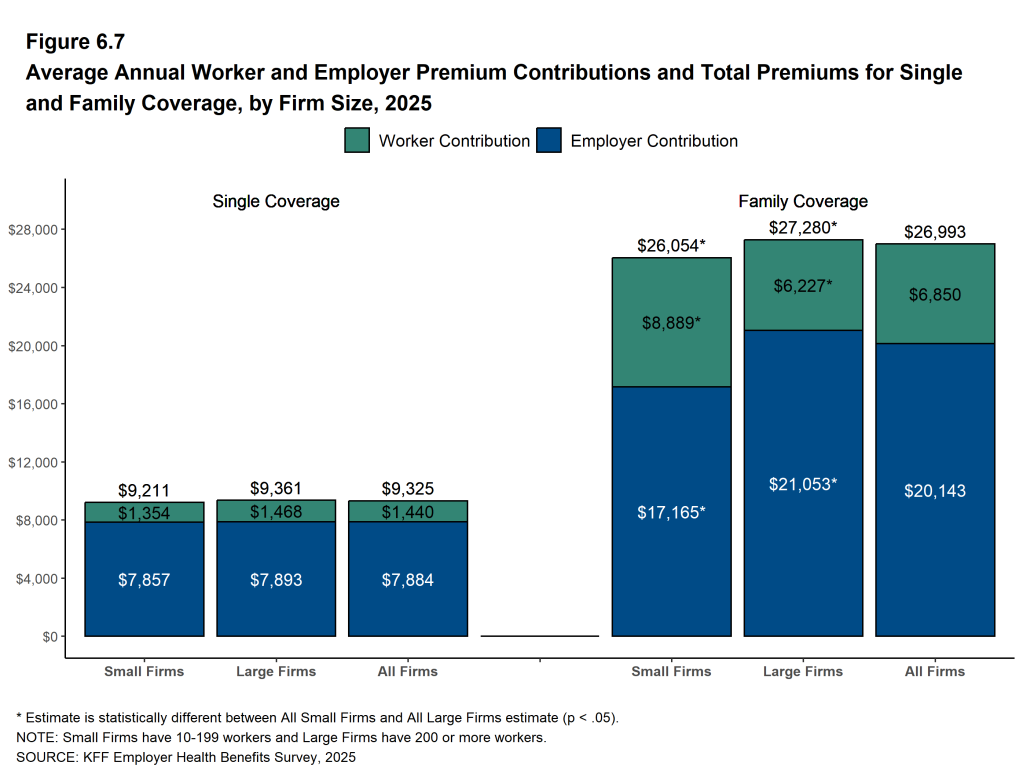
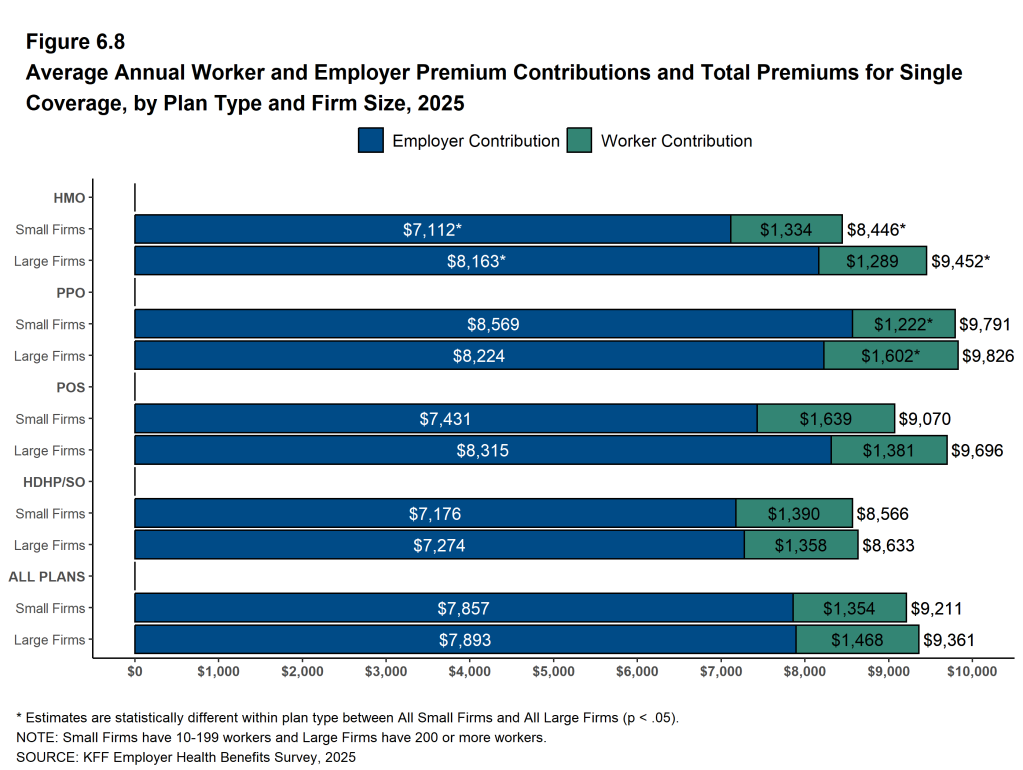
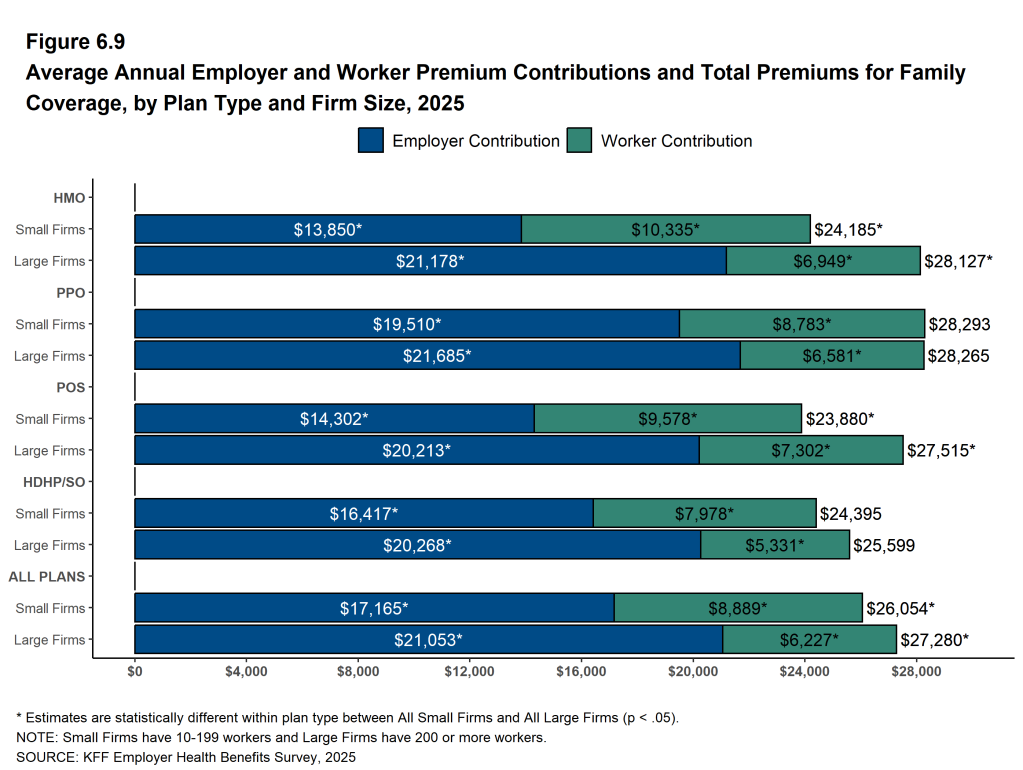
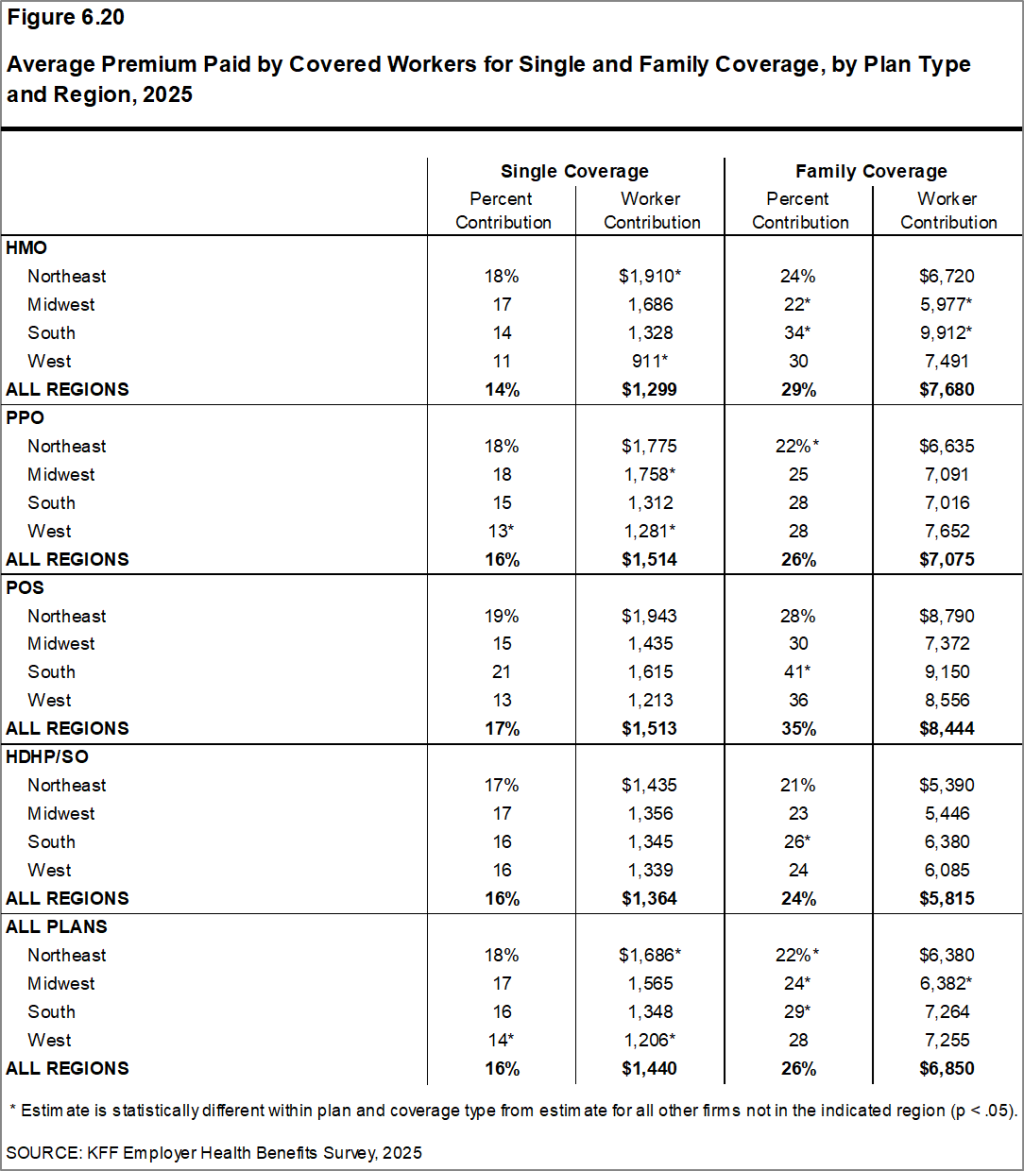
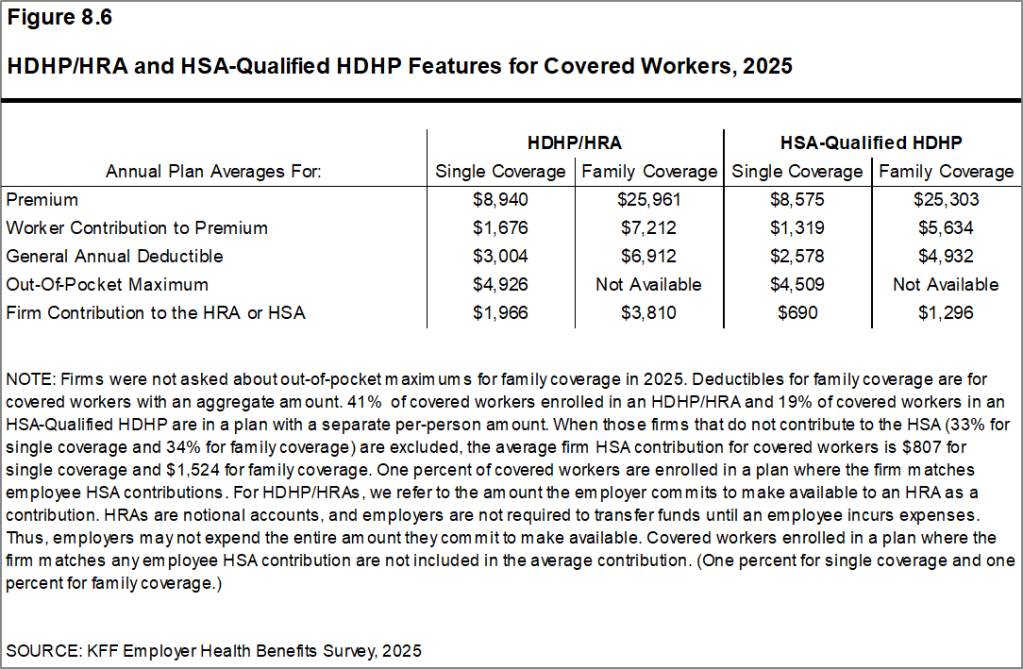
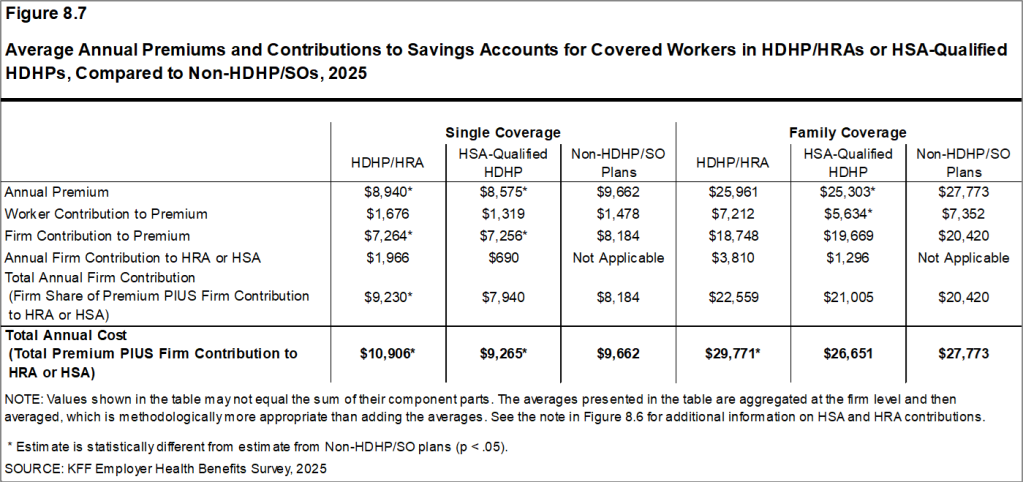
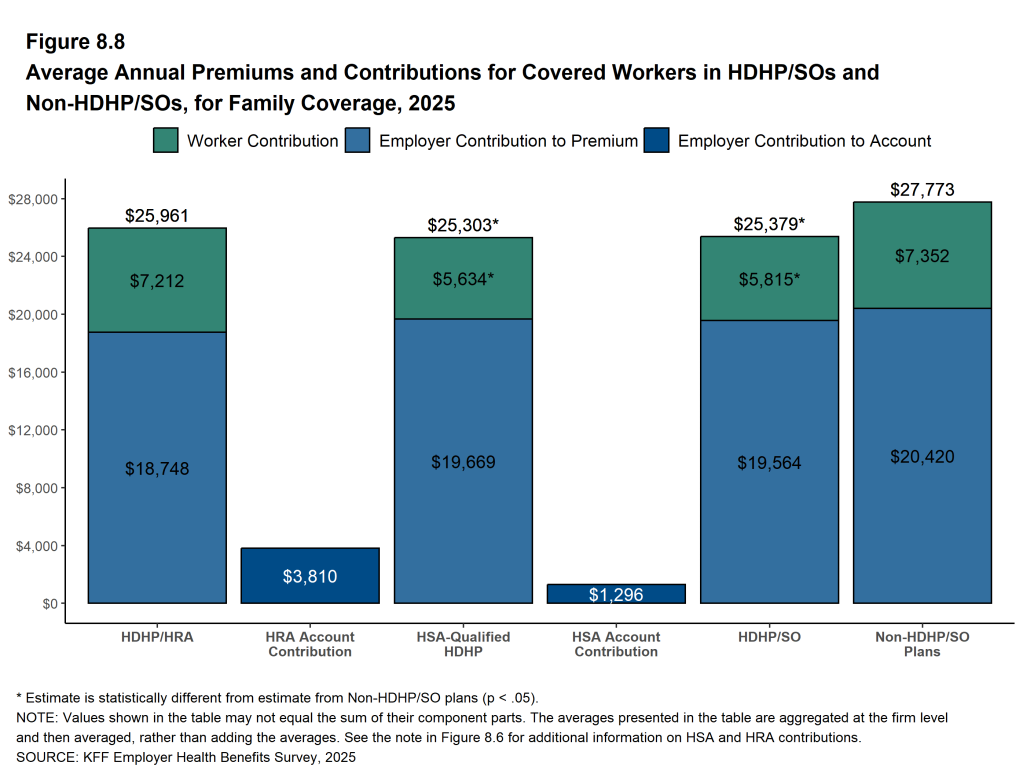
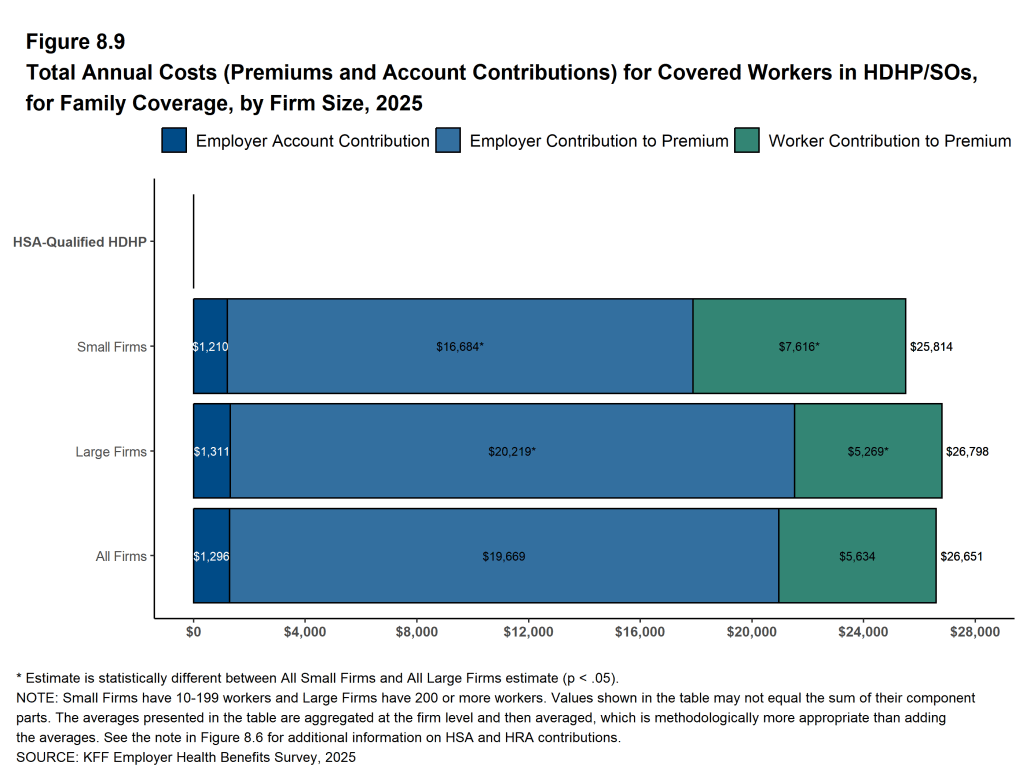
The average premium for firms with 10 to 199 workers is comparable to the average premium at larger firms for covered workers with single coverage ($9,211 and $9,361) but lower for family coverage ($26,054 vs. $27,280). The average premiums for covered workers in high-deductible health plans with a savings option (HDHP/SO) are lower than the overall average premiums for both single coverage ($8,620) and family coverage ($25,379). In contrast, average premiums for covered workers enrolled in PPOs are higher than the overall average premiums for both single ($9,818) and family coverage ($28,272).
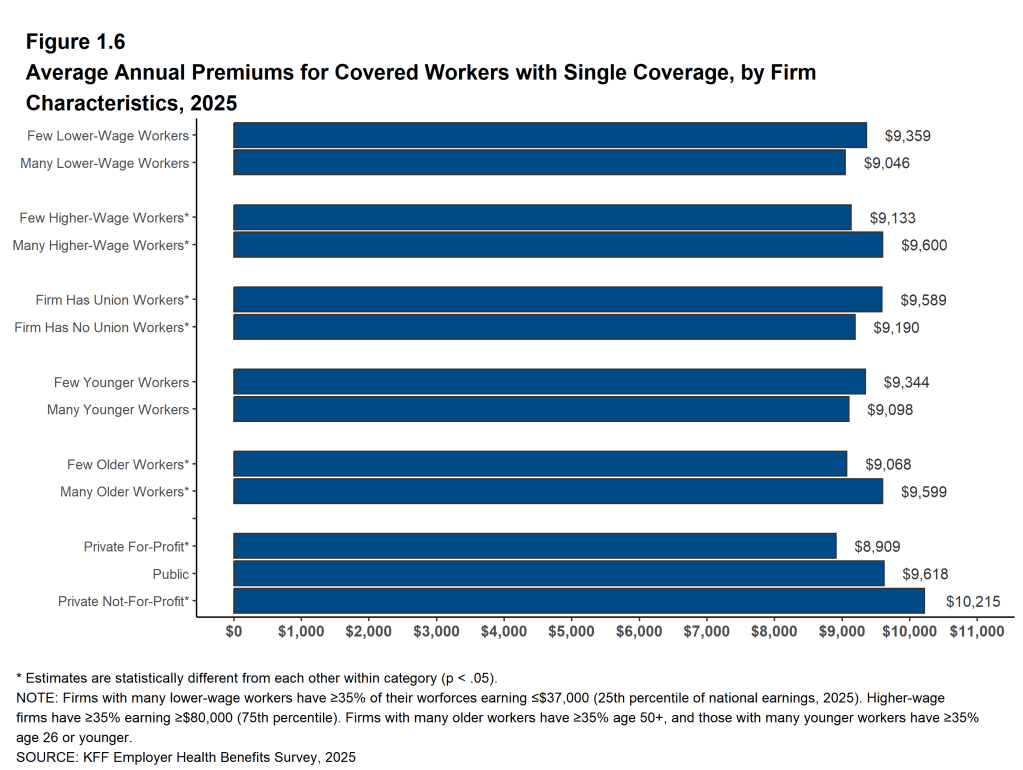
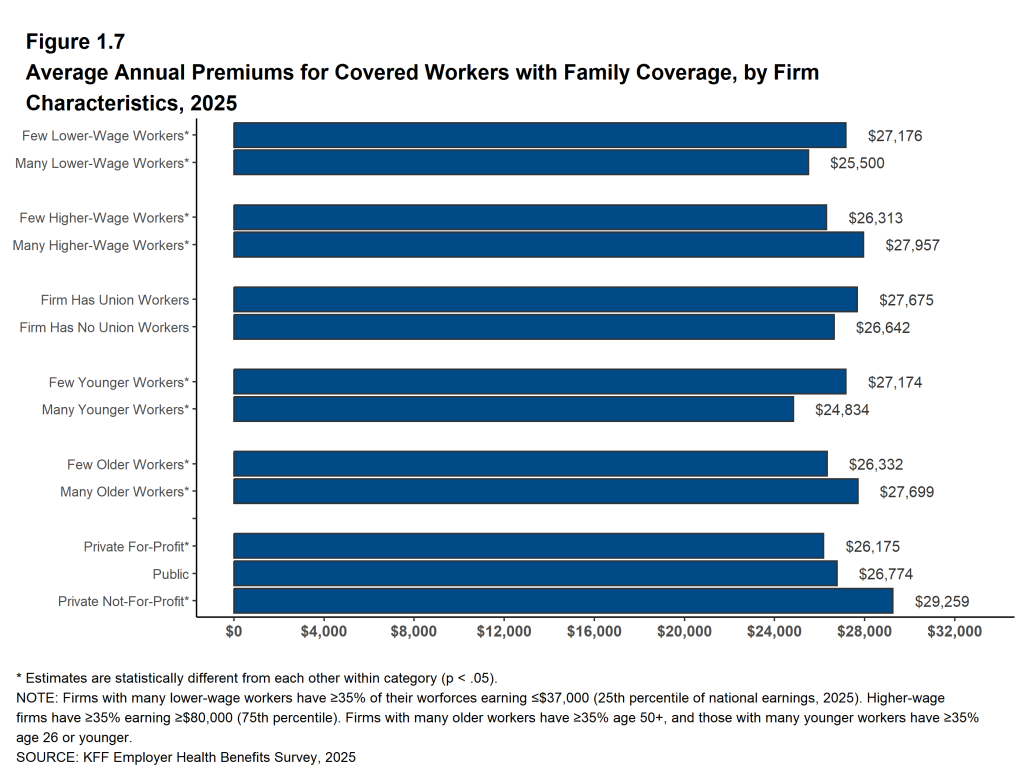
Premiums also differ with firm characteristics. The average premiums for both single and family coverage are relatively low for covered workers at private for-profit firms and relatively high for covered workers in private not-for-profit firms. The average premiums for covered workers at firms with larger shares of older workers (where at least 35% of the workers are age 50 or older) are higher than the average premiums for covered workers at firms with smaller shares of older workers for both single ($9,599 vs. $9,068) and family ($27,699 vs. $26,332) coverage. The average premiums for covered workers at firms with relatively large shares of higher-wage workers (where at least 35% of workers earn $80,000 a year or more) are higher than the average premiums for covered workers at firms with smaller shares of higher-wage workers for both single ($9,600 vs. $9,133) and family ($27,957 vs. $26,313) coverage [Figure C].
Figure A: Average Annual Worker and Employer Premium Contributions for Family Coverage, 2015, 2020, and 2025
Figure B: Average Annual Increases in Premiums for Family Coverage Compared to Other Indicators, 2015-2025
Figure C: Average Annual Premiums and Worker Contributions for Family Coverage, by Firm Characteristics, 2025
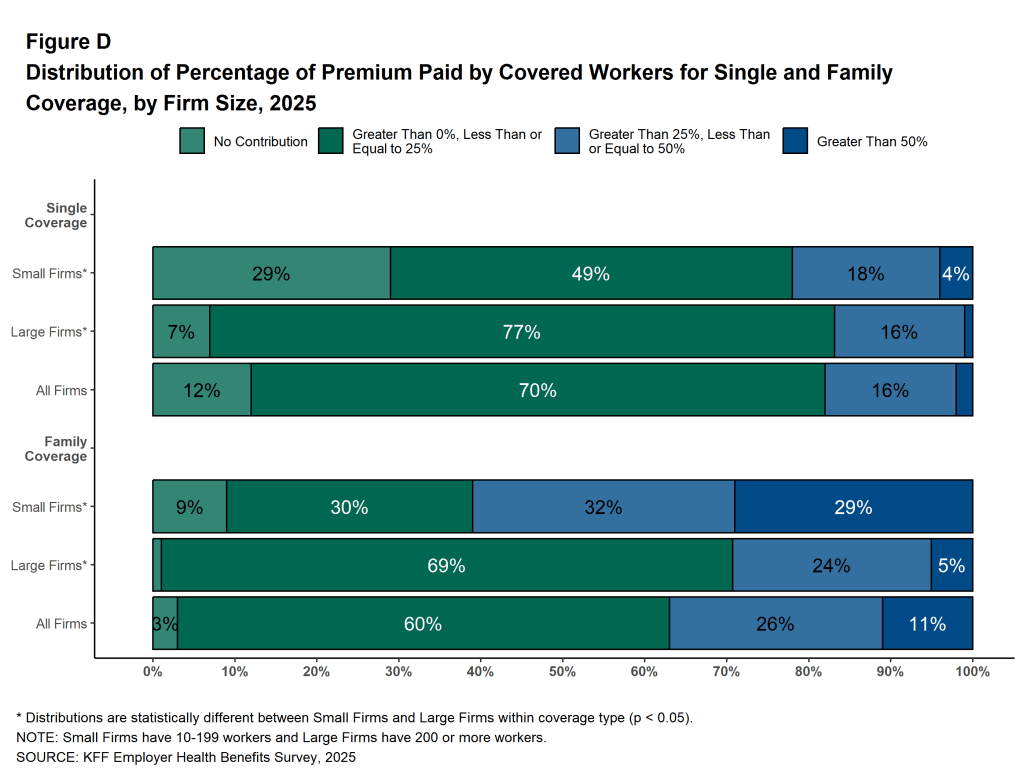
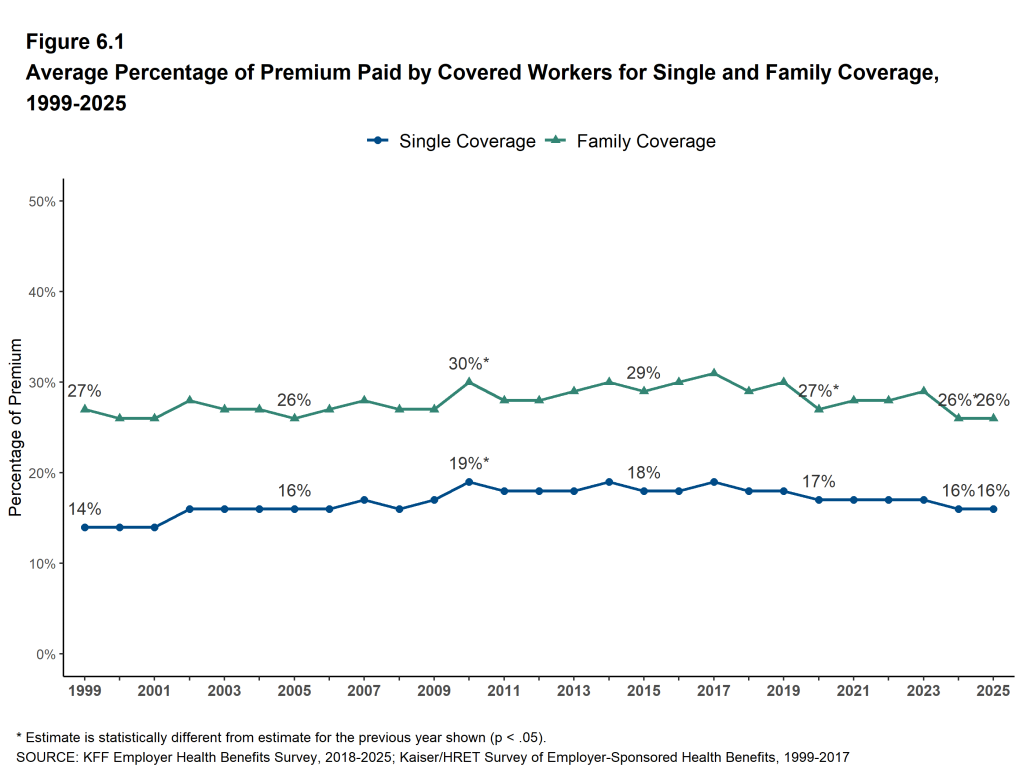
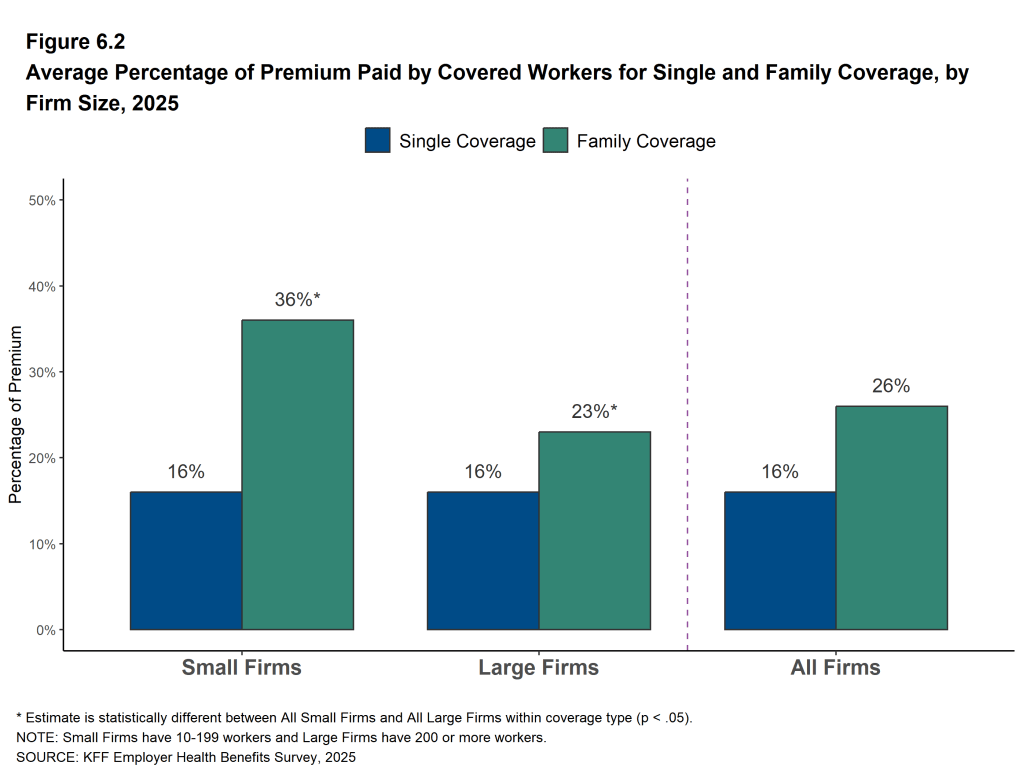
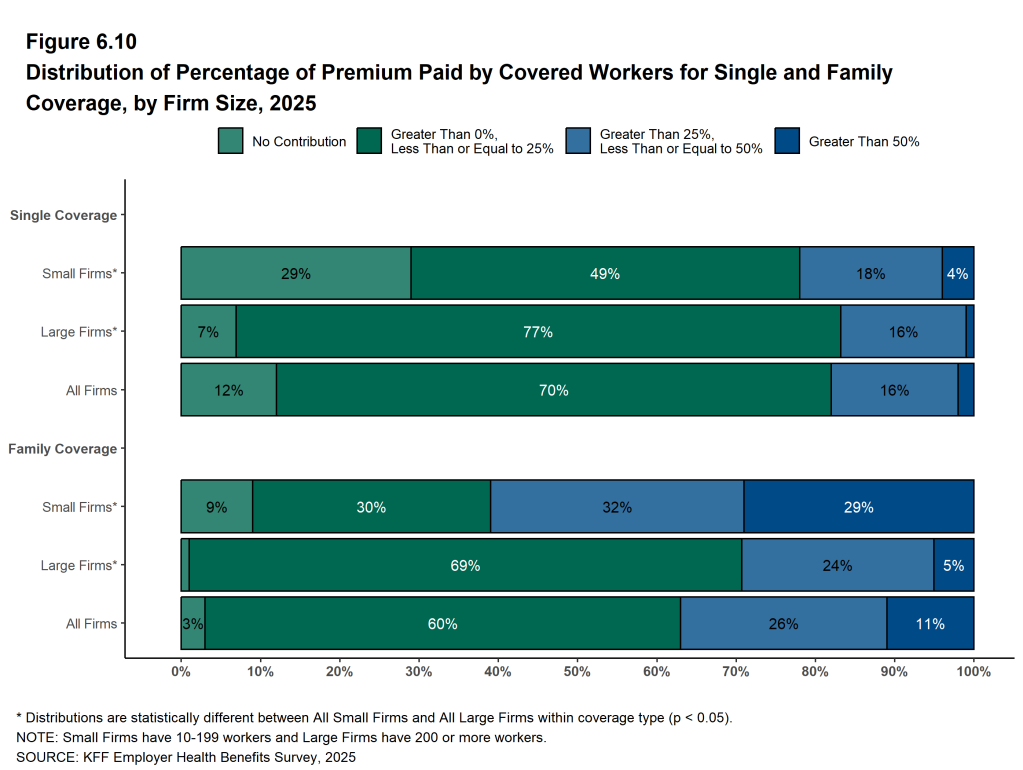
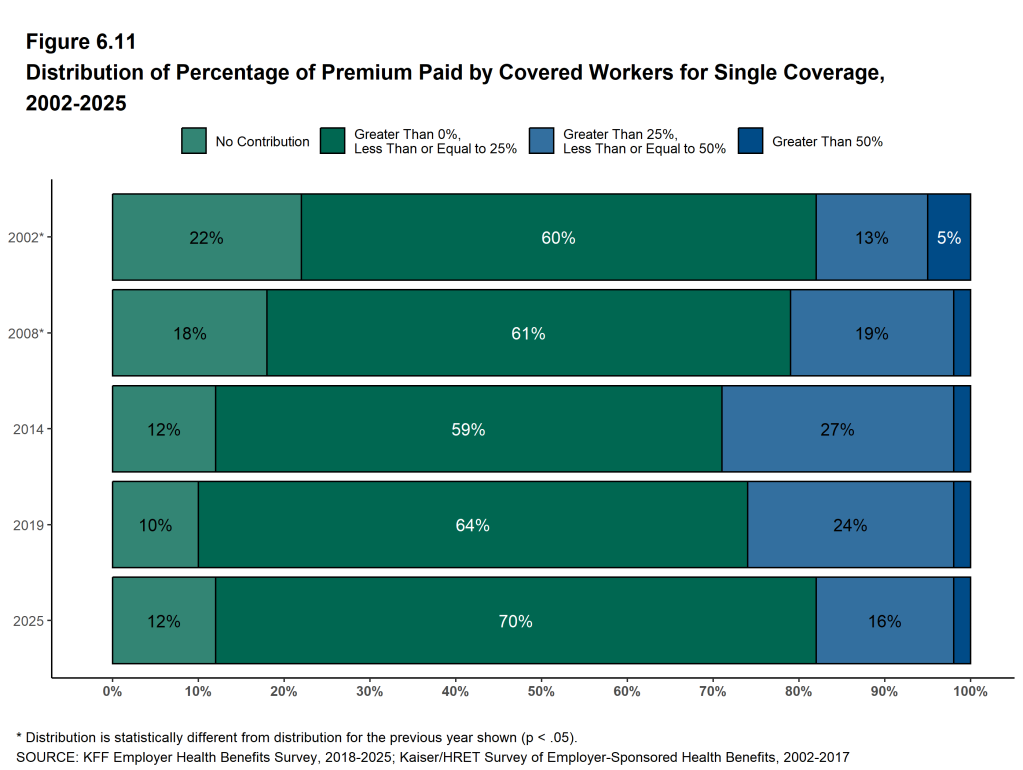
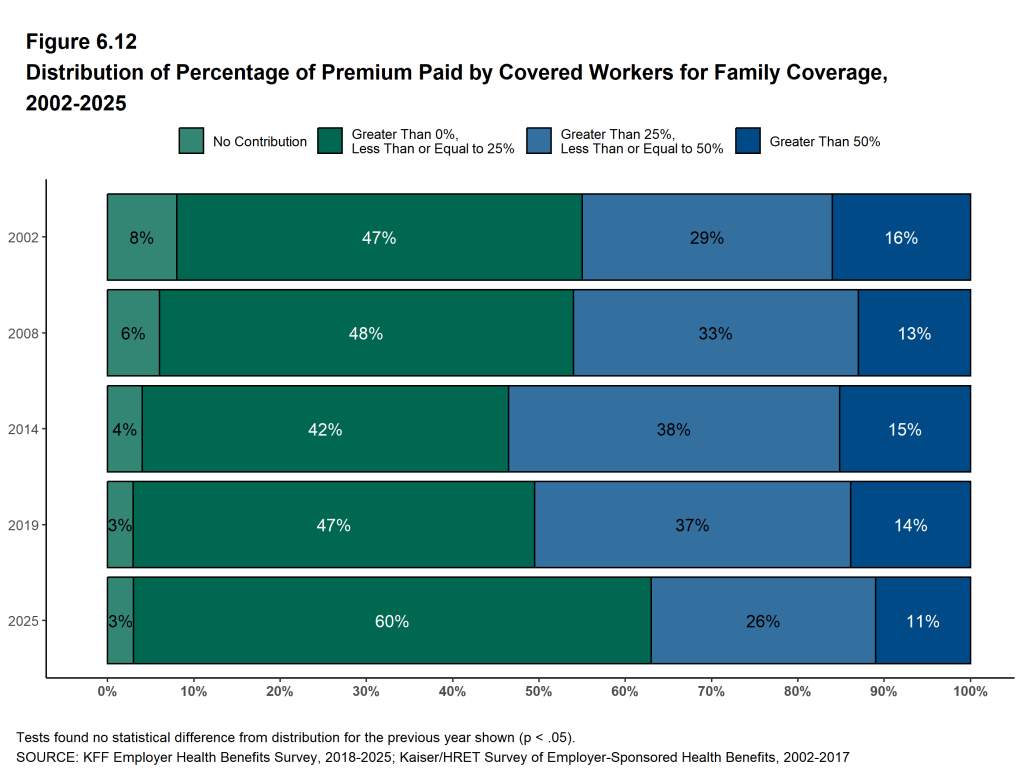
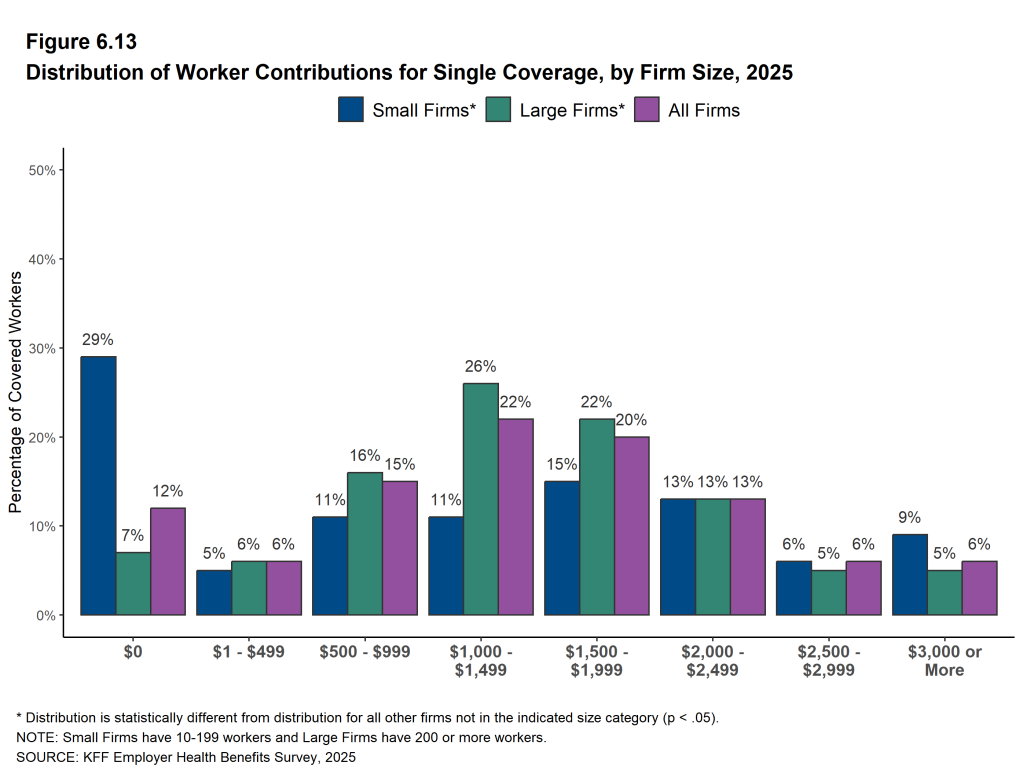
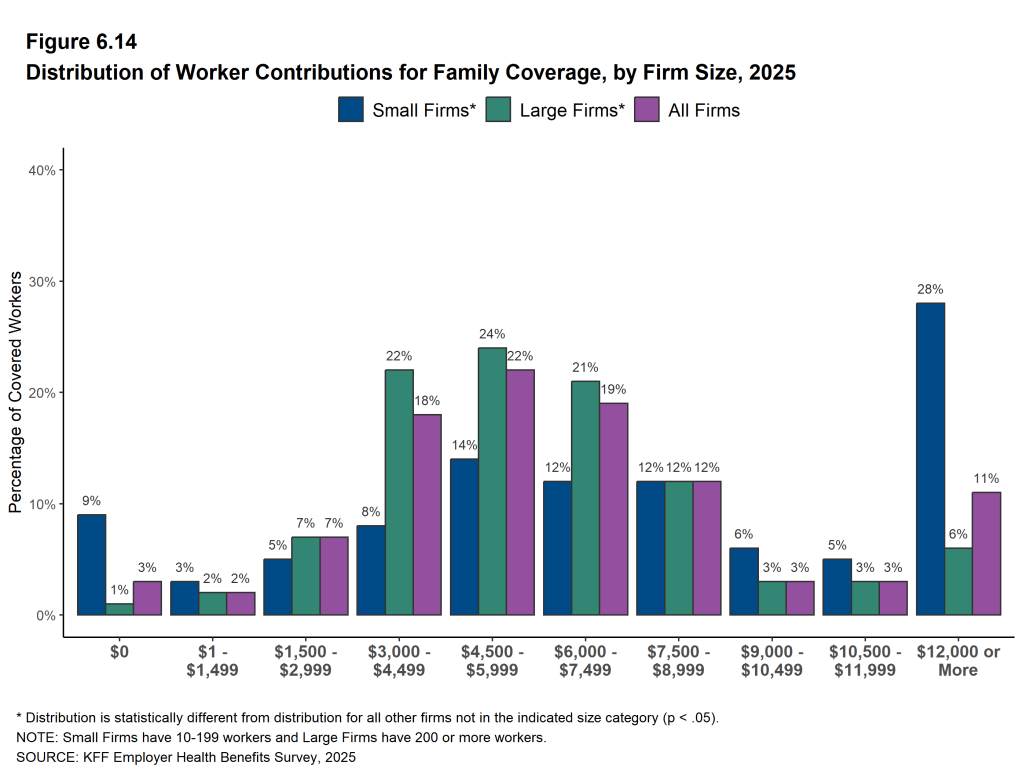
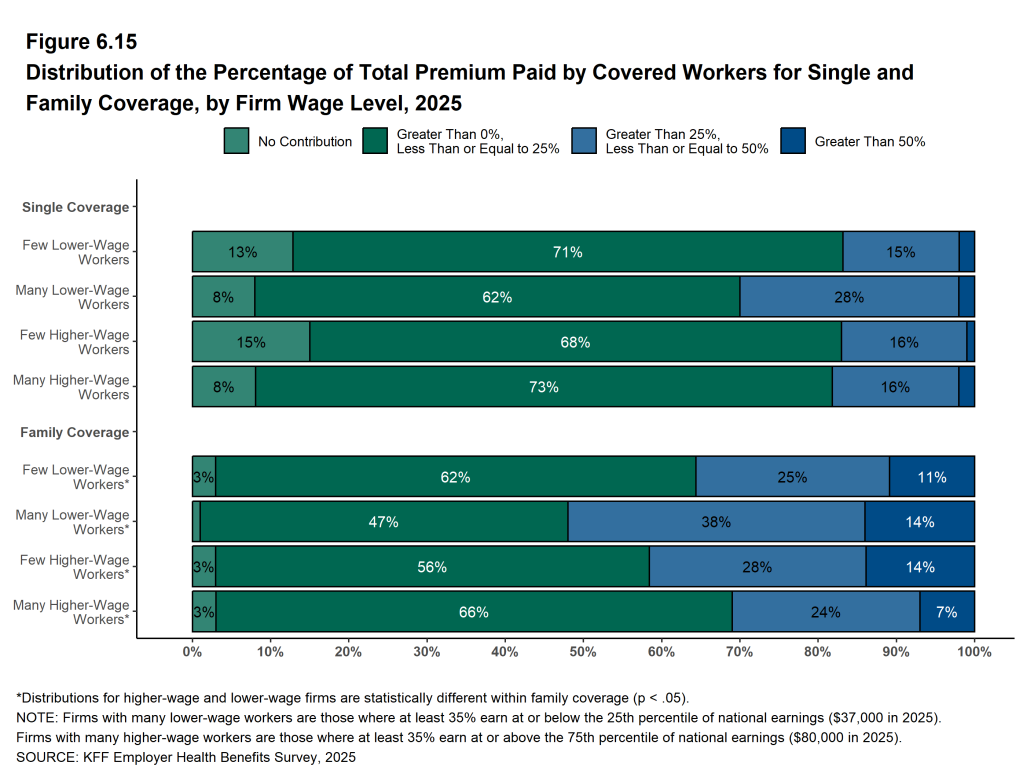
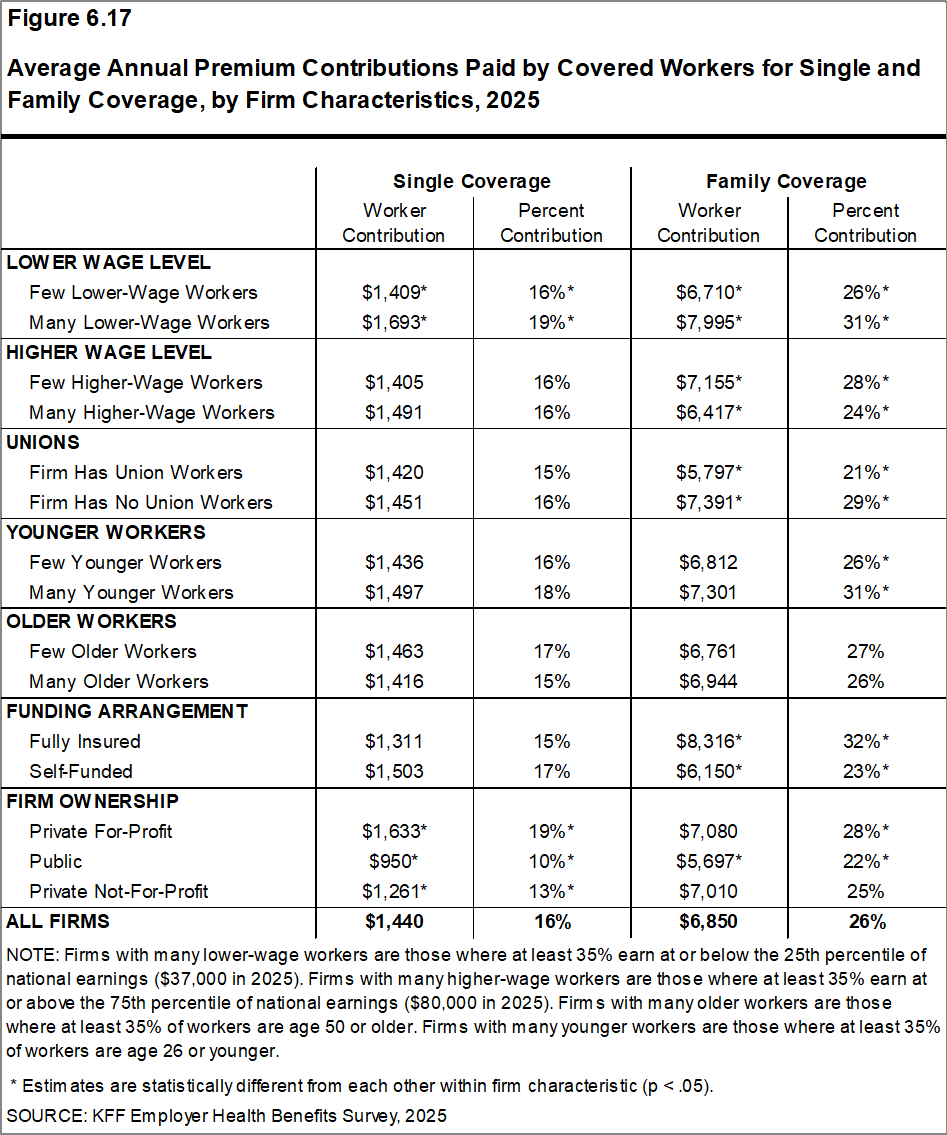
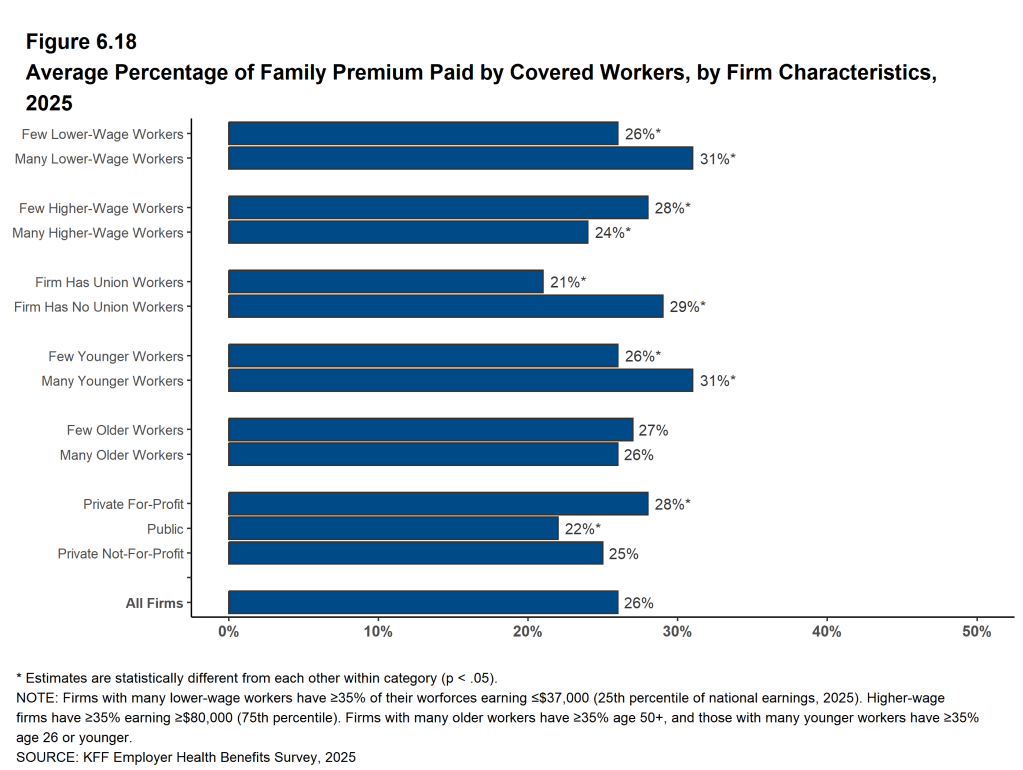
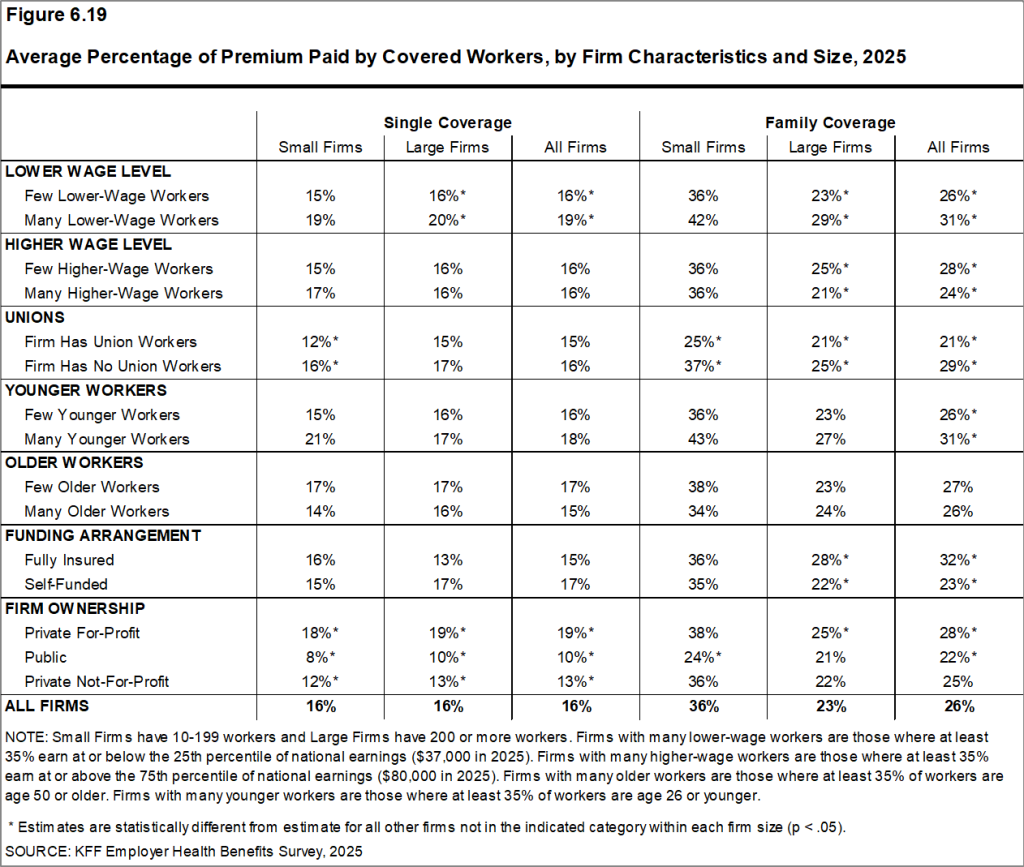
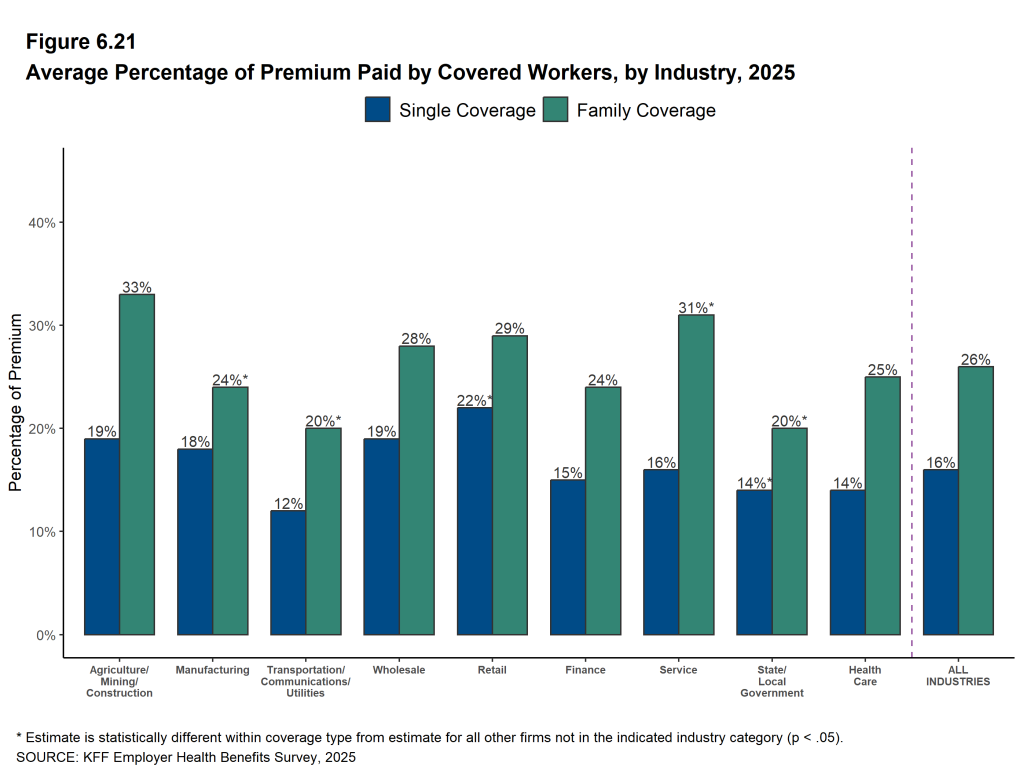
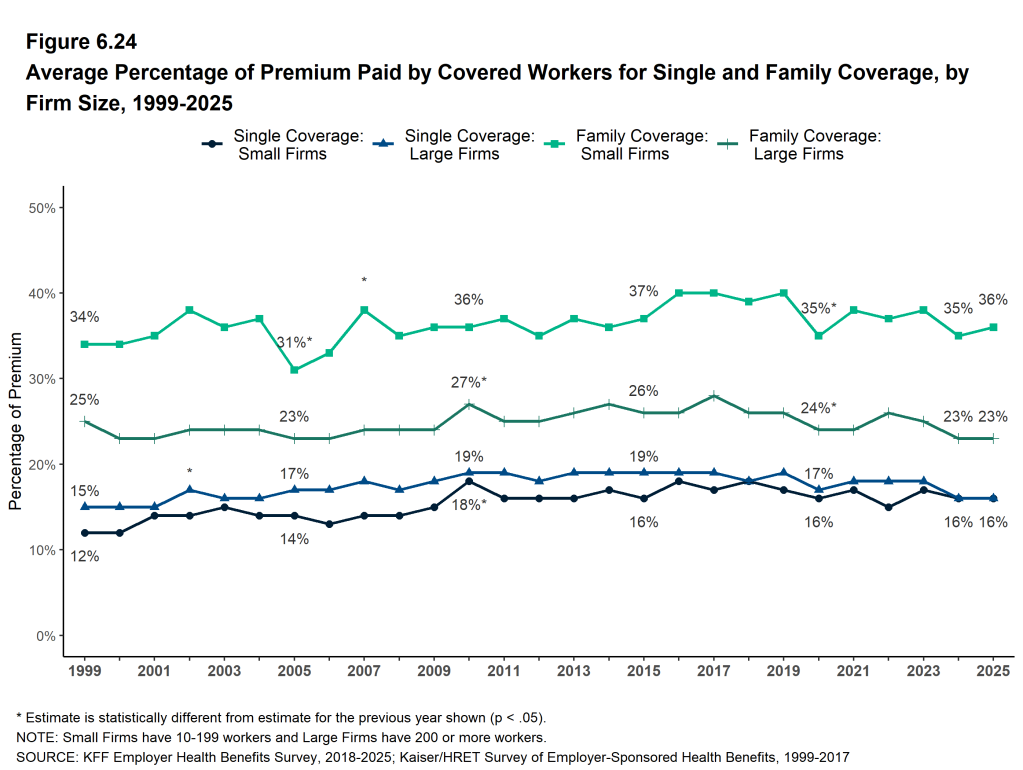
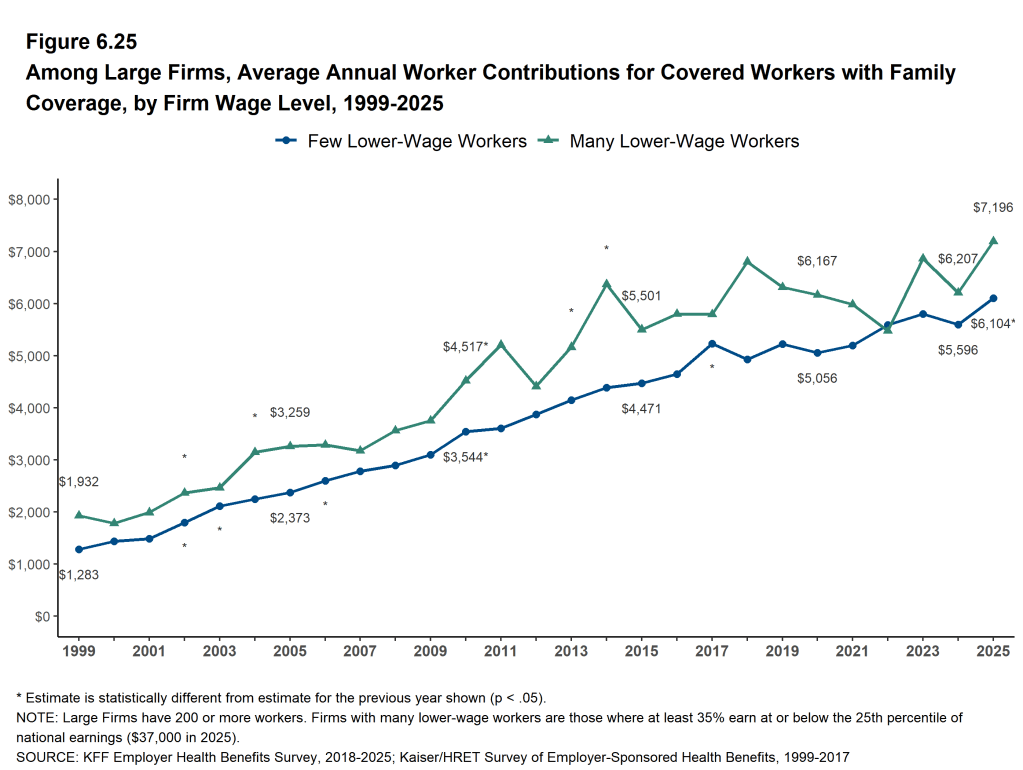
Most covered workers contribute to the cost of the premium directly. On average, covered workers contribute 16% of the premium for single coverage and 26% of the premium for family coverage, similar to the percentages contributed in 2024. The average contribution rates for single coverage are the same for covered workers in firms with 10 to 199 workers and in larger firms (16%) but the average contribution rate for family coverage is higher for covered workers in firms with 10 to 199 workers than for those in larger firms (36% vs. 23%). On average, covered workers at private, for-profit firms have relatively high premium contribution rates and covered workers in public firms have relatively low contribution rates for both single coverage and family coverage.
Twenty-nine percent of covered workers at firms with 10 to 199 workers are enrolled in a plan where the employer pays the entire premium for single coverage, compared with only 7% of covered workers at larger firms. In contrast, 29% of covered workers at firms with 10 to 199 workers are in a plan where they must contribute more than half of the premium for family coverage, compared to 5% of covered workers at larger firms [Figure D].
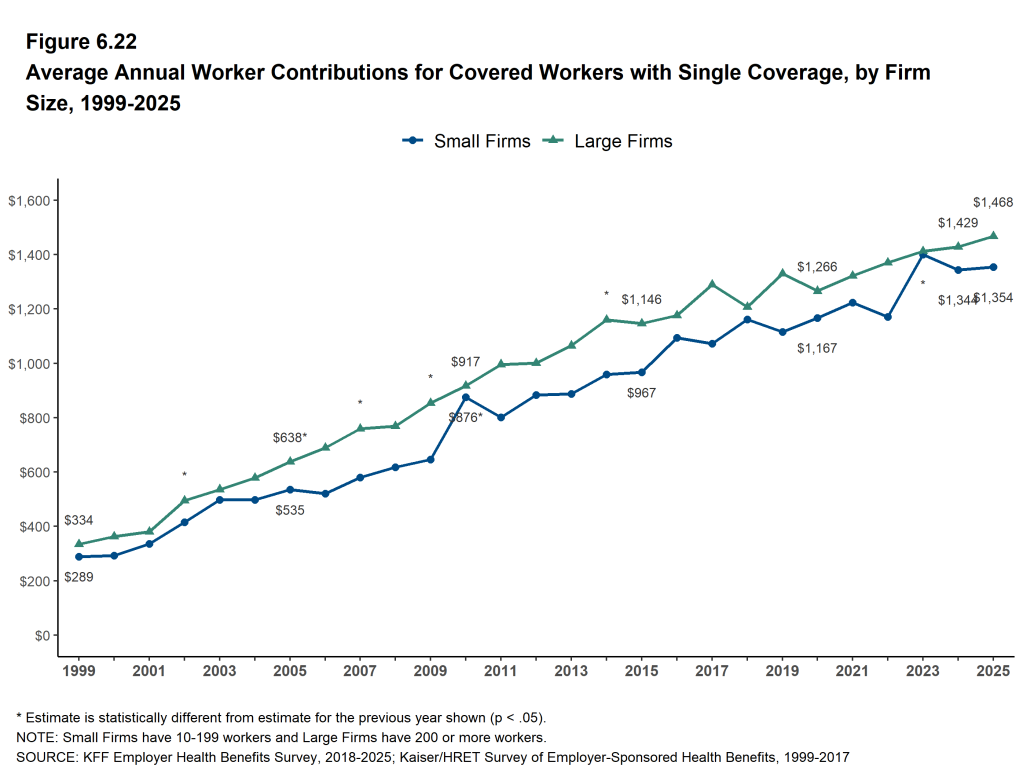
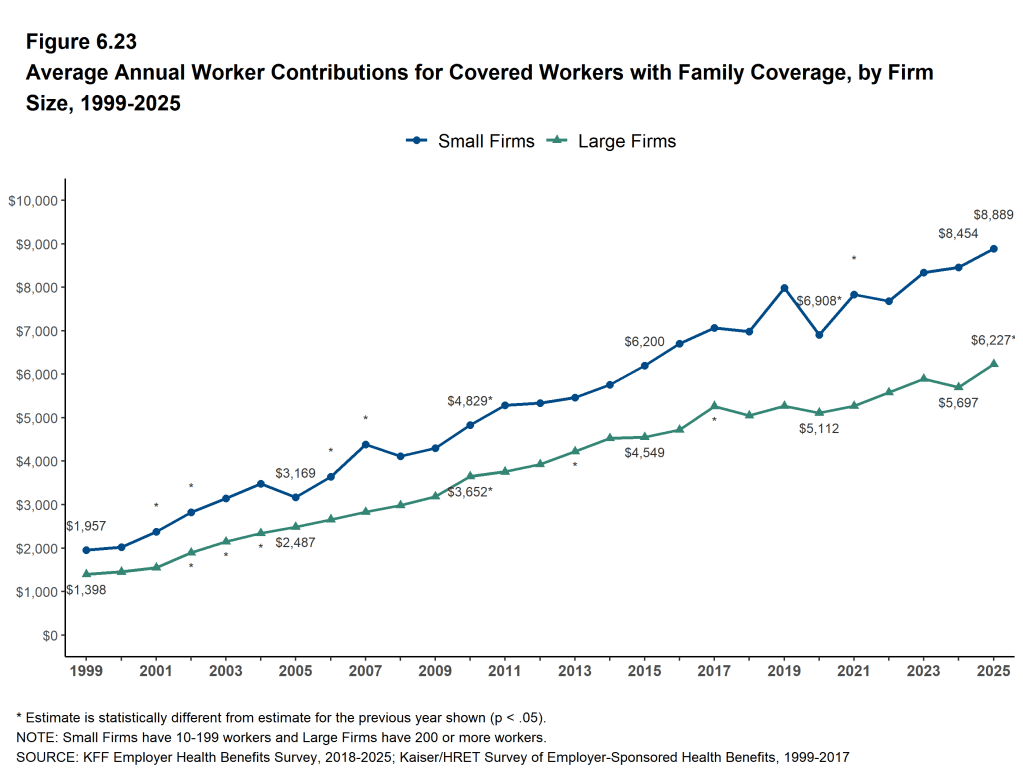
The average annual contribution amounts for covered workers are $1,440 for single coverage, similar to the amount last year, and $6,850 for family coverage, higher than the amount last year. The average contribution amount for family coverage for covered workers at firms with 10 to 199 workers ($8,889) is higher than the amount for covered workers at larger firms ($6,227) [Figure C]. Eleven percent of covered workers, including 28% of covered workers at firms with 10 to 199 workers, are in a plan with a worker contribution of $12,000 or more for family coverage.
Figure D: Distribution of Percentage of Premium Paid by Covered Workers for Single and Family Coverage, by Firm Size, 2025
PLAN ENROLLMENT
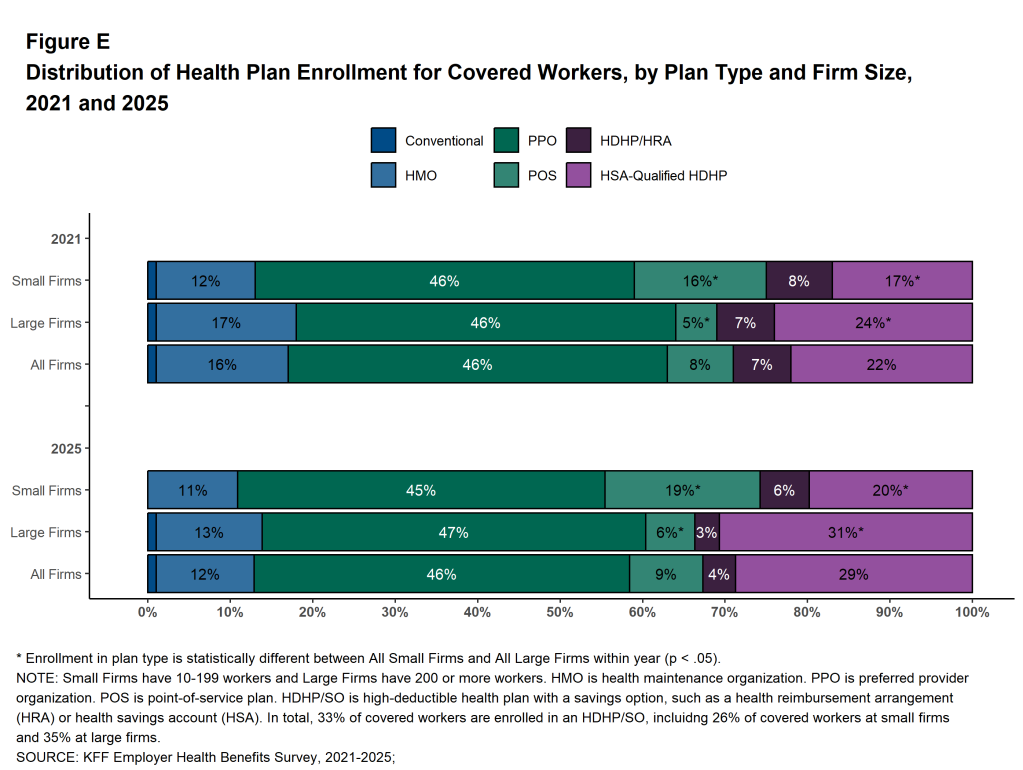
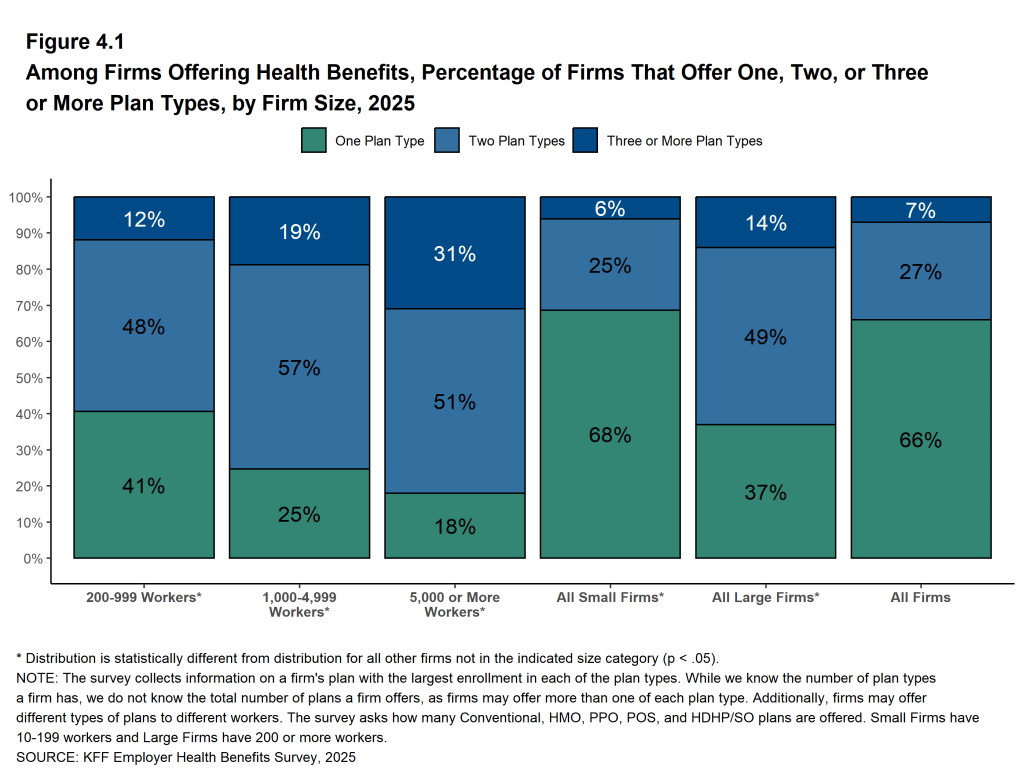
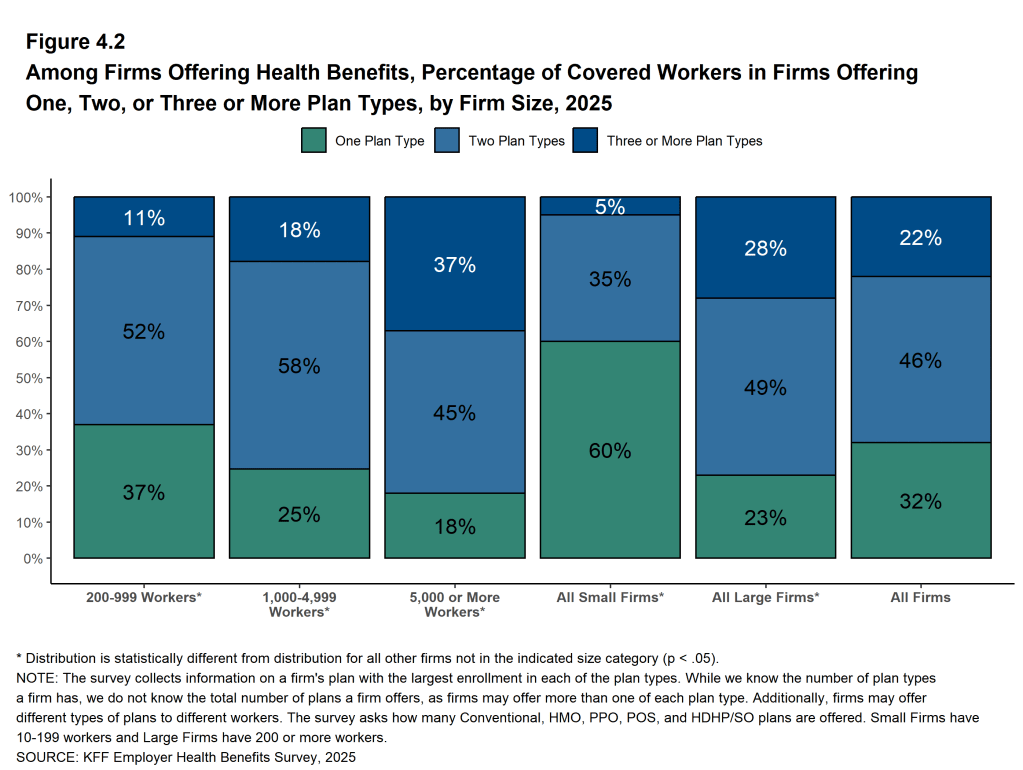
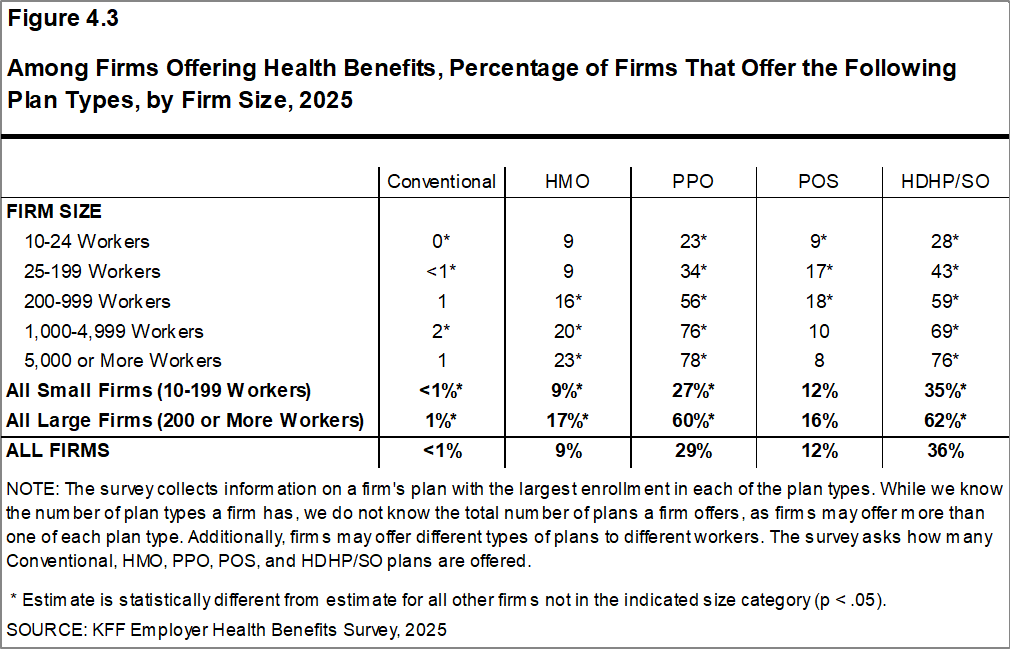
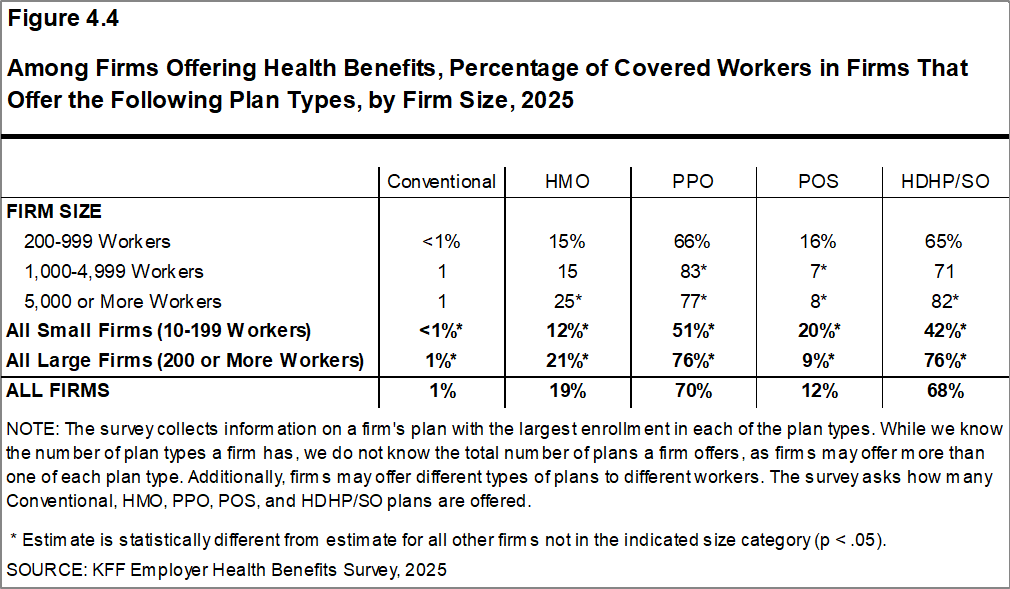
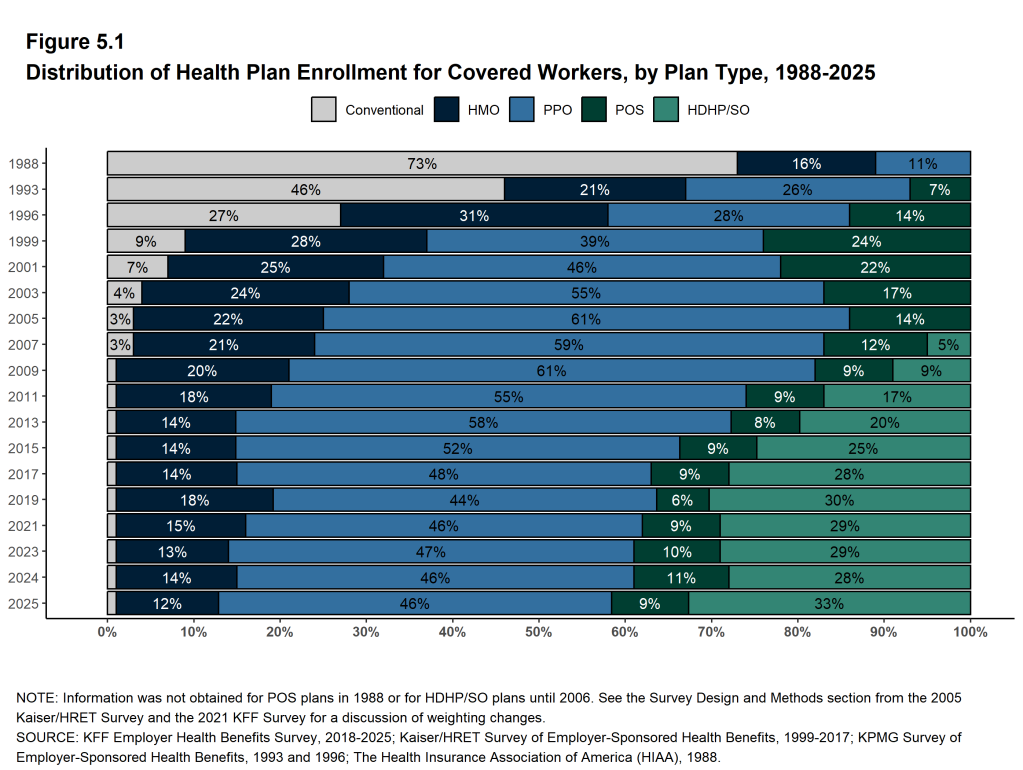
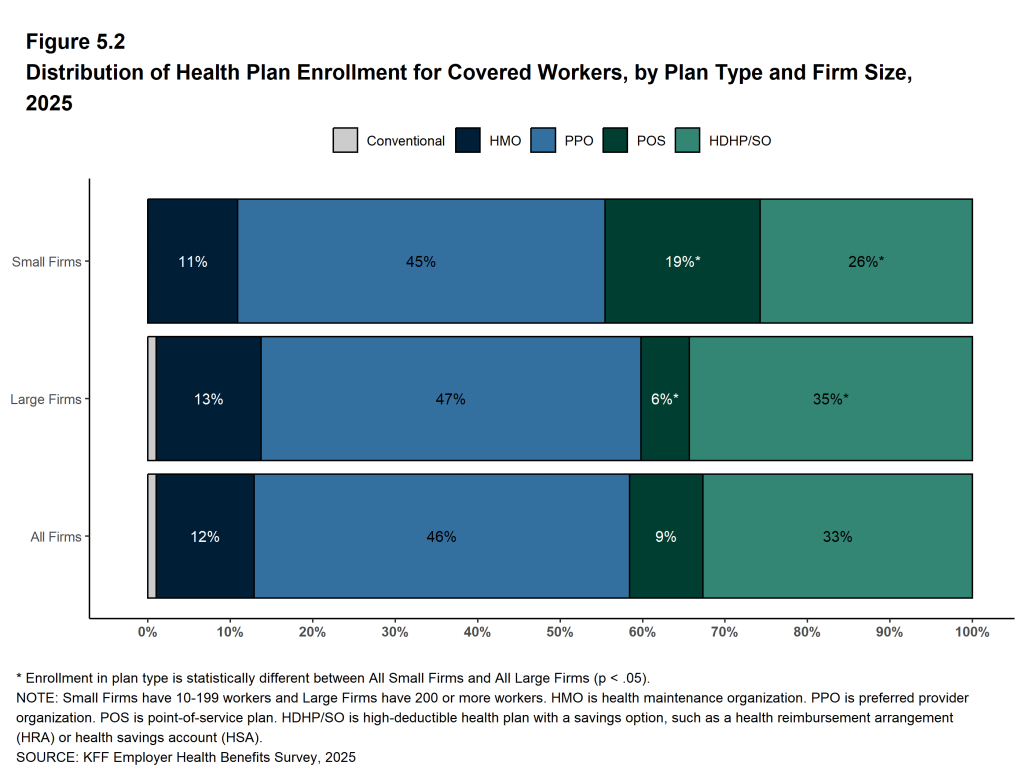
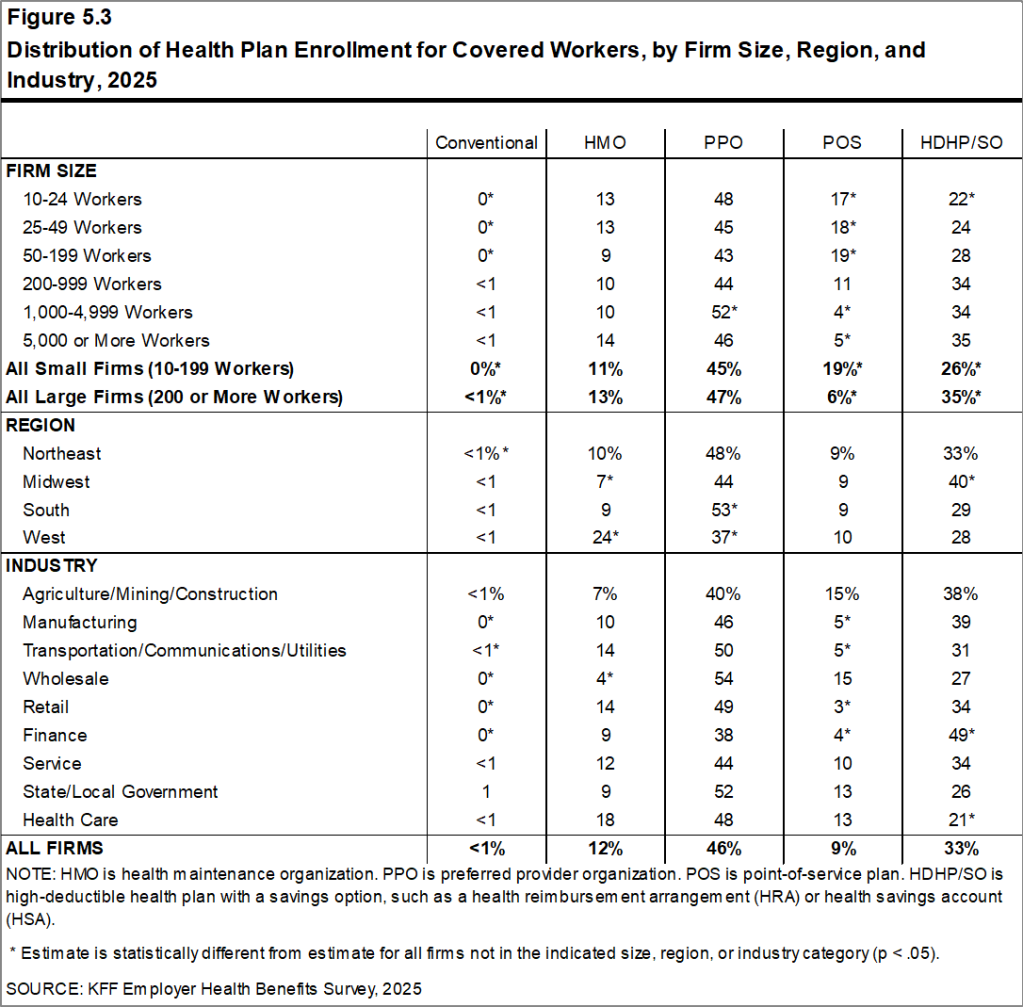
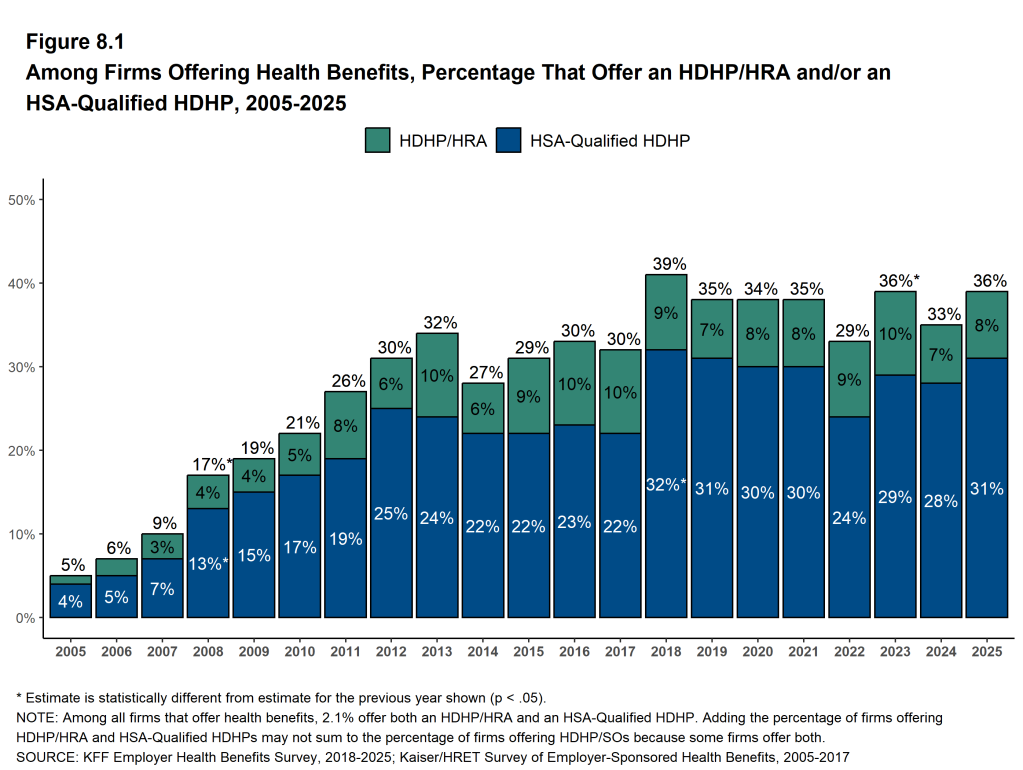
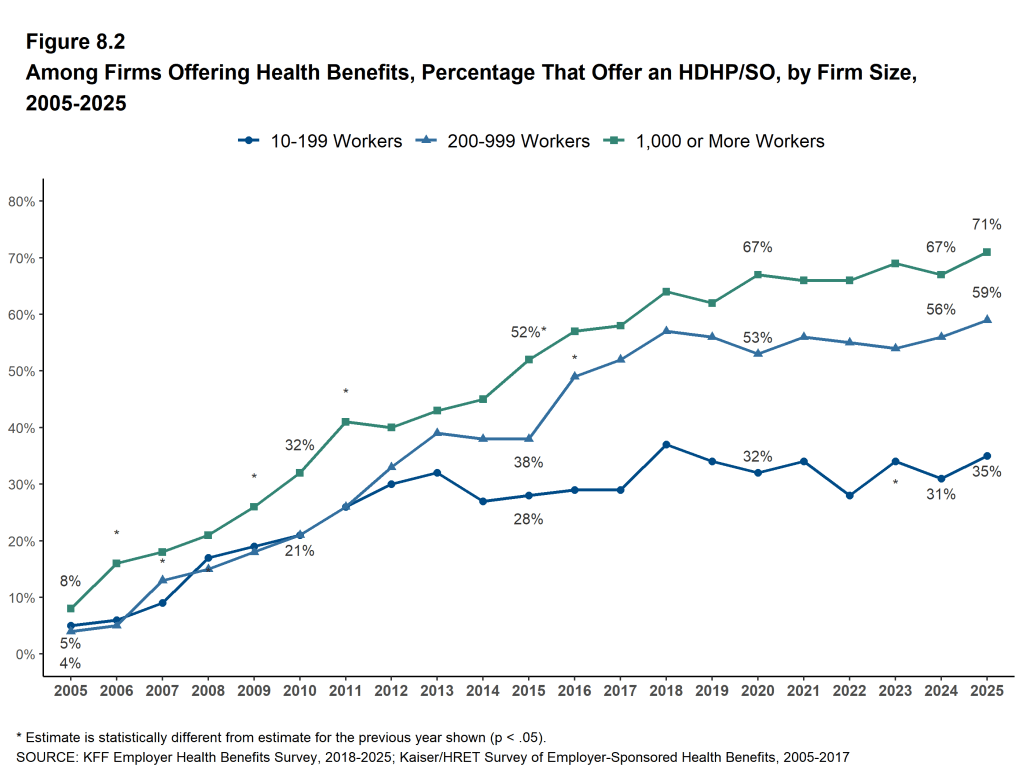
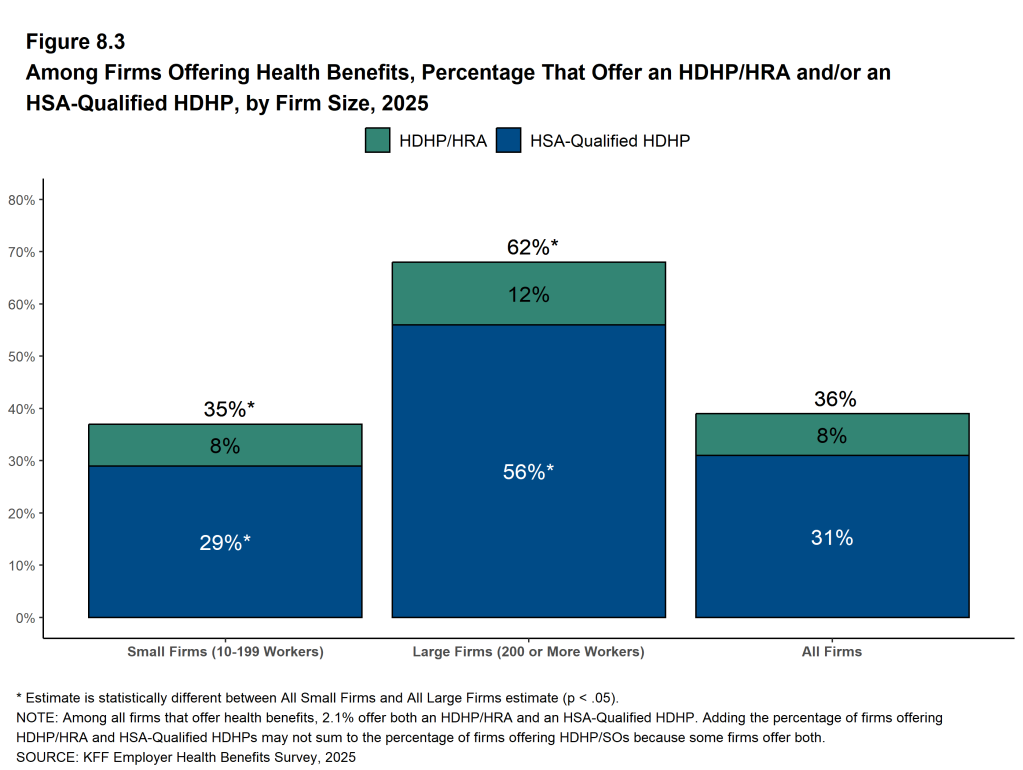
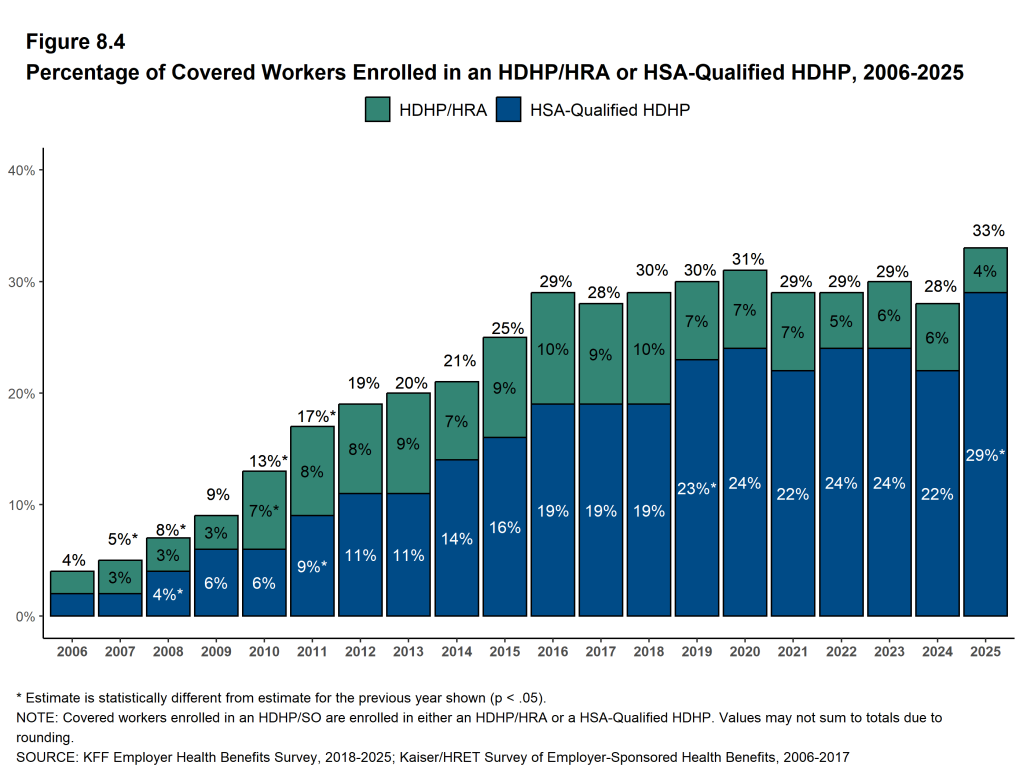
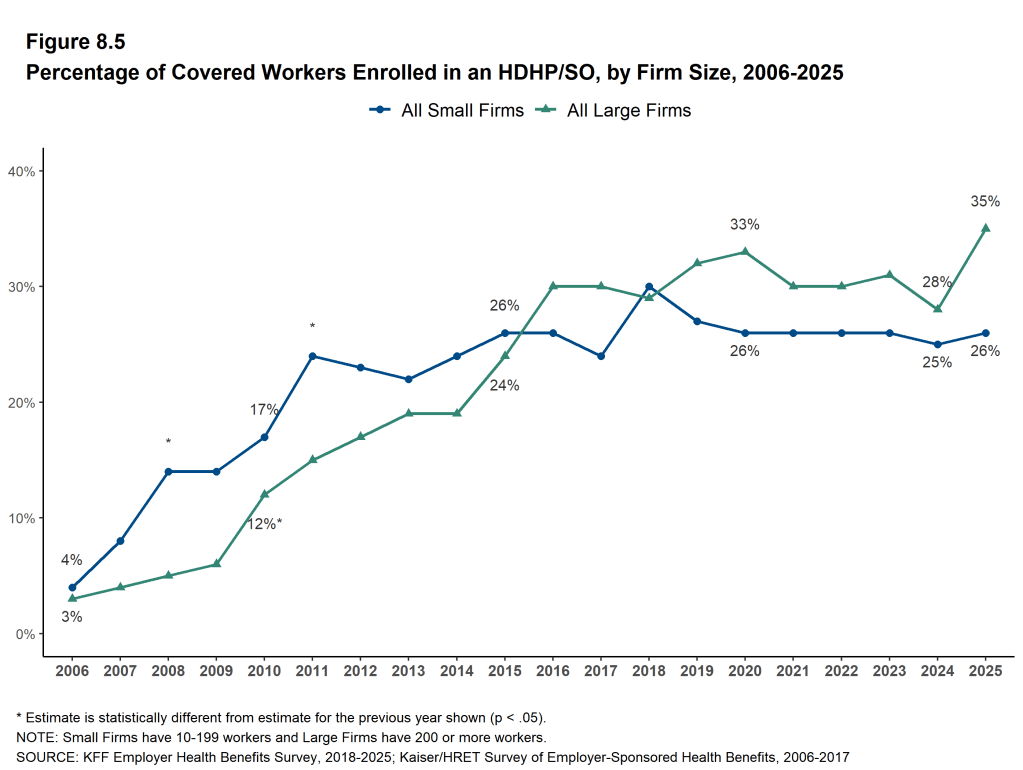
PPOs continue to be the most common plan type in 2025. Forty-six percent of covered workers are enrolled in a PPO, 33% are enrolled in a high-deductible plan with a savings option (HDHP/SO), 12% are enrolled in an HMO, 9% are enrolled in a POS plan, and less than one percent are enrolled in a conventional (also known as an indemnity) plan [Figure E].
Figure E: Distribution of Health Plan Enrollment for Covered Workers, by Plan Type and Firm Size, 2021 and 2025
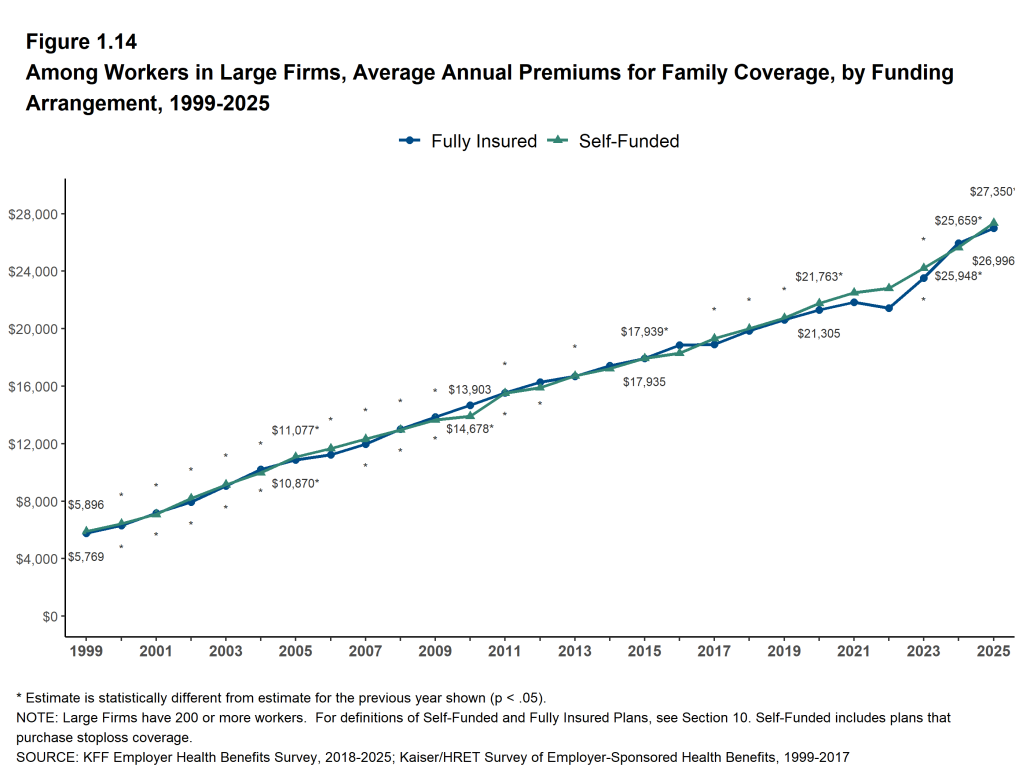
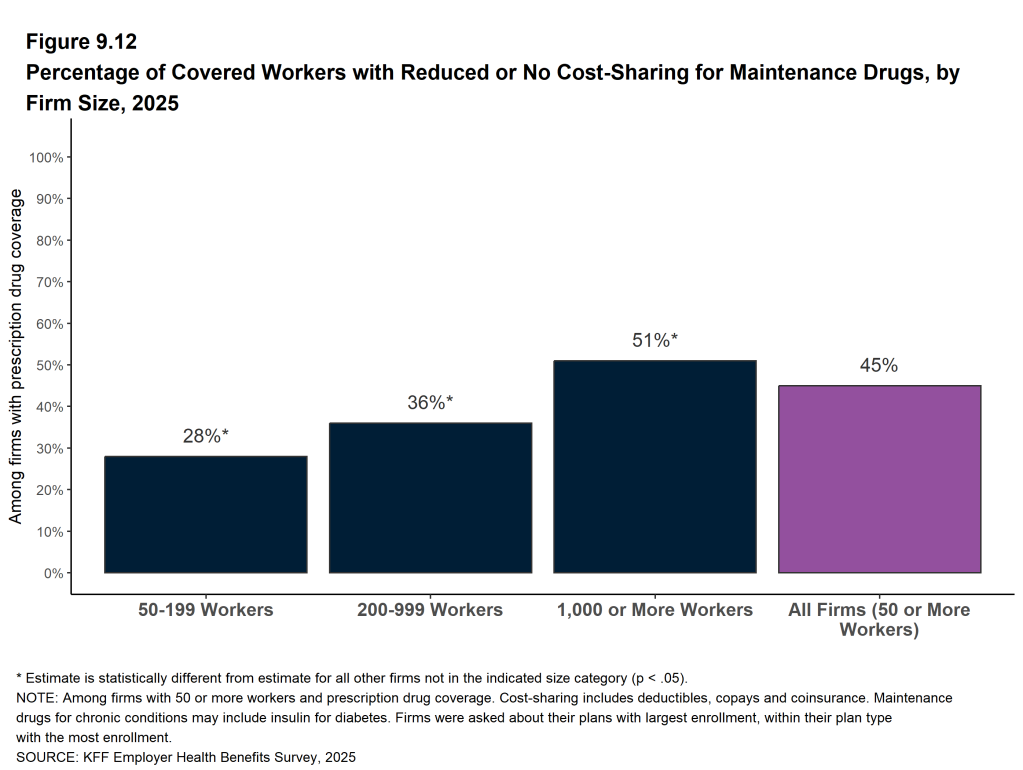
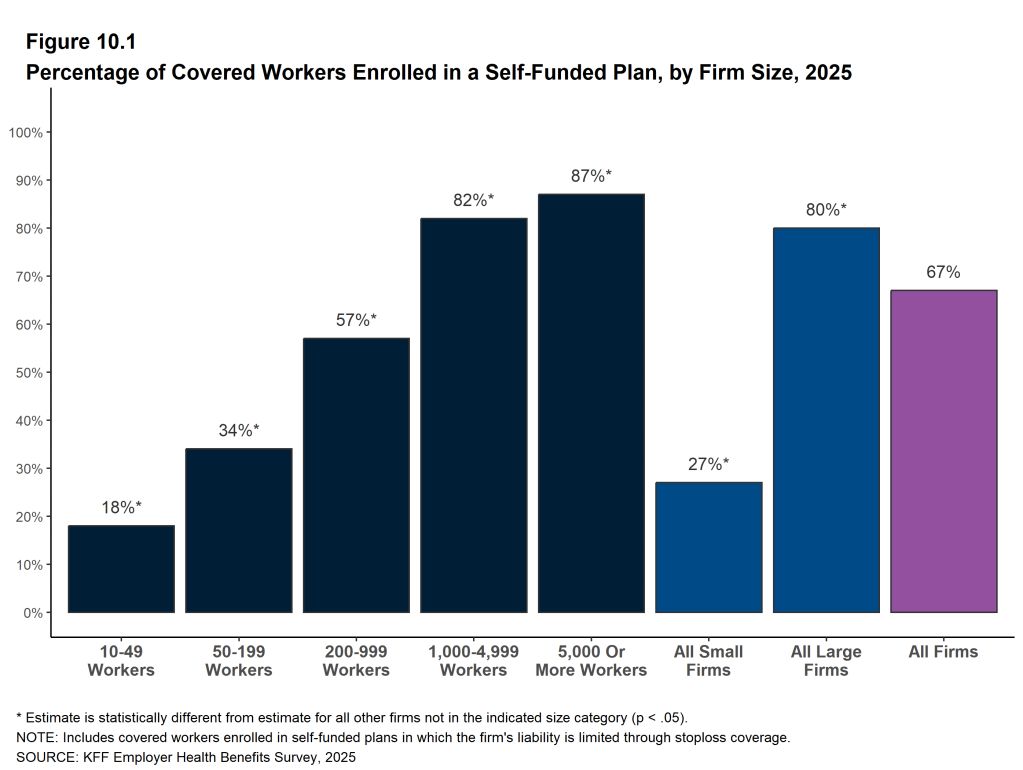
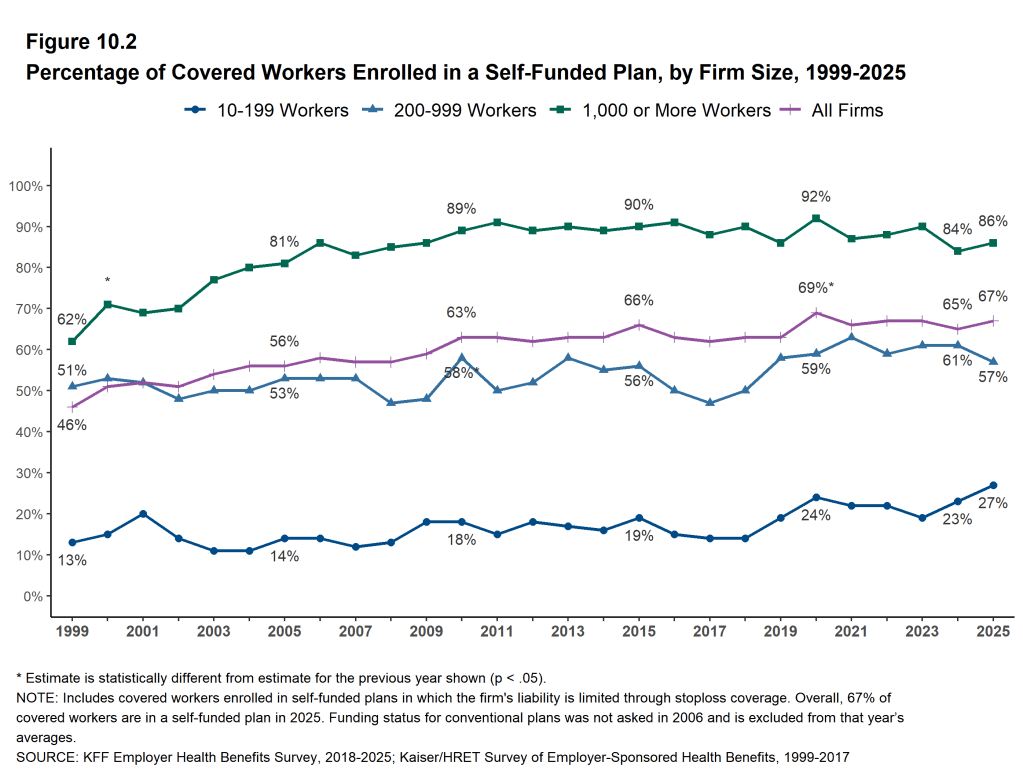
SELF FUNDING
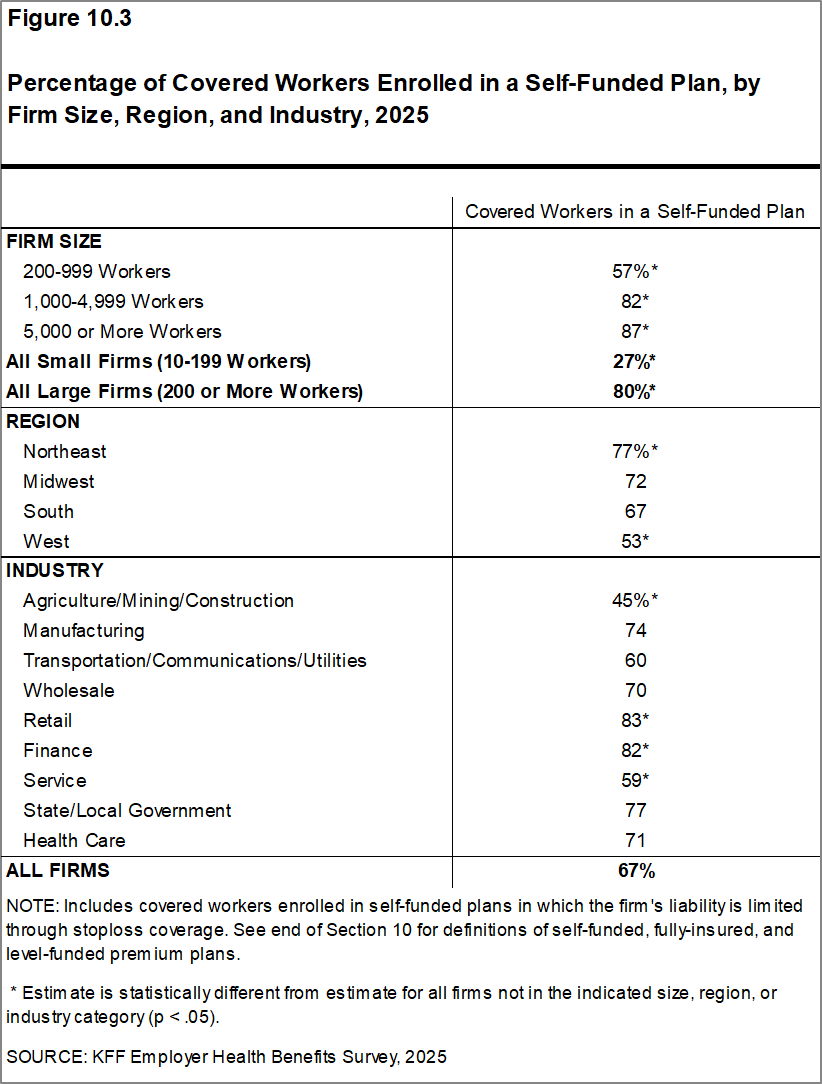
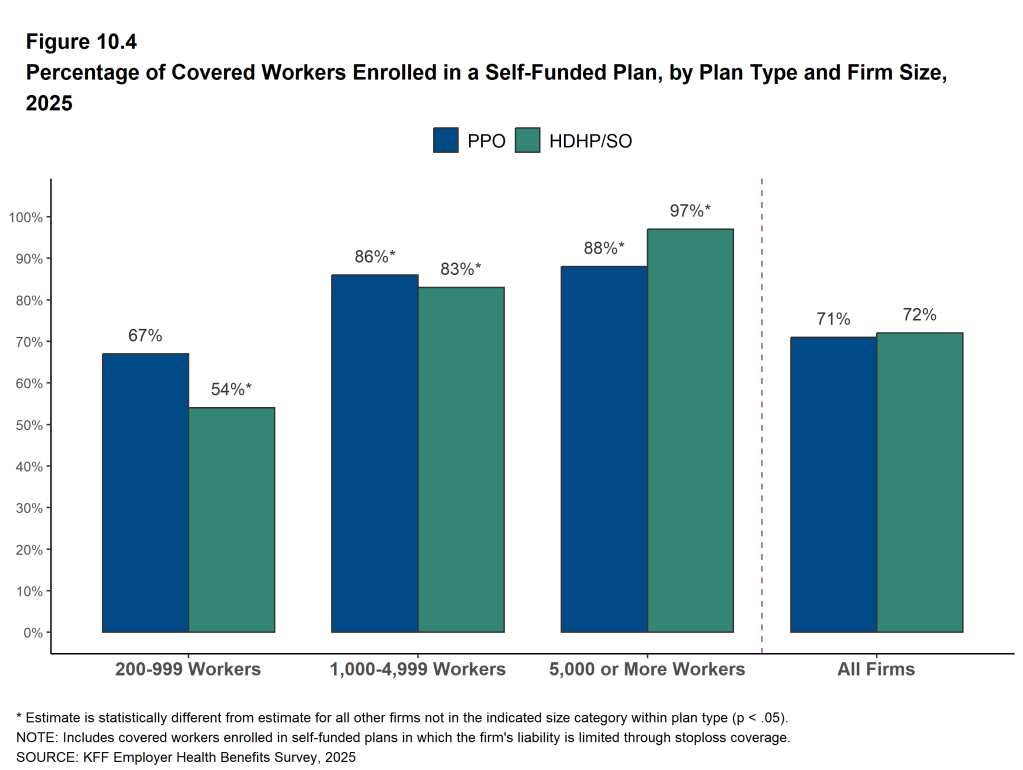
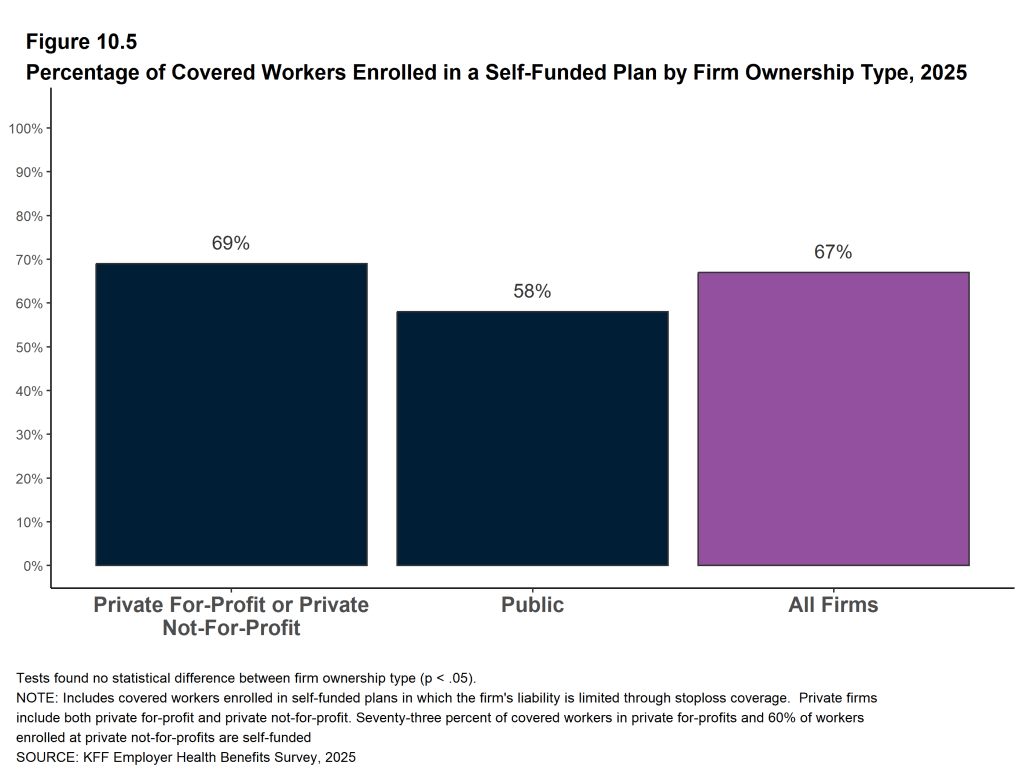
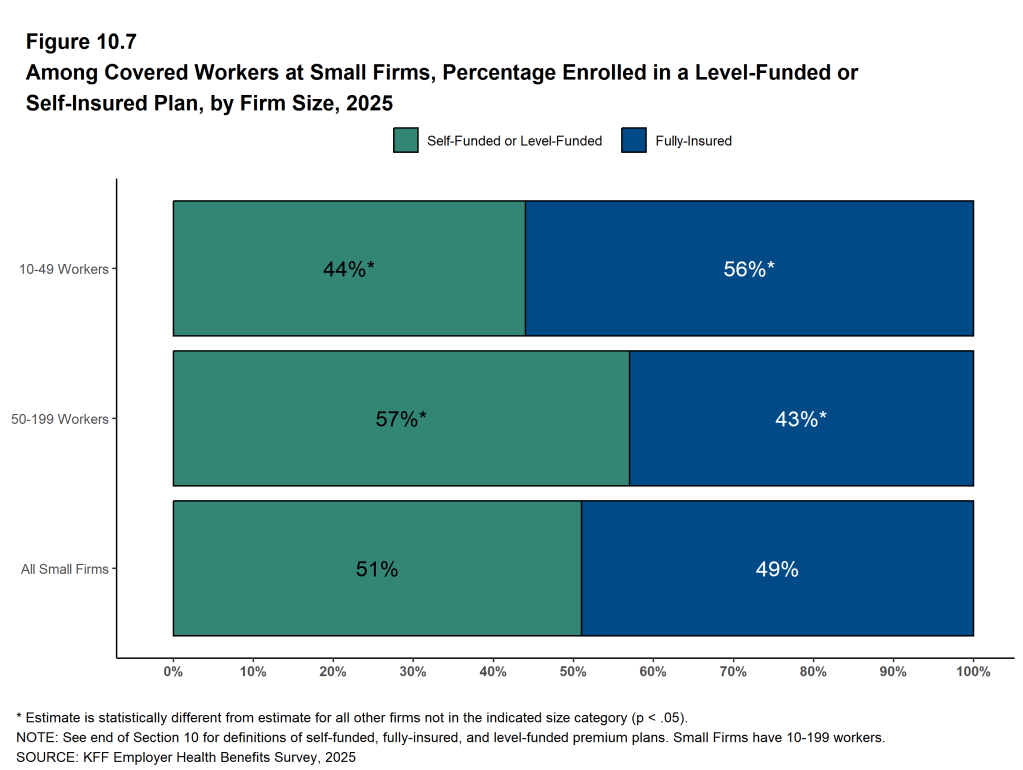
Many firms – particularly larger firms – have self-funded health plans, which means that they pay for the health services of enrollees directly from their own funds rather than through the purchase of health insurance. Sixty-seven percent of covered workers, including 27% of covered workers at firms with 10 to 199 workers and 80% at larger firms, are enrolled in plans that are self-funded.
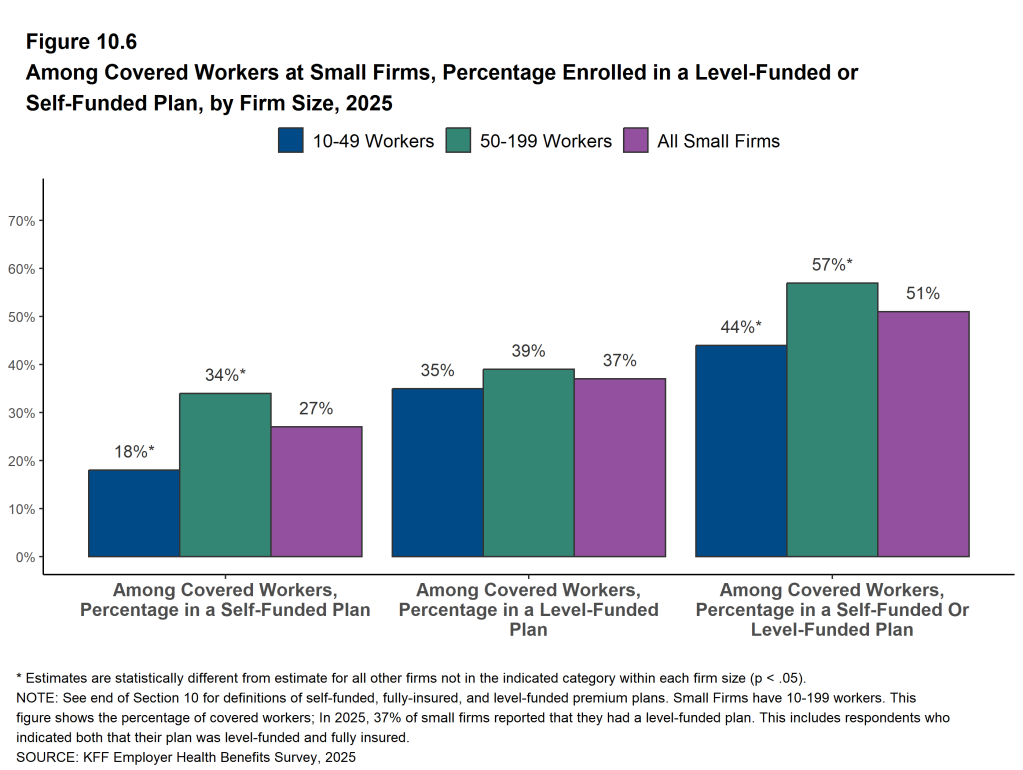
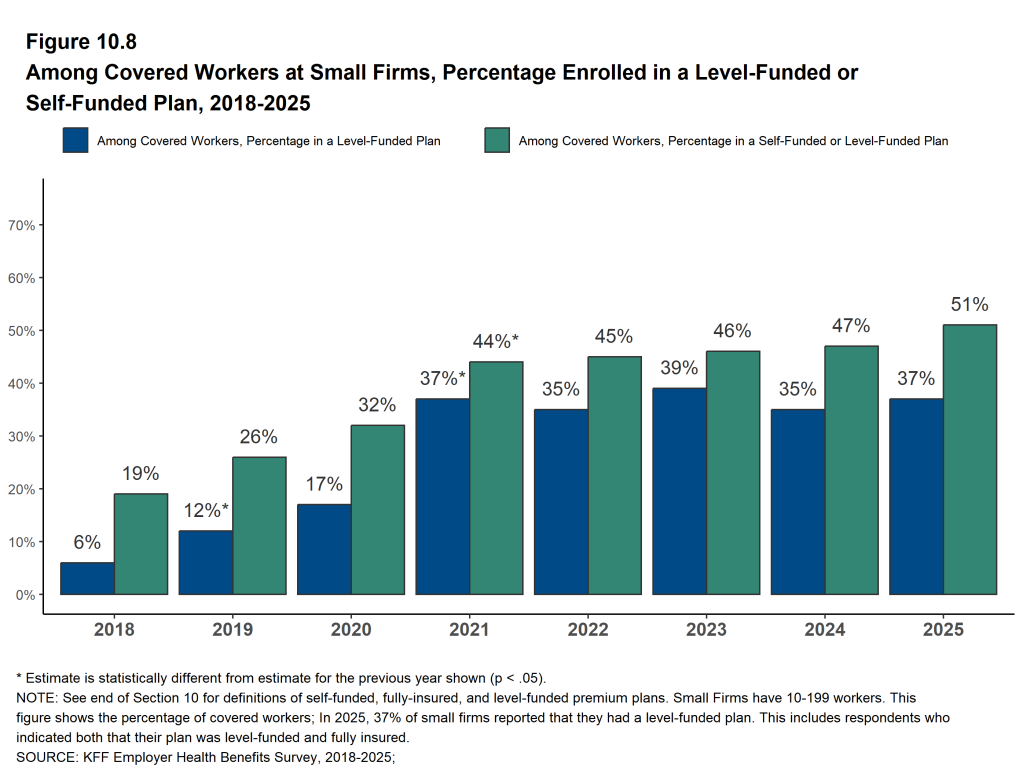
Thirty-seven percent of covered workers in firms with 10 to 199 workers are covered by a level-funded plan, similar to the percentage in 2024. Level-funded arrangements combine a relatively small self-funded component with stop-loss insurance, which limits the employer’s liability and transfers a substantial share of risk to insurers. These plans have the potential to meaningfully affect competition in the small group market because, unlike insured plans, they use health status in rating and underwriting, and are not required to provide all of the essential health benefits that are mandatory for insured plans.
EMPLOYEE COST SHARING
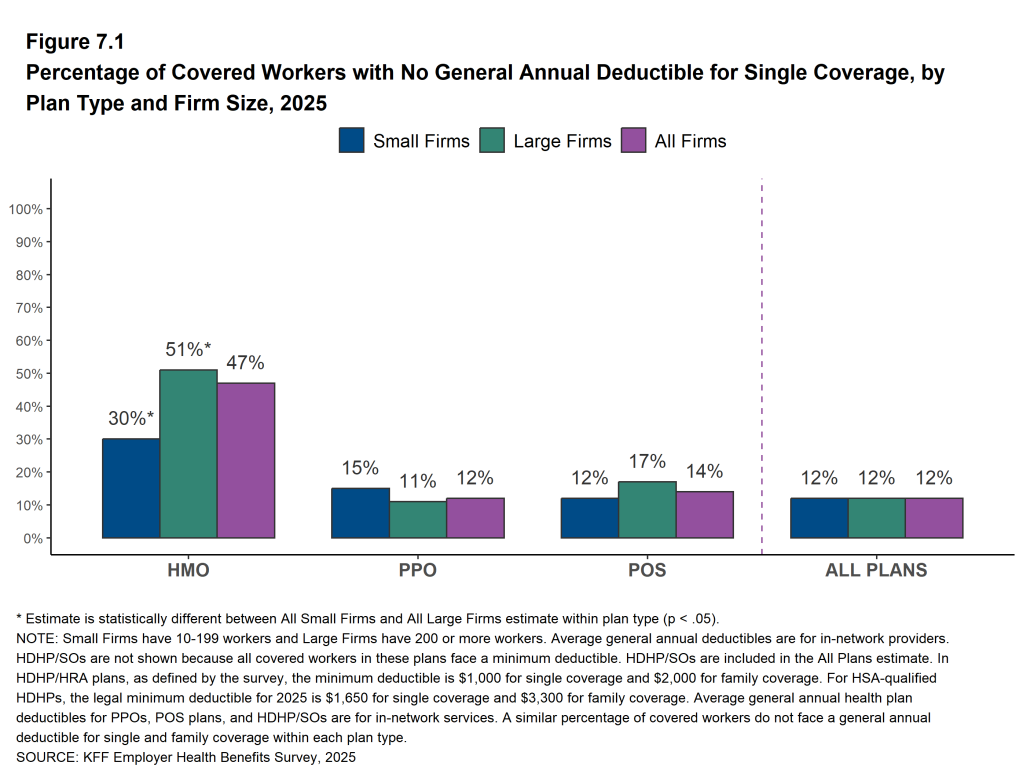
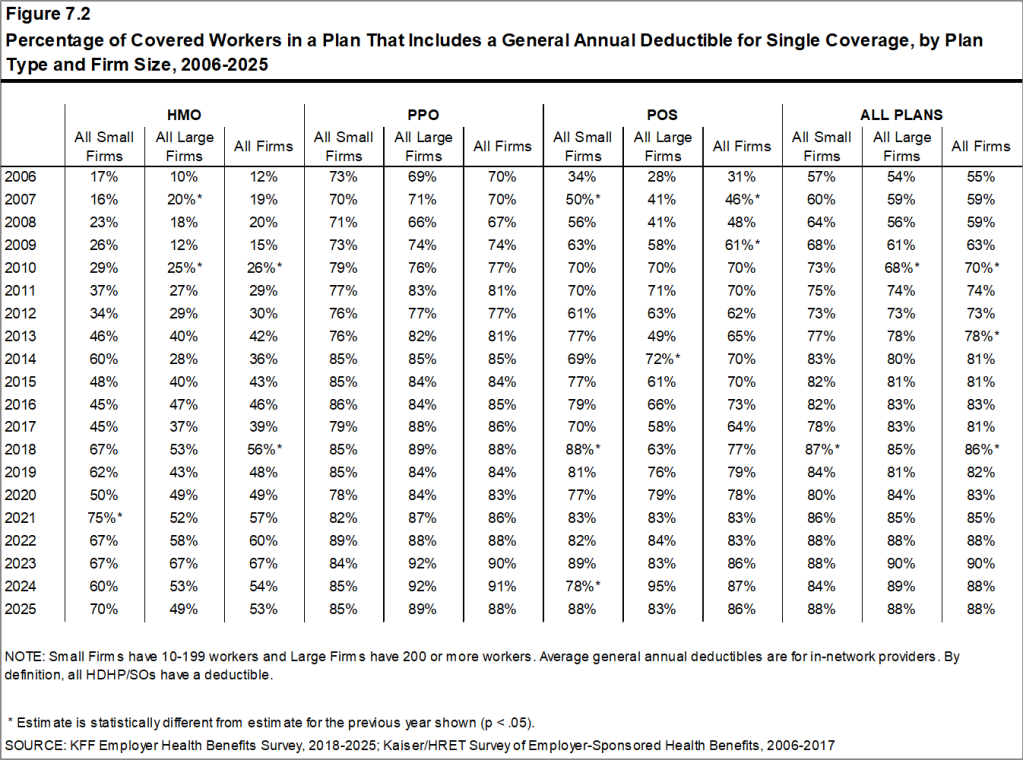
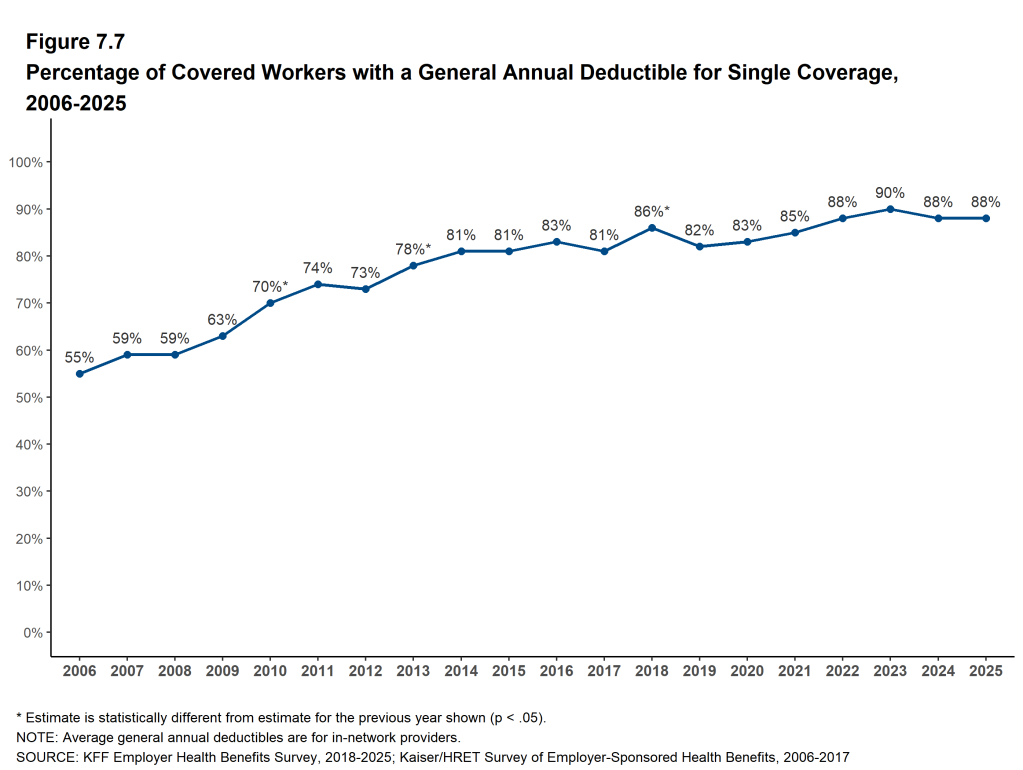
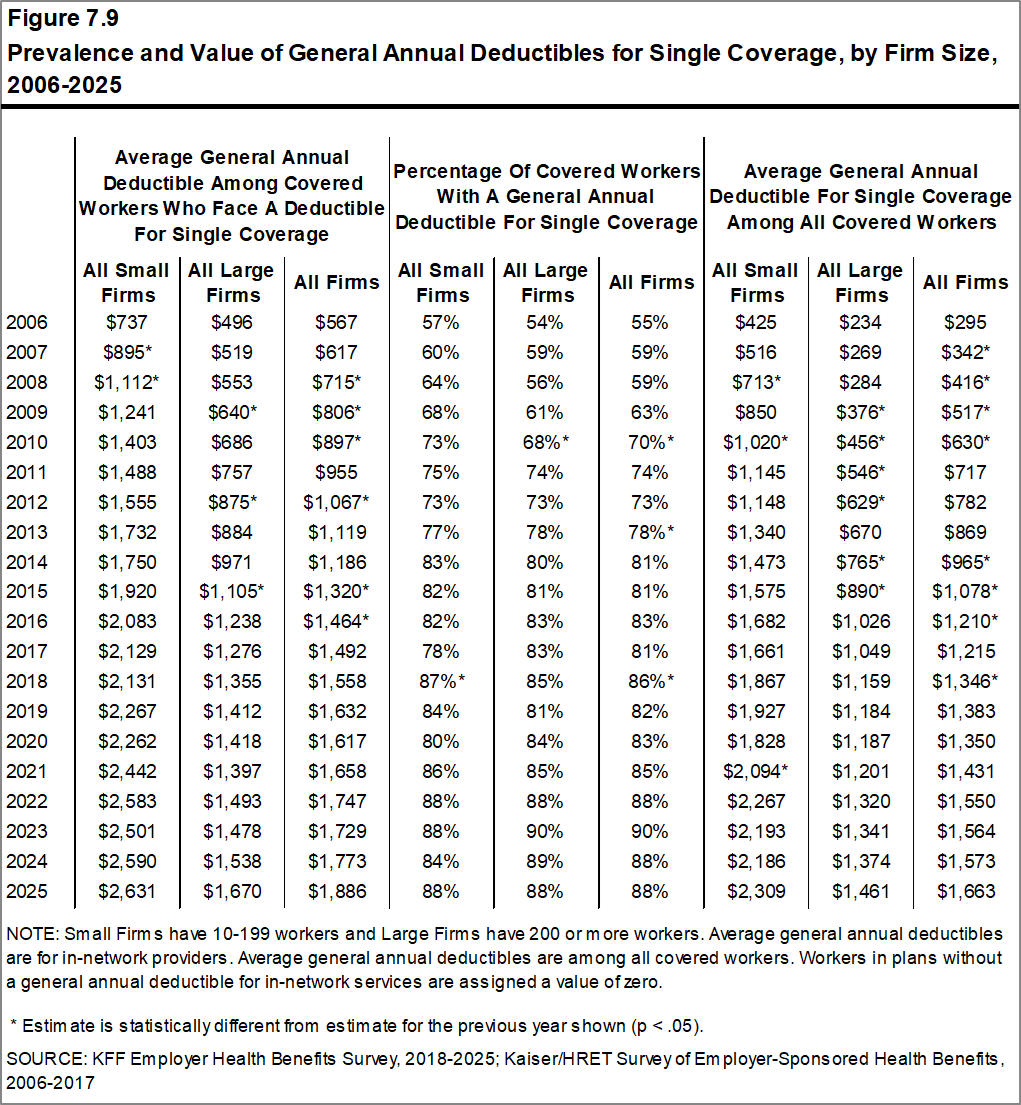
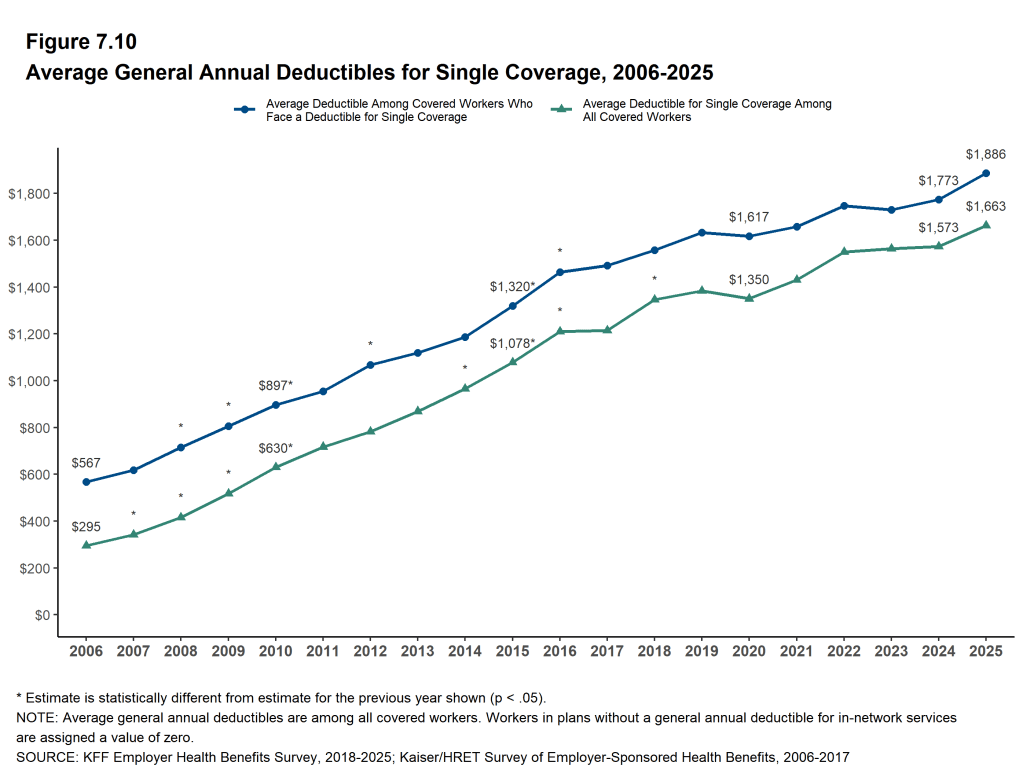
Eighty-eight percent of workers with single coverage have a general annual deductible that must be met before most services are paid for by the plan, the same percentage last year (88%).
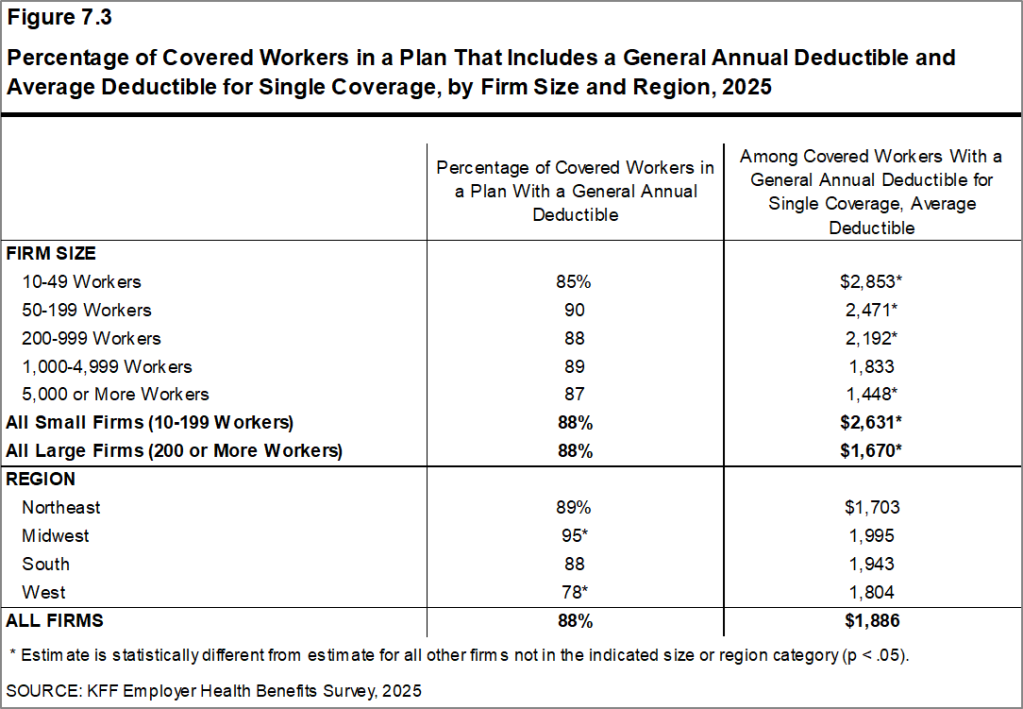
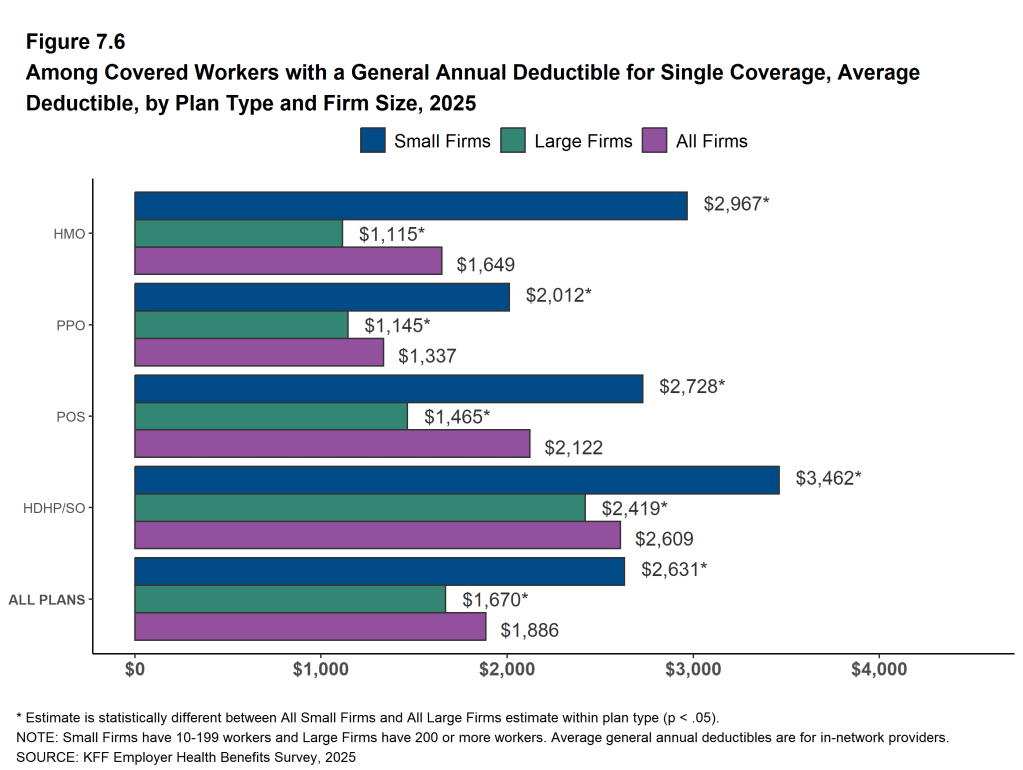
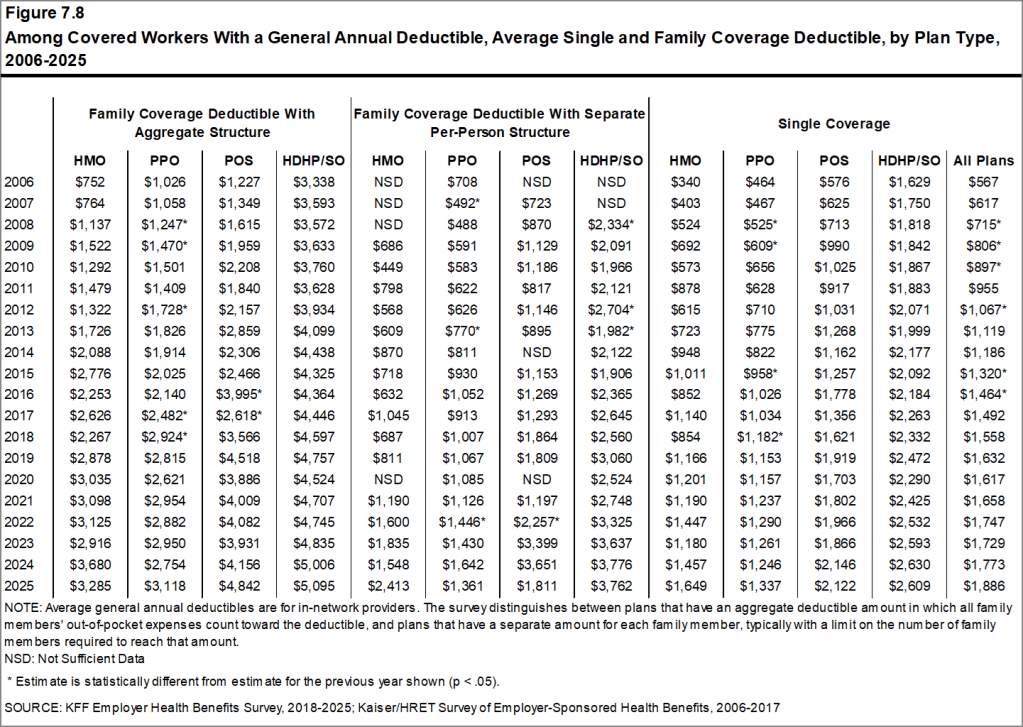
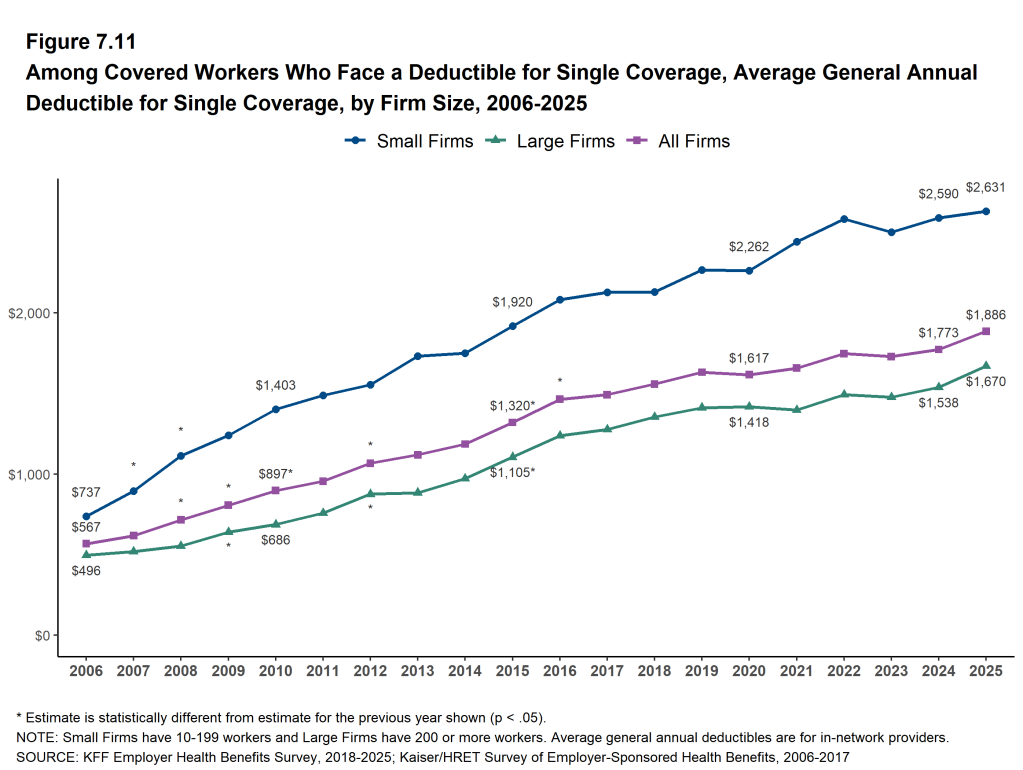
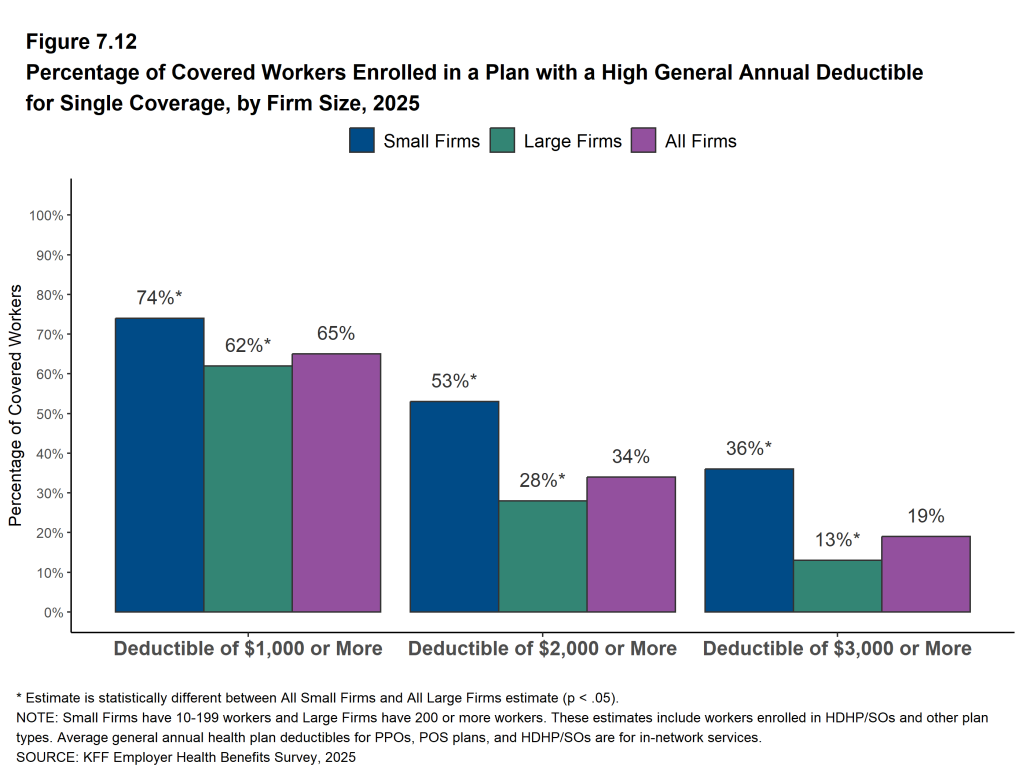
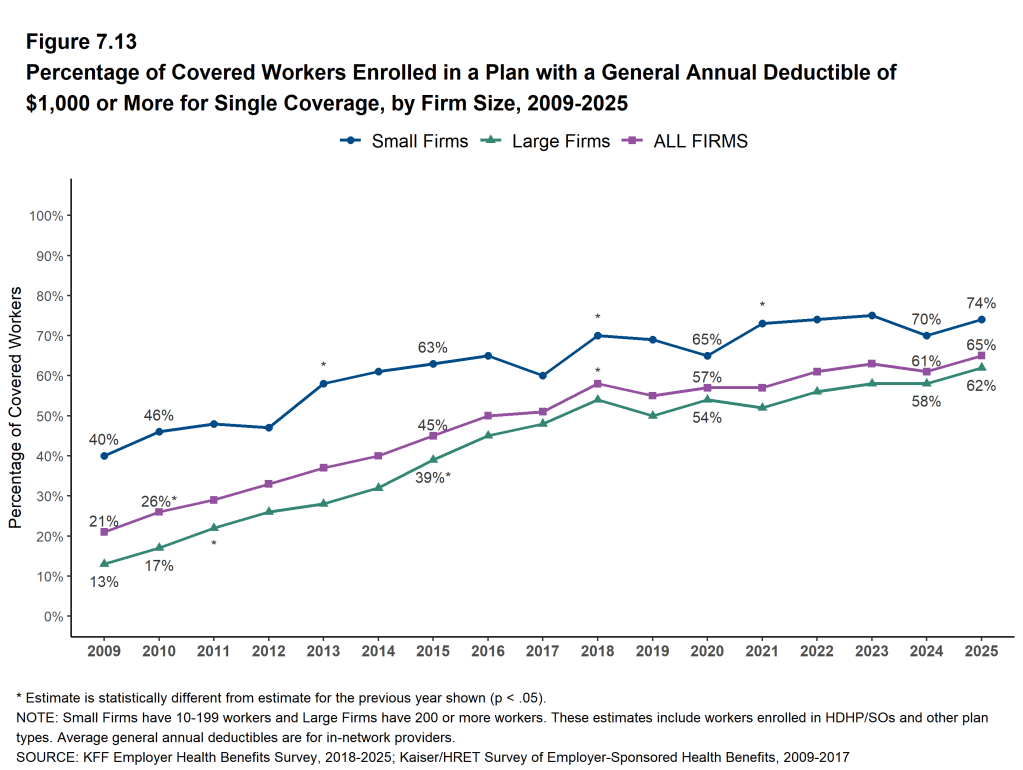
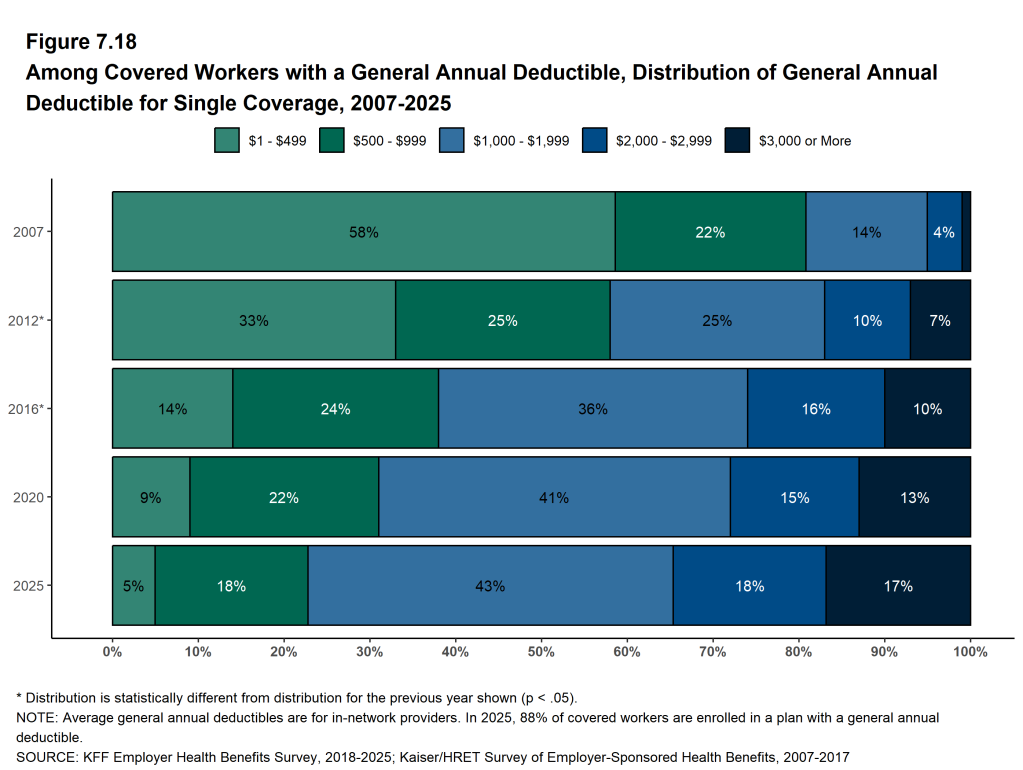
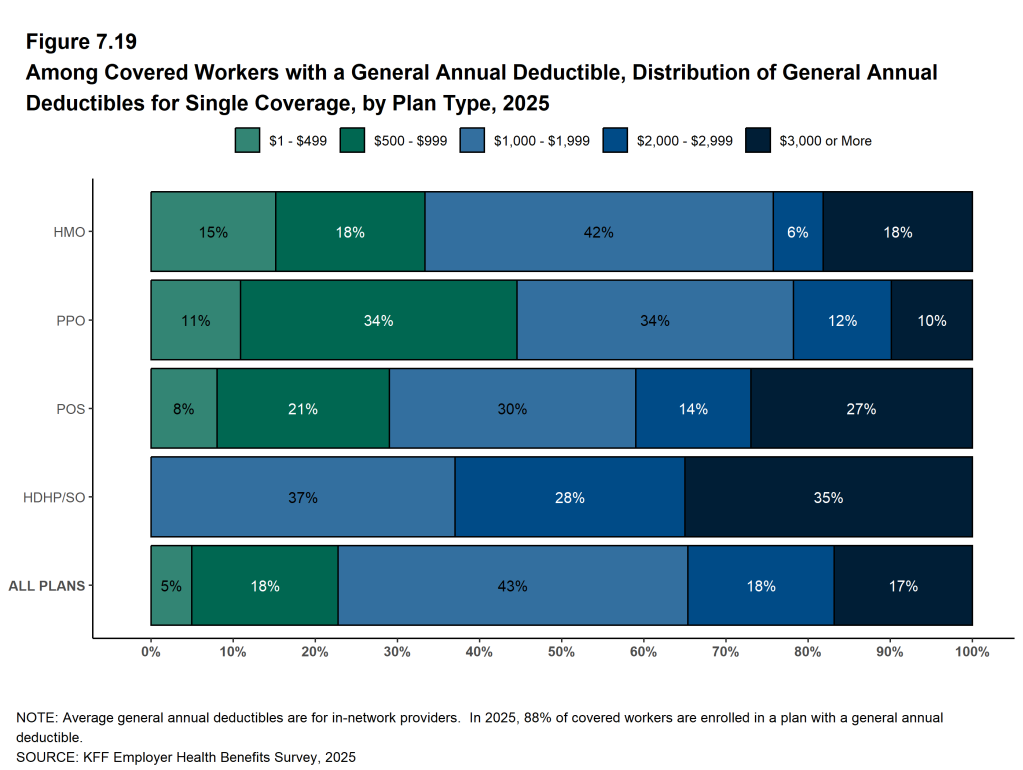
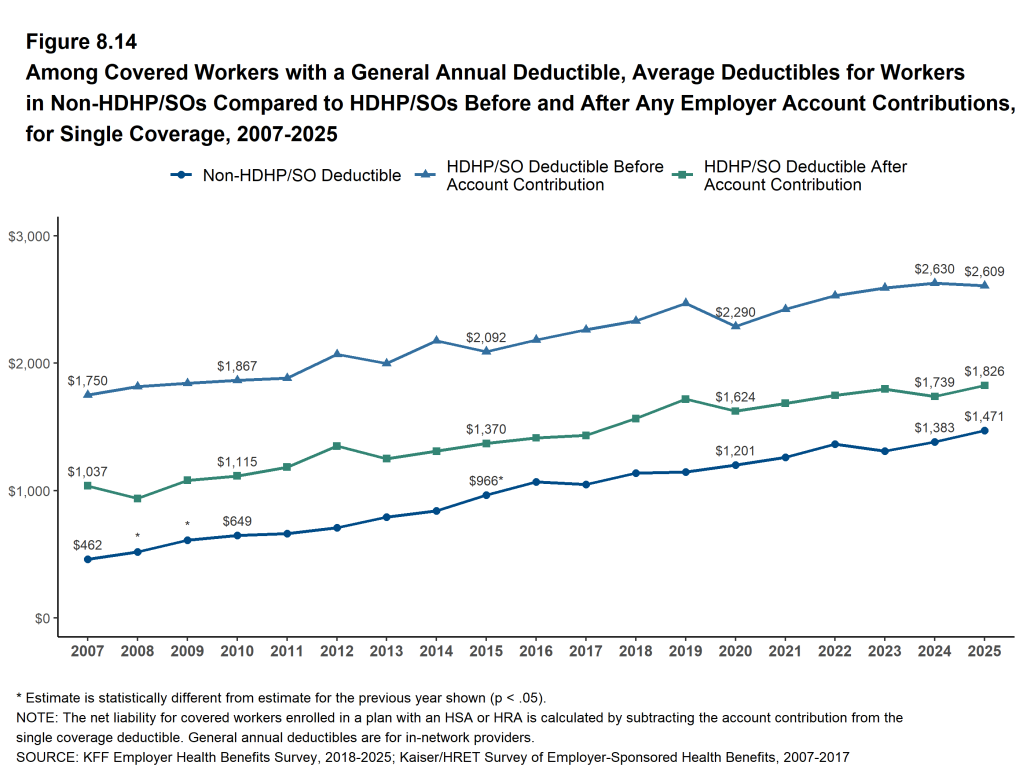
The average deductible amount in 2025 for workers with single coverage and a general annual deductible is $1,886, similar to last year. The average deductible for covered workers at firms with 10 to 199 workers ($2,631) is higher than the average deductible at larger firms ($1,670). For covered workers with an annual deductible, the average deductible for single coverage has increased 17% over the last five years and 43% over the last 10 years.
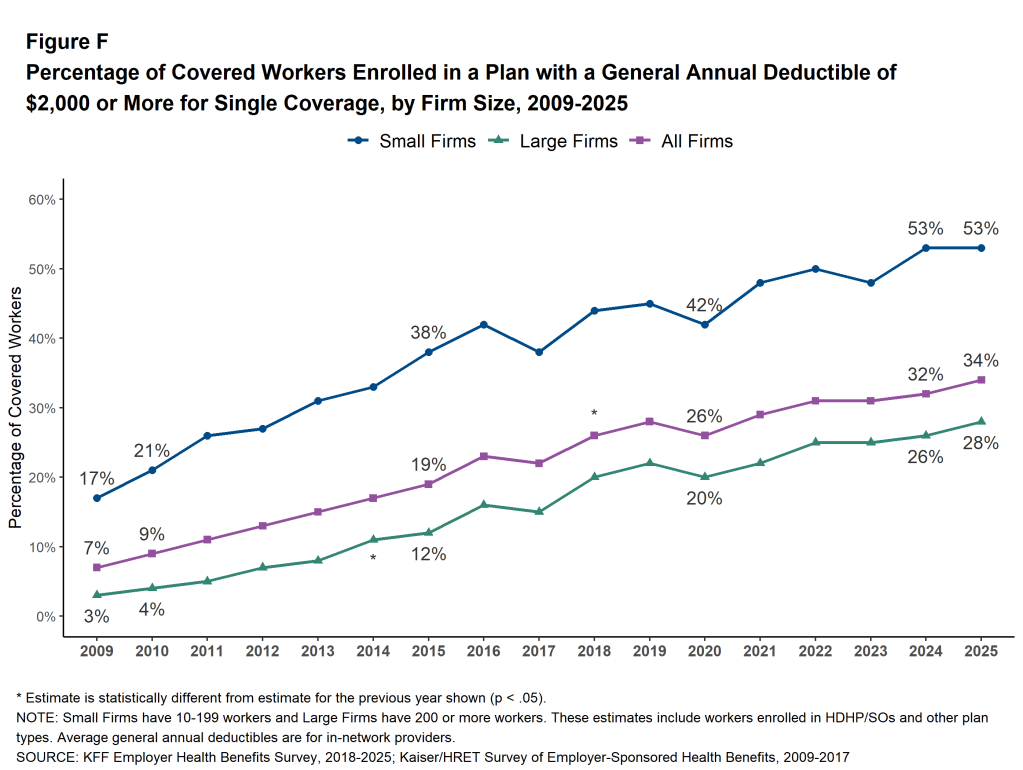
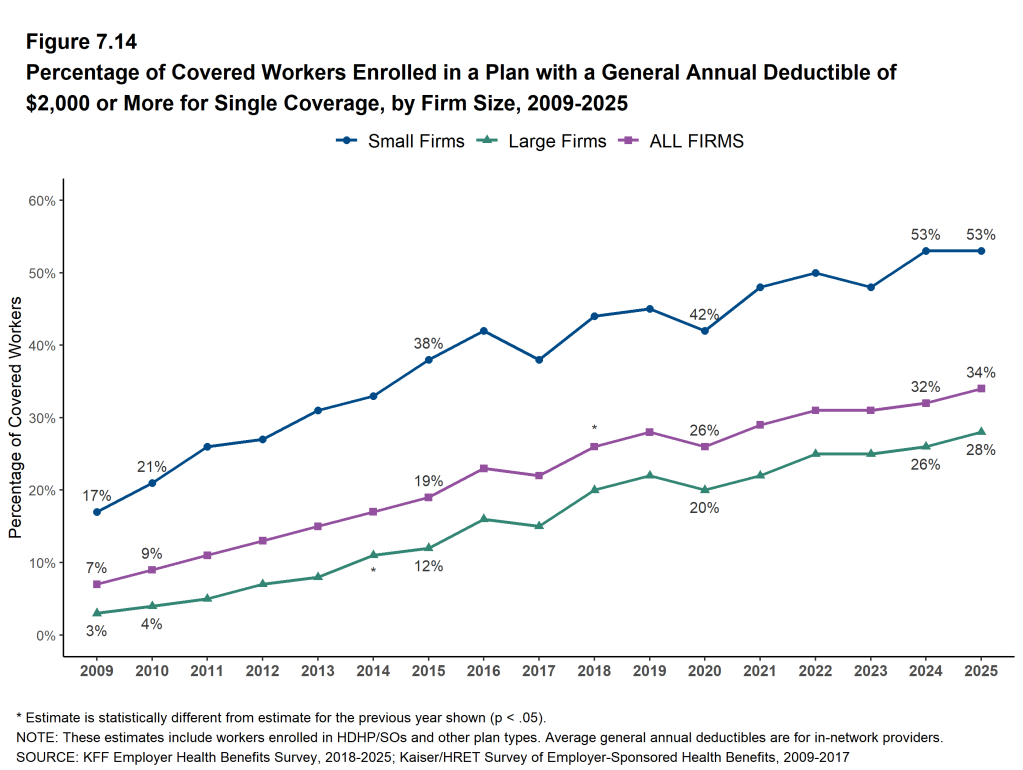
Thirty-four percent of covered workers in 2025 are in a plan with a general annual deductible of $2,000 or more for single coverage, similar to the percentage (32%) last year. Over half (53%) of covered workers in firms with 10 to 199 workers are in such a plan, compared with 28% of covered workers in larger firms. The share of covered workers in a plan with a general annual deductible of $2,000 or more for single coverage has increased 32% over the last five years and 77% over the last ten years [Figure F].
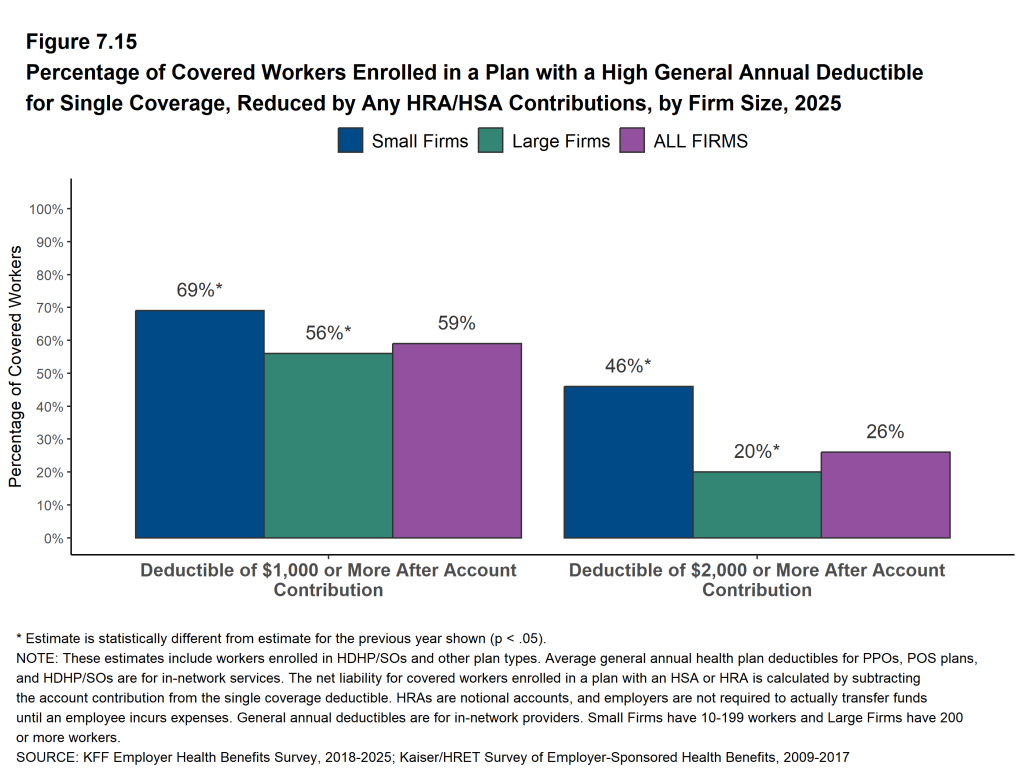
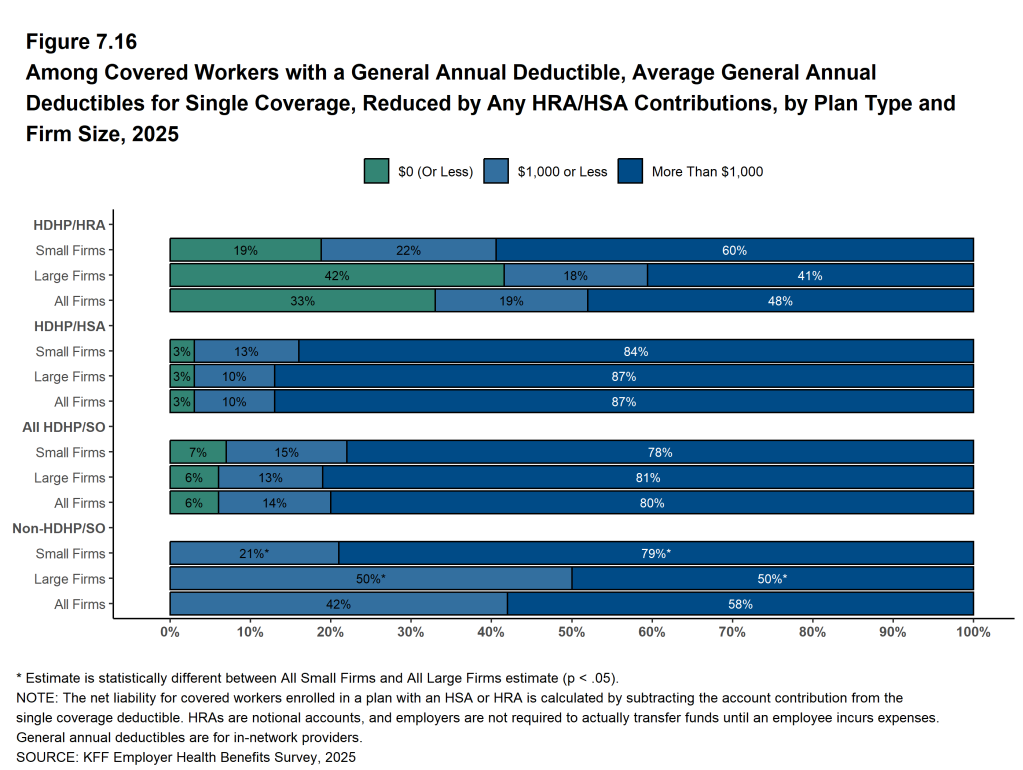
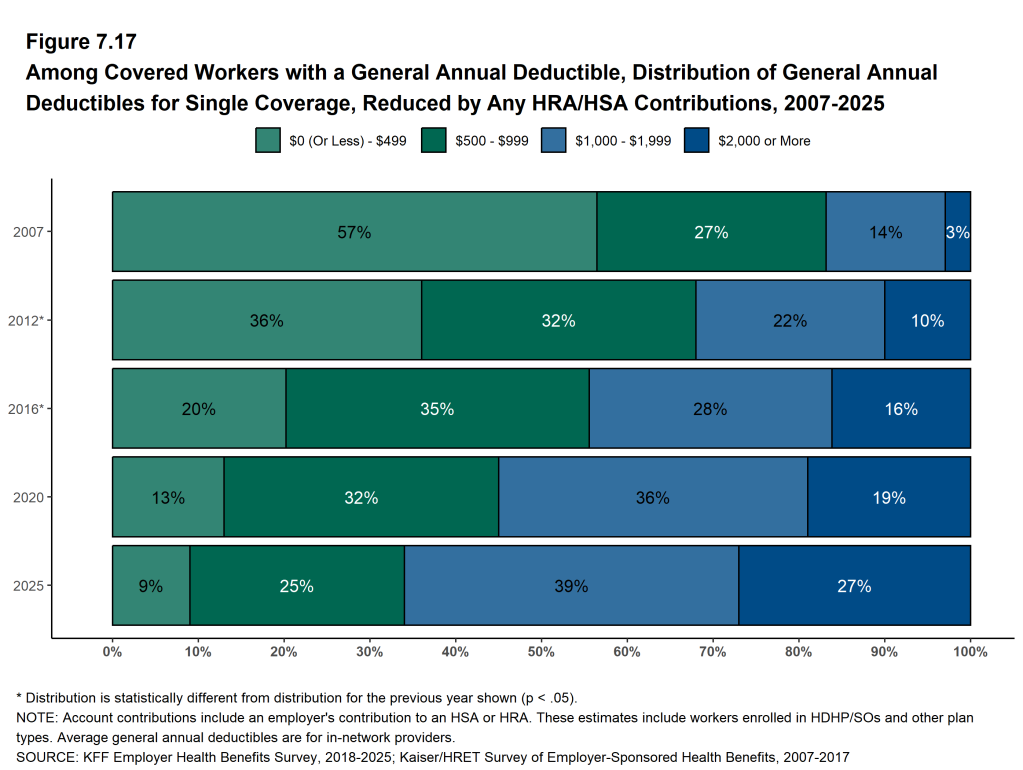
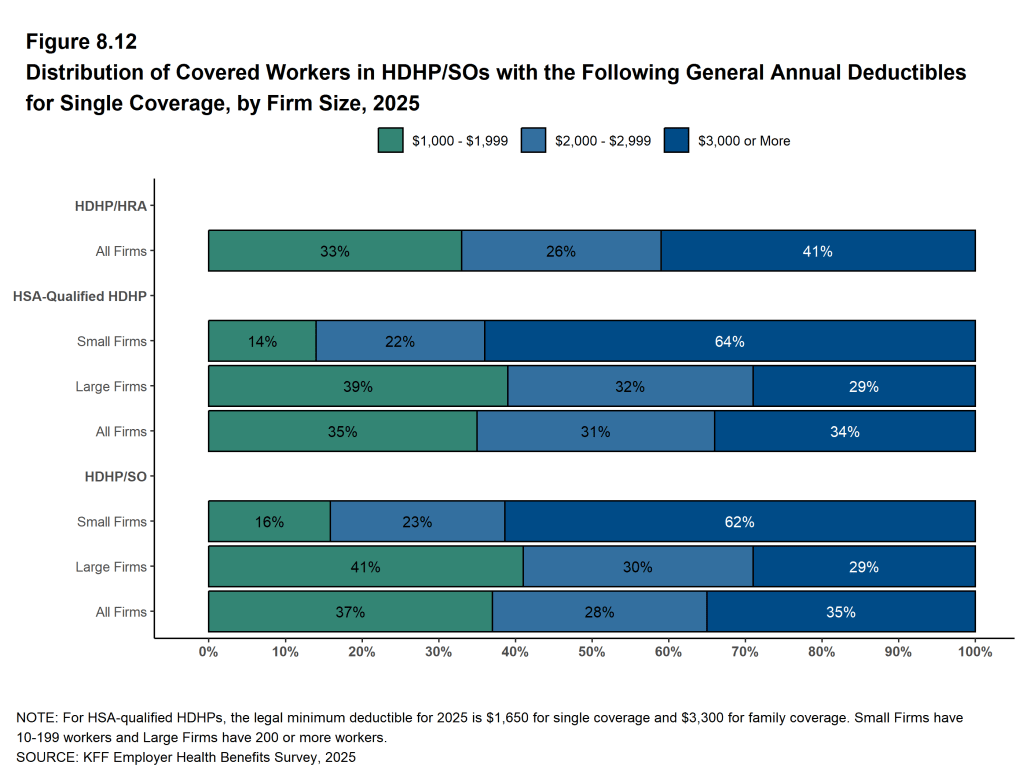
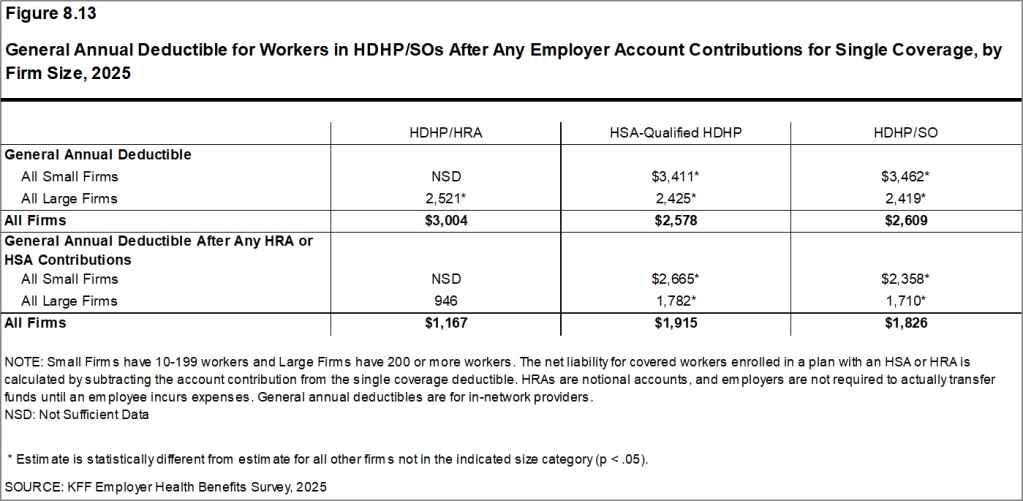
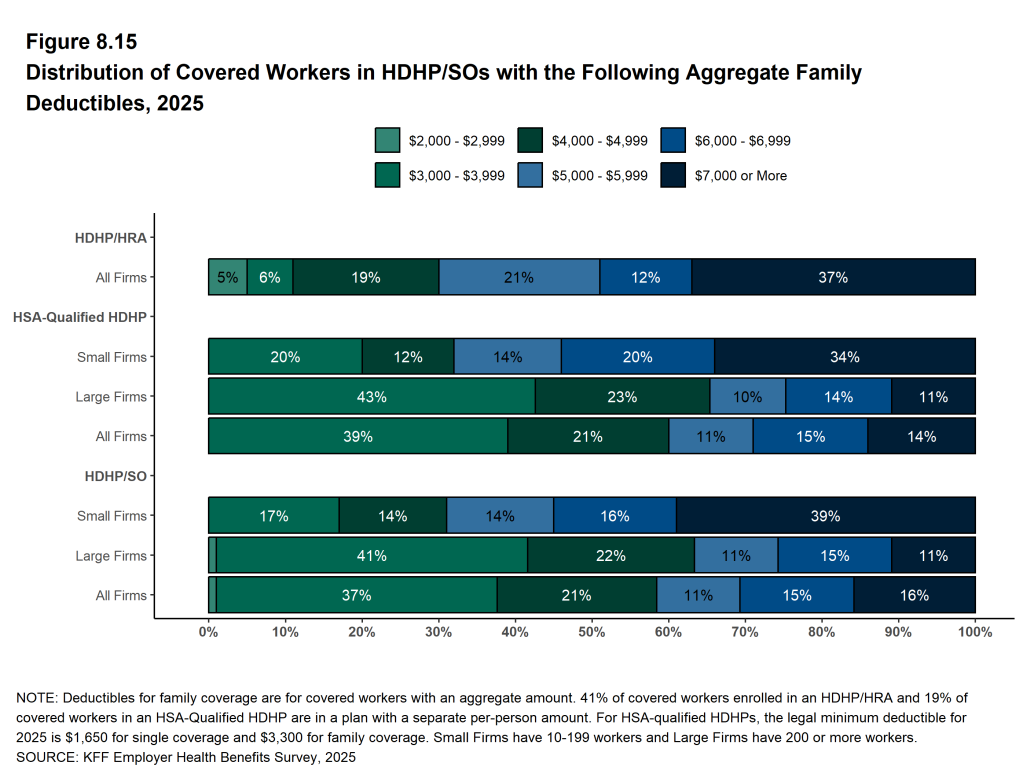
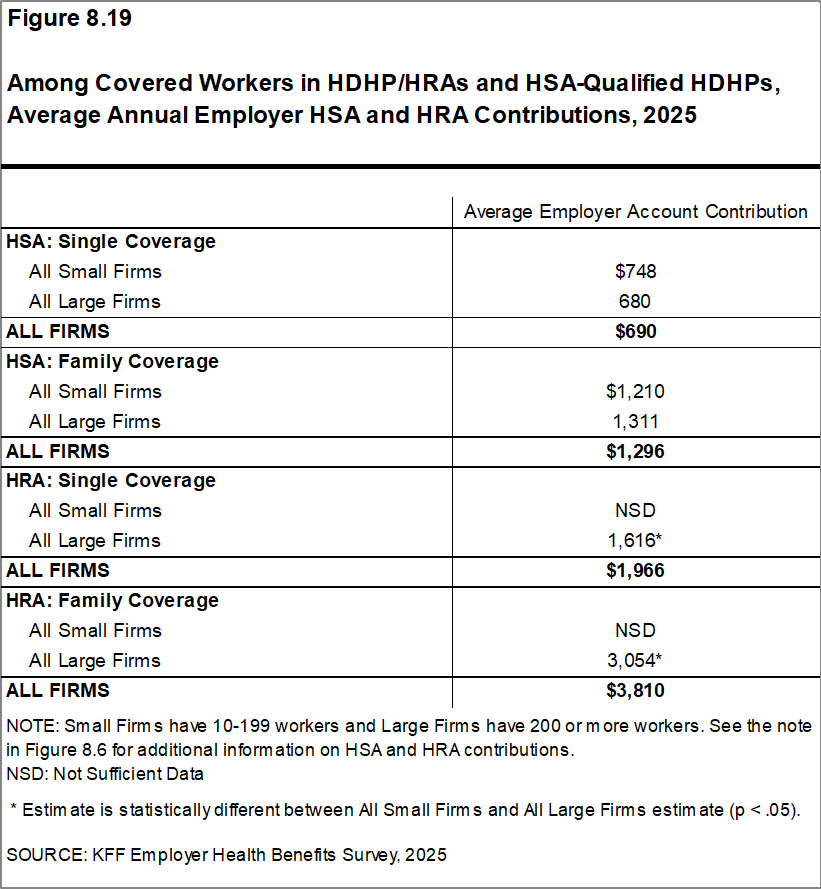
Some workers in health plans with high deductibles also receive contributions to savings accounts from their employers. These contributions can be used to reduce cost sharing amounts. Thirty-three percent of covered workers in an HDHP with a Health Reimbursement Arrangement (HRA), and 3% of covered workers in a Health Savings Account (HSA)-qualified HDHP receive an account contribution for single coverage that is greater than or equal to their deductible amount. Additionally, 19% of covered workers in an HDHP with an HRA and 10% of covered workers in an HSA-qualified HDHP receive account contributions that, if applied to their deductible, would reduce their personal annual liability to less than $1,000.
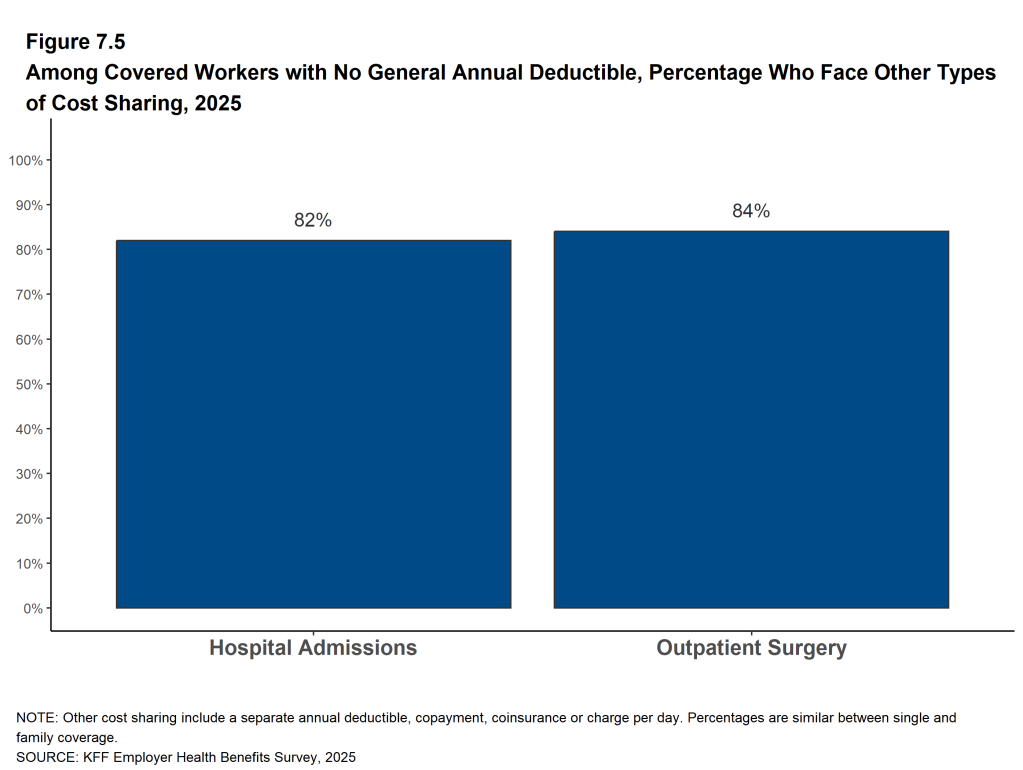
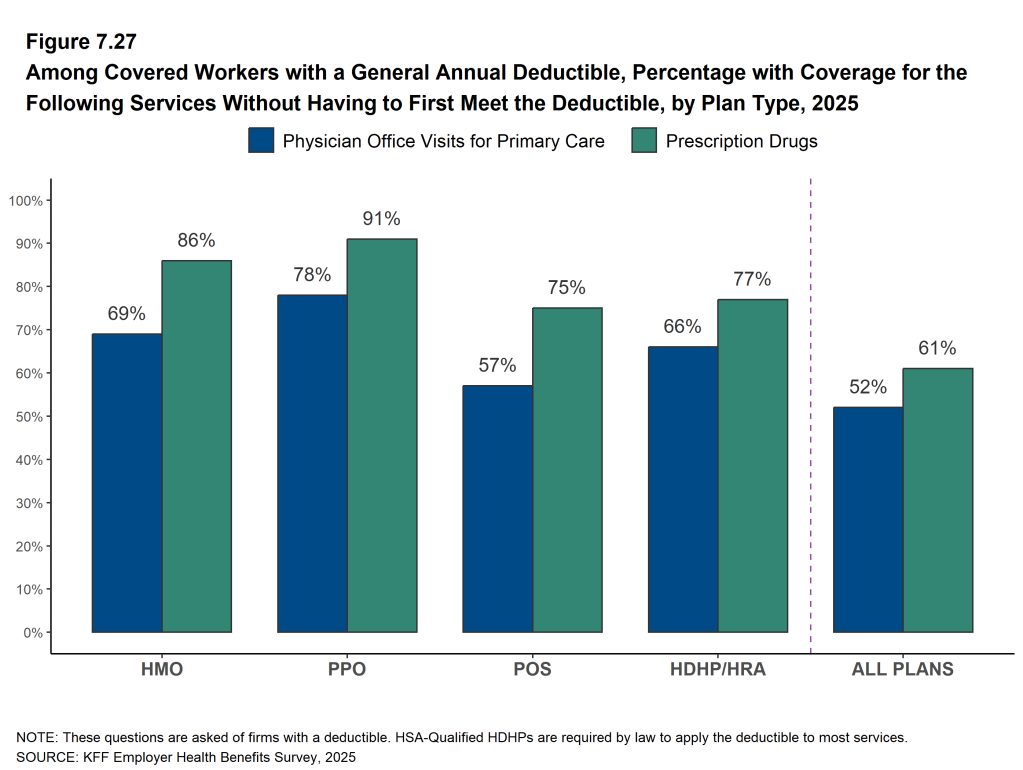
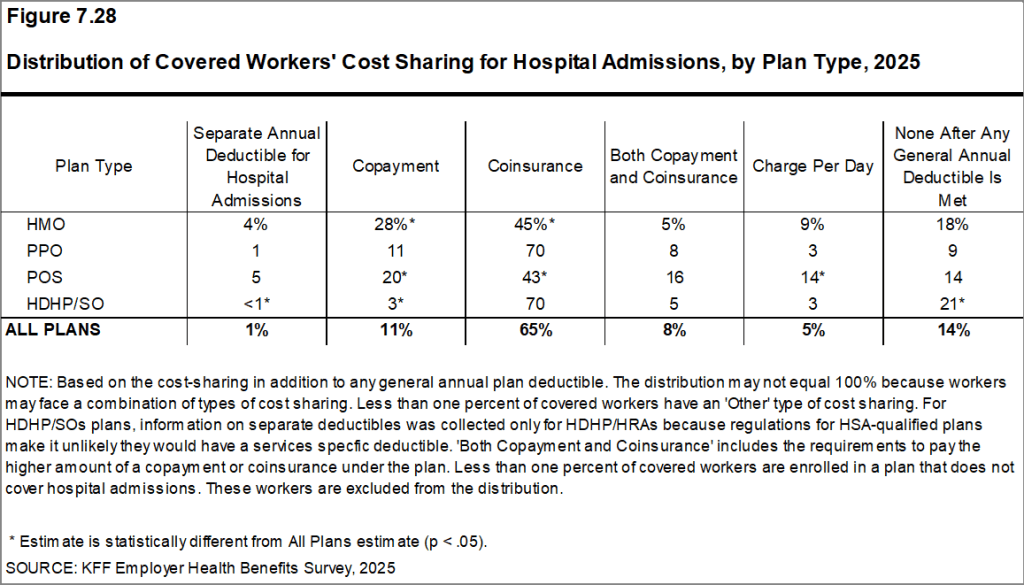
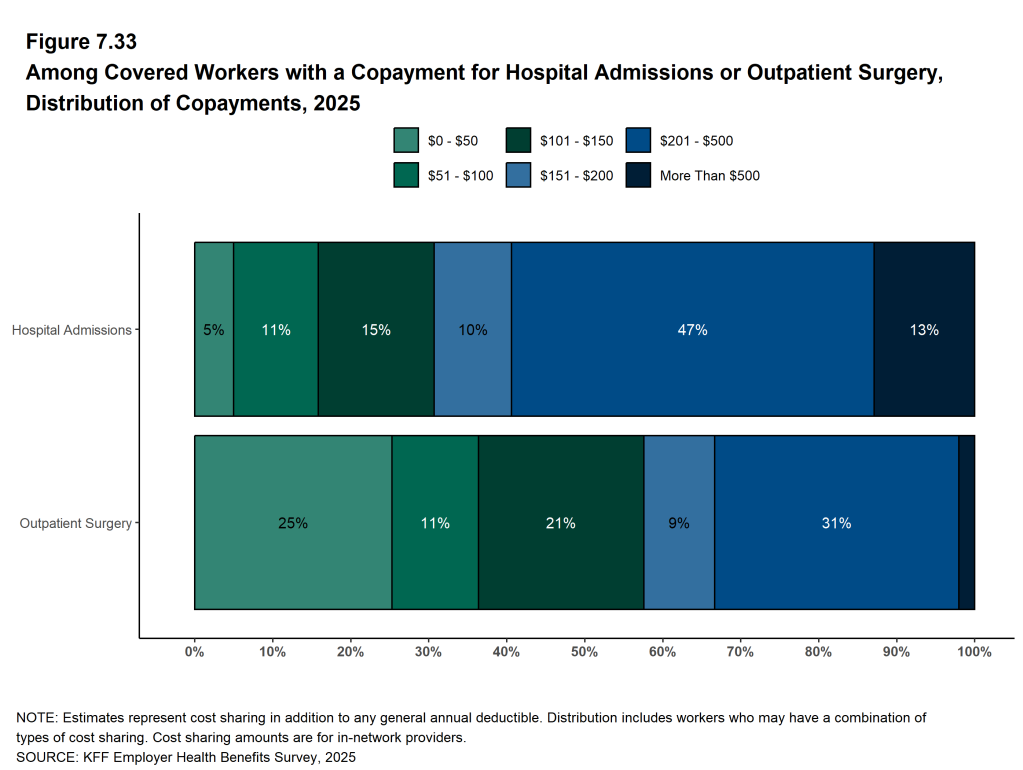
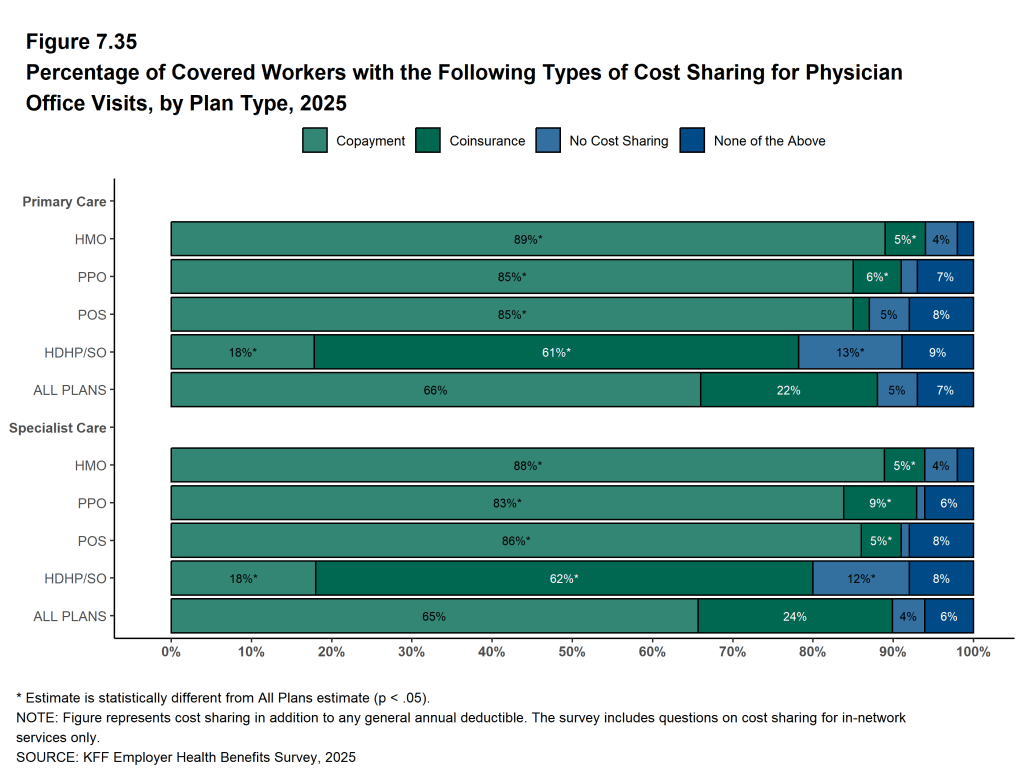
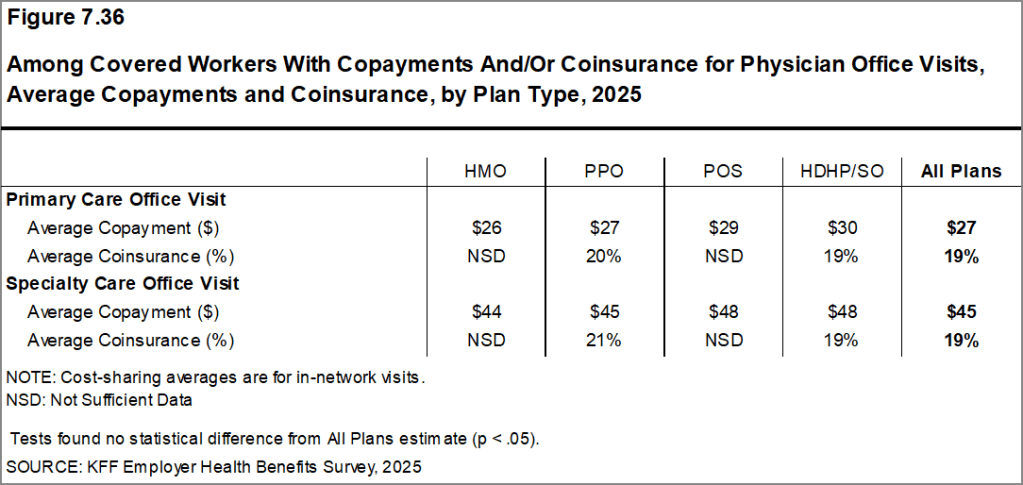
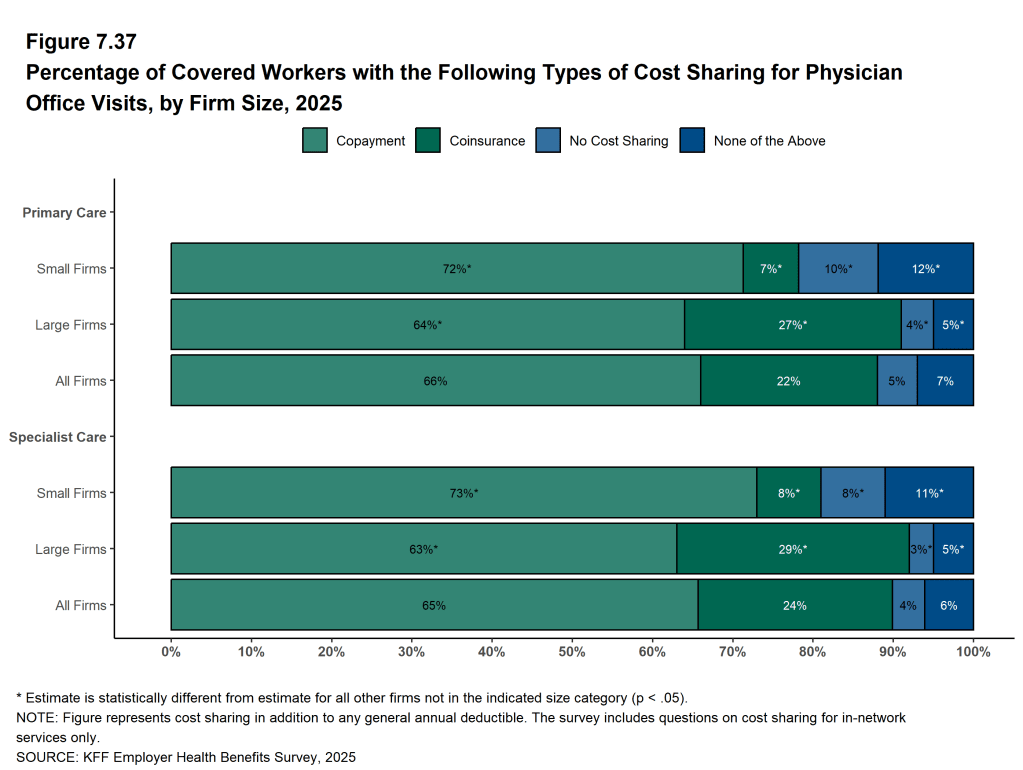
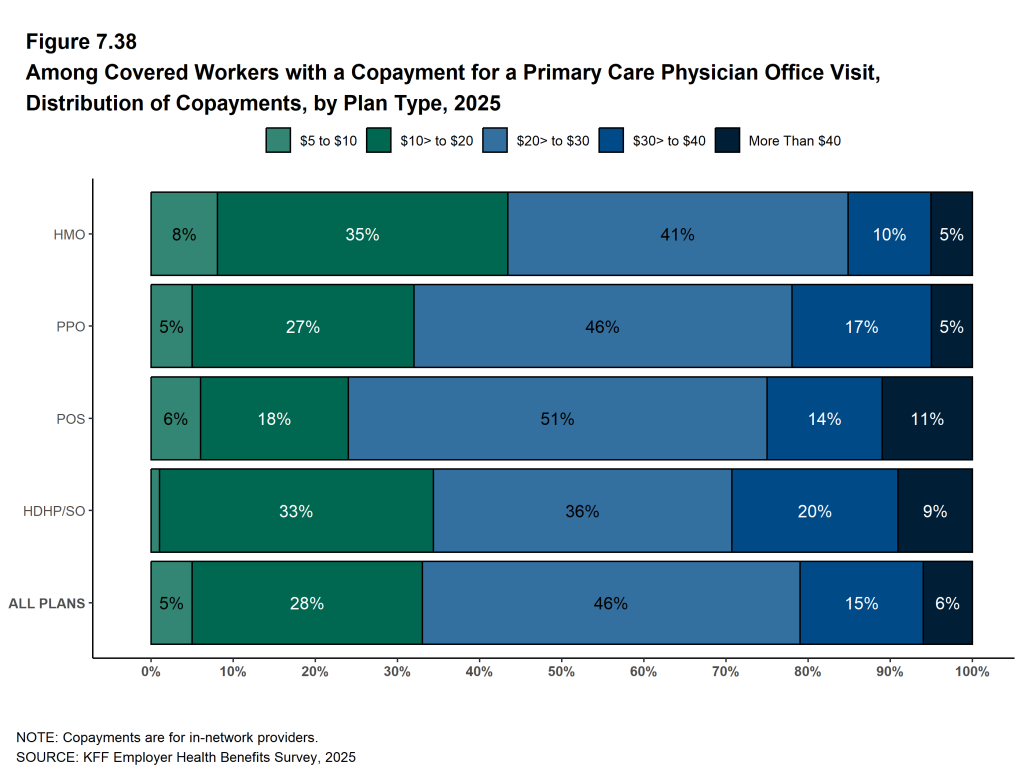
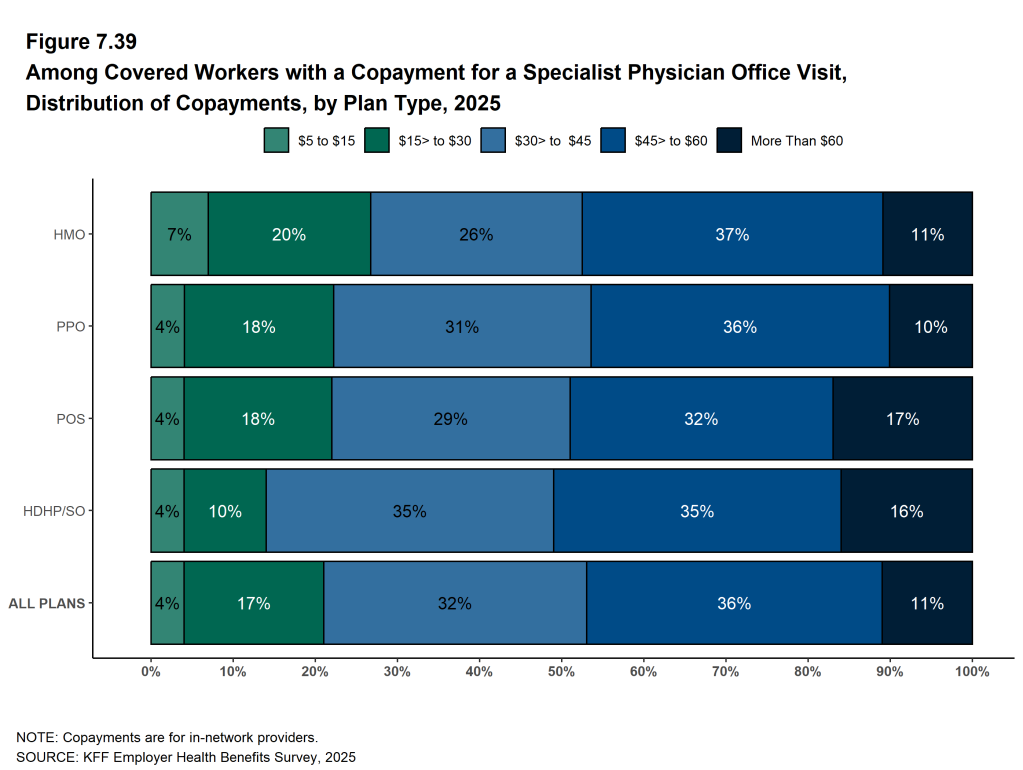
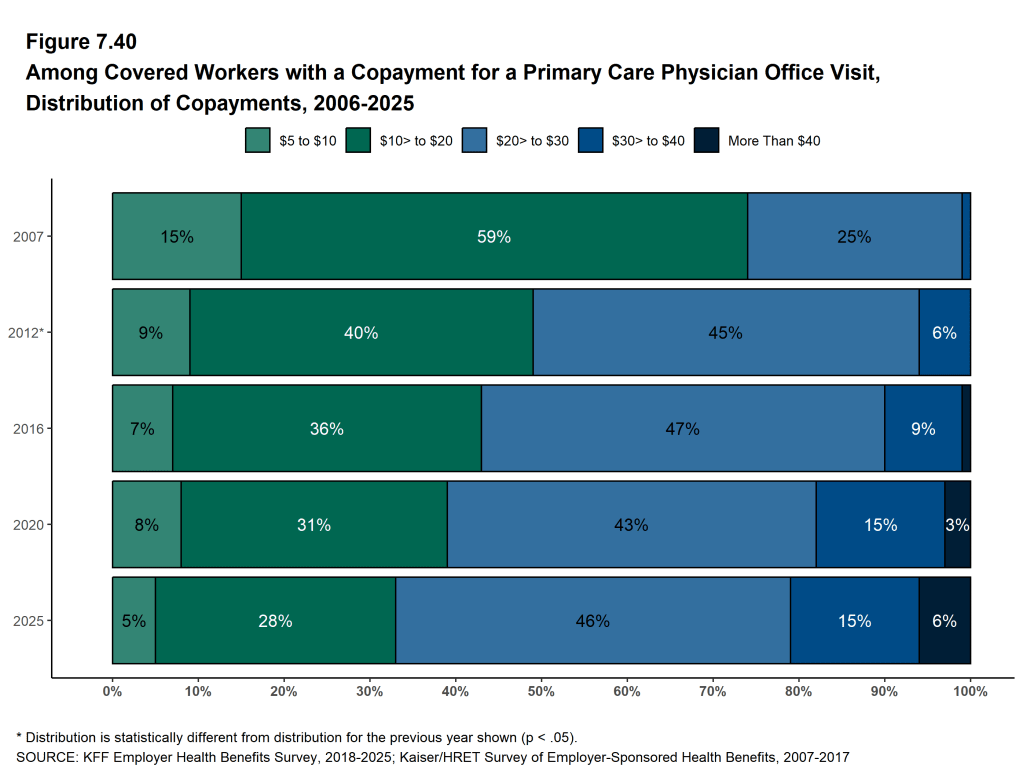
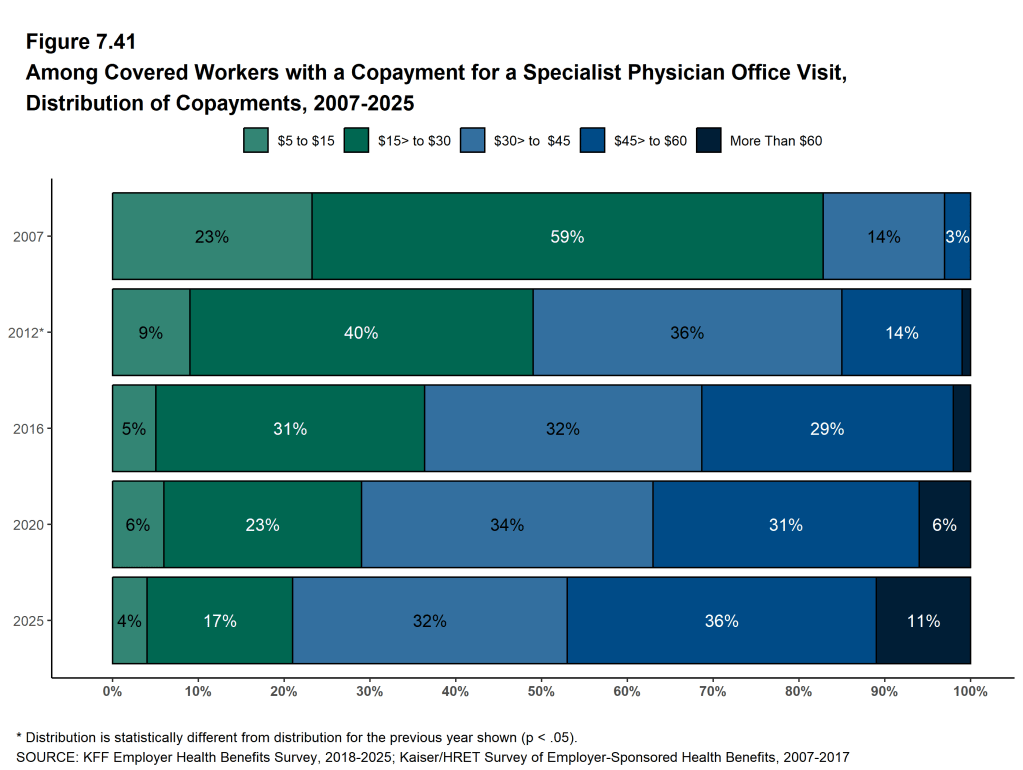
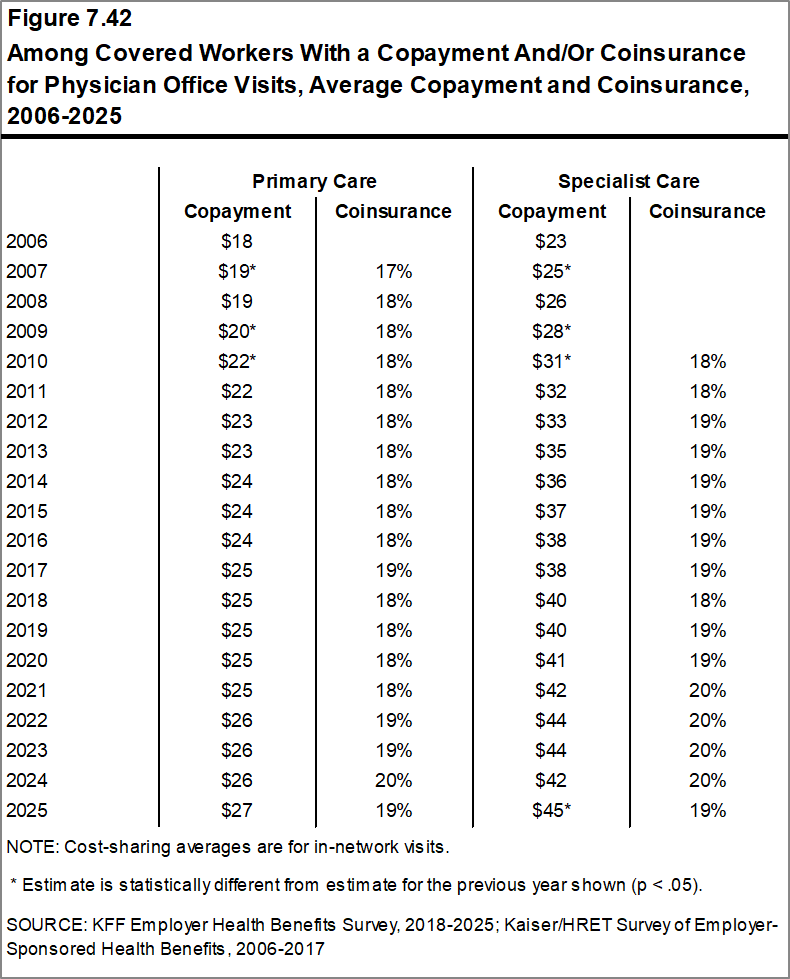
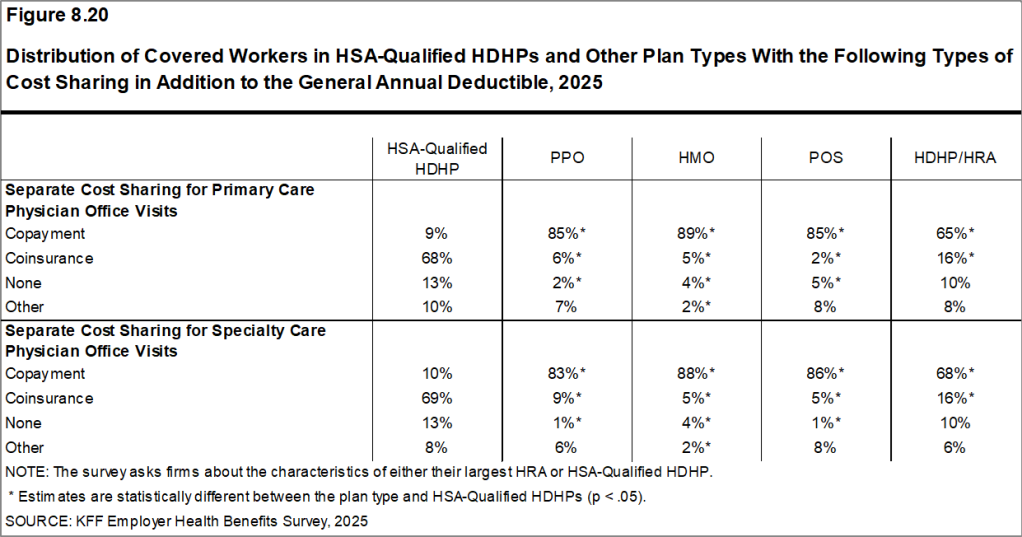
In addition to any general annual deductible they may have, most covered workers also pay a portion of the cost of care when they use health care services, typically a copayment (a fixed dollar amount) or coinsurance (a percentage of the covered amount). For physician office visits, the average copayment for a primary care visit is $27, similar to the amount last year, and the average copayment for a visit to a specialist is $45, higher than the amount last year. The average coinsurance rate is 19% for both primary care and specialist visits, similar to the percentages last year.
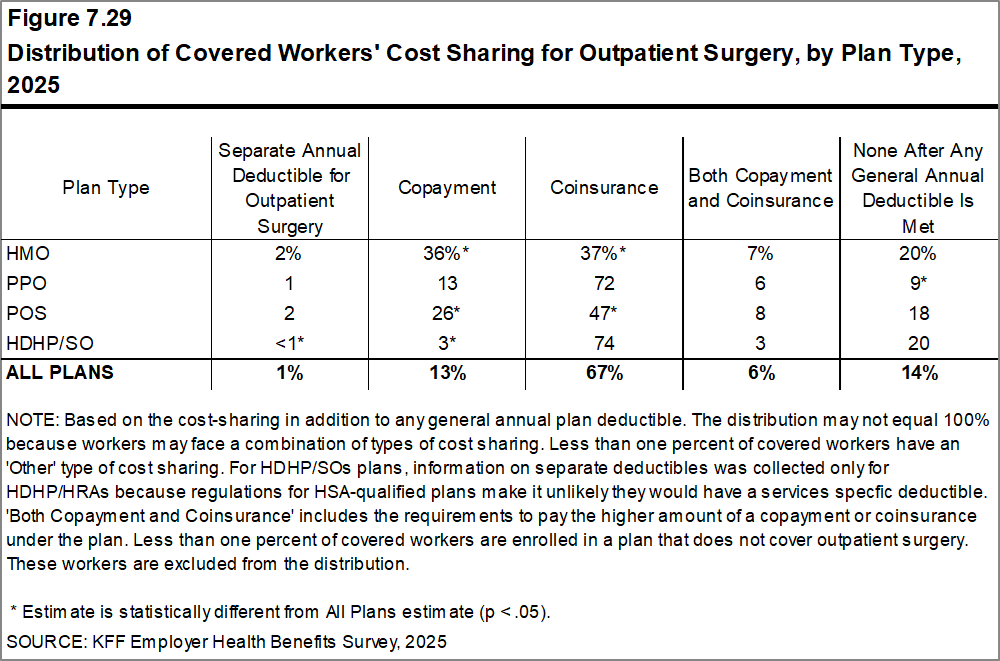
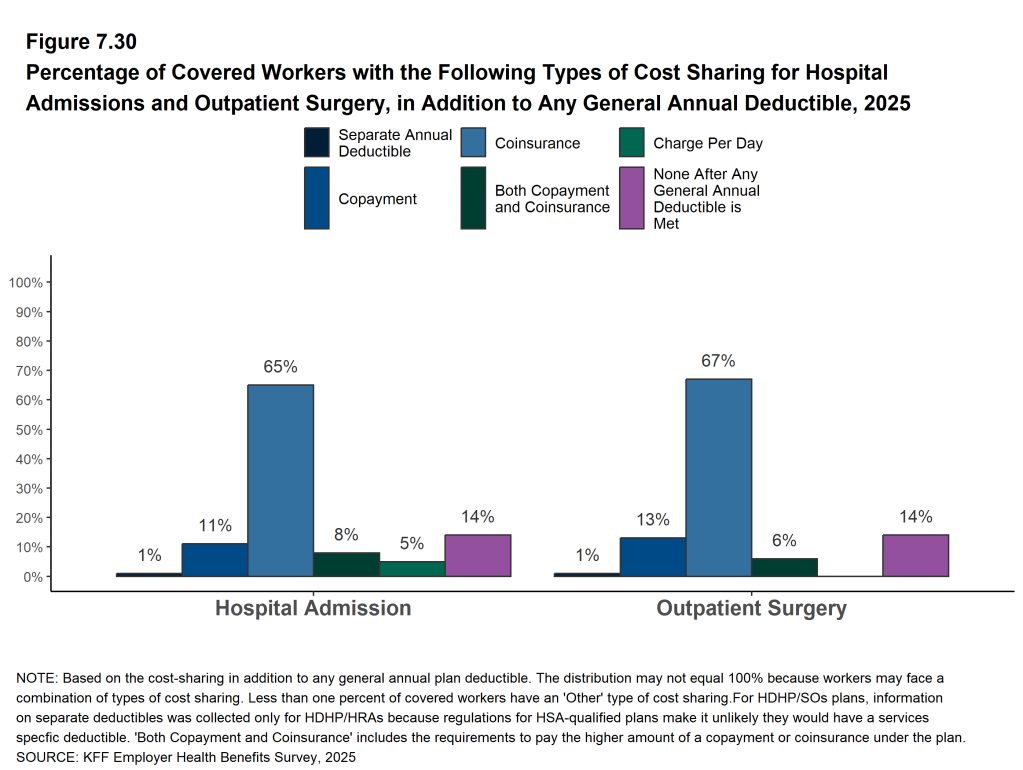
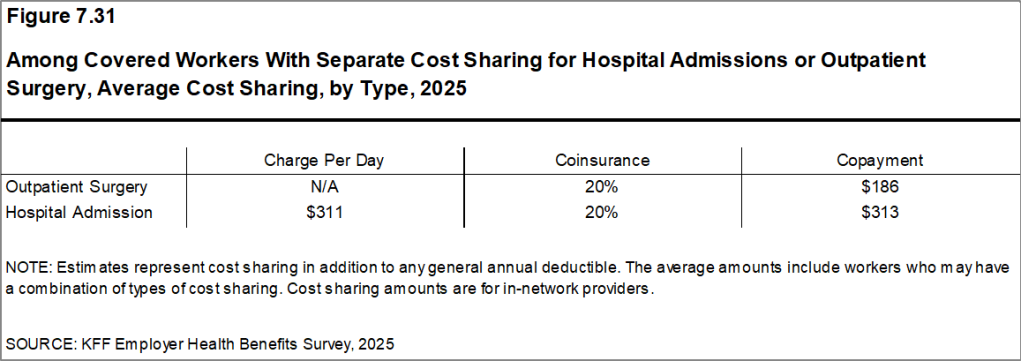
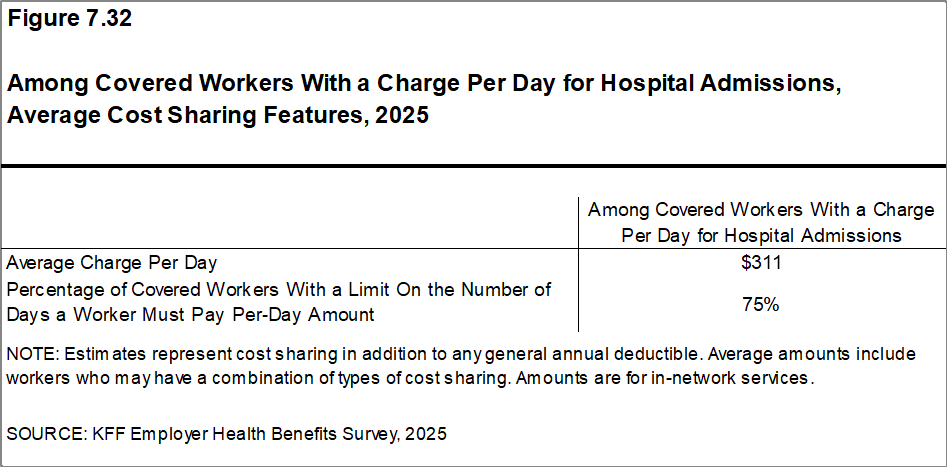
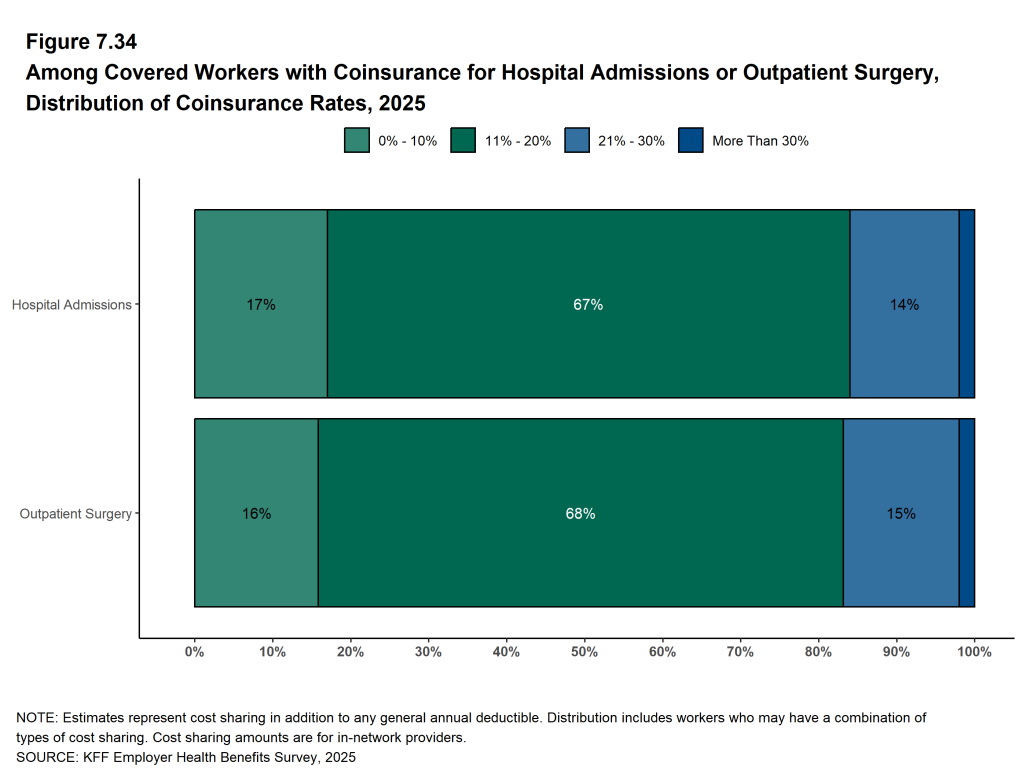
When admitted to the hospital, 65% of covered workers have coinsurance requirements, 11% have a copayment, and 8% have both a copayment and coinsurance requirement. The average coinsurance rate for a hospital admission is 20% and the average copayment amount is $313. The cost sharing requirements for outpatient surgery follow a similar pattern to those for hospital admissions, although the average copayment amount for outpatient surgery is lower ($186).
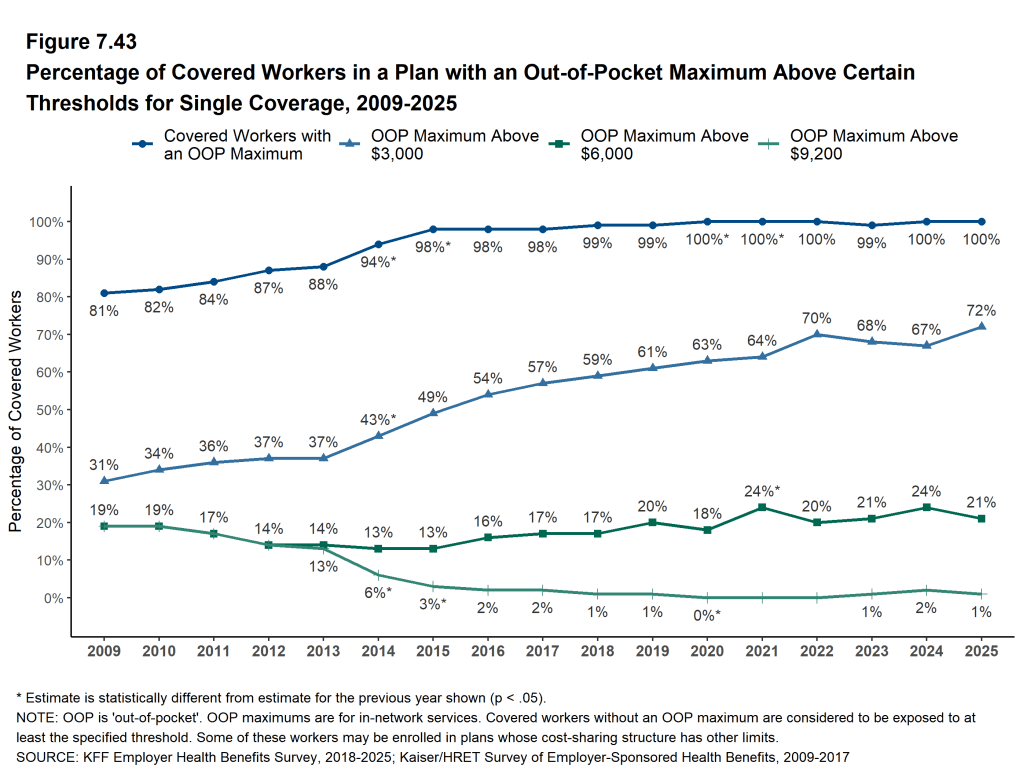
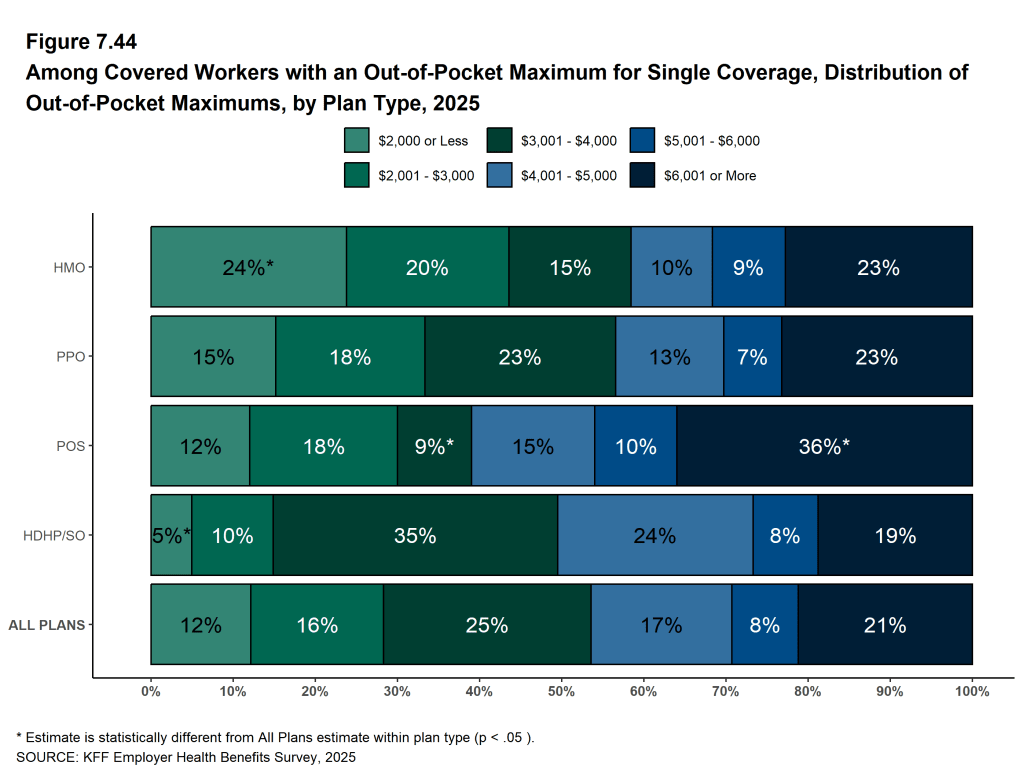
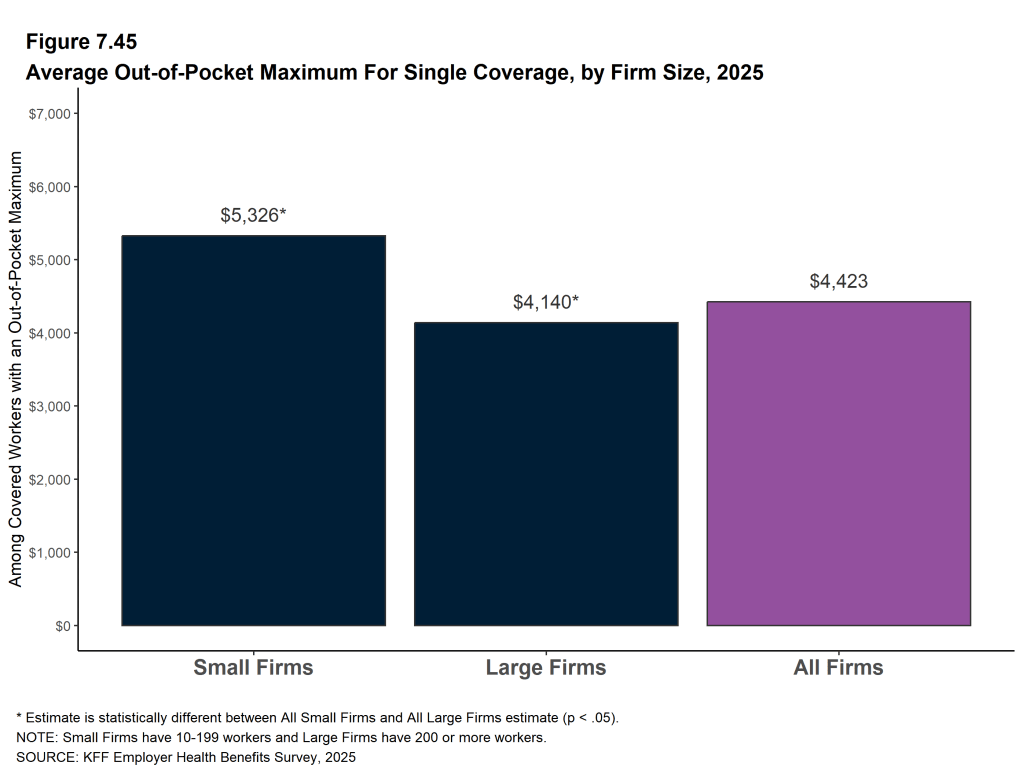
Virtually all covered workers are in plans with an annual limit on in-network cost sharing (called an out-of-pocket maximum) for single coverage, although these limits vary significantly. Among covered workers in plans with an out-of-pocket maximum for single coverage, 12% are in a plan with an out-of-pocket limit of $2,000 or less, while 21% are in a plan with a limit above $6,000.
Figure F: Percentage of Covered Workers Enrolled in a Plan With a General Annual Deductible of $2,000 or More for Single Coverage, by Firm Size, 2009-2025
AVAILABILITY OF EMPLOYER-SPONSORED COVERAGE
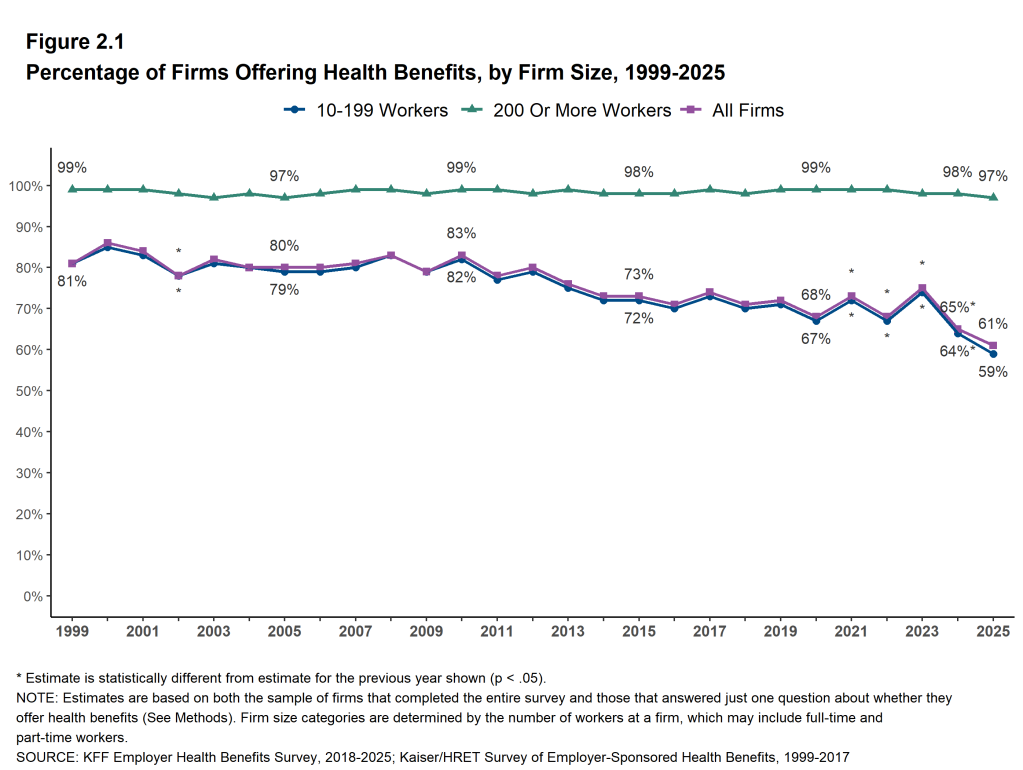
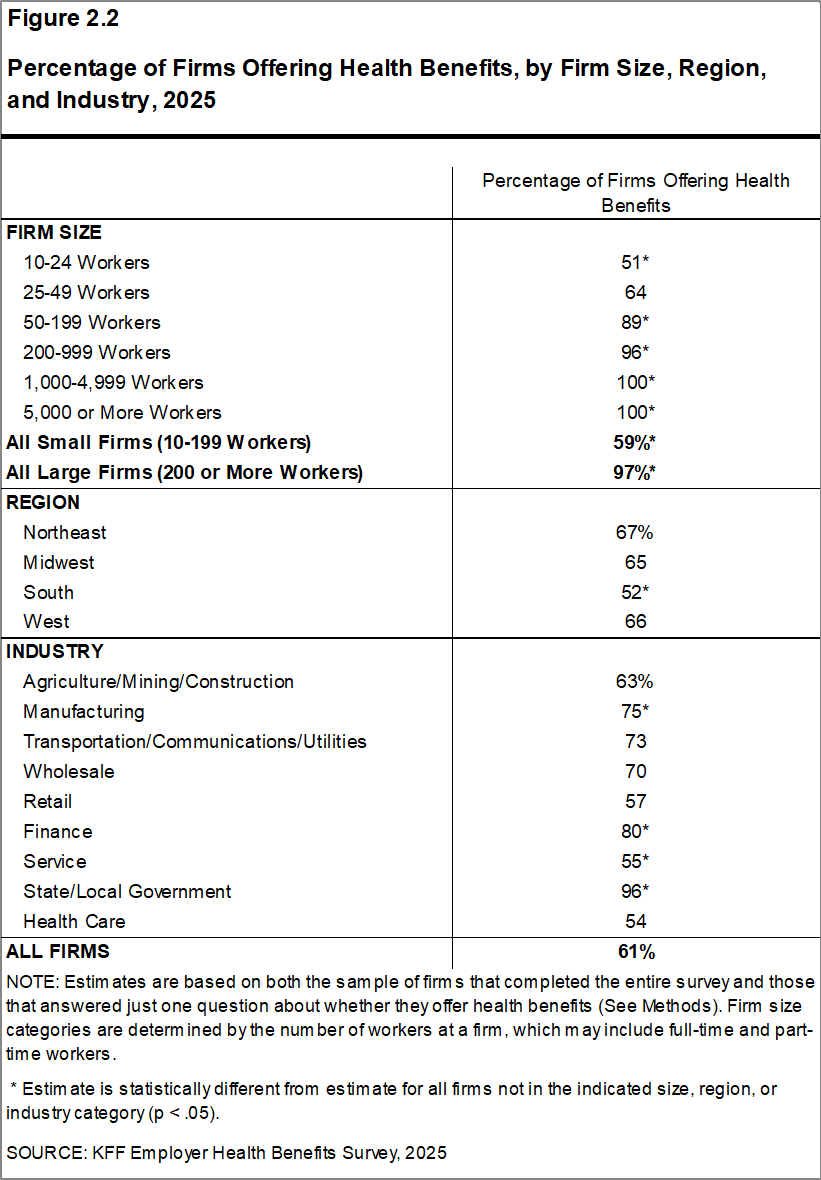
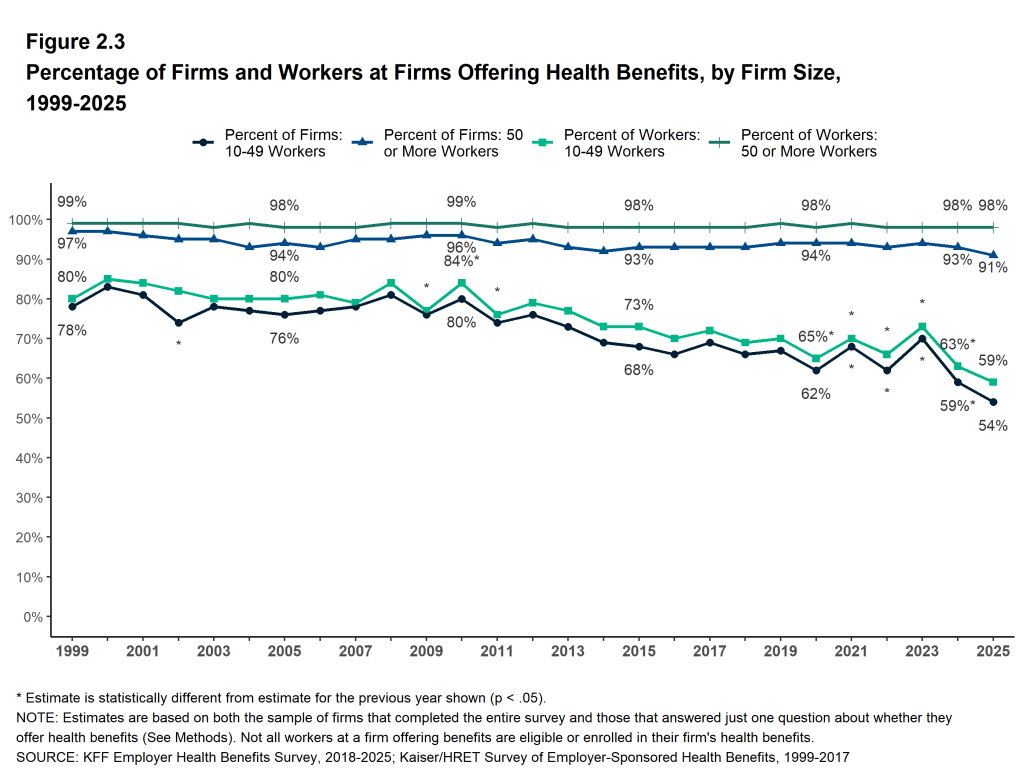
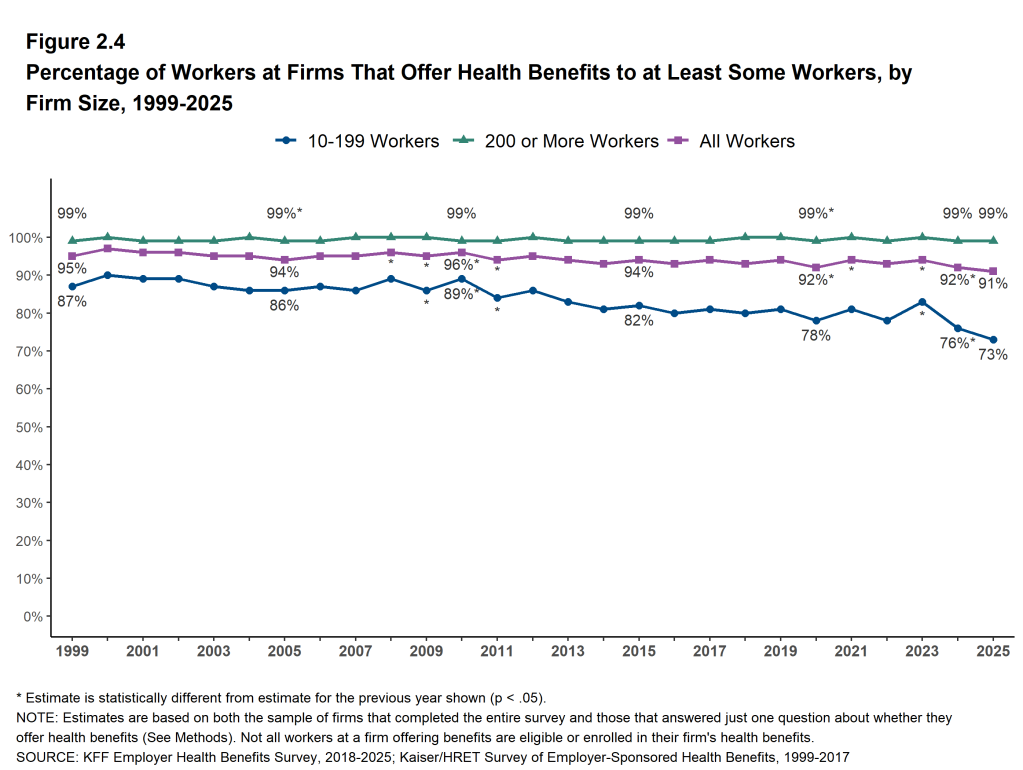
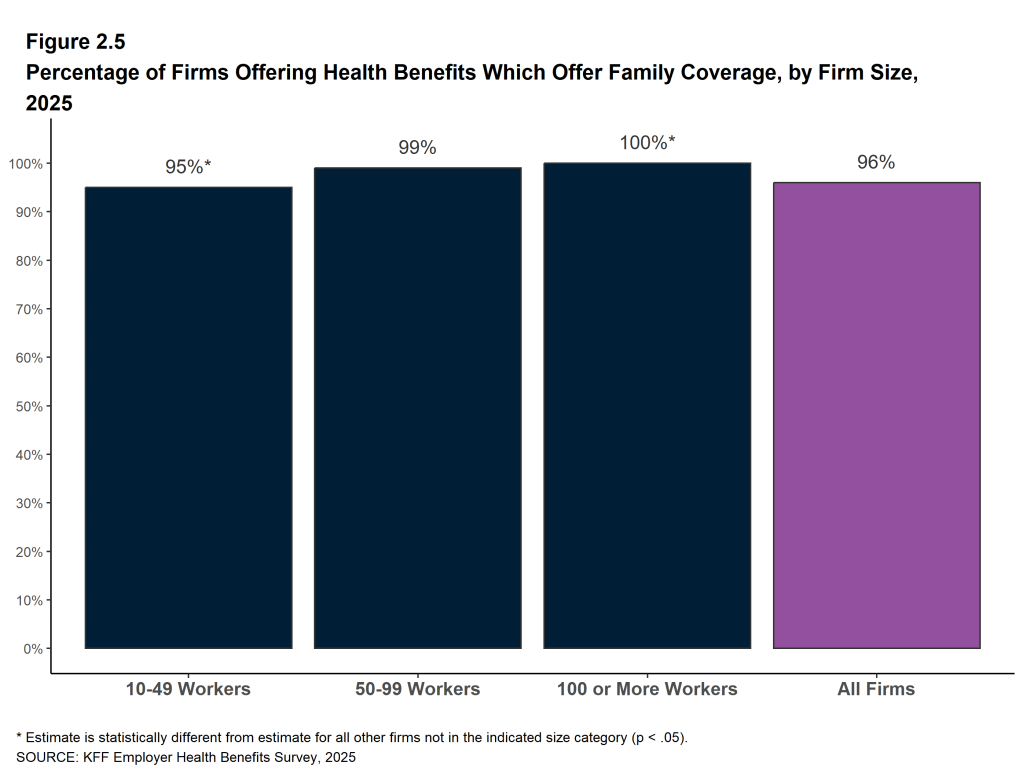
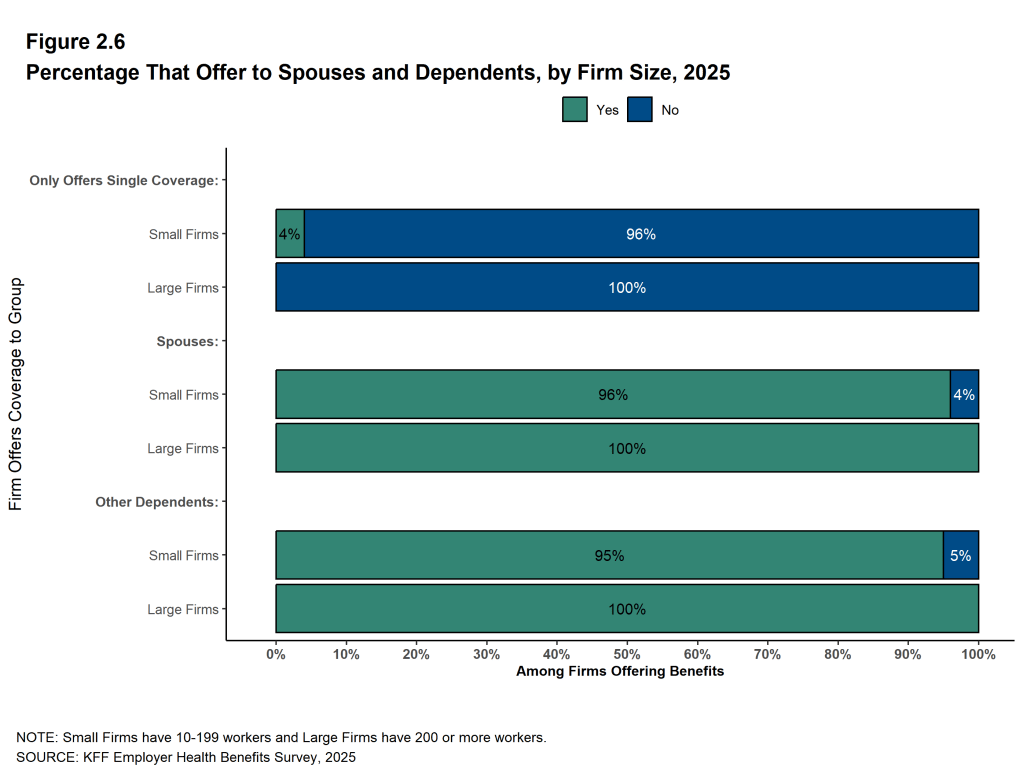
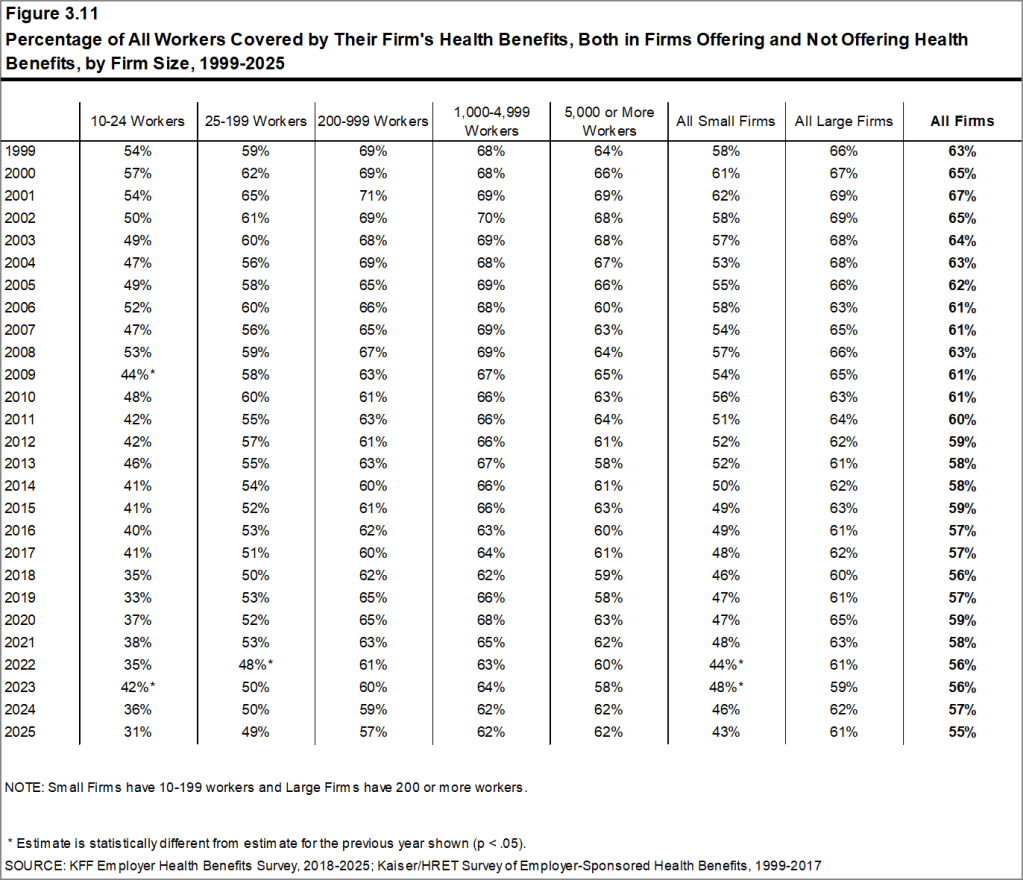
Sixty-one percent of firms with 10 or more workers offer health benefits to at least some of their workers, similar to the percentage last year (65%). As explained in the Methods, the 2025 survey sample was limited to firms with 10 or more employees, resulting in a higher overall offer rate than previously published estimates. Firms with 200 or more workers are much more likely than smaller firms to offer health benefits (97% vs. 59%).
Because most firms are small, the overall offer rate can fluctuate over time, as estimates for smaller firms tend to vary considerably from year to year. Most workers, however, work for larger firms, where offer rates are higher and much more stable. Among firms with 200 or more workers, 96% of firms with 200 to 999 workers, and over 99% of firms with 1,000 or more workers, offer health benefits to at least some of their workers. Overall, 91% of workers are employed by a firm that offers health benefits to at least some of its workers. This percentage is similar to the percentages five years ago (92%).
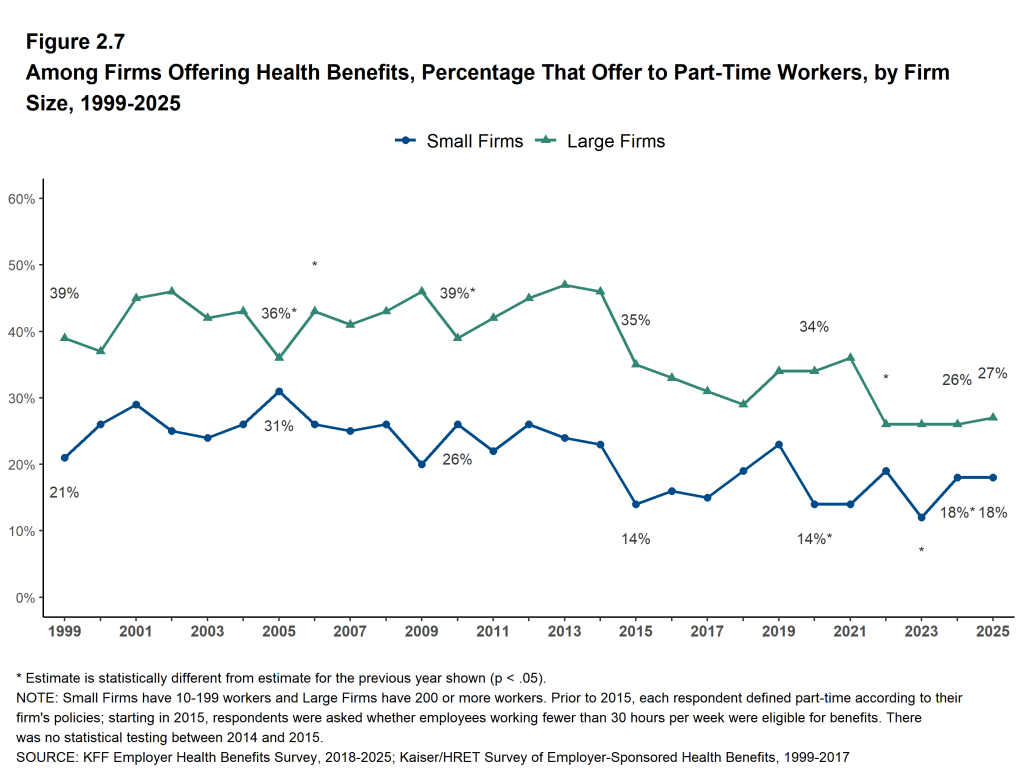
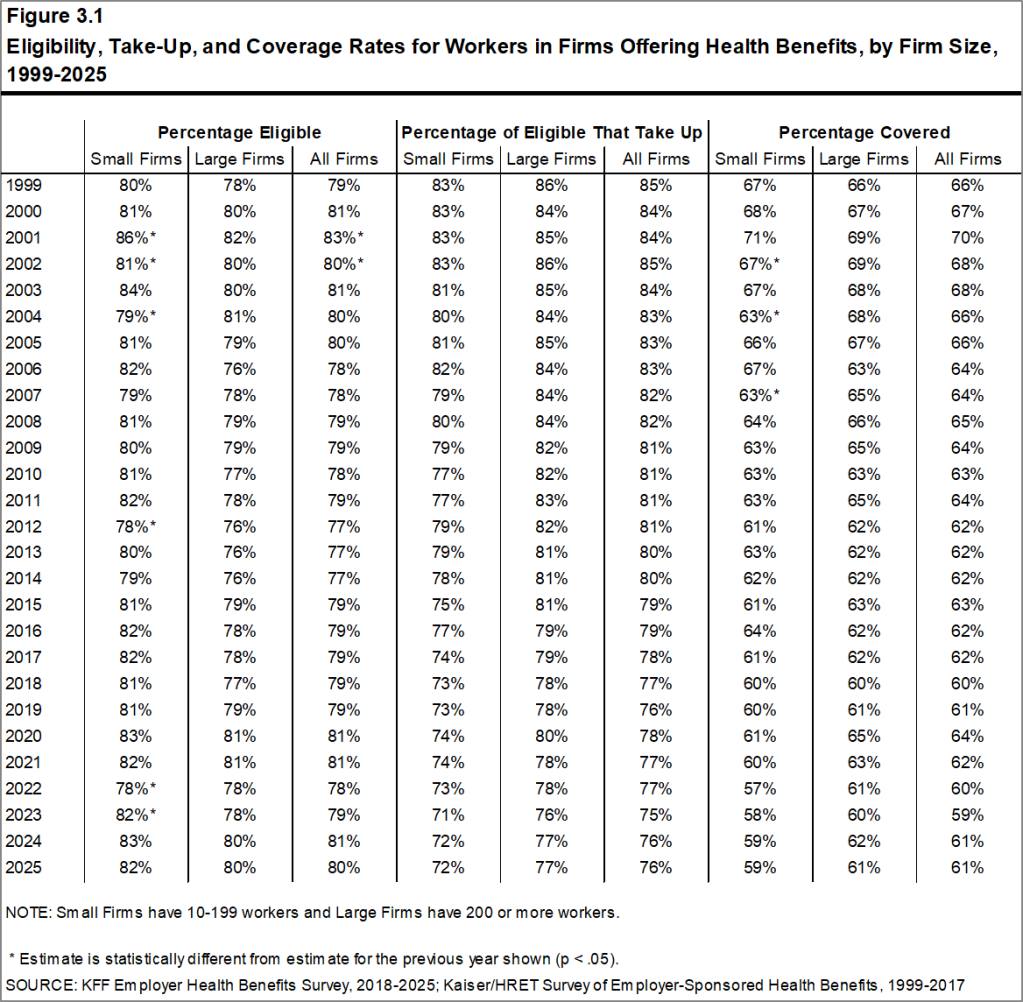
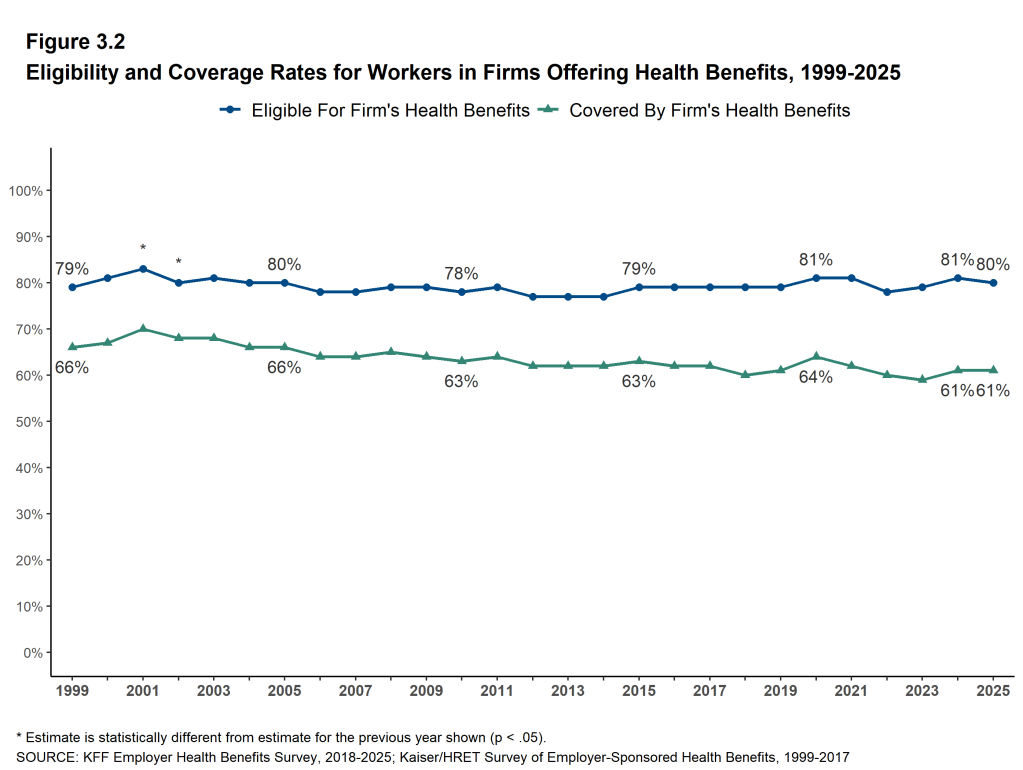
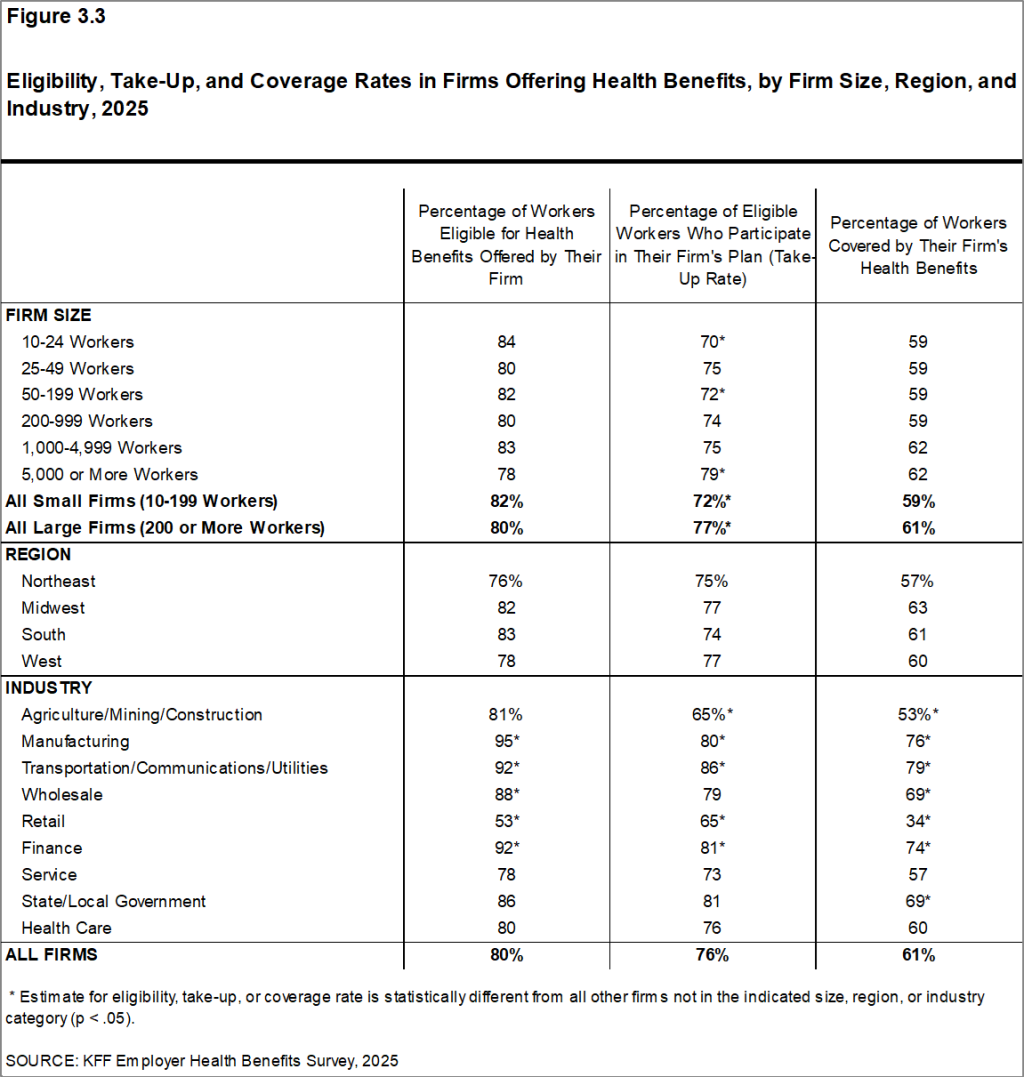
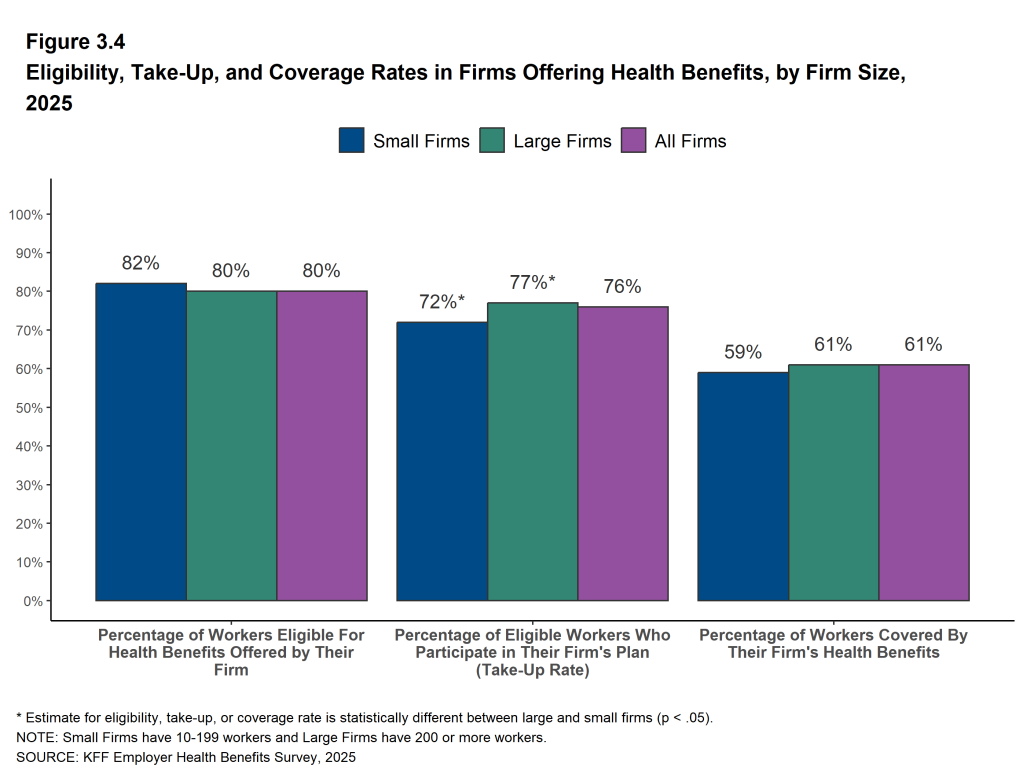
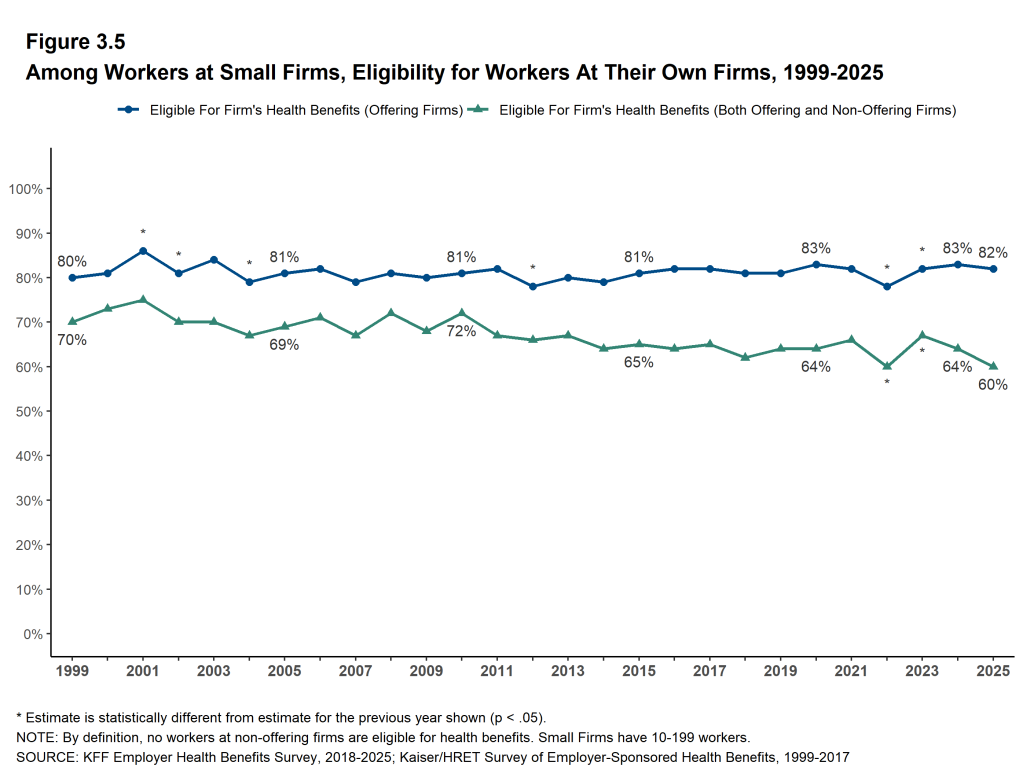
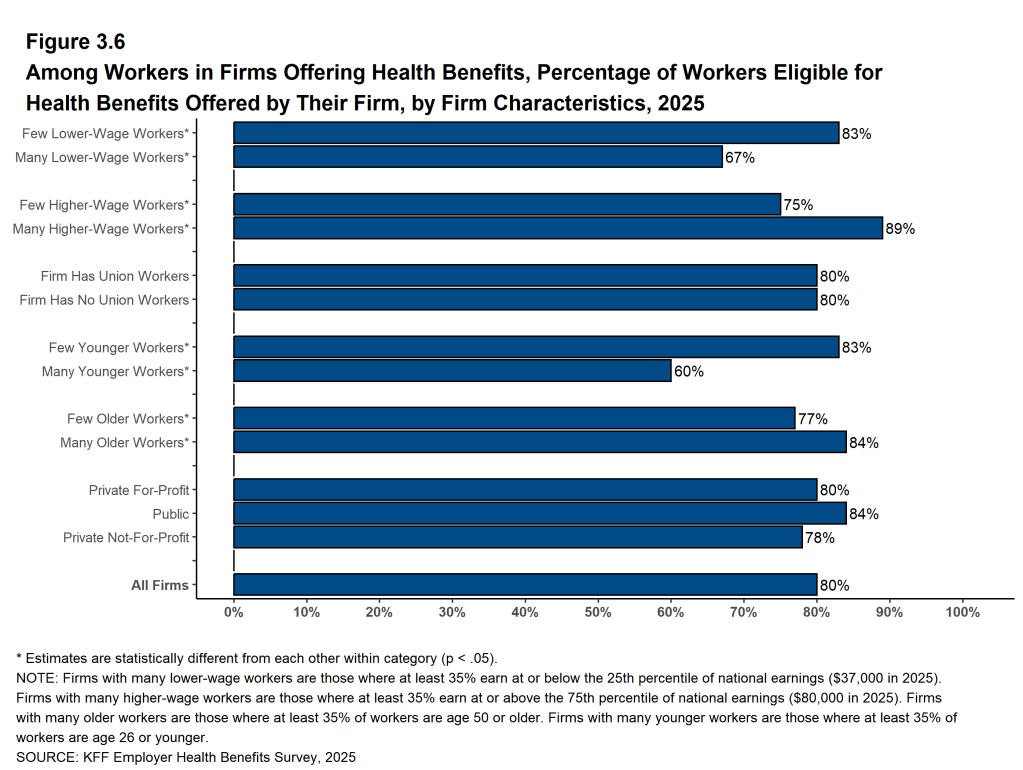
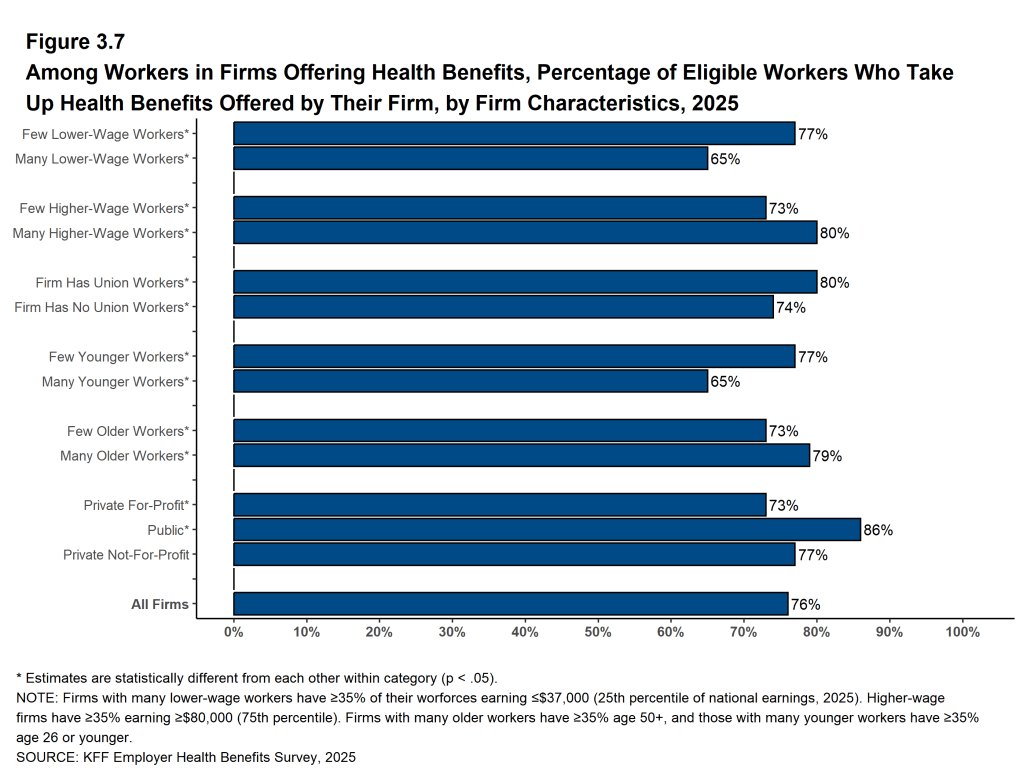
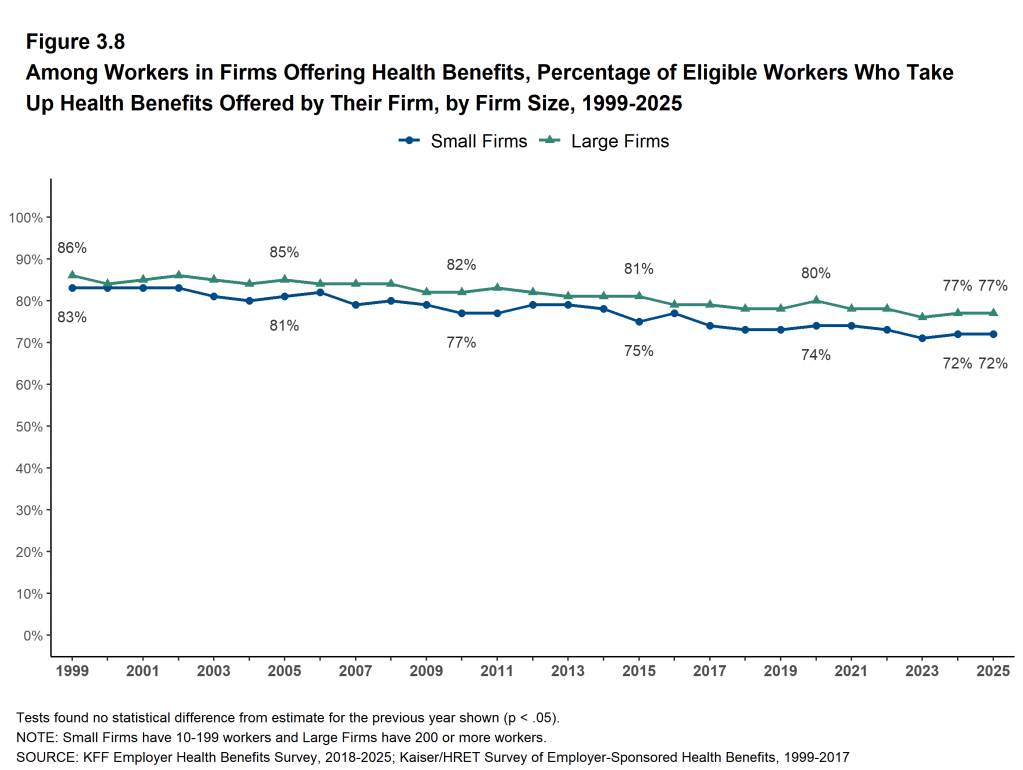
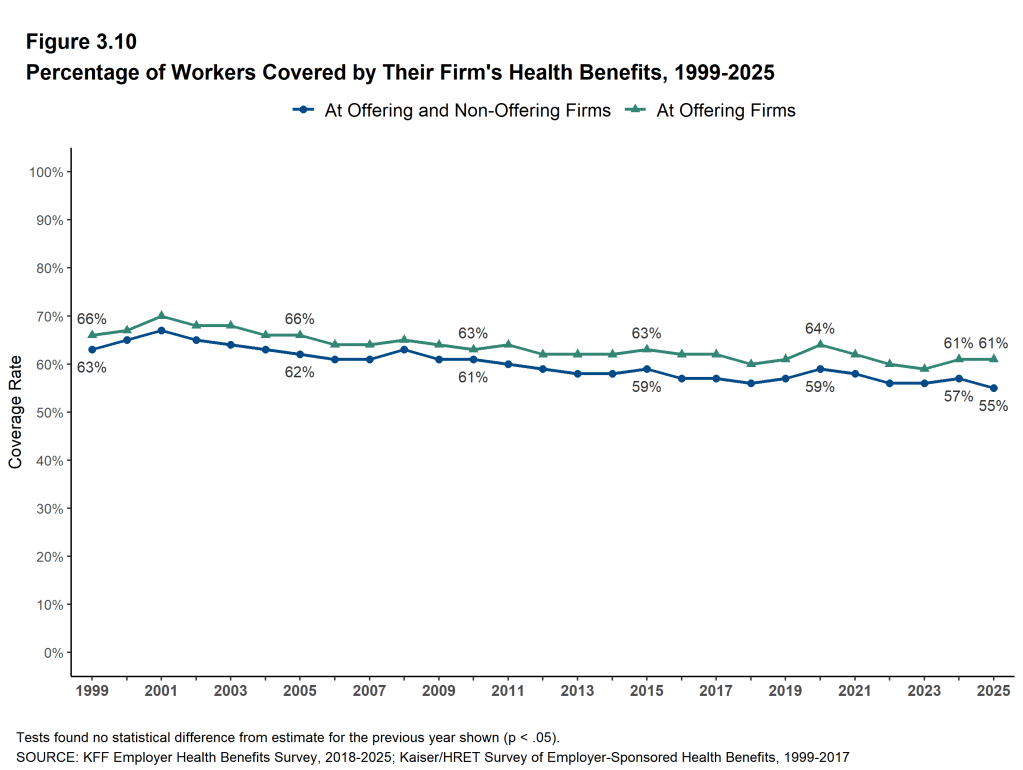
Even in firms offering health benefits, many workers are not covered by health benefits provided by the firm. Some are not eligible to enroll (due to factors such as waiting periods or part-time or temporary work status), while others who are eligible choose not to enroll (they may feel the coverage is too expensive, or they may be covered through another source). Additionally, some firms provide incentives for workers or spouses of workers not to enroll in their plans, or to enroll in a spouses’ plan. On average, at firms that offer coverage, 80% of workers are eligible. Among eligible workers, 76% take up the firm’s offer. Overall, 61% of workers at firms that offer health benefits are enrolled in that coverage.
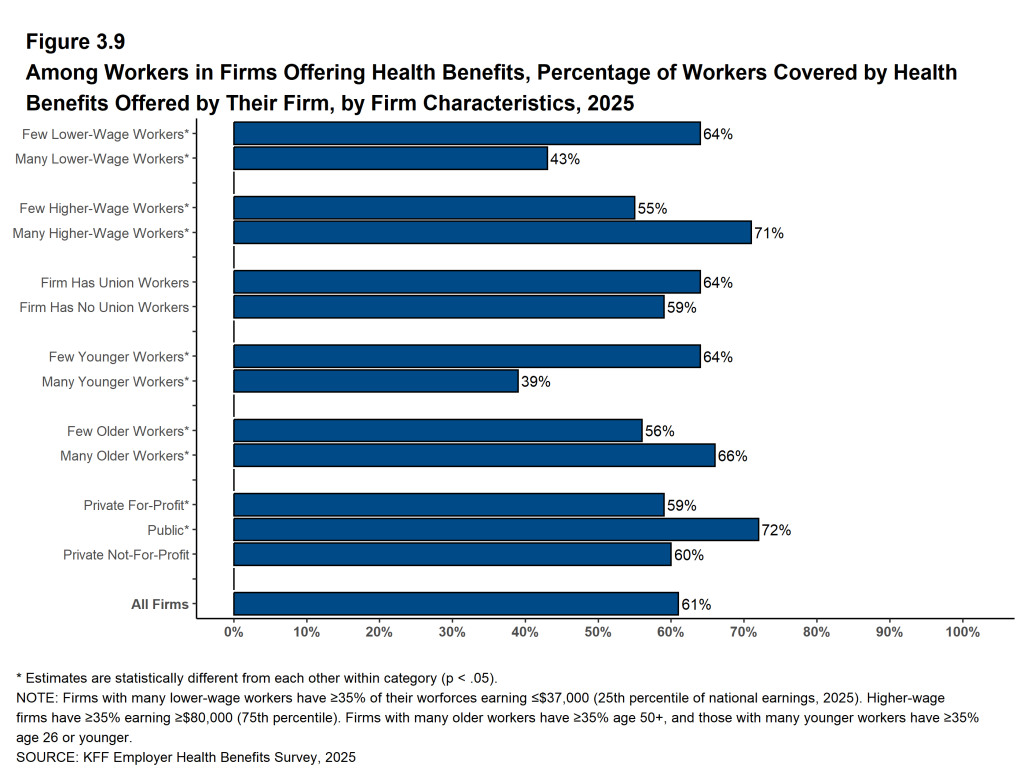
The coverage rate varies with workforce characteristics. Among workers at firms offering health benefits, those working for firms with a relatively large share of younger workers are less likely to be covered by their own firm than workers in firms with a smaller share of younger workers (39% vs. 64%) and those working at firms with a relatively large share of lower-wage workers are less likely to be covered by their own firm than workers at firms with a smaller share of lower-wage workers (43% vs. 64%)4 The share of workers employed at public organizations covered by their own employer (72%) is higher than the shares of workers covered that are employed at private for-profit firms (59%), or private non-for-profit firms (60%).
Across firms that offer health benefits and firms that do not, 55% of workers are covered by a health plan offered by their employer, similar to the percentage last year (57%).
HEALTH PROMOTION AND WELLNESS PROGRAMS
Many firms sponsor programs to help workers identify health issues and manage chronic conditions. These programs include health risk assessments, biometric screenings, and health promotion programs.
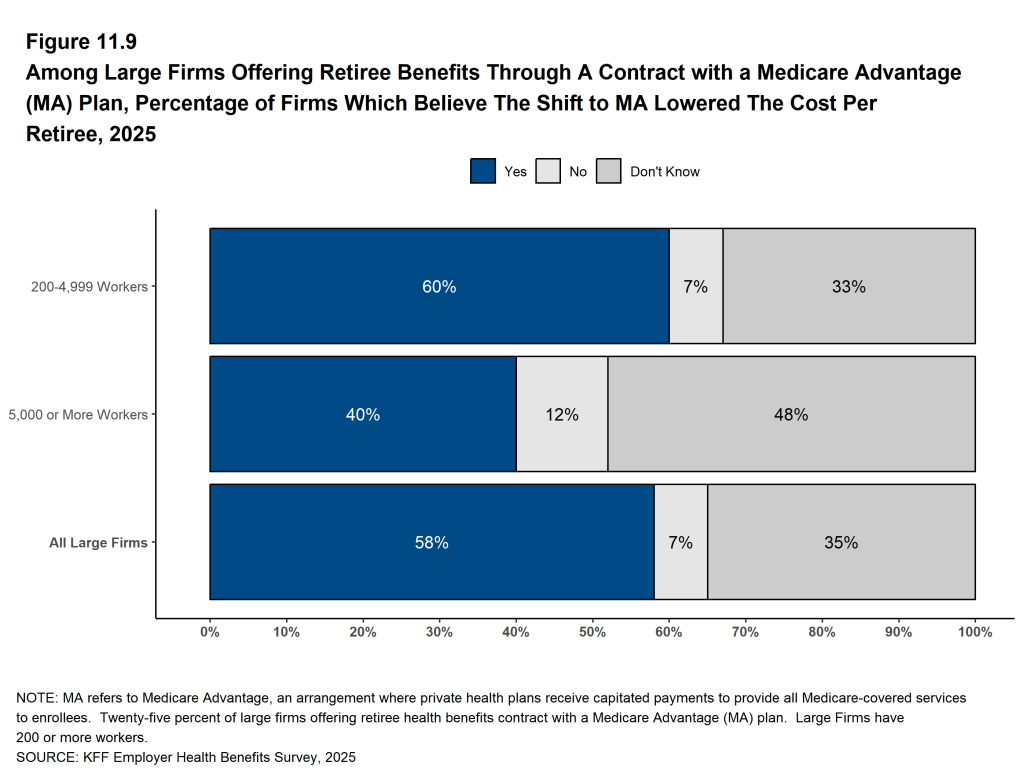
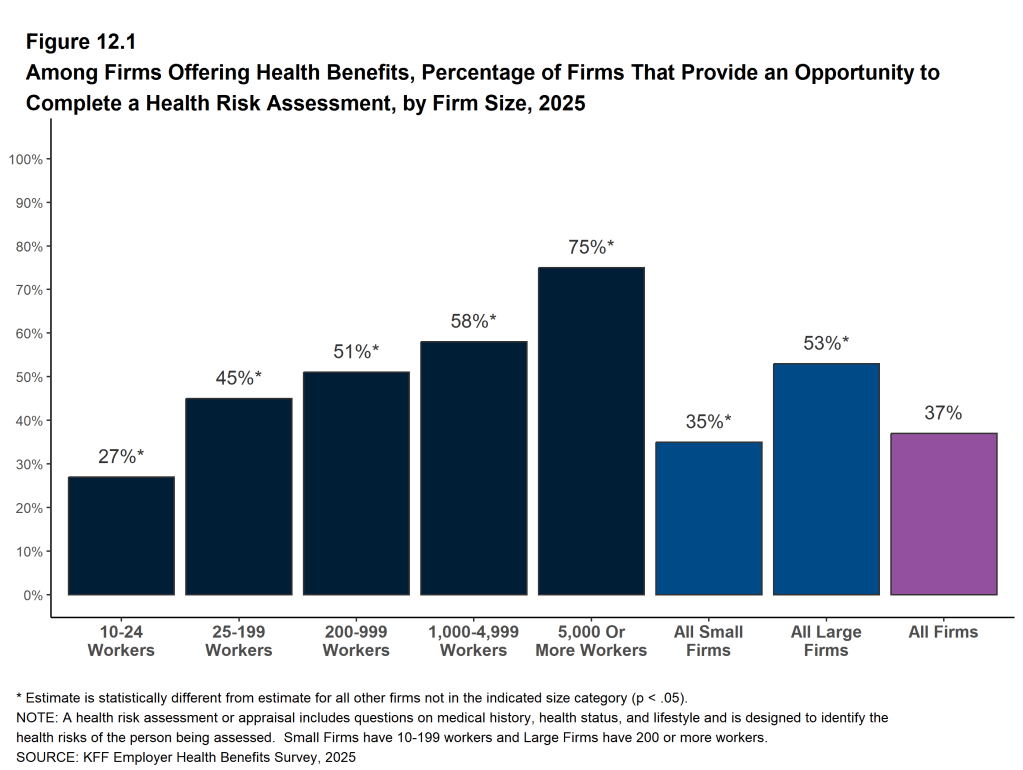
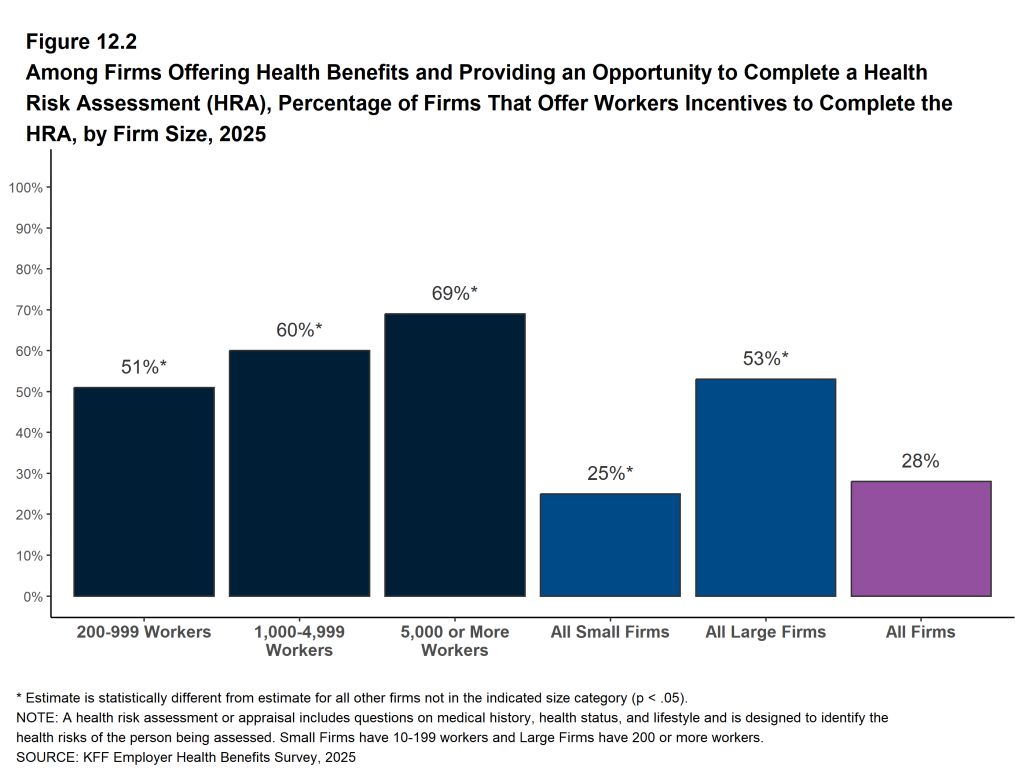
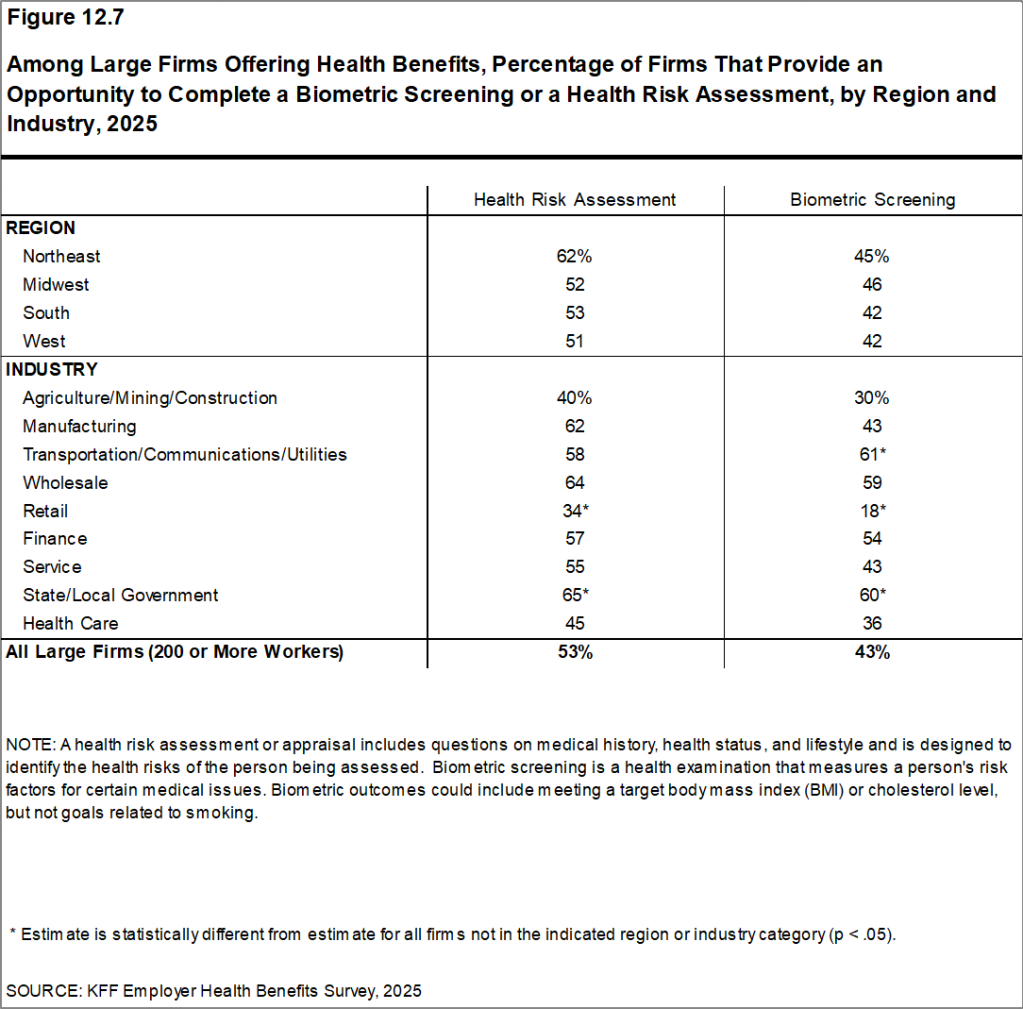
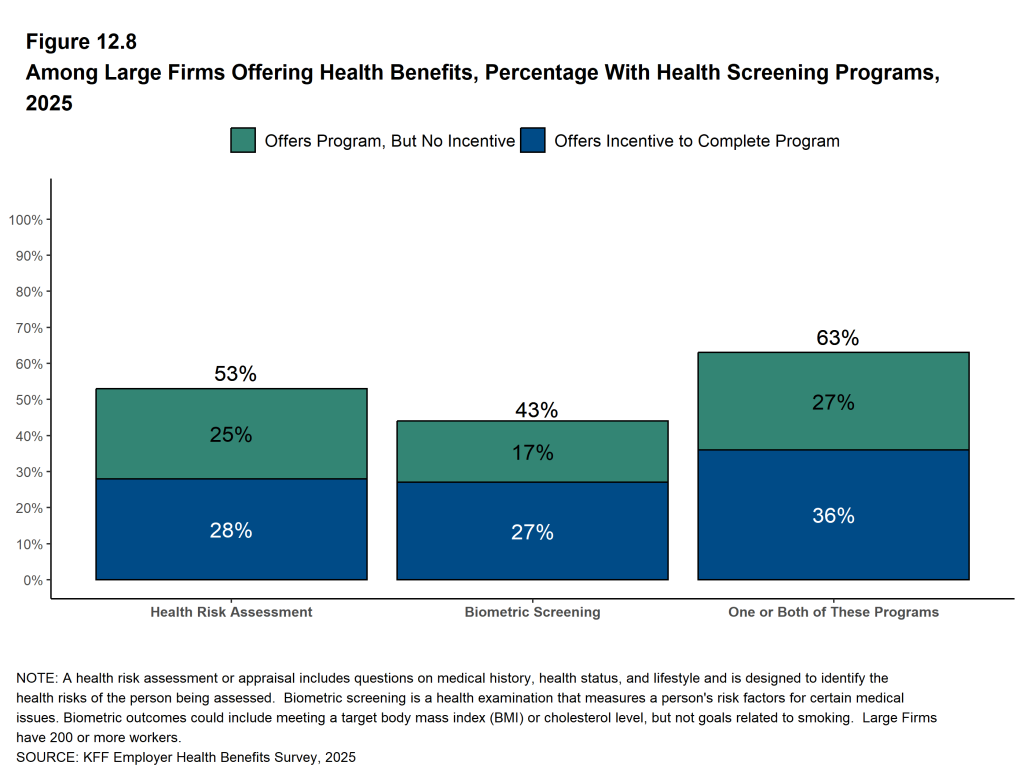
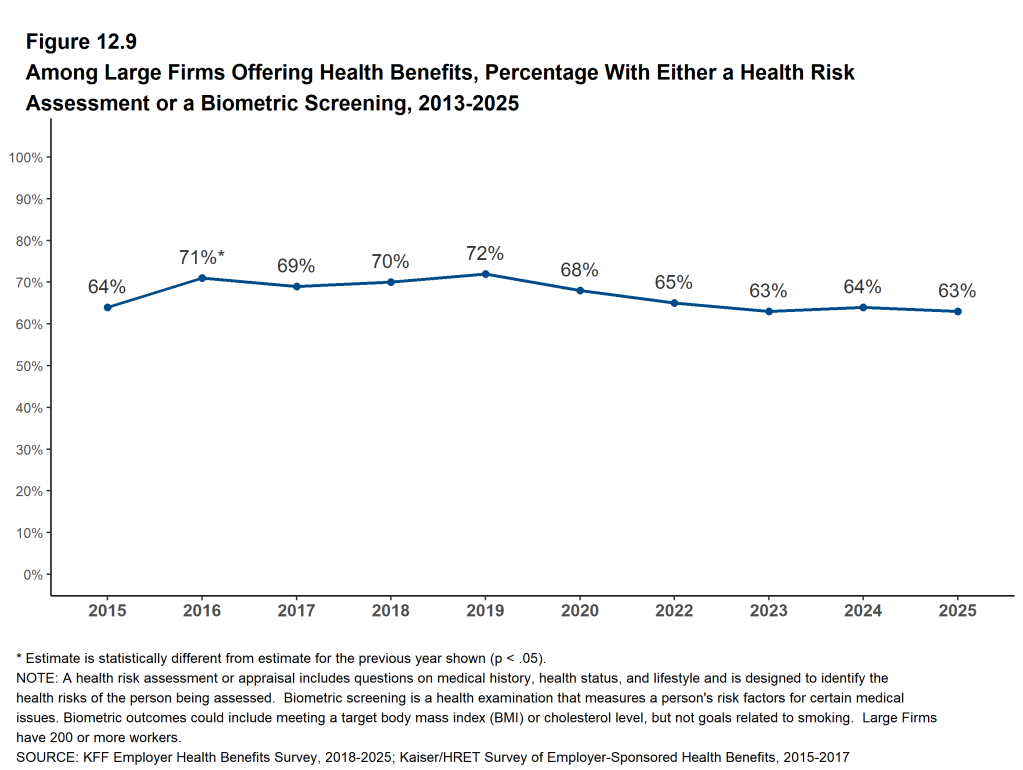
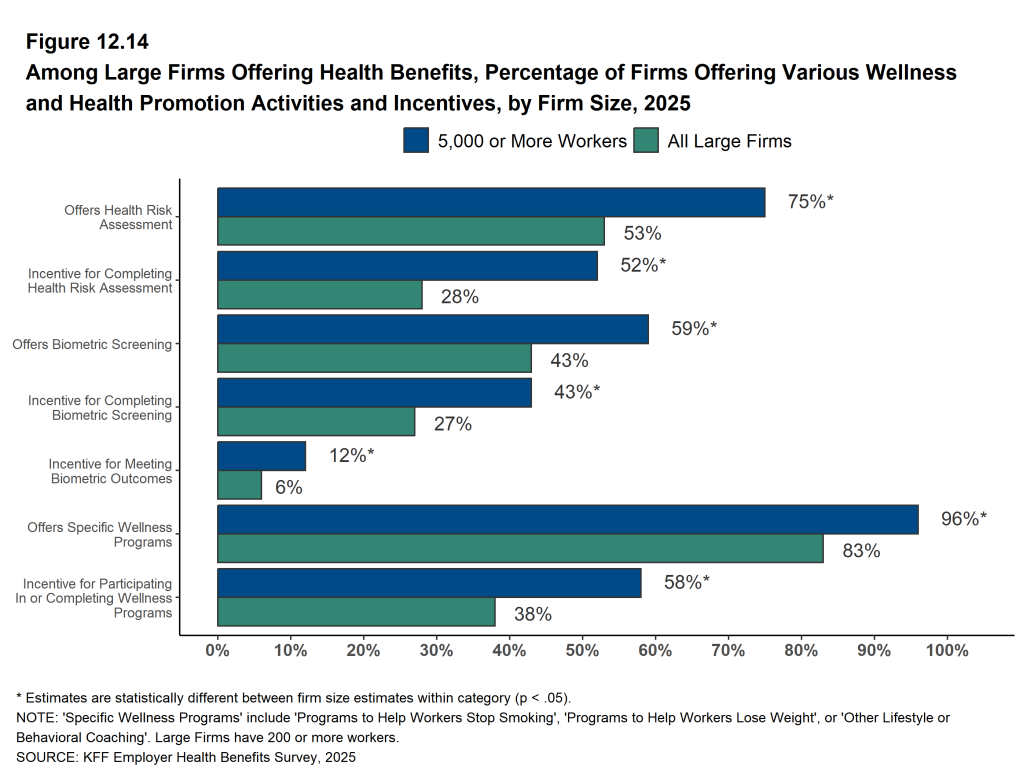
Health Risk Assessments. Among firms offering health benefits, 35% of firms with 10 to 199 workers and 53% of larger firms provide workers the opportunity to complete a health risk assessment. Among large firms that offer a health risk assessment, 53% use incentives or penalties to encourage workers to complete the assessment, similar to the percentage last year.
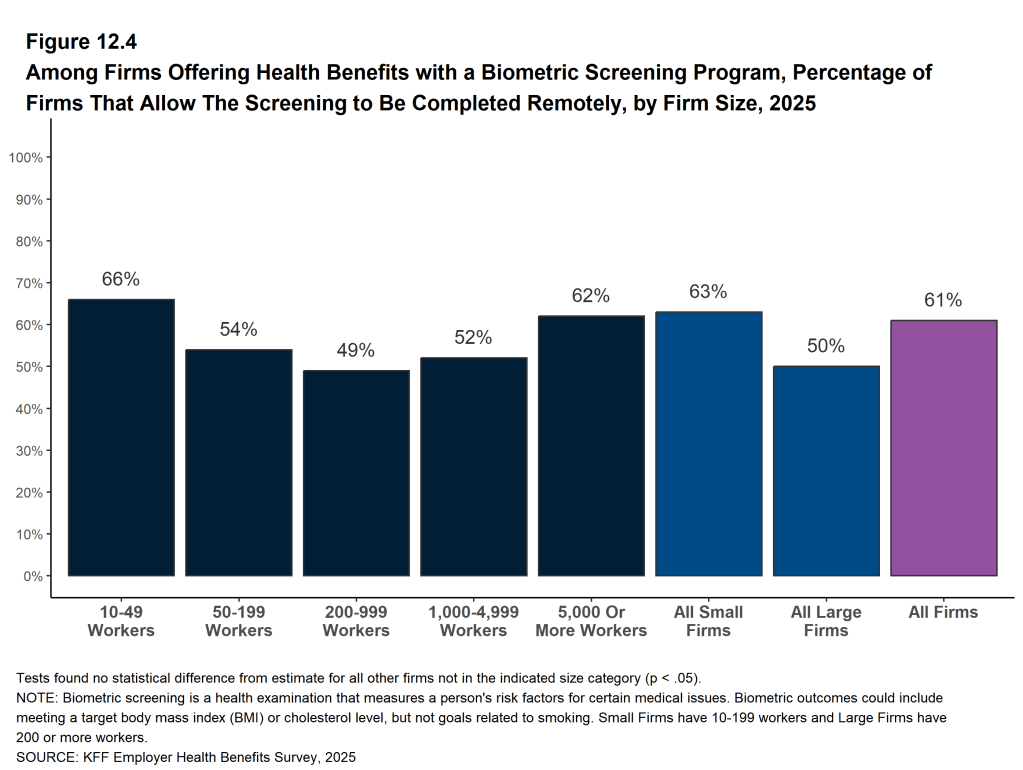
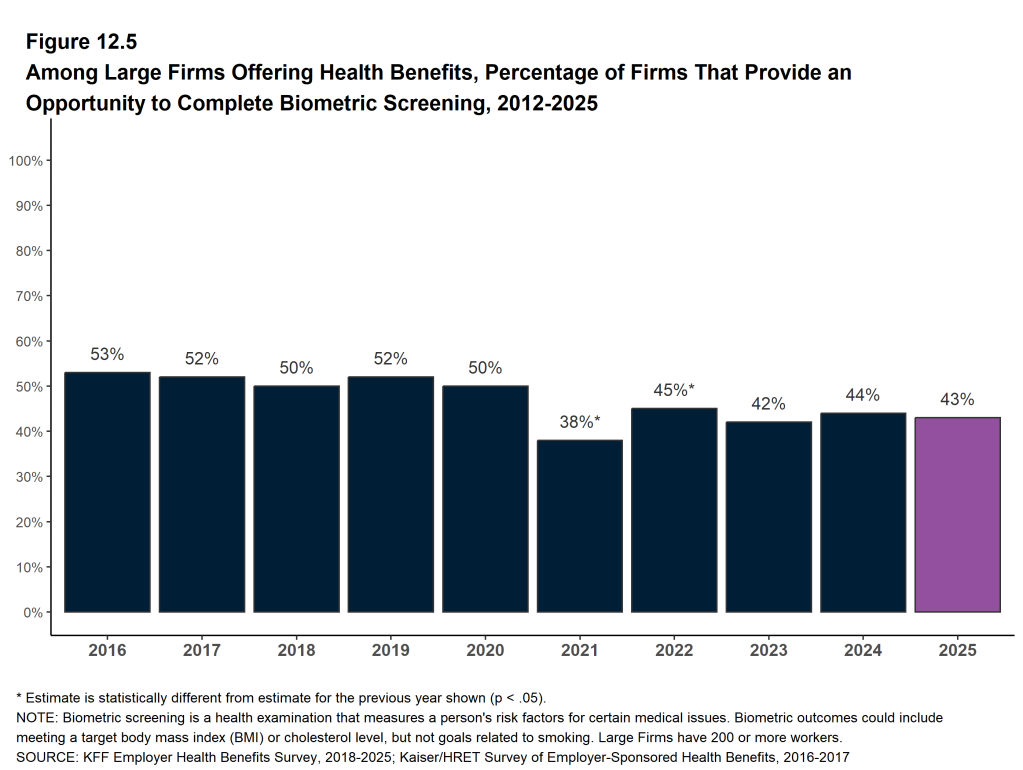
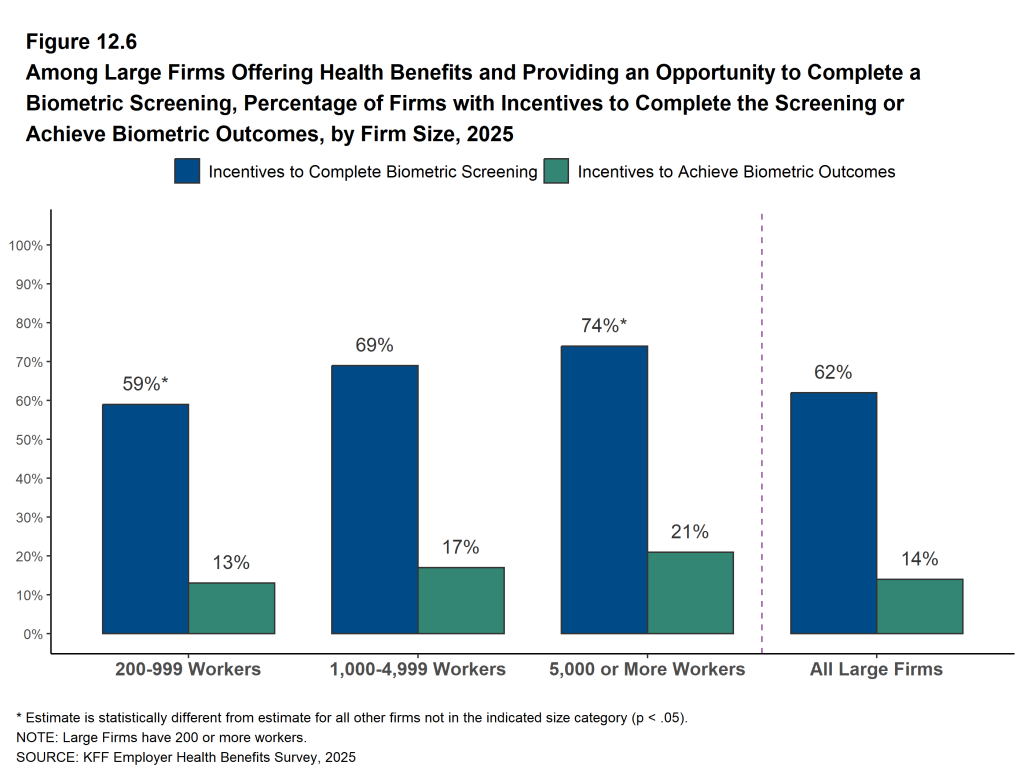
Biometric Screenings. Among firms offering health benefits, 22% of firms with 10 to 199 workers and 43% of larger firms provide workers the opportunity to complete a biometric screening. Among large firms with a biometric screening program, 62% use incentives or penalties to encourage workers to complete the assessment, similar to the percentage last year.
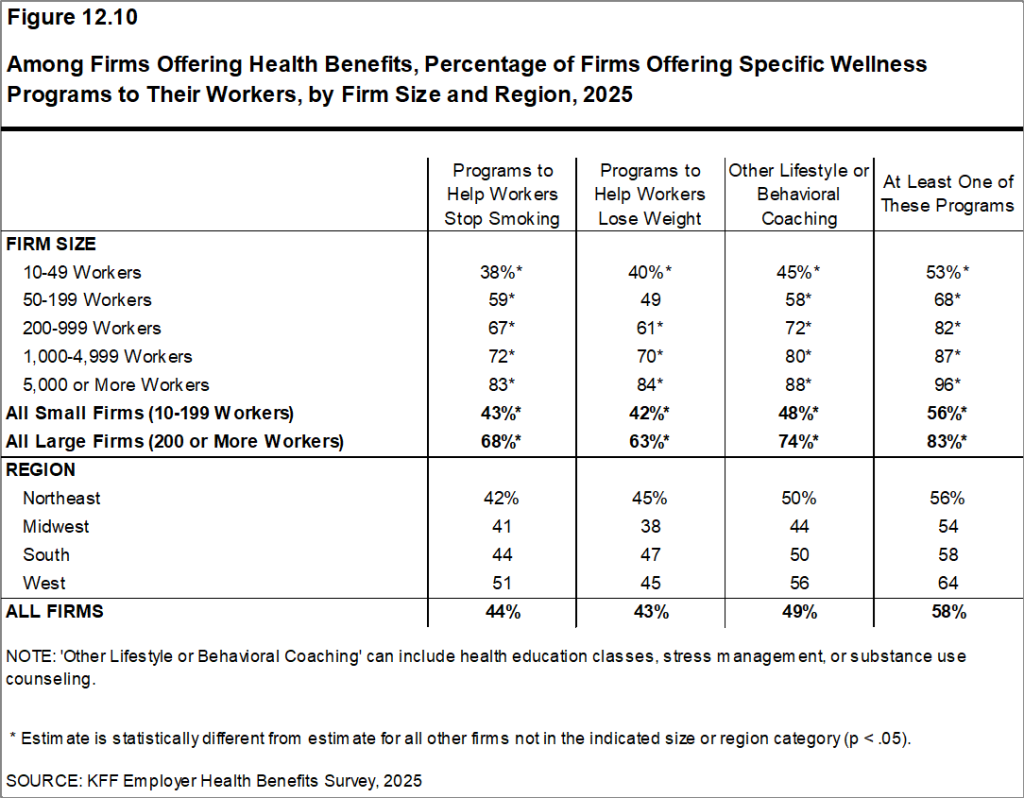
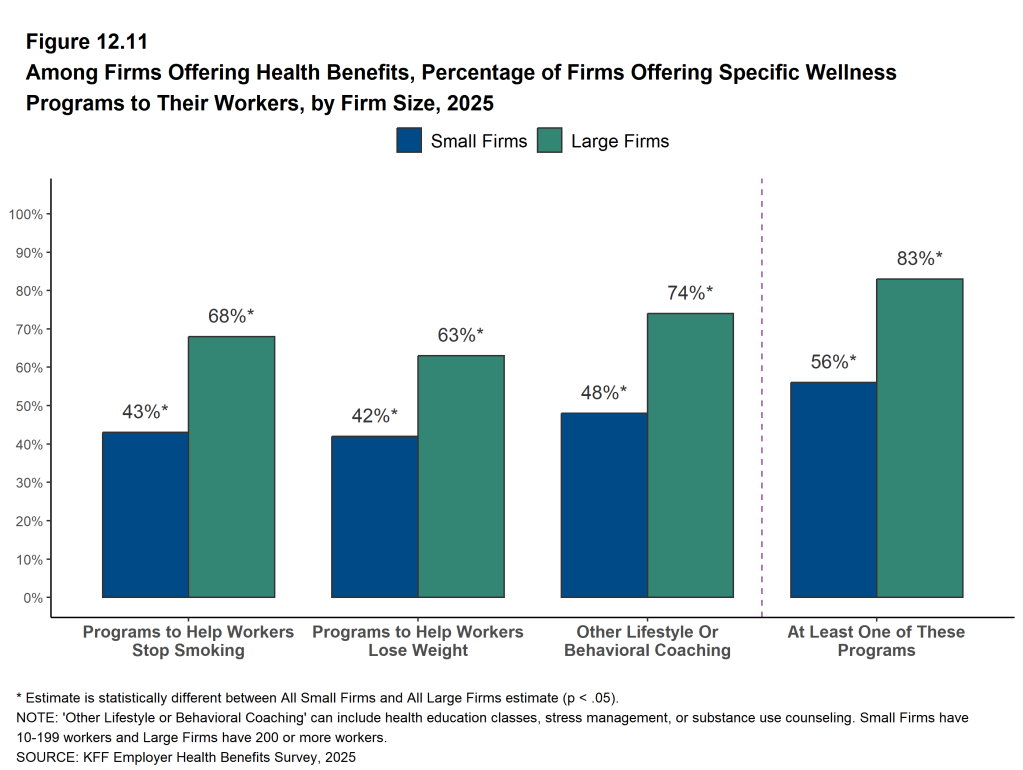
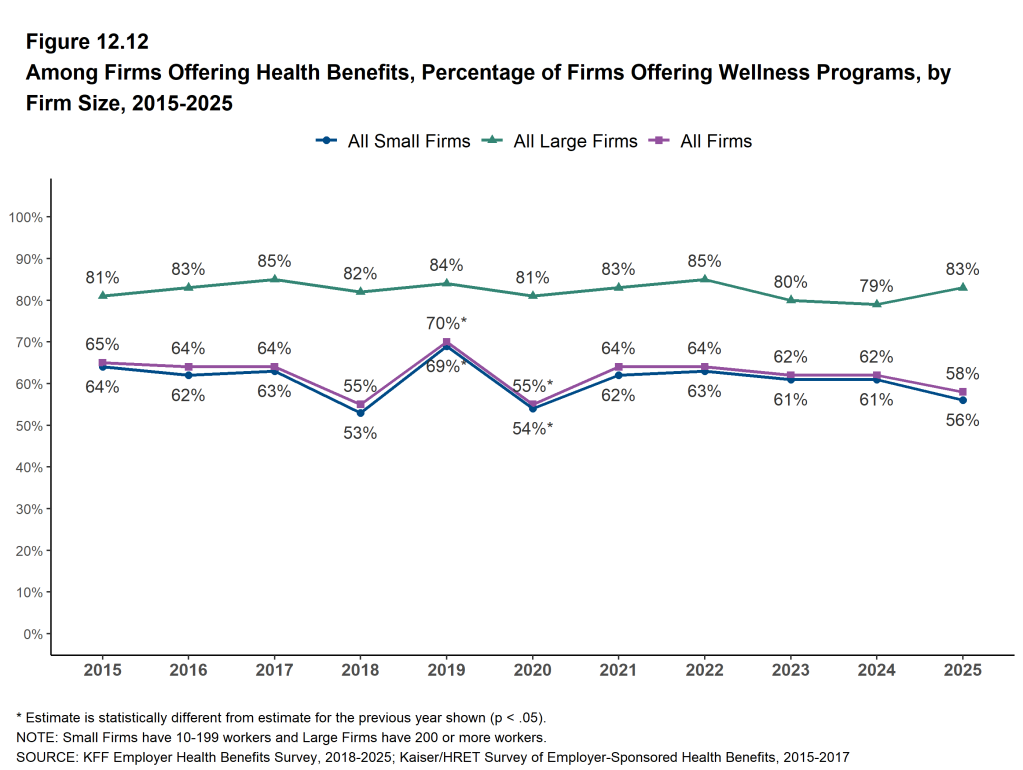
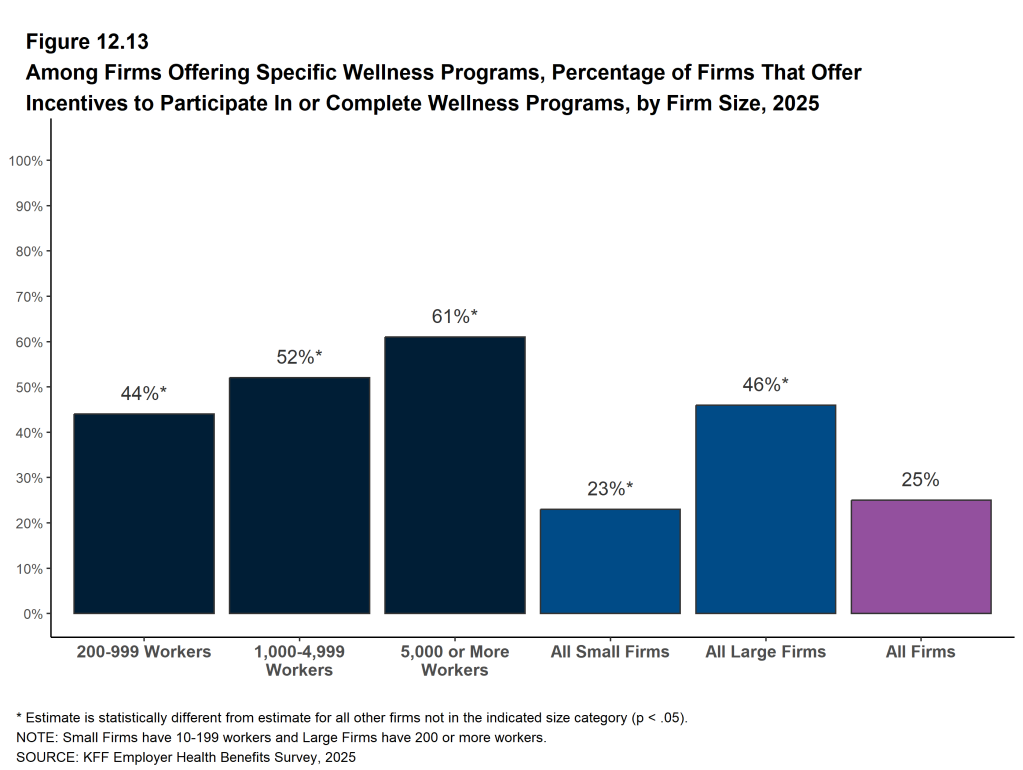
Health and Wellness Promotion Programs. Many firms offering health benefits offer programs to help workers identify and address health risks and unhealthy behaviors. Fifty-six percent of firms with 10 to 199 workers and 83% of larger firms offer a program in at least one of these areas: smoking cessation, weight management, and behavioral or lifestyle coaching. The percentage of both smaller firms and larger firms offering one of these programs are similar to the percentages last year (61% and 79%, respectively).
GLP-1 DRUG COVERAGE FOR WEIGHT LOSS
GLP-1 (Glucagon-like peptide-1) agonists, used to help control blood sugar levels in people with type 2 diabetes and certain other conditions, have also been shown to be an effective drug to help people lose weight. The high cost of these drugs, however, combined with the large number of people who could benefit and the potential for long-term usage, has raised concerns about the costs of covering them as a weight-loss treatment.
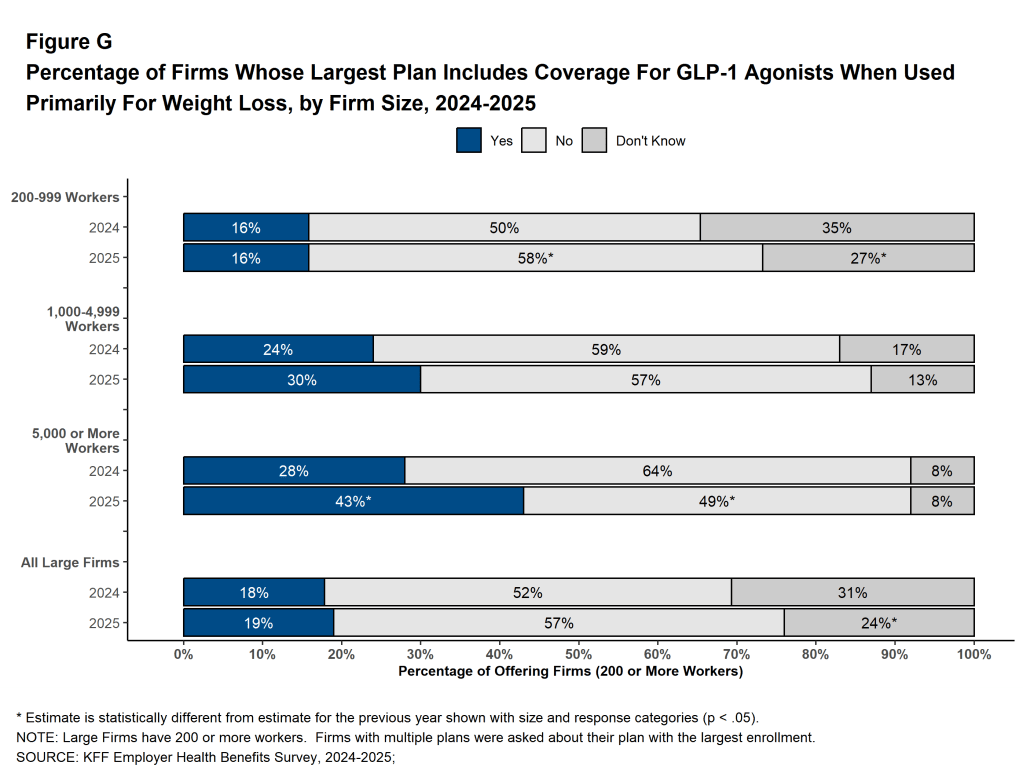
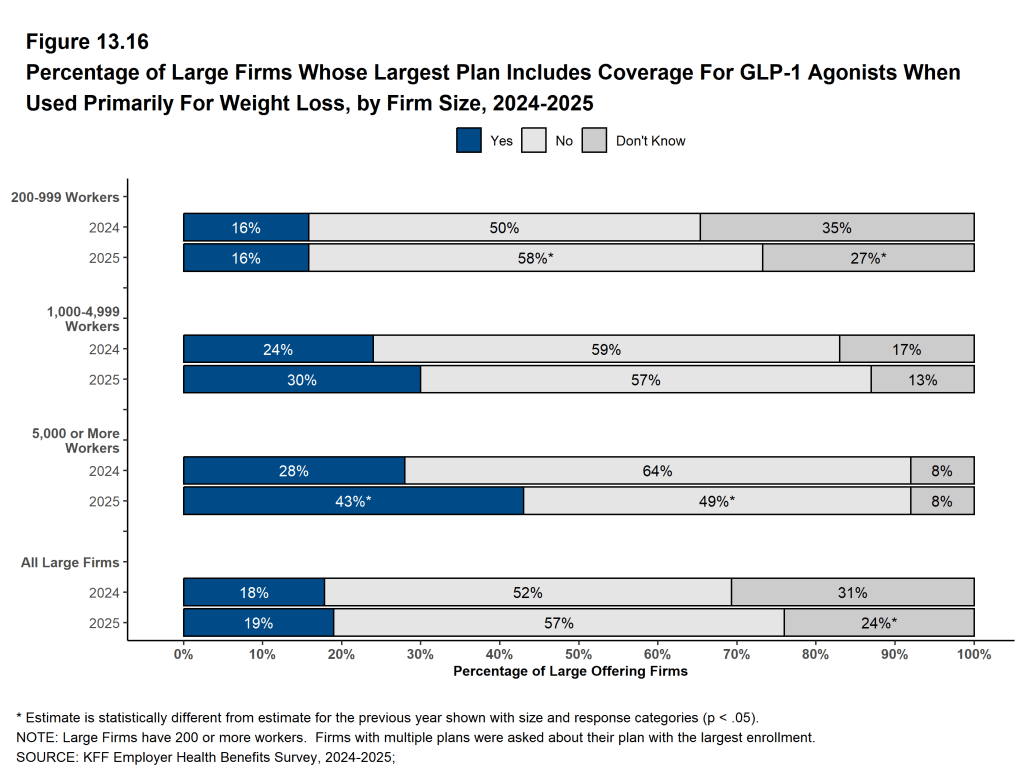
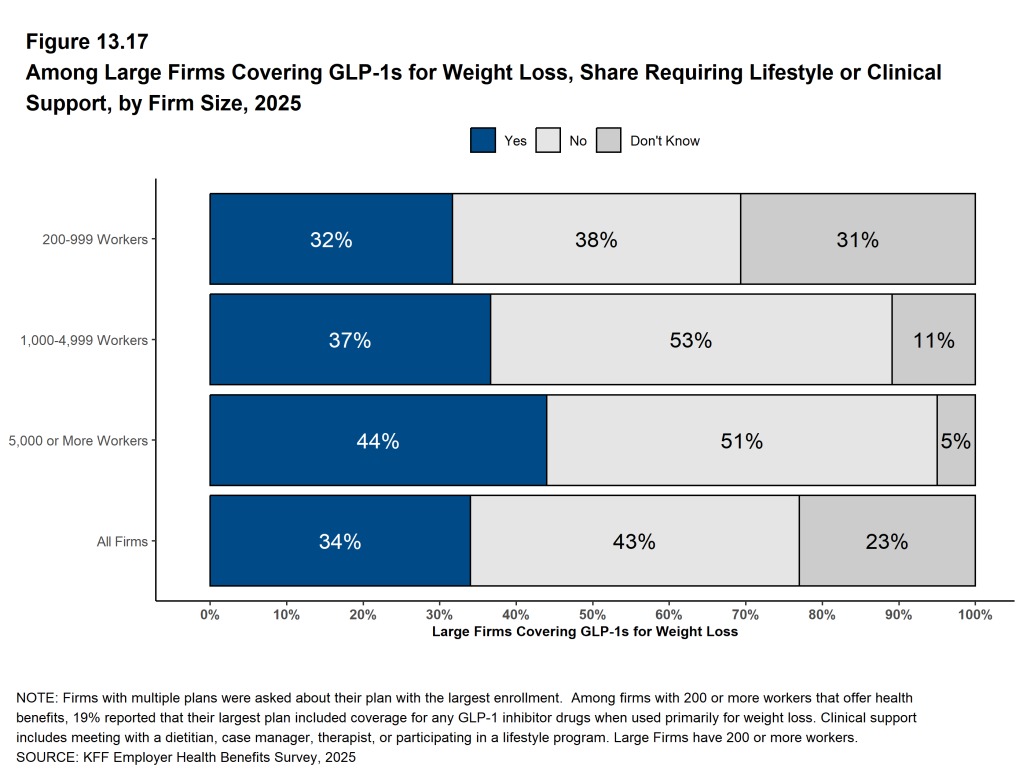
Among firms that offer health benefits with 200 or more workers, 16% of firms with 200 to 999 workers, 30% of firms with 1,000 to 4,999 workers, and 43% of firms with 5,000 or more workers cover GLP-1 agonists when used primarily for weight loss in 2025. The percentage of firms with 5,000 or more workers covering GLP-1 agonists for weight loss is higher than the percentage last year (43% vs. 28%) [Figure G]. Thirty-four percent of firms covering these drugs for weight loss require enrollees to meet with a dietitian, case manager, or therapist, or participate in a lifestyle program in order to receive the coverage.
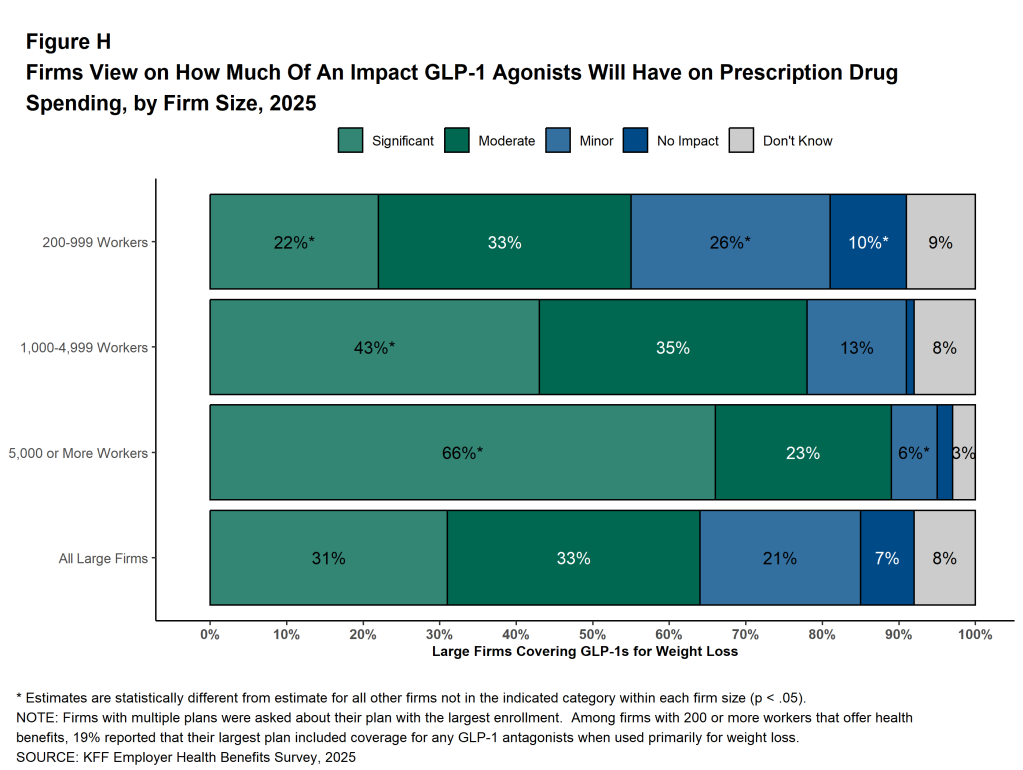
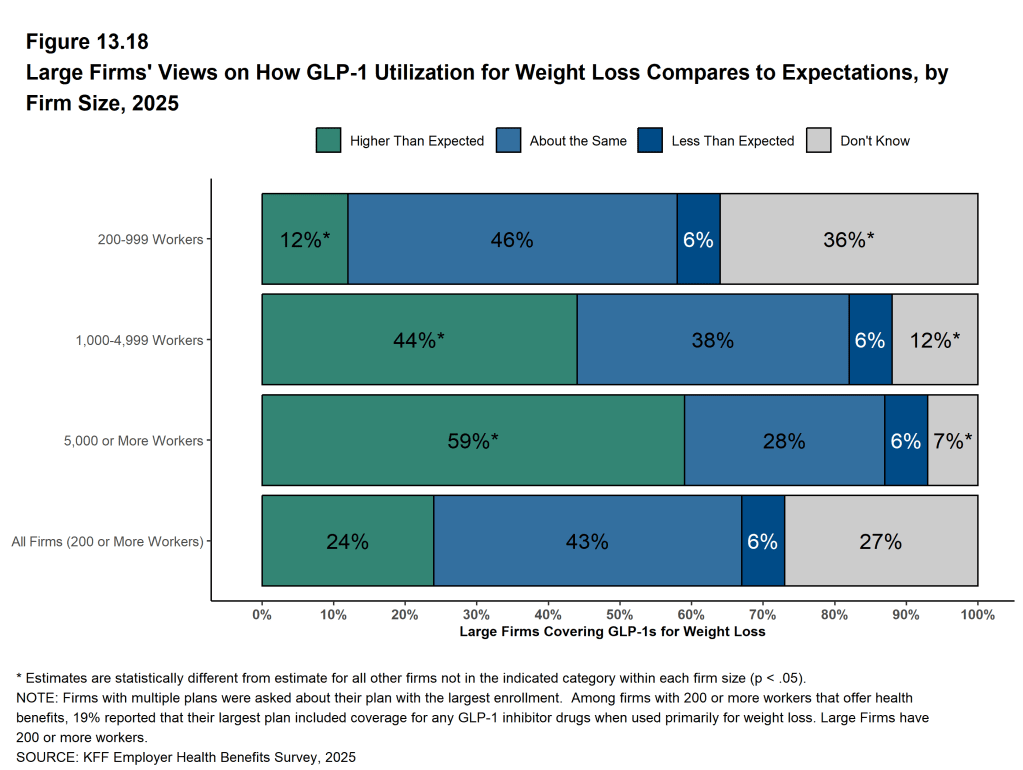
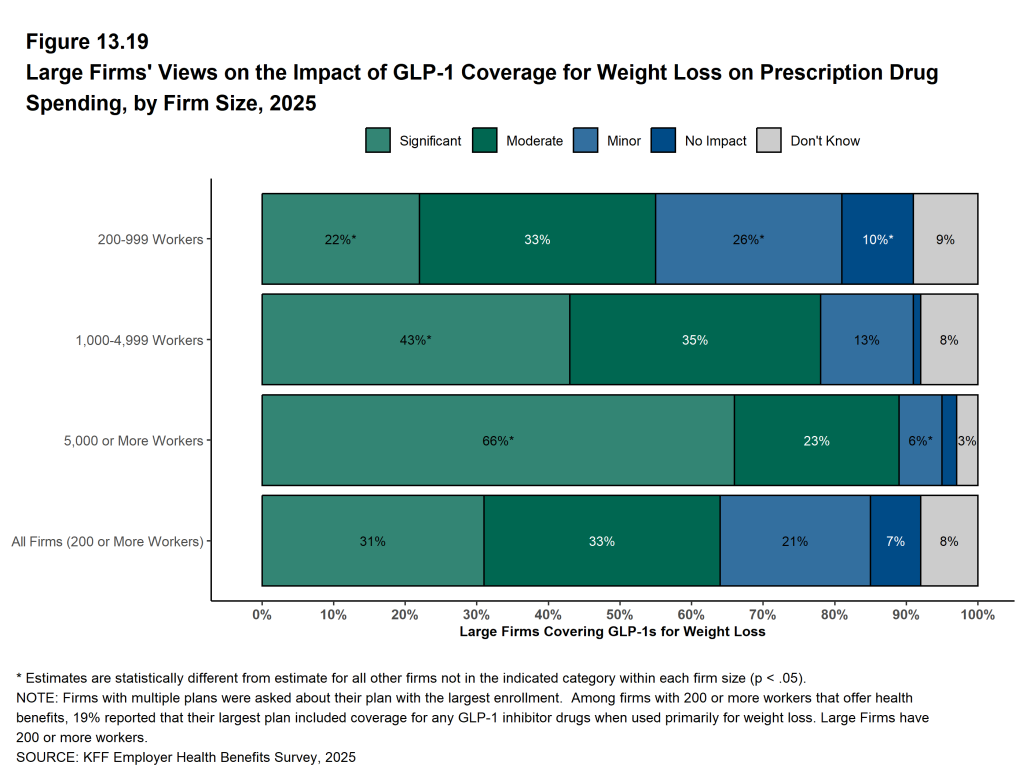
Firms covering GLP-1 agonists primarily for weight loss were asked how the use of the drug compared to expectations and about the impact on the firm’s spending for prescription drugs. Forty-four percent of these firms with 1,000 to 4,999 workers, and 59% of these firms with 5,000 or more workers, say that the use of these medications for weight loss was higher than expected. Forty-three percent of these firms with 1,000 to 4,999 workers, and 66% of these firms with 5,000 or more workers say that covering GLP-1 agonists for weight loss had a “significant” impact on the health plan’s prescription drug spending [Figure H].
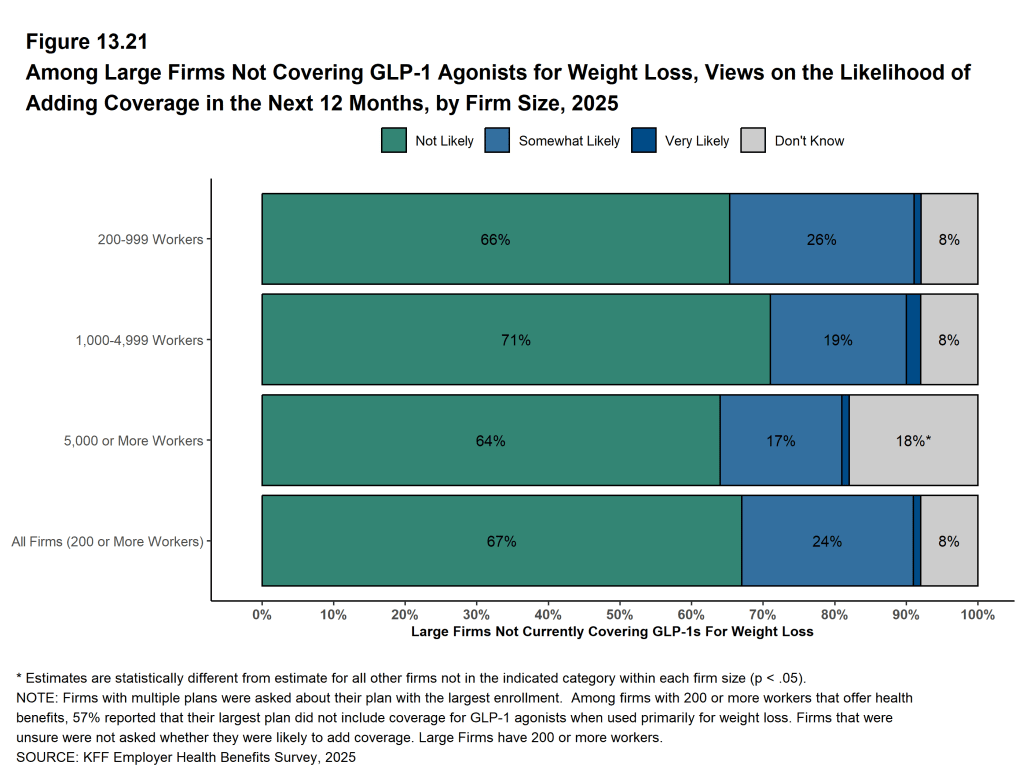
Among firms with 200 or more workers that offer health benefits and do not cover GLP-1 agonists for weight loss, only 1% say that they are “very likely” to begin covering GLP-1 agonists for weight loss within the next 12 months, 24% say that they were “somewhat likely,” 67% say that they were “not likely,” and 8% do not know the answer to the question.
Figure G: Percentage of Firms Whose Largest Plan Includes Coverage for GLP-1 Agonists When Used Primarily for Weight Loss, by Firm Size, 2024-2025
Figure H: Firms View On How Much of an Impact GLP-1 Agonists Will Have On Prescription Drug Spending, by Firm Size, 2025
EMPLOYEE CONCERNS WITH PLAN AND UTILIZATION MANAGEMENT
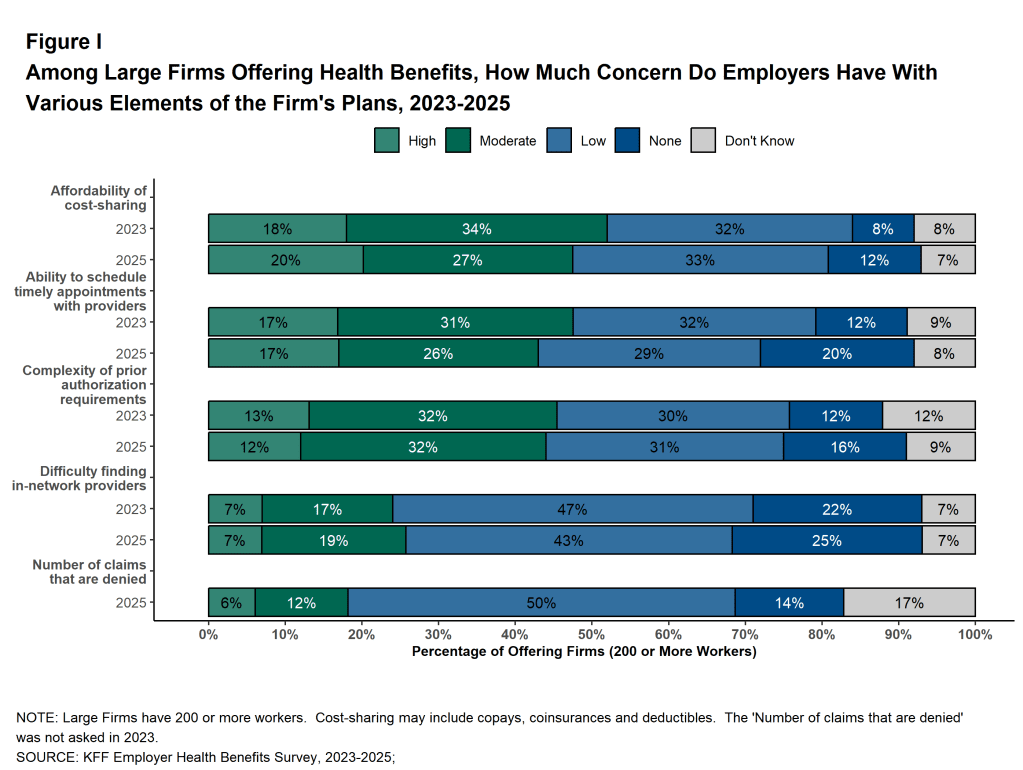
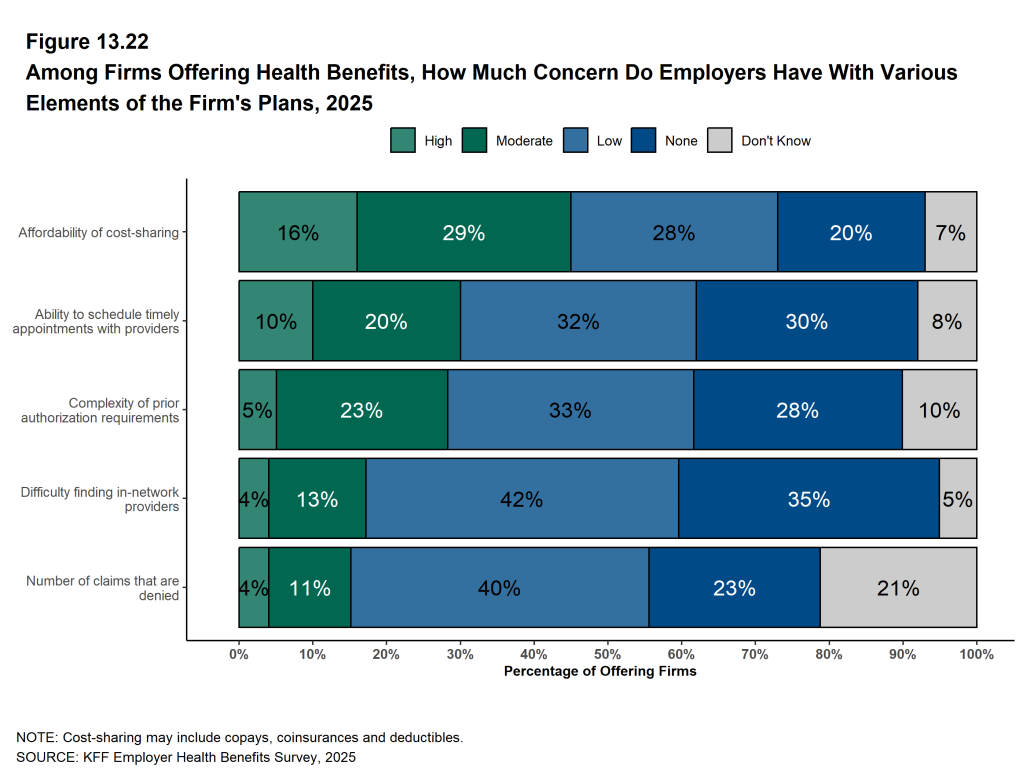
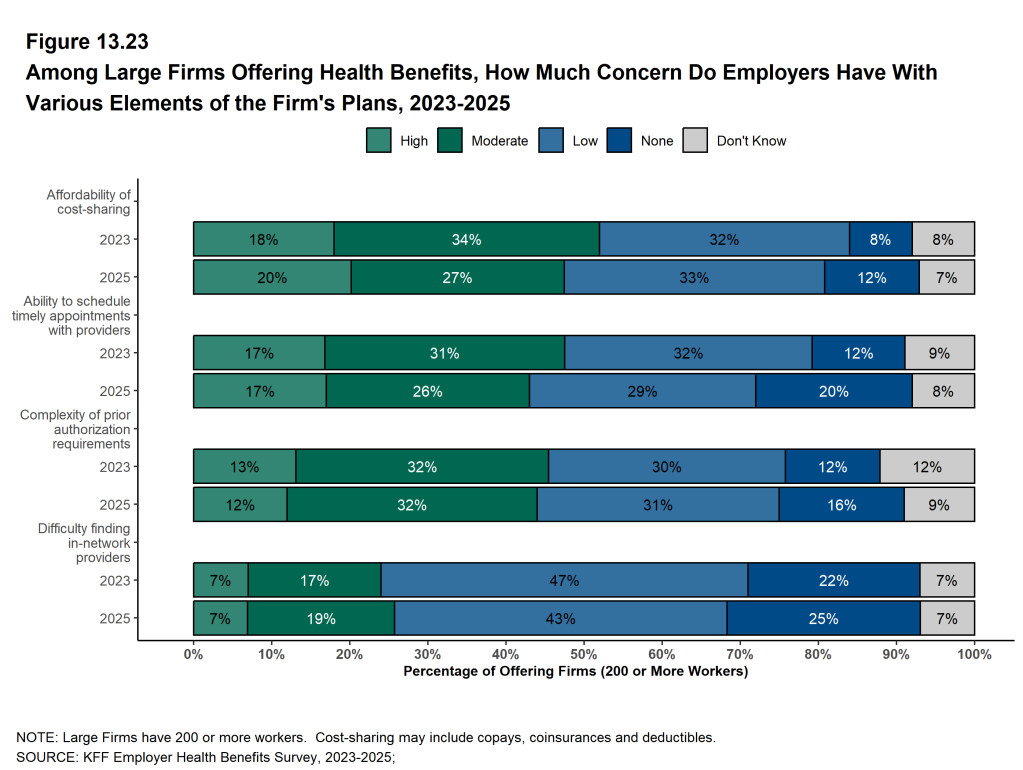
Consumer concerns about health plan management—such as prior authorization requirements—have received growing public attention in recent years. Firms offering health benefits were asked to assess how concerned they believe their employees are about various aspects of health plan management. Among large firms (200 or more workers):
Affordability of Cost Sharing. Twenty percent believe that their employees level of concern over the affordability of cost sharing is “high,” 27% believe the level of concern is “moderate,” 33% believe the level of concern is “low,” 12% believe the level of concern is “none,” and 7% do not know the level of concern [Figure I]. Firms with 10 to 199 workers are more likely than larger employers to believe their employees have no concern about the affordability of cost sharing (21%).
Scheduling Timely Appointments With Providers. Seventeen percent believe that their employees level of concern over their ability to schedule timely appoints is “high,” 26% believe the level of concern is “moderate,” 29% believe the level of concern is “low,” 20% believe the level of concern is “none,” and 8% do not know the level of concern [Figure I]. Firms with 200 or more workers are more likely than smaller firms to believe that employees have a “high” or “moderate” level of concern about their ability to schedule timely appointments with providers (29%).
Complexity of Prior Authorization Requirements. Twelve percent believe that their employees level of concern over the complexity of prior authorization requirements is “high,” 32% believe the level of concern is “moderate,” 31% believe the level of concern is “low,” 16% believe the level of concern is “none,” and 9% do not know the level of concern [Figure I].
Finding In-Network Providers. Seven percent believe that their employees level of concern over the difficulty of finding in-network providers is “high,” 19% believe the level of concern is “moderate,” 43% believe the level of concern is “low,” 25% believe the level of concern is “none,” and 7% do not know the level of concern [Figure I]. Firms with 10 to 199 workers are more likely than larger employers to believe their employees have no concern about their ability to find in-network providers (29%).
Number of Denied Claims. Six percent believe that their employees level of concern about the number of denied claims is “high,” 12% believe the level of concern is “moderate,” 50% believe the level of concern is “low,” 14% believe the level of concern is “none,” and 17% do not know the level of concern [Figure I].
Figure I: Among Large Firms Offering Health Benefits, How Much Concern Do Employers Have With Various Elements of the Firm’s Plans, 2023-2025
SUFFICIENCY OF PROVIDER NETWORKS
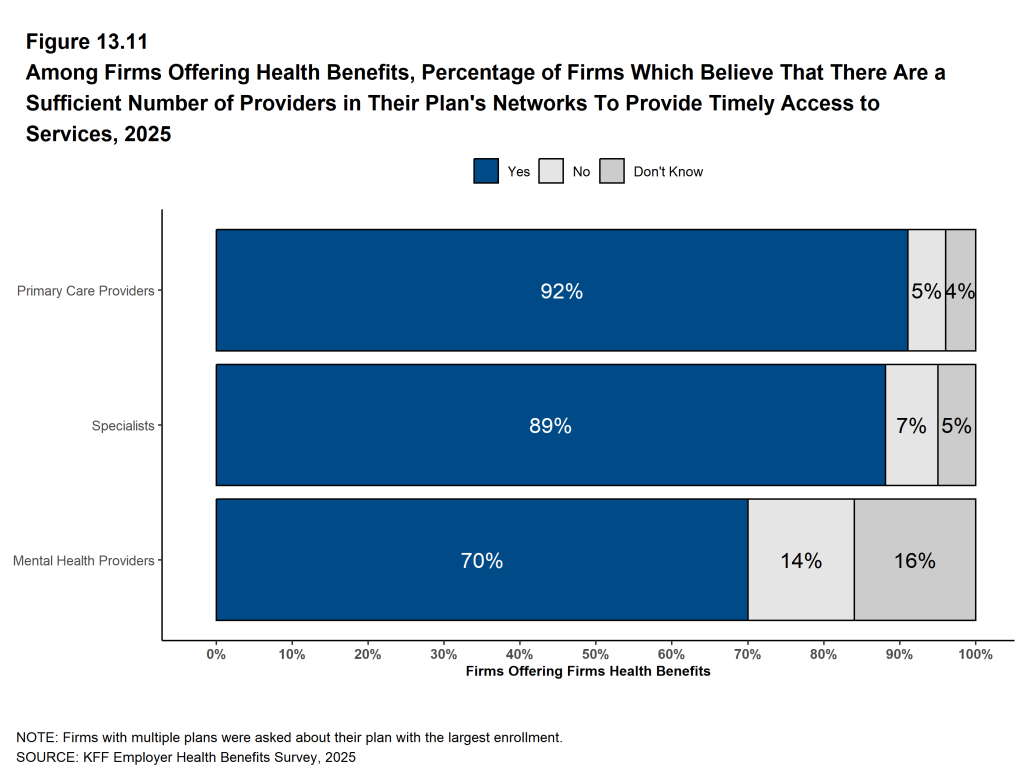
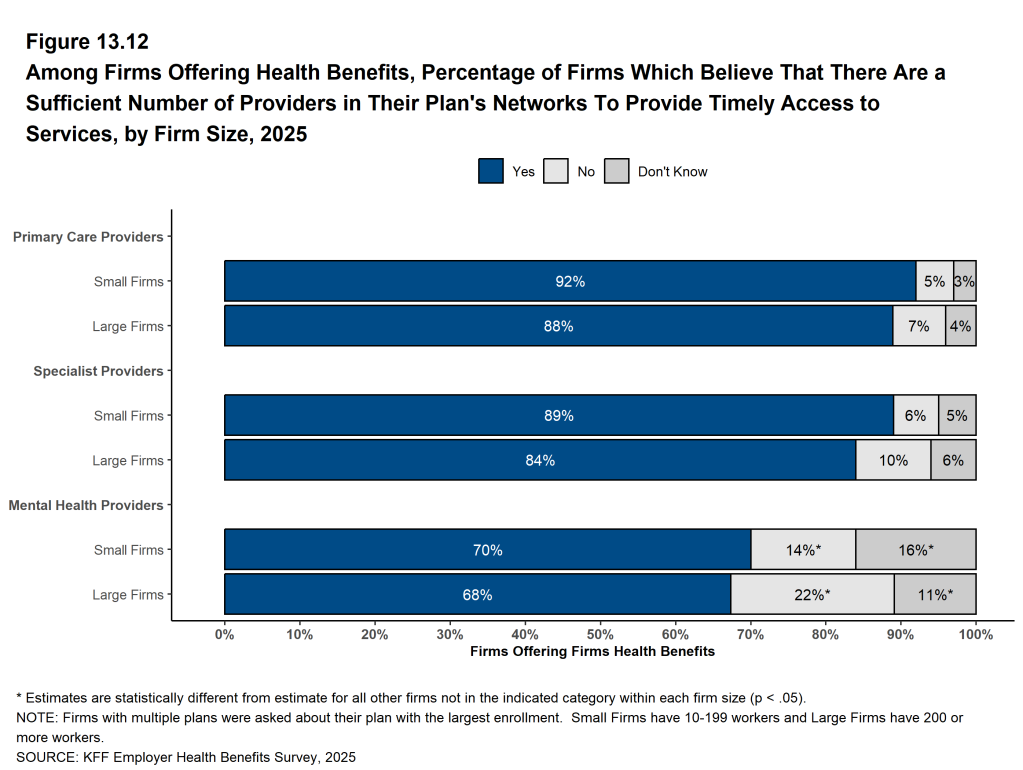
Firms offering health benefits were asked whether they believed the provider network for their health plan with the largest enrollment included a sufficient number of providers to ensure timely access to primary care, specialty care, and mental health services. Ninety-two percent of these firms believe their largest health plan provides timely access to primary care services, 89% believe it provides timely access to specialty care, and 70% believe it provides timely access to mental health services. These percentages are similar among small and large firms.
HEALTH PLAN PROVIDER NETWORKS
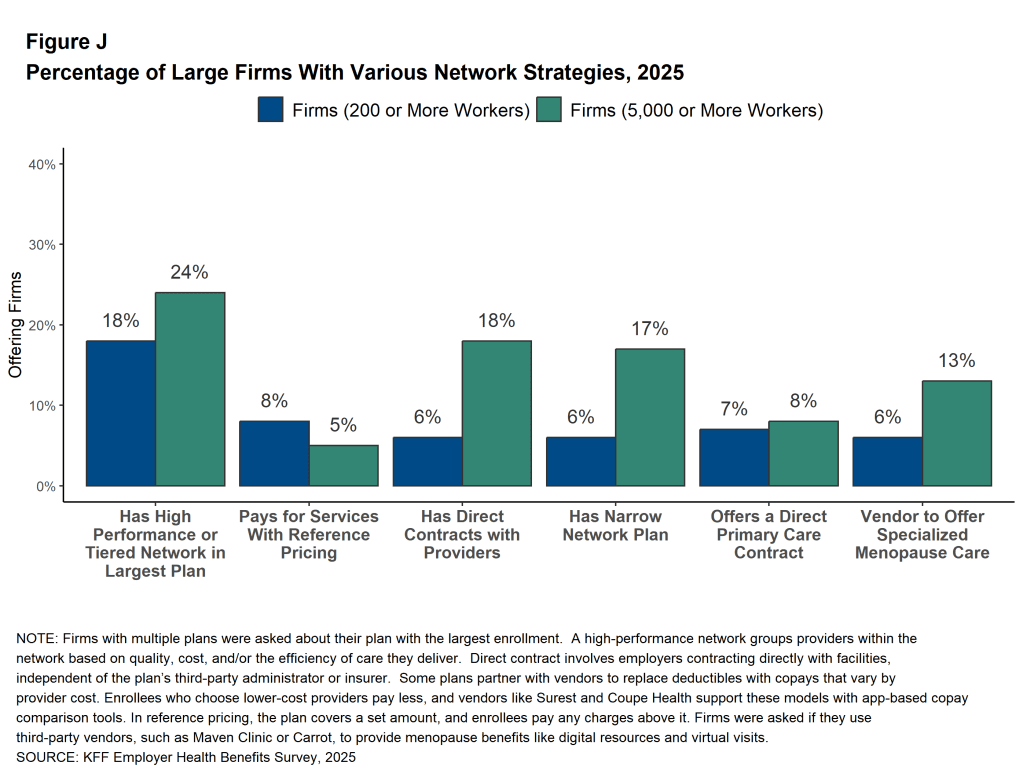
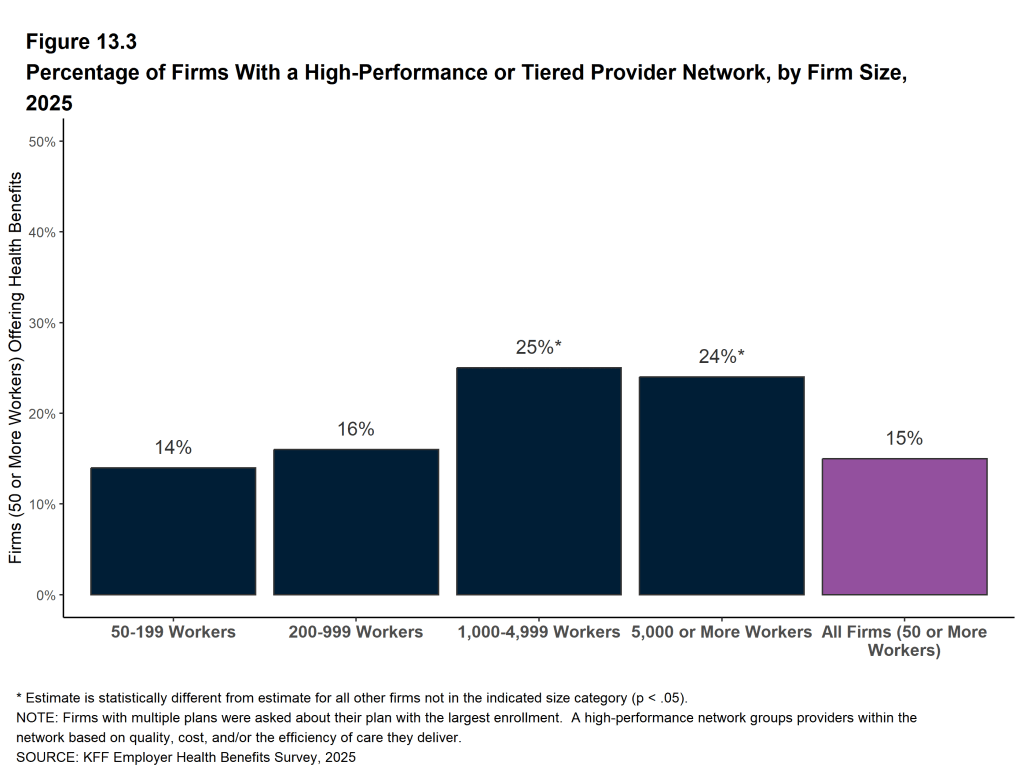
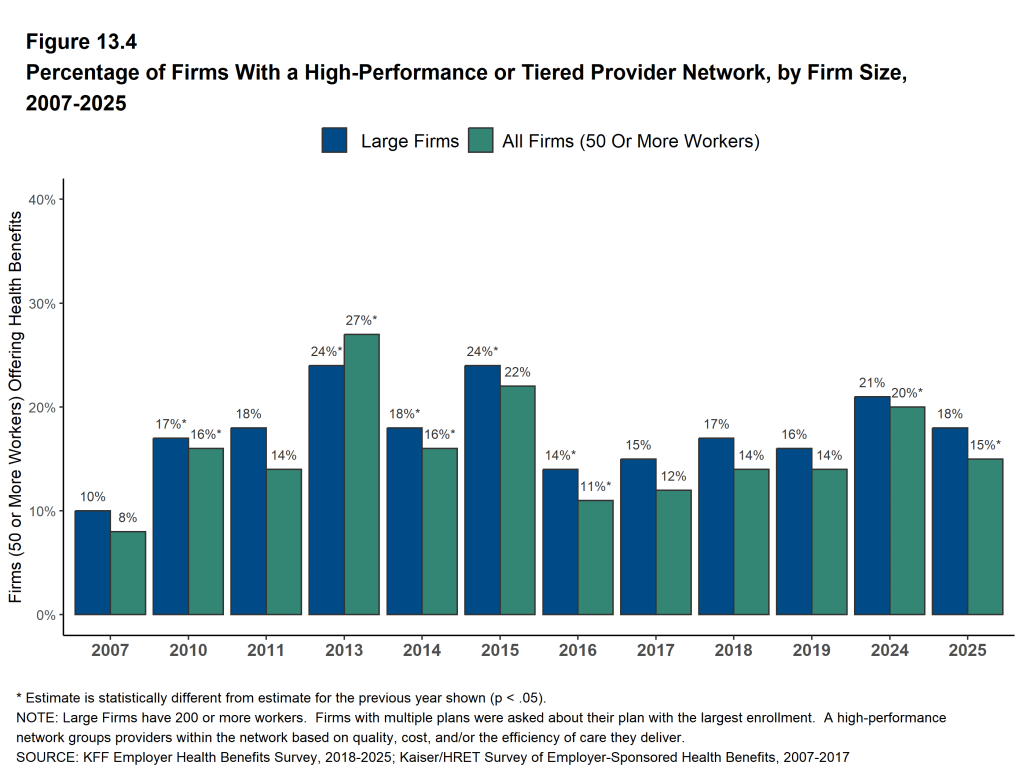
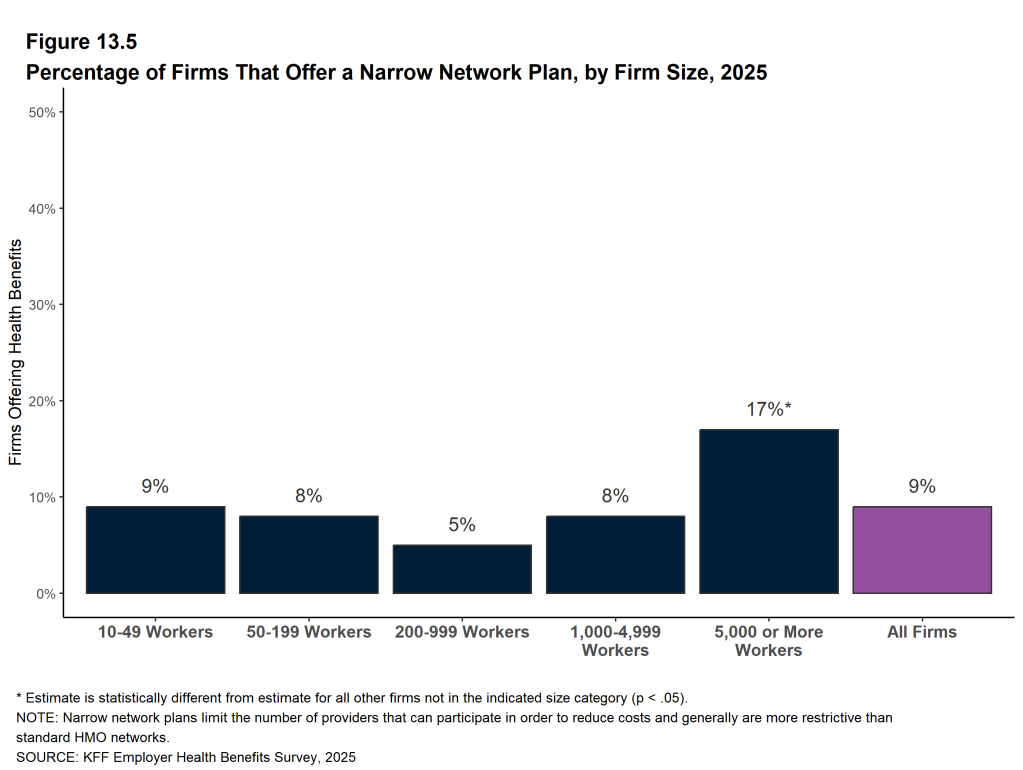
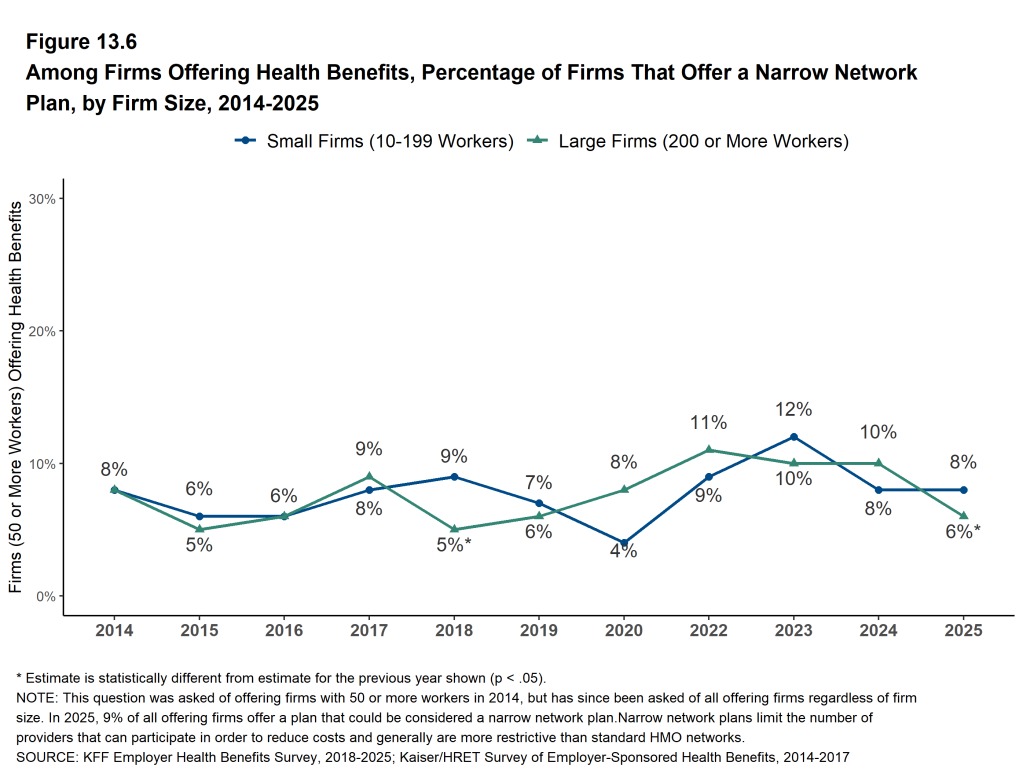
Tiered and Narrow Networks. Health plans structure their networks of providers to provide access to care and to encourage enrollees to use providers that are lower cost, or that provide better care. One option to accomplish these goals are high-performance or tiered network plans, which use cost-sharing or other incentives to encourage enrollees to certain in-network providers. Another option are narrow network plans, which significantly restrict the number of participating providers in order to reduce costs.
Among firms with 50 or more employees that offer health benefits, 15% have a high-performance network or tiered network as part of their health plan with the largest enrollment in 2025. Firms with 5,000 or more employees are more likely to include a high-performance or tiered network in their largest health plan than smaller employers (24% vs. 15%). Eight percent of firms with 50 or more employees that offer health benefits offer a health plan that can be considered a narrow network in 2025, similar to the percentage last year (8%). Firms with 5,000 or more employees are more likely to offer a narrow network plan than employers with fewer employees (17% vs. 8%) [Figure J].
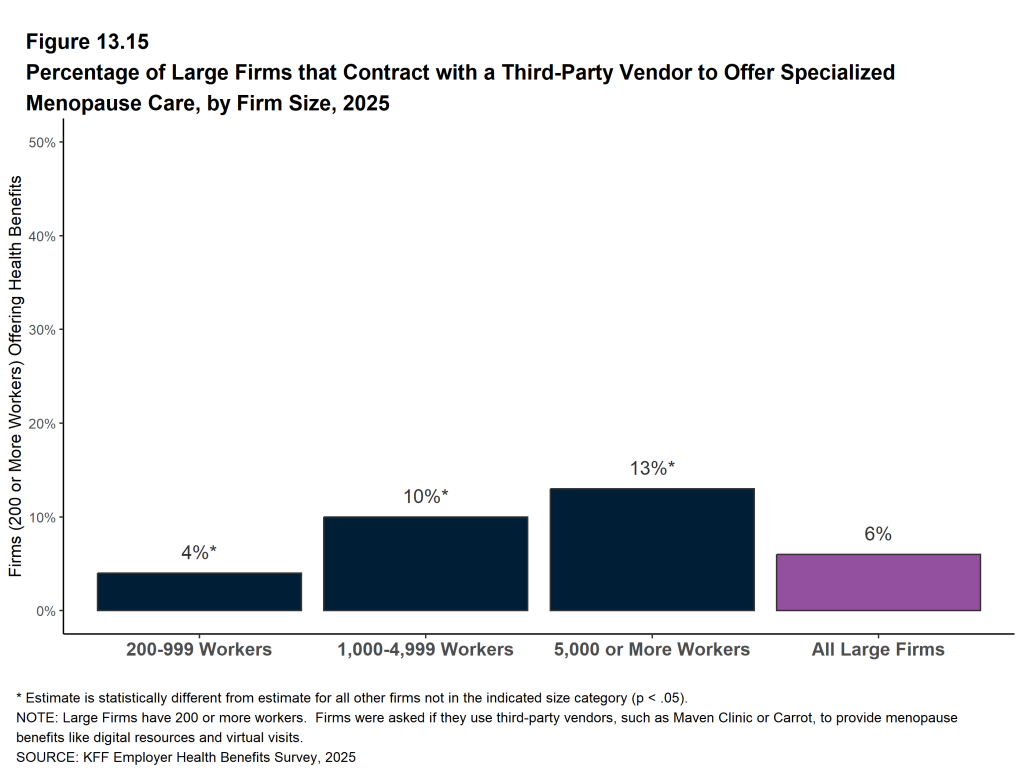
MENOPAUSE SUPPORT BENEFITS
Some employers contract with a vendor to offer specialized care or a virtual care benefit to provide support for enrollees during menopause. These services may include education, access to specialty care, and mental health support. Among employers with 200 or more workers that offer health benefits, 4% of firms with 200 to 999 workers, 10% of firms with 1,000 to 4,999 workers, and 13% of firms with 5,000 or more workers have vendor contracts to provide support for workers or their dependents during menopause [Figure J].
Figure J: Percentage of Large Firms With Various Network Strategies, 2025
APPROACHES TO PRIMARY CARE
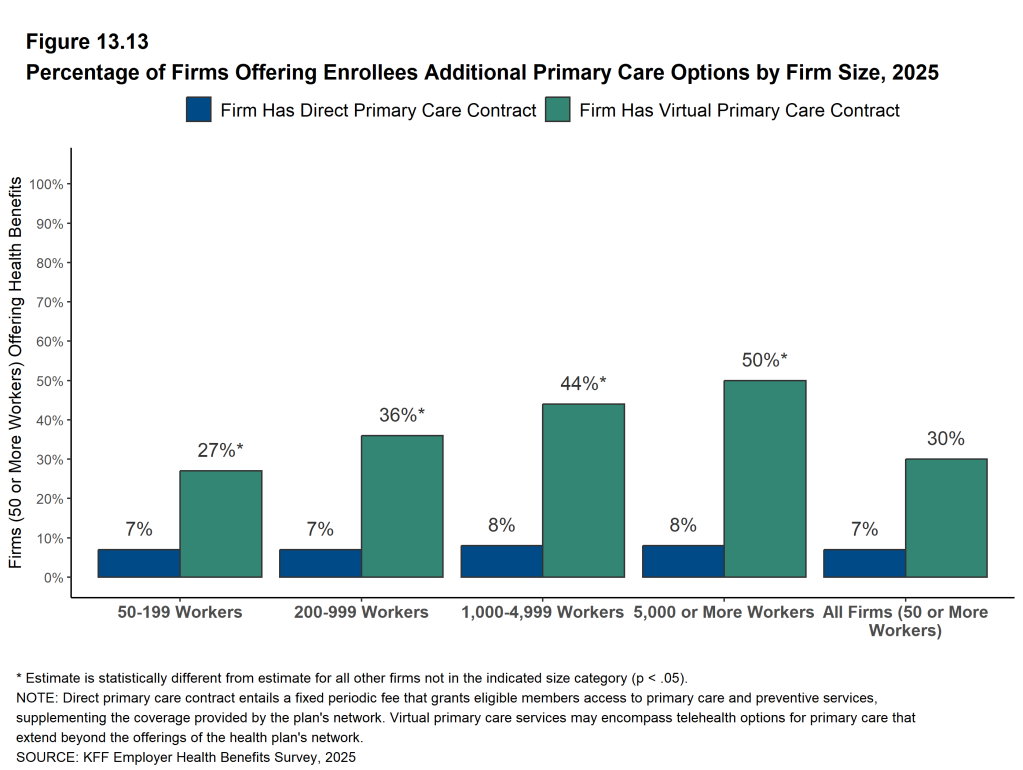
Some employers are using alternative approaches to provide primary care options for their workers. These include approaches using virtual care and direct contracts with networks of primary care providers. Among firms with 50 or more workers that offer health benefits, 30% have a contract to provide virtual primary care services, including telehealth primary care options, that go beyond the services provided to workers in their health plan networks. Firms with 1,000 or more workers are more likely than smaller firms to have a contract for virtual primary care services (45% vs. 29%).
Seven percent of firms with 50 or more workers that offer health benefits contract directly with an organization to provide primary care services to their workers in addition to the primary care providers offered through their health plan networks. The percentage is similar for smaller and larger firms [Figure J].
ICHRA AND ASSISTING EMPLOYEES WITH PURCHASING COVERAGE IN THE NON-GROUP MARKET
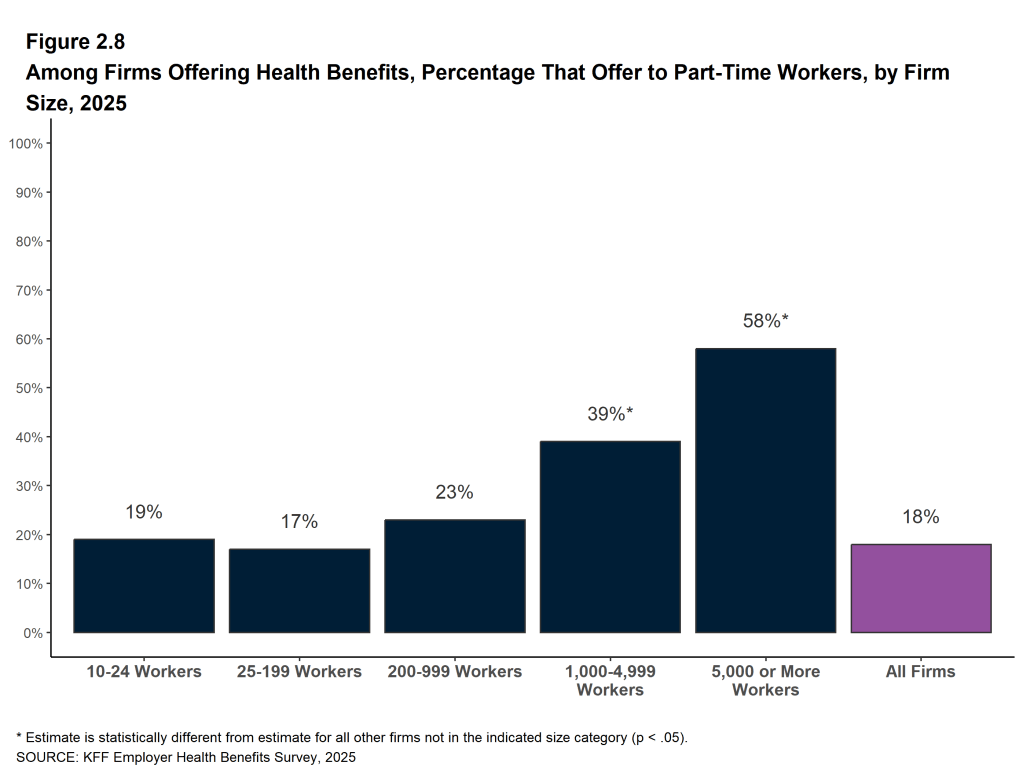
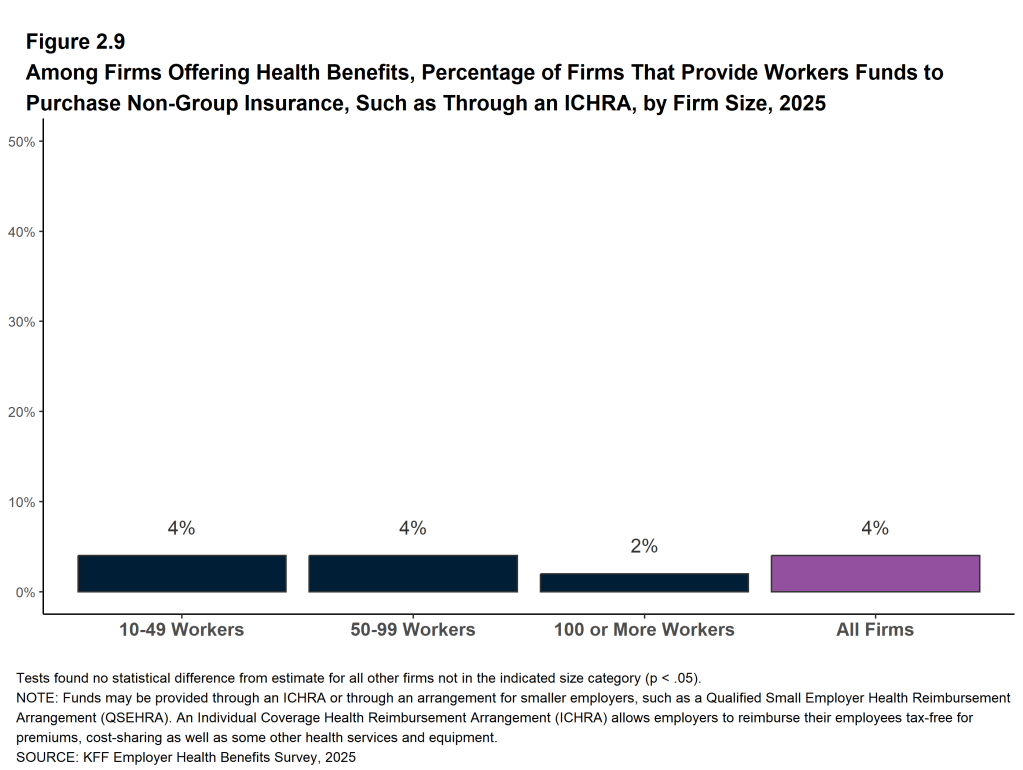
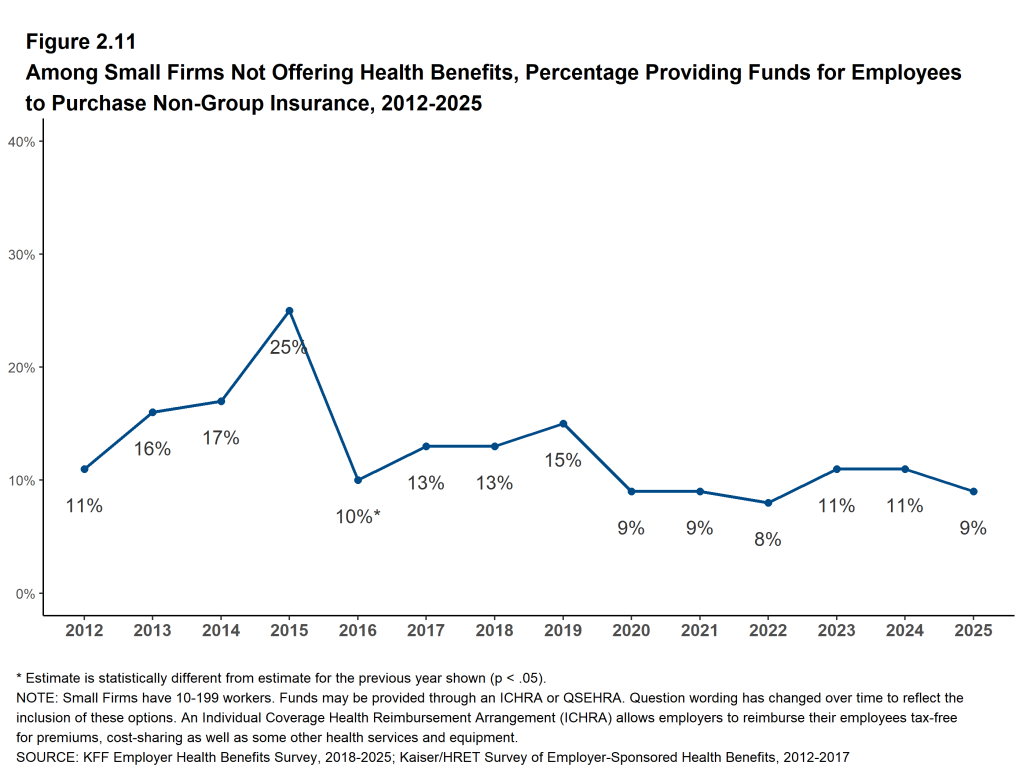
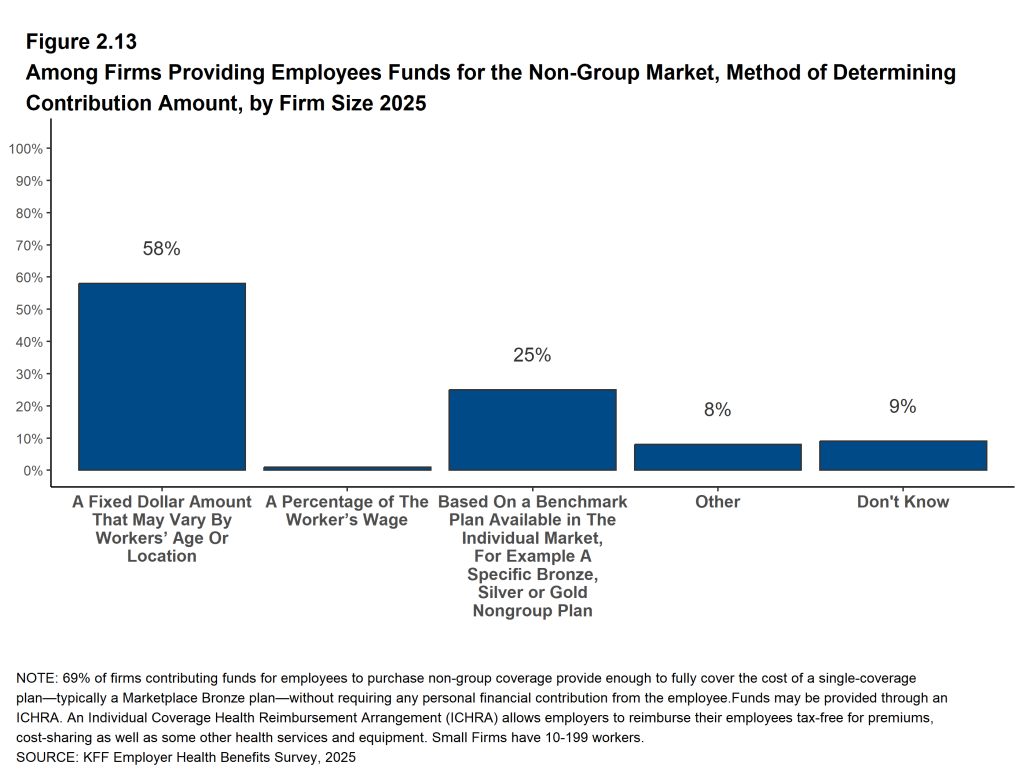
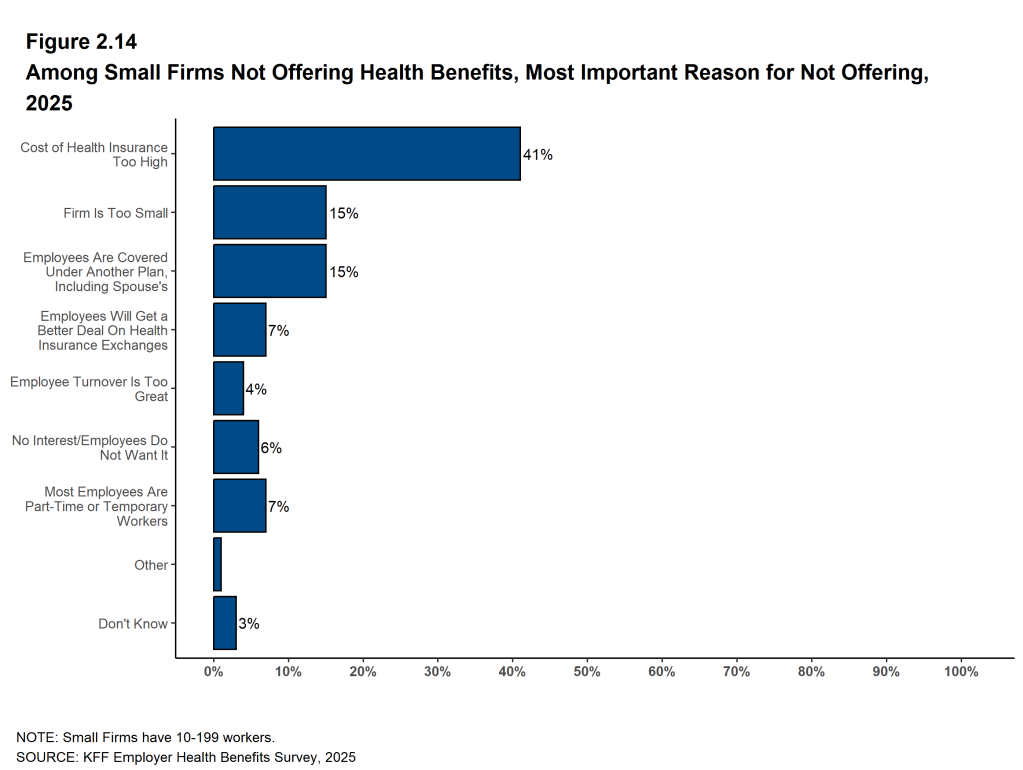
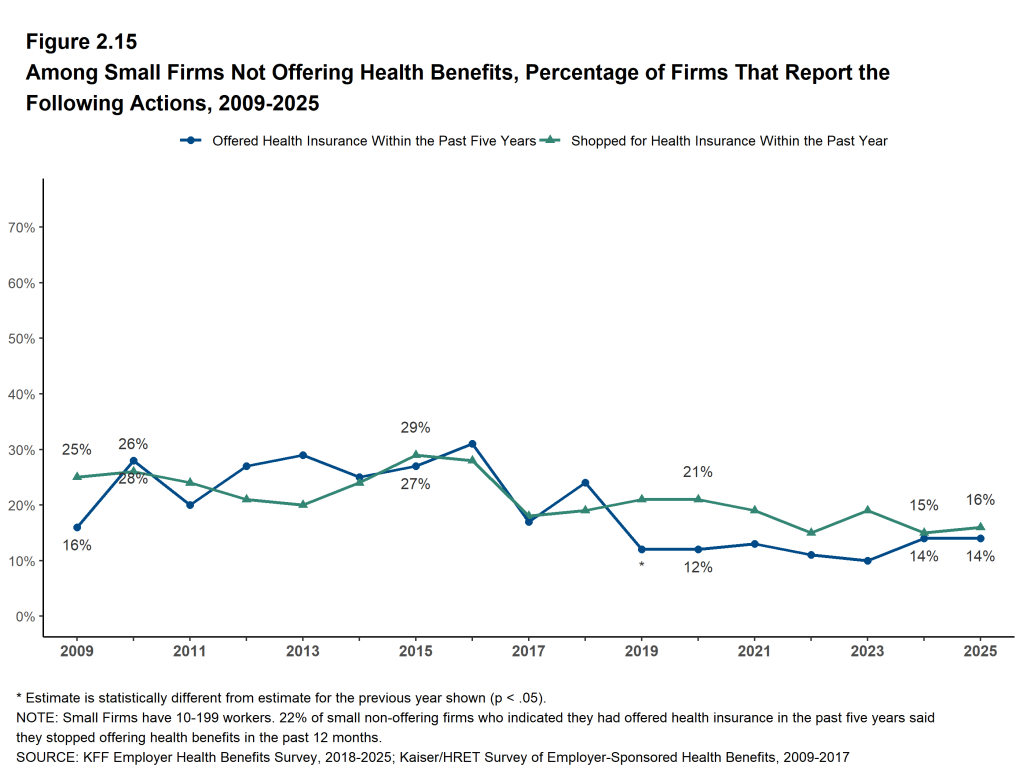
Some employers provide funds to some or all of their employees to help them purchase coverage in the individual (“non-group”) market. Employers that do not otherwise offer health benefits may offer these funds as an alternative to offering a group plan. Additionally, employers that offer a group plan to some employees may use this approach for other types or classes of workers, such as those working part time or remotely. One way an employer can provide tax-preferred assistance for employees to purchase non-group coverage is through an Individual Coverage Health Reimbursement Arrangement, or ICHRA. In 2025, 4% of firms that offer health benefits and 9% of firms that do not offer health benefits offered funds to one or more of their employees to purchase non-group coverage.
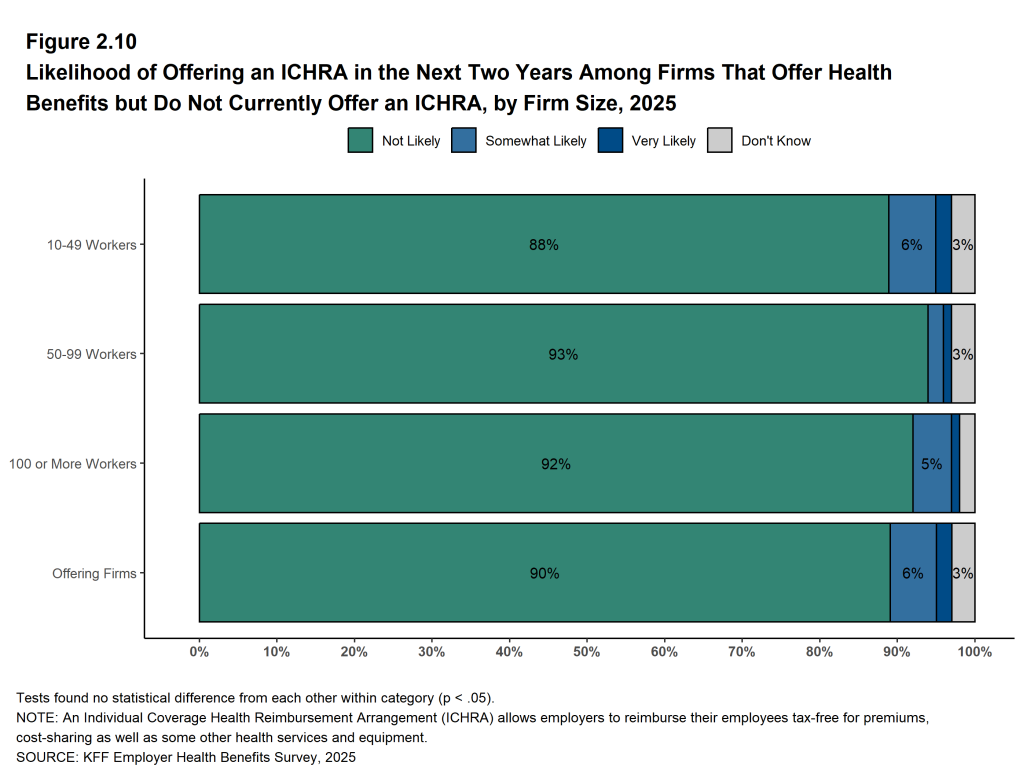
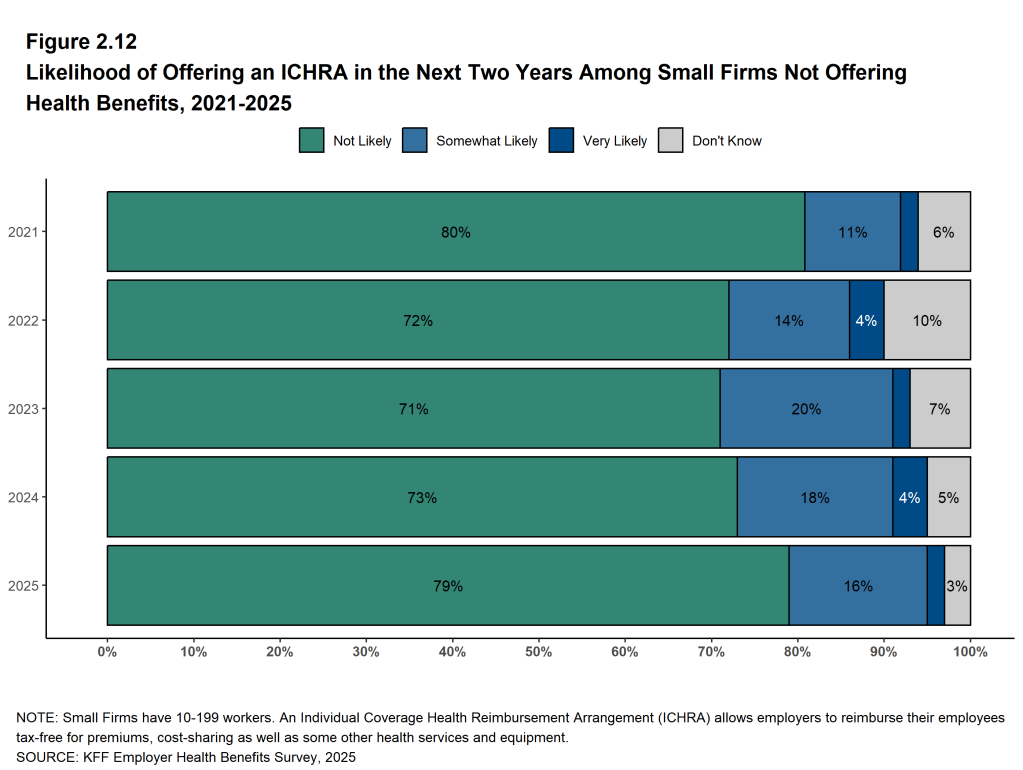
Modest shares of employers not currently offering an ICHRA option are considering doing so in the near future. Among firms with 10 or more workers that offer health benefits, 2% say they are “very likely” and an additional 6% are “somewhat likely” to offer an ICHRA to at least some employees in the next two years. Among firms with 10 to 199 workers that do not offer health benefits, 2% say they are “very likely” and an additional 16% say they are “somewhat likely” to offer an ICHRA to at least some employees in the next two years.
DISCUSSION
Average annual premiums increased by 5% for single coverage and 6% for family coverage in 2025, similar to the rate of growth over the past two years. Over the last five years, average family premiums have risen 26%, roughly in line with the cumulative increase in inflation (23.5%) and wage growth (28.6%) over the same period.
Early reports suggest that cost trends will be higher for 2026, potentially leading to higher premium increases unless employers and plans find ways to offset higher costs through changes to benefits, cost sharing, or plan design. One place where this story is playing out is coverage of GLP-1 agonists for weight loss. The share of the largest firms covering these medications for weight loss increased significantly in 2025, but many of these firms also reported higher than expected use, as well as a significant impact on prescription costs. Discussions with individual employers suggest that some have stopped covering these medications for weight loss, with a few even tightening up coverage for those with diabetes. While concerns over the negative health impacts of obesity remain, they are now in competition with concerns about the high cost and proper use of GLP-1 agonist medications, particularly at a time when other cost pressures may be growing. Whether and how to provide coverage for GLP-1 agonists will continue to be an important topic for employers and workers over the next few years.
Another potential strategy for managing rising costs is to increase employee cost sharing. While key measures such as the average deductible have grown more modestly in recent years, continued premium growth could prompt employers to raise out-of-pocket amounts for workers. Yet many may feel constrained in doing so; nearly half of large employers report that their employees have “high” or “moderate” concern about current cost-sharing levels. Many covered workers already face substantial cost-sharing, for example more than one-third of covered workers are enrolled in a plan with a deductible of $2,000 or more for single coverage.
METHODOLOGY
The KFF 2025 Employer Health Benefits Survey reports findings from a survey of 1,862 randomly selected non-federal public and private employers with ten or more workers. Davis Research, LLC conducted the field work between January and July 2025. The overall response rate is 13%, which includes firms that offer and do not offer health benefits. Unless otherwise noted, differences referred to in the text and figures use the 0.05 confidence level as the threshold for significance. Small firms have 10-199 workers unless otherwise noted. Values below 3% are not shown on graphs to improve readability. Some distributions may not sum due to rounding. For more information about survey methodology, see the Survey Design and Methods section at https://kff.org/ehbs.
Filling the need for trusted information on national health issues, KFF is a nonprofit organization based in San Francisco, California.
- KFF’s analysis of data from the 2023 American Community Survey. See KFF. Health insurance coverage of the population ages 0–64 [Internet]. San Francisco (CA): KFF; [cited 2025 Sep 15]. [Time frame: 2023]. Available from: https://www.kff.org/state-health-policy-data/stateindicator/health-insurancecoverage-population-0-64/↩︎
- Bureau of Labor Statistics, Mid-Atlantic Information Office. Consumer Price Index historical tables for U.S. city average (1967=100), Consumer Price Index for All Urban Consumers (CPI-U) (not seasonally adjusted) [Internet]. Philadelphia (PA): BLS, Mid-Atlantic Information Office; [cited 2025 Sep 15]. Available from: https://www.bls.gov/regions/mid-atlantic/data/consumerpriceindexhistorical1967base_us_table.htm↩︎
- Average hourly earnings of production and nonsupervisory employees (seasonally adjusted) from the Current Employment Statistics survey. See Bureau of Labor Statistics. Current Employment Statistics—CES (national) [Internet]. Washington (DC): BLS; [cited 2025 Sep 15]. Available from: https://www.bls.gov/ces/data/↩︎
- This threshold is based on the twenty-fifth percentile of workers’ earnings ($37,000 in 2025). Seasonally adjusted data from the Current Employment Statistics Survey. Bureau of Labor Statistics. Current Employment Statistics—CES (national) [Internet]. Washington (DC): BLS. Available from: https://www.bls.gov/ces/publications/highlights/highlights-archive.htm↩︎
Survey Design and Methods
KFF has conducted this annual survey of employer-sponsored health benefits since 1999. Since 2020, KFF has employed Davis Research LLC (Davis) to field the survey. From January to July 2025, Davis interviewed business owners as well as human resource and benefits managers at 1,862 firms.
SURVEY TOPICS
The survey includes questions on the cost of health insurance, offer rates, coverage, eligibility, plan type enrollment, premium contributions, employee cost sharing, prescription drug coverage, retiree health benefits, and wellness programs.
Firms that offer health benefits are asked about the attributes of their largest HMO, PPO, POS and HDHP/SO plans. Exclusive provider organizations (EPOs) are grouped with HMOs, and conventional (or indemnity) plans are grouped with PPOs.
Plan Definitions:
- HMO (Health Maintenance Organization): A plan that does not cover non-emergency services provided out of network.
- PPO (Preferred Provider Organization): A plan that allows use of both in-network and out-of-network providers, with lower cost sharing for in-network services and no requirement for a primary care referral.
- POS (Point-of-Service Plan): A plan with lower cost sharing for in-network services, but that requires a primary care gatekeeper for specialist or hospital visits.
- HDHP/SO (High-Deductible Health Plan with a Savings Option): A plan with a deductible of at least $1,000 for single coverage or $2,000 for family coverage, paired with either a health reimbursement arrangement (HRA) or a health savings account (HSA). While HRAs can be offered with non-HDHPs, the survey collects data only on HRAs paired with HDHPs. (See the introduction to Section 8 for more detail on HDHPs, HRAs, and HSAs.)
To reduce respondent burden, questions on cost sharing for office visits, hospitalization, outpatient surgery, and prescription drugs are limited to the firm’s largest plan. Firms offering multiple plan types report premium contributions and deductibles for their two largest plans. Within each plan type, respondents are asked about the plan with the highest enrollment.
Firms report attributes of their current plans as of the time of the interview. While the survey fielding begins in January, many firms have plan years that do not align with the calendar year. In some cases, firms may report data based on the prior year’s plan. As a result, some reported attributes—such as HSA deductible thresholds—may not align with current regulatory requirements. Additionally, plan decisions may have been made months prior to the interview.
SAMPLE DESIGN
The sample for the annual KFF Employer Health Benefits Survey includes private firms and nonfederal government employers with ten or more employees. The universe is defined by the U.S. Census’ 2021 Statistics of U.S. Businesses (SUSB) for private firms and the 2022 Census of Governments (COG) for non-federal public employers. At the time of sample design (December 2024), this data represented the most current information on the number of public and private firms. The sample size is determined based on the number of firms needed to achieve a target number of completes across five firm-size categories and whether the firm was located in California.
We attempted to re-interview prior survey respondents who participated in either the 2023 or 2024 survey, or both. In total,* 186 firms participated in 2023,* 423 firms participated in 2024, and* 693 firms participated in both years.
Non-panel firms were randomly selected within size and industry groups.
Since 2010, the sample has been drawn from a Dynata list (based on a census compiled by Dun & Bradstreet) of the nation’s private employers, and from the COG for public employers. Starting in 2025, we included an augmented sample of 50 firms from the Forbes America’s Largest Private Companies list. This list includes U.S.-based firms with annual revenue of $2 billion or more and is intended to complement the Dynata sample frame.
To increase precision, the sample is stratified by ten industry categories and six size categories. Education is treated as a separate category for sampling but included in the “Service” category for weighting.
For more information on changes to sampling methods over time, please consult the extended methods (https://kff.org/ehbs) which describes changes made in each year’s survey.
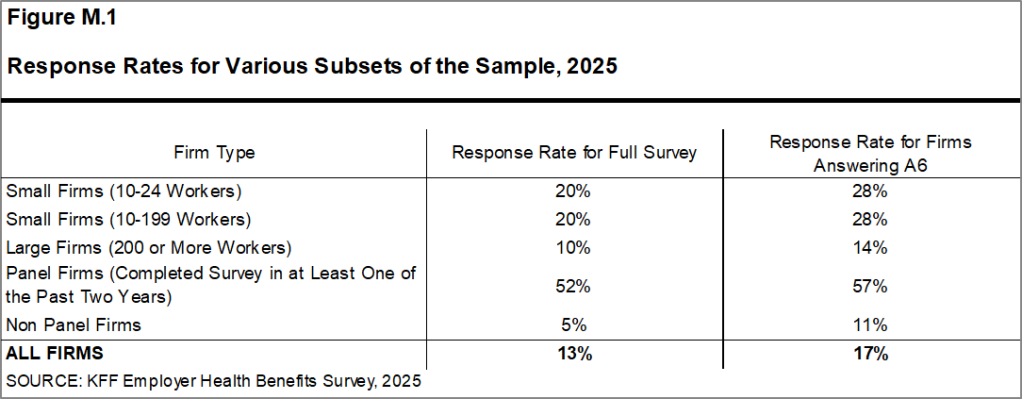
RESPONSE RATE
Response rates are calculated using a CASRO method, which accounts for firm eligibility in the study. The rate is computed by dividing the number of completes by the sum of refusals and the estimated number of eligible firms among those with unknown eligibility. The overall response rate is 13% [Figure M.1]. As in prior years, the response rate for panel firms is higher than for non-panel firms.
Similar to other employer and household surveys, response rates have declined over time. Since 2017, we have attempted to increase the number of completes by expanding the number of non-panel firms in the sample. While this strategy improves the precision of estimates—particularly for subgroups—it tends to reduce the overall response rate.
Most survey questions are asked only of firms that offer health benefits. A total of 1,610 of the 1,862 firms responding to the full survey indicated that they offer health benefits.
We asked one question of all firms we contacted by phone, even if they declined to complete the full survey: “Does your company offer a health insurance program as a benefit to any of your employees?” A total of 2,560 firms responded to this question, including 1,862 full survey respondents and 698 firms who responded to this question only.
These responses are included in the estimates of the percentage of firms offering health benefits presented in Chapter 2. The response rate for this question is 17.4% [Figure M.1].
Figure M.1: Response Rates for Various Subsets of the Sample, 2025
While response rates have decreased, elements of the survey design limit the potential impact of a response bias. Most major statistics are weighted by the number of covered workers at a firm. Collectively, 3,600,000 of the 67,600,000 workers covered by their own employer’s health benefits nationwide were employed at firms that completed the survey. The most important statistic weighted by the number of employers is the offer rate. Firms that do not complete the full survey are still asked whether they offer health benefits, ensuring a larger sample. As in previous years, most responding firms are very small. As a result, fluctuations in the offer rate for these small firms significantly influence the overall offer rate.
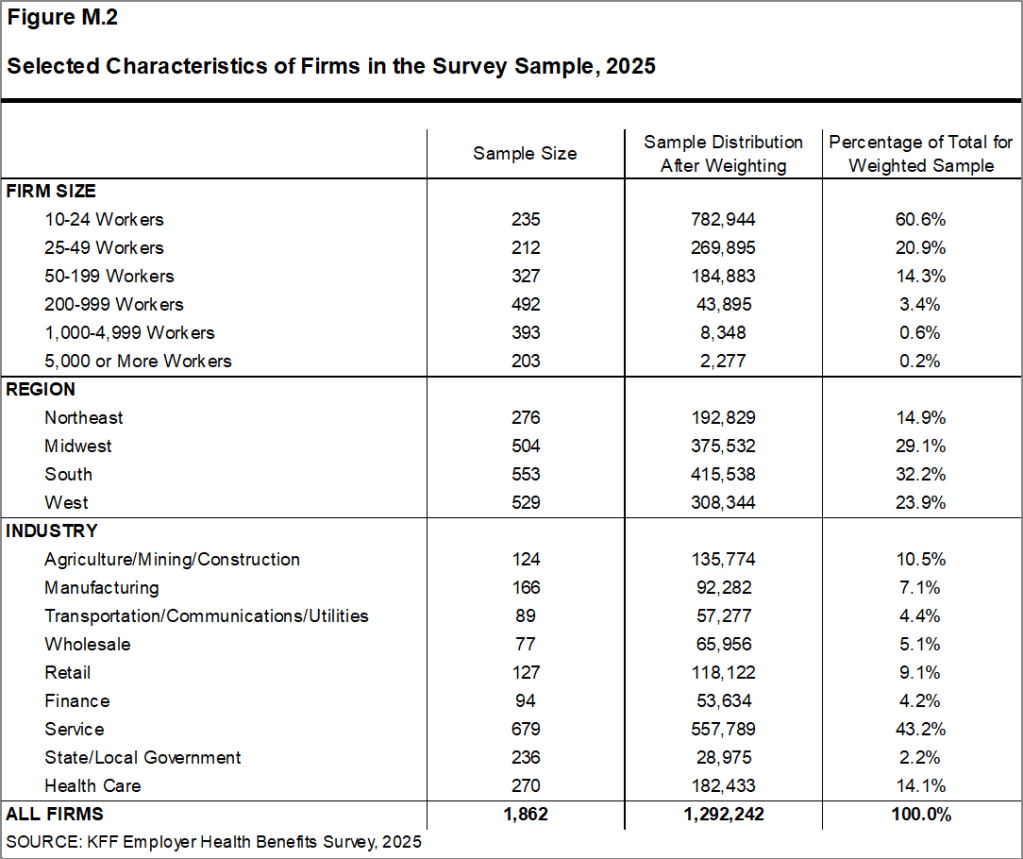
FIRM SIZES AND KEY DEFINITIONS
Throughout the report, we present data by firm size, region, and industry; [Figure M.2] displays selected characteristics of the sample. Unless otherwise noted, firm size is defined as follows: small firms have 10-199 workers, and large firms have 200 or more workers.
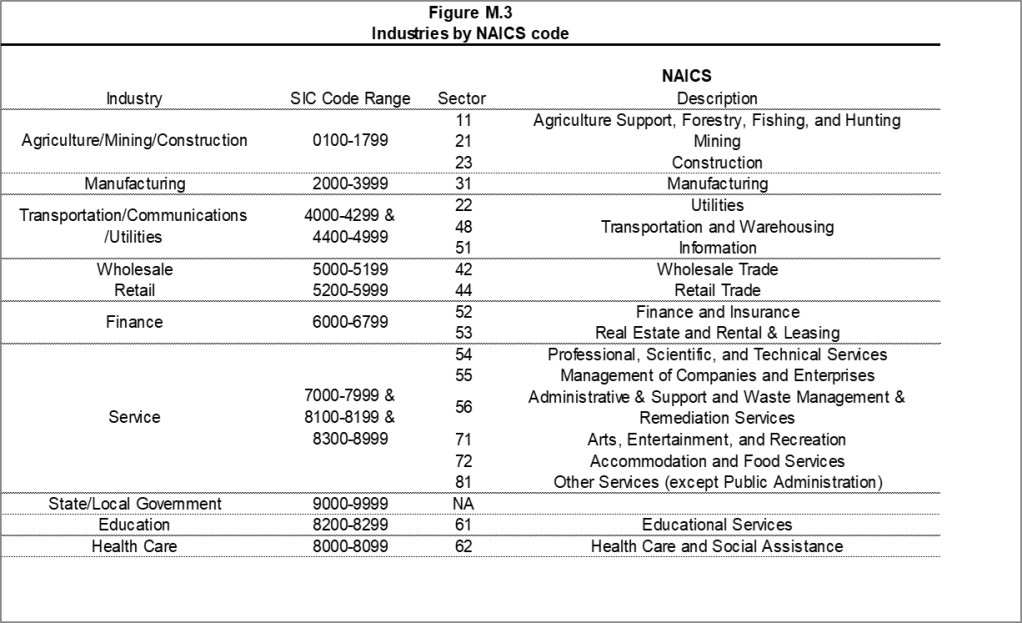
A firm’s primary industry classification is based on Dynata’s designation, which in turn is derived from the U.S. Census Bureau’s North American Industry Classification System (NAICS) [Figure M.3]. Firm ownership type, average wage level, and workforce age are based on respondents’ self-reported information.
While there is considerable overlap between firms categorized as “State/Local Government” in the industry classification and those identified as publicly owned, the two categories are not identical. For example, public school districts are included in the “Service” industry category, even though they are publicly owned.
Family coverage is defined as health insurance coverage for a family of four.
Figure M.2: Selected Characteristics of Firms in the Survey Sample, 2025
Figure M.3: Industries by NAICS code
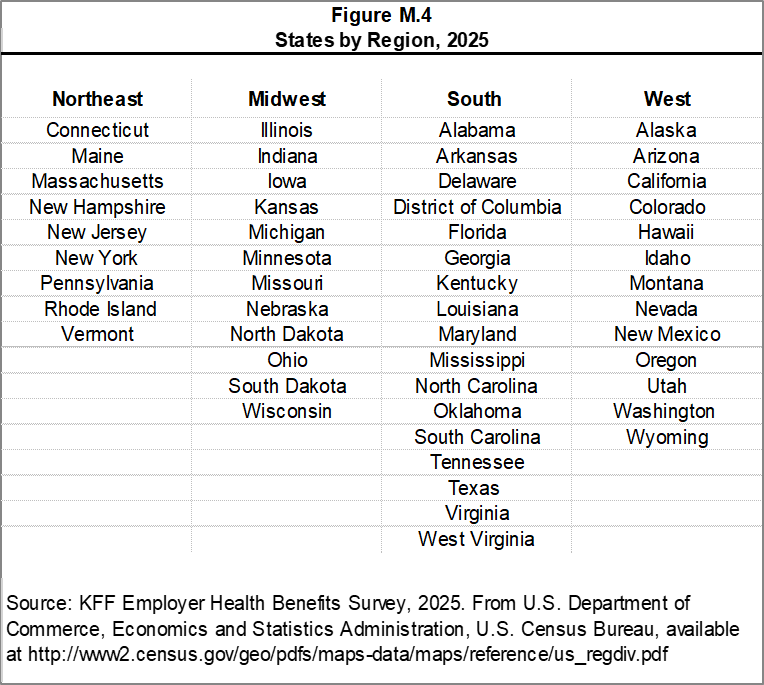
[Figure M.4] shows the categorization of states into regions, based on the U.S. Census Bureau’s regional definitions. State-level data are not reported due to limited sample sizes in many states and because the survey collects information only on a firm’s primary location—not where employees may be based. Some mid-size and large employers operate in multiple states, so the location of a firm’s headquarters may not correspond to the location of the health plan for which premium information was collected.
Figure M.4: States by Region, 2025
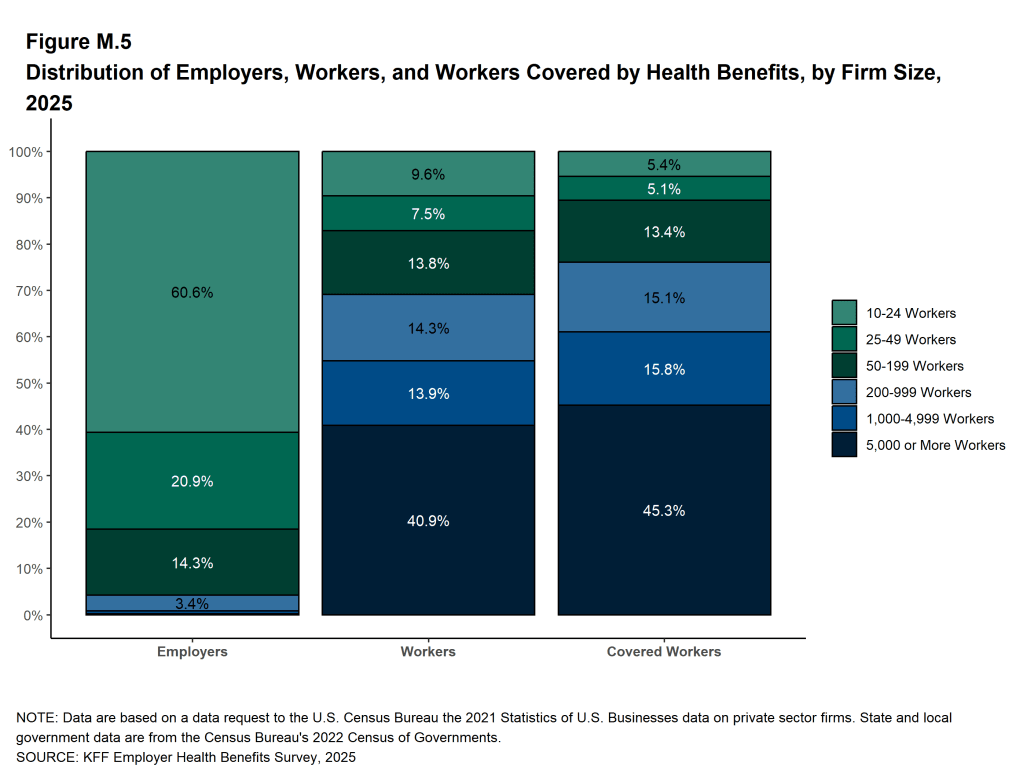
[Figure M.5] displays the distribution of the nation’s firms, workers, and covered workers (employees receiving health coverage from their employer). Beginning in 2025, firms with fewer than 10 employees were excluded from the survey universe. Although most firms in the United States are small, most workers covered by health benefits are employed at large firms: 76% of the covered worker weight is controlled by firms with 200 or more employees. Conversely, firms with 10-199 employees represent 96% percent of the employer weight.
Because small firms make up the vast majority of all firms, they heavily influence statistics weighted by the number of employers. For this reason, most firm-level statistics are reportedc by firm size. In contrast, large firms—especially those with 1,000 or more workers—have the greatest influence on statistics related to covered workers. Even with the large firm category (those with 200 or more workers), 81% of the employer weight is driven by firms with 200-999 employees.
Statistics for small firms and employer-weighted measures tend to exhibit greater variability.
Figure M.5: Distribution of Employers, Workers, and Workers Covered by Health Benefits, by Firm Size, 2025
The survey asks firms what percentage of their employees earn more or less than a specified amount in order to identify the portion of the workforce that has relatively lower or higher wages. This year, the income threshold is $37,000 or less per year for lower-wage workers and $80,000 or more for higher-wage workers. These thresholds are based on the 25th and 75th percentile of workers’ earnings as reported by the Bureau of Labor Statistics using data from the Occupational Employment Statistics (OES) (2023).5 The cutoffs were inflation-adjusted and rounded to the nearest thousand.
Annual inflation estimates are calculated as an average of the first three months of the year. The 12 month percentage change for this period was 2.7%.6 Data presented is nominal unless indicated specifically otherwise.
ROUNDING AND IMPUTATION
Some figures may not sum to totals due to rounding. While overall totals and totals by firm size and industry are statistically valid, some breakdowns are not reported due to limited sample sizes or high relative standard errors. Where the unweighted sample size is fewer than 30 observations, figures are labeled “NSD” (Not Sufficient Data). Estimates with high relative standard errors are reviewed and, in some cases, suppressed. Many subset estimates may have large standard errors, meaning that even large differences between groups may not be statistically significant.
To improve readability, values below 3% are not shown in graphical figures. The underlying data for all estimates presented in graphs are available in Excel files accompanying each section at https://kff.org/ehbs.
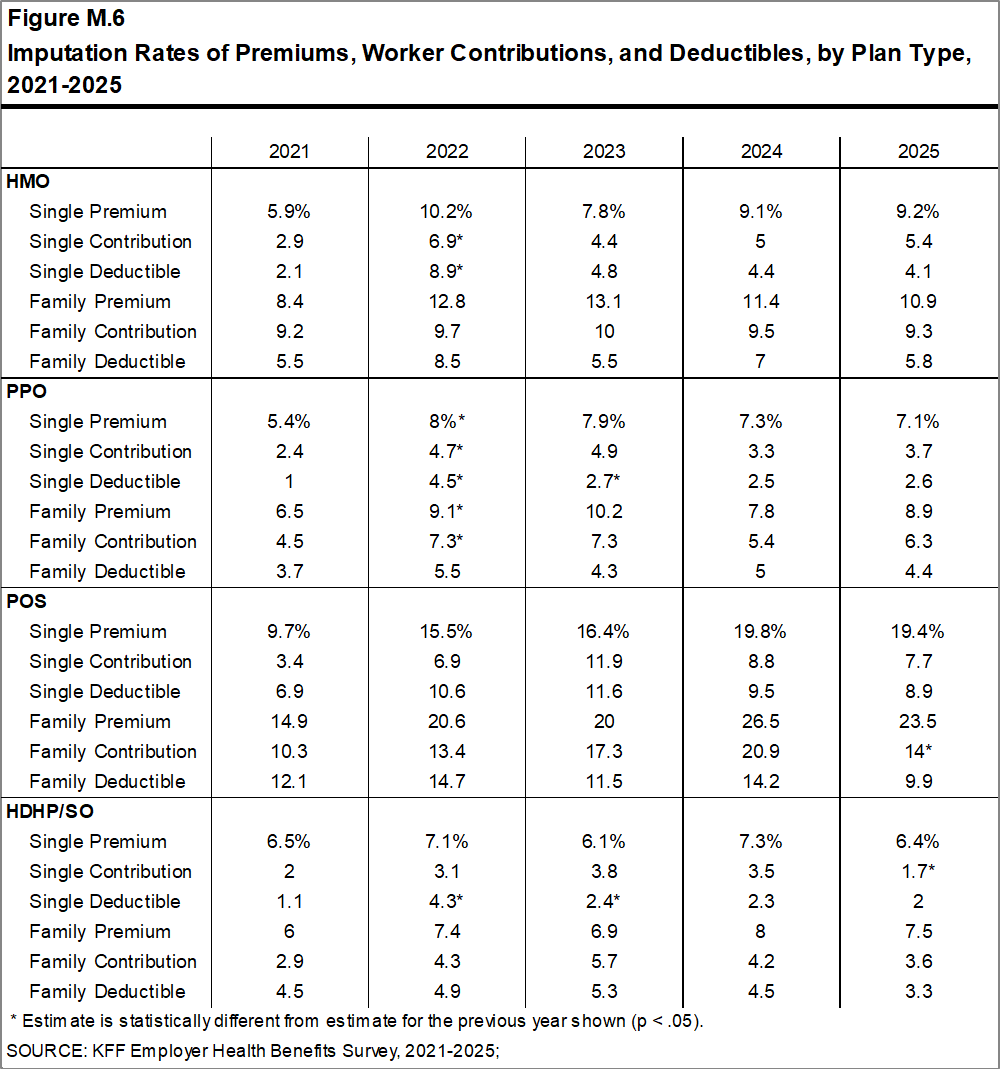
To control for item nonresponse bias, we impute missing values for most variables. On average, 10% of observations are imputed. All variables—except single coverage premiums—are imputed using a hotdeck method, which replaces missing values with observed values from a similar firm (based on size and industry).
When both single and family coverage premiums are missing for a firm, the single coverage premium is first predicted using a random forest algorithm based on other known plan and firm characteristics. This predicted value is then used to impute related variables, such as family premiums and worker contributions, using the hotdeck approach. Some variables are hotdecked based on their relationship to another variable. For example, if a firm reports a family worker contribution but not a family premium, we impute a ratio between the two and then calculate the missing premium.
In 2025, there were forty-six variables where the imputation rate exceeded 20%, most of which were related to plan-level statistics. When constructing aggregate estimates across all plans, the imputation rate is typically much lower. A few variables are not imputed—these are usually cases where a “don’t know” response is considered valid.
To ensure data quality, we conduct multiple reviews of outliers and illogical responses. Each year, several hundred firms are recontacted to verify or correct their responses. In some cases, responses are edited based on open-ended comments or established logic rules.
Figure M.6: Imputation Rates of Premiums, Worker Contributions, and Deductibles, by Plan Type, 2021-2025
WEIGHTING
Because we select firms randomly, it is possible through the use of weights to extrapolate results to national (as well as firm size, regional, and industry) averages. These weights allow us to present findings based on the number of workers covered by health plans, the number of workers, and the number of firms. In general, findings in dollar amounts (such as premiums, worker contributions, and cost sharing) are weighted by covered workers. Other estimates, such as the offer rate, are weighted by firms.
The employer weight was determined by calculating the firm’s probability of selection. This weight was trimmed of overly influential weights and calibrated to U.S. Census Bureau’s 2021 Statistics of U.S. Businesses for firms in the private sector, and the 2022 Census of Governments totals. The worker weight was calculated by multiplying the employer weight by the number of workers at the firm and then following the same weight adjustment process described above. The covered-worker weight and the plan-specific weights were calculated by multiplying the percentage of workers enrolled in each of the plan types by the firm’s worker weight. These weights allow analyses of workers covered by health benefits and of workers in a particular type of health plan.
The trimming procedure follows the following steps: First, we grouped firms into size and offer categories of observations. Within each strata, we calculated the trimming cut point as the median plus six times the interquartile range (M + [6 * IQR]). Weight values larger than this cut point are trimmed. In all instances, very few weight values were trimmed.
To account for design effects, the statistical computing package R version 4.5.1 (2025-06-13 ucrt) and the library “survey” version 4.4.8 were used to calculate standard errors.
STATISTICAL SIGNIFICANCE AND LIMITATIONS
All statistical tests are performed at the 0.05 confidence level. For figures spanning multiple years, comparisons are made between each year and the previous year shown, unless otherwise noted. No statistical tests are conducted for years prior to 1999.
Subgroup comparisons are made against all other firm sizes not included in the specified group. For example, firms in the Northeast are compared to an aggregate of firms in the Midwest, South, and West. For plan type comparisons (e.g., average premiums in PPOs), results are tested against the “All Plans” estimate. In some cases, plan-specific estimates are also compared to similar estimates for other plan types (e.g., single and family premiums in HDHP/SOs vs. HMO, PPO, and POS plans); such comparisons are noted in the text.
Two statistical tests are used: the t-test and the Wald test. A small number of observations for certain variables can result in large variability around point estimates. Readers should be cautious of these when interpreting year-to-year changes, as large shifts may not be statistically significant. Standard errors for selected estimates are available in a technical supplement at http://ehbs.kff.org.
Due to the complexity of many employer health benefit programs, the survey may not capture all elements of any given plan. For instance, employers may offer intricate and varying prescription drug benefits, premium contributions, or wellness incentives. Interviews were conducted with the individual most knowledgeable about the firm’s health benefits, though some respondents may not have complete information on all aspects of the plan. While the survey collects data on the number of workers enrolled in coverage, it does not capture the characteristics of those offered or enrolled in specific plans.
DATA COLLECTION AND SURVEY MODE
Starting in 2022, we expanded the use of computer assisted web interview (CAWI), offering most respondents the opportunity to complete the survey using an online questionnaire rather a telephone interview. In 2025, fifty-seven percent of survey responses were completed via telephone interview, and the remainder were completed online. Previous analysis has found that survey mode had little impact on major statistics such as annual premiums, contributions, and deductibles.
Preferred Reporting Items for Complex Sample Survey Analysis (PRICSSA)
In their Journal of Survey Statistics and Methodology article, Seidenberg, Moser, and West (2023) propose a checklist for survey administrators and sponsoring organizations to help external researchers quickly understand the methods used to create a complex sample dataset.7 The Preferred Reporting Items for Complex Sample Survey Analysis (PRICSSA) recommends a standard format to enumerate data collection and analysis techniques across a variety of different surveys. KFF has adopted this checklist to increase transparency for our readership and also to promote reproducibility among external researchers granted access to our public use files.
- 1.1 Data collection dates: January 27, 2025-July 23, 2025.
- 1.2 Data collection mode(s): fifty-seven percent computer-assisted telephone interviewing (CATI), and the remainder completed with computer assisted web interview (CAWI).
- 1.3 Target population: Private firms as well as state and local government employers with ten or more employees in 50 US states and Washington DC.
- 1.4 Sample design: A sample stratified by ten industry categories and six size categories drawn from a Dynata list (based on a census assembled by Dun and Bradstreet) of the nation’s private employers and the Census of Governments for public employers.
- 1.5 Full Survey response rate: 13 percent (CASRO method).
- 2.1 Missingness rates: On average, 10% of observations are imputed.
- 2.2 Observation deletion: Observations found to be duplicated firms, out of business, or no longer exisiting in the sample universe.
- 2.3 Sample sizes: 1,862 firms completed the entire survey, 2,560 completed at least the offer question, out of 30,150 initially sampled firms, generalizing to a total of about one million firms.
- 2.4 Confidence intervals / standard errors: All statistical tests are performed at the .05 confidence level.
- 2.5 Weighting:
empwt(firms),empwt_a6(firms, including those answering only the offer question),wkrwt(workers),covwt(policyholders),hmowt,ppowt,poswt, andhdpwt(plan weights) - 2.6 Variance estimation: Taylor Series Linearization with
newcellused as the stratum variable but no PSU variable. - 2.7 Subpopulation analysis: The R
surveypackage toolkit such assvybyand a complex sample design’ssubsetmethod allowed for most analysis of subdomains. - 2.8 Suppression rules: Where the unweighted sample size is fewer than 30 observations, figures include the notation “NSD” (Not Sufficient Data). Estimates with high relative standard errors are reviewed and in some cases not published.
- 2.9 Software and code: All design-based analyses were performed using R version 4.5.1 (2025-06-13 ucrt) and
surveylibrary version 4.4.8.
2025 SURVEY
The 2025 survey includes new questions on primary care, menopause benefits, direct contracting, specialty networks, and transparency, among other topics. As in previous years, modifications were also made to existing questions to improve clarity and reflect changes in the health care marketplace.
California Oversample
In 2025, we fielded an oversample of California-based employers to generate separate state-level estimates for the CHCF/KFF California Employer Health Benefits Survey (CHBS). KFF and the California Health Care Foundation (CHCF) have previously included California-specific questions and an oversample of firms located in the state. The 2025 California Employer Health Benefits Survey will produce estimates comparable to those in the 2022 CHBS. Firms with workers in California are included in both the 2025 EHBS and CHBS. To ensure statistical reliability at both the national and state levels, firm weights for the California sample were calibrated to state-specific targets from the U.S. Census Bureau’s Statistics of U.S. Businesses (SUSB). All firms were asked about the characteristics of their workforce nationwide and if applicable in California.
Augmented Sample
Firms with 70,000 or more employees account for 14% of workers in the United States. As a result, the accuracy of estimates depends heavily on the participation of these large employers. In recent years, however, participation among the largest firms has declined. In 2014, survey respondents included firms of this size employing about 9% of the nation’s covered workforce; by 2024, this share had fallen to 4%. While the total number of responding firms has remained relatively stable, the survey now includes fewer firms that have large workforces. Although there are likely multiple reasons for the decline in participation among large firms, one potential concern is that these firms may be underrepresented in the sample frame.
To address this issue, beginning in 2025, we implemented an augmented sample drawn from the Forbes America’s Largest Private Companies list, which includes U.S.-based firms with annual revenues of $2 billion or more. This supplemental sample was designed to enhance representation of the largest employers and complement the primary Dynata sample frame. For this augmented sample, Davis Research conducted outreach to multiple individuals at each firm, targeting staff with human resources-related titles.
Exclusion of Firms with Fewer than 10 Employees
Beginning in 2025, the survey will no longer include firms with 3 to 9 employees. This change reflects longstanding challenges in surveying the smallest firms and their limited influence on national estimates. Although there are 1.95 million such firms in the U.S., they employ a very small share of the workforce and present significant methodological difficulties.
In 2024, only 151 firms in this size range responded to the survey, and just 29 reported offering health benefits. Due to their small numbers, each responding firm carried substantial weight in employer-level estimates—on average, offering firms with 3-9 employees were weighted 58 times more heavily than larger firms. As a result, a small number of responses have disproportionate influence on employer-weighted estimates, even though these firms often had more limited knowledge of their health plans. The response rate for offering firms in this group was also significantly lower than the overall rate (6.5% vs. 14%).
At the same time, these firms have minimal impact on most covered worker-weighted estimates, such as premiums, contributions, deductibles and other cost-sharing. For example, the average family premium when including versus excluding 3-9 employee firms in 2024 differed by only $13 because they account for just 3.7% of all covered workers. For more information on the sample distribution and responses rates including firms with 3 to 9 employees see the 2024 methods section.
Given these factors — low response rates, high variability, and limited influence on key national estimates — firms with fewer than 10 employees were removed from the sample universe starting in 2025.
This change most directly affects the firm offer rate. In 2024, the offer rate among firms with 10 or more employees was 65% compared to 54% among firms with 3 or more employees. While this adjustment reduces insight into the smallest firms, it improves the precision and reliability of estimates for the remaining sample universe.
Decline in Single-Question A6 Firm Counts
After fielding the 2025 survey, we discovered a skip pattern mistake that led to a sharp reduction in the number of firms refusing the full survey but responding to the question “Does your company offer a health insurance program as a benefit to any of your employees?” In the past few years, more than 2,000 firms have answered only this question but not the full survey; however, the error reduced this segment’s 2025 unweighted sample to only about 700 firms. Although this oversight decreased the precision of our 2025 offer rate estimates, we reviewed the questionnaire pathways and do not believe to have introduced bias in the manner of data collection. Both including and excluding these additional firms yielded the same percentage point estimates both last year and this year: 65% in 2024 and 61% in 2025. This oversight also reduced our 2025 combined response rate to 17% compared to 30% last year, since fewer eligible firms were given an opportunity to answer this standalone question. (The 2024 Table M.1 shows 31% including firms with 3-9 employees.) We expect to remedy this issue in the 2026 setup and hope to collect single-question information from a larger pool of firms as consistent with recent years.
OTHER RESOURCES
Additional information about the Employer Health Benefits Survey is available at https://kff.org/ehbs, including a Health Affairs article, an interactive graphic, and historical reports. Researchers may also request access to a public use dataset at https://www.kff.org/contact-us/.
The Survey Design and Methods section on our website includes an extended methodology document that is not available in the PDF or printed versions of this report. Readers interested in more detailed information on survey methods should consult the online edition.
Published: October 22, 2025. Last Updated: October 16, 2025.
HISTORICAL DATA
Data in this report focus primarily on findings from surveys conducted and authored by KFF since 1999. Between 1999 and 2017, the Health Research & Educational Trust (HRET) co-authored this survey. HRET’s divestiture had no impact on our survey methods, which remain the same as years past. Prior to 1999, the survey was conducted by the Health Insurance Association of America (HIAA) and KPMG using a similar survey instrument, but data are not available for all the intervening years. Following the survey’s introduction in 1987, the HIAA conducted the survey through 1990, but some data are not available for analysis. KPMG conducted the survey from 1991-1998. However, in 1991, 1992, 1994, and 1997, only larger firms were sampled. In 1993, 1995, 1996, and 1998, KPMG interviewed both large and small firms. In 1998, KPMG divested itself of its Compensation and Benefits Practice, and part of that divestiture included donating the annual survey of health benefits to HRET.
This report uses historical data from the 1993, 1996, and 1998 KPMG Surveys of Employer-Sponsored Health Benefits and the 1999-2017 Kaiser/HRET Survey of Employer-Sponsored Health Benefits. For a longer-term perspective, we also use the 1988 survey of the nation’s employers conducted by the HIAA, on which the KPMG and KFF surveys are based. The survey designs for the three surveys are similar.
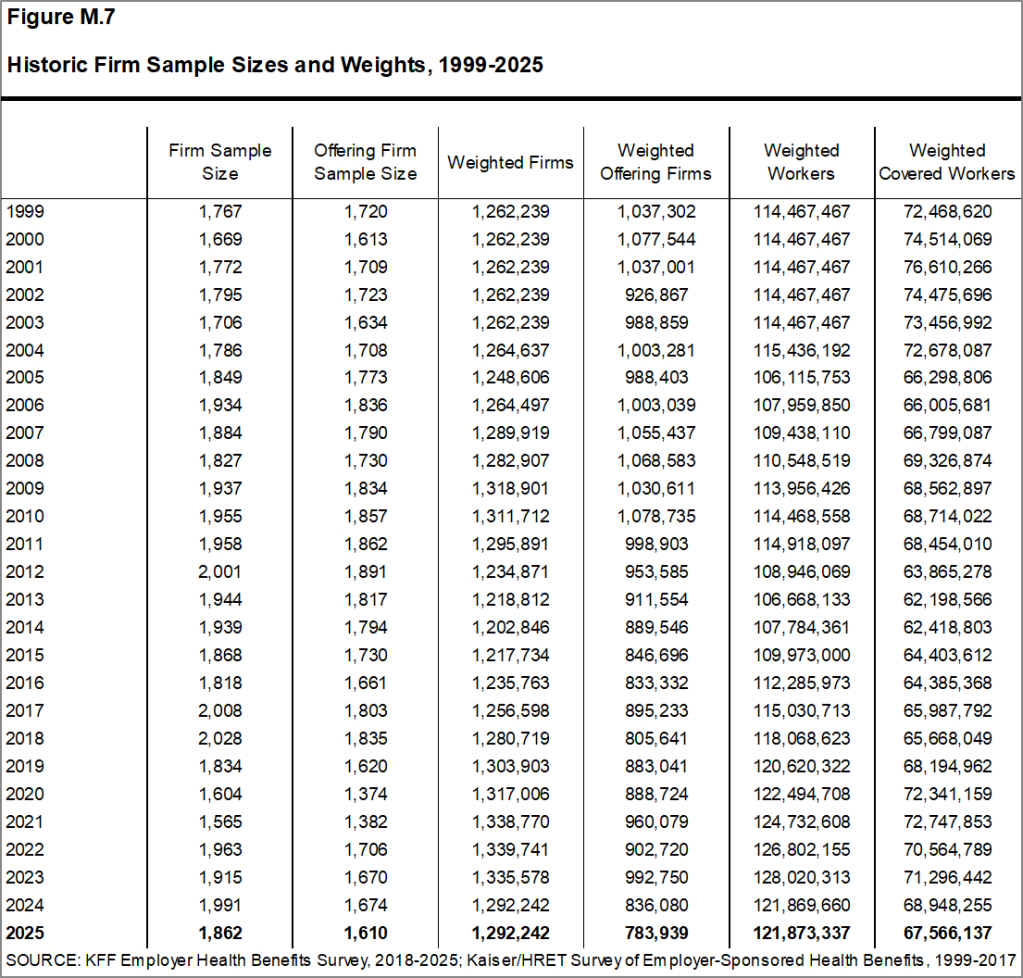
[Figure M.7] displays the historic sample sizes and weights of firms, workers, and covered workers (employees receiving coverage from their employer).
Figure M.7: Historic Firm Sample Sizes and Weights, 1999-2025
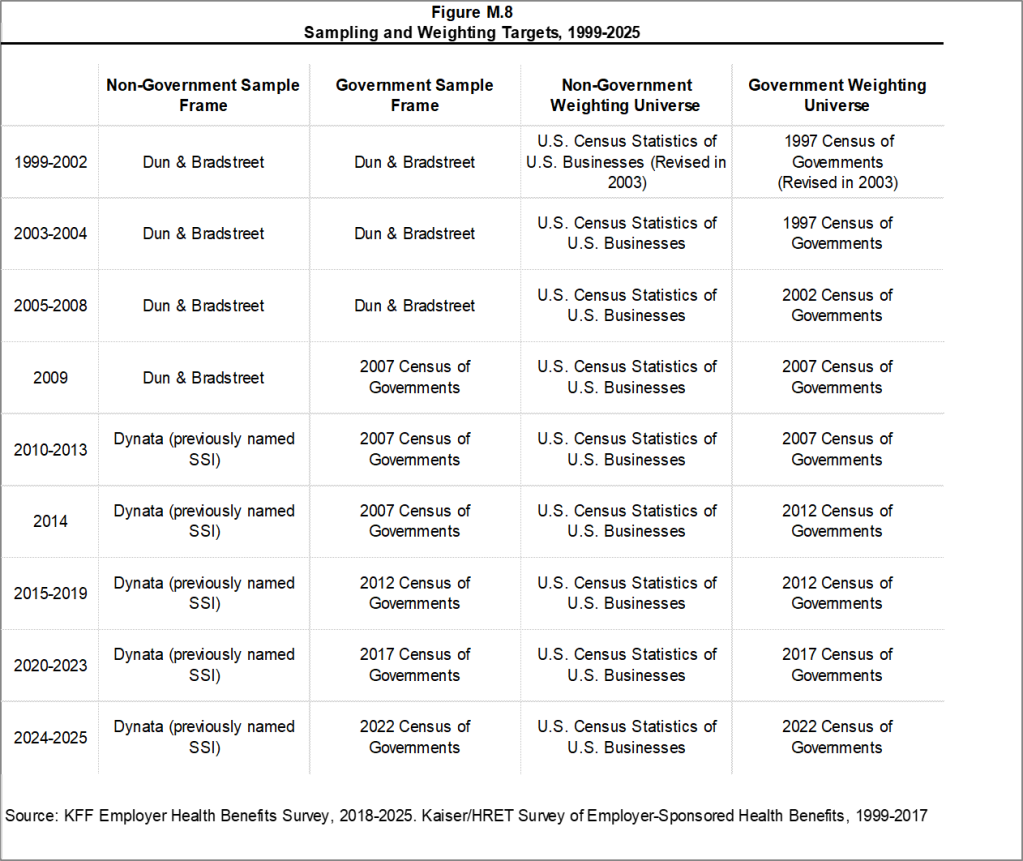
[Figure M.8] displays the historic sample frames and weighting universes.
Figure M.8: Sampling and Weighting Targets, 1999-2025
1999
The Kaiser Family Foundation and The Health Research and Educational Trust (Kaiser/HRET) began sponsoring the survey of employer-sponsored health benefits supported for many years by KPMG Peat Marwick LLP, an international consulting and accounting firm. In 1998, KPMG divested itself of its Compensation and Benefits Practice, and donated the annual survey of health benefits to HRET, a non-profit research organization affiliated with the American Hospital Association. From 1999 until 2017, the survey was conducted under a partnership between HRET and The Kaiser Family Foundation, a health care philanthropy and policy research organization that is not affiliated with Kaiser Permanente or Kaiser Industries. Starting in 1999, survey continued a core set of questions from prior KPMG surveys, but was expanded to include small employers and a variety of policy-oriented questions. Some reports include data from the 1993, 1996 and 1998 KPMG Surveys of Employer-Sponsored Health Benefits. For a longer-term perspective, we also use the 1988 survey of the nation’s employers conducted by the Health Insurance Association of America (HIAA), on which the KPMG, Kaiser/HRET, and Kaiser Family Foundation surveys were based. Many of the questions in the HIAA, KPMG, Kaiser/HRET, and Kaiser Family Foundation surveys are identical, as is the sample design. Since Point-of-Service (POS) plans did not exist in 1988, reports do not include statistics for this plan type in that year. Starting in 1999, Kaiser/HRET drew its sample from a Dun & Bradstreet list of the nation’s private and public employers with three or more workers. To increase precision, Kaiser/HRET stratified the sample by industry and the number of workers in the firm. Kaiser/HRET attempted to repeat interviews with many of the 2,759 firms interviewed in 1998 and replaced non-responding firms with another firm from the same industry and firm size. As a result, 1,377 firms in the 1999 total sample of 1,939 firms participated in both the 1998 and 1999 surveys.
For more detail about the 1999 survey, see the Survey Methodology section of that year’s report.
2000
Kaiser/HRET attempted to repeat interviews with many of the 1,939 firms interviewed in 1999 and replaced non-responding firms with other firms of the same industry and firm size. As a result, 982 firms in the 2000 survey’s total sample of 1,887 firms participated in both the 1999 and 2000 surveys. The overall response rate was 45% down from 60% in 1999. Contributing to the declining response rate was the decision not to re-interview any firms with 3-9 workers who participated in the 1999 survey. In 1999, the survey weights had instead been adjusted to control for the fact that firms with 3-9 workers that are in the panel (responded in either 1998 or 1999) are biased in favor of offering a health plan. The response rate in 2000 for firms with 3-9 workers was 30%.
For more detail about the 2000 survey, see the Survey Methodology section of that year’s report.
2001
For more detail about the 2001 survey, see the Survey Methodology section of that year’s report.
2002
The list of imputed variables was greatly expanded in 2002 to also include self-insurance status, level of benefits, prescription drug cost-sharing, copay and coinsurance amounts for prescription drugs, and firm workforce characteristics such as average income, age and part-time status. On average, 2% of these observations are imputed for any given variable. The imputed values are determined based on the distribution of the reported values within stratum defined by firm size and region.
For more detail about the 2002 survey, see the Survey Methodology section of that year’s report.
2003
The calculation of the weights followed a similar approach to previous years, but with several notable changes in 2003. First, as in years past, the basic weight was determined, followed by a nonresponse adjustment added this year to reflect the fact that small firms that do not participate in the full survey are less likely to offer health benefits and, consequently, are unlikely to answer the single offer rate question. To make this adjustment, Kaiser/HRET conducted a follow-up survey of all firms with 3-49 workers that did not participate in the full survey. Each of these 1,744 firms was asked the single question, “Does your company offer or contribute to a health insurance program as a benefit to its employees?” The main difference between this follow-up survey and the original survey is that in the follow-up survey the first person who answered the telephone was asked whether the firm offered health benefits, whereas in the original survey the question was asked of the person who was identified as most knowledgeable about the firm’s health benefits. Conducting the follow-up survey accomplished two objectives. First, statistical techniques (a McNemar analysis which was confirmed by a chi-squared test) demonstrated that the change in method-speaking with the person answering the phone rather than a benefits manager-did not bias the results of the follow-up survey. Analyzing firms who responded to the offer question twice, in both the original and follow-up survey, proved that there was no difference in the likelihood that a firm offers coverage based on which employee answered the question about whether a firm offers health benefits. Second, the follow-up survey demonstrated that very small firms not offering health benefits to their workers are less likely to answer the one survey question about coverage. Kaiser/HRET analyzed the group of firms that only responded to the follow-up survey and performed a t-test between the firms who had responded to the initial survey as well as the follow-up, and those who only responded to the follow-up. Tests confirmed the hypothesis that the firms that did not answer the single offer rate question in the original survey were less likely to offer health benefits. To adjust the offer rate data for this finding an additional non-response adjustment was applied to increase the weight of firms in the sample that do not offer coverage. The second change to the weighting method in 2003 was to trim the weights in order to reduce the influence of weight outliers. On occasion one or two firms will, through the weighting process, represent a highly disproportionate number of firms or covered workers. Rather than excluding these observations from the sample, a set cut point that would minimize the variances of several key variables (such as premium change and offer rate) was determined. The additional weight represented by outliers is then spread among the other firms in the same sampling cell. Finally, a post-stratification adjustment was applied. In the past, Kaiser/HRET was poststratified back to the Dun & Bradstreet frequency counts. Concern over volatility of counts in recent years led to the use of an alternate source for information on firm and industry data. This year the survey uses the recently released Statistics of U.S. Businesses conducted by the U.S. Census as the basis for the post-stratification adjustment. These Census data indicate the percentage of the nation’s firms with 3-9 workers is 59% rather than the higher percentages (e.g., 76% in 2002) derived from Dun & Bradstreet’s national database. This change has little impact on worker-based estimates, since firms with 3-9 workers accounted for less than 10% of the nation’s workforce. The impact on estimates expressed as a percentage of employers (e.g., the percent of firms offering coverage), however, may be significant. Due to these changes, Kaiser/HRET recalculated the weights for survey years 1999-2002 and modified estimates published in the survey where appropriate. The vast majority of these estimates are not statistically different. However, please note that the survey data published starting in 2003 varies slightly from previously published reports.
For more detail about the 2003 survey, see the Survey Methodology section of that year’s report.
2004
For more detail about the 2004 survey, see the Survey Methodology section of that year’s report.
2005
In 2005, the Kaiser/HRET survey added two additional sections to the questionnaire to collect information about high-deductible health plans (HDHP) that are offered along with a health reimbursement account (HRA) or are health savings account (HSA) qualified. Questions in these sections were asked of all firms offering these plan types, regardless of enrollment. Specific weights were also created to analyze the HDHP plans that are offered along with HRAs or are HSA qualified. These weights represent the proportion of employees enrolled in each of these arrangements.
We updated our data to reflect the 2002 Census of Governments. We also removed federal government employee counts from our post-stratification.
For more detail about the 2005 survey, see the Survey Methodology section of that year’s report.
2006
For the first time in 2006, Kaiser/HRET asked questions about the highest enrollment HDHP/SO as a separate plan type, equal to the other plan types. In prior years, data on HDHP/SO plans were collected as part of one of the other types of plans. Therefore, the removal of HDHP/SOs from the other plan types may affect the year to year comparisons for the other plan types. Given the decline in conventional health plan enrollment and the addition of HDHP/SO as a plan type option, Kaiser/HRET eliminated nearly all questions pertaining to conventional coverage from the survey instrument. We continue to ask firms whether or not they offer a conventional health plan and, if so, how much their premium for conventional coverage increased in the last year, but respondents are not asked additional questions about the attributes of the conventional plans they offer. Because we have limited information about conventional health plans, we must make adjustments in calculating all plan averages or distributions. In cases where a firm offers only conventional health plans, no information from that respondent is included in all plan averages. The exception is for the rate of premium growth, for which we have information. If a firm offers a conventional health plan and at least one other plan type, for categorical variables we assign the values from the health plan with the largest enrollment (other than the conventional plan) to the workers in the conventional plan. In the case of continuous variables, covered workers in conventional plans are assigned the weighted average value of the other plan types in the firm.
The survey newly distinguished between plans that have an aggregate deductible amount in which all family members’ out-of-pocket expenses count toward the deductible and plans that have a separate amount for each family member, typically with a limit on the number of family members required to reach that amount.
In 2006, Kaiser/HRET began asking employers if they had a health plan that was an exclusive provider organization (EPO). We treat EPOs and HMOs together as one plan type and report the information under the banner of “HMO”; if an employer sponsors both an HMO and an EPO, they are asked about the attributes of the plan with the larger enrollment.
Kaiser/HRET made a slight change to one of the industry groups: we removed Wholesale from the group that also included Agriculture, Mining and Construction. The nine industry categories now reported are: Agriculture/Mining/Construction, Manufacturing, Transportation/Communications/Utilities, Wholesale, Retail, Finance, Service, State/Local Government, and Health Care.
Starting in 2006, we made an important change to the way we test the subgroups of data within a year. Statistical tests for a given subgroup (firms with 25-49 workers, for instance) are tested against all other firm sizes not included in that subgroup (all firm sizes NOT including firms with 25-49 workers in this example). Tests are done similarly for region and industry: Northeast is compared to all firms NOT in the Northeast (an aggregate of firms in the Midwest, South, and West). Statistical tests for estimates compared across plan types (for example, average premiums in PPOs) are tested against the “All Plans” estimate. In some cases, we also test plan specific estimates against similar estimates for other plan types (for example, single and family premiums for HDHP/SOs against single and family premiums in HMO, PPO, and POS plans). Those are noted specifically in the text. This year, we also changed the type of Chi-square test from the Chi-square test for goodness-of-fit to the Pearson Chi-square test. Therefore, in 2006, the two types of statistical tests performed are the t-test and the Pearson Chi-square test.
For more detail about the 2006 survey, see the Survey Methodology section of that year’s report.
2007
Kaiser/HRET drew its sample from a Survey Sampling Incorporated list (based on an original Dun and Bradstreet list) of the nation’s private and public employers with three or more workers.
In prior years, many variables were imputed following a hotdeck approach, while others followed a distributional approach (where values were randomly determined from the variable’s distribution, assuming a normal distribution). This year, all variables are imputed following a hotdeck approach. This imputation method does not rely on a normal distribution assumption and replaces missing values with observed values from a firm with similar characteristics, in this case, size and industry. Due to the low imputation rate for most variables, the change in methodology is not expected to have a major impact on the results. In some cases, due to small sample size, imputed outliers are excluded. There are a few variables that Kaiser/HRET has decided should not be imputed; these are typically variables where “don’t know” is considered a valid response option (for example, firms’ opinions about effectiveness of various strategies to control health insurance costs).
The survey now contains a few questions on employee cost sharing that are asked only of firms that indicate in a previous question that they have a certain cost-sharing provision. For example, the copayment amount for prescription drugs is asked only of those that report they have copayments for prescription drugs. Because the composite variables are reflective of only those plans with the provision, separate weights for the relevant variables were created in order to account for the fact that not all covered workers have such provisions.
For more detail about the 2007 survey, see the Survey Methodology section of that year’s report.
2008
National Research, LLC (NR), our Washington, D.C.-based survey research firm, introduced a new CATI (Computer Assisted Telephone Interview) system at the end of 2007, and, due to several delays in the field, obtained fewer responses than expected. As a result, an incentive of $50 was offered during the final two and a half weeks the survey was in the field. Kaiser/HRET compared the distribution of key variables between firms receiving the incentive and firms not receiving the incentive to determine any potential bias. Chi-square test results were not significant, suggesting minimal to no bias.
In 2008, we changed the method used to report the annual percentage premium increase. In prior years, the reported percentage was based on a series of questions that asked responding firms the percentage increase or decrease in premiums from the previous year to the current year for a family of four in the largest plan of each plan type (e.g., HMO, PPO). The reported premium increase was the average of the reported percentage changes (i.e., 6.1% for 2007) weighted by covered workers. This year, we calculate the overall percentage increase in premiums from year to year for family coverage using the average of the premium dollar amounts for a family of four in the largest plan of each plan type reported by respondents and weighted by covered workers (i.e., $12,106 for 2007 and $12,680 for 2008, an increase of 5%). A principal advantage of using the premium dollar amounts to calculate the annual change in premiums is that we are better able to capture changes in the cost of health insurance for those firms that are newly in the market or that change plan types, especially those that move to plans with very different premium levels. For example, in the first year that a firm offers a plan of a new plan type, such as a consumer-directed plan, the firm can report the level of the premium they paid, but using the previous method would be unable to report the rate of change from the previous year since the plan was not previously offered. If the premium for the new plan is relatively low compared to other premiums in the market, the relatively low premium amount that the firm reports will tend to lower the weighted average premium dollar amount reported in the survey, but the firm responses would not provide any information to the percentage premium increase question. Another advantage of using premium dollar amounts to examine trends is that these data directly relate to the other findings in the survey and better address a principal public policy issue (i.e., what was the change in the cost of insurance over some past period). Many users noted, for example, that the percentage change calculated from the reported premium dollar amounts between two years did not directly match the reported average premium increase for the same period. There are several reasons why we would not expect these questions to produce identical results: 1) they are separate questions subject to varying degrees of reporting error, 2) firms could report a premium dollar amount for a plan type they might not have offered in the previous year, therefore, contributing information to one measure but not the other, or 3) firms could report a premium dollar amount for a plan that was not the largest plan of that type in the previous year. Although the two approaches have generated similar results in terms of the long-term growth rate of overall family premiums, there are greater discrepancies in trends for subgroups like small employers and self-funded firms. Focusing on the dollar amount changes over time will provide a more reliable and consistent measure of premium change that also is more sensitive to firms offering new plan options.
As we have in past years, this year we collected information on the cost-sharing provisions for hospital admissions and outpatient surgery that is in addition to any general annual plan deductible. However, for the 2008 survey, we changed the structure of the question and now include “separate annual deductible or hospital admissions” as a response option rather than collecting the information through a separate question. We continue to examine and sometimes modify the questions on hospital and outpatient surgery cost sharing because this can be a complex component of health benefit plans. For example, for some plans it is difficult to distinguish a separate hospital deductible from one categorized as a general annual deductible, where office visits and preventive care are covered and the deductible only applies to hospital use. Because this continues to be a point of confusion, we continue to refine the series of questions in order to clearly convey the information we are attempting to collect from respondents.
As in 2007, we asked firms if they offer health benefits to opposite-sex or same-sex domestic partners. However, this year, we changed the response options because during early tests of the 2008 survey, several firms noted that they had not encountered the issue yet, indicating that the responses of “yes,” “no,” and “don’t know” were insufficient. Therefore, this year we added the response option “not applicable/not encountered” to better capture the number of firms that report not having a policy on the issue.
For more detail about the 2008 survey, see the Survey Methodology section of that year’s report.
2009
In the fall of 2008, with guidance from experts in survey methods and design from NORC, we reviewed the methods used for the survey. As a result of this review, several important modifications were made to the 2009 survey, including the sample design and questionnaire. For the first time, this year we determined the sample requirements based on the universe of firms obtained from the U.S. Census rather than Dun and Bradstreet. Prior to the 2009 survey, the sample requirements were based on the total counts provided by Survey Sampling Incorporated (SSI) (which obtains data from Dun and Bradstreet). Over the years, we have found the Dun and Bradstreet frequency counts to be volatile because of duplicate listings of firms, or firms that are no longer in business. These inaccuracies vary by firm size and industry. In 2003, we began using the more consistent and accurate counts provided by the Census Bureau’s Statistics of U.S. Businesses and the Census of Governments as the basis for post-stratification, although the sample was still drawn from a Dun and Bradstreet list. In order to further address this concern at the time of sampling, we now also use Census data as the basis for the sample. This change resulted in shifts in the sample of firms required in some size and industry categories.
This year, we also defined Education as a separate sampling category, rather than as a subgroup of the Service category. In the past, Education firms were a disproportionately large share of Service firms. Education is controlled for during post-stratification, and adjusting the sampling frame to also control for Education allows for a more accurate representation of both Education and Service industries.
In past years, both private and government firms were sampled from the Dun and Bradstreet database. For the 2009 sample, Government firms were sampled in-house from the 2007 Census of Governments. This change was made to eliminate the overlap of state agencies that were frequently sampled from the Dun and Bradstreet database. Each year the survey attempts to repeat interviews with respondents from past years (see “Response Rate” section below), and in order to maintain government firms that had completed the survey in the past (firms that have completed the survey in the past are known as panel firms), government firms from the 2008 survey were matched to the Census of Governments to identify phone numbers. All panel government firms were included in the sample (resulting in an oversample). In addition, the sample of private firms is screened for firms that are related to state/ local governments, and if these firms are identified in the Census of Governments, they are reclassified as government firms and a private firm is randomly drawn to replace the reclassified firm. These changes to the sample frame resulted in an expected slight reduction in the overall response rate, since there were shifts in the number of firms needed by size and industry. Therefore, the data used to determine the 2009 Employer Health Benefits sample frame include the U.S. Census’ 2005 Statistics of U.S. Businesses and the 2007 Census of Governments. At the time of the sample design (December 2008), these data represented the most current information on the number of public and private firms nationwide with three or more workers. As in the past, the post- stratification is based on the most up-to-date Census data available (the 2006 update to the Census of U.S. Businesses was purchased during the survey field period) and the 2007 Census of Governments. The Census of Governments is conducted every five years, and this is the first year the data from the 2007 Census of Governments have been available for use.
Based on recommendations from cognitive researchers at NORC and internal analysis of the survey instrument, a number of questions were revised to improve the clarity and flow of the survey in order to minimize survey burden. For example, in order to better capture the prevalence of combinations of inpatient and outpatient surgery cost sharing, the survey was changed to ask a series of yes or no questions. Previously, the question asked respondents to select one response from a list of types of cost sharing, such as separate deductibles, copayments, coinsurance, and per diem payments (for hospitalization only). We have also expanded the number of questions for which respondents can provide either the number of workers or the percentage of workers. Previously, after obtaining the total number of employees, the majority of questions asked about the percentage of workers with certain characteristics. Now, for questions such as the percentage of workers making $23,000 a year or less or the enrollment of workers in each plan type, respondents are able to respond with either the number or the percentage of workers. Few of these changes have had any noticeable impact on responses.
For more detail about the 2009 survey, see the Survey Methodology section of that year’s report.
2010
New topics in the 2010 survey include questions on eligibility for dependent coverage, coverage for care received at retail clinics, health plan changes as a result of the Mental Health Parity and Addiction Equity Act of 2008, and disease management. As in past years, this year’s survey included questions on the cost of health insurance, offer rates, coverage, eligibility, enrollment patterns, premiums, employee cost sharing, prescription drug benefits, retiree health benefits, wellness benefits, and employer opinions.
Firms in the sample with 3-49 workers that did not complete the full survey are contacted and asked (or re-asked in the case of firms that previously responded to only one question about offering benefits) whether or not the firm offers health benefits. As part of the process, we conduct a McNemar test to verify that the results of the follow-up survey are comparable to the results from the original survey. If the test indicates that the results are comparable, a nonresponse adjustment is applied to the weights used when calculating firm offer rates. This year, for the first time since we began conducting the follow-up survey, the test indicated that the results from those answering the one question about offering health benefits in the original survey and those answering the follow-up survey were different (statistically significant difference at the p<0.05 level between the two surveys), suggesting the results are not comparable. Therefore, we did not use the results of this follow-up survey to adjust the weights as we have in the past. In the past, the nonresponse adjustment lowered the offer rate for smaller firms by one to three percentage points, so not making the adjustment this year makes the offer rate look somewhat higher when making comparisons to prior years. For 2010, we saw a very large and unexpected increase in the offer rate (from 60 percent in 2009 to 69 percent in 2010) overall and particularly for firms with 3 to 9 workers (from 46 percent in 2009 to 59 percent in 2010). While not making the adjustment this year added to the size of the change, there would have been a large and difficult to explain change even if a nonresponse adjustment comparable to previous years had been made.
For more detail about the 2010 survey, see the Survey Methodology section of that year’s report.
2011
New topics in the 2011 survey include questions on stoploss coverage for self-funded plans, cost sharing for preventive care, plan grandfathering resulting from the Affordable Care Act (ACA), and employer awareness of tax credits authorized under the ACA.
This year, we became aware that the way we have been using the data from the Census Bureau for calibration was incorrect and resulted in an over-count of the actual number of firms in the nation. Specifically, firms operating in more than one industry were counted more than once in computing the total firm count by industry, and firms with establishments were counted more than once in computing the total firm count by state (which affects the regional count). Because smaller firms are less likely to operate in more than one industry or state, the miscounts occurred largely for larger from sizes. The error affects only statistics that are weighted by the number of firms (such as the percent of firms offering health benefits or sponsoring a disease management plan). Statistics that are weighted by the number of workers or covered workers (such as average premiums, contributions, or deductibles) were not affected. We addressed this issue by proportionally distributing the correct national total count of firms within each firm size as provided by the U.S. Census Bureau across industry and state based on the observed distribution of workers. This effectively weights each firm within each category (industry or state) in proportion to its share of workers in that category. The end result is a synthetic count of firms across industry and state that sums to the national totals. Firm-weighted estimates resulting from this change show only small changes from previous estimates, because smaller firms have much more influence on national estimates. For example, the estimate of the percentage of firms offering coverage was reduced by about .05 percentage points in each year (in some years no change is evident due to rounding). Estimates of the percentage of large firms offering retiree benefits were reduced by a somewhat larger amount (about 2 percentage points). Historical estimates used in the 2011 survey release have been updated following this same process. As noted above, worker-weighted estimates from prior years were not affected by the miscount and remain the same.
For more detail about the 2011 survey, see the Survey Methodology section of that year’s report.
2012
New topics in the 2012 survey include the use of biometric screening, domestic partner benefits, and emergency room cost sharing. In addition, many of the questions on health reform included in the 2011 survey were retained, including stoploss coverage for self-funded plans, cost sharing for preventive care, and plan grandfathering resulting from the Affordable Care Act (ACA).
There are several variables in which missing data is calculated based on respondents’ answers to other questions (for example, when missing employer contributions to premiums is calculated from the respondent’s premium and the ratio of contributions to premiums). In 2012 the method to calculate missing premiums and contributions was revised; if a firm provides a premium for single coverage or family coverage, or a worker contribution for single coverage or family coverage, that information was used in the imputation. For example, if a firm provided a worker contribution for family coverage but no premium information, a ratio between the family premium and family contribution was imputed and then the family premium was calculated. In addition, in cases where premiums or contributions for both family and single coverage were missing, the hotdeck procedure was revised to draw all four responses from a single firm. The change in the imputation method did not make a significant impact on the premium or contribution estimates.
In 2012, the method for calculating the size of the sample was adjusted. Rather than using a combined response rate for panel and non-panel firms, separate response rates were used to calculate the number of firms to be selected in each strata. In addition, the mining stratum was collapsed into the agriculture and construction industry grouping. In sum, changes to the sampling method required more firms to be included and may have reduced the response rate in order to provide more balanced power within each strata.
To account for design effects, the statistical computing package R and the library package “survey” were used to calculate standard errors. All statistical tests are performed at the .05 level, unless otherwise noted. For figures with multiple years, statistical tests are conducted for each year against the previous year shown, unless otherwise noted. No statistical tests are conducted for years prior to 1999. In 2012 the method to test the difference between distributions across years was changed to use a Wald test which accounts for the complex survey design. In general this method was more conservative than the approach used in prior years.
In 2012, average coinsurance rates for prescription drugs, primary care office visits, specialty office visits, and emergency room visits include firms that have a minimum and/or maximum attached to the rate. In years prior to 2012 we did not ask firms the structure of their coinsurance rate. For most prescription drug tiers, and most services, the average coinsurance rate is not statically different depending on whether the plan has a minimum or maximum.
In 2012 the calculation of the response rates was adjusted to be slightly more conservative than previous years.
For more detail about the 2012 survey, see the Survey Methodology section of that year’s report.
2013
Starting in 2013, information on conventional plans was collected under the PPO section and therefore the covered worker weight was representative of all plan types.
For more detail about the 2013 survey, see the Survey Methodology section of that year’s report.
2014
Starting in 2014, we elected to estimate separate single and family coverage premiums for firms that provided premium amounts as the average cost for all covered workers, instead of differentiating between single and family coverage. This method more accurately accounted for the portion that each type of coverage contributes to the total cost for the 1 percent of covered workers who are enrolled at firms affected by this adjustment.
Several provisions of the ACA took effect on January 1, 2014 which impacted non-grandfathered plans as well as plans renewing in calendar year 2014, such as the requirement to have an out of pocket limit and a waiting period of not more than three months. As a result, firms with non-grandfathered plans that reported that they did not have out-of-pocket limits, or waiting periods exceeding three months, were contacted during our data-confirmation calls. We did not have information on the month in which a firm’s plan or plans was renewed. Many of these firms indicated that they had a plan year starting prior to January 2014, so these ACA provision were not yet in effect for these plans.
Firms with 200 or more workers were asked: “Does your firm offer health benefits for current employees through a private or corporate exchange? A private exchange is one created by a consulting firm or an insurance company, not by either a federal or state government. Private exchanges allow employees to choose from several health benefit options offered on the exchange.” Employers were still asked for plan information about their HMO, PPO, POS and HDHP/SO plan regardless of whether they purchased health benefits through a private exchange or not.
Beginning in 2014, we collected whether firms with a non-final disposition code (such as a firm that requested a callback at a later time or date) offered health benefits. By doing so we attempt to mitigate any potential non-response bias of firms either offering or not offering health benefits on the overall offer rate statistic.
For more detail about the 2014 survey, see the Survey Methodology section of that year’s report.
2015
To increase response rates, firms with 3-9 employees were offered an incentive of $75 in cash or as a donation to a charity of their choice to complete the full survey.
In 2015, weights were not adjusted using the nonresponse adjustment process described in previous years’ methods. As in past years, Kaiser/HRET conducted a small follow-up survey of those firms with 3 to 49 workers that refused to participate in the full survey. Based on the results of a McNemar test, we were not able to verify that the results of the follow-up survey were comparable to the results from the original survey. In 2010, the results of the McNemar test were also significant and we did not conduct a nonresponse adjustment.
The 2015 survey contains new information in several areas, including on wellness and biometric screening. In most cases, information reported in this section is not comparable with previous years’ findings. Data presented in the 2015 report reflect the firm’s benefits at the time they completed the interview. Some firms may report on a plan which took effect in the prior calendar year. Starting in 2015, firms were able to have a contribution and deductible in compliance with HSA requirements for the plan year.
Starting in 2015, employers were asked how many full-time equivalents they employed. In cases in which the number of full-time equivalents was relevant to the question, interviewer skip patterns may have depended on the number of FTEs.
In cases where a firm had multiple plans, they were asked about their strategies for containing the cost of specialty drugs for the plan with the largest enrollment.
Under the Affordable Care Act, non-grandfathered plans are required to have an out-of- pocket maximum. Non-grandfathered plans who indicated that they did not have an out of pocket maximum were asked to confirm whether their plan was grandfathered and whether that plan had an out-of-pocket maximum.
For more detail about the 2015 survey, see the Survey Methodology section of that year’s report.
2016
Between 2015 and 2016, we conducted a series of focus groups that led us to the conclusion that human resource and benefit managers at firms with between 20 and 49 employees think about health insurance premiums more similarly to benefit managers at smaller firms than larger firms. Therefore, starting in 2016, we altered the health insurance premium question pathway for firms with between 20-49 employees to match that of firms with 3-19 employees rather than firms with 50 or more employees. This change affected firms representing 8% of the total covered worker weight. We believe that these questions produce comparable responses and that this edit does not create a break in trend.
Starting in 2016, we made significant revisions to how the survey asks employers about their prescription drug coverage. In most cases, information reported in the Prescription Drug Benefits section is not comparable with previous years’ findings. First, in addition to the four standard tiers of drugs (generics, preferred, non-preferred, and lifestyle), we began asking firms about cost sharing for a drug tier that covers only specialty drugs. This new tier pathway in the questionnaire has an effect on the trend of the four standard tiers, since respondents to the 2015 survey might have previously categorized their specialty drug tier as one of the other four standard tiers. We did not modify the question about the number of tiers a firm’s cost-sharing structure has, but in cases in which the highest tier covered exclusively specialty drugs we reported it separately. For example, a firm with three tiers may only have copays or coinsurances for two tiers because their third tier copay or coinsurance is being reported as a specialty tier. Furthermore, in order to reduce survey burden, firms were asked about the plan attributes of only their plan type with the most enrollment. Therefore, in most cases, we no longer make comparisons between plan types. Lastly, prior to 2016, we required firms’ cost sharing tiers to be sequential, meaning that the second tier copay was higher than the first tier, the third tier was higher than the second, and the fourth was higher than the third. As drug formularies have become more intricate, many firms have minimum and maximums attached to their copays and coinsurances, leading us to believe it was no longer appropriate to assume that a firm’s cost sharing followed this sequential logic.
In cases where a firm had multiple plans, they were asked about their strategies for containing the cost of specialty drugs for the plan type with the largest enrollment. Between 2015 and 2016, we modified the series of ‘Select All That Apply’ questions regarding cost containment strategies for specialty drugs. In 2016, we elected to impute firms’ responses to these questions. We removed the option “Separate cost sharing tier for specialty drugs” and added specialty drugs as their own drug tier questionnaire pathway. We added question options on mail order drugs and prior authorization.
In 2016, we modified our questions about telemedicine to clarify that we were interested in the provision of health care services, and not merely the exchange of information, through telecommunication. We also added dependent and spousal questions to our health risk assessment question pathway.
For more detail about the 2016 survey, see the Survey Methodology section of that year’s report.
2017
While the Kaiser/HRET survey similar to other employer and household surveys has seen a general decrease in response rates over time, the decrease between the 2016 and 2017 response rates is not solely explained by this trend. In order to improve statistical power among sub-groups, including small firms and those with a high share of low income workers, the size of the sample was expanded from 5,732 in 2016 to 7,895 in 2017. As a result, the 2017 survey includes 204 more completes than the 2016 survey. While this generally increases the precision of estimates (for example, a reduction in the standard error for the offer rate from 2.2% to 1.8%), it has the effect of reducing the response rate. In 2017, non-panel firms had a response rate of 17%, compared to 62% for firms that had participated in one of the last two years.
To increase response rates, firms with 3-9 employees were offered an incentive for participating in the survey. A third of these firms were sent a $5 Starbucks gift card in the advance letter, a third were offered an incentive of $50 in cash or as a donation to a charity of their choice after completing the full survey, and a third of firms were offered no incentive at all. Our analysis does not show significant differences in responses to key variables among these incentive groups.
In 2017, weights were not adjusted using the nonresponse adjustment process described in previous years’ methods. As in past years, Kaiser/HRET conducted a small follow-up survey of those firms with 3-49 workers that refused to participate in the full survey. Based on the results of a McNemar test, we were not able to verify that the results of the follow-up survey were comparable to the results from the original survey. In 2010 and 2015, the results of the McNemar test were also significant and we did not conduct a nonresponse adjustment.
To reduce the length of survey, in several areas, including stoploss coverage for self-funded firms and cost sharing for hospital admissions, outpatient surgery, and emergency room visits, we revised the questionnaire to ask respondents about the attributes of their largest health plan rather than each plan type they may offer. This expands on the method we used for prescription drug coverage in 2016. Therefore, for these topics, aggregate variables represent the attributes of the firm’s largest plan type, and are not a weighted average of all of the firms plan types. In previous surveys, if a firm had two plan types, one with a copayment and one with a coinsurance for hospital admissions, the covered worker weight was allotted proportionally toward the average copayment and coinsurance based on the number of covered workers with either feature. With of this change, comparison among plans types is now a comparison of firms where any given plan type is the largest. The change only affects firms that have multiple plan types (58% of covered workers). After reviewing the responses and comparing them to prior years where we asked about each plan type, we find that the information we are receiving is similar to responses from previous years. For this reason, we will continue to report our results for these questions weighted by the number of covered workers in responding firms.
Starting in 2017, respondents were allowed to volunteer that their plans did not cover outpatient surgery or hospital admissions. Less than 1% of respondents indicated that their plan did not include coverage for these services. Cost sharing for hospital admissions, outpatient surgery and emergency room visits was imputed by drawing a firm similar in size and industry within the same plan type.
For more detail about the 2017 survey, see the Survey Methodology section of that year’s report.
2018
As in past years, we conducted a small follow-up survey of those firms with 3-49 workers that refused to participate in the full survey. Based on the results of a McNemar test, we were not able to verify that the results of the follow-up survey were comparable to the results from the original survey, and weights were not adjusted using the nonresponse adjustment process described in previous years’ methods. In 2010, 2015, and 2017, the results of the McNemar test were also significant and we did not conduct a nonresponse adjustment.
In light of a number of regulatory changes and policy proposals, we included new questions on the anticipated effects of the ACA’s individual mandate penalty repeal on the firm’s health benefits offerings, and the impact of the delay of the high cost plan tax, also known as the Cadillac tax, on the firm’s health benefits decisions. Also new in 2018 are questions asking about smaller firms’ use of level-funded premium plans, an alternative self-funding method with integrated stop loss coverage and a fixed monthly premium.
In 2018, we moved the battery of worker demographics questions from near the beginning of the survey to the end of the survey in an effort to improve the flow. There is no evidence that this move has impacted our survey findings and we will continue to monitor any suspected impacts.
The 2018 survey also expands on retiree health benefits questions, asking firms about cost reduction strategies, whether they contribute to the cost of coverage, and how retiree benefits are offered (e.g., through a Medicare Advantage contract, a traditional employer plan, private exchange, etc.).
Starting in 2018, we allowed respondents who did not know the combined maximum incentive or penalty an employee could receive for health screening and/or wellness and health promotion to answer a categorical question with specified ranges. This method is consistent with how we handle the percent of low-wage and high-wage workers at a firm. In 2018, 18% of respondents did not know the dollar value of the their incentive or penalty and 39% were able to estimate a range.
Starting in 2018, the survey began asking small firms who indicated that their plan was fully-insured whether the plan was level-funded. In a level-funded plan, employers make a set payment each month to an insurer or third party administrator which funds a reserve account for claims, administrative costs, and premiums for stop-loss coverage. These plans are often integrated and firms may not understand the complexities of the self-funded mechanisms underlying them. Some small employers who indicate that their plan is self-funded may also offer a plan that meets this definition. Respondents offering level funded plans were asked about any attachment points applying to enrollees. These firms were not less likely to answer this question, and including them doesn’t not substantially change the average. Prior to 2018, all firms reporting coverage as underwritten by an insurer were excluded from the stop-loss calculations.
The response option choices for the type of incentive or penalty for completing biometric screening or a health risk assessment changed from 2017 to 2018.
For more detail about the 2018 survey, see the Survey Methodology section of that year’s report.
2019
Starting in 2019, we discontinued a weighting adjustment informed by a follow-back survey of firms with 3-49 workers that refused to participate in the full survey. This adjustment was intended to reduce non-response bias in the offer rate statistic, under the assumption that firms that did not complete the survey were less likely to offer health benefits. The adjustment involves comparing the distribution of offering to non-offering firms in the full survey and the follow-back sample in the three smallest size categories (3-9, 10-24, 25-49). The adjustment is based on the differences between the two groups of firms and generally operates to adjust the weights of offering firms and non-offering firms to bring the counts closer together. However, if the distributions of the two groups differ to a statistically significant extent, we consider the follow-back survey to be a different population from the full survey and do not make any adjustment to the weights.
Although we cannot be sure of the reason, we are no longer witnessing the systematic upward bias on estimates for the offer rates of small firms that gave rise to the adjustment. Looking at the decade from 2010 to 2019, offer rates among firms responding to the follow-up survey have been higher for five of ten surveys. Firms with 3-49 employees responding to this follow-up survey have reported a higher offer rate than the full EHBS survey during the 2014, 2016, 2017, 2018, and 2019 surveys. An alternative way to measure non-response bias is to compare estimates throughout the fielding period.
In 2019, the percent of firms offering health benefit was similar in the last month of fielding to offer rates throughout the entire fielding period. Changes in both the survey methodology and the health insurance market have led us to become increasingly cautious about assuming that the follow back survey is a suitable proxy for the true population. Since 2014, we have collected offer rate information from firms before a final disposition is assigned. This method was introduced to reduce a bias in which firms who offer health benefits face a longer average survey than non-offering firms. This had the effect of increasing the percentage of firms for whom contact was made from whom we collected offer rate information. Additionally, we have also attempted to reduce non-response bias by increasing our data collection.
Recent changes in the marketplace also raise some concerns about the validity of the follow-back survey to be the basis for a weight adjustment. We have in recent years seen an increase in non-offering firms reporting that they are providing funds to employees to purchase non-group health insurance. We do not consider this to be an offer of health insurance by the firm, but we are concerned that the person who responds to the follow-back survey may not be able to make that distinction. The follow-back survey is a very simple set of questions asked to whoever answers the phone at a firm that refused to participate in the survey. In contrast, during the full-survey, we attempt to talk to the person most knowledgeable about health benefits, and the interviewers are trained to distinguish between types of benefit programs.
For 2019, making the weight adjustment would change offer rate statistic for all firms from 57% to 60%. Neither estimate is different than the 57% we reported last year (when the weight adjustment was not made because the statistical test indicated that the follow-back group was significantly different than the full survey group).
Starting in 2019, all presented calculations of out-of-pocket maximums strictly relied on an arithmetic average across all plans weighted by covered worker plan enrollment. In prior surveys, some figures (for example Figures 7.43, 7.45, and 7.46 in the 2018 report) were calculated based on the out-of-pocket maximum of the largest plan. This change did not meaningfully change any findings and ensured consistency within the out-of-pocket maximum section of the Employee Cost Sharing section.
For prescription drug coverage, similar to years past, if the firm reports that the worker pays the full cost for drugs on a particular tier and/or that the plan only offers access to a discount program, we do not consider this as offering covering for that drug tier. Starting this year, firms with multiple tiers that cover exclusively specialty drugs, were asked about the cost-sharing of the tier that is used most often. Cost-sharing for prescription drugs does not typically include mail order. Hospital, outpatient surgery and prescription drug cost-sharing was only asked of a firm’s largest plan type.
For 2019, we clarified the question that we use to ask firms whether or not they provide retiree health benefits; particularly, we added language that explicitly stated that firms that had terminated retiree health benefits but still has some retirees currently getting coverage, or that had current employees who will get retiree health coverage in the future, should answer yes to the question. We made this clarification in response to a large decline in the 2018 survey in the prevalence of retiree coverage (from 25% in 2017 to 18% in 2018). In the 2018 survey, we expressed concern that the then current public focus on public entities eliminating retiree benefits for future (not existing) retirees may be influencing the responses we were getting and said that we were going to add clarifying language to the survey question in future years.
For 2019, two open-ended questions were added to the survey in order to examine employer responses to the opioid crisis and obstacles preventing firms from adopting narrow network health plans. All responses to these questions were reviewed in a consistent manner by KFF staff to determine whether they could be recoded as an earlier multiple choice item, or if they could be sorted into new categories.
To increase participation in the final two weeks of the survey, a financial incentive was offered to firms with 3-9 employees, but only 6 firms that completed the survey within that time period qualified for the incentive. All respondents received a printed copy of the survey findings.
For more detail about the 2019 survey, see the Survey Methodology section of that year’s report.
2020
2020 was a challenging year both in administering the survey, as well as for many of our respondents who were scrambling to respond to the pandemic and the ensuing economic downturn. Our questionnaire was developed before the extent of the pandemic became apparent and the fielding period included response from both before and after. We asked respondents about their plans at the time of the interview, with approximately half of the responses (composing 50% of the covered worker weight) collected between January and March. The remaining interviews were completed before the middle of July. The survey is designed to track changes in benefit and cost between years and is not well suited to answer many of the important questions that emerged this year for a couple of reasons. Firstly, employers make decisions about their plans before the plan year begins. Premiums for self-funded employers are usually reported as the cost for a former worker to enroll in COBRA (deflated by an administrative fee) and do not reflect real-time spending. Many other plan features, including provider networks and cost-sharing, are set before a plan’s open enrollment period. We expect to learn more about how changes in benefits and utilization affected cost in the 2021 survey. Secondly, the month in which a respondent completes the survey is not random, the data collection firm completes interviews with larger panel firms first. We do not believe that these firms are similar to the non-panel firms that complete the survey later in the year. We believe these firms differ in ways which are not corrected for by weighting, which means we cannot look at how responses changed over the period to detect patterns of change. Thirdly, our sample is not sufficient to make many comparisons across fielding period. We plan to ask employers about changes to their plans and the impact of COVID-19 on their decision making in the 2021 survey.
In the summer of 2019, National Research LLC, which had conducted the Employer Health Benefit Survey since its inception, ceased operation. We engaged in a search to identify a new firm to conduct the 2020 survey and selected Davis Research LLC, based on their extensive experience in research on firms and establishments. While we believe that the sampling methodology, questionnaire and survey procedures were consistent between years, readers are strongly encouraged to consider “total survey error” when drawing conclusions about differences between statistics. Survey-adjusted standard errors (and statistical testing) measure uncertainty in estimates based on the sampling strategy, but do not measure biases that may be introduced through the data collection process such as interviewer or house effects. House effects refer to the impact of a data collection firm’s management and workflow processes on final statistics. We do not know how, or if at all, changing the data collection firm from National Research to Davis impacted estimates. Empirical studies of house effects vary greatly, with some reporting almost no impact and others observing significant differences in point estimates.
In order to minimize house effect impacts, we conducted extensive interview training with managers and interviewers at Davis, including sessions lead by interviewers with prior experience on the project. In addition, KFF pretested and observed interviews to verify that Davis’ quality assurance process was consistent with our understanding of how the survey had been conducted historically.
Starting in 2020, we limited the number of margins used to calibrate weights and adjust for non-response. Until 2019, our weighting procedure incorporated offer status, firm size, geographic region, and metropolitan status to adjust for unit nonresponse. Our 2020 weighting algorithm no longer relies on metropolitan vs. non-metropolitan as part of the non-response calculation. Separately, earlier surveys post-stratified each firm’s set of weights to industry, firm size, census division, and panel versus non-panel margins. Starting in 2020, we reduced this weight calibration to only industry and firm size controls. Finally, we collapsed industries in our 5,000+ employee firm size category, owing to the fact that many large businesses operate across multiple industries. All three of these changes were prompted by an increase in the number of calibration cells with low sample, which can result in individual firms with highly influential weights if not revised. Without this revision, some 2020 statistics would had been driven by a small number of firms with overly influential weights. Reducing the number of variables in these improves the stability of some published estimates. This issue arose in part due to the smaller number of completed interviews in 2020 relative to 2019.
Historically we measured the annual changes in workers’ wages and in inflation by comparing the values for April of the previous year and April of the current year. This year the labor market underwent significant disruptions in March and April as employers laid off and furloughed large numbers of workers in response to the COVID-19 pandemic. A relatively high share of lower-wage workers were furloughed and laid off during these months, resulting in a high change in wages as measured from April to April. In response to this unprecedented change in the labor market, we have elected to change how we calculate workers wages and inflation. Beginning with our 2020 publication, we are now calculating the change in workers wages and inflation based on an average of the first quarter of each year. Using this method, workers wages increased 3.4% compared to 7.7% between April and April. And similarly inflation increased 2.1% compared to 0.3%. Prior to 2020, both methods produced very similar estimates.
For more detail about the 2020 survey, see the Survey Methodology section of that year’s report.
2021
This year we made several changes to the survey questionnaire in order to reduce the length and burden of the survey; rather than asking benefit managers about the characteristics of up to four plan types, we asked for the premiums and deductibles of the largest two plan types and other cost information for only the largest. We now only ask about cost-sharing for prescription drugs, hospitalizations, outpatient surgery and office visits for the plan type with the most enrollment. This change mostly impacts the largest firms which are more likely to sponsor multiple plan types. As in prior years, if a firm sponsors multiple plans, of the same plan type, for example, several PPOs across the country, we ask about only the one with the most enrollment. In 2021, 13% of respondents offered three or more plan types – in total the largest plan type accounts for 82% of workers covered by health benefits and the largest two plan types represents 98%. For this reason, this change will only have a minimal impact on most estimates. Furthermore, in prior years we observed no systematic bias in key metrics across the plan type rank at each firm. For example, in 2020, among firms with three or more plan types, the third-largest plan had statistically similar premiums and deductibles to the larger plan types on average. This change did not require a change in how many of the the all firm variables are calculated. To determine the all plan value for categorical variables describing plans, we continue to use the largest type as a proxy. To do so, we identify the plan type that has the largest enrollment within the observation and use data from that plan as a proxy for the all-plan aggregate for that firm. For example, in previous years, we would ask an employer whether their HMO, PPO, POS and HDHP/SO were self-funded, and then report the response from largest plan type as the all firm response.
For the first time, a subset of employers were invited to complete the survey online, though in total 99% of the interviews were completed through computer-assisted telephone interviewing.
For more detail about the 2021 survey, see the Survey Methodology section of that year’s report.
2022
In 2022, we incorporated the California Employer Health Benefits Survey (CHBS) from the California Health Care Foundation (CHCF) into EHBS by oversampling firms with any presence in California and including new questions into the main EHBS instrument to determine firms with any employment in the state of California. Unlike other years, the 2022 EHBS used as its panel both respondents to either of the prior two years of EHBS (2020 and 2021) and also respondents to either of the prior two years of CHBS (2018 and 2020). Since many larger firms operate across state lines, the integration of CHBS with EHBS aimed to reduce survey burden among firms that had previously responded to both surveys. Among the N=1,140 large firms responding to the 2022 EHBS, 419 of those responding firms (37%) had any presence in California, highlighting the overlap across these two projects. Given the size of the California oversample needed to assure statistical reliability both nationally and within California, firm weights were calibrated to California-specific targets from the SUSB.
In 2022, Davis extended computer assisted web interview (CAWI) capacity, offering most respondents the opportunity to complete the survey using an online questionnaire rather a telephone interview. Although only 1% of respondents used this survey mode during the initial 2021 attempt, 43% of 2022 survey respondents answered EHBS via CAWI.
Survey mode did not impact the survey results in a systematic or obvious manner. The effects of mode and firm size on major firm characteristics such as annual premiums, contributions, and deductibles was modeled using standard linear regression. For certain plan types, survey implementation through telephone interview had a negative effect on the reported value. However, the plan types affected were random, so this effect is more likely due to confounding variables. When examining demographic characteristics between the two modes, there were small differences in the distribution of categorical variables such as region and age. However, without multiple years of data utilizing the two modes, it is impossible to determine if these are systematic biases. The imputation rate between the two modes was almost identical.
For more detail about the 2022 survey, see the Survey Methodology section of that year’s report.
2023
The 2023 survey features questions which have not been asked for several years including questions on spousal benefits, voluntary benefits, such as dental and vision coverage, waiting periods and emergency room cost-sharing. In addition, the survey includes new questions, on abortion coverage, prior authorization, coverage limits and coverage for gender-affirming care.
In 2022, the Employer Health Benefit Survey over-sampled California based firms in order to provide estimates for the California Health Care Foundation’s Health Benefit Survey. For more information please see: https://www.chcf.org/publication/2023-edition-california-employer-health-benefits/. As a result, both our weighting and sampling in 2022 took into account whether a firm was located in California. In 2023, we sampled non-panel firms based on whether they were located in California. Our 2023 sampling method is similar to the methods used prior to 2022, and is based on a firms size and industry.
As in previous years, modification were made to existing survey questions, both to improve clarity or respond to changes in the marketplace.
- Starting in 2023, respondents are able to provide either monthly or annual HSA contribution amounts.
- The interview notes for the question on level-funding was editing to clarify that employing a third-party administrator does not necessarily mean a plan is level-funded.
- The question on whether a firm or plan gives workers the opportunity to complete biometeric screening was edited to include take-home kits, which collect biometetric data, not just in-person exams.
- The distribution of cost-sharing for hospital admission and outpatient surgery was edited, to make the categories “copay”, “coninsurance”, and “both copay and coinsurance”, mutually exclusive. The both category may include covered workers who face either both cost-sharing requirements or which ever is greater.
Based on interview debriefs, we elected not to report the share of employers who believe that telehealth will be important for enrollees in remote settings. We continue to revise our data cleaning and editing procedures.
For more detail about the 2023 survey, see the Survey Methodology section of that year’s report.
2024
The 2024 survey features new questions, on prescription drug policy, mental health and substance use, GLP-1 drug coverage, family-building services, transparency, and affordability issues for lower-wage workers.
As in previous years, modification were made to existing survey questions, both to improve clarity or respond to changes in the marketplace. Starting in 2024, the introductory text for web-based interviews was condensed. In an effort to reduce respondent burden, we removed questions on waiting periods, emergency room cost sharing, wellness program incentives, disease management, sites of care, and prior authorization. We also restricted clarification follow-up calls (or callbacks) to only firms with at least one premium or cost sharing-related item: observations for firms with outliers only in the drug tier section of the questionnaire were imputed based on logic rules.
In some cases respondents report they offer coverage, but do not offer a comprehensive major medical plan. This year we added additional questions to clarify whether plans with low premiums were major medical plans. We dropped fewer than five firms where the respondent told us they did not cover most physician services and hospital admissions other than preventative care from the premium average.
9.8 percent of respondents in 2024 were either unable to provide their firm’s single coverage premium, or provided a response which was logically inconsistent with other values. In these cases, in order to minimize non-response bias, missing responses were imputed. In prior years, if a firm was missing a single premium value, this value was imputed using a ‘hot deck’ approach in which a single premium was selected among firms with similar demographic characteristics. This year we revised this method. In cases in which both the single and family premiums were missing, the single premium was estimated based on other known characteristics of the plan and firm. This method is advantageous because it predicts single premiums based on specific firm characteristics related to the premium, such as cost-sharing and deductibles, as well as demographics. Then, the family premium, as well as single and family worker contributions (if missing), were subsequently hot decked based on their relationship to the single premium. In cases in which a firm provides a response to the family premium, the single premium is imputed based on a ratio of the premiums. Therefore, in total, 8% of responses were affected by this change.
The updated imputation process uses a random forest machine learning model. The model was trained on EHBS data from 2021-2023. Features were selected using step wise regression. The hyper-parameters of the model were tuned using the grid search algorithm. Compared to hot-decking, this method is significantly better at explaining the variation in the observed data (R-squared of 0.2071 versus 0.00018540). This methodological change has a relatively minor impact on the overall premium; the 2024 premium would be 0.8% different if we did not implement the new method. However, this change meaningfully impacts the precision of premium estimates for demographic subgroups.
For more detail about the 2024 survey, see the Survey Methodology section of that year’s report.
- Seasonally Adjusted Data from the Current Employment Statistics Survey. Bureau of Labor Statistics. Current Employment Statistics—CES (National) [Internet]. Washington (DC): BLS; [cited 2024 Aug 1]. Available from: https://www.bls.gov/ces/publications/highlights/highlights-archive.htm↩︎
- Bureau of Labor Statistics, Mid-Atlantic Information Office. Consumer Price Index historical tables for, U.S. City Average (1967 = 100) of Annual Inflation [Internet]. Washington (DC): BLS; [cited 2024 Aug 1]. Available from: https://www.bls.gov/regions/mid-atlantic/data/consumerpriceindexhistorical1967base_us_table.htm↩︎
- Seidenberg, Andrew B, Richard P Moser, and Brady T West. 2023. “Preferred Reporting Items for Complex Sample Survey Analysis (PRICSSA).” Journal of Survey Statistics and Methodology 11 (4): 743-57. https://doi.org/10.1093/jssam/smac040.↩︎
Cost of Health Insurance
The average annual health insurance premiums in 2025 are $9,325 for single coverage and $26,993 for family coverage. The average single coverage premium increased 5% in 2025 while the average family premium increased 6%. The average family premium has increased 26% since 2020 and 53% since 2015.
As part of this report, KFF publishes an online tool which allows users to look at changes in premiums and worker contributions for covered workers at different types of firms over time: https://www.kff.org/interactive/premiums-and-worker-contributions/
PREMIUMS FOR SINGLE AND FAMILY COVERAGE
The average premium for single coverage in 2025 is $9,325 per year. The average premium for family coverage is $26,993 per year [Figure 1.1].
- The average annual premiums for single coverage are similar for covered workers at firms with 10 to 199 workers ($9,211) and at larger firms ($9,361) [Figure 1.3].
- The average annual premiums for family coverage are lower for covered workers at firms with 10 to 199 workers ($26,054) than for those at larger firms ($27,280) [Figure 1.3].
- The average annual premiums for covered workers in HDHP/SOs are lower than the average premiums for coverage overall for both single coverage ($8,620 vs. $9,325) and family coverage ($25,379 vs. $26,993). The average premiums for covered workers in PPOs are higher than the overall average premiums for both single coverage ($9,818 vs. $9,325) and family coverage ($28,272 vs. $26,993) [Figure 1.1].
- The average premium for covered workers with both single and family coverage is relatively higher in the Northeast and relatively lower in the South [Figure 1.4].
- The average premium for covered workers at firms with relatively large shares of lower-wage workers (where at least 35% of workers earn $37,000 a year or less) is lower than the average premium for covered workers at firms with smaller shares of lower-wage workers for family coverage ($25,500 vs. $27,176). The average premium for covered workers at firms with relatively large shares of higher-wage workers (where at least 35% of workers earn $80,000 a year or more) is higher than the average premium for covered workers at firms with smaller shares of higher-wage workers for both single coverage ($9,600 vs. $9,133) and family coverage ($27,957 vs. $26,313) [Figure 1.6] and [Figure 1.7].
- The average premiums for covered workers at firms with relatively large shares of younger workers (firms where at least 35% of the workers are age 26 or younger) are lower than the average premiums for covered workers at firms with smaller shares of younger workers for family coverage ($24,834 vs. $27,174). The average premiums for covered workers at firms with relatively large shares of older workers (firms where at least 35% of the workers are age 50 or older) are higher than the average premiums for covered workers at firms with smaller shares of older workers for both single coverage ($9,599 vs. $9,068) and family coverage ($27,699 vs. $26,332) [Figure 1.6] and [Figure 1.7].
- The average premiums for single coverage and family coverage are relatively lower for covered workers at private for-profit firms and relatively higher for covered workers at private not-for profit firms [Figure 1.6] and [Figure 1.7].
Figure 1.1: Average Annual Premiums for Covered Workers, Single and Family Coverage, by Plan Type, 2025
Figure 1.2: Average Annual Premiums for Covered Workers, Single and Family Coverage, by Firm Size, 2025
Figure 1.3: Average Monthly and Annual Premiums for Covered Workers, by Plan Type and Firm Size, 2025
Figure 1.4: Average Monthly and Annual Premiums for Covered Workers, by Plan Type and Region, 2025
Figure 1.5: Average Monthly and Annual Premiums for Covered Workers, by Plan Type and Industry, 2025
Figure 1.6: Average Annual Premiums for Covered Workers With Single Coverage, by Firm Characteristics, 2025
Figure 1.7: Average Annual Premiums for Covered Workers With Family Coverage, by Firm Characteristics, 2025
Figure 1.8: Average Annual Premiums for Covered Workers, by Firm Characteristics and Firm Size, 2025
PREMIUM DISTRIBUTION
There is considerable variation in premiums for both single and family coverage.
- Seventeen percent of covered workers are employed at a firm where the single coverage premium is at least 20% higher than the average single premium, while 19% of covered workers are at firms with a single premium less than 80% of the average single premium [Figure 1.9].
- For family coverage, 17% of covered workers are employed at a firm with a family premium at least 20% higher than the average family premium, while 19% of covered workers are at firms with a family premium less than 80% of the average family premium [Figure 1.9].
- Nine percent of covered workers are employed at a firm with an average annual premium of at least $12,500 for single coverage [Figure 1.10]. Fifteen percent of covered workers are employed at a firm with an average annual premium of at least $33,000 for family coverage [Figure 1.11].
Figure 1.9: Distribution of Annual Premiums for Single and Family Coverage Relative to the Average Annual Single or Family Premium, 2025
Figure 1.10: Distribution of Annual Premiums for Covered Workers With Single Coverage, 2025
Figure 1.11: Distribution of Annual Premiums for Covered Workers With Family Coverage, 2025
PREMIUM CHANGES OVER TIME
The average premiums for covered workers for single and family coverage increased 5% and 6% respectively from last year [Figure 1.12].
- The average premium for single coverage has grown 24% in the past five years [Figure 1.12].
- The $26,993 average family premium in 2025 is 26% higher than the average family premium in 2020 and 53% higher than the average family premium in 2015. The 26% family premium growth in the past five years is similar to the 21% growth between 2015 and 2020 [Figure 1.15].
- The average family premiums for covered workers at firms with 10 to 199 workers and at larger firms have grown at similar rates since 2020 (26% at firms with 10 to 199 workers and 26% at larger firms). For firms with 10 to 199 workers, the average family premium rose from $20,616 in 2020 to $26,054 in 2025. For larger firms, the average family premium rose from $21,691 in 2020 to $27,280 in 2025 [Figure 1.13].
- The average family premiums for covered workers at firms with 10 to 199 workers and at larger firms have grown at similar rates since 2015 (53% at firms with 10 to 199 workers and 52% at larger firms). For firms with 10 to 199 workers, the average family premium rose from $16,977 in 2020 to $26,054 in 2025. For larger firms, the average family premium rose from $17,938 in 2020 to $27,280 in 2025 [Figure 1.13].
- Over the past five years, the average family premium for covered workers at large firms that are fully insured has grown at a similar rate to the average family premium for covered workers in fully or partially self-funded plan (27% for fully-insured plans and 26% for self-funded firms) [Figure 1.14].
- The average family premium grew 6% in 2025 while the rate of inflation was 2.7%. Over the last 5 years, family premiums grew 26%, similar to the rate of inflation during this period (23.5%). Over the last ten years, the growth in the average premium for family coverage far outpaced inflation (53% vs. 35.8%) [Figure 1.15].
- The average family premium grew 6% in 2025 while wages grew 4%. Over the last 5 years, family premiums grew 26%, similar to the 28.6% growth in wages. Over the last ten years, the average family premium and average wages grew at roughly comparable rates (53% vs. 48.2%) [Figure 1.15].
Figure 1.12: Average Annual Premiums for Single and Family Coverage, 1999-2025
Figure 1.13: Average Annual Premiums for Covered Workers With Family Coverage, by Firm Size, 1999-2025
Figure 1.14: Among Workers in Large Firms, Average Annual Premiums for Family Coverage, by Funding Arrangement, 1999-2025
Figure 1.15: Cumulative Premium Increases, Inflation, and Earnings for Covered Workers With Family Coverage, 2000-2025
Health Benefits Offer Rates
Nearly all (97%) firms with 200 or more workers offer health benefits to at least some workers, while almost two in three (59%) smaller firms do. Almost all (96%) firms that offer health benefits offer both single and family coverage.
Firms with fewer than 200 workers that do not offer health benefits say the most important reason they do not offer coverage is that the “cost of insurance is too high”.
This year, the survey sample frame changed from including firms with 3 or more employees to only those with 10 or more employees. Since the majority of firms have fewer than 10 employees, this change will affect certain statistics, such as offer rates, which are weighted by the number of firms. Historically, offer rates have been lower among firms with 3 to 9 employees. As a result, excluding these smaller firms will lead to higher overall offer rates compared to previous years. Additionally, because many non-offering employers fell within the 3 to 9 employee range, their removal will affect estimates based on responses from firms that do not offer coverage. For more information, see the Methods section.
FIRM OFFER RATES
- In 2025, 61% of firms with 10 or more workers offer health benefits, similar to the percentage last year (65%) but lower than the percentage (68%) five years ago.
- Among smaller firms (10 to 199 workers), the likelihood of offering health benefits increases with firm size: 51% of firms with 10-24 workers, 64% of firms with 25-49 workers, and 89% of firms with 50-199 workers offer health benefits to at least some of their workers [Figure 2.3].
- The percentage of firms with 10 to 199 workers that offer health benefits (59%) is similar to the percentage last year (64%) but lower than the percentage (67%) five years ago.
- Over ninety percent (91%) of firms with 50 or more workers offer health benefits in 2025; this percentage has remained over ninety percent for each of the last 10 years.
- A large majority of firms are small, so the fluctuation we see across years in the small firm offer rate drives fluctuations in the overall offer rate. Most workers, however, work for larger firms, where offer rates are much higher.
- Among firms with 200 or more workers, 96% of firms with 200 to 999 workers and over 99% of firms with 1,000 or more workers offer health benefits to at least some of their workers. These percentages are similar to those last year.
- Because most workers are employed by larger firms, most workers work at a firm that offers health benefits to at least some of its employees. In 2025, 91% of all workers are employed by a firm that offers health benefits to at least some of its workers. This percentage is similar to the percentages last year (92%) and five years ago (92%)[Figure 2.4].
Figure 2.1: Percentage of Firms Offering Health Benefits, by Firm Size, 1999-2025
Figure 2.2: Percentage of Firms Offering Health Benefits, by Firm Size, Region, and Industry, 2025
Figure 2.3: Percentage of Firms and Workers at Firms Offering Health Benefits,
Figure 2.4: Percentage of Workers at Firms That Offer Health Benefits to at Least Some Workers, by Firm Size, 1999-2025
OFFERS TO SPOUSES AND DEPENDENTS
- Almost all firms that offer health benefits offer family coverage; in 2025, nearly all firms with 200 or more workers and 96% of smaller firms that offer health benefits offer family coverage to their workers [Figure 2.5].
- The vast majority of firms with 10 or more workers that offer health benefits offer them to spouses and dependents, such as children. Ninety-six percent of firms with 10 to 199 workers and virtually all larger firms that offer health benefits offer coverage to spouses. These percentages are similar to the percentages in 2024 [Figure 2.7].
- Ninety-six percent of firms with 10 to 199 workers and virtually all larger firms that offer health benefits offer coverage to dependents other that spouses, such as children. These percentages are similar to the percentages in 2024 [Figure 2.7].
- Five percent of firms with 10 to 49 workers offering health benefits offer only single coverage to their workers, similar to the percentage as last year [Figure 2.7].
Figure 2.5: Percentage of Firms Offering Health Benefits Which Offer Family Coverage, by Firm Size, 2025
Figure 2.6: Percentage That Offer to Spouses and Dependents, by Firm Size, 2025
PART-TIME WORKERS
Among firms that offer health benefits, relatively few offer benefits to part-time workers.
The Affordable Care Act (ACA) defines “full-time” workers as those who work an average of at least 30 hours per week, and “part-time” workers as those who work fewer than 30 hours. The employer shared responsibility provision of the ACA requires that firms with at least 50 full-time equivalent employees offer most of their full-time employees coverage that meets minimum standards or be assessed a penalty.8
- Twenty-seven percent of firms with 200 or more workers that offer health benefits in 2025 offer health benefits to part-time workers, similar to the percentage (26%) that did so in 2024 [Figure 2.7]. The share of firms with 200 or more workers that offer health benefits to part-time workers increases with firm size [Figure 2.8].
Figure 2.7: Among Firms Offering Health Benefits, Percentage That Offer to Part-Time Workers, by Firm Size, 1999-2025
Figure 2.8: Among Firms Offering Health Benefits, Percentage That Offer to Part-Time Workers, by Firm Size, 2025
ICHRA AND ASSISTING EMPLOYEES WITH PURCHASING COVERAGE IN THE NON-GROUP MARKET
Some employers provide funds to some or all of their employees to help them purchase coverage in the individual (“non-group”) market. Employers that do not otherwise offer health benefits may offer these funds as an alternative to offering a group plan. Additionally, employers that offer a group plan to some employees may use this approach for other types or classes of workers, such as those working part time or remotely. One way an employer can provide tax-preferred assistance for employees to purchase non-group coverage is through an Individual Coverage Health Reimbursement Arrangement, or ICHRA. Both employers that offer and those that do not offer health benefits were asked if they provide funds to any employee to purchase non-group coverage. Starting in 2025, we revised the question wording to include contributions through a Qualified Small Employer Health Reimbursement Arrangement, or QSEHRA.
- Four percent of firms that offer health benefits, and 9% of firms that do not offer health benefits, offer funds to one or more of their employees to purchase non-group coverage in 2025 [Figure 2.9].
- Among firms with 10 to 199 workers that do not offer health benefits, 9% offered funds to one or more of their employees to purchase non-group coverage, a similar percentage (11%) as last year [Figure 2.11].
- Firms that do not offer funds to any employees to purchase non-group coverage in 2025 were asked if they were likely to do so in the next two years.
- Among firms with 10 or more workers that offer health benefits, 2% say they are “very likely” and an additional 6% are “somewhat likely” to offer an ICHRA to at least some employees in the next two years [Figure 2.10].
- Among firms with 10 to 199 workers that do not offer health benefits, 2% say they are “very likely” and an additional 16% say they are “somewhat likely” to offer an ICHRA to at least some employees in the next two years [Figure 2.12].
Figure 2.9: Among Firms Offering Health Benefits, Percentage of Firms That Provide Workers Funds to Purchase Non-Group Insurance, Such As Through an ICHRA, by Firm Size, 2025
Figure 2.10: Likelihood of Offering an ICHRA in the Next Two Years Among Firms That Offer Health Benefits But Do Not Currently Offer an ICHRA, by Firm Size, 2025
Figure 2.11: Among Small Firms Not Offering Health Benefits, Percentage Providing Funds for Employees to Purchase Non-Group Insurance, 2012-2025
Figure 2.12: Likelihood of Offering an ICHRA in the Next Two Years Among Small Firms Not Offering Health Benefits, 2021-2025
Figure 2.13: Among Firms Providing Employees Funds for the Non-Group Market, Method of Determining Contribution Amount, by Firm Size 2025
FIRMS NOT OFFERING HEALTH BENEFITS
Firms that do not offer health benefits were asked several questions, including whether they have offered insurance or shopped for insurance in the recent past, what their most important reasons for not offering coverage are, and their opinion on whether their employees would prefer an increase in wages or health insurance if additional funds were available to increase their compensation. Because such a small percentage of larger firms report not offering health benefits, we present responses only for firms with 10 to 199 workers that do not offer health benefits.
- The “cost of insurance is too high” is the most common reasons small firms cite for not offering health benefits. Among small firms asked about the most important reason for not offering health benefits, 41% say the “cost of insurance is too high,” 15% say the “firm is too small,” 15% say that their “employees are covered under another plan, including coverage on a spouse’s plan,” 7% say that “their employees will get a better deal on the health insurance exchanges,” 7% say that “most employees are part-time or temporary workers”, and 6% say their “employees are not interested.” [Figure 2.14]
- Some small non-offering firms have either offered health insurance in the past five years or shopped for health insurance in the past year.
- Fourteen percent of small non-offering firms have offered health benefits in the past five years [Figure 2.15]. Among these small non-offering firms, 22% stopped offering coverage within the past year.
- Sixteen percent of small non-offering firms have shopped for coverage in the past year, similar to the percentage last year (15%) [Figure 2.15].
- Eighty-one percent of small firms not offering health benefits agreed with the statement that their employees would prefer a two dollar per hour increase in wages rather than health insurance [Figure 2.1].
Figure 2.14: Among Small Firms Not Offering Health Benefits, Most Important Reason for Not Offering, 2025
Figure 2.15: Among Small Firms Not Offering Health Benefits, Percentage of Firms That Report the Following Actions, 2009-2025
Figure 2.16: Among Small Firms Not Offering Health Benefits, Firms’ View of Employees’ Preference for Higher Wages or Health Insurance Benefits, 2008-2025
- Employer Responsibility Under the Affordable Care Act. KFF. https://www.kff.org/infographic/employer-responsibility-under-the-affordable-care-act/.↩︎
Employee Coverage, Eligibility, and Participation
Employers are the principal source of health insurance in the United States, providing health benefits for 154 million non elderly people.9 Most workers are offered health coverage at work, and most of the workers who are offered coverage take it. Workers may not be covered by their own employer for several reasons: their employer may not offer coverage, they may not be eligible for the benefits offered by their firm, they may elect to receive coverage from another source (such as through their spouse’s employer), or they may just refuse the offer of coverage from their firm. In 2025, 61% of workers in firms offering health benefits are covered by their own firm, similar to the percentages last year, five years ago, and ten years ago.
ELIGIBILITY
- Some workers employed at firms that offer health benefits may not be eligible to participate. Many firms, for example, do not offer coverage to part-time or temporary workers10. Among workers in firms offering health benefits in 2025, 80% are eligible to enroll in the benefits offered by their firm, similar to the percentages last year, five years ago, and ten years ago [Figure 3.1].
- Eligibility varies considerably with firm wage level. Workers in firms with a relatively large share of lower-wage workers (where at least 35% of workers earn $37,000 a year or less) have a lower average eligibility rate than workers in firms with a smaller share of lower-wage workers (67% vs. 83%) [Figure 3.6].
- Workers in firms with a relatively large share of higher-wage workers (where at least 35% earn $80,000 or more annually) have a higher average eligibility rate than workers in firms with a smaller share of higher-wage workers (89% vs. 75%) [Figure 3.6].
- Eligibility also varies by the age of the workforce within firms. Those in firms with a relatively small share of younger workers (where fewer than 35% of the workers are age 26 or younger) have a higher average eligibility rate than those in firms with a larger share of younger workers (83% vs. 60%). Those in firms with a relatively large share of older workers (where more than 35% of the workers are age 50 or older) have a higher average eligibility rate than those in firms with a smaller share of older workers (84% vs. 77%) [Figure 3.6].
- Eligibility rates vary considerably for workers in different industries. The average eligibility rate remains particularly low for workers in retail firms (53%) [Figure 3.3].
Figure 3.1: Eligibility, Take-Up, and Coverage Rates for Workers in Firms Offering Health Benefits, by Firm Size, 1999-2025
Figure 3.2: Eligibility and Coverage Rates for Workers in Firms Offering Health Benefits, 1999-2025
Figure 3.3: Eligibility, Take-Up, and Coverage Rates in Firms Offering Health Benefits, by Firm Size, Region, and Industry, 2025
Figure 3.4: Eligibility, Take-Up, and Coverage Rates in Firms Offering Health Benefits, by Firm Size, 2025
Figure 3.5: Among Workers at Small Firms, Eligibility for Workers at Their Own Firms, 1999-2025
Figure 3.6: Among Workers in Firms Offering Health Benefits, Percentage of Workers Eligible for Health Benefits Offered by Their Firm, by Firm Characteristics, 2025
TAKE-UP RATE
- On average, 76% of eligible workers take up coverage when it is offered to them, the same percentage as last year [Figure 3.7].
- Eligible workers in firms with 10 to 199 workers have a lower average take up rate than those in larger firms (72% vs. 77%) [Figure 3.8].
- Eligible workers in firms with a relatively large share of lower-wage workers have a lower average take up rate than those in firms with a smaller share of lower-wage workers (65% vs. 77%) [Figure 3.7].
- Eligible workers in firms with a relatively large share of higher-wage workers have a higher average take up rate than those in firms with a smaller share of higher-wage workers (80% vs. 73%) [Figure 3.7].
- Eligible workers in private, for-profit firms have a lower average take up rate (73%) and eligible workers in public firms have a higher average take up rate (86%) than workers in other firm types [Figure 3.7].
- Eligible workers in firms with some union workers have a higher average take up rate (80%) than eligible workers in firms with no union workers (74%) [Figure 3.7].
- Eligible workers in firms with 10 to 199 workers have a lower average take up rate than those in larger firms (72% vs. 77%) [Figure 3.8].
- The average percentages of eligible workers taking up benefits in offering firms also varies across industries [Figure 3.3].
- The share of eligible workers taking up benefits in offering firms (76%) is similar to the share in 2020 (78%) but lower than the share in 2015 (79%) [Figure 3.1].
Figure 3.7: Among Workers in Firms Offering Health Benefits, Percentage of Eligible Workers Who Take Up Health Benefits Offered by Their Firm, by Firm Characteristics, 2025
Figure 3.8: Among Workers in Firms Offering Health Benefits, Percentage of Eligible Workers Who Take Up Health Benefits Offered by Their Firm, by Firm Size, 1999-2025
COVERAGE
- In 2025, the percentage of workers at firms offering health benefits covered by their firm’s health plan is 61%, the same percentage as last year [Figure 3.10].
- The coverage rate at firms offering health benefits is similar for smaller firms (10 to 199 workers) and larger firms in 2025. These rates are similar to the rates last year for both smaller firms and larger firms [Figure 3.1].
- There is significant variation by industry in the coverage rate among workers in firms offering health benefits. The average coverage rate is particularly low in the retail industry (34%) [Figure 3.3].
- The coverage rate also varies with firm wage levels. Among workers in firms offering health benefits, those in firms with a relatively large share of lower-wage workers are less likely to be covered by their own firm than workers in firms with a smaller share of lower-wage workers (43% vs. 64%). A similar pattern exists in firms with a relatively large share of higher-wage workers, with workers in these firms being more likely to be covered by their employer’s health benefits than those in firms with a smaller share of higher-wage workers (71% vs. 55%) [Figure 3.9].
- The age distribution of workers is also related to variation in coverage rates. Among workers in firms offering health benefits, those in firms with a relatively small share of younger workers are more likely to be covered by their own firm than those in firms with a larger share of younger workers (64% vs. 39%). Similarly, workers in offering firms with a relatively large share of older workers are more likely to be covered by their own firm than those in firms with a smaller share of older workers (66% vs. 56%) [Figure 3.9].
- Among workers in firms offering health benefits, those working in public firms are more likely than workers in other firm types to be covered by their own firm [Figure 3.9].
- Among workers in all firms, including those that offer and those that do not offer health benefits, 55% are covered by health benefits offered by their employer, similar to the percentages last year (57%) and ten years ago (59%) but lower than five years ago (59%) [Figure 3.10].
Figure 3.9: Among Workers in Firms Offering Health Benefits, Percentage of Workers Covered by Health Benefits Offered by Their Firm, by Firm Characteristics, 2025
Figure 3.10: Percentage of Workers Covered by Their Firm’s Health Benefits, 1999-2025
Figure 3.11: Percentage of All Workers Covered by Their Firm’s Health Benefits, Both in Firms Offering and Not Offering Health Benefits, by Firm Size, 1999-2025
WAITING PERIODS
- Waiting periods are a specified length of time after beginning employment before a worker is eligible to enroll in health benefits. With some exceptions, the Affordable Care Act (ACA) requires that waiting periods cannot exceed 90 days. For example, employers are permitted to have orientation periods before the waiting period begins which, in effect, means a worker is not eligible for coverage three months after being hired. If a worker is eligible to enroll on the 1st of the month after three months of employment, this survey rounds up and considers the firm’s waiting period four months. For these reasons, some employers still have waiting periods exceeding the 90-day maximum.
- Sixty-eight percent of covered workers are in firms where they face a waiting period before coverage is available, similar to the percentage in 2023, the last time we asked this question [Figure 3.14]. Covered workers in firms with 10 to 199 workers are more likely than those in larger firms to have a waiting period (79% vs. 64%) [Figure 3.12].
- The average waiting period among covered workers who face a waiting period is 1.8 months [Figure 3.12]. A small percentage (5%) of covered workers with a waiting period have a waiting period of more than 3 months.
Figure 3.12: Percentage of Covered Workers in Firms With a Waiting Period for Coverage and Average Waiting Period in Months, by Firm Size, Region, and Industry, 2025
Figure 3.13: Distribution of Covered Workers With the Following Waiting Periods for Coverage, by Firm Size, 2025
Figure 3.14: Percentage of Covered Workers in Firms With a Waiting Period for Coverage, by Firm Size, 2002-2025
Figure 3.15: Among Covered Workers With a Waiting Period for Health Benefits, Average Waiting Period in Months, by Firm Size, 2002-2025
- KFF. Health Insurance Coverage of the Non elderly [Internet]. San Francisco (CA): KFF; 2023 [cited 2025 Aug 5. Available from: https://www.kff.org/other/state-indicator/nonelderly-0-64/.↩︎
- See Section 2 for part-time and temporary worker offer rates.↩︎
Types of Plans Offered
Most firms (66%) that offer health benefits offer only one type of health plan. Firms with 200 or more workers are more likely than smaller firms to offer more than one plan type.
NUMBER OF PLAN TYPES OFFERED
- Among firms that offer health benefits, 66% offer only one type of health plan in 2025. Firms with 200 or more workers are more likely than smaller firms to offer more than one plan type (63% vs. 32%) [Figure 4.1].
- While most firms are small, most workers work for larger firms and are more likely to be offered more than one type of health plan. Sixty-eight percent of covered workers in 2025 are employed in a firm that offers more than one type of health plan. Seventy-seven percent of covered workers in firms with 200 or more workers are employed by a firm that offers more than one plan type, compared to 40% of covered workers in smaller firms [Figure 4.2].
- Seventy percent of covered workers in firms that offer health benefits work in firms that offer one or more PPOs; 68% work in firms that offer one or more HDHP/SOs; 19% work in firms that offer one or more HMOs; 12% work in firms that offer one or more POS plans; and 1% work in firms that offer one or more conventional plans [Figure 4.4].
- Among covered workers in firms offering only one type of health plan, 52% are in firms that offer only PPOs and 26% are in firms that offer only HDHP/SOs [Figure 4.5].
Figure 4.1: Among Firms Offering Health Benefits, Percentage of Firms That Offer One, Two, or Three or More Plan Types, by Firm Size, 2025
Figure 4.2: Among Firms Offering Health Benefits, Percentage of Covered Workers in Firms Offering One, Two, or Three or More Plan Types, by Firm Size, 2025
Figure 4.3: Among Firms Offering Health Benefits, Percentage of Firms That Offer the Following Plan Types, by Firm Size, 2025
Figure 4.4: Among Firms Offering Health Benefits, Percentage of Covered Workers in Firms That Offer the Following Plan Types, by Firm Size, 2025
Figure 4.5: Among Firms Offering Only One Type of Health Plan, Percentage of Covered Workers in Firms That Offer the Following Plan Type, by Firm Size, 2025
The survey collects information on a firm’s plan with the largest enrollment in each of the plan types. While we know the number of plan types a firm has, we do not know the total number of plans a firm offers workers. In addition, firms may offer different types of plans to different workers. For example, some workers might be offered one type of plan at one location, while workers at another location are offered a different type of plan.
- HMO
- is a health maintenance organization. The survey defines an HMO as a plan that does not cover non-emergency out-of-network services.
- PPO
- is a preferred provider organization. The survey defines PPOs as plans that have lower cost sharing for in-network provider services, and do not require a primary care gatekeeper to screen for specialist and hospital visits.
- POS
- is a point-of-service plan. The survey defines POS plans as those that have lower cost sharing for in-network provider services, but do require a primary care gatekeeper to screen for specialist and hospital visits.
- HDHP/SO
- is a high-deductible health plan with a savings option such as an HRA or HSA. HDHP/SOs are treated as a distinct plan type even if the plan would otherwise be considered a PPO, HMO, POS plan, or indemnity plan. These plans have a deductible of at least $1,000 for single coverage and $2,000 for family coverage and are offered with an HRA, or are HSA-qualified. See Section 8 for more information on HDHP/SOs.
- Conventional/Indemnity
- The survey defines conventional or indemnity plans as those that have no preferred provider networks and the same cost sharing regardless of physician or hospital.
Market Shares of Health Plans
Health plans are often characterized into plan types based on their coverage for out-of-network services and their use of primary care gate keeping. In 2025, PPOs remain the most common plan type.
- Forty-six percent of covered workers are enrolled in PPOs in 2025, followed by HDHP/SOs (33%), HMOs (12%), POS plans (9%), and conventional plans (less than one percent). All of these percentages are similar to the enrollment percentages in 2024 [Figure 5.1].
- The percentage of covered workers enrolled in HDHP/SOs is similar to last year (28%) and five years ago (31%), but higher than the percentage 10 years ago (25%). The percentage of covered workers enrolled in PPOs has decreased 6% over the past decade [Figure 5.1].
- The percentage of covered workers enrolled in HMOs (12%) is similar to the percentages last year (14%) and five years ago (13%) [Figure 5.1].
- A larger share of covered workers are enrolled in HDHP/SOs than in HMOs in both smaller firms (10 to 199 workers) and larger firms (200 or more workers) [Figure 5.2].
- The share of covered workers enrolled in an HDHP/SO plan is larger in firms with 200 or more workers than the share in smaller firms (35% and 26%). The share of covered workers enrolled in a POS plan is larger in firms with 10 to 199 workers than the share in larger firms (19% vs. 6%) [Figure 5.2].
- Plan enrollment patterns also differ across regions.
- Covered workers in the West (24%) are more likely to be enrolled in a HMO than workers in other regions while covered workers in the Midwest (7%) and South (9%) are less likely to be enrolled in an HMO [Figure 5.3].
- Covered workers in the Midwest (40%) are more likely to be enrolled in HDHP/SOs than workers in other regions [Figure 5.3].
- Covered workers in the South (53%) are more likely to be enrolled in a PPO plan than workers in other regions and covered workers in the West (37%) are less likely to be enrolled in a PPO plan [Figure 5.3].
Figure 5.1: Distribution of Health Plan Enrollment for Covered Workers, by Plan Type, 1988-2025
Figure 5.2: Distribution of Health Plan Enrollment for Covered Workers, by Plan Type and Firm Size, 2025
Figure 5.3: Distribution of Health Plan Enrollment for Covered Workers, by Firm Size, Region, and Industry, 2025
Worker and Employer Contributions for Premiums
The vast majority of covered workers make contributions towards the cost of their coverage.
- In 2025, the average contribution amounts for covered workers are 16% of the premium for single coverage and 26% of the premium for family coverage, the same as the levels last year [Figure 6.1].11
- Covered workers in firms with 10 to 199 workers contribute, on average, a much higher percentage of the premium for family coverage than covered workers in larger firms (36% vs. 23%) [Figure 6.2].
- The average contribution percentage for single coverage is the same for covered workers in firms with 10 to 199 workers and those in larger firms [Figure 6.2].
- The average contribution amount for covered workers for single coverage is $120 per month ($1,440 annually), similar to the amount last year [Figure 6.4]. The average contribution amount for covered workers for family coverage is $571 per month ($6,850 annually), higher than the amount ($6,366 annually) last year [Figure 6.5].
- The average contribution amount for covered workers for family coverage in firms with 10 to 199 workers is much higher than the average contribution amount for covered workers in larger firms ($8,889 vs. $6,227) [Figure 6.7].
- The average contribution amount for family coverage for covered workers enrolled in HDHP/SOs is lower than the overall average contribution amount for covered workers ($5,815 vs. $6,850) [Figure 6.6].
- The average contribution amount for covered workers for family coverage in firms with 10 to 199 workers is much higher than the average contribution amount for covered workers in larger firms ($8,889 vs. $6,227) [Figure 6.7].
Figure 6.1: Average Percentage of Premium Paid by Covered Workers for Single and Family Coverage, 1999-2025
Figure 6.2: Average Percentage of Premium Paid by Covered Workers for Single and Family Coverage, by Firm Size, 2025
Figure 6.3: Average Monthly Worker Premium Contributions for Single and Family Coverage, 1999-2025
Figure 6.4: Average Annual Worker and Employer Contributions to Premiums and Total Premiums for Single Coverage, 1999-2025
Figure 6.5: Average Annual Worker and Employer Contributions to Premiums and Total Premiums for Family Coverage, 1999-2025
Figure 6.6: Average Annual Worker and Employer Premium Contributions and Total Premiums for Single and Family Coverage, by Plan Type, 2025
Figure 6.7: Average Annual Worker and Employer Premium Contributions and Total Premiums for Single and Family Coverage, by Firm Size, 2025
Figure 6.8: Average Annual Worker and Employer Premium Contributions and Total Premiums for Single Coverage, by Plan Type and Firm Size, 2025
Figure 6.9: Average Annual Employer and Worker Premium Contributions and Total Premiums for Family Coverage, by Plan Type and Firm Size, 2025
DISTRIBUTIONS OF WORKER CONTRIBUTIONS TO THE PREMIUM
Almost nine in ten (89%) of covered workers are in a plan where the employer contributes at least half of the premium for both single and family coverage.
- Twelve percent of covered workers are in a plan where the employer pays the entire premium for single coverage, while only 3% of covered workers are in a plan where the employer pays the entire premium for family coverage [Figure 6.10].
- Covered workers in firms with 10 to 199 workers are much more likely than covered workers in larger firms to be in a plan where the employer pays the entire premium for single coverage.
- Twenty-nine percent of covered workers in firms with 10 to 199 workers are in a firm where their employer pays the full premium for single coverage, compared to 7% of covered workers in larger firms [Figure 6.10].
- For family coverage, 9% of covered workers in firms with 10 to 199 workers have an employer that pays the full premium, compared to 1% of covered workers in larger firms [Figure 6.10].
- Eleven percent of covered workers are in a plan where the worker contributes more than half of the premium for family coverage [Figure 6.10].
- This percentage differs significantly with firm size. Twenty-nine percent of covered workers in firms with 10 to 199 workers are in a plan where the worker contribution for family coverage is more than half of the premium, compared to 5% of covered workers in larger firms [Figure 6.10].
- Small shares of covered workers in firms with 10 to 199 workers (4%) or in larger firms (1%) are in a plan where the worker must contribute more than 50% of the premium for single coverage [Figure 6.10].
- There is substantial variation in the dollar amounts that covered workers must contribute towards health coverage.
- Among covered workers in firms with 10 to 199 workers, 34% have a contribution for single coverage of less than $500 a year, while 29% have a contribution of $2,000 or more [Figure 6.13]. For family coverage, 12% have a contribution of less than $1,500, while 33% have a contribution of $10,500 or more [Figure 6.14].
- Among covered workers in firms with 200 or more workers, 13% contribute less than $500 a year for single coverage, while 23% have a contribution of $2,000 or more [Figure 6.13]. For family coverage, only 3% contribute less than $1,500 a year, while 9% have a contribution of $10,500 or more [Figure 6.14].
Figure 6.10: Distribution of Percentage of Premium Paid by Covered Workers for Single and Family Coverage, by Firm Size, 2025
Figure 6.11: Distribution of Percentage of Premium Paid by Covered Workers for Single Coverage, 2002-2025
Figure 6.12: Distribution of Percentage of Premium Paid by Covered Workers for Family Coverage, 2002-2025
Figure 6.13: Distribution of Worker Contributions for Single Coverage, by Firm Size, 2025
Figure 6.14: Distribution of Worker Contributions for Family Coverage, by Firm Size, 2025
DIFFERENCES BY FIRM CHARACTERISTICS
The average share of the premium paid by covered workers varies with firm characteristics.
- Covered workers in private, for-profit firms have relatively high average contribution rates for single coverage (19%) and for family coverage (28%). Covered workers in public firms have relatively low average premium contribution rates for single coverage (10%) and for family coverage (22%) [Figure 6.17].
- Covered workers in firms with relatively large shares of younger workers (where at least 35% are age 26 or younger) have a higher average contribution rate for family coverage than those in firms with smaller shares of older workers (31% vs. 26%) [Figure 6.17].
- Covered workers in firms with relatively large shares of lower-wage workers (where at least 35% earn $37,000 or less annually) have higher average contribution rates than those in firms with smaller shares of higher-wage workers for both single coverage (19% vs. 16%) and family coverage (31% vs. 26%) [Figure 6.17].
- Covered workers in firms with relatively large shares of higher-wage workers (where at least 35% earn $80,000 or more annually) have a lower average contribution rate for family coverage than those in firms with a smaller share of higher-wage workers (24% vs. 28%) [Figure 6.17].
- Covered workers in firms that have at least some union workers have a lower average contribution rate for family coverage than those in firms without any union workers (21% vs. 29%) [Figure 6.17].
- Covered workers in large firms that are fully insured have a higher average contribution rate for family coverage than those in firms with self-funded plans (28% vs. 22%) [Figure 6.17].
Figure 6.15: Distribution of the Percentage of Total Premium Paid by Covered Workers for Single and Family Coverage, by Firm Wage Level, 2025
Figure 6.16: Average Annual Worker and Employer Contributions to Premiums and Total Premiums for Single and Family Coverage, by Firm Wage Level, 2025
Figure 6.17: Average Annual Premium Contributions Paid by Covered Workers for Single and Family Coverage, by Firm Characteristics, 2025
Figure 6.18: Average Percentage of Family Premium Paid by Covered Workers, by Firm Characteristics, 2025
Figure 6.19: Average Percentage of Premium Paid by Covered Workers, by Firm Characteristics and Size, 2025
DIFFERENCES BY REGION AND INDUSTRY
The average worker contribution rate for single coverage is relatively low in the West (14%) [Figure 6.20].
The average worker contribution rate for family coverage is relatively low in the Northeast (22%) and the Midwest (24%) and relatively high in the South (29%) [Figure 6.20].
Average worker contribution rates vary across industries for both single and family coverage [Figure 6.21].
Figure 6.20: Average Premium Paid by Covered Workers for Single and Family Coverage, by Plan Type and Region, 2025
Figure 6.21: Average Percentage of Premium Paid by Covered Workers, by Industry, 2025
CHANGES OVER TIME
The average worker contribution amount in 2025 for single coverage ($1,440) is similar to the amount last year ($1,408). The average worker contribution amount for family coverage ($6,850) is higher than the amount last year ($6,366) [Figure 6.4] and [Figure 6.5].
- Over the last five years, the average worker contribution amount for single coverage has increased 16% and the average worker contribution for family coverage increased 23%.
- Over the last 10 years, the average worker contribution amount for single coverage has increased 31% and the average worker contribution amount for family coverage has increased 37% [Figure 6.4] and [Figure 6.5].
Figure 6.22: Average Annual Worker Contributions for Covered Workers With Single Coverage, by Firm Size, 1999-2025
Figure 6.23: Average Annual Worker Contributions for Covered Workers With Family Coverage, by Firm Size, 1999-2025
Figure 6.24: Average Percentage of Premium Paid by Covered Workers for Single and Family Coverage, by Firm Size, 1999-2025
Figure 6.25: Among Large Firms, Average Annual Worker Contributions for Covered Workers With Family Coverage, by Firm Wage Level, 1999-2025
- The average percentage contribution is calculated as a weighted average of all a firm’s plan types and may not necessarily equal the average worker contribution divided by the average premium.↩︎
Employee Cost Sharing
In addition to any required premium contributions, most covered workers must pay a share of the cost for the medical services they use. The most common forms of cost sharing are deductibles (an amount that must be paid before most services are covered by the plan), copayments (fixed dollar amounts), and coinsurance (a percentage of the charge for services). Some plans combine cost-sharing forms, such as requiring coinsurance for a service up to a maximum amount, or assessing either coinsurance or a copayment for a service, whichever is higher. The type and level of cost-sharing may vary with the type of plan in which the worker is enrolled. Cost sharing may also vary by the type of service, with separate classifications for office visits, hospitalizations, or prescription drugs.
The cost-sharing amounts reported here are for covered workers using in-network services. Plan enrollees receiving services from providers that do not participate in plan networks often face higher cost-sharing and may be responsible for charges that exceed the plan’s allowable amounts. The framework of this survey does not allow us to capture all of the complex cost-sharing requirements in modern plans, including ancillary services (such as durable medical equipment or physical therapy) or cost-sharing arrangements that vary across different settings (such as tiered networks). Therefore, we do not collect information on all plan provisions and limits that affect enrollee out-of-pocket liability.
GENERAL ANNUAL DEDUCTIBLES FOR WORKERS IN PLANS WITH DEDUCTIBLES
We consider a general annual deductible to be an amount that must be paid by enrollees before most services are covered by their health plan. Non-grandfathered health plans are required to cover some services, such as preventive care, without cost-sharing. Some plans require enrollees to meet a specific deductible for certain services, like prescription drugs or hospital admissions, in lieu of or in addition to a general annual deductible. As discussed below, some plans with a general annual deductible for most services exclude specified classes of care from the deductible, such as prescriptions or physician office visits.
- Eighty-eight percent of covered workers in 2025 are enrolled in a plan with a general annual deductible for single coverage, similar to the percentage last year (88%) but higher than the percentages five years ago (83%) and ten years ago (81%) [Figure 7.2].
- The percent of covered workers enrolled in a plan with a general annual deductible for single coverage is the same for covered workers in firms with 10 to 199 workers (88%) and for those in larger firms (88%) [Figure 7.2].
- The likelihood of a plan having a general annual deductible varies by plan type. Forty-seven percent of covered workers in HMOs do not have a general annual deductible for single coverage, compared to 14% of workers in POS plans and 12% of workers in PPOs [Figure 7.1].
- For workers with single coverage in a plan with a general annual deductible, the average annual deductible is $1,886, similar to the average deductible last year ($1,773) [Figure 7.3] and [Figure 7.8].
- For covered workers in plans with a general annual deductible, the average deductibles for single coverage are $1,649 in HMOs, $1,337 in PPOs, $2,122 in POS plans, and $2,609 in HDHP/SOs [Figure 7.6].
- The average deductibles for single coverage are higher for covered workers at firms with 10 to 199 workers than at larger firms across plan types. For covered workers in PPOs, the most common plan type, the average deductibles for single coverage are $2,012 in firms with 10 to 199 workers and $1,145 in firms with 200 or more workers [Figure 7.6]. Overall, for covered workers in plans with a general annual deductible, the average deductible for single coverage at firms with 10 to 199 workers ($2,631) is higher than the average deductible at larger firms ($1,670) [Figure 7.3].
- The average general annual deductible for single coverage ($1,886) for workers in plans with a deductible is higher than the amounts five years ago ($1,617) and ten years ago ($1,320) [Figure 7.8].
Figure 7.1: Percentage of Covered Workers With No General Annual Deductible for Single Coverage, by Plan Type and Firm Size, 2025
Figure 7.2: Percentage of Covered Workers in a Plan That Includes a General Annual Deductible for Single Coverage, by Plan Type and Firm Size, 2006-2025
Figure 7.3: Percentage of Covered Workers in a Plan That Includes a General Annual Deductible and Average Deductible for Single Coverage, by Firm Size and Region, 2025
Figure 7.4: Percentage of Covered Workers in a Plan That Includes a General Annual Deductible and Average Deductibles for Single Coverage, by Firm Characteristics, 2025
Figure 7.5: Among Covered Workers With No General Annual Deductible, Percentage Who Face Other Types of Cost Sharing, 2025
Figure 7.6: Among Covered Workers With a General Annual Deductible for Single Coverage, Average Deductible, by Plan Type and Firm Size, 2025
Figure 7.7: Percentage of Covered Workers With a General Annual Deductible for Single Coverage, 2006-2025
Figure 7.8: Among Covered Workers With a General Annual Deductible, Average Single and Family Coverage Deductible, by Plan Type, 2006-2025
GENERAL ANNUAL DEDUCTIBLES AMONG ALL COVERED WORKERS
As discussed above, the share of covered workers in plans with a general annual deductible has increased over time, from 81% in 2015 to 88% this year [Figure 7.7]. The average deductible amount for covered workers in plans with a deductible has also increased over this period, from $1,320 in 2015 to $1,886 in 2025 [Figure 7.10]. Neither trend by itself, however, captures the full impact that changes in deductibles have had on all covered workers. We can look at the average impact of both trends together by assigning a zero deductible value to covered workers in plans with no deductible and looking at how the resulting averages change over time. These average deductible amounts are lower in any given year than the averages for only people in plans with deductibles, but the changes over time reflect both workers facing higher monetary deductible amounts and a greater number of workers facing deductibles.
- Using this approach, the average general annual deductible for single coverage for all covered workers (with or without a deductible) in 2025 is $1,663, similar to the amount last year ($1,573) [Figure 7.10].
- The 2025 value is 23% higher than the average general annual deductible in 2020 ($1,350) and 54% higher than in 2015 ($1,078) [Figure 7.10].
- Another way to examine the impact of deductibles on covered workers is to look at the percent of all covered workers who are in a plan with a deductible that exceeds a certain amount. Thirty-four percent of covered workers are in plans with a general annual deductible of $2,000 or more for single coverage, similar to the percentages last year (32%) but higher than the amount five years ago (26%) [Figure 7.14].
- Workers at firms with 10 to 199 workers are considerably more likely to have a general annual deductible of $2,000 or more for single coverage than workers at larger firms (53% vs. 28%) [Figure 7.12].
Figure 7.9: Prevalence and Value of General Annual Deductibles for Single Coverage, by Firm Size, 2006-2025
Figure 7.10: Average General Annual Deductibles for Single Coverage, 2006-2025
Figure 7.11: Among Covered Workers Who Face a Deductible for Single Coverage, Average General Annual Deductible for Single Coverage, by Firm Size, 2006-2025
Figure 7.12: Percentage of Covered Workers Enrolled in a Plan With a High General Annual Deductible for Single Coverage, by Firm Size, 2025
Figure 7.13: Percentage of Covered Workers Enrolled in a Plan With a General Annual Deductible of $1,000 or More for Single Coverage, by Firm Size, 2009-2025
GENERAL ANNUAL DEDUCTIBLES AND ACCOUNT CONTRIBUTIONS
HDHP/SOs, which are defined by their relatively higher deductibles, have an important impact on the average deductible amounts across the market. The higher deductibles in these plans, however, often are paired with contributions to an HRA or an HSA funded by the employer, partially or sometimes fully offsetting the higher cost-sharing in these plans.
- Thirty-three percent of covered workers in an HDHP with an HRA and 3% of covered workers in an HSA-qualified HDHP receive an account contribution from their employer for single coverage that is at least equal to their deductible. Another 19% of covered workers in an HDHP with an HRA and 10% of covered workers in an HSA-qualified HDHP receive account contributions that, if applied to their deductible, would reduce the deductible to $1,000 or less [Figure 7.16].
- If we subtract employer account contributions from the general annual deductibles, the percent of covered workers with a deductible of $2,000 or more would be reduced from 34% to 26% [Figure 7.14] and [Figure 7.15].
Figure 7.14: Percentage of Covered Workers Enrolled in a Plan With a General Annual Deductible of $2,000 or More for Single Coverage, by Firm Size, 2009-2025
Figure 7.15: Percentage of Covered Workers Enrolled in a Plan With a High General Annual Deductible for Single Coverage, Reduced by Any HRA/HSA Contributions, by Firm Size, 2025
Figure 7.16: Among Covered Workers With a General Annual Deductible, Average General Annual Deductibles for Single Coverage, Reduced by Any HRA/HSA Contributions, by Plan Type and Firm Size, 2025
Figure 7.17: Among Covered Workers With a General Annual Deductible, Distribution of General Annual Deductibles for Single Coverage, Reduced by Any HRA/HSA Contributions, 2007-2025
Figure 7.18: Among Covered Workers With a General Annual Deductible, Distribution of General Annual Deductible for Single Coverage, 2007-2025
Figure 7.19: Among Covered Workers With a General Annual Deductible, Distribution of General Annual Deductibles for Single Coverage, by Plan Type, 2025
GENERAL ANNUAL DEDUCTIBLES FOR WORKERS ENROLLED IN FAMILY COVERAGE
General annual deductibles for family coverage are structured in two primary ways: (1) an aggregate family deductible, where the out-of-pocket expenses of all family members count against a specified family deductible amount and where the deductible is considered met when the combined family expenses exceed the deductible amount, or (2) a separate per-person family deductible, where each family member is subject to a specified deductible amount before the plan covers expenses for that member. Many plans with a per-person deductible, however, consider the deductible for all family members met once a certain number of family members (such as two or three) meet their specified deductible amount.12
- Forty-seven percent of covered workers in HMOs are in plans without a general annual deductible for family coverage. The percent of workers in plans without family deductibles is lower for workers in PPOs (12%) and POS plans (15%). As defined, all covered workers in HDHP/SOs have a general annual deductible for family coverage [Figure 7.20].
- Among covered workers enrolled in family coverage, the percent of covered workers in a plan with an aggregate general annual deductible is 41% for workers in HMOs, 58% for workers in PPOs, 64% for workers in POS plans, and 79% for workers in HDHP/SOs [Figure 7.20].
- The average deductible amounts for covered workers in plans with an aggregate annual deductible for family coverage are $3,285 for HMOs, $3,118 for PPOs, $4,842 for POS plans, and $5,095 for HDHP/SOs [Figure 7.21]. The average deductible amounts for aggregate family deductibles are similar to last year for each plan type.
- For covered workers in plans with an aggregate deductible for family coverage, the average annual family deductibles at firms with 10 to 199 workers are higher than at larger firms for covered workers in all four plan types [Figure 7.21].
- Among workers enrolled in family coverage, the percent of workers in plans with a separate per-person annual deductible for family coverage is 12% for workers in HMOs, 30% for workers in PPOs, 21% for workers in POS plans, and 21% for workers in HDHP/SOs [Figure 7.20].
- The average deductible amounts for covered workers in plans with separate per-person annual deductibles for family coverage are $1,361 for PPOs, and $3,762 for HDHP/SOs [Figure 7.21].
- Thirty-five percent of covered workers in plans with a separate per-person annual deductible for family coverage have a limit for the number of family members required to meet the separate deductible amounts [Figure 7.24]. Among those covered workers, the most frequent number of family members who are required to meet the separate per-person deductible is two [Figure 7.25].
Figure 7.20: Distribution of Type of General Annual Deductible for Covered Workers With Family Coverage, by Plan Type, 2025
Figure 7.21: Among Covered Workers With a General Annual Deductible, Average Deductibles for Family Coverage, by Deductible Type, Plan Type, and Firm Size, 2025
Figure 7.22: Among Covered Workers With a Separate Per-Person General Annual Deductible for Family Coverage, Distribution of Deductibles, by Plan Type, 2025
Figure 7.23: Among Covered Workers With an Aggregate General Annual Deductible for Family Coverage, Distribution of Deductibles, by Plan Type, 2025
Figure 7.24: Among Covered Workers With a Separate Per-Person General Annual Deductible for Family Coverage, Structure of Deductible Limits, by Plan Type, 2025
Figure 7.25: Among Covered Workers With a Separate Per-Person General Annual Deductible for Family Coverage and a Per-Person Limit, Distribution of Maximum Number of Family Members Required to Meet the Deductible, by Plan Type, 2025
Figure 7.26: Among Covered Workers With an Aggregate General Annual Deductible for Family Coverage, Distribution of Aggregate Deductibles, by Plan Type, 2020 and 2025
COVERAGE OF SERVICES AND PRODUCTS BEFORE MEETING THE GENERAL ANNUAL DEDUCTIBLES
The majority of covered workers with a general annual deductible are enrolled in plans where the deductible does not have to be met before certain services, such as physician office visits or prescription drugs, are covered. Covered workers in HSA qualified HDHP/SOs are not included in these estimates, because HSA-qualified plans generally only pay for preventive services before the deductible is met.
- Among covered workers enrolled in a plan with a general annual deductible, large shares (69% in HMOs, 78% in PPOs, 57% in POS plans, and 66% in HDHP/HRAs) are enrolled in plans where the deductible does not have to be met before physician office visits for primary care are covered [Figure 7.27].
- Similarly, among covered workers enrolled in a plan with a general annual deductible, large shares (86% in HMOs, 91% in PPOs, 75% in POS plans, and 77% in HPHD/HRAs) do not have to meet the general annual deductible before prescription drugs are covered [Figure 7.27].
Figure 7.27: Among Covered Workers With a General Annual Deductible, Percentage With Coverage for the Following Services Without Having to First Meet the Deductible, by Plan Type, 2025
HOSPITAL ADMISSIONS AND OUTPATIENT SURGERY
Whether or not a worker has a general annual deductible, most workers face additional types of cost-sharing (such as a copayment, coinsurance, or a per diem charge) when admitted to a hospital or having outpatient surgery. The distribution of workers with cost-sharing for hospital admissions or outpatient surgery does not equal 100%, as workers may face a complex combination of types of cost-sharing. For this reason, the average copayment and coinsurance rates include workers who may have a combination of these cost-sharing methods. Coinsurance, in particular, may include minimums or maximums which affect an enrollee’s liability. We report the distribution of cost-sharing for covered workers enrolled in a plan which covers hospital admissions and outpatient surgery, respectively. A small share of firms indicate that they have some “other” type of cost-sharing arrangement.
- In addition to any general annual deductible that may apply, 65% of covered workers have coinsurance and 11% have a copayment that apply to an inpatient hospital admission. A lower percentage of covered workers have per-day (per diem) payments (5%), a separate hospital deductible (1%), or both a copayment and coinsurance (8%). Fourteen percent of covered workers have no additional cost-sharing for hospital admissions after any general annual deductible has been met [Figure 7.28]. Covered workers with both a copay and coinsurance may be required to pay both or to pay the greater or lesser amount.
- On average, covered workers in HMO and POS plans are more likely than workers in other plan types to have a copayment for hospital admissions, while workers in HDHP/SOs are less likely to have a copayment [Figure 7.28].
- On average, covered workers in PPO plans and HDHP/SOs are more likely than workers in other plan types to have a coinsurance requirement for hospital admissions [Figure 7.28].
- The average coinsurance rate for a hospital admission is 20%, the average copayment is $313 per hospital admission, and the average per diem charge is $311 [Figure 7.31]. Seventy-five percent of workers enrolled in a plan with a per diem for hospital admissions have a limit on the number of days for which a worker must pay the cost-sharing amount [Figure 7.32].
- The cost-sharing provisions for outpatient surgery are similar to those for hospital admissions, as most workers have coinsurance or copayments. In 2025, 13% of covered workers have a copayment and 67% have a coinsurance rate for outpatient surgery. In addition, 6% have both a copayment and a coinsurance rate, while 14% have no additional cost-sharing after any general annual deductible has been met [Figure 7.29] and [Figure 7.30].
- For covered workers with cost-sharing for outpatient surgery, the average coinsurance rate is 20% and the average copayment is $186 [Figure 7.31].
Figure 7.28: Distribution of Covered Workers’ Cost Sharing for Hospital Admissions, by Plan Type, 2025
Figure 7.29: Distribution of Covered Workers’ Cost Sharing for Outpatient Surgery, by Plan Type, 2025
Figure 7.30: Percentage of Covered Workers With the Following Types of Cost Sharing for Hospital Admissions and Outpatient Surgery, in Addition to Any General Annual Deductible, 2025
Figure 7.31: Among Covered Workers With Separate Cost Sharing for Hospital Admissions or Outpatient Surgery, Average Cost Sharing, by Type, 2025
Figure 7.32: Among Covered Workers With a Charge Per Day for Hospital Admissions, Average Cost Sharing Features, 2025
Figure 7.33: Among Covered Workers With a Copayment for Hospital Admissions or Outpatient Surgery, Distribution of Copayments, 2025
Figure 7.34: Among Covered Workers With Coinsurance for Hospital Admissions or Outpatient Surgery, Distribution of Coinsurance Rates, 2025
COST-SHARING FOR PHYSICIAN OFFICE VISITS
The majority of covered workers are enrolled in health plans that require cost-sharing for an in-network physician office visit, in addition to any general annual deductible.13
- The most common form of cost-sharing for an in-network physician office visit is a copayment. Sixty-six percent of covered workers have a copayment for a primary care physician office visit and 22% have coinsurance. For office visits with a specialty physician, 65% of covered workers have a copayment and 24% have coinsurance [Figure 7.35].
- The form of cost-sharing for physician office visits varies by firm size.
- Covered workers at firms with 10 to 199 workers are more likely to have a copayment than workers at larger firms for in-network primary care office visits (72% vs. 64%) [Figure 7.37].
- Covered workers at firms with 10 to 199 workers are less likely to have coinsurance than workers at larger firms for in-network primary care office visits (7% vs. 27%), and for in-network office visits with specialists (8% vs. 29%) [Figure 7.37].
- Covered workers in HMOs, PPOs, and POS plans are much more likely to have copayments for both primary care and specialty care physician office visits than workers in HDHP/SOs. For primary care physician office visits, 18% of covered workers in HDHP/SOs have a copayment, 61% have coinsurance, and 13% have no cost-sharing after the general annual plan deductible is met [Figure 7.35].
- Among covered workers with a copayment for in-network physician office visits, the average copayment for primary care physician office visits is $27, which is similar to the average copayment ($26) last year [Figure 7.36].
- Among covered workers with a copayment for in-network physician office visits, the average copayment for specialty physician office visits is $45, an increase from the amount ($42) last year [Figure 7.36].
- For covered workers with a copayment for physician office visits, average copayment amounts are higher for workers at firms with 10 to 199 workers than for those at larger firms for both primary care physician office visits ($29 vs. $26) and specialty physician office visits ($51 vs. $43).
- Among covered workers with coinsurance for in-network physician office visits, the average coinsurance rates are 19% for a visit with a primary care physician and 19% for a visit with a specialist, similar to the rates last year [Figure 7.36].
Figure 7.35: Percentage of Covered Workers With the Following Types of Cost Sharing for Physician Office Visits, by Plan Type, 2025
Figure 7.36: Among Covered Workers With Copayments And/Or Coinsurance for Physician Office Visits, Average Copayments and Coinsurance, by Plan Type, 2025
Figure 7.37: Percentage of Covered Workers With the Following Types of Cost Sharing for Physician Office Visits, by Firm Size, 2025
Figure 7.38: Among Covered Workers With a Copayment for a Primary Care Physician Office Visit, Distribution of Copayments, by Plan Type, 2025
Figure 7.39: Among Covered Workers With a Copayment for a Specialist Physician Office Visit, Distribution of Copayments, by Plan Type, 2025
Figure 7.40: Among Covered Workers With a Copayment for a Primary Care Physician Office Visit, Distribution of Copayments, 2006-2025
Figure 7.41: Among Covered Workers With a Copayment for a Specialist Physician Office Visit, Distribution of Copayments, 2007-2025
Figure 7.42: Among Covered Workers With a Copayment And/Or Coinsurance for Physician Office Visits, Average Copayment and Coinsurance, 2006-2025
OUT-OF-POCKET MAXIMUMS
Virtually all covered workers are in a plan that either partially or totally limits the cost-sharing that enrollees must pay in a year. This limit is generally referred to as an out-of-pocket maximum. The Affordable Care Act (ACA) requires that non-grandfathered health plans have an annual out-of-pocket maximum of no more than $9,200 for single coverage and $18,400 for family coverage in 2025. Out-of-pocket limits in HSA qualified HDHP/SOs are required to be somewhat lower.14 Many plans have complex out-of-pocket structures, which makes it difficult to accurately collect information on this element of plan design.
- In 2025, more than 99% of covered workers are in a plan that has an out-of-pocket maximum for single coverage [Figure 7.43].
- For covered workers in plans with an out-of-pocket maximum for single coverage, there is wide variation in spending limits:12% of covered workers in plans with an out-of-pocket maximum have an out-of-pocket maximum of $2,000 or less for single coverage, while 21% of these workers have an out-of-pocket maximum above $6,000 [Figure 7.44].
Figure 7.43: Percentage of Covered Workers in a Plan With an Out-Of-Pocket Maximum Above Certain Thresholds for Single Coverage, 2009-2025
Figure 7.44: Among Covered Workers With an Out-Of-Pocket Maximum for Single Coverage, Distribution of Out-Of-Pocket Maximums, by Plan Type, 2025
Figure 7.45: Average Out-Of-Pocket Maximum for Single Coverage, by Firm Size, 2025
- Some workers with separate per-person deductibles or out-of-pocket maximums for family coverage do not have a specific number of family members that are required to meet the deductible amount and instead have another type of limit, such as a per-person amount with a total dollar amount limit. These responses are included in the averages and distributions for separate family deductibles and out-of-pocket maximums.↩︎
- Starting in 2010, the survey asked about the prevalence and cost of physician office visits separately for primary care and specialty care. Prior to the 2010 survey, if the respondent indicated the plan had a copayment for office visits, we assumed the plan had a copayment for both primary and specialty care visits. The survey did not allow for a respondent to report that a plan had a copayment for primary care visits and coinsurance for visits with a specialist physician. The changes made in 2010 allow for variations in the type of cost-sharing for primary care and specialty care visits. The survey includes cost-sharing for in-network services only.↩︎
- For those enrolled in an HDHP/HSA, the out-of-pocket maximum may be no more than $8,300 for an individual plan and $16,600 for a family plan in 2025.↩︎
High-Deductible Health Plans with Savings Option
To help cover out-of-pocket expenses not covered by a health plan, some firms offer high-deductible plans paired with an account that allows enrollees to use tax-preferred funds to pay cost sharing and other out-of-pocket medical expenses. The two most common types of accounts are health reimbursement arrangements (HRAs) and health savings accounts (HSAs). HRAs and HSAs are both financial accounts that workers or their family members can use to pay for health care services. These savings arrangements are often (or, in the case of HSAs, always) paired with health plans with high deductibles. This survey treats high-deductible plans paired with a savings option as a distinct plan type – High-Deductible Health Plan with Savings Option (HDHP/SO) – even if the plan would otherwise be considered a PPO, HMO, POS plan, or conventional health plan. Specifically for the survey, HDHP/SOs are defined as (1) health plans with a deductible of at least $1,000 for single coverage and $2,000 for family coverage15, offered with an HRA (referred to as HDHP/HRAs), or (2) high-deductible health plans that meet the federal legal requirements to permit an enrollee to establish and contribute to an HSA (referred to as HSA-qualified HDHPs).16
PERCENTAGE OF FIRMS OFFERING HDHP/HRAS AND HSA-QUALIFIED HDHPS
Thirty-six percent of firms with 10 or more workers offering health benefits offer an HDHP/HRA, an HSA-qualified HDHP, or both. Among firms offering health benefits, 8% offer an HDHP/HRA and 31% offer an HSA-qualified HDHP [Figure 8.1]. The percentage of firms offering an HDHP/SO is similar to last year.
- Firms with 200 or more workers more likely than smaller firms to offer an HDHP/SO to at least some workers (62% vs. 35%) [Figure 8.3].
Figure 8.1: Among Firms Offering Health Benefits, Percentage That Offer an HDHP/HRA And/Or an HSA-Qualified HDHP, 2005-2025
Figure 8.2: Among Firms Offering Health Benefits, Percentage That Offer an HDHP/SO, by Firm Size, 2005-2025
Figure 8.3: Among Firms Offering Health Benefits, Percentage That Offer an HDHP/HRA And/Or an HSA-Qualified HDHP, by Firm Size, 2025
ENROLLMENT IN HDHP/HRAS AND HSA-QUALIFIED HDHPS
Thirty-three percent of covered workers are enrolled in an HDHP/SO in 2025, similar to the percentage last year (28%) [Figure 8.4].
- The percentage of covered workers enrolled in HDHP/SOs is similar to the percentage five years ago (33% v. 31%) but is higher than the percentage ten years ago (33% v. 25%) [Figure 8.4].
- Four percent of covered workers are enrolled in HDHP/HRAs and 29% of covered workers are enrolled in HSA-qualified HDHPs in 2025.
- The percentage of enrollees in HDHP/HRAs is similar to the percentage last year [Figure 8.4].
- The percentage of enrollees in HSA-qualified HDHPs in 2025 (29%) is higher than the percentage (22%) last year but is similar to the percentage (24%) five years ago [Figure 8.4].
- The percentage of covered workers enrolled in HDHP/SOs is higher in firms with 200 or more workers than the percentage enrolled in smaller firms (35% vs.26%) [Figure 8.5].
- The percentage of covered workers enrolled in HSA-qualified HDHPs is higher in firms with 200 or more workers than the percentage enrolled in smaller firms (32% vs.19%).
Figure 8.4: Percentage of Covered Workers Enrolled in an HDHP/HRA or HSA-Qualified HDHP, 2006-2025
Figure 8.5: Percentage of Covered Workers Enrolled in an HDHP/SO, by Firm Size, 2006-2025
PREMIUMS AND WORKER CONTRIBUTIONS
In 2025, average annual premiums for covered workers in HDHP/HRAs are $8,940 for single coverage and $25,961 for family coverage [Figure 8.6]. The average single annual premium amount is lower than the average single premium for covered workers in plans that are not HDHP/SOs [Figure 8.7].
The average annual premiums for workers in HSA-qualified HDHPs are $8,575 for single coverage and $25,303 for family coverage [Figure 8.6]. These amounts are lower than the average single and family premiums for covered workers in plans that are not HDHP/SOs [Figure 8.7].
The average annual worker premium contribution amounts for covered workers enrolled in HDHP/HRAs are $1,676 for single coverage and $7,212 for family coverage [Figure 8.6]. These amounts are similar to the average premium contribution amounts for covered workers in plans that are not HDHP/SOs [Figure 8.7].
The average annual worker premium contribution amounts for covered workers in HSA-qualified HDHPs are $1,319 for single coverage and $5,634 for family coverage [Figure 8.6]. The average family premium contribution amount is lower than the average premium family contribution amount for covered workers in plans that are not HDHP/SOs [Figure 8.7].
Figure 8.6: HDHP/HRA and HSA-Qualified HDHP Features for Covered Workers, 2025
Figure 8.7: Average Annual Premiums and Contributions to Savings Accounts for Covered Workers in HDHP/HRAs or HSA-Qualified HDHPs, Compared to Non-HDHP/SOs, 2025
Figure 8.8: Average Annual Premiums and Contributions for Covered Workers in HDHP/SOs and Non-HDHP/SOs, for Family Coverage, 2025
Figure 8.9: Total Annual Costs (Premiums and Account Contributions) for Covered Workers in HDHP/SOs, for Family Coverage, by Firm Size, 2025
Figure 8.10: Average Annual Premiums for Covered Workers With Family Coverage, by Plan Type, 2007-2025
Figure 8.11: Average Annual Premiums for Covered Workers With Single Coverage, by Plan Type, 2007-2025
OUT-OF-POCKET MAXIMUMS AND PLAN DEDUCTIBLES
HSA-qualified HDHPs are legally required to have an annual out-of-pocket maximum of no more than $8,300 for single coverage and $16,600 for family coverage in 2025. Non-grandfathered HDHP/HRA plans are required to have out-of-pocket maximums of no more than $9,200 for single coverage and $18,400 for family coverage.
- The average annual out-of-pocket maximum amounts for single coverage are $4,926 for HDHP/HRAs and $4,509 for HSA-qualified HDHPs [Figure 8.6].
As expected, workers enrolled in HDHP/SOs have higher deductibles than workers enrolled in HMOs, PPOs, or POS plans [Figure 8.14].
- The average general annual deductible for single coverage is $3,004 for HDHP/HRAs and $2,578 for HSA-qualified HDHPs [Figure 8.6]. There is wide variation around these averages: 37% of covered workers enrolled in an HDHP/SO are in a plan with a deductible between $1,000 and $1,999 for single coverage while 35% have a deductible of $3,000 or more [Figure 8.12].
- The survey asks firms whether the family deductible amount is (1) an aggregate amount (i.e., the out-of-pocket expenses of all family members are counted until the deductible is satisfied), or (2) a per-person amount that applies to each family member (typically with a limit on the number of family members that would be required to meet the deductible amount) (see Section 7 for more information).
- The average aggregate deductibles for workers with family coverage are $6,912 for HDHP/HRAs and $4,932 for HSA-qualified HDHPs [Figure 8.6]. As with single coverage, there is wide variation around these averages for family coverage: 28% of covered workers enrolled in HDHP/SOs with an aggregate family deductible have a deductible between $2,000 and $3,500 while 16% have a deductible of $7,000 dollars or more [Figure 8.15].
Figure 8.12: Distribution of Covered Workers in HDHP/SOs With the Following General Annual Deductibles for Single Coverage, by Firm Size, 2025
Figure 8.13: General Annual Deductible for Workers in HDHP/SOs After Any Employer Account Contributions for Single Coverage, by Firm Size, 2025
Figure 8.14: Among Covered Workers With a General Annual Deductible, Average Deductibles for Workers in Non-HDHP/SOs Compared to HDHP/SOs Before and After Any Employer Account Contributions, for Single Coverage, 2007-2025
Figure 8.15: Distribution of Covered Workers in HDHP/SOs With the Following Aggregate Family Deductibles, 2025
EMPLOYER CONTRIBUTIONS
Employers contribute to HDHP/SOs in two ways: through their contributions toward the premium for the health plan, and through their contributions (if any, in the case of HSAs) to the savings account option (the HRAs or HSAs themselves).
- The average annual employer contributions to premiums for covered workers in HDHP/HRAs are $7,264 for single coverage and $18,748 for family coverage [Figure 8.7]. The average employer contribution amount for single coverage is lower than the average employer contribution amount for workers in plans that are not HDHP/SOs [Figure 8.7].
- The average annual employer contributions to premiums for covered workers in HSA-qualified HDHPs are $7,256 for single coverage and $19,669 for family coverage. These amounts are higher than the average employer contribution amounts to premiums for single and family coverage for covered workers in HSA-qualified HDHPs last year [Figure 8.7].
- The average employer contributions to premiums for covered workers in HSA-qualified HDHPs for single coverage are lower than the average employer contribution amounts for workers in plans that are not HDHP/SOs [Figure 8.7].
Covered workers enrolled in HDHP/HRAs on average receive an annual employer contribution to their HRA of $1,966 for single coverage and $3,810 for family coverage [Figure 8.7].
- HRAs are generally structured in such a way that employers may not actually spend the whole amount that they make available to their employees’ HRAs.17 Amounts committed to an employee’s HRA that are not used by the employee generally roll over and can be used in future years, but any balance may revert back to the employer if the employee leaves his or her job. Thus, the employer contribution amounts to HRAs that we capture in the survey may exceed the amount that employers will actually spend.
Covered workers enrolled in HSA-qualified HDHPs receive an average annual employer HSA contribution of $690 for single coverage and $1,296 for family coverage [Figure 8.7].
- In many cases, employers that sponsor HSA-qualified HDHP/SOs do not make a contributions to HSAs established by their employees. Thirty-three percent of employers offering single coverage and 34% offering family coverage through HSA-qualified HDHPs do not make contributions toward the HSAs that their workers might establish. Among covered workers enrolled in an HSA-qualified HDHP, 14% enrolled in single coverage and 15% enrolled in family coverage do not receive an account contribution from their employer [Figure 8.16] [Figure 8.17].
- The average HSA contributions reported above include the portion of covered workers whose employer contribution to the HSA is zero. When those firms that do not contribute to the HSA are excluded from the calculation, the average employer contribution for covered workers is $806 for single coverage and $1,523 for family coverage.
- The percentages of covered workers enrolled in a plan where the employer makes no HSA contribution, (14% for single coverage and 15% for family coverage), are similar to the percentages in recent years.
- The amounts that employers contribute to savings accounts varies considerably.
- 17% of covered workers in an HDHP/HRA receive an annual HRA contribution of less than $1,000 for single coverage, while 21% receive an annual HRA contribution of $3,000 or more.
- Twenty-five percent of covered workers in an HSA-qualified HDHP receive an annual HSA contribution of less than $400 for single coverage, including 14% who receive no HSA contribution from their employer [Figure 8.16]. In contrast, 13% of covered workers in an HSA-qualified HDHP receive an annual HSA contribution of $1,200 or more. One percent of covered workers have an employer that matches worker HSA contributions for single coverage.
Employer contributions to savings account options (i.e., the HRAs and HSAs themselves) for their workers can be added to their health plan premium contributions to calculate total employer contributions toward HDHP/SOs. We note that HRAs are a promise by an employer to pay up to a specified amount and that many employees will not use the full amount available to their HRA in a year, so adding the employer premium contribution amount and the HRA contribution represents an upper bound for employer liability. Since employer contributions to employee HSAs immediately transfer the full amount to the employee, adding employer premium and HSA contributions is an instructive way to look at their total liability under these plans.
- For HDHP/HRAs, the average annual total employer contribution for covered workers is $9,230 for single coverage and $22,559 for family coverage. The average total employer contribution for single coverage for covered workers in HDHP/HRAs is higher than the average employer contribution for single coverage in plans that are not HDHP/SOs [Figure 8.7].
- For HSA-qualified HDHPs, the average total annual employer contribution for covered workers is $7,940 for single coverage and $21,005 for workers with family coverage. These amounts are similar to the average employer contributions for single and family coverage in health plans that are not HDHP/SOs [Figure 8.7].
Figure 8.16: Distribution of Covered Workers With the Following Annual Employer Contributions to Their HSA-Qualified HDHP, for Single Coverage, 2025
Figure 8.17: Distribution of Covered Workers With the Following Annual Employer Contributions to Their HSA-Qualified HDHP, for Family Coverage, 2025
Figure 8.18: Average Annual Employer Contributions to HSA Accounts for Covered Workers Enrolled in an HSA-Qualified HDHP, 2009-2025
Figure 8.19: Among Covered Workers in HDHP/HRAs and HSA-Qualified HDHPs, Average Annual Employer HSA and HRA Contributions, 2025
COST SHARING FOR OFFICE VISITS
The cost-sharing pattern for physician office visits in HSA-qualified plans is quite different than the pattern in other plan types.
- For primary care office visits, 68% of covered workers in HSA qualified HDHPs have a coinsurance requirement, compared to 6% of covered workers enrolled in PPOs, 5% of covered workers enrolled in HMOs, 2% of covered workers enrolled in POS plans, and 16% of covered workers enrolled in HDHP/HRAs [Figure 8.20]. Workers in other plan types are much more likely to face copayments than coinsurance for physician office visits (see Section 7 for more information).
- The pattern is similar for office visits for specialty services, where 69% of covered workers in HSA qualified plans have a coinsurance requirement, compared to 9% of covered workers enrolled in PPOs, 5% of covered workers enrolled in HMOs, 5% of covered workers enrolled in POS plans, and 16% of covered workers enrolled in HDHP/HRAs [Figure 8.20]
Figure 8.20: Distribution of Covered Workers in HSA-Qualified HDHPs and Other Plan Types With the Following Types of Cost Sharing in Addition to the General Annual Deductible, 2025
Health Reimbursement Arrangements (HRAs) are medical care reimbursement plans established by employers that can be used by employees to pay for health care. HRAs are funded solely by employers. Employers may commit to make a specified amount of money available in the HRA for premiums and medical expenses incurred by employees or their dependents. HRAs are accounting devices, and employers are not required to expend funds until an employee incurs expenses that would be covered by the HRA. Unspent funds in the HRA usually can be carried over to the next year (sometimes with a limit). Employees cannot take their HRA balances with them if they leave their job, although an employer can choose to make the remaining balance available to former employees to pay for health care. HRAs often are offered along with a high-deductible health plan (HDHP). In such cases, the employee pays for health care first from his or her HRA and then out-of-pocket until the health plan deductible is met. Sometimes certain preventive services or other services such as prescription drugs are paid for by the plan before the employee meets the deductible.
Health Savings Accounts (HSAs) are savings accounts created by individuals to pay for health care. An individual may establish an HSA if he or she is covered by a “qualified health plan” – a plan with a high deductible (at least $1,600 for single coverage and $3,200 for family coverage in 2025 or $1,500 and $3,000, respectively, in 2024) that also meets other requirements. Employers can encourage their employees to create HSAs by offering an HDHP that meets the federal requirements. Employers in some cases also may assist their employees by identifying HSA options, facilitating applications, or negotiating favorable fees from HSA vendors.Both employers and employees can contribute to an HSA, up to the statutory cap of $4,300 for single coverage and $8,550 for family coverage in 2025. Employee contributions to the HSA are made on a pre-income tax basis, and some employers arrange for their employees to fund their HSAs through payroll deductions. Employers are not required to contribute to HSAs established by their employees but if they elect to do so, their contributions are not taxable to the employee. Interest and other earnings on amounts in an HSA are not taxable. Withdrawals from the HSA by the account owner to pay for qualified health care expenses are not taxed. The savings account is owned by the individual who creates the account, so employees retain their HSA balances if they leave their job.
- There is no legal requirement for the minimum deductible in a plan offered with an HRA. The survey defines a high-deductible HRA plan as a plan with a deductible of at least $1,000 for single coverage and $2,000 for family coverage. Federal law requires a deductible of at least $1,600 for single coverage and $3,200 for family coverage for HSA-qualified HDHPs in 2025 (or $1,500 and $3,000, respectively, for plans in their 2024 plan year). Not all firms’ plan years correspond with the calendar year, so some firms may report a plan with limits from the prior year. See definitions at the end of this Section for more information on HDHP/HRAs and HSA-qualified HDHPs.↩︎
- The definitions of HDHP/SOs do not include other consumer-driven plan options, such as arrangements that combine an HRA with a lower-deductible health plan or arrangements in which an insurer (rather than the employer as in the case of HRAs or the enrollee as in the case of HSAs) establishes an account for each enrollee. Other arrangements may be included in future surveys as the market evolves.↩︎
- The survey asks “Up to what dollar amount does your firm promise to contribute each year to an employee’s HRA or health reimbursement arrangement for single coverage?” We refer to the amount that the employer commits to make available to an HRA as a contribution for ease of discussion. As discussed, HRAs are notional accounts, and employers are not required to actually transfer funds until an employee incurs expenses. Thus, employers may not expend the entire amount that they commit to make available to their employees through an HRA. Some employers may make their HRA contribution contingent on other factors, such as completing wellness programs.↩︎
Prescription Drug Benefits
Nearly all (99%) covered workers are at a firm that provides prescription drug coverage to enrollees in its largest health plan. Over time, employer plans have incorporated more complex benefit designs for prescription drugs as employers and insurers expand the use of formularies with multiple cost-sharing tiers, as well as other management approaches. To reduce the burden on respondents, we ask offering firms about the attributes of prescription drug coverage only for their largest health plan. This survey asks employers about the cost-sharing in up to four tiers, plus, if applicable, a tier exclusively for specialty drugs. Some plans may have more than one tier for specialty drugs or other variations that are not captured in the survey. There also may be other areas of variation in how plans structure their formularies that also are not captured.
DISTRIBUTION OF COST SHARING
The large majority of covered workers (92%) are in a plan with tiered cost sharing for prescription drugs [Figure 9.1]. Cost-sharing tiers generally refer to a health plan placing a drug on a formulary or preferred drug list that classifies drugs into categories that are subject to different cost sharing or management. Often, there are different tiers for generic, preferred and non-preferred drugs. Plans also create additional tiers that may be used for specialty drugs or more expensive drugs such as biologics. Some plans may have multiple tiers for different categories.
- Eighty-four percent of covered workers are in a plan with three, four, or even more tiers of cost sharing for prescription drugs [Figure 9.1]. These totals include tiers that cover only specialty drugs, although the cost-sharing information for the specialty tier is reported separately below.
- Compared to covered workers in other plan types, those in HDHP/SOs are less likely to be in a plan with four or more tiers of cost sharing (49% vs. 65%) [Figure 9.2].
- Compared to covered workers in other plan types, those in HDHP/SOs are more likely to be in a plan that has no cost sharing for prescriptions once the plan deductible is met (9% vs. 2%) [Figure 9.2].
- Covered workers in firms with 10 to 199 workers are more likely than those in larger firms to have no cost sharing after the deductible is met (8% vs. 2%) [Figure 9.2].
Figure 9.1: Distribution of Covered Workers Facing Different Cost-Sharing Formulas for Prescription Drug Benefits, 2017-2025
Figure 9.2: Distribution of Covered Workers Facing Different Cost-Sharing Formulas for Prescription Drug Benefits, by Plan Type and Plan Size, 2025
TIERS NOT EXCLUSIVELY FOR SPECIALTY DRUGS
Even when formulary tiers covering only specialty drugs are not counted, a large share (82%) of covered workers are in a plan with three or more tiers of cost sharing for prescription drugs. The cost-sharing statistics presented in this section do not include information about tiers that cover only specialty drugs. In cases in which a plan covers specialty drugs on a tier with other drugs, they will be included in these averages. Cost-sharing statistics for tiers covering only specialty drugs are presented separately below.
- For covered workers in a plan with three or more tiers of cost sharing for prescription drugs, copayments are the most common form of cost sharing in the first three tiers and coinsurance is the second-most common [Figure 9.3].
- Among covered workers in plans with three or more tiers of cost sharing for prescription drugs, the average copayment is $12 for first-tier drugs, $40 second-tier drugs, $71 for third-tier drugs, and $123 for fourth-tier drugs [Figure 9.6].
- Among covered workers in plans with three or more tiers of cost sharing for prescription drugs, the average coinsurance rate is 19% for first-tier drugs, 25% for second-tier drugs, 35% for third-tier drugs, and 31% for fourth-tier drugs [Figure 9.6].
- Five percent of covered workers are in a plan with two tiers for prescription drug cost sharing (excluding tiers covering only specialty drugs).
- For these workers, copayments are more common than coinsurance in both tiers [Figure 9.3]. The average copayment is $12 for the first tier and $37 for the second tier. The average coinsurance rate is 18% for the first tier and 25% for the second tier [Figure 9.6].
- Eight percent of covered workers are in a plan with the same cost sharing for prescriptions regardless of the type of drug (excluding tiers covering only specialty drugs) [Figure 9.2].
- Among these workers, 18% have copayments and 82% have a coinsurance rate [Figure 9.3].
Figure 9.3: Among Covered Workers With Prescription Drug Coverage, Distribution With the Following Types of Cost Sharing for Prescription Drugs, 2025
Figure 9.4: Among Covered Workers With Three or More Tiers of Prescription Drug Cost Sharing, Distribution With the Following Types of Cost Sharing, by Firm Size, 2025
Figure 9.5: Among Covered Workers With Three or More Tiers of Prescription Drug Cost Sharing, Distribution With the Following Types of Cost Sharing, by Plan Type, 2025
Figure 9.6: Among Covered Workers With Prescription Drug Coverage, Average Copayments and Coinsurance, 2025
COINSURANCE MAXIMUMS
Coinsurance rates for prescription drugs often include maximum and/or minimum dollar amounts. Depending on the plan design, coinsurance maximums can significantly limit the amount an enrollee must spend out-of-pocket for higher-cost drugs. Even in plans without explicit coinsurance maximum amounts, the overall plan out-of-pocket maximum limits enrollee cost sharing on covered services, including prescription drugs.
Coinsurance minimum and maximum amounts vary across tiers and plan designs.
- For example, among covered workers in a plan with coinsurance for the third cost-sharing tier, 42% have only a maximum dollar amount attached to the coinsurance rate, 6% have only a minimum dollar amount, 22% have both a minimum and maximum dollar amount, and 28% have neither.
- For those in a plan with coinsurance for the fourth cost-sharing tier, 69% have only a maximum dollar amount attached to the coinsurance rate, 5% have only a minimum dollar amount, 6% have both a minimum and maximum dollar amount, and 19% have neither [Figure 9.7].
Figure 9.7: Distribution of Coinsurance Structures for Covered Workers Facing a Coinsurance for Prescription Drugs, 2025
SEPARATE TIERS FOR SPECIALTY DRUGS
Specialty drugs, such as biologics that may be used to treat chronic conditions or some cancer drugs, can be quite expensive and often require special handling and administration. In 2016, we revised our survey questions to obtain more information about formulary tiers that are exclusively for specialty drugs.
- In 2025, 87% of covered workers at firms with 10 or more workers to be in a plan with coverage for specialty drugs, the same percentage as last year.
- Covered workers in firms with 200 or more workers are more likely than workers in smaller firms to be in a plan with coverage for specialty drugs (92% vs. 71%).
- Covered workers in firms with 10 to 199 workers are more likely than workers in larger firms to be in a firm that did not know if its plan with the largest enrollment covers specialty drugs (18% vs. 4%).
- Among covered workers in firms with 200 or more workers in a plan with coverage for specialty drugs, 63% are in a plan with at least one cost-sharing tier just for specialty drugs [Figure 9.8].
- Among covered workers at firms with 200 or more workers in a plan with at least one separate tier for specialty drugs, 40% have a copayment for specialty drugs and 58% have coinsurance [Figure 9.10]. The average copayment is $111 and the average coinsurance rate is 27% [Figure 9.11]. Sixty-two percent of those with coinsurance have a maximum dollar limit on the amount of coinsurance they must pay.
Figure 9.8: Among Large Firms With Prescription Drug Coverage, Percentage of Workers With Coverage for Specialty Drugs, 2025
Figure 9.9: Among Large Firms Whose Prescription Drug Coverage Includes Specialty Drugs, Percentage of Covered Workers Enrolled in a Plan That Has a Separate Tier for Specialty Drugs, by Firm Size, 2025
Figure 9.10: Among Covered Workers at Large Firms Enrolled in a Plan With a Separate Tier for Specialty Drugs, Distribution of the Following Types of Cost Sharing, by Firm Size, 2025
Figure 9.11: Among Covered Workers at Large Firms Enrolled in a Plan With a Separate Tier for Specialty Drugs, Average Copayments and Coinsurance, by Firm Size, 2017 & 2025
PRESCRIPTION DRUG ADMINISTRATION
Forty-five percent of covered workers in firms with 50 or more workers are enrolled in a plan that reduces or waives cost sharing for prescription drugs needed to maintain health for one or more chronic illnesses, such as insulin products for diabetics [Figure 9.12]. Firms with 5,000 or more workers are more likely to have this policy (52%) [Figure 9.13].
Figure 9.12: Percentage of Covered Workers With Reduced or No Cost-Sharing for Maintenance Drugs, by Firm Size, 2025
Figure 9.13: Among Covered Workers With Prescription Drug Coverage at Large Firms, Percentage of Covered Workers With Reduced or No Cost-Sharing for Maintenance Drugs, Within Firm Size, 2019-2025
Generic drugs
- Drugs that are no longer covered by patent protection and thus may be produced and/or distributed by multiple drug companies.
Preferred drugs
- Drugs included on a formulary or preferred drug list; for example, a brand-name drug without a generic substitute.
Non-preferred drugs
- Drugs not included on a formulary or preferred drug list; for example, a brand-name drug with a generic substitute.
Fourth-tier drugs
- New types of cost-sharing arrangements that typically build additional layers of higher copayments or coinsurance for specifically identified types of drugs, such as lifestyle drugs or biologics.
Specialty drugs
- Specialty drugs such as biological drugs are high cost drugs that may be used to treat chronic conditions such as blood disorder, arthritis or cancer. Often times they require special handling and may be administered through injection or infusion.
Plan Funding
Many firms, particularly larger firms, choose to pay for some or all of the health services of their workers directly from their own funds rather than by purchasing health insurance to cover them. This is called self-funding. Both public and private employers can use self-funding to provide health benefits. Federal law (the Employee Retirement Income Security Act of 1974, or ERISA) exempts self-funded plans established by private employers (but not public employers) from most state insurance laws, including reserve requirements, mandated benefits, premium taxes, and some consumer protection regulations. In 2025, 67% of covered workers are in a self-funded health plan. Some employers which sponsor self-funded plans purchase stoploss coverage to limit their liabilities.
In recent years, a complex funding option, often called level-funding, has become more widely available to small employers. Level-funded arrangements are nominally self-funded options that package together a self-funded plan with extensive stoploss coverage that significantly reduces the risk retained by the employer. Thirty-seven percent of covered workers in firms with 10 to 199 workers are in a level-funded plan in 2025.
SELF-FUNDED PLANS
- Sixty-seven percent of covered workers are in a plan that is self-funded, similar to the percentage (65%) last year [Figure 10.2].
- The percentage of covered workers enrolled in self-funded plans is similar to the percentages five years ago (69%) and ten years ago (66%) [Figure 10.2].
- As expected, covered workers in firms with 200 or more workers are significantly more likely to be in a self-funded plan than covered workers in smaller firms (80% vs. 27%) [Figure 10.1] and [Figure 10.3].
Figure 10.1: Percentage of Covered Workers Enrolled in a Self-Funded Plan, by Firm Size, 2025
Figure 10.2: Percentage of Covered Workers Enrolled in a Self-Funded Plan, by Firm Size, 1999-2025
Figure 10.3: Percentage of Covered Workers Enrolled in a Self-Funded Plan, by Firm Size, Region, and Industry, 2025
Figure 10.4: Percentage of Covered Workers Enrolled in a Self-Funded Plan, by Plan Type and Firm Size, 2025
Figure 10.5: Percentage of Covered Workers Enrolled in a Self-Funded Plan by Firm Ownership Type, 2025
LEVEL-FUNDED PLANS
In recent years, insurers have been offering health plans that provide a nominally self-funded option for small and mid-sized employers that incorporates stoploss insurance with relatively low attachment points. In these arrangements, the insurer calculates an expected monthly expense for the employer, which includes a share of the estimated annual cost for benefits, premiums for the stoploss protection, and an administrative fee. The employer pays this “level premium” amount, with the potential for some reconciliation between the employer and the insurer at the end of the year, although small employers are often protected from any meaningful additional liability. These policies are sold as self-funded plans, so they generally are not subject to state requirements for insured plans and, for those sold to employers with fewer than 50 employees, are not subject to the rating and benefit standards in the ACA for small firms.
Due to the complexity of the funding (and regulatory status) of these plans, and because employers often pay a monthly amount that resembles a premium, respondents may be confused as to whether or not their health plan is self-funded or insured. There also may be confusion because different plan administrators (generally insurers) use different labels to refer to these arrangements. We asked employers with fewer than 200 workers whether they have a level-funded plan.
- Thirty-seven percent of firms that offer health benefits with 10 to 199 workers offer a level-funded plan in 2025, the same percentage as last year.
- Thirty-seven percent of covered workers in firms with 10 to 199 workers are enrolled in a level-funded plan in 2025, similar to the percentage last year [Figure 10.6] [Figure 10.8]. Fifty-one percent of covered workers in firms with 10 to 199 workers are enrolled in either a level-funded plan or a self-insured plan, similar to the percentage (47%) last year [Figure 10.7] and [Figure 10.8].
Figure 10.6: Among Covered Workers at Small Firms, Percentage Enrolled in a Level-Funded or Self-Funded Plan, by Firm Size, 2025
Figure 10.7: Among Covered Workers at Small Firms, Percentage Enrolled in a Level-Funded or Self-Insured Plan, by Firm Size, 2025
Figure 10.8: Among Covered Workers at Small Firms, Percentage Enrolled in a Level-Funded or Self-Funded Plan, 2018-2025
STOPLOSS COVERAGE
Employers purchase insurance, often referred to as “stoploss” coverage, to protect themselves from unexpected losses for claims incurred by a self-funded plan. There are different types of stoploss; for example a stoploss policy may cover any amount that the plan sponsor must pay over a specified amount for each worker or enrollee (referred to as specific stoploss coverage) or it may limit the total amount the plan sponsor must pay for all claims in the plan over the plan year (referred to as aggregate stoploss coverage). Stoploss coverage also may be focused on particular types of claims (e.g., transplants). A firm may have more than one type of stoploss coverage.
- At firms with 200 or more workers, 75% of covered workers in self-funded health plans are in plans that have stoploss insurance, similar to the percentage last year (75%) [Figure 10.9]. Covered workers in firms with 5,000 or more workers are less likely than covered workers in smaller firms to be in a plan with stopless insurance [Figure 10.10].
Figure 10.9: Among Covered Workers Enrolled in a Self-Funded Plan, Percentage Covered by Stoploss Insurance (At Firms With 50 or More Workers), by Firm Size, 2011-2025
Figure 10.10: Among Covered Workers Enrolled in a Self-Funded Plan, Percentage Covered by Stoploss Insurance (At Firms With 50 or More Workers), by Firm Size, 2025
- Self-Funded Plan
- An insurance arrangement in which the employer assumes direct financial responsibility for the costs of enrollees’ medical claims. Employers sponsoring self-funded plans typically contract with a third-party administrator or insurer to provide administrative services for the self-funded plan. In some cases, the employer may buy stoploss coverage from an insurer to protect the employer against very large claims.
- Fully-Insured Plan
- An insurance arrangement in which the employer contracts with a health plan that assumes financial responsibility for the costs of enrollees’ medical claims.
- Level-Funded Plan
- An insurance arrangement in which the employer makes a set payment each month to an insurer or third party administrator which funds a reserve account for claims, administrative costs, and premiums for stop-loss coverage. When claims are lower than expected, surplus claims payments may be refunded at the end of the contract.
- Stoploss Coverage
- Stoploss coverage limits the amount that a plan sponsor has to pay in claims. Stoploss coverage may limit the amount of claims that must be paid for each employee or may limit the total amount the plan sponsor must pay for all claims over the plan year.
- Attachment Point
- Attachment points refer to the amount at which the insurer begins to pay its obligations for stoploss coverage, either because plan, individual or claim spending exceed a designated value.
Retiree Health Benefits
Retiree health benefits are an important consideration for older workers making decisions about retirement, and can be a crucial source of coverage for people retiring before Medicare eligibility. For retirees with Medicare coverage, retiree health benefits can provide an important supplement to Medicare, helping them pay for cost sharing and benefits not otherwise covered by Medicare.
Twenty-seven percent of large firms offering health benefits offer retiree health benefits in 2025, similar to the percentage in 2024 (24%).
This survey asks retiree health benefits questions only of firms with 200 or more workers.
EMPLOYER RETIREE BENEFITS
In 2025, 27% of firms with 200 or more workers that offer health benefits offer retiree health benefits for at least some current workers or retirees [Figure 11.1]. Starting in 2019, we instructed firms to respond “yes” if they were providing coverage for retirees but weren’t offering current employees these benefits, or if they were planning to give current employees retiree health coverage in the future.
- Retiree health benefits offer rates vary with firm characteristics.
- Among firms with 200 or more workers that offer health benefits, firms with 5,000 or more workers are more likely to offer retiree health benefits than smaller firms (41% v. 26%) [Figure 11.2].
- The share of firms with 200 or more workers that offer retiree health benefits varies considerably by industry [Figure 11.2].
- Among firms with 200 or more workers that offer health benefits, public employers are more likely (63%) and private for-profit employers are less likely (13%) to offer retiree health benefits than other firm types [Figure 11.3].
- Firms with 200 or more workers that offer health benefits and that have at least some union workers are more likely to offer retiree health benefits than firms without any union workers (46% vs. 20%) [Figure 11.3].
- Among firms with 200 or more workers that offer health benefits, firms with 5,000 or more workers are more likely to offer retiree health benefits than smaller firms (41% v. 26%) [Figure 11.2].
Figure 11.1: Among Large Firms Offering Health Benefits to Active Workers, Percentage of Firms Offering Retiree Health Benefits, 1988-2025
Figure 11.2: Among Large Firms Offering Health Benefits to Active Workers, Percentage of Firms Offering Retiree Health Benefits, by Firm Size, Region, and Industry, 2025
Figure 11.3: Among Large Firms Offering Health Benefits to Active Workers, Percentage of Firms Offering Retiree Health Benefits, by Firm Characteristics, 2025
BENEFIT ELIGIBILITY
Among firms with 200 or more workers that offer retiree health benefits,
- Eighty-two percent offer benefits to early retirees under the age of 65 [Figure 11.4].
- Fifty-four percent offer them to Medicare-age retirees [Figure 11.4].
- Forty-seven percent offer benefits to both early and Medicare-age retirees.
Among firms with 200 or more workers that offer retiree benefits, three-in-four (74%) offer health benefits to the spouses of retirees [Figure 11.5].
Figure 11.4: Among Large Firms Offering Health Benefits to Active Workers and Retirees, Percentage of Firms Offering Health Benefits to Early and Medicare-Age Retirees, 2000-2025
Figure 11.5: Among Large Firms Offering Health Benefits to Active Workers and Retirees, Percentage of Firms Offering Health Benefits to Retirees’ Spouse, by Firm Size, 2025
MEDICARE ADVANTAGE
Forty-seven percent of firms with 200 or more workers that offer retiree health benefits to Medicare-age retirees offer coverage to at least some Medicare-age retirees through a contract with a Medicare Advantage plan, similar to the share last year (56%) [Figure 11.7]. This share has risen considerably since 2017 (26%).
- Among firms with 200 or more workers that offer retiree health benefits through a Medicare Advantage plan,
- Sixty-one percent offer retiree health benefits only through Medicare Advantage plans while 39% offer a choice of other types of plans for retiree for retiree health benefits [Figure 11.8]. Both of these shares are similar to last year.
- Fifty-eight percent said to the best of their knowledge that the shift to offering Medicare Advantage plans lowered their per retiree costs, 7% said the shift to Medicare Advantage plans did not lower their per retiree costs, while 35% did not know the answer [Figure 11.9].
- Among firms with 200 or more workers that offer retiree health benefits that do not offer benefits through a Medicare Advantage plan in 2025, 6% are “Very Likely” or “Somewhat Likely” to do so in the next two years [Figure 11.10].
Figure 11.6: Among Large Firms That Offer Retiree Health Benefits to Medicare-Age Retirees, Percentage of Firms That Contract With a Medicare Advantage Plan, 2025
Figure 11.7: Among Large Firms That Offer Retiree Health Benefits to Medicare-Age Retirees, Percentage of Firms That Contract With a Medicare Advantage Plan, 2017-2025
Figure 11.8: Among Large Firms Offering Retiree Benefits Through a Contract With a Medicare Advantage Plan, Percentage of Firms Which Offer Workers a Choice, 2025
Figure 11.9: Among Large Firms Offering Retiree Benefits Through a Contract With a Medicare Advantage (MA) Plan, Percentage of Firms Which Believe the Shift to MA Lowered the Cost Per Retiree, 2025
Figure 11.10: Among Large Firms Offering Retiree Benefits But Not Currently Contracting With a Medicare Advantage (MA) Plan, Percentage of Firms Which Plan to Start Offering Health Benefits Through a MA Plan in the Next Two Years, 2025
Health Screening and Health Promotion and Wellness Programs
Most large firms offer some form of wellness program to help workers and their family members identify health issues and manage chronic conditions. Some employers believe that improving the health of workers and their family members can improve well-being and productivity, as well as reduce health care spending.
In addition to offering wellness programs, many large firms offer health screening programs. These include health risk assessments, which are questionnaires asking workers about lifestyle, stress, or physical health, and biometric screenings, which we define as in-person health examinations conducted by a medical professional. Firms and insurers may use the health information collected during screenings to target wellness offerings or other health services to workers with certain conditions or behaviors. Some firms have incentive programs that reward or penalize workers for different activities, including participating in wellness programs or completing health screenings.
Among large firms (more than 200 workers) offering health benefits in 2025, 53% offer workers the opportunity to complete a health risk assessment, 43% offer workers the opportunity to complete a biometric screening, and 83% offer workers one or more wellness programs, such as programs to help them stop smoking or lose weight, or lifestyle and behavioral coaching. Substantial shares of these firms provide incentives for workers to participate in or complete the programs.
Only firms offering health benefits were asked about their wellness and health promotion programs.
HEALTH RISK ASSESSMENTS
Many firms give their workers the option to complete a health risk assessment to identify potential health issues. Health risk assessments generally include questions about medical history, health status, and lifestyle. Health risk assessments may be administered by an insurer.
- Among firms that offer health benefits, 35% of firms with 10 to 199 workers and 53% of larger firms provide workers with the option to complete a health risk assessment, similar to the percentages last year [Figure 12.1].
- Focusing on firms with 200 or more workers, firms with 5,000 or more workers are more likely than smaller firms to provide workers with an opportunity to complete a health risk assessment (75% vs. 52%) and firms with 200 to 999 workers are less likely to do so compared to larger firms (51% vs. 61%) [Figure 12.1].
- Some firms offer incentives to encourage workers to complete a health risk assessment.
- Among firms with 200 or more workers that offer workers an opportunity to complete a health risk assessment, 51% of firms with 200 to 999 workers, 60% of firms with 1,000 to 4,999 workers, and 69% of firms with 5,000 or more workers use incentives or penalties to encourage workers to complete the assessment.
- The percentage for firms with 200 or more workers that use incentives or penalties to encourage workers to complete a health risk assessment (53%) is similar to the percentage (54%) last year [Figure 12.2].
Figure 12.1: Among Firms Offering Health Benefits, Percentage of Firms That Provide an Opportunity to Complete a Health Risk Assessment, by Firm Size, 2025
Figure 12.2: Among Firms Offering Health Benefits and Providing an Opportunity to Complete a Health Risk Assessment (HRA), Percentage of Firms That Offer Workers Incentives to Complete the HRA, by Firm Size, 2025
BIOMETRIC SCREENING
Biometric screening is a health examination that looks at a person’s key health metrics, such such as cholesterol level, body mass index (BMI), blood pressure, and blood glucose levels, to assess a person’s general health and to identify their risk factors for different health conditions. As defined by this survey, assessing smoking status is not considered biometric screening.
- Among firms that offer health benefits, 22% of firms with 10 to 199 workers and 43% of larger firms provide workers the opportunity to complete a biometric screening. These percentages are similar to those last year [Figure 12.3] [Figure 12.5].
- Some firms developed options for workers to complete biometric screening remotely.
- Among firms providing workers the opportunity to complete a biometric screening, 61% allow employees to complete the screening remotely, similar to the percentage last year (62%) [Figure 12.4].
- Some firms with biometric screening programs offer incentives to encourage workers to complete the screening.
- Among firms with a biometric screening program, 34% of firms with 10 to 199 workers and 62% of larger firms use incentives or penalties to encourage workers to complete the assessment. These percentages are similar to those last year year [Figure 12.6].
- In addition to incentives for completing a biometric screening, some firms have incentives or penalties based on whether or not workers meet specified biometric outcomes, such as maintaining a certain cholesterol level or body weight. Incentives related to tobacco use are not considered for this question.
- Among firms with a biometric screening program, 21% have incentives or penalties tied to whether workers meet specified biometric outcomes. This percentage is similar to the percentage (15%) last year.
Figure 12.3: Among Firms Offering Health Benefits, Percentage of Firms That Provide an Opportunity to Complete a Biometric Screening, by Firm Size, 2025
Figure 12.4: Among Firms Offering Health Benefits With a Biometric Screening Program, Percentage of Firms That Allow the Screening to Be Completed Remotely, by Firm Size, 2025
Figure 12.5: Among Large Firms Offering Health Benefits, Percentage of Firms That Provide an Opportunity to Complete Biometric Screening, 2012-2025
Figure 12.6: Among Large Firms Offering Health Benefits and Providing an Opportunity to Complete a Biometric Screening, Percentage of Firms With Incentives to Complete the Screening or Achieve Biometric Outcomes, by Firm Size, 2025
HEALTH SCREENING PROGRAMS
- Among firms offering health benefits, 42% of firms with 10 to 199 workers and 63% of larger firms offer workers a health risk assessment, biometric screening, or both, to their workers. These percentages are similar to those last year [Figure 12.9].
Figure 12.7: Among Large Firms Offering Health Benefits, Percentage of Firms That Provide an Opportunity to Complete a Biometric Screening or a Health Risk Assessment, by Region and Industry, 2025
Figure 12.8: Among Large Firms Offering Health Benefits, Percentage With Health Screening Programs, 2025
Figure 12.9: Among Large Firms Offering Health Benefits, Percentage With Either a Health Risk Assessment or a Biometric Screening, 2013-2025
WELLNESS AND HEALTH PROMOTION PROGRAMS
Large shares of employers offer wellness and health promotion programs to help workers engage in healthy lifestyles and reduce health risks. These may include exercise programs, health education classes, health coaching, and stress-management counseling. These programs may be offered directly by the firm, or by an insurer or third-party vendor.
- Stop Smoking or Using Tobacco. Among firms offering health benefits, 43% of firms with 10 to 199 workers and 68% of larger firms offer programs to help workers stop smoking or using tobacco [Figure 12.11]. Firms with 5,000 or more workers are more likely than other larger firms to offer such a program (83% vs. 68%).
- Weight Loss. Among firms offering health benefits, 42% of firms with 10 to 199 workers and 63% of larger firms offer programs to help workers lose weight [Figure 12.11]. Firms with 5,000 or more workers are more likely than other larger firms to offer such a program (84% vs. 62%).
- Life Style Coaching. Among firms offering health benefits, 48% of firms with 10 to 199 workers and 74% of larger firms offer one or more other lifestyle or behavioral coaching programs to their workers [Figure 12.11]. Firms with 5,000 or more workers are more likely than other larger firms to offer such programs (88% vs. 73%).
- Overall, 56% of small firms and 83% of large firms offering health benefits offer at least one of these three types of programs to their workers [Figure 12.10] and [Figure 12.11]. These percentages are similar to those last year.
- Twenty-three percent of firms with 10 to 199 workers and 46% of larger firms offering one of these wellness or health promotion programs offer an incentive for workers to participate in or complete the program. These percentages of firms with 200 or more workers offering an incentive is similar to the percentage last year. [Figure 12.13].
- Firms with 5,000 or more workers are more likely than other larger firms to offer an incentive for workers to participate in or complete a wellness or health promotion program (61% vs. 45%) [Figure 12.13].
Figure 12.10: Among Firms Offering Health Benefits, Percentage of Firms Offering Specific Wellness Programs to Their Workers, by Firm Size and Region, 2025
Figure 12.11: Among Firms Offering Health Benefits, Percentage of Firms Offering Specific Wellness Programs to Their Workers, by Firm Size, 2025
Figure 12.12: Among Firms Offering Health Benefits, Percentage of Firms Offering Wellness Programs, by Firm Size, 2015-2025
Figure 12.13: Among Firms Offering Specific Wellness Programs, Percentage of Firms That Offer Incentives to Participate in or Complete Wellness Programs, by Firm Size, 2025
Figure 12.14: Among Large Firms Offering Health Benefits, Percentage of Firms Offering Various Wellness and Health Promotion Activities and Incentives, by Firm Size, 2025
SURCHARGES AND INCENTIVES RELATED TO TOBACCO USE
Some firms require employees that use tobacco products to pay higher premium contributions or cost sharing. A small share of firms say that not smoking is a condition of employment and they are not included in the estimates here.
- Among firms that offer health benefits, 5% of firms with 10 to 199 workers and 14% of larger firms have higher premium contributions or cost-sharing for employees who use tobacco products or vape [Figure 12.15].
- Firms with 5,000 or more workers are more likely than other larger firms (200 to 4,999 workers) to have higher contributions or cost sharing for employees that use tobacco produces or vape (38% vs. 13%) [Figure 12.15].
- Among firms that offer health benefits, 1% of firms with 10 to 199 workers and 7% of larger firms provide employees with some form of direct payment (such as a higher account contribution) or payroll deduction based on whether or not an employee uses tobacco products or vapes [Figure 12.16].
- Firms with 5,000 or more workers are more likely than other larger firms (200 to 4,999 workers) to provide employees with some form of direct payment incentive or payroll deduction based on whether or not an employee uses tobacco products or vapes (19% vs. 7%) [Figure 12.16].
Figure 12.15: Among Firms Offering Health Benefits, Percentage of Firms Which Charge Penalties to Employees Who Use Tobacco or Vape, by Firm Size, 2015-2025
Figure 12.16: Among Firms Offering Health Benefits, Percentage of Firms Which Offer Direct Payments or Charge Penalties to Employees Based On Tobacco or Vape Usage, by Firm Size, 2025
Figure 12.17: Among Large Firms Offering Workers an Incentive or Penalty for Smoking or Vaping, Maximum Annual Value of the Incentive Based On an Enrollee’s Smoking Status, 2025
Employer Practices, Employee Concerns, and Access to Care: Provider Networks, Coverage for GLP-1s, and Primary Care
Employers frequently review and modify their health plans to incorporate new options or adapt to circumstances. The topics this year include: factors contributing to higher premiums; the structure and breadth of provider networks; direct contracting; specialty networks; alternative pricing approaches, such as reference pricing and variable copayments; access to primary care; menopause benefits; GLP-1 drug coverage for weight loss; employee concerns with plans and utilization management; price and cost-sharing information for enrollees; employer coverage and Medicaid; and flexible spending accounts (FSAs).
FACTORS CONTRIBUTING TO HIGHER PREMIUMS
Firms that offer health benefits with 200 or more workers were asked about the factors that they believe have contributed to higher health plan premiums in recent years.
- Thirty-six percent of large firms say that prescription drug prices contributed “a great deal” to higher premiums, 35% say that they contributed “somewhat” to higher premiums, while smaller shares say prescription drug prices contributed “very little” (10%) or “not at all” (6%) [Figure 13.1].Firms with 1,000 or more workers are more likely than firms with 200 to 999 workers to say that prescription drug prices contributed “a great deal” to higher premiums.
- Thirty percent of large firms say that the prevalence of chronic diseases contributed “a great deal” to higher premiums, 39% say that it contributed “somewhat” to higher premiums, 12% say that it contributed “very little” to higher premiums, and 6% say that it contributed “not at all” [Figure 13.1]. Firms with 5,000 or more workers are more likely to say that the prevalence of chronic diseases contributed “a great deal” to higher premiums while firms with 200 to 999 workers are less likely to respond so.
- Twenty-six percent of large firms say that higher utilization of health care services contributed “a great deal” to higher premiums, 37% say that it contributed “somewhat” to higher premiums, 18% say that it contributed “very little” to higher premiums, and 6% say that it contributed “not at all” [Figure 13.1]. Firms with 1,000 or more workers are more likely than firms with 200 to 999 workers to say that higher utilization of health care services contributed “somewhat” to higher premiums.
- Twenty-two percent of large firms say that higher prices for hospital services contributed “a great deal” to higher premiums, 41% say that they contributed “somewhat” to higher premiums, 13% say that they contributed “very little” to higher premiums, and 7% say that contributed “not at all” [Figure 13.1]. Firms with 1,000 or more workers are more likely than firms with 200 to 999 workers to say that higher prices for hospital services contributed “somewhat” to higher premiums.
- Twenty-two percent of large firms say that new prescription drugs contributed “a great deal” to higher premiums, 36% say that they contributed “somewhat” to higher premiums, 17% say that they contributed “very little” to higher premiums, and 9% say that contributed “not at all” [Figure 13.1]. Firms with 1,000 or more workers are more likely than firms with 200 to 999 workers to say that new prescription drugs contributed “a great deal” to higher premiums.
Figure 13.1: Large Firms’ Perspectives On the Factors Contributing to Rising Premiums in Recent Years, 2025
Figure 13.2: Largest Firms’ Perspectives On the Factors Contributing to Rising Premiums in Recent Years, 2025
PROVIDER NETWORKS AND CONTRACTING APPROACHES
Firms and health plans structure their networks of providers to ensure access to care, and to encourage enrollees to use providers who are lower cost, or who provide better care. Some firms, particularly larger firms, are incorporating direct contracting arrangements with providers or using tiered cost-sharing to encourage employees to use lower-cost or higher quality providers.
HIGH PERFORMANCE OR TIERED PROVIDER NETWORKS
Some firms offer high-performance networks or tiered networks. These types of networks use cost-sharing or other incentives to encourage enrollees to use in-network providers that have better performance or quality or have lower costs.
- Among firms that offer health benefits with 50 or more workers, 15% offer a health plan with a high-performance or tiered network in 2025, lower than the percentage (20%) last year [Figure 13.3].
- Firms with 1,000 or more workers are more likely to include a high-performance or tiered network in their largest health plan than smaller firms (25% vs. 15%) [Figure 13.4].
Figure 13.3: Percentage of Firms With a High-Performance or Tiered Provider Network, by Firm Size, 2025
Figure 13.4: Percentage of Firms With a High-Performance or Tiered Provider Network, by Firm Size, 2007-2025
NARROW NETWORKS
Some employers offer a health plan with a relatively small, or narrow, network of providers to their employees. Narrow network plans limit the number of providers that can participate in order to reduce costs, and are generally more restrictive than standard HMO networks.
- Among firms that offer health benefits, 9% offer a health plan that can be considered a narrow network in 2025, similar to the percentage (8%) last year. Firms with 5,000 or more workers are more likely to offer a narrow network plan than smaller firms [Figure 13.5].
Figure 13.5: Percentage of Firms That Offer a Narrow Network Plan, by Firm Size, 2025
Figure 13.6: Among Firms Offering Health Benefits, Percentage of Firms That Offer a Narrow Network Plan, by Firm Size, 2014-2025
DIRECT CONTRACTING WITH HOSPITALS AND HEALTH SYSTEMS
Some large employers contract directly with providers, such as hospital or health systems, to provide for their employees outside of their health plan’s network.
- Among firms that offer health benefits with 200 or more workers, 5% of firms with 200 to 999 workers, 10% of firms with 1,000 to 4,999 workers, and 18% of firms with 5,000 or more workers have direct contracts with hospitals or health systems to provide services to enrollees separate from their health plan contracts. A larger percentage of firms with 5,000 or more workers have direct contracts in 2025 compared to 2019 [Figure 13.7].
Figure 13.7: Percentage of Large Firms Offering Health Benefits That Have Any Direct Contracts With Hospitals or Health Systems, Separate From Provider Networks, 2019-2025
SPECIALTY NETWORKS
Some large employers contract with vendors that offer networks of specialists to provide care for certain types of services. These can include cancer, heart disease, musculoskeletal care or other types of specialty care. These networks offer access to specialty services beyond those that otherwise would be available in the firm’s health plans’ networks.
- Among firms that offer health benefits with 500 or more workers, 4% of firms with 500 to 999 workers, 8% of firms with 1,000 to 4,999 workers, and 19% of firms with 5,000 or more workers have vendor contracts to provide specialty care for their employees outside of their health plan network [Figure 13.8].
- Firms with vendor contracts for specialty care were asked if enrollees had lower out-of-pocket costs if they received services through the specialty network. Among these firms, 26% have lower cost sharing for enrollees who use services through the specialty network, 17% cover some services only through the specialty network, 32% do not have lower cost sharing for services provided through the specialty network, and 25% did not know.
Figure 13.8: Percentage of Firms Whose Plans Include a Specialty Provider Network Focused On Specific Conditions, by Firm Size, 2025
VARIABLE COPAYMENTS AND REFERENCE PRICING
Some plans and vendors, such as Surest and Coupe Health, have developed products that eliminate deductibles for some services but use copayment amounts that vary based on the cost and practices of the provider they choose. The approach allows enrollees to lower their cost sharing by choosing more cost efficient providers.
- Among firms that offer health benefits with at least 500 workers, 9% offer a plan to at least some employees that uses the variable copayment approach. This percentage is similar across firm sizes for these large firms [Figure 13.9].
Reference pricing is an approach where a health plan pays a prescribed amount for a service and the enrollee is responsible for the difference between the plan payment and the amount charged by the provider. The reference price may be based on a benchmark, such as a percentage of Medicare payments or some percentile of the cost for similar services. Larger firms were asked if their plan with the largest enrollment paid for any services other than prescription drugs using reference pricing.
- Among firms that offer health benefits with at least 500 workers, 7% use reference pricing for at least some services other than prescriptions in their plan with the largest enrollment. This percentage is similar to the percentage of firms that used reference pricing in 2018 and 2014 [Figure 13.10].
Figure 13.9: Percentage of Firms That Vary Copays Based On Provider Costs, by Firm Size, 2025
Figure 13.10: Percentage of Large Firms Offering Health Benefits That Use Reference Pricing for Any Medical Services, 2014-2025
SUFFICIENCY OF PROVIDER NETWORKS
Firms offering health benefits were asked about whether they believed that the provider network for their health plan with the largest enrollment had sufficient numbers of providers to provide timely access to primary care, specialty care, and mental health services.
- Ninety-two percent of firms that offer health benefits believe that there are a sufficient number of providers in their health plan with the largest enrollment to provide timely access to primary care services for their workers [Figure 13.11]. This percentage is similar for smaller and larger firms [Figure 13.12].
- Although there appears to be broad satisfaction in the sufficiency of provider networks for primary care, 4% of small firms with 50 or more workers and 8% of large firms, including 14% of firms with 5,000 or more workers, asked their insurer or plan administrator to increase the number of in-network primary care providers within the last two years [Figure 13.14].
- Eighty-nine percent of firms that offer health benefits believe that there are a sufficient number of providers in their health plan with the largest enrollment to provide timely access to specialty care services for their workers [Figure 13.11]. This percentage is similar for smaller and larger firms [Figure 13.12].
- Seventy percent of firms that offer health benefits believe that there are a sufficient number of providers in their health plan with the largest enrollment to provide timely access to mental health services for their workers [Figure 13.11]. This percentage is similar for smaller and larger firms [Figure 13.12].
Figure 13.11: Among Firms Offering Health Benefits, Percentage of Firms Which Believe That There Are a Sufficient Number of Providers in Their Plan’s Networks to Provide Timely Access to Services, 2025
Figure 13.12: Among Firms Offering Health Benefits, Percentage of Firms Which Believe That There Are a Sufficient Number of Providers in Their Plan’s Networks to Provide Timely Access to Services, by Firm Size, 2025
APPROACHES TO PRIMARY CARE
Some employers are using alternative approaches to provide primary care options for their workers. These include approaches using virtual care and direct contracts with networks of primary care providers.
- Among firms with 50 or more workers that offer health benefits, 30% have a contract to provide virtual primary care services, including telehealth primary care options, that go beyond the services provided to workers in their health plan networks [Figure 13.14]. Firms with 1,000 or more workers are more likely than smaller firms to have a contract for virtual primary care services (45% vs. 29%).
- Among firms with 50 or more workers that offer health benefits, 7% contract directly with an organization to provide primary care services to their workers in addition to the primary care providers offered through their health plan networks [Figure 13.14]. The percentage is similar for smaller and larger firms.
Figure 13.13: Percentage of Firms Offering Enrollees Additional Primary Care Options by Firm Size, 2025
Figure 13.14: Percentage of Firms Which Have Taken Any Steps to Increase the Number of Primary Care Providers, by Firm Size, 2025
MENOPAUSE SUPPORT BENEFITS
Some employers contract with a vendor to offer specialized care or a virtual care benefit to provide support for enrollees during menopause. These services may include education, access to specialty care and mental health support.
- Among employers with 200 or more workers that offer health benefits, 4% of firms with 200 to 999 workers, 10% of firms with 1,000 to 4,999 workers, and 13% of firms with 5,000 or more workers have vendor contracts to provide support for workers or their dependents during menopause [Figure 13.15].
Figure 13.15: Percentage of Large Firms That Contract With a Third-Party Vendor to Offer Specialized Menopause Care, by Firm Size, 2025
GLP-1 DRUG COVERAGE FOR WEIGHT LOSS
GLP-1 agonists, used to help control blood sugar levels in people with type 2 diabetes, have also been shown to be an effective drug to help people lose weight. Common brand names include Ozempic, Wegovy, Mounjaro, Saxenda, and Victoza. Health plans generally have covered these medications when prescribed for people with diabetes, but there has been a growing interest in the extent to which employer plans and other payers cover them for people who have a clinical need to lose weight. The relatively high cost of these drugs, combined with the likelihood of long-term usage, has raised questions about the potential costs to plans that cover them.
Firms that offer health benefits with 200 or more workers were asked about their coverage of GLP-1 agonists when used primarily for weight loss.
- Among firms that offer health benefits with 200 or more workers, 16% of firms with 200 to 999 workers, 30% of firms with 1,000 to 4,999 workers, and 43% of firms with 5,000 or more workers cover GLP-1 agonists when used primarily for weight loss [Figure 13.16].
- The overall percentage of firms with 200 or more workers that cover GLP-1 agonists for weight loss (19%) is similar to the percentage last year (18%).
- The percentage of firms with 5,000 or more workers that cover GLP-1 agonists for weight loss is higher than the percentage last year (43% vs. 28%).
- The percentage of firms that did not know if they covered GLP-1 agonists for weight loss is higher for firms with 200 to 999 workers than for larger firms [Figure 13.16].
Thirty-four percent of firms with 200 or more workers that cover GLP-1 agonists for weight loss require enrollees to meet with a dietitian, case manager, or therapist, or participate in a lifestyle program in order for the drug to be covered. Firms with 200 to 999 workers are more likely than larger firms to respond that they do not to know the answer to this question [Figure 13.17].
Firms with 200 or more workers that cover GLP-1 agonists for weight loss were asked how the use of GLP-1 agonists for weight loss compared to their expectations.
- 44% of firms with 1,000 to 4,999 workers, and 59% of firms with 5,000 or more workers say that the use of these medications for weight loss was higher than expected.
- Firms with 200 to 999 workers were much less likely than larger firms to say that the use of these medications for weight loss was higher than expected (12% vs. 48%) and were more likely to respond that they did not know the answer to the question (36% vs. 11%). These smaller firms may not receive as much information about the utilization of specific services as larger firms [Figure 13.18].
Firms with 200 or more workers that cover GLP-1 agonists for weight loss were asked about the impact that covering GLP-1 agonists had on their spending for prescription drugs.
- Forty-three percent of firms with 1,000 to 4,999 workers, and 66% of firms with 5,000 or more workers say that covering GLP-1 agonists for weight loss had a “significant” impact on the health plan’s prescription drug spending.
- Firms with 200 to 999 workers were less likely than larger firms to say that covering these medications for weight loss had a “significant” impact on their health plan’s prescription drug spending (22% vs. 49%) and were more likely than larger firms to say that the impact on plan prescription drug spending was “minor” (26% vs. 11%) [Figure 13.19].
Firms with 200 or more workers were asked about the importance of covering GLP-1 agonists for weight loss for employee satisfaction with their health plan.
- Among these firms that cover GLP-1 agonists for weight loss, 26% say that covering these medications for weight loss is “very important” for employee satisfaction, 37% say that it is “important,” 20% say it is “somewhat important,” 5% say that it is “not important,” and 12% do not know the answer to this question [Figure 13.20].
- Among these firms that do not cover GLP-1 agonists for weight loss, 18% say that covering these medications for weight loss is “very important” for employee satisfaction, 27% say that it is “important,” 36% say it is “slightly important,” 13% say that it is “not important,” and 6% do not know the answer to this question.
Firms with 200 or more workers that offer health benefits but do not cover GLP-1 agonists for weight loss were asked how likely it is that they would begin doing so within the next 12 months.
- Among these firms, only 1% say that they are “very likely” to begin covering GLP-1 agonists for weight loss within the next 12 months, 24% say that they were “somewhat likely,” 67% say that they were “not likely,” and 8% do not know the answer to the question [Figure 13.21].
Figure 13.16: Percentage of Large Firms Whose Largest Plan Includes Coverage for GLP-1 Agonists When Used Primarily for Weight Loss, by Firm Size, 2024-2025
Figure 13.17: Among Large Firms Covering GLP-1s for Weight Loss, Share Requiring Lifestyle or Clinical Support, by Firm Size, 2025
Figure 13.18: Large Firms’ Views On How GLP-1 Utilization for Weight Loss Compares to Expectations, by Firm Size, 2025
Figure 13.19: Large Firms’ Views On the Impact of GLP-1 Coverage for Weight Loss On Prescription Drug Spending, by Firm Size, 2025
Figure 13.20: Large Firms’ Views On the Importance of Covering GLP-1s for Weight Loss to Enrollee Satisfaction, by Firm Size, 2025
Figure 13.21: Among Large Firms Not Covering GLP-1 Agonists for Weight Loss, Views On the Likelihood of Adding Coverage in the Next 12 Months, by Firm Size, 2025
EMPLOYEE CONCERNS WITH PLAN AND UTILIZATION MANAGEMENT
Consumer concerns about health plan management—such as prior authorization requirements—have received growing public attention in recent years. Firms offering health benefits were asked to assess how concerned they believe their employees are about various aspects of health plan management.
Affordability of Cost Sharing. Among firms offering health benefits, 16% believe that their employees level of concern over the affordability of cost sharing is “high,” 29% believe the level of concern is “moderate,” 28% believe the level of concern is “low,” 20% believe the level of concern is “none,” and 7% do not know the level of concern [Figure 13.22].
- Firms with 10 to 199 workers are more likely than larger employers to believe their employees have no concern about the affordability of cost sharing (21% vs. 12%).
Scheduling Timely Appointments With Providers. Among firms offering health benefits, 10% believe that their employees level of concern over their ability to schedule timely appoints is “high,” 20% believe the level of concern is “moderate,” 32% believe the level of concern is “low,” 30% believe the level of concern is “none,” and 8% do not know the level of concern [Figure 13.22].
- Firms with 200 or more workers are more likely than smaller firms to believe that employees have a “high” or “moderate” level of concern about their ability to schedule timely appointments with providers (43% vs. 29%).
- Firms with 10 to 199 workers are more likely than larger employers to believe their employees have no concern about their ability to schedule timely appointments with providers (31% vs. 20%).
Complexity of Prior Authorization Requirements. Among firms offering health benefits, 5% believe that their employees level of concern over the complexity of prior authorization requirements is “high,” 23% believe the level of concern is “moderate,” 33% believe the level of concern is “low,” 28% believe the level of concern is “none,” and 10% do not know the level of concern.
- Firms with 200 or more workers are more likely than smaller firms to believe that employees have a “high” or “moderate” level of concern about the complexity of prior authorization requirements (44% vs. 27%).
- Firms with 10 to 199 workers are more likely than larger employers to believe their employees have no concern about the complexity of prior authorization requirements (29% vs. 16%).
Finding In-Network Providers. Among firms offering health benefits, 4% believe that their employees level of concern over the difficulty of finding in-network providers is “high,” 13% believe the level of concern is “moderate,” 42% believe the level of concern is “low,” 35% believe the level of concern is “none,” and 5% do not know the level of concern.
- Firms with 10 to 199 workers are more likely than larger employers to believe their employees have no concern about their ability to find in-network providers (29% vs. 16%).
Number of Denied Claims. Among firms offering health benefits, 4% believe that their employees level of concern about the number of denied claims is “high,” 11% believe the level of concern is “moderate,” 40% believe the level of concern is “low,” 23% believe the level of concern is “none,” and 21% do not know the level of concern.
Figure 13.22: Among Firms Offering Health Benefits, How Much Concern Do Employers Have With Various Elements of the Firm’s Plans, 2025
Figure 13.23: Among Large Firms Offering Health Benefits, How Much Concern Do Employers Have With Various Elements of the Firm’s Plans, 2023-2025
PRICE AND COST SHARING INFORMATION FOR ENROLLEES
Firms that offer health benefits with 200 or more workers were asked how they think enrollees use information on the cost of services provided by their health plan.
- Among these firms, 8% say that enrollees use cost information provided by their health plans “a great deal,” 41% say that they use it “somewhat,” 36% say that they use it “very little,” and 5% say that they use it “not at all,” and 10% do not know the answer to the question [Figure 13.24].
Federal rules require health plans (including self-funded plans) to make information available to enrollees about the estimated cost of services and cost-sharing on a “real-time” basis. Firms that offer health benefits with 200 or more workers were asked about the potential effectiveness of these new requirements.
- Among these firms, 27% say that providing employees with additional information about the cost of services will help their health care decision making “a great deal,” 45% say that it will help their decision making “somewhat,” 21% say that it will help their decision making “very little,” and 3% say that it will help their decision making “not at all” [Figure 13.25].
Firms also were asked if they have conducted or received data analyses that used price transparency information.
- Eighteen percent of firms that offer health benefits with 200 or more workers say that they have conducted or received analyses using price transparency data [Figure 13.26].
Figure 13.24: Large Firms’ Views On How Often Enrollees Use Cost Information Provided by Their Plans, by Firm Size, 2025
Figure 13.25: Firms’ Views On How Much Providing Employees With Service Cost Information Helps Their Healthcare Decision-Making, by Firm Size, 2025
Figure 13.26: Percentage of Firms That Have Conducted or Received an Analysis Using Price Transparency Data, by Firm Size, 2025
EMPLOYER COVERAGE AND MEDICAID
Some lower-income employees are covered by Medicaid. Firms that offer health benefits and firms that do not were each asked about the importance of Medicaid coverage of their employees, both as primary coverage for employees not covered by the firm and as a source of payment for out of pocket expenses for employees covered by the firm.
- Among firms that do not offer health benefits with 10 to 199 workers, 34% say that Medicaid is “very important” in providing health coverage to their employees, 22% say that Medicaid is “somewhat important,” 9% say that Medicaid is “neither important nor unimportant,” 12% say that Medicaid is “not very important,” 13% say Medicaid is “not at all important,” and 11% did not know the answer to the question [Figure 13.27].
- Firms with 50 to 199 employees were more likely than smaller firms to say that Medicaid is “very important” in providing health coverage to the firm’s employees (63% vs. 33%).
- Among small firms that offer health benefits, 29% say that Medicaid is “very important” in providing health coverage to employees not covered by the firm’s health plan, 18% say that Medicaid is “somewhat important,” 10% say that Medicaid is “neither important nor unimportant,” 14% say that Medicaid is “not very important,” 16% say Medicaid is “not at all important,” and 13% did not know the answer to the question [Figure 13.27].
- Firms with 10 to 49 workers that offer health benefits are less likely than larger firms to say that Medicaid is “very important” or “somewhat important” in providing health coverage to employees not covered by the firm’s health plan (43% vs. 60%).
- Firms with 10 to 49 workers that offer health benefits are more likely than larger firms to say that Medicaid is “not at all important” in providing health coverage to employees not covered by the firm’s health plan (19% vs. 6%).
- Among large firms that offer health benefits, 17% say that Medicaid is “very important” in helping to pay for out-of-pocket expenses or to pay for services for employees covered by the firm’s health plan, 25% say that Medicaid is “somewhat important,” 15% say that Medicaid is “neither important nor unimportant,” 16% say that Medicaid is “not very important,” 11% say Medicaid is “not at all important,” and 17% did not know the answer to the question [Figure 13.28].
Figure 13.27: Among Large Firms Offering Health Benefits, Firms’ Views On the Importance of Medicaid in Covering Employees and Offsetting Health Costs for Plan Enrollees, 2025
Figure 13.28: Among Small Firms, Firms’ Views On the Importance of Medicaid in Covering Employees, 2025
PRE-TAX ACCOUNTS FOR MEDICAL EXPENSES
Flexible spending accounts (FSAs) allow employees to set aside funds on a pre-tax basis to pay for medical expenses not covered by health insurance. The legal maximum contribution for employee FSA contributions for 2025 is $3,300.
- Among firms that offer health benefits, 30% of small firms and 70% of large firms offer their employees an FSA for medical care [Figure 13.29]. The likelihood that a firm will offer an FSA for medical care increases with firm size, ranging from 25% for firms with 10 to 49 workers up to 96% for firms with 5,000 or more workers [Figure 13.30].
Firm contributions towards health plan premiums are not subject to federal income or payroll taxes. Firms have the option of sponsoring a plan under Section 125 of the Internal Revenue Code, which allows employees to make their contributions for health plan premiums on a pre-tax basis.
- Among firms that offer health benefits, 70% of small firms and 85% of large firms sponsor a plan that allows their employees to make their health plan premium contributions on a pre-tax basis.
- Firms with 10 to 49 workers are less likely than larger firms to offer such a plan (66% vs. 84%) [Figure 13.30].
- Firms with 1000 or more workers are more likely small larger firms to offer such a plan (92% vs. 71%).
Figure 13.29: Among Firms Offering Health Benefits, Percentage of Firms Offering a Flexible Spending Account, by Firm Size, 2007-2025
Figure 13.30: Among Firms Offering Health Benefits, Percentage of Firms Offering Flexible Spending Accounts and Pre-Tax Employee Premium Contributions, by Firm Size, 2025