Examining New Medicaid Resources to Expand School-Based Behavioral Health Services
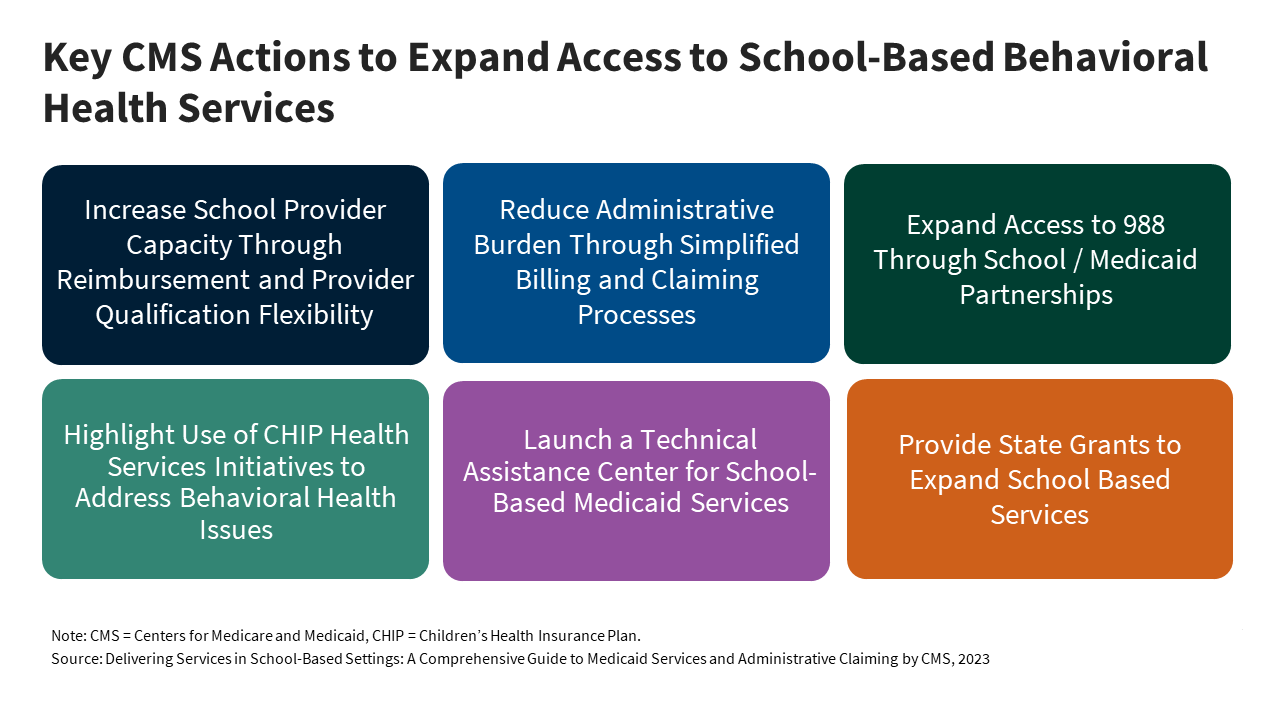
In light of worsening mental health among youth, strategies have been implemented to improve access to behavioral health services in recent years, including expanding school-based care for students. Leveraging Medicaid to improve and address gaps in school-based behavioral health services has been a key strategy in recent years as youth mental health concerns have grown. Provisions from the Safer Communities Act of 2022 utilize Medicaid to expand both school-based health care and other mechanisms of youth behavioral health care. This issue brief explores the implementation of these provisions from the Safer Communities Act thus far, with a focus on the guidance issued from CMS.