The Recovery of Community Health Centers in Puerto Rico and the US Virgin Islands One Year after Hurricanes Maria and Irma
Executive Summary
One year after hurricanes Maria and Irma struck Puerto Rico and the U.S. Virgin Islands (USVI), recovery has progressed but remains slow. This issue brief presents findings from the Geiger Gibson/Kaiser Family Foundation survey of community health centers in Puerto Rico and USVI one year after the hurricanes. It describes the current state of health center recovery and examines shifts in need and capacity, which have potential longer-term implications. Key findings include:
Health centers experienced an increase in the overall number of patients and an increase in patients with more complex mental and physical health needs in the year following the hurricanes. Nearly three-quarters of health centers reported an increase in the number of patients served, and some have experienced increases of 10% or more. Additionally, reflecting the lingering effects of the hurricanes, increasing numbers of health center patients are from suffering mental health problems, stress-related conditions, and poorly managed chronic health conditions. Health centers reported a substantial uptick in patients suffering from depression and anxiety, including post-traumatic stress disorder (PTSD), and said their patients are more likely to have suicidal thoughts and attempts than before the storms.
Many health centers expanded staff to meet patient needs, but some have experienced staffing losses over the past year. Most health centers have been able to retain or add key staff, including physicians and nurses as well as mental health staff. At the same time, losses of other professionals, including nurses, substance use disorder staff, and dental staff present challenges to service delivery for some health centers.
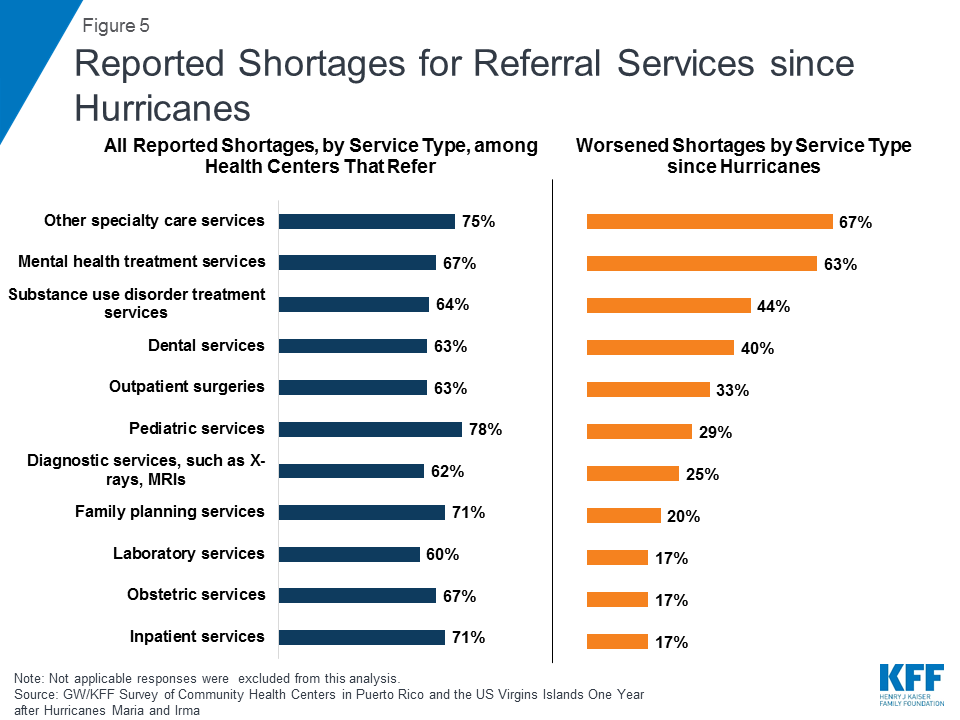
Health centers face increasing challenges referring patients with complex needs for more specialized care. While health centers have faced long-standing shortages when referring their patients for inpatient and specialty care, among health centers that refer patients, many said that these shortages have gotten worse since the hurricanes, likely due to outmigration of other community providers, and, in the USVI in particular, ongoing operational disruptions at hospitals. Provider shortages are particularly acute for mental health and other specialty care as well as substance use disorder treatment and dental care.
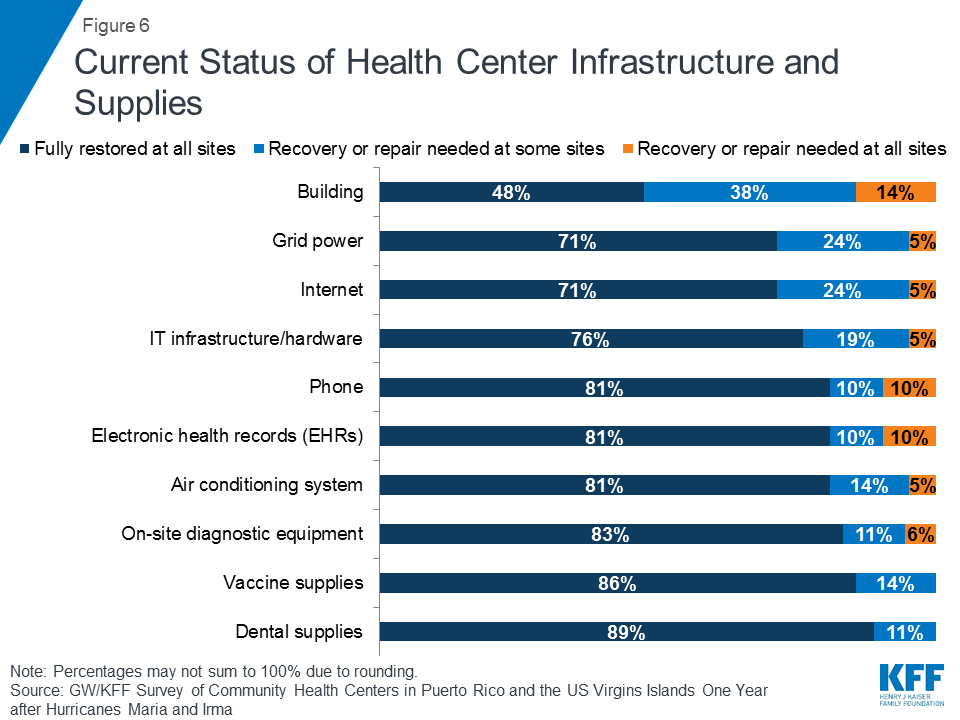
While most health centers reported that operations are back to normal at all sites, many continue to face critical infrastructure challenges. Over half of health centers reported that some or all sites still need repairs to their buildings and nearly 30% reported ongoing power grid and internet problems at some or all of their sites.
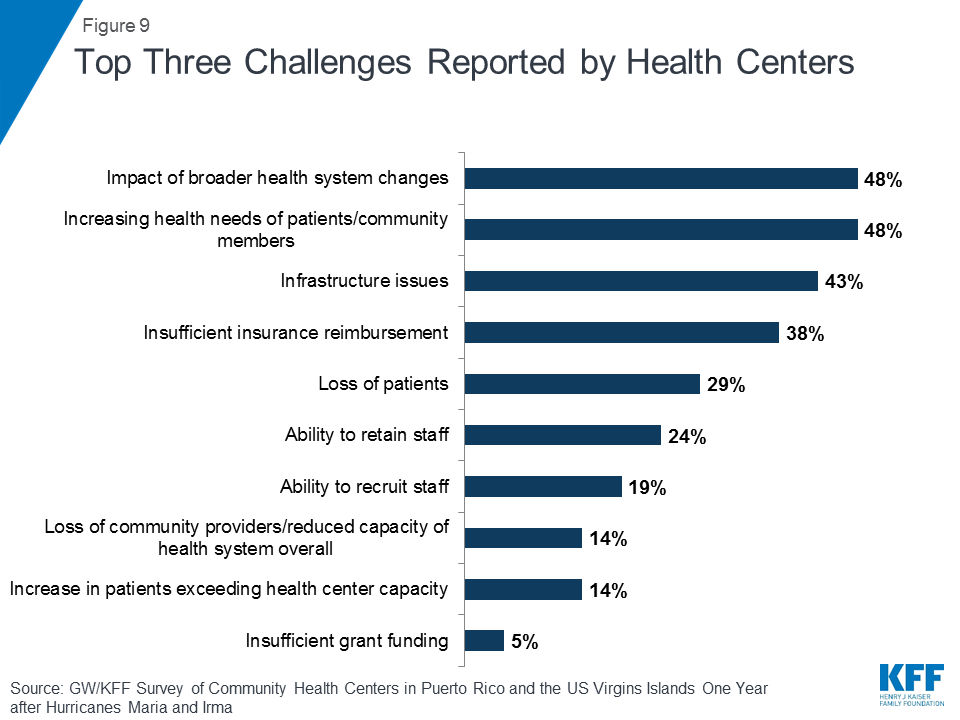
Meeting the increasing health needs of the community, and operating in a complex and insufficiently funded environment, emerged as top challenges. The most commonly cited challenges currently facing health centers were their patients’ growing health needs, broader health system changes, and infrastructure issues. Insurance revenue that is inadequate to cover the cost of care was reported as a top challenge by health centers in Puerto Rico, while health centers in USVI cited the loss of community providers and reduced capacity of the health system overall as a major concern.
Issue Brief
Introduction
In September 2017, hurricanes Maria and Irma struck Puerto Rico and the U.S. Virgin Islands (USVI), causing immediate widespread destruction and precipitating lingering infrastructure and health problems. In the year since the hurricanes hit, recovery of the health care system has been slow. Community health centers are an important part of the health care system and while most are fully operational, significant challenges remain.
In the wake of the hurricanes, researchers at the Geiger Gibson Program in Community Health Policy at George Washington University’s (GW’s) Milken Institute School of Public Health have been chronicling the recovery experiences of health centers in both Puerto Rico and the USVI. A report issued in early 2018 found that, a few months after the hurricanes, 65% of health centers required building repairs and nearly half (48%) needed repair or replacement of their internet and phone service.1 Health centers cited difficulties in recruiting and retaining physicians, pharmacy staff, mental health staff, and substance use disorder staff. Health centers reported that the loss of employees’ homes, transportation problems, and increased demand for care in community settings were among the top three challenges facing their staff.
This brief presents findings from the most recent Geiger Gibson/KFF survey of community health centers in Puerto Rico and USVI one year after the hurricanes. It describes the current state of health center recovery and examines shifts in need and capacity, which have potential longer-term implications.
Background
Community health centers play an especially important role in providing access to health care in both Puerto Rico and the USVI. In 2017, 20 federally-funded health centers2 and one look-alike health center3 in Puerto Rico served nearly 370,000 patients and the two health centers in the USVI served 16,010 patients.4 Together, federally-funded health centers on the islands, which operated in a total of 98 sites, registered over 1.5 million patient visits in 2017 (Table 1). Medicaid is the most important source of revenue for health centers in Puerto Rico and USVI, but they are also heavily reliant on federal Section 330 grant funding, and in the USVI, local grant funding. Health centers in Puerto Rico and USVI have been recognized by the federal government for quality and efficiency.5 In September 2018, the Department of Health and Human Services (HHS) awarded Capital Assistance for Hurricane Response and Recovery Efforts (CARE) funding to community health centers in states and territories affected by last year’s hurricanes.6 The two USVI health centers were awarded $1.26 million,7 while 19 health centers in Puerto Rico were awarded $12.8 million.8
| Table 1. Federally-funded Health Centers in Puerto Rico and US Virgin Islands | ||
| Puerto Rico | US Virgin Islands | |
| Number of sites | 93 | 5 |
| Total Patients | 358,528 | 16,010 |
| Total visits | 1,465,692 | 47,122 |
| Revenues | ||
| Total revenues | $301,397,359 | $17,783,678 |
| Medicaid | 51% | 30% |
| Medicare | 8% | 4% |
| Private insurance | 3% | 4% |
| Federal 330 grants | 31% | 30% |
| State/local/private grants/contracts | 1% | 23% |
| Self-pay/Other | 6% | 9% |
| Source: GW analysis of 2017 Uniform Data System data, Health Resources and Services Administration | ||
A recent analysis increased Puerto Rico’s death toll from hurricane Maria. A study commissioned by Puerto Rico’s Governor reported that the disaster was associated with 2,975 excess deaths in the six months following the hurricane.9 This number far exceeds the official death toll of 64 reported in the immediate aftermath of the storm. The analysis, conducted by scientists at GW’s Milken Institute School of Public Health in collaboration with the University of Puerto Rico’s Graduate School of Public Health, also found that death rates were far more elevated in the poorest municipalities. While the study focuses on near-term mortality impact, its findings underscore systemic challenges and suggest that the 2017 hurricane events will carry major longer-term health consequences.
Key Findings
Greater demand and more complex needs
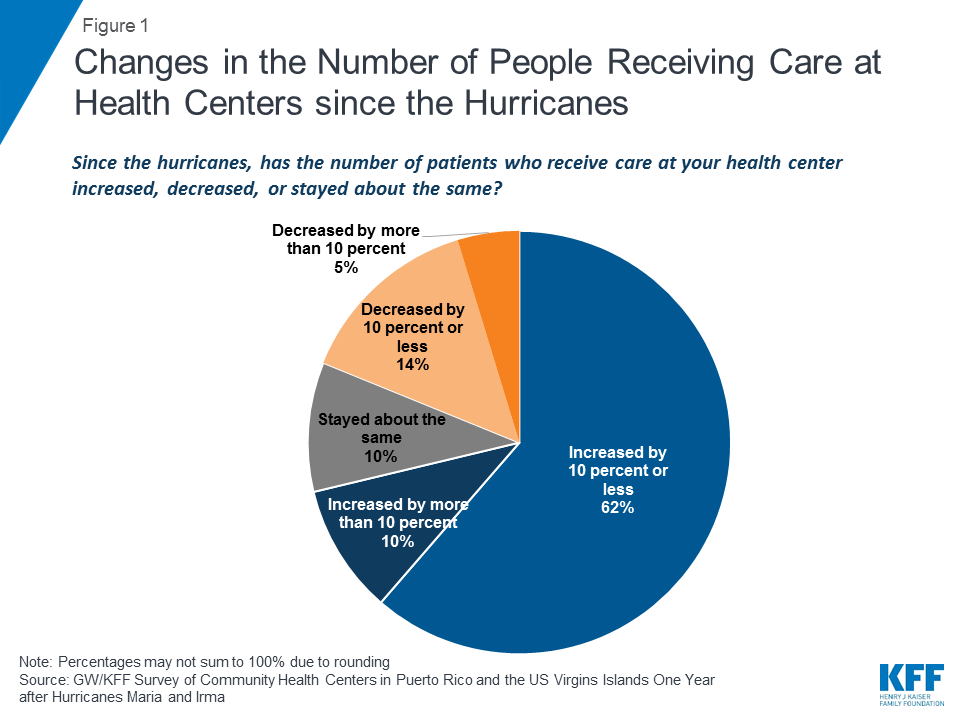
Most health centers experienced an increase in the number of patients seeking care in the year following the hurricanes. More than seven in ten (71%) health centers reported an increase in the number of patients they served (Figure 1). Both USVI health centers reported an increase in patients of 5-10%, while 68% of Puerto Rico health centers reported an increase in patients (Appendix Table 1). Still, one in five health centers said the number of patients they served had decreased, possibly due to ongoing infrastructure issues, staffing constraints, or population shifts.
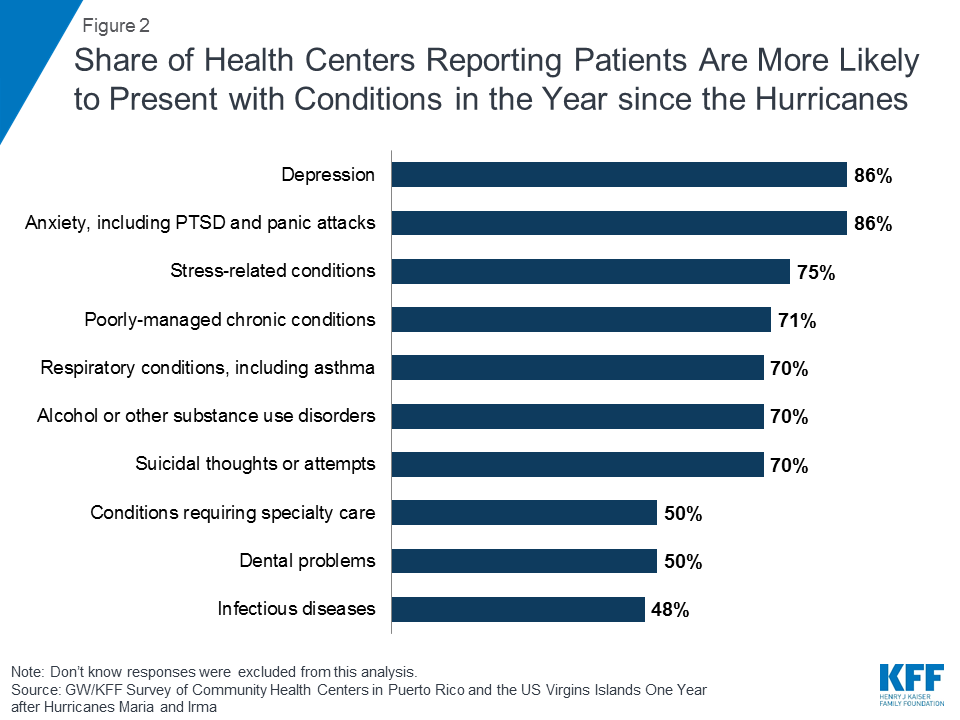
Reflecting the lingering effects of the hurricanes, increasing numbers of health center patients are suffering mental health problems, stress-related conditions, and poorly managed chronic health conditions. The trauma of living through the hurricanes and the stress of the recovery have taken a toll on the residents of Puerto Rico and USVI. Over eight in ten (86%) health centers reported an uptick in patients with depression and anxiety compared to the time period before the hurricanes, and seven in ten reported that patients were more likely to have suicidal thoughts or attempts and alcohol or other substance use disorders (Figure 2). Large shares of health centers also reported their patients were more likely to present with stress-related conditions such as insomnia and heart palpitations (75%), chronic conditions, such as diabetes and hypertension, that were not well-managed (71%), and respiratory conditions including asthma (70%).
Meeting patient demand for services
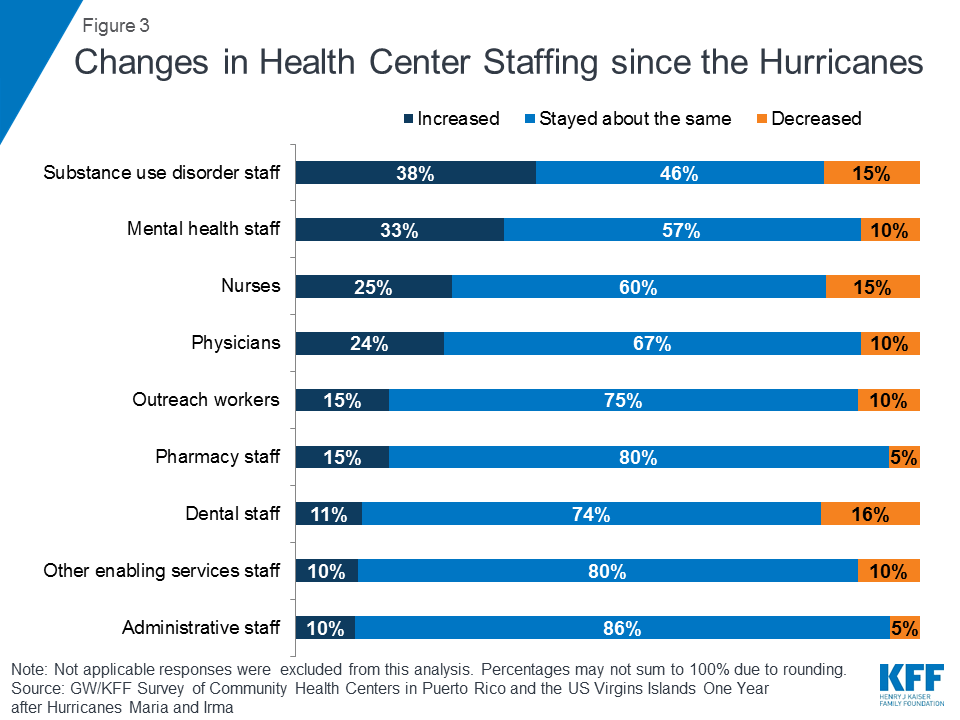
Many health centers have maintained or added staff to meet patient needs, but some have experienced staffing losses since the hurricanes. While many private providers left the islands in the aftermath of the hurricanes, most health centers were able to retain or expand key staff (Figure 3). As patient needs have increased, health centers have responded by expanding key staff. About a third of health centers reported an increase in mental health and substance use disorder staff, and one-quarter reported increased physicians and nurses. However, a small but sizable share of health centers reported decreased staffing, including dental staff (16%), nurses (15%), and substance use disorder staff (15%).
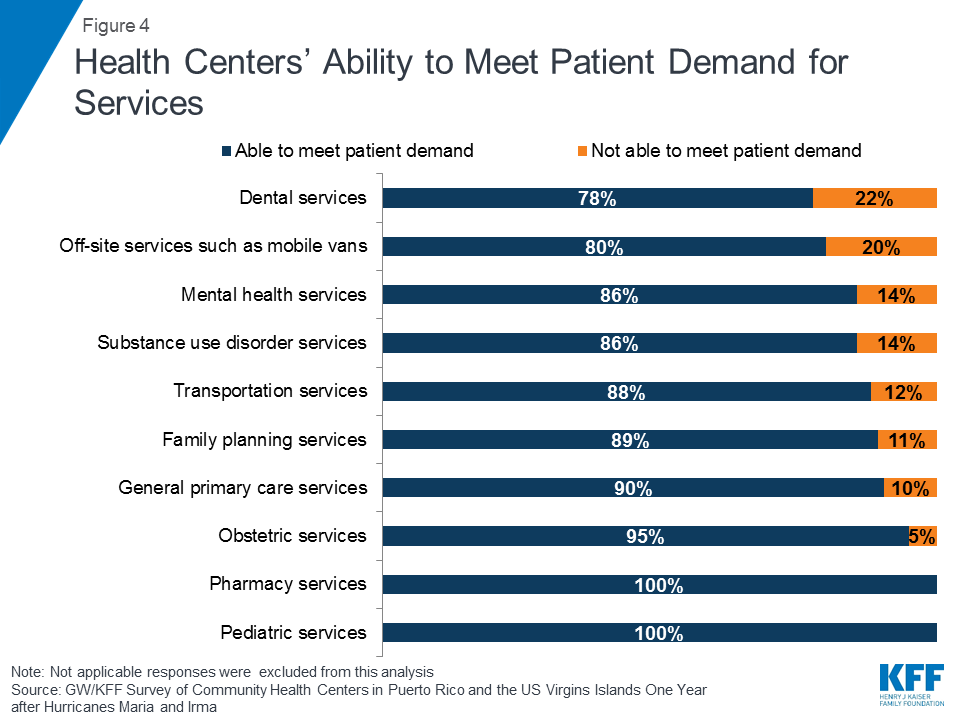
Despite increases in demand, most health centers were able to meet the need for services with available staffing. Health centers in Puerto Rico and USVI increased their capacity in response to the rising demand for services. All responding health centers reported that they were able to provide needed pediatric and pharmacy services, and nearly all were able to meet patient demand for obstetric care, family planning services, and general primary care services (Figure 4). At the same time, health centers were most likely to report not being able to meet patient demand for dental services (22%), off-site services (20%), mental health services (14%), and substance use disorder services (14%).
Health centers are experiencing growing constraints on their ability to secure specialty referrals for patients with complex needs. While health centers have increased capacity to meet the demand for a wide range of services at their facilities, some patients require more specialized services from other health care providers. Health centers in both Puerto Rico and USVI have faced longstanding provider shortages (defined as either no available providers or long wait times for appointments) when referring patients, but in some cases, these shortages have worsened since the hurricanes hit. Health centers that refer for services were most likely to report facing provider shortages when referring patients for inpatient hospital care, specialty care, and mental health care (Figure 5). While problems with access to hospital-based care predated the hurricanes, this remains a particular challenge in USVI where the hospital on St. Croix is operating at significantly reduced capacity.10 Although most health centers said they were able to provide needed pediatric and obstetric care on-site, when they did need to refer for these services, likely for pediatric specialty care and high-risk obstetric care, they faced significant challenges.
Even as more patients have presented with behavioral health and stress-related conditions and are in need of specialty care, shortages have worsened for mental health and other specialty care referrals. Among health centers that face shortages when referring patients, two-thirds said shortages for specialty and mental health care have gotten worse over the past year, and four in ten said access to substance use disorder treatment and dental care have worsened (Figure 5).
Current status of operations, services, and supplies
While most health centers are fully operational, many continue to face disruption and critical infrastructure challenges. Four in five (81%) health centers reported that operations are back to normal nearly a year after the hurricanes; however, this masks serious challenges facing some health centers (Appendix Table 2). Both health centers in the USVI are back to normal operations, while in Puerto Rico, three health centers continue to face minor disruptions at some or all sites and one reported critical disruptions at some sites. Over half (52%) of health centers still need repairs to buildings at some or all of their sites (Figure 6). Nearly three in ten health centers reported that grid power and internet have not been fully restored, and nearly a quarter reported that their IT infrastructure and hardware are in need of repair or replacement. While most said vaccine supplies are available at pre-hurricane levels, 14 percent noted that supplies have not been fully restocked at all sites.
Hurricane preparation and community-wide recovery actions
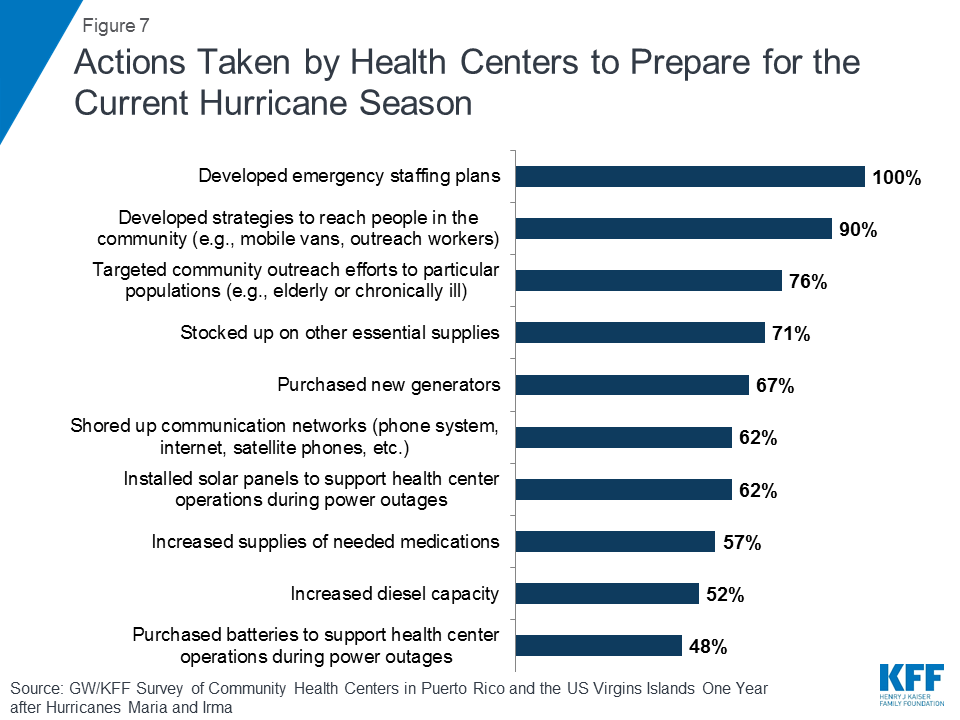
All responding health centers reported taking action to prepare for the current hurricane season, and developing emergency staffing plans was a top priority. Having withstood an unexpectedly catastrophic hurricane season, health centers have taken numerous steps to ensure they are prepared for the next storm. All said they had developed staffing plans for future emergencies and nine in ten reported developing strategies for community outreach, such as through mobile vans or community outreach workers (Figure 7). Over 70% said they planned to target community outreach to vulnerable populations like the elderly or people with chronic conditions and had stocked up on essential supplies. With ongoing electrical power problems for many health centers, over six in ten reported preparing for future power outages by purchasing new generators or installing solar panels.
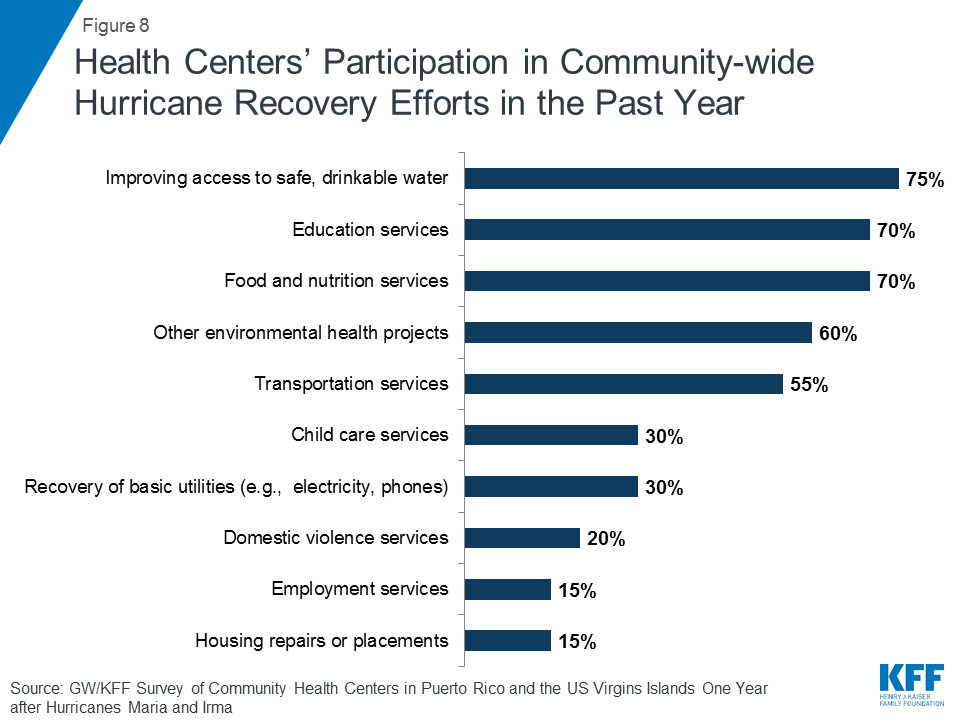
To assist in the broader hurricane recovery effort, most health centers participated in activities to improve access to critical health, social, and infrastructure services in their communities. Nearly all respondents indicated that their health centers had been involved in activities, either alone or with other community agencies and organizations, to address community-wide needs for recovery from the hurricanes in the past year. Three in four respondents reported participating in efforts to improve access to safe drinking water, seven in ten worked on education and food and nutrition initiatives, and six in ten reported participation in other environmental health projects (Figure 8).
Greatest challenges currently facing health centers
Meeting patients’ increasingly serious health care needs and operating in an insufficiently funded, complex, and rapidly evolving system emerged as top challenges. Health centers in Puerto Rico and USVI face many ongoing challenges as they work to recover fully from the hurricanes. The impact of broader health system change occurring in both territories, managing the increasingly complex health needs of patients, and ongoing infrastructure issues were among the top three challenges facing health centers in both Puerto Rico and USVI (Figure 9). More than four in five (83%) reported that the hurricanes worsened the impact of these challenges. Insufficient insurance reimbursement was reported as a top-three challenge by 42% of health centers in Puerto Rico, while health centers in USVI cited the loss of community providers and reduced capacity of the health system overall as a major concern (Appendix Table 3).
Discussion
One year after the hurricanes, health centers are grappling with a far sicker patient population, a fact that is not surprising given the devastating impact of the catastrophe on the health and well-being of the general population. Health centers continue to show recovery but still require repair, particularly of buildings, grid power, and internet. Staffing growth is underway, but health centers are also reporting the loss of key staff. Specialized referrals, never easy, present a growing challenge for some services. Nearly all health centers have been involved in community-wide recovery efforts as well as their own.
Consistent with the findings, health centers report that their top challenges are caring for a sicker patient population, meeting demand with limited revenue, and operating within the constraints of the broader changes in the health system, intensified in Puerto Rico by efforts to control health care costs in the face of the island’s ongoing financial crisis. The recovery grants awarded to health centers in both Puerto Rico and the USVI are an important step, but they are modest in size and do not obviate the need to maintain the strength of Medicaid funding, the most important source of health care financing for health centers operating on both islands. The greater reliance on federal health center funding in Puerto Rico and the USVI also underscores the importance of sustained federal grant funding to ensure that these community health centers are able to fully and effectively serve their patients.
The authors express their appreciation to Feygele Jacobs at the RCHN Community Health Foundation (RCHN CHF) for her assistance with the survey and invaluable insights on the brief. Additional funding support for this brief was provided to the George Washington University by RCHN CHF.
| Methods The Survey of Community Health Centers in Puerto Rico and US Virgin Islands One Year after Hurricanes Maria and Irma was conducted by the Geiger Gibson Program in Community Health Policy at the George Washington University (GW) and the Kaiser Family Foundation with support from the RCHN CHF. The online survey was distributed in August-September 2018 by email to upper-level management of the 23 community health centers in Puerto Rico and the USVI (21 health centers in Puerto Rico and two in USVI). Nineteen community health centers in Puerto Rico and both health centers in the USVI responded to the survey, for a 91% response rate. Survey findings are presented for all surveyed health centers and, for some questions, separately for Puerto Rico and USVI health centers. |
Appendix
| Appendix Table 1: Change in the number of patients who receive care at health centers since the hurricanes | |||
Percent of health centers where the number of patients since the hurricanes… | All(N=21) | Puerto Rico(N=19) | US Virgin Islands(N=2) |
| Stayed about the same | 10% | 11% | 0% |
| Increased by less than 5% | 19% | 21% | 0% |
| Increased by 5-10% | 43% | 37% | 100% |
| Increased by more than 10% | 10% | 11% | 0% |
| Decreased by 5-10% | 14% | 16% | 0% |
| Decreased by more than 10% | 5% | 5% | 0% |
| Appendix Table 2: Status of health center operations a year after the hurricanes | |||
Percent of health centers where… | All(N=21) | Puerto Rico(N=19) | US Virgin Islands(N=2) |
| Operations are mostly back to normal at all sites | 81% | 79% | 100% |
| Operations remain disrupted in minor ways at some or all sites | 14% | 16% | 0% |
| Operations remain disrupted in critical ways at some sites | 5% | 5% | 0% |
| Appendix Table 3: The three biggest challenges currently facing health centers | |||
Percentages reported for responses selected as a top three challenge | All(N=21) | Puerto Rico(N=19) | US Virgin Islands(N=2) |
| Infrastructure issues | 43% | 42% | 50% |
| Ability to recruit staff | 19% | 21% | 0% |
| Ability to retain staff | 24% | 26% | 0% |
| Loss of patients | 29% | 26% | 50% |
| Increase in patients exceeding health center capacity | 14% | 16% | 0% |
| Loss of community providers/reduced capacity of health system overall | 14% | 5% | 100% |
| Increasing health needs of patients/community members | 48% | 47% | 50% |
| Insufficient insurance reimbursement | 38% | 42% | 0% |
| Insufficient grant funding | 5% | 5% | 0% |
| Impact of broader health system changes | 48% | 47% | 50% |
| Other challenge | 19% | 21% | 0% |
Endnotes
- Sharac, J. & Rosenbaum, S. (2018). The state of recovery: an update on community health centers in Puerto Rico and the Virgin Islands. Geiger Gibson/RCHN Community Health Foundation Research Collaborative, George Washington University. Policy Research Brief No. 52. https://www.rchnfoundation.org/?p=6694 ↩︎
- Bureau of Primary Health Care. (2018). 2017 Health Center Data: Puerto Rico Data. Health Resources and Services Administration. https://bphc.hrsa.gov/uds/datacenter.aspx?q=tall&year=2017&state=PR ↩︎
- Bureau of Primary Health Care. (2018). 2017 Puerto Rico Health Center Data: Community Health Foundation of Puerto Rico Inc. Health Resources and Services Administration. https://bphc.hrsa.gov/uds/lookalikes.aspx?q=&bid=02E01268&state=PR&year=2017 Look-alike health centers must abide by health center program requirements but do not receive Bureau of Primary Health Care (BPHC) health center program funding. ↩︎
- Bureau of Primary Health Care. (2018). 2017 Health Center Data: Virgin Islands Data. Health Resources and Services Administration. https://bphc.hrsa.gov/uds/datacenter.aspx?q=tall&year=2017&state=VI ↩︎
- HRSA (2018). Health Center Quality Improvement FY2018 Grant Awards. https://bphc.hrsa.gov/programopportunities/qualityimprovement/awards.aspx?state=PR https://bphc.hrsa.gov/programopportunities/qualityimprovement/awards.aspx?state=VI ↩︎
- HHS.gov. (September 6, 2018). HHS awards nearly $60 million to support community health centers impacted by Hurricanes Harvey, Irma, and Maria. https://www.hhs.gov/about/news/2018/09/06/hhs-awards-60-million-support-community-health-centers-impacted-by-hurricanes.html ↩︎
- HRSA. (2018). FY 2018 Capital Assistance for Hurricane Response and Recovery Efforts (CARE) awards – Virgin Islands. https://bphc.hrsa.gov/programopportunities/fundingopportunities/care/fy2018awards/vi.html ↩︎
- HRSA. (2018). FY 2018 Capital Assistance for Hurricane Response and Recovery Efforts (CARE) awards – Puerto Rico. https://bphc.hrsa.gov/programopportunities/fundingopportunities/care/fy2018awards/pr.html ↩︎
- The George Washington University in Collaboration with the University of Puerto Rico Graduate School of Public Health (2018). Ascertainment of the estimated excess mortality from Hurricane María in Puerto Rico. https://publichealth.gwu.edu/sites/default/files/downloads/projects/PRstudy/Acertainment%20of%20the%20Estimated%20Excess %20Mortality%20from%20Hurricane%20Maria%20in%20Puerto%20Rico.pdf ↩︎
- Hall, C., Rudowitz, R., Artiga, S., and Lyons, B. (2018) One Year after the Storms: Recovery and Health Care in Puerto Rico and the U.S. Virgin Islands. Kaiser Family Foundation. ↩︎