The Uninsured at the Starting Line: Findings from the 2013 Kaiser Survey of Low-Income Americans and the ACA
Executive Summary
In January 2014, the major coverage provisions of the 2010 Affordable Care Act (ACA) went into full effect. These provisions include the creation of new Health Insurance Marketplaces where low and moderate income families can receive premium tax credits to purchase coverage and, in states that opted to expand their Medicaid programs, the expansion of Medicaid eligibility to almost all adults with incomes at or below 138% of the federal poverty level (FPL). The ACA has the potential to reach many of the 47 million Americans who lack insurance coverage, as well as millions of insured people who face financial strain or coverage limits related to health insurance.
Though implementation is underway and people are already enrolling in coverage, policymakers continue to need information to inform coverage expansions. Data on the population targeted for coverage expansions can help policymakers target early efforts, provide insight into some of the challenges that are arising in the first months of new coverage, and evaluate the ACA’s longer-term effects. The Kaiser Family Foundation has launched a new series of comprehensive surveys of the low and moderate income population to provide data on these groups’ experience with health coverage, current patterns of care, and family situation. This report, based on the baseline 2013 Kaiser Survey of Low-Income Americans and the ACA, provides a snapshot of health insurance coverage, health care use and barriers to care, and financial security among insured and uninsured adults across the income spectrum at the starting line of ACA implementation. The report also examines how findings from the baseline survey can help policymakers understand and address early challenges in implementing health reform. Detailed information on the survey design, sample, and analysis can be found in the Methods section at the end of the full report.
Background
Prior to implementation of the ACA, over 47 million Americans—nearly 18% of the population—were without health insurance coverage. Because publicly-financed coverage has been expanded to most low-income children and Medicare covers nearly all of the elderly, the vast majority of uninsured people are nonelderly adults.1 The main barrier that people have faced in obtaining health insurance coverage is cost: health coverage is expensive, and few people can afford to buy it on their own. While most Americans traditionally obtain health insurance coverage as a fringe benefit through an employer, not all workers are offered employer coverage, and not all adults are working. Medicaid and the Children’s Health Insurance Program (CHIP) cover many low-income children, but eligibility for parents and adults without dependent children is limited, leaving many adults without affordable coverage.
These barriers to coverage are reflected in the characteristics of the uninsured population. Uninsured adults are more likely to be low-income than people with private health insurance, while adults with Medicaid coverage are particularly low-income (reflecting very low pre-ACA eligibility limits). Corresponding to their lower incomes, uninsured adults are less likely than privately insured adults to be in a working family; however, the majority of uninsured adults are in a family with either a full- or part-time worker. Uninsured adults also differ from insured adults with regards to other demographic characteristics, often reflecting association with income or work status. For example, they are more likely to be younger than insured adults, as younger adults have lower incomes and looser ties to employment than older adults. There also are significant racial and ethnic differences in health coverage among nonelderly adults, primarily reflecting differences in income by race/ethnicity.
I. Patterns of Coverage and the Need for Assistance
Examining patterns of coverage and the reasons the uninsured lack coverage can inform both outreach avenues and potential barriers to outreach and enrollment. Key survey findings on access to coverage include:
For most currently uninsured adults, lack of coverage is a long-term issue. While some people experience short spells of uninsurance due to job changes, income fluctuations, or renewal issues, for most uninsured adults, lack of coverage is a chronic issue. The survey shows that almost half (47%) of uninsured report being uninsured for 5 years or more, and 18% report that they have never had coverage in their lifetime.
Many uninsured adults report trying to obtain insurance coverage in the past, but most did not have access to affordable coverage. Prior to the ACA, the uninsured reported difficulty gaining insurance coverage due to the high cost of coverage and limits on Medicaid eligibility for adults. Eight in ten uninsured adults report no access to employer insurance, and the majority of people who had access to coverage through an employer report that the coverage offered to them is not affordable. One in three uninsured adults (31%) reported trying to sign up for Medicaid in the past five years, and the majority of them were unsuccessful because they were told they were ineligible. And one in five uninsured adults (22%) reported trying to obtain non-group coverage in the past five years, with most not purchasing a plan because the policy they were offered was too expensive.
Health insurance coverage is not always stable. For most insured adults, coverage is continuous throughout the year and over time, but a sizable number have a gap or change in coverage. When accounting for both insured people with a gap in their coverage and uninsured people who recently lost coverage, the survey indicates that nearly 18 million adults lose or gain coverage over the course of a year. In addition to those who lose or gain coverage over the course of a year, 17 million continuously insured adults have a change in their health insurance plan. The most common reasons for a change in coverage appear to be related to employment. Last, a small number of insured adults report challenges in either renewing or keeping their coverage, another indication of instability in coverage throughout the year.
Informing ACA Implementation: Many of the barriers to coverage that the uninsured report facing in the past are addressed by the ACA’s provisions to expand Medicaid and provide premium tax credits for Marketplace coverage. However, some uninsured adults may continue to face barriers to coverage, as not all employers are required to offer coverage and not all states are expanding their Medicaid programs. People targeted by the ACA have varying levels of experience with the insurance system. A large share of uninsured adults has been outside the insurance system for quite some time, and the long-term uninsured may require targeted outreach and education efforts to link them to the health care system and help them navigate their new health insurance. In addition, people who have attempted to obtain coverage in the past may be unaware that rules and costs have changed under the ACA; outreach and education will be needed to inform people that eligibility rules have changed and that financial assistance is available to offset the cost of coverage.
Survey findings on changes in insurance coverage over the course of the year indicate that, even after implementation, adults are likely to experience coverage changes due to job changes or income fluctuation. While there has been much focus on the early effort to enroll currently uninsured people in coverage, these findings demonstrate that implementation is not a “one shot” effort that will be done once people are enrolled in the early part of 2014 but rather will require a continuous effort to enroll and keep people in coverage.
II. What to Look for in Enrolling in New Coverage
While many currently uninsured adults have limited experience in signing up for and using health coverage, the past successes and challenges of insured low-and moderate income adults can inform the experiences of those seeking coverage under the ACA. Key survey findings related to plan enrollment and plan choice are:
Most adults did not report problems in applying for and enrolling in Medicaid coverage prior to the ACA, but some encountered difficulties in the process of gaining public coverage in the past. Adults who currently have Medicaid or who have attempted to enroll in the past five years report little difficulty in taking steps to enroll in Medicaid, with half saying the entire process was very or somewhat easy. However, the rest found at least one aspect of the process – finding out how to apply, filling out the application, assembling the required paperwork, or submitting the application – to be somewhat or very difficult.
In choosing their Medicaid or private insurance plan, adults do not always prioritize costs, and many find some aspect of the plan choice process to be a challenge. Adults choose health plans for various reasons, with 32% reporting that they chose their plan because it covered a wide range of benefits or a specific benefit that they need, 29% because their costs would be low, and 22% because the plan had a broad selection of providers or included their doctor. In choosing a plan, people may face challenges in comparing costs, services, and provider networks, as these factors typically varied greatly across plans in the past. In general, insured adults report that they did not have difficulty in comparing their plan choices, but 36% found some aspect of plan choice—comparing services, comparing costs, and comparing providers— to be difficult.
Overall, insured adults report satisfaction with their current coverage but also report gaps in covered services and problems when using their coverage. Most (85%) insured adults rate their pre-ACA coverage as excellent or good, but they also report gaps in services that are covered by their current insurance. One in six (17%) insured adults report needing a service that is not covered by their current plan, typically ancillary services such as dental, vision care, and chiropractor services. Many insured adults reported experiencing a problem with their current insurance plan covering a specific benefit, either because they were denied coverage for a service they thought was covered (25%) or their out-of-pocket costs for a service were higher than they expected (37%).
Informing ACA Implementation. The ACA includes provisions to simplify the Medicaid application and enrollment process for coverage in all states, regardless of whether they are expanding their Medicaid program. The ACA also requires plans in the Marketplace to provide detailed, standardized plan information for people to compare coverage options. Uninsured adults applying for coverage after these new processes are implemented should encounter fewer challenges in navigating enrollment and plan choice than applicants have in the past. However, in evaluating the success of plan enrollment, it is important to bear in mind historical challenges people have faced in comparing and selecting insurance coverage. It is also important to remember that people place utility on a range of factors related to insurance, including scope of services and provider networks. Assessments of whether people are choosing the optimal plan for themselves and their family will need to consider the multiple priorities that people balance in plan selection. Last, while the ACA aims to ensure coverage of at least a basic set of essential health benefits (EHB), many of the ancillary services that people report needing coverage for—such as dental services—are not included in the EHB. Newly-insured people may be surprised to learn that some ancillary services are not included in their plan, and education efforts will be needed to make sure people understand their coverage.
III. Gaining Coverage, Getting Care
As uninsured adults gain coverage, there are likely to be changes in how often they seek care, what type of care they seek, and where they seek care. By comparing their current interactions with the health care system to their insured counterparts, the survey can provide insight into likely changes. Key findings in this area include:
A large segment of the uninsured has little or no connection to the health care system. Most uninsured adults report few connections to the health care system. Only 51% of uninsured adults report that they have a usual source of care, or a place to go when sick or need advice about their health, and only 33% of uninsured adults have a regular doctor, half the rate of insured adults. This lack of a connection to the health care system leads many uninsured adults to go without care. More than four in ten uninsured adults (41%) reported no health care visits in the past year, compared to 10% of Medicaid beneficiaries and 13% of adults with employer coverage.
A substantial share of the uninsured has health needs, many of which are unmet or only met with difficulty. Despite being as likely as those with private insurance to report having an ongoing health condition, uninsured adults are less likely than their insured counterparts to receive care. When uninsured individuals do receive care, they sometimes receive free or reduced-cost care, though the majority who use services do not. Almost half (49%) of the uninsured report needing but postponing care compared to 28% of adults with employer coverage, 36% with nongroup coverage, and 41% of Medicaid beneficiaries. The most common reason for postponing care among the uninsured is cost, as the uninsured must pay the full cost of their care.
Many of the uninsured report limited options for receiving health care when they need it. Uninsured adults are less likely than their insured counterparts to receive care in a private physician office when they do get care. Uninsured adults are more likely than other adults to report that they have limited options for their usual source of care, with 18% of uninsured people reporting that they chose their usual source of care because it is the only option available to them, compared to 10% of adults with Medicaid and 4% with employer coverage.
Informing ACA Implementation: The survey findings reinforce conclusions based on prior research: having health insurance affects the way that people interact with the health care system, and people without insurance have poorer access to services than those with coverage. Thus, gaining coverage is likely to connect many currently uninsured adults to the health care system. Given the health profile of the currently uninsured population, there is likely to be some pent-up demand for health care services among the newly-covered. However, outreach may be needed to link the newly-insured to a regular provider and help them establish a pattern of regular preventive care. In particular, some individuals who have relied on emergency rooms or urgent care centers as their usual source of care may require help in establishing new patterns of care and navigating the primary care system. While the uninsured may have more options for where to receive their care once they obtain coverage under the ACA, clinics and hospitals that already see a large share of uninsured adults may play an important role in serving this population once they gain insurance. Last, while coverage gains may reduce cost barriers to coverage, it will be important to monitor whether other barriers to care among the low-income population—such as transportation or wait times for appointments—continue to pose a challenge for access.
IV. Health Coverage and Financial Security
In addition to facilitating access to health care, health insurance serves primarily to protect people from high, unexpected medical costs. However, for low-income families, health costs can still be a burden, even if they have insurance. Understanding these issues can help policymakers monitor ongoing financial barriers to health services.
Health care costs pose a challenge for low- and moderate-income families, even if they have insurance coverage. Even among those with insurance, health care costs can be a burden, particularly for low- and moderate-income adults. About a third low- and moderate-income adults covered by employer coverage report that their share is somewhat hard or very hard for them to afford, and 76% of the low-income and 58% of moderate income adults with nongroup coverage report such difficulty. Health care costs translate to medical debt for many l0w-income adults, and these medical bills can cause serious financial strain. Among those who reported a problem with medical bills, the vast majority in every coverage and income category reported that medical bills caused them to either use up all or most of their savings, have difficulty paying for necessities, borrow money, or be contacted by a collection agency. Notable shares of low-income insured adults also report that they lack confidence in their ability to afford health care, given their current finances and health insurance situation. Of particular note is the finding that about half of adults with nongroup coverage do not feel confident that they could afford costs related to a major illness given their coverage and financial situation.
Low-income families face fragile financial circumstances. Low- and moderate-income adults across coverage groups report not being financially secure. However, adults who are low-income and uninsured or covered by Medicaid are particularly vulnerable to financial insecurity even outside of health care. General financial insecurity translates to concrete financial difficulties in making ends meet. Uninsured adults and those on Medicaid are more likely than privately-insured adults to have difficulty paying for other necessities such as food, housing, or utilities, with 58% reporting such difficulty compared to 19% of those with employer coverage and a quarter of those with nongroup coverage. While low-income adults across the coverage spectrum report high rates of difficulty paying for necessities, those with employer coverage report the lowest rates in this income group. These individuals may have the stronger or more stable ties to employment than their counterparts with other or no insurance coverage.
Informing ACA Implementation: Both insured and uninsured low-income adults struggle with medical bills and debt, and coverage expansions, assistance with premium costs, and limits on out-of-pocket costs under the ACA have the potential to ameliorate the financial issues associated with the cost of health care. However, given survey findings that many low-income insured people continue to face financial challenges related to health care, it will be important to track whether there are ongoing financial barriers as people enroll in coverage and seek care. While insurance coverage can provide financial protection in the event of illness or injury, it is not curative of all of the financial burdens faced by low-income families. Given their overall situation, health insurance alone may not lift low-income people out of poverty, and many low-income adults may continue to face financial challenges even after gaining coverage.
V. Low- and Moderate-income Uninsured Adults’ Readiness for the ACA
As outreach and enrollment efforts are underway, information on low- and moderate-income adults’ access to tools for signing up and connections to outreach avenues can be helpful in addressing barriers. Key survey findings in this area include:
A majority of uninsured adults who are income eligible for coverage expansions reported knowing little or nothing about Medicaid and Marketplace programs prior to the start of open enrollment. Despite ongoing media attention to the ACA, seven in ten uninsured adults with incomes in the Medicaid target range (<138% FPL) said they knew nothing at all or only a little about their state’s Medicaid program, and eight in ten uninsured adults in the income range for Marketplace subsidies (139-400% FPL) reported that they knew nothing at all or only a little about the Marketplaces. More recent polling data indicates that lack of knowledge remains high despite recent media attention to the ACA.
While most uninsured adults have the necessary tools for enrolling in coverage, some will experience additional logistical issues in signing up. Under the ACA, internet access is an important tool in accessing coverage. While the majority of uninsured adults have access to the internet either at home or outside the home, 19% of low-income (<138% FPL) and 14% of moderate income (139-400% FPL) uninsured adults report that they do not have internet access readily available. For Marketplace coverage, people will require a means to pay their premiums on a regular basis. While plans must accept various forms of payment, direct withdrawal from a checking account is a simple and reliable way to ensure that premiums are paid on time. However, nearly a quarter (23%) of uninsured adults in the income range for Marketplace subsidies report that they do not have a checking or savings account.
Many uninsured adults could be reached through targeted outreach avenues. Among uninsured adults with incomes in the range for Medicaid eligibility (<138% FPL), over six in ten (62%) report that they or someone in their immediate family receives either SNAP, cash assistance, disability payments, or Medicaid or CHIP, making “fast track” enrollment efforts through using information collected by other agencies a promising avenue for outreach. For those without a connection to social services agencies, outreach through providers may be a promising approach, as about one in five low- or moderate-income uninsured adults report that they use a clinic or health center as their usual source of care. While fewer report using a hospital outpatient department for regular care, hospitals reach many uninsured adults through periodic visits.
Informing ACA Implementation: Both survey findings and more recent polling data indicate that there is a great need for education of new coverage options among people targeted for expansions. Even once eligible individuals learn about coverage options, they may face logistical challenges in signing up. People without internet access via a computer may be able to enroll through other more traditional avenues such as over the phone or in person at county offices or providers, but efforts may be needed to inform people of these other application routes, and some using them may experience slower enrollment process than they would if they applied online. Finally, “fast track” enrollment efforts are a promising approach to facilitating enrollment, but broader efforts will also be needed to reach the eligible uninsured population.
Report: Introduction
In January 2014, the major coverage provisions of the 2010 Affordable Care Act (ACA) went into full effect. These provisions include the creation of new Health Insurance Marketplaces where low and moderate income families can receive premium tax credits to purchase coverage and, in states that opted to expand their Medicaid programs, the expansion of Medicaid eligibility to almost all adults with incomes at or below 138% of the federal poverty level (FPL) ($15,856 for an individual or $26,951 for family of three in 2013). With these coverage provisions, ACA has the potential to reach many of the 47 million Americans who lack insurance coverage, as well as millions of insured people who face financial strain or coverage limits related to health care.
Though ACA implementation is underway and people are already enrolling in coverage, policymakers continue to need information to inform coverage expansions. Reports of difficulties in enrolling in coverage, continued confusion and lack of information about the law point to challenges in the early stages of implementation. In the future, data will be needed to assess whether and how the ACA is helping low- and moderate-income families gain affordable coverage, access needed care, and obtain financial security. Detailed data on the population targeted for coverage expansions’ experience with health coverage, current patterns of care, and family situation can help policymakers target early efforts, provide insight into some of the challenges that are arising in the first months of new coverage, and evaluate the ACA’s longer-term affects.
To that end, the Kaiser Family Foundation has launched a new series of comprehensive surveys of the low and moderate income population. This report, based on the baseline 2013 Kaiser Survey of Low-Income Americans and the ACA, provides a snapshot of health insurance coverage, health care use and barriers to care, and financial security among insured and uninsured adults across the income spectrum at the starting line of ACA implementation. It also provides a baseline for future assessment of the impact of the ACA on health coverage, access, and financial security of low- and moderate-income individuals nationwide. Future reports using this baseline survey will provide additional in-depth analysis of issues in ACA implementation, such as differences between states expanding their Medicaid programs and those not expanding; in-depth analysis of issues in affordability of health care and family finances; Medicaid’s role in facilitating access to care; and challenges facing part-time workers, among others. Forthcoming separate state reports focusing on California, Missouri, and Texas will analyze these issues in the context of state-specific efforts to implement the law.
This report examines how findings from the baseline survey can help policymakers understand and address early challenges in implementing health reform. Throughout sections that focus on findings related to i) patterns of insurance coverage, ii) the process of selecting and enrolling in health coverage, iii) interactions with the health care system, iv) financial security, and v) readiness for ACA coverage expansions, the report highlights findings that can inform outreach and enrollment workers, health plans, and providers and health systems. A detailed explanation of the methods underlying the survey and analysis is available in the Methods section of the report.
Report: Background: The Challenge Of Gaining Insurance Coverage Prior To The Aca
Prior to implementation of the ACA, over 47 million Americans—nearly 18% of the population—were without health insurance coverage. Because publicly-financed coverage has been expanded to most low-income children and Medicare covers nearly all of the elderly, the vast majority of uninsured people are nonelderly adults.2 Not having health insurance has well-documented adverse effects on people’s use of health care, health status, and mortality, as the uninsured are more likely to delay or forgo needed care leading to more severe health problems.3 Lack of insurance coverage also has implications for people’s personal finances, providers’ revenue streams, and system-wide financing.4 ,5 ,6 The coverage provisions in the 2010 Affordable Care Act (ACA) sought to address these issues by making coverage more available and affordable, particularly for people with low or moderate incomes.
The main barrier that people have faced in obtaining health insurance coverage is cost: health coverage is expensive, and few people can afford to buy it on their own. While most Americans traditionally obtain health insurance coverage as a fringe benefit through an employer, not all workers are offered employer coverage, and not all adults are working. Medicaid and the Children’s Health Insurance Program (CHIP) cover many low-income children, but eligibility for parents and adults without dependent children is limited, leaving many adults without affordable coverage.
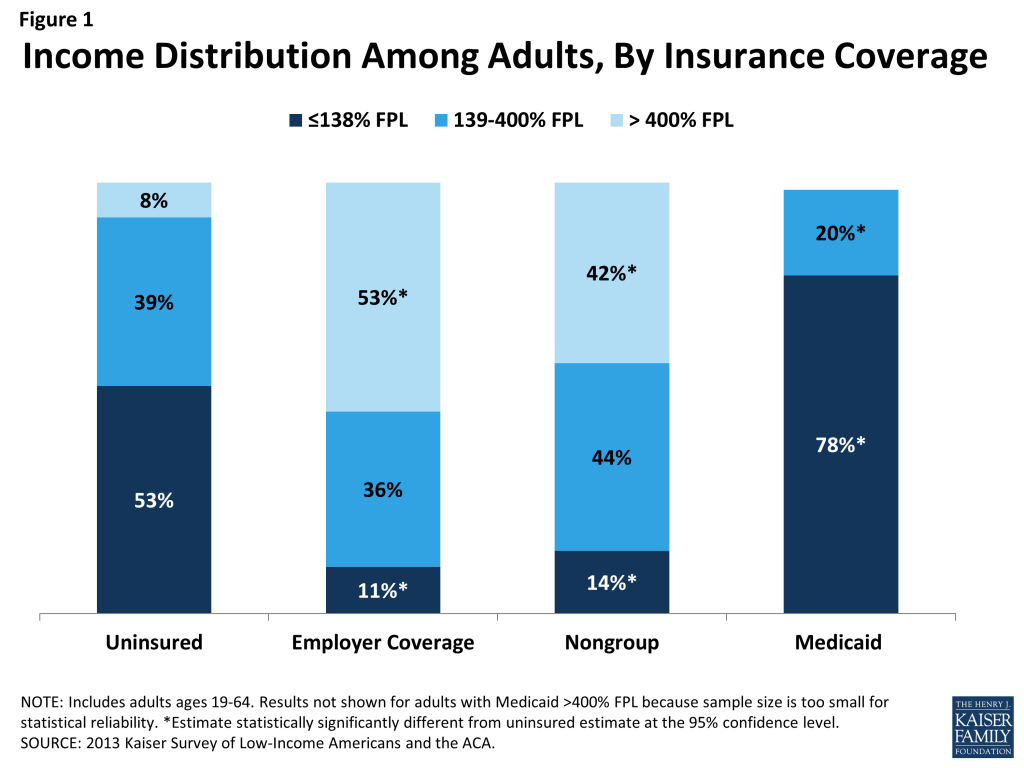
These barriers to coverage are reflected in the characteristics of the uninsured population. Compared to those with private coverage, uninsured adults are more likely to be low-income (Figure 1). A majority of uninsured adults (53%) are low-income, or have incomes at or below 138% FPL, in contrast to 11% of adults with employer coverage and 14% of adults with nongroup. Adults with Medicaid are the most likely of any coverage group to be low-income, reflecting the fact that prior to the ACA, adult income eligibility limits were generally very low (often below half the poverty level). Less than one in ten uninsured adults have incomes greater than 400% FPL, compared to over half of adults with employer coverage (53%) and 42% of adults with nongroup coverage.
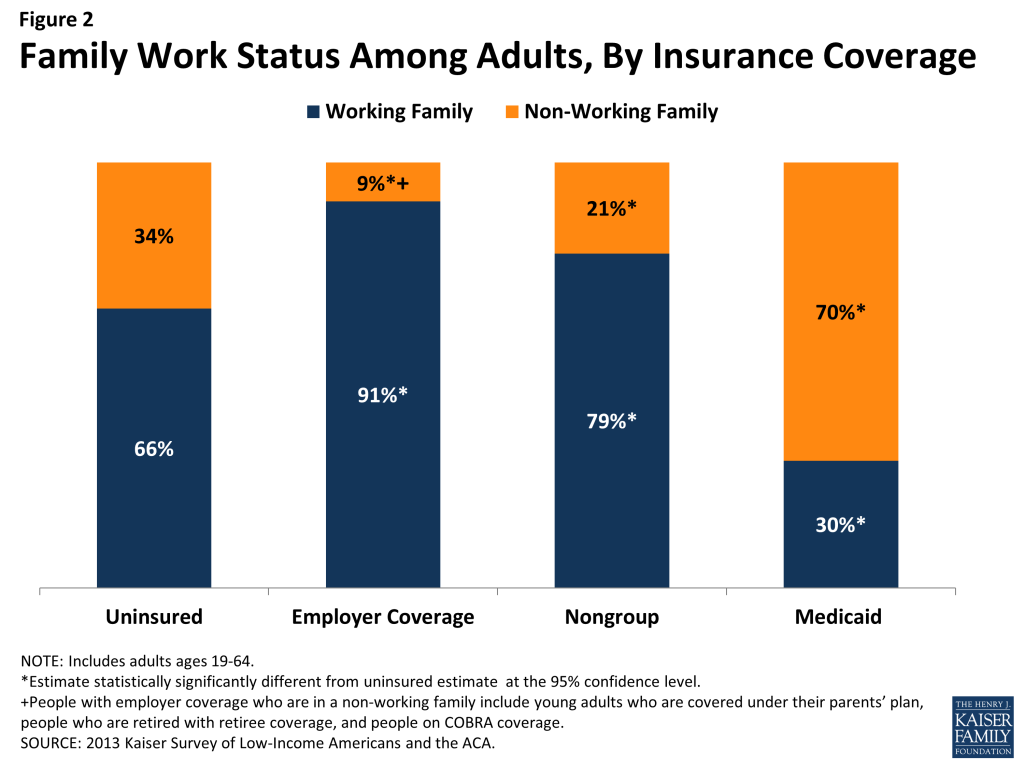
Corresponding to their lower incomes, uninsured adults are less likely than privately insured adults to be in a working family; however, the majority of uninsured adults are in a family with either a full- or part-time worker. About two-thirds (66%) of uninsured adults are in a working family (that is, either they, or their spouse if they are married, report working either full or part-time), in contrast to 91% of adults with employer coverage and 79% of adults with nongroup coverage (Figure 2). Adults with Medicaid are the least likely to be in a working family (30%), again reflecting very low income eligibility limits for adults prior to the ACA.
Uninsured adults also differ from insured adults with regards to other demographic characteristics. Uninsured adults are likely to be younger than insured adults, as younger adults have lower incomes and looser ties to employment than older adults. Two-thirds (67%) of uninsured adults are ages 19-44 as compared to 56% of adults with employer coverage or Medicaid and 41% of adults with nongroup coverage (Appendix Table A1).
There also are significant racial and ethnic differences in health coverage among nonelderly adults. For example, uninsured adults are more likely to be Hispanic – 30% of uninsured adults are Hispanic – than adults with employer coverage (11%), nongroup coverage (9%), or Medicaid (18%). About half (49%) of uninsured adults are White, non-Hispanic, compared to 75% of adults with nongroup coverage, and 70% of adults with employer sponsored insurance. Racial and ethnic differences in coverage rates, which are reflective of differences in income and work status by race/ethnicity, have implications for efforts to address health care disparities. Also, about one in five uninsured adults is a noncitizen (19%), compared to less than 7% of adults with Medicaid or employer coverage. Citizenship status may leave many uninsured adults ineligible for Medicaid, increasing the likelihood they will remain uninsured.
Among the primary goals of the ACA were filling in gaps in the availability of public coverage by expanding Medicaid eligibility for low-income adults and making private coverage more affordable for moderate-income adults who lack access to coverage through a job. The ACA also aims to simplify and coordinate eligibility and enrollment across programs, ensure coverage for a basic package of health benefits, and facilitate innovations in service delivery. As policymakers embark on early implementation of the law, it is important to remember who the ACA aims to help and how their characteristics may inform efforts to reach them.
Report: I. Patterns Of Coverage And The Need For Assistance
Coverage Dynamics among the Insured and Uninsured
Health insurance coverage is dynamic, and every year millions of Americans gain, lose, or change their health coverage. However, for most uninsured adults, lack of coverage is a long-term issue that spans many years. Many uninsured adults report trying to obtain coverage in the past but were unsuccessful due to barriers such as ineligibility for public coverage or high costs of private coverage. Under the ACA, millions of uninsured are projected to gain coverage as those barriers are removed, but some may continue to experience gaps or changes in coverage.
For most currently uninsured adults, lack of coverage is a long-term issue.
While some people lack health insurance coverage during short periods of unemployment or job transitions, for many uninsured adults, lack of coverage is a chronic problem. The survey shows that a large share of uninsured adults have been without insurance for a very long period of time: Almost half (47%) report being uninsured for 5 years or more, and 18% report that they have never had coverage in their lifetime (Figure 3 and Appendix Table A2).
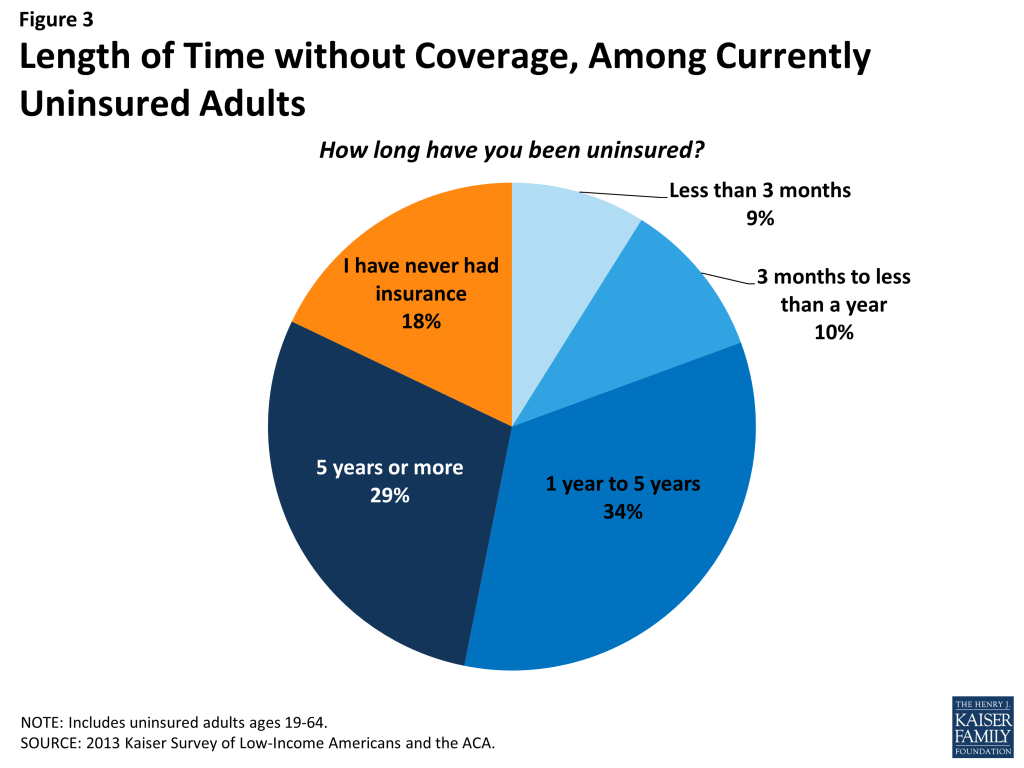
Perhaps not surprisingly, adults who have been without insurance coverage for at least five years are, on average, older than those who have been uninsured for shorter periods of time. Nearly two-thirds (63%) of adults who have been uninsured for five years or more are ages 35-64, compared to just 47% of adults who have been uninsured for less than a year (data not shown). However, on other characteristics, such as race, gender, citizenship, income, and health status, long-term and short-term uninsured adults resemble each other.
“I don’t know how to go about getting insurance.”
Alexa (TX), long-term uninsured
It is important for policymakers implementing coverage expansions to be aware that people targeted by the ACA have varying levels of experience with the insurance system. While some only recently lost coverage, a large share of uninsured adults has been outside the insurance system for quite some time. The long-term uninsured may require targeted outreach and education efforts to link them to the health care system and help them navigate their new health insurance.
Many uninsured adults report trying to obtain insurance coverage in the past, but most did not have access to affordable coverage.
The uninsured report a desire to obtain coverage, but prior to implementation of the ACA, options for coverage—particularly for the low-income—were limited. The vast majority of uninsured adults do not have access to employer coverage. Eight in ten uninsured adults report no access to employer insurance, either because no one in their family is working for an employer, their or their spouse’s employer does not offer coverage, or they are ineligible for that coverage (Table 1). For example, 47% of uninsured adults are in a family without an employer, meaning both they and their spouse (if married) are either not working or are working but are self-employed. A quarter of uninsured adults are in a family that has an employer who does not offer coverage to any workers, and 10% are in a family that works for an employer who offers coverage but they are ineligible for that coverage. Most are ineligible because they work part-time or are in a waiting period. Less than one in five (18%) uninsured adults does have access to coverage through an employer, but the majority of those people report that the coverage offered to them is not affordable.
| Table 1: Access to Employer Health Coverage Among Uninsured Adults | |||||
| All Uninsured | Uninsured by Income | ||||
| <138% FPL | 139-400% FPL | >400% FPL | |||
| % | % | % | % | ||
| No Access to ESI | 82% | 86% | 78%^ | 78% | |
| No one in family has an employer* | 47% | 54% | 37%^ | 51% | |
| Firm doesn’t offer coverage | 25% | 25% | 30% | — | |
| Not eligible for coverage | 10% | 7% | 12% | — | |
| Access to ESI | 18% | 14% | 22%^ | — | |
| Cannot afford premium | 11% | 8% | 12% | — | |
| Don’t think need coverage | — | — | — | — | |
| Some other reason | 6% | 5% | 9% | — | |
| Note: Don’t Know and Refused responses are not shown, they account for less than 3% of the uninsured population.”–“: Estimates with relative standard errors greater than 30% or cell sizes below 50 are not provided.NA: Not applicable* Individuals who are self-employed without other employment are treated as not having an employer.^ Estimate statistically significantly different from <138% FPL estimate at the 95% confidence level.SOURCE: 2013 Kaiser Survey of Low-Income Americans and the ACA. | |||||
Prior to the ACA, Medicaid eligibility for adults was very limited in most states. Eligibility generally was limited to parents with very low incomes (often below about half the federal poverty level), and in all but a handful of states, adults without dependent children were ineligible for Medicaid regardless of their income.7 Further, application processes were sometimes very complex, requiring face-to-face interviews, assessments of assets, or paper documentation.8 Eligibility and application processes posed barriers for many low-income adults seeking Medicaid coverage.
One in three uninsured adults (31%) reported trying to sign up for Medicaid in the past five years (Figure 4). Low-income uninsured adults (those with family income up to 138% FPL) were more likely than those with moderate incomes to report trying to sign up for Medicaid (38%) (see Appendix Table A2). The majority of adults who tried to sign up for Medicaid (22% of the uninsured) were unsuccessful, and among those, most (19% of the uninsured) were unable to sign up because they were told they were ineligible. Notably, a quarter of uninsured adults in the income range for Medicaid expansion under the ACA (<138% FPL) have tried to sign up for Medicaid in the past but were told they were ineligible.
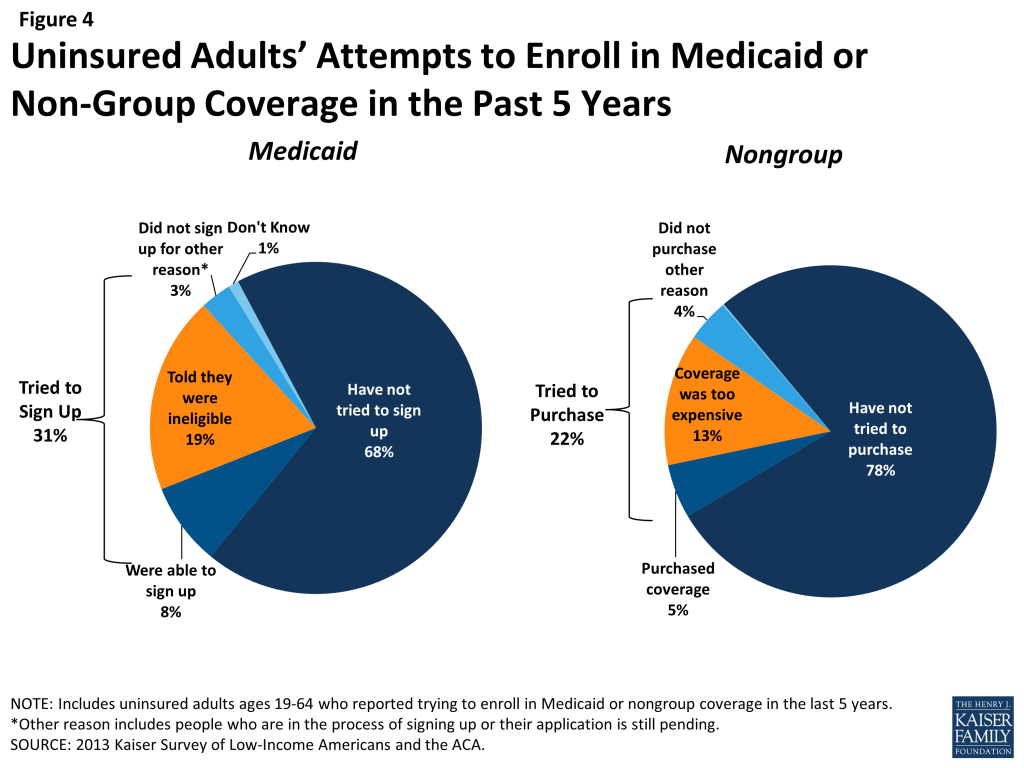
Prior to the ACA, there were also barriers to obtaining coverage on the non-group, or individual market. This type of coverage was not guaranteed in all states, and insurance companies could often charge higher premiums for sicker individuals or place limits on coverage for pre-existing conditions, making coverage unaffordable for many uninsured adults. The uninsured also report trying to obtain non-group coverage prior to the ACA. One in five uninsured adults (22%) reported trying to obtain non-group coverage in the past five years. Most of these adults (13% of the uninsured) did not purchase a plan because the policy they were offered was too expensive (Figure 4).
“We are very lucky that we have not had any catastrophic incidents, because we could not afford the catastrophic insurance premiums [for nongroup coverage] that we were quoted.”
Jose (FL), on trying to buy coverage on his own before the ACA
Many of the barriers to coverage that the uninsured report facing in the past are addressed by the ACA. Large employers (>50 workers) face penalties if they do not offer affordable coverage to their workers, and in states that chose to expand Medicaid, eligibility for Medicaid includes almost all adults with incomes at or below 138% FPL. Further, millions of uninsured families are now able to purchase coverage in the Marketplaces and receive premium tax credits to reduce the cost. Insurers are no longer able to deny coverage based on health status and are limited in what they charge people based on age, location, and tobacco use status. However, some uninsured adults may continue to face barriers to coverage. Employers are not required to offer coverage to part-time employees, and only large businesses will be subject to a fine for not offering affordable coverage to full-time employees, beginning in 2015. In states that did not expand Medicaid, eligibility remains limited, leaving many ineligible for Medicaid and without an affordable coverage option. Last, people who have attempted to obtain coverage in the past may be unaware that rules and costs have changed under the ACA. Outreach and education will be needed to inform people that eligibility rules have changed and that financial assistance is available to offset the cost of coverage.
Health insurance coverage is not always stable.
For most insured adults, coverage is continuous throughout the year and over time, but a sizable number experience a gap or change in coverage. When accounting for both insured people with a gap in their coverage and uninsured people who recently lost coverage, the survey indicates that nearly 18 million adults lose or gain coverage over the course of a year.
Among adults who were insured at the time of the survey, 7% reported being uninsured at some point in the past year (see Figure 5 and Table 2), and those who had a gap in coverage were uninsured for nearly half the year (5.7 months) on average (data not shown). Low-income insured adults (those with family income up to 138% FPL) are particularly vulnerable to gaps in coverage, with 13% reporting a coverage gap in the past 12 months compared to 8% of those with incomes between 139 and 400% FPL (Figure 5).
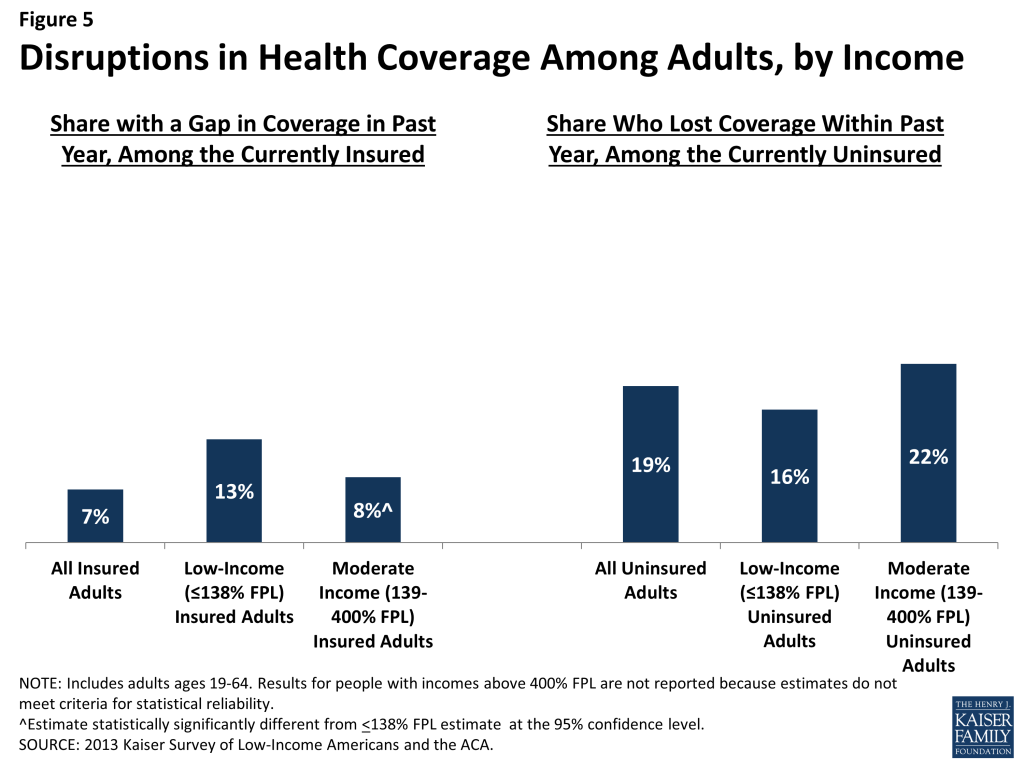
Further, some currently uninsured adults had coverage at some point within the past year. Among uninsured adults, nearly one in five (19%) report having lost coverage within the last year. Among both those with a gap in coverage or who recently lost coverage, the majority report that they most recently had employer coverage (data not shown).
| Table 2: Coverage Dynamics among Insured and Uninsured Adults, by Income and Current Coverage | |||||||||
| All | By Income | By Current Coverage | |||||||
| <138% FPL | 139-400% FPL | >400% FPL | Employer | Nongroup | Medicaid | ||||
| % | % | % | % | % | % | % | |||
| Insured Adults | 100% | 100% | 100% | 100% | 100% | 100% | 100% | ||
| Gap in Coverage in Past Year | 7% | 13% | 8%^ | — | 5%* | — | 13% | ||
| Changed Coverage During Year | 12% | 7% | 11%^ | 16%^ | 14%* | — | 3% | ||
| Same Coverage for Full Year | 81% | 79% | 81% | 82% | 80% | 84% | 81% | ||
| Uninsured Adults | 100% | 100% | 100% | 100% | 100% | 100% | 100% | ||
| Uninsured Full Year | 80% | 83% | 78% | 75% | NA | NA | NA | ||
| Lost Coverage Within Past Year | 19% | 16% | 22% | — | NA | NA | NA | ||
| Notes: Don’t Know and Refused responses not shown. Excludes people covered by other sources, such as Medicare, VA/CHAMPUS, or other state programs.”–“: Estimates with relative standard errors greater than 30% or cell sizes below 50 are not provided.NA: Not applicable.^ Estimate statistically significantly different from <138% FPL estimate at the 95% confidence level.* Estimate statistically significantly different from Medicaid estimate at the 95% confidence level. SOURCE: 2013 Kaiser Survey of Low-Income Americans and the ACA. | |||||||||
In addition to those who lose or gain coverage over the course of a year, millions of adults who have coverage throughout the entire year have a change in their health insurance plan. Among adults with insurance coverage, 12% (17 million people) had coverage for the entire year but report that they had a change in their coverage (Table 2). Coverage changes may be due to a number of different factors including changes in employment, changes in eligibility for public programs, or simply a change in insurance carrier. The most common reasons for a change in coverage appear to be related to employment, as most people with a coverage change report changing from an employer plan to another employer plan.
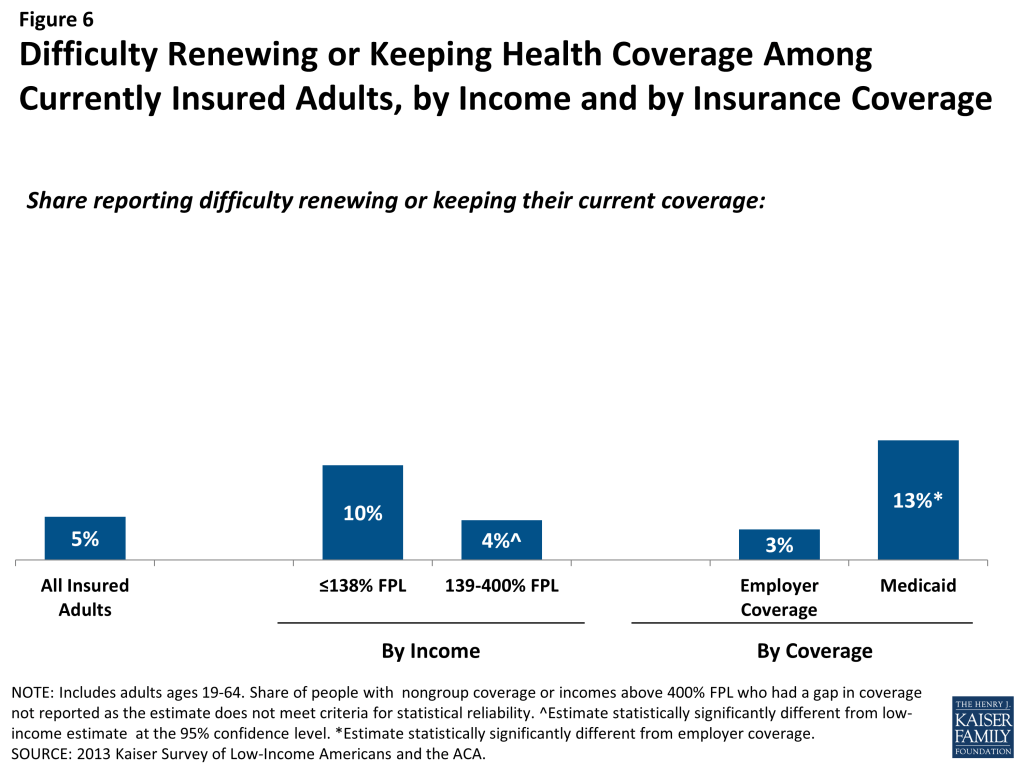
Last, a small number of insured adults report challenges in either renewing or keeping their coverage, another indication of instability in coverage throughout the year. Reflecting eligibility rules and sometimes burdensome renewal processes, adults with Medicaid are the most likely to report a challenge (13%) compared to adults with employer coverage (Figure 6). Medicaid eligibility is closely tied to income, and adults’ income may fluctuate throughout the year; in addition, adults must renew their Medicaid coverage annually.
“So there for a while, for a few weeks, a month, 6 weeks, I’m without insurance. And then during that time, I cannot get medical care.”
Julie (MO), on having gaps in coverage
The survey findings on changes in insurance coverage over the course of the year have implications for implementation of health reform. Prior to the ACA, many people lost and gained employer coverage over the course of a year, due to changing economic conditions and the delicate relationship between employment and health insurance. Further, there was some churning in insurance coverage resulting from Medicaid income eligibility limits: as adults’ income fluctuates, they may gain or lose Medicaid eligibility. Adults also experienced gaps in Medicaid coverage due to frequent renewal requirements. Gaps in coverage can cause people to postpone or forgo health care or accumulate medical bills.9 By providing for insurance options across the income spectrum and facilitating coverage outside the employment-based system, the ACA may help adults have coverage continuously throughout the year. However, even after implementation, adults are likely to experience coverage changes due to job changes or income fluctuation. While there has been much focus on the early effort to enroll currently uninsured people in coverage, these findings demonstrate that people will continue to move around within the insurance system throughout the year. Thus, implementation is not a “one shot” effort that will be done once people are enrolled in the early part of 2014 but rather will require a continuous effort to enroll and keep people in coverage.
Report: Ii. What To Look For In Enrolling In New Coverage
How Low and Moderate Income Adults Sign Up For and View Their Coverage
While many currently uninsured adults have limited experience in signing up for and using health coverage, the past successes and challenges of insured low-and moderate income adults can inform the experiences of those seeking coverage under the ACA. A majority of insured adults do not experience problems in choosing, enrolling in, and using their coverage, and this pattern holds true for both people with Medicaid and private insurance. Still, based on the experience of their insured counterparts, the uninsured population targeted by the ACA coverage expansions is likely to encounter some barriers in the process of choosing and enrolling in coverage. While the ACA aims to make the process smoother, it is likely that some challenges inherent in the complexity of health coverage will require concerted efforts to address.
Most adults did not report problems in applying for and enrolling in Medicaid coverage prior to the ACA, but some encountered difficulties in the process of gaining public coverage in the past.
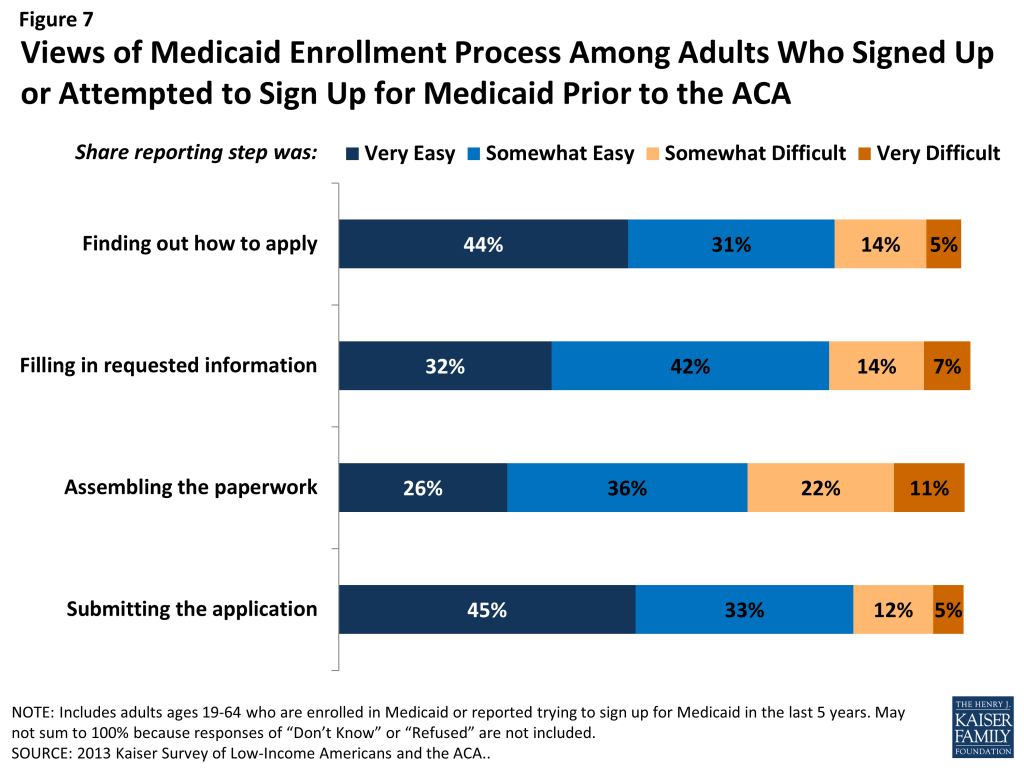
In comparison to the process for gaining coverage through an employer—which is typically facilitated by the firm or a representative and may require limited action on the part of the insured—applying for publicly-financed coverage typically requires proactive steps to gain coverage. Adults who currently have Medicaid or who have attempted to enroll in the past five years report little difficulty in taking steps to enroll in Medicaid. Half of adults (50%) who applied to Medicaid said the entire process was very or somewhat easy. However, the rest found at least one aspect of the process – finding out how to apply, filling out the application, assembling the required paperwork, or submitting the application – to be somewhat or very difficult. The most commonly reported difficulty was assembling the required paperwork, which a third (33%) of people who enrolled or applied said was a somewhat or very difficult (Figure 7 and Appendix Table A3).
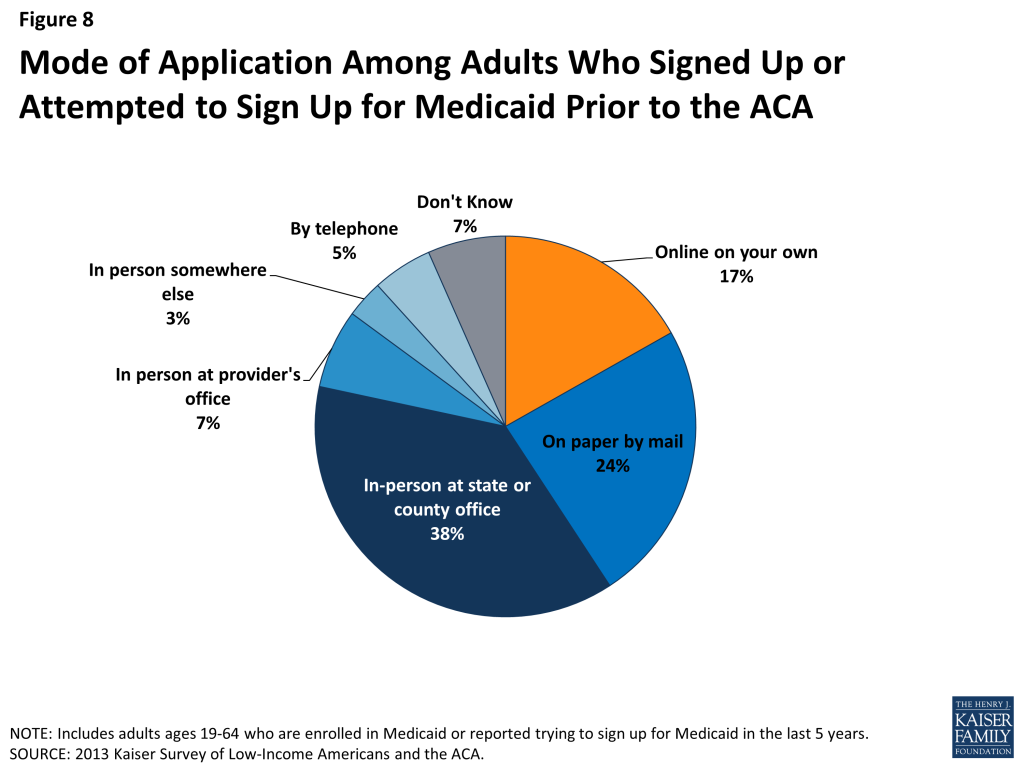
Historically, the Medicaid application process often required in-person visits to state or county welfare offices and completion of paper-based applications. In recent years, most states have made strides towards developing web-based applications to facilitate access to coverage and ease administrative burdens.10 However, a plurality (38%) of people who have applied to Medicaid in the past five years report that they did so through traditional routes—that is, in person at a state or county government office—and only 17% reported using an online application (Figure 8).
The ACA includes provisions to simplify the application and enrollment process for coverage in all states, regardless of whether they are expanding their Medicaid program. For example, the ACA establishes new requirements for simplifying the Medicaid application, coordinating enrollment across programs, and moving toward paperless verification of eligibility. These requirements include state adoption of a single streamlined application that is available online, by phone, and on paper and that screens for all health coverage options; electronic transfers of accounts between agencies to facilitate coordination across health coverage programs; and reliance on trusted sources of electronic data rather than requesting paper documentation to verify eligibility criteria.11 Further, under the ACA, assisters are available in each state to help individuals and families enroll in coverage. Thus, uninsured adults applying for coverage should encounter fewer challenges in navigating the enrollment process than applicants have in the past. However, in states that do not expand their Medicaid programs, few adults applying for coverage are likely to be eligible, given very low income eligibility limits in those states. As a result, the primary barrier of lack of eligibility will remain.
In choosing their Medicaid or private insurance plan, adults do not always prioritize costs, and many find some aspect of the plan choice process to be a challenge.
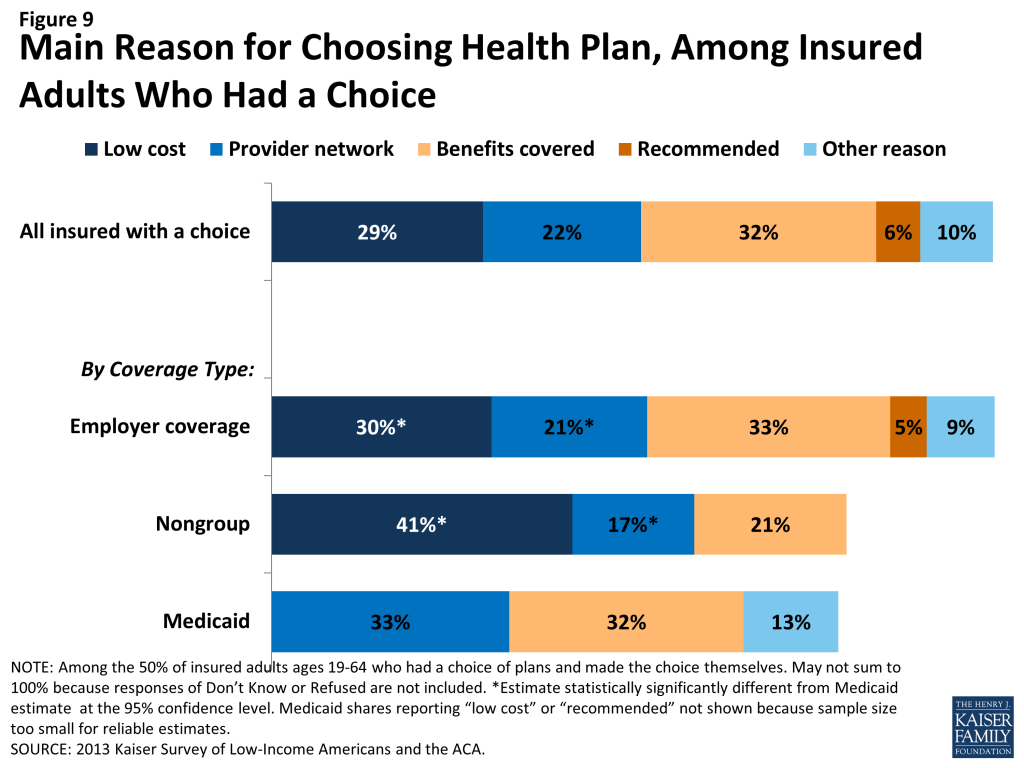
As people gain coverage, many will have the option to select an insurance plan. People may chose a particular plan for a variety of reasons, including low cost, choice of providers, recommendations from friends and family, or coverage of a particular benefit. Among the 50% of insured adults who chose a health plan,[endnote 101630-5] 32% reported that they chose their plan because it covered a wide range of benefits or a specific benefit that they need, while 29% reported that they chose their plan because their costs would be low and 22% because the plan had a broad selection of providers or included their doctor (Figure 9). This pattern differs by coverage type (see Appendix Table A4). For example, among Medicaid beneficiaries who had a plan choice, 33% reported provider network as the main reason for plan choice compared to 17% of adults with non-group coverage and 21% with employer coverage. These findings may reflect the fact that Medicaid benefits and costs are largely standardized across plans, while networks may vary.
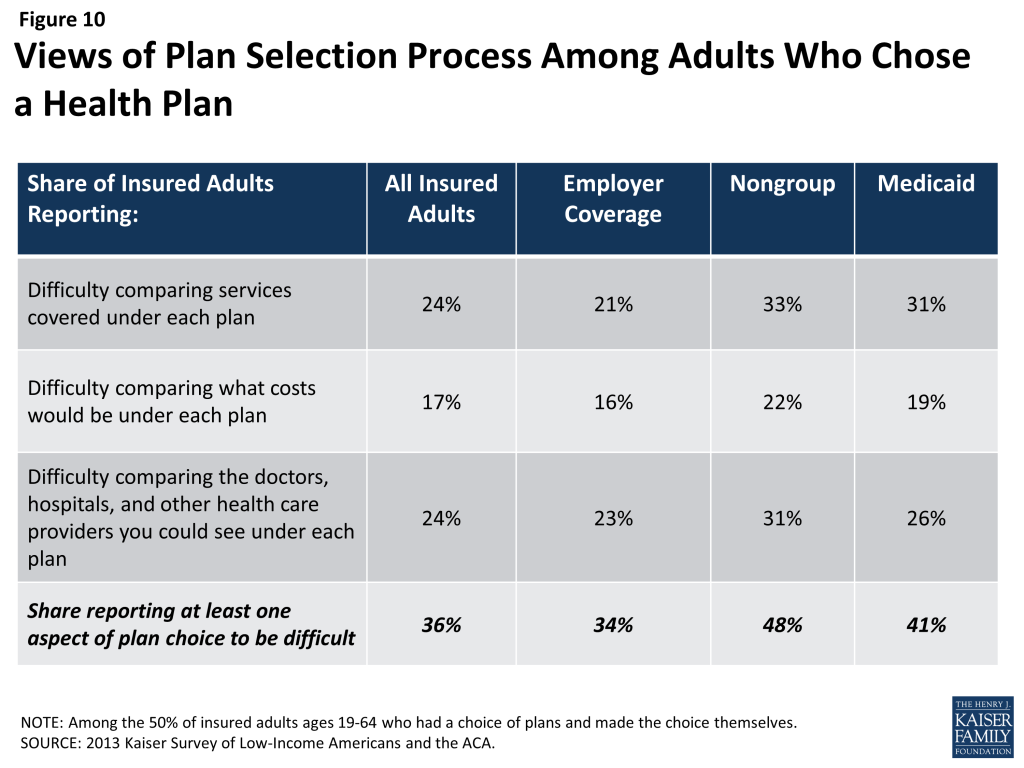
In choosing a plan, people may face challenges in comparing costs, services, and provider networks, as these factors typically varied greatly across plans in the past. In general, insured adults report that they did not have difficulty in comparing their plan choices, but 36% found some aspect of plan choice—comparing services, comparing costs, and comparing providers— to be difficult (Figure 10 and Appendix Table A4). Insured adults were least likely to report difficulty comparing costs across plans (17%). This finding is particularly interesting as most people reported choosing their plan based on covered services or benefits as compared to costs. As enrollment numbers for particular plans are released and policymakers begin to assess plan choice among new enrollees, these findings can inform evaluations of plan choice under the ACA. Contrary to expectations that people may opt for the lowest cost plan,12 survey findings indicate that people place value on a range of factors related to insurance, including scope of services and provider networks. Thus, assessments of whether people are choosing the optimal plan for themselves and their families will need to consider the multiple priorities that people balance in plan selection. Further, while ACA provisions requiring plans in the Marketplace to provide a standard set of benefits as well as more detailed information on what is included in plans could potentially increase the ease of plan selection, it is important to bear in mind historical challenges people have faced in comparing and selecting insurance coverage. In particular, low-income adults who receive Medicaid may require assistance in navigating plan choices, as provisions requiring comparable information on plans for coverage in the Marketplaces do not apply to Medicaid. However, states can make such information available to Medicaid enrollees as part of an effort to improve the plan selection process.
Overall, insured adults report satisfaction with their current coverage but also report gaps in covered services and problems when using their coverage.
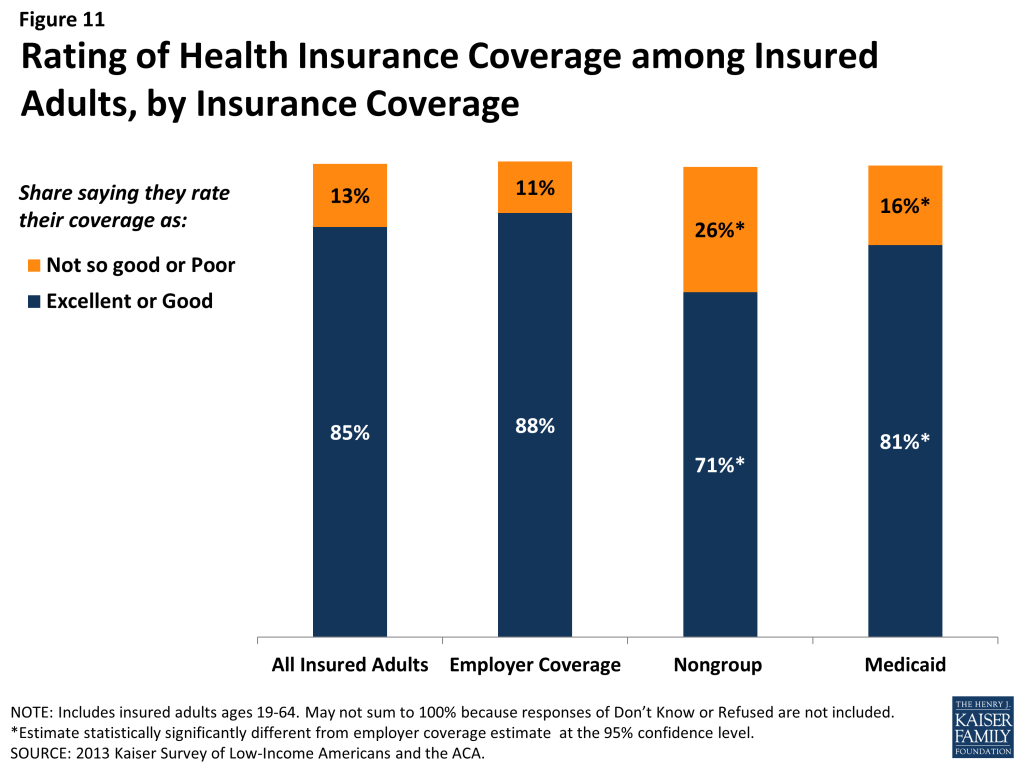
Most insured adults report high levels of satisfaction with their current coverage, but they also report gaps in services that are covered by their current insurance. Nearly 85% of insured adults rate their coverage as excellent or good, while 13% rate their coverage as not so good or poor (Figure 11). Adults with employer coverage gave their plans the highest ratings, 88% grading their plans as excellent or good. Adults with nongroup coverage or Medicaid were less likely to give their plans high ratings, but a majority (71% and 81%, respectively) still rates their plans as excellent or good.
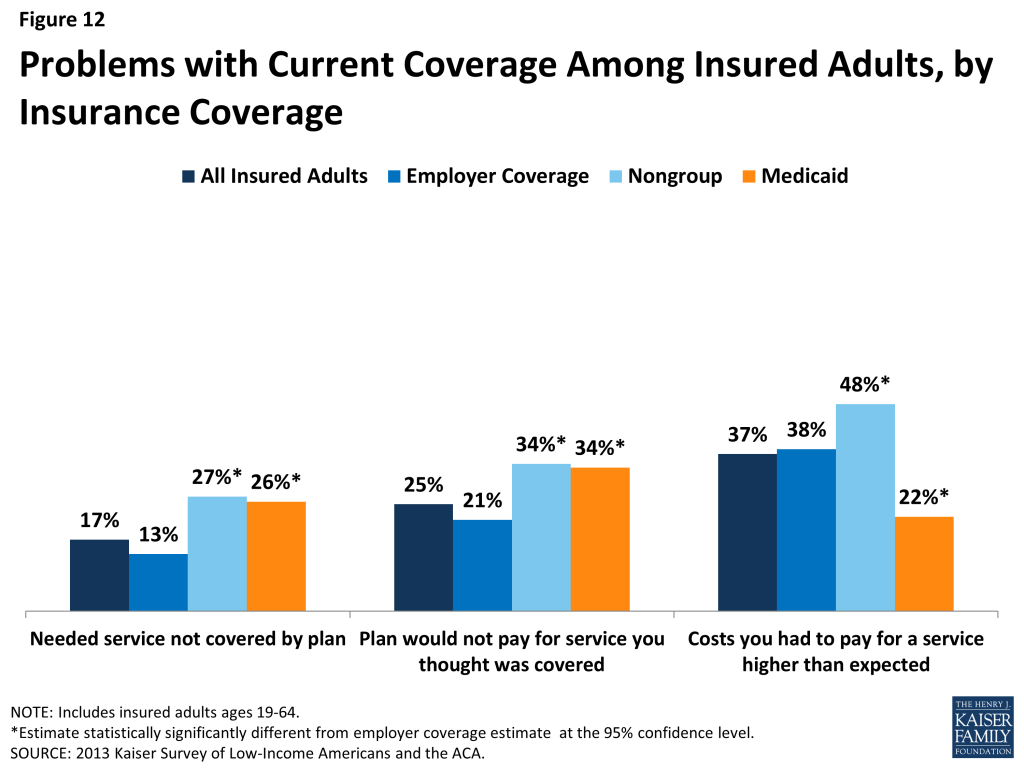
Despite the high ratings, notable shares of insured adults report a problem with their plan. Specifically, one in six (17%) insured adults report needing a service that is not covered by their current plan (Figure 12 and Appendix Table A5). People with Medicaid coverage (26%) or non-group coverage (27%) are more likely to report that their plan does not cover certain services compared to those with employer coverage (13%). The most frequently-reported services people say they need but lack coverage for are ancillary services such as dental, vision care, and chiropractor services. In private health coverage, these ancillary services are often covered under stand-alone private insurance policies that must be purchased separately from health coverage. In Medicaid, most are not federally-required benefits for adults but rather are covered at state option; while states must provide a broad spectrum of Medicaid benefits for children, they have more flexibility in designing benefits for adults. Lack of coverage for adult dental services in Medicaid—the most frequently reported service needed but excluded from coverage—has been a longstanding issue facing beneficiaries and providers, despite a particularly high need among the low-income population.13
Insured adults also report experiencing other problems with their insurance plan. Many insured adults reported experiencing a problem with their current insurance plan covering a specific benefit, either because they were denied coverage for a service they thought was covered (25%) or their out-of-pocket costs for a service were higher than they expected (37%). Some of these services may be over-the-counter products, which are excluded from the majority of insurance plans but which people believe their plan should cover. Reports of these difficulties varied by insurance coverage. Adults with Medicaid or with nongroup coverage (both 34%) were more likely than those with employer coverage (21%) to report they were surprised that their plan would not cover a service they believed was covered. However, adults with Medicaid (22%) were less likely to report facing higher costs than expected than privately insured adults (38% among those employer coverage and 48% among those with non-group). This pattern most likely reflects the nominal out of pocket costs Medicaid beneficiaries are required to pay compared to the high cost-sharing of many private plans.
Among the goals of the ACA are ensuring that the coverage people gain provides at least a basic level of coverage and that new ways of purchasing coverage via the Marketplaces make it easier for people to navigate the insurance system. Thus, new coverage must include a set of essential health benefits (EHB), and participating plans in the Marketplace must report information on claims payment policies, cost-sharing requirements, out-of-network policies, and enrollee rights in plain language. These provisions may address some of the problems that insured adults have experienced with their coverage in the past, but uninsured adults—particularly those with limited experience enrolling in coverage—may need more help with plan selection. Further, many of the services that people report needing coverage for—such as dental and vision services—are not included in the EHB. Many newly-insured people may be surprised to learn that some ancillary services are not included in their plan, and education efforts will be needed to make sure people understand their coverage. Despite these possible challenges, most insured people—even those who report difficulties—are satisfied with their coverage overall.
Report: Iii. Gaining Coverage, Getting Care
How New Insurance Coverage Could Change How People Use Health Care
Uninsured adults generally do not seek or receive health care services at the same rate as insured adults, even when they have a need for care. Many uninsured adults have substantial health care needs that are not monitored by a physician. Cost is the main reason the uninsured do not receive care when needed, and many lack a regular provider to facilitate follow-up or ongoing care. When uninsured adults do receive care, they often have limited options. As coverage expands under the ACA, uninsured adults are likely to get care more frequently and establish relationships with physicians. Patterns of care may shift, and providers may see an increase in patients who may have previously untreated or undiagnosed health care problems.
A large segment of the uninsured has little or no connection to the health care system.
While some uninsured adults do report receiving health care services, most uninsured adults report few connections to the health care system. Only about half of uninsured adults (51%) report that they have a usual source of care, or a place to go when sick or need advice about their health (not counting the emergency room). Having a usual source of care is an indicator of being linked in to the health care system and having regular access to services. In comparison to the uninsured, most insured adults—82% of those with employer coverage, 78% of those with nongroup coverage, and 76% of those with Medicaid coverage— have a usual source of care (Figure 13). Uninsured adults also are less likely to have a regular doctor at their usual source of care – only 33% of uninsured adults have a regular doctor, half the rate of insured adults. Notably, low-income uninsured adults are the least likely to have a usual source of care or a regular physician (Table 3).
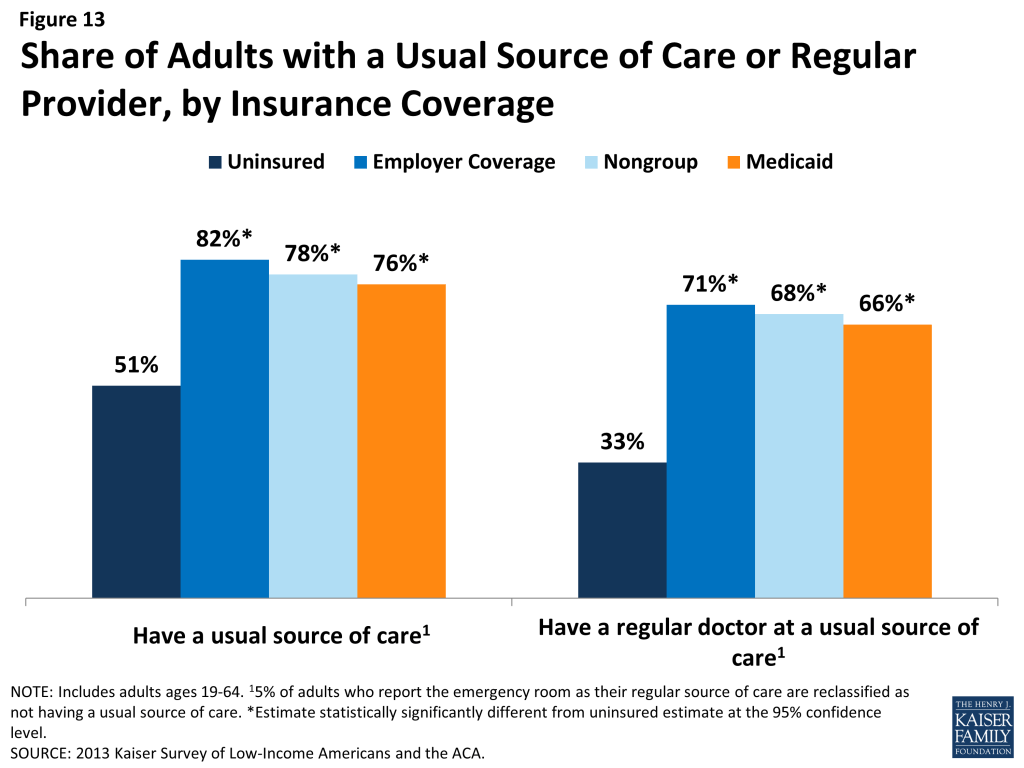
| Table 3: Share of Adults with Usual Source of Care or Regular Provider, by Income and Coverage | |||||
| Uninsured | Insured | ||||
| Employer | Nongroup | Medicaid | |||
| Has a usual source of care^ | |||||
| All | 51% | 82%* | 78%* | 76%* | |
| By Income | |||||
| <138% FPL | 49% | 67%* | 73%* | 74%* | |
| 139-400% FPL | 51% | 81%* | 69%* | 80%* | |
| >400% FPL | 67% | 85% | 89% | — | |
| Has a regular provider at usual source of care^ | |||||
| All | 33% | 71%* | 68%* | 66%* | |
| By Income | |||||
| <138% FPL | 27% | 56%* | 61%* | 64%* | |
| 139-400% FPL | 36% | 70%* | 56%* | 71%* | |
| >400% FPL | — | 74% | 84%* | — | |
| Notes: Don’t Know and Refused responses not shown. Excludes people covered by other sources, such as Medicare, VA/CHAMPUS, or other state programs.”–“: Estimates with relative standard errors greater than 30% or cell sizes below 50 are not provided.^ 5% of adults who report the emergency room as their regular source of care are reclassified as not having a usual source of care.* Estimate statistically significantly different from uninsured estimate at the 95% confidence level. SOURCE: 2013 Kaiser Survey of Low-Income Americans and the ACA. | |||||
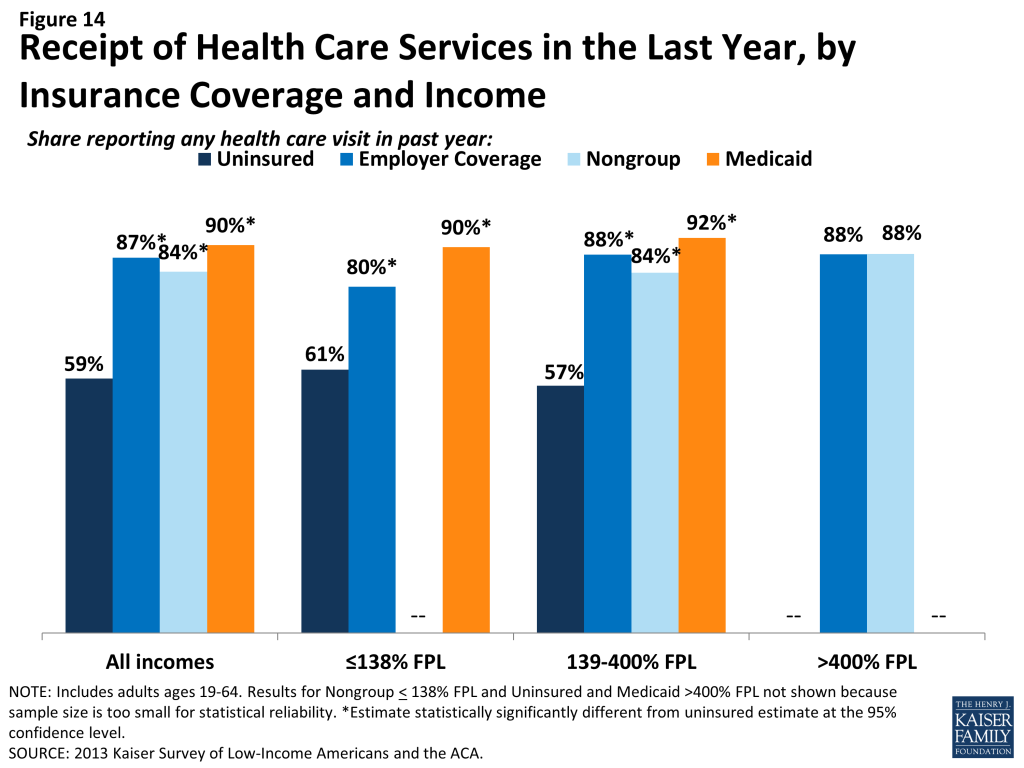
This lack of a connection to the health care system leads many uninsured adults to go without care. More than four in ten uninsured adults (41%) reported no health care visits (including hospital visits, doctors’ or clinic visits, mental health services, or trips to the emergency room) in the past year, compared to 10% of Medicaid beneficiaries and 13% of adults with employer coverage (Figure 14). This pattern holds across income groups. Of particular concern is the lack of preventive visits among the uninsured. Only 1 in 3 uninsured adults (33%) reported a preventive visit with a physician in the last year (data not shown), compared to 74% of adults with employer coverage and 67% of adults with Medicaid.
The survey findings reinforce conclusions based on prior research: having health insurance affects the way that people interact with the health care system, and people without insurance have poorer access to services than those with coverage.14 ,15 ,16 Thus, gaining coverage is likely to connect many currently uninsured adults to the health care system. However, outreach may be needed to link the newly-insured to a regular provider and help them establish a pattern of regular preventive care.
A substantial share of the uninsured has health needs, many of which are unmet or only met with difficulty.
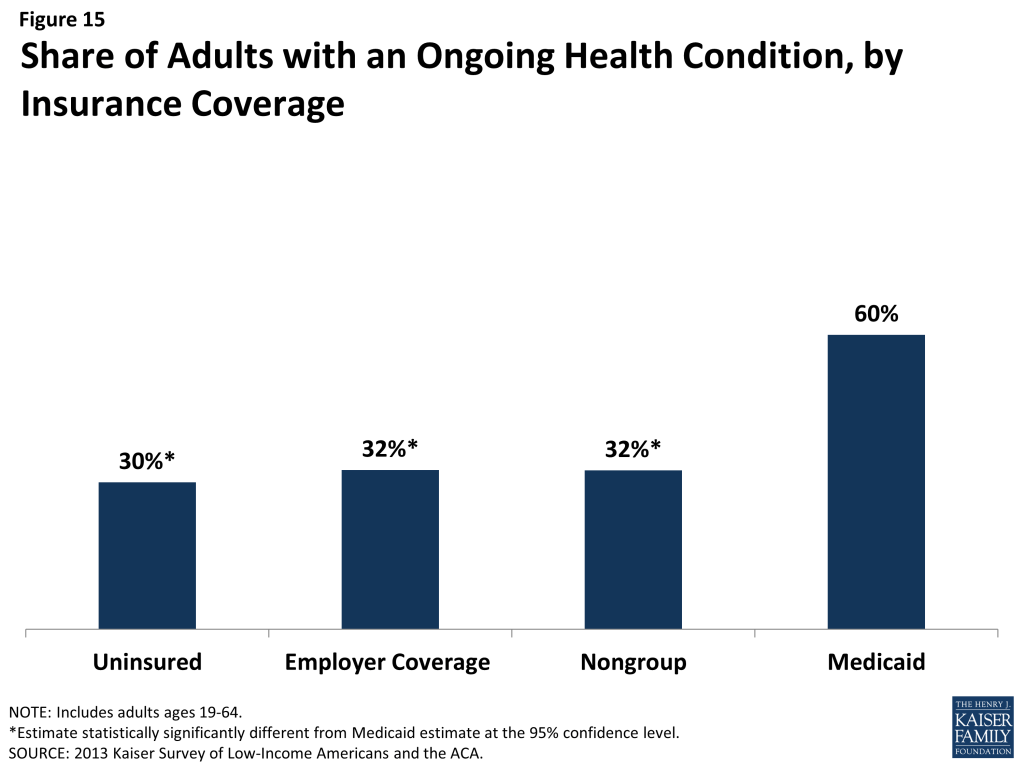
People who lack health insurance still have health care needs. In fact, uninsured adults in the survey were just as likely as those with private insurance to report having an ongoing health condition, with about 3 in 10 uninsured (30%) and privately insured adults (32% for both employer and nongroup coverage) reporting having an ongoing health condition (Figure 15). Given that the uninsured are more likely than people with coverage to have undiagnosed illness,17 actual rates of illness among the uninsured may be even higher. In contrast to those with private insurance, adults with Medicaid are twice as likely as uninsured adults to report having a health condition, with 60% of Medicaid beneficiaries reporting an ongoing health condition. This finding, which holds across income groups (Table 4) reflects Medicaid’s pre-ACA role in caring for people with substantial health needs (such as individuals with disabilities or people who become impoverished due to high health care expenses). As low-income uninsured gain coverage under reform, Medicaid’s role will expand to include a broader scope of the adult population.
| Table 4: Health Status of Adults by Income and Coverage | |||||
| Uninsured | Insured | ||||
| Employer | Nongroup | Medicaid | |||
| Fair or poor overall health | |||||
| All | 32% | 12%* | 14%* | 45%* | |
| By Income | |||||
| <138% FPL | 37% | 18%* | — | 47%* | |
| 139-400% FPL | 29% | 14%* | — | 35% | |
| >400% FPL | — | 9%* | — | — | |
| Fair or poor mental health | |||||
| All | 18% | 6%* | — | 34%* | |
| By Income | |||||
| <138% FPL | 21% | 12%* | — | 33%* | |
| 139-400% FPL | 18% | 9%* | — | 38%* | |
| >400% FPL | — | — | — | — | |
| Have an ongoing health condition that needs to be monitored regularly orneeds regular care | |||||
| All | 30% | 32% | 32% | 60%* | |
| By Income | |||||
| <138% FPL | 32% | 23%* | — | 63%* | |
| 139-400% FPL | 29% | 30% | 33% | 50%* | |
| >400% FPL | — | 36% | 27% | — | |
| Take prescription medication on regular basis^ | |||||
| All | 28% | 42%* | 45%* | 71%* | |
| By Income | |||||
| <138% FPL | 31% | 34% | — | 71%* | |
| 139-400% FPL | 28% | 37%* | 43% | 74%* | |
| >400% FPL | — | 47% | 45% | — | |
| Notes: Don’t Know and Refused responses not shown. Excludes people covered by other sources, such as Medicare, VA/CHAMPUS, or other state programs.”–“: Estimates with relative standard errors greater than 30% or cell sizes below 50 are not provided.^ Excludes birth control.* Estimate statistically significantly different from uninsured estimate at the 95% confidence level.Source: 2013 Kaiser Survey of Low-Income Americans and the ACA. | |||||
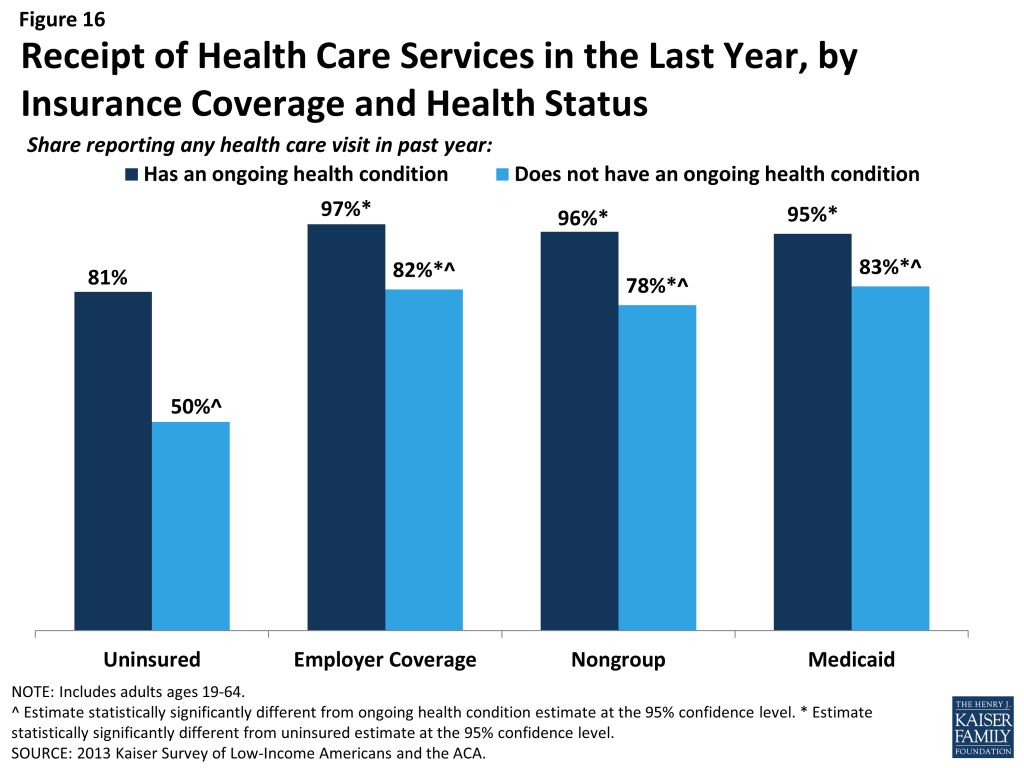
While uninsured individuals with an ongoing health condition are more likely than those without to report receiving services (Figure 16), they are still less likely than their insured counterparts to receive care. Half (50%) of uninsured adults without an ongoing health condition, received services in the past year compared to 81% of uninsured adults with a health condition. However, this rate is still lower than adults who have a health condition and have employer coverage, nongroup coverage, or Medicaid, nearly all of whom (97%, 96%, and 95%, respectively) received medical services over the course of the year.
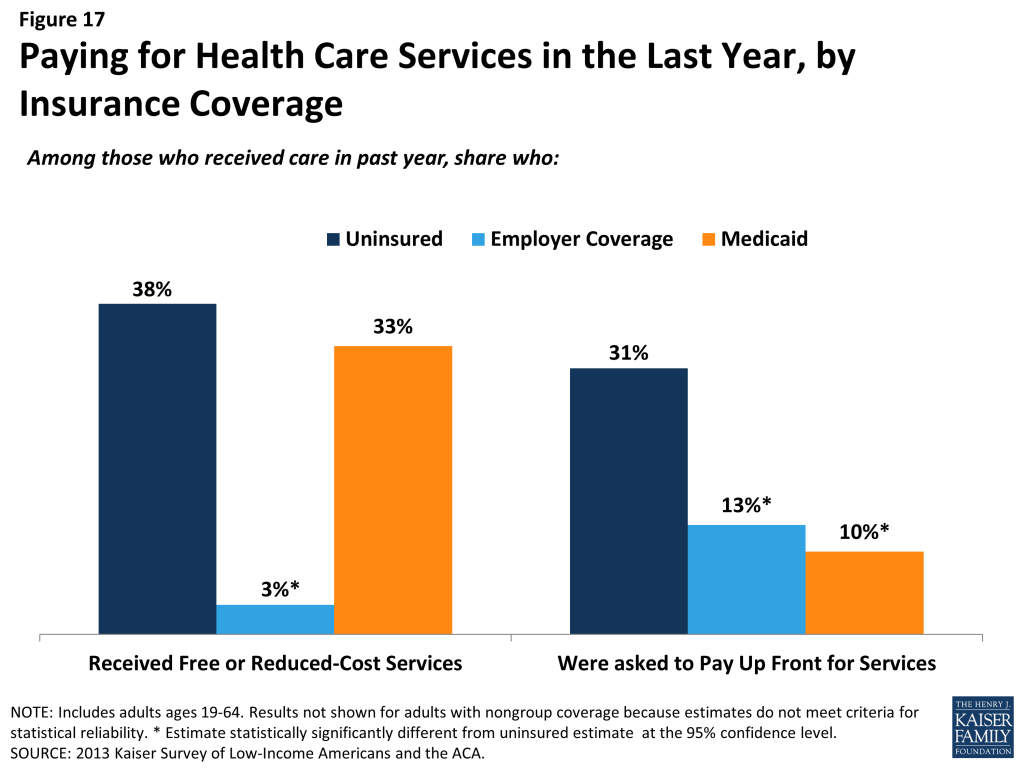
When uninsured individuals do receive care, they sometimes receive free or reduced-cost care, though the majority who use services do not. Among adults who reported that they received a health care service in the past year, 38% of uninsured adults report receiving free or reduced cost care, versus just 3% of those with employer coverage (Figure 17). Notably, about a third of adults with Medicaid who received services reported that they received free or reduced cost care. They may have done so during a period of uninsurance in the previous year or may associate the fact that they pay little or no costs when they see a provider as receiving “free or reduced cost” care. Uninsured adults who received care were much more likely than their insured counterparts to be asked to pay up front for care: nearly a third (31%) report being asked to pay for the full cost of medical care (not counting copayments) before they could see the doctor or provider, versus just 13% of those with employer coverage and 10% of adults with Medicaid. Again, insured adults may have experienced these issues during a period in the past year when they lacked coverage.
Despite some uninsured adults reporting that they receive free or reduced cost services, a larger share report an unmet need for care. Almost half (49%) of the uninsured report needing but postponing care compared to 28% of adults with employer coverage, 36% with nongroup coverage, and 41% of Medicaid beneficiaries (Figure 18). The relatively high rate among Medicaid beneficiaries reflects higher need: among Medicaid beneficiaries without a disability or ongoing health condition, rates of unmet need are similar to adults with other sources of coverage (data not shown).
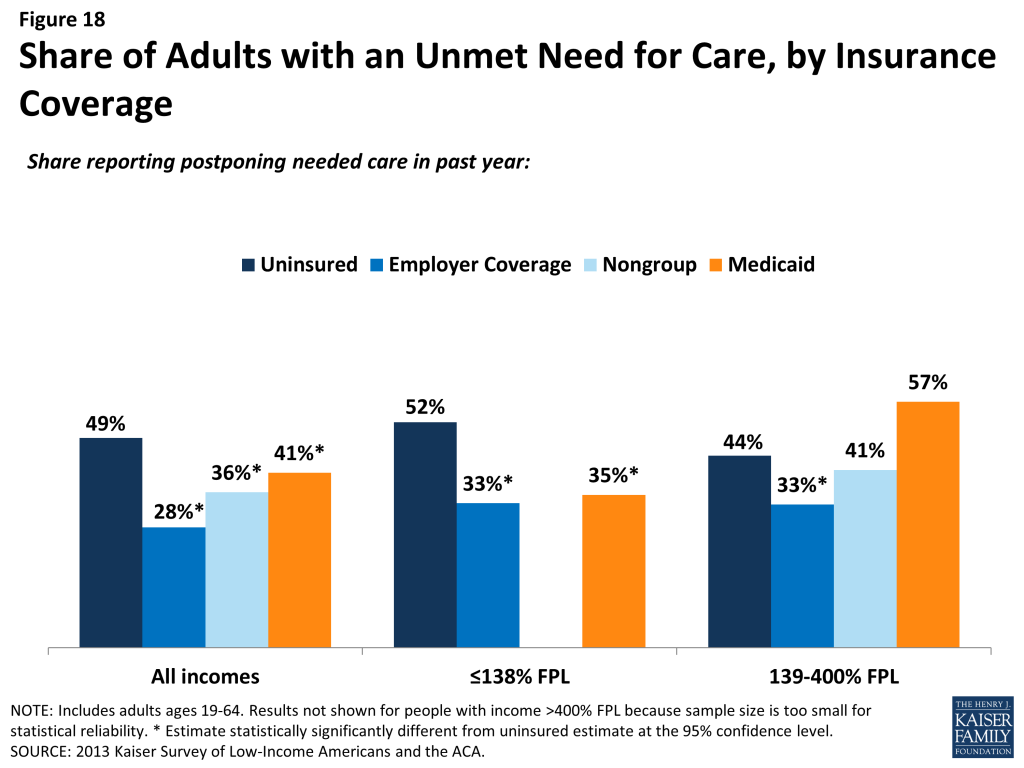
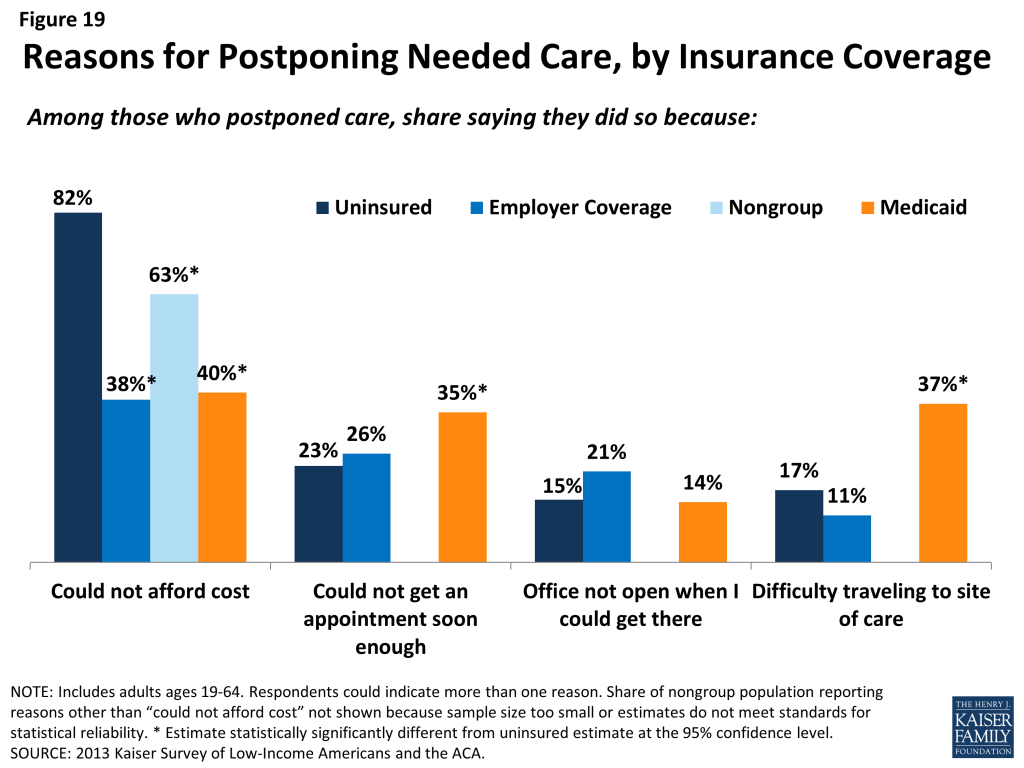
The most common reason for postponing care among the uninsured is cost, as the uninsured must pay the full cost of their care. Adults with employer coverage (38%), nongroup coverage (63%) or Medicaid (40%) are less likely to report cost as a reason for postponing care because presumably their insurance pays most or all of that cost (Figure 19). However, adults with Medicaid were more likely than other adults to report that they postponed care because they were unable to get an appointment soon enough or because they had difficulty traveling to the doctor’s office or clinic. These issues may reflect problems with provider participation in Medicaid, limits on Medicaid coverage of transportation services, or transportation barriers unique to the low-income population (such as not having a car). The only barrier that adults with employer coverage were more likely than other adults to report is the clinic or doctor’s office not being open at times when they could get there. This issue is a particular challenge for low-income workers, who often lose income when they take time off for a medical appointment during the day.
Given the health profile of the currently uninsured population, there is likely to be some pent-up demand for health care services among the newly-covered. Health systems may see increases in adults seeking care and will need to prepare for the newly insured. As people gain coverage under the ACA, the cost barriers to health care services will be reduced, but other barriers such as transportation or wait times for appointments may remain. The ACA included funds to expand service capacity in medically underserved areas, including expansion of community health centers, nurse-managed health centers and school-based clinics. To meet the health care needs of both insured and uninsured individuals, it is important that these systems develop flexible treatment times to accommodate people’s availability and expand capacity in areas where low-income individuals reside or seek care.
Many of the uninsured report limited options for receiving health care when they need it.
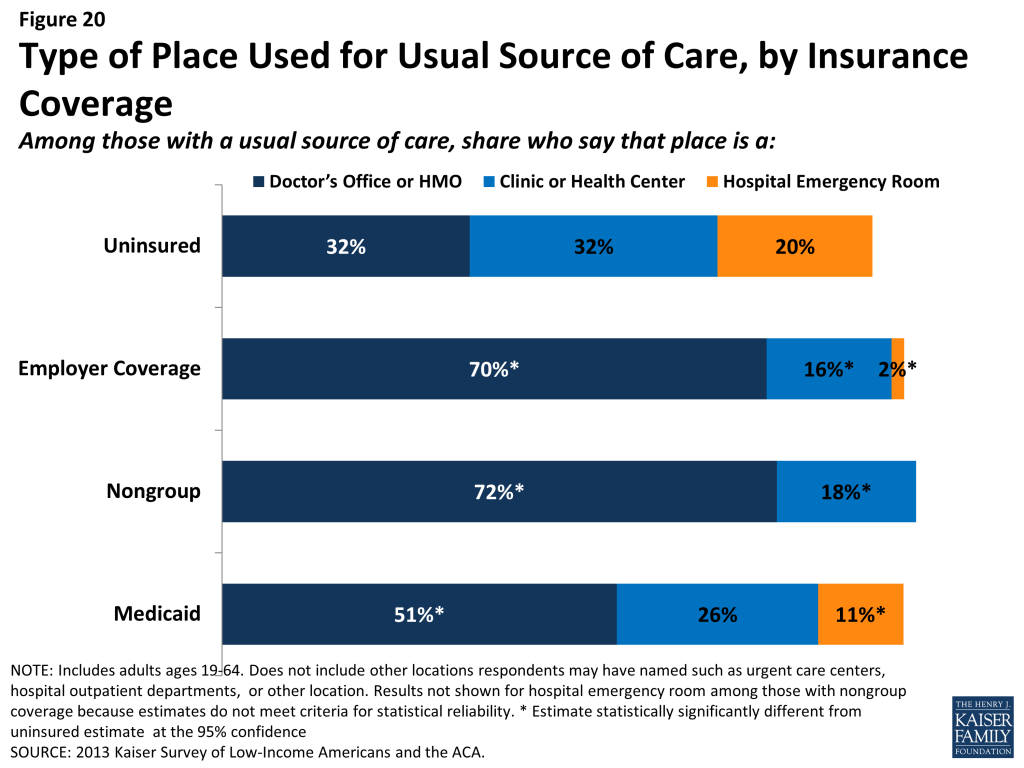
Uninsured adults are less likely than their insured counterparts to receive care in a private physician office when they do get care. About a third of uninsured adults (32%) report that a physician’s office or HMO is their regular source of care, compared to 70% of adults with employer coverage and more than half with Medicaid or other coverage (Figure 20). A third of uninsured adults who have a regular source of care (32%) report clinics or health centers as their usual source of care, twice as high as adults with employer coverage (16%). Notably, 20% of uninsured adults report the emergency room as their usual source of care – almost double the share of adults with Medicaid and ten times higher than adults with employer coverage (2%).
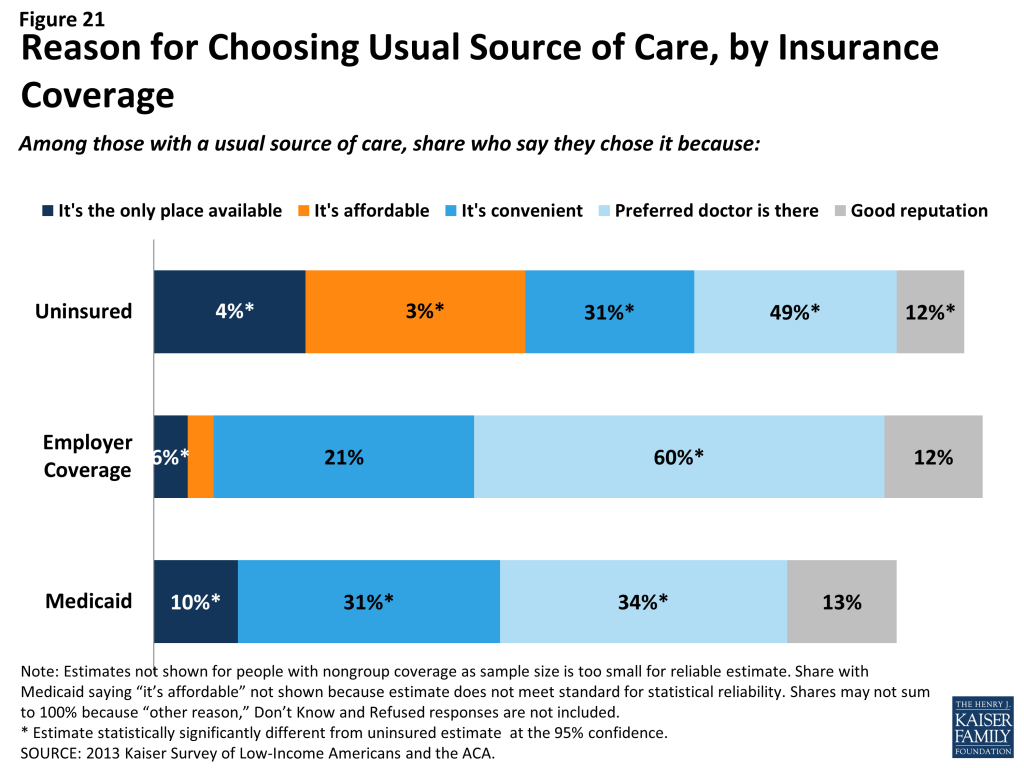
Uninsured adults are more likely than other adults to report that they have limited options for their usual source of care. Among people with a usual source of care, 18% of uninsured people report that they chose their usual source of care because it is the only option available to them, compared to 10% of adults with Medicaid and 4% with employer coverage (Figure 21). Of uninsured adults who say they had only one choice for care, almost half say that choice was the emergency department (data not shown). Uninsured adults are also more likely than other adults to choose their usual source of care because it’s affordable and less likely than other adults to choose their site of care because of convenience or ability to see their preferred provider. Most of those who say they chose their usual source of care based on cost say they chose a clinic or health center, reflecting that these providers often have a mission to serve low-income populations and offer services on a sliding scale.18
Based on the experience of their insured counterparts, the uninsured may have more options for where to receive their care once they obtain coverage under the ACA. Clinics and hospitals that already see a large share of uninsured adults may play an important role in enrolling this population in coverage and serving them once they gain insurance. However, these providers’ ongoing role—and people’s continuity of treatment— will depend in part on whether they are included in plan networks under both Medicaid and Marketplace plans. Further, many uninsured adults live in medically underserved areas, and it will be important to monitor whether coverage provisions are accompanied by delivery system reforms and new resources for primary care to expand access. Some individuals who have relied on emergency rooms or urgent care centers as their usual source of care may require help in establishing new patterns of care and navigating the primary care system. Last, in states that do not expand Medicaid, clinics and hospitals may continue to see high levels of the uninsured population and will remain the “safety net” for people who lack financial resources but need care.
Report: Iv. Health Coverage And Financial Security
How the ACA Might Affect Low and Moderate Income People’s Financial Situation
Low-income families face multiple financial challenges on a daily basis, but a major challenge is the cost of health care. Insurance provides some financial protection for many low-income adults, but many still struggle to pay their share of premiums or other costs associated with care. Low-income adults without coverage are particularly vulnerable, facing even more financial strain than their insured counterparts. Both insured and uninsured low-income adults struggle with medical bills and debt, and coverage expansions, assistance with premium costs, and limits on out-of-pocket costs under the ACA have the potential to ameliorate the financial issues associated with the cost of health care.
Health care costs pose a challenge for low- and moderate-income families, even if they have insurance coverage.
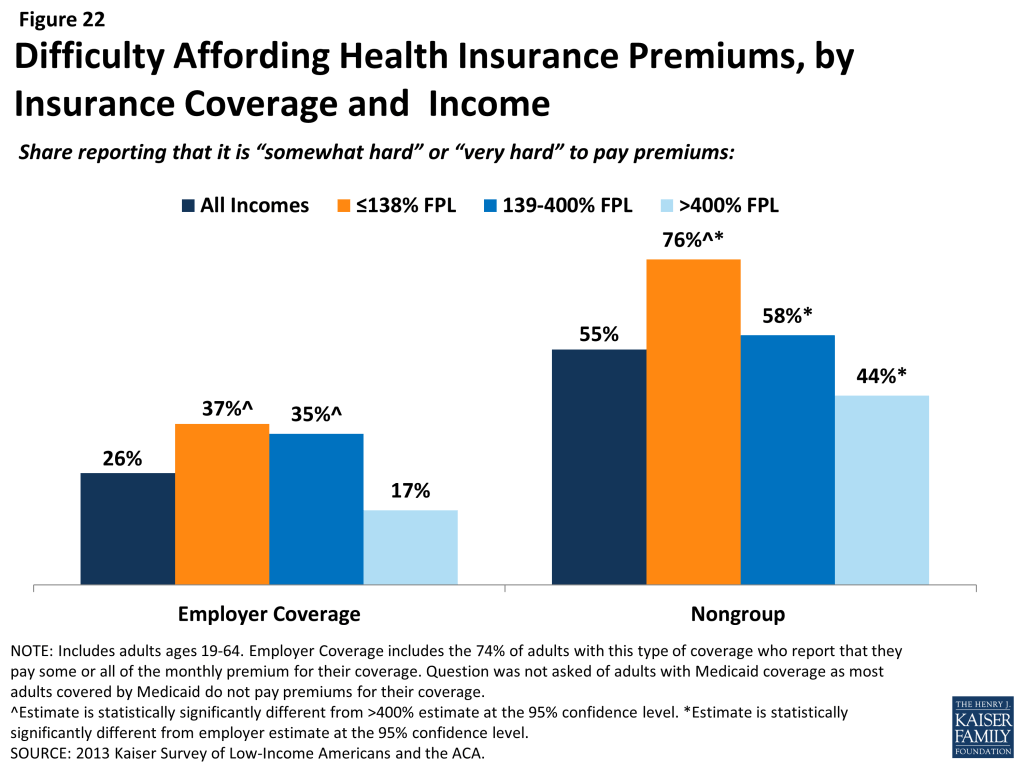
Health care accounts for a major budget item for low-income families, and affordability is a concern for many. Even among those with insurance, costs can be a burden. One source of cost burden is the cost of insurance itself. Nearly three-quarters of adults with employer coverage (74%) say they pay at least some part of their premium (data not shown), and adults with non-group coverage pay premiums directly to insurers themselves. Of adults who pay at least some portion of their premium, those with low incomes are most likely to report difficulty paying these costs (Figure 22). Thirty-seven percent of low-income (< 138% FPL) adults and 35% of moderate-income adults (139%-400% FPL) who pay a share of the premium for employer coverage report that their share is somewhat hard or very hard for them to afford, compared to 17% of higher-income (>400% FPL) adults with this coverage. For adults with non-group coverage, the rates are higher, with 76% of the low-income, 58% of the moderate income, and 44% of the higher income reporting difficulty paying their premiums. Since most adults with employer coverage share the cost of the premium with their employer, it is not surprising that rates of difficulty are higher among those with non-group coverage, who all pay the entire cost themselves.
Health care costs translate to medical debt for many l0w-income adults. While uninsured adults of all incomes are most likely to have outstanding medical bills, many low- and moderate-income insured adults also report high rates of medical bills that are unpaid or being paid off over time (Table 5). For example, 26% of low-income (<138% FPL) adults with employer coverage and 28% of low-income adults with Medicaid coverage report having medical debt. Some of these bills may reflect people’s coverage not covering all of their medical expenses, and some have been incurred during periods of uninsurance: 34% of insured adults with a gap in coverage have outstanding medical bills, compared to 23% with no gaps in coverage (data not shown). Some adults with Medicaid may have become eligible for their coverage as a result of having high medical bills, qualifying through a “medically needy” pathway for people who have high medical expenses.19 Once uninsured adults gain coverage, they may still have lingering medical bills from the past.
Regardless of coverage, medical bills can cause serious financial strain. People may report medical debt but not have a problem paying that debt. However, when asked directly whether they had problems paying medical bills in the past year, notable shares of low- and moderate-income adults reported that they did (Table 5). In many cases, the problems people had paying medical bills were severe. Adults in every coverage and income category reported that medical bills caused them to use up all or most of their savings, have difficulty paying for necessities, borrow money, or be contacted by a collection agency (Table 5).
| Table 5: Medical Debt and Problems with Medical Bills among Adults, by Income and Coverage | |||||
| Uninsured | Insured | ||||
| Employer | Nongroup | Medicaid | |||
| Has Outstanding Medical Bills or Paying Off Bills Over Time | |||||
| All | 39% | 21%* | 28%* | 30%* | |
| By Income | |||||
| <138% FPL | 40% | 26%* | — | 28%* | |
| 139-400% FPL | 38% | 28%* | 31% | — | |
| >400% FPL | — | 15% | — | — | |
| Had Problem Paying Medical Bills in Past Year^ | |||||
| All | 22% | 9%* | 12%* | 15%* | |
| By Income | |||||
| <138% FPL | 25% | 18% | — | 17%* | |
| 139-400% FPL | 17% | 13% | — | — | |
| >400% FPL | — | 4% | — | — | |
| Medical Bills Led to Serious Financial Strain^,^^ | |||||
| All | 20% | 7%* | 11%* | 12%* | |
| By Income | |||||
| <138% FPL | 23% | 13%* | — | 14%* | |
| 139-400% FPL | 15% | 11% | — | — | |
| >400% FPL | — | — | — | — | |
| Notes: Excludes people covered by other sources, such as Medicare, VA/CHAMPUS, or other state programs.”–“: Estimates with relative standard errors greater than 30% or cell sizes below 50 are not provided.^ Excludes people who reported a problem with medical bills that were not their own.^^ Defined as reporting that medical bills caused them to use up all or most savings; have difficulty paying for necessities; borrow money; or be contacted by a collection agency.* Estimate statistically significantly different from uninsured estimate at the 95% confidence level.SOURCE: 2013 Kaiser Survey of Low-Income Americans and the ACA. | |||||
In addition to many low-income adults reporting that they have experienced financial strain or difficulty with health care costs, many live with worry about their ability to afford costs in the future. The vast majority of low- and moderate-income uninsured adults report that they lack confidence that they could afford either the cost of care for services they typically require (Figure 23) or the cost of care should they face a major illness (Figure 24). While not surprising, this finding indicates that uninsured adults are aware of the high cost of health care services, as even those with moderate or high incomes do not believe they can afford these costs. One role of insurance coverage is to protect people against these costs, particularly unexpected costs related to major illnesses or accidents. However, notable shares of low-income insured adults report that they lack confidence in their ability to afford health care, given their current finances and health insurance situation. Over a third of adults on Medicaid report lack of confidence in affording usual costs, a finding that appears to be driven by higher need among Medicaid beneficiaries (as those with disabilities report particularly high rates) or worry about keeping coverage (as those who had problems with renewal also report high rates) (data not shown). Of particular note is the finding that about half of adults with nongroup coverage do not feel confident that they could afford costs related to a major illness given their coverage and financial situation. This lack of confidence may reflect worry about affording out-of-pocket costs or concerns over limits on coverage.
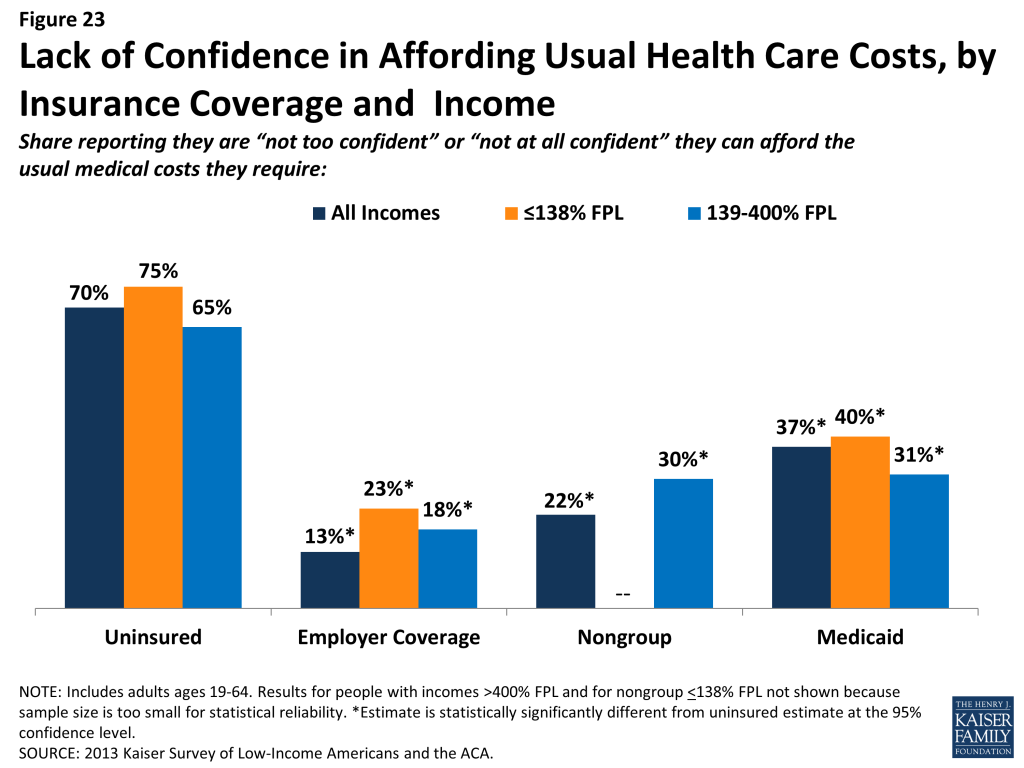
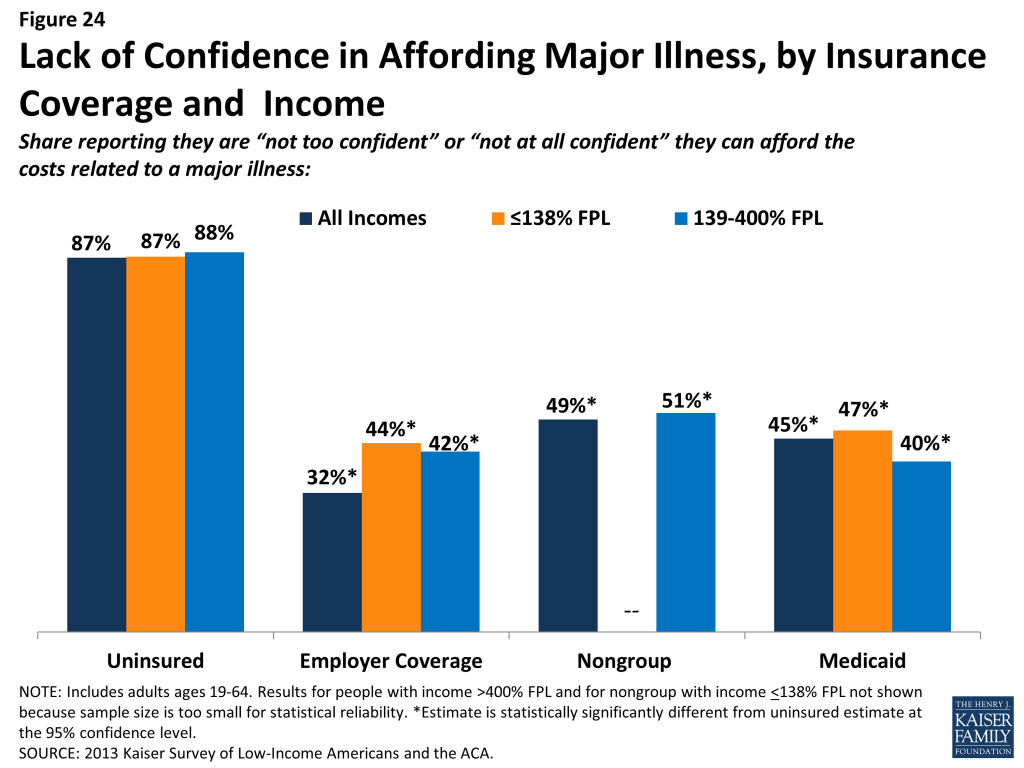
Affordability provisions in the ACA may ameliorate some of the challenges that low-income insured individuals face in affording care. Under the law, qualified health plans must cover preventive services with no cost sharing and are prohibited from placing annual or lifetime caps on the dollar value of insurance coverage. In addition, plans may not exclude coverage for pre-existing conditions, which often was excluded from nongroup plans in the past and may have led to high out-of-pocket costs for insured individuals. Last, people who purchase coverage through the Marketplaces and have incomes up to 400% FPL receive tax credits to help them afford their premiums, and those with incomes up to 250% FPL also receive subsidies to help with cost sharing under their plans. As was the case in the past, people covered by Medicaid do not pay premiums and face only nominal cost sharing for services. However, given survey findings that many low-income insured people continue to face financial challenges related to health care, it will be important to track whether there are ongoing financial barriers as people enroll in coverage and seek care.
Low-income families face fragile financial circumstances.
“We went from basically not having any debt to $25,000 I think so far just in medical debt by itself. It’s very challenging- very rough.”
Jeff (MO), on medical costs while uninsured
As discussed above, low- and moderate-income adults across coverage groups experience difficulty or worry paying for health care. These challenges translate to expenses in other areas as well, and low- and moderate-income adults across coverage groups report not being financially secure. However, adults who are low-income and uninsured or covered by Medicaid are particularly vulnerable to financial insecurity even outside of health care. Among the low-income, uninsured adults are more likely than adults with employer coverage to report that they feel generally financially insecure (Figure 25). Notably, adults with Medicaid coverage reported rates of financial insecurity closer to those of their uninsured counterparts. This pattern may reflect historical Medicaid eligibility rules, which were targeted very vulnerable adults: in most states, adults were only eligible if their incomes were below half the federal poverty level, and some adults had to deplete their income or resources before they could be eligible for assistance.
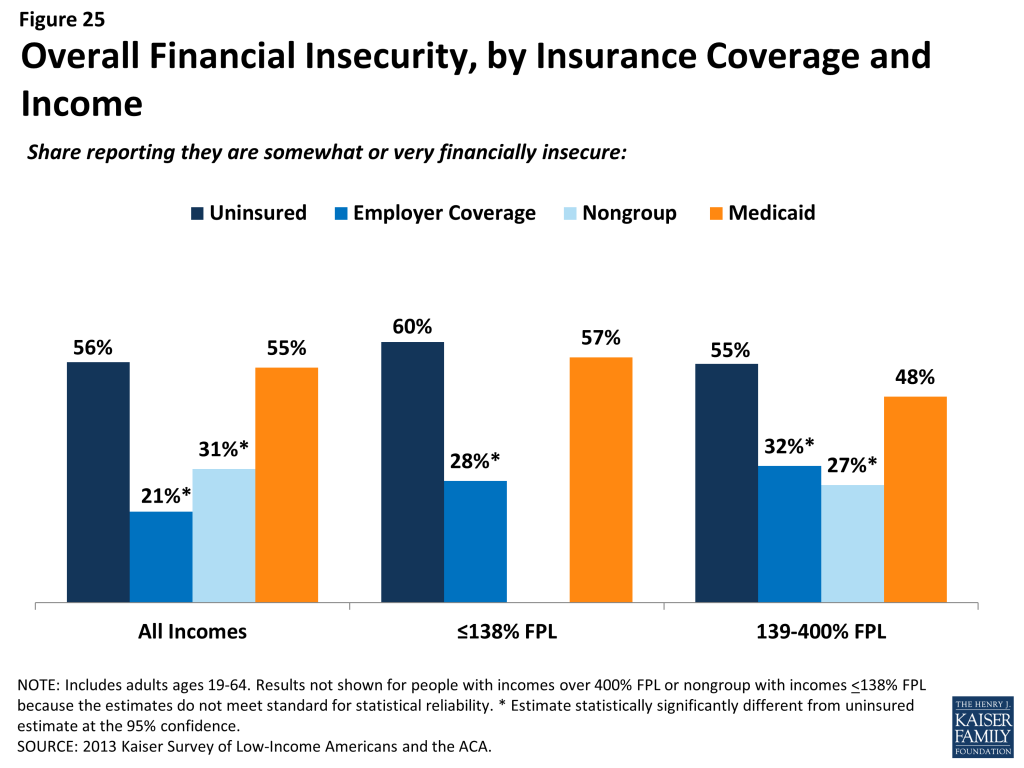
General financial insecurity translates to concrete financial difficulties in making ends meet. Uninsured adults and those on Medicaid are more likely than privately-insured adults to have difficulty paying for other necessities such as food, housing, or utilities, with 58% reporting such difficulty compared to 19% of those with employer coverage and a quarter of those with nongroup coverage (Table 6). While low-income adults across the coverage spectrum report high rates of difficulty paying for necessities, those with employer coverage report the lowest rates in this income group. These individuals may have the stronger or more stable ties to employment than their counterparts with other or no insurance coverage. A similar pattern holds for people’s ability to get ahead financially, either saving money or paying off debt.
While similarly high levels of adults across income and coverage groups report that they have taken on debt or taken money out of their savings to pay bills in the past year (Table 6), uninsured adults are more likely than adults with employer or nongroup coverage to report changing their living situation or postponing marriage or children for financial reasons.
| Table 6: Financial Difficulty among Adults, by Income and Coverage | |||||
| Uninsured | Insured | ||||
| Employer | Nongroup | Medicaid | |||
| Has difficulty paying for necessities | |||||
| All | 58% | 19%* | 25%* | 58% | |
| By Income | |||||
| <138% FPL | 68% | 40%* | — | 59%* | |
| 139-400% FPL | 54% | 26%* | 23%* | 55% | |
| >400% FPL | — | — | — | — | |
| Has difficulty saving money | |||||
| All | 82% | 50%* | 61%* | 80% | |
| By Income | |||||
| <138% FPL | 87% | 61%* | 73% | 82% | |
| 139-400% FPL | 78% | 60%* | 69% | 76% | |
| >400% FPL | 73% | 41%* | 48%* | — | |
| Has difficulty paying off debt | |||||
| All | 57% | 30%* | 37%* | 59% | |
| By Income | |||||
| <138% FPL | 61% | 41%* | — | 63% | |
| 139-400% FPL | 53% | 38%* | 43% | 49% | |
| >400% FPL | — | 22%* | — | — | |
| Taken on debt or took money out of savings to pay bills | |||||
| All | 46% | 42% | 53% | 45% | |
| By Income | |||||
| <138% FPL | 44% | 41% | — | 43% | |
| 139-400% FPL | 50% | 52% | 54% | 53% | |
| >400% FPL | — | 36% | 49% | — | |
| Changed living situation or postponed marriage/children for financial reasons | |||||
| All | 39% | 17%* | 11%* | 32% | |
| By Income | |||||
| <138% FPL | 46% | 35%* | — | 32%* | |
| 139-400% FPL | 35% | 20%* | — | — | |
| >400% FPL | — | 11% | — | — | |
| Notes: Excludes people covered by other sources, such as Medicare, VA/CHAMPUS, or other state programs.”–“: Estimates with relative standard errors greater than 30% or cell sizes below 50 are not provided.* Estimate statistically significantly different from uninsured estimate at the 95% confidence level.SOURCE: 2013 Kaiser Survey of Low-Income Americans and the ACA. | |||||
“I don’t have enough for health insurance, rent, and bills.”
Celina (MO), on family finances and health insurance
While it is not surprising that many low-income families are in a precarious financial situation, it is notable that low-income adults who lack insurance coverage or who were covered by Medicaid before the ACA are more financially unstable than their privately-insured counterparts. Prior to the ACA, Medicaid coverage for adults was targeted to those with the greatest need, and this role is reflected in the fact that they face similar financial challenges as their uninsured counterparts. While insurance coverage can provide financial protection in the event of illness or injury, it is not curative of all of the financial burdens faced by low-income families. Given their overall situation, health insurance alone may not lift low-income people out of poverty, and many low-income adults may continue to face financial challenges even after gaining coverage. However, gains in coverage under the ACA may address some of the consequences of financial instability among low-income families, and linking low-income adults with other support systems may help address the broader financial challenges that they face.
Report: V. Poised At The Starting Line
Low- and Moderate-income Uninsured Adults’ Readiness for the ACA
Low-and moderate income adults are the main targets of the ACA expansions, but prior to the start of open enrollment, many remained unaware of their coverage options under the law. Confusion over state decisions about whether to expand their Medicaid programs or operate their own Marketplaces may have clouded messaging on new coverage options. Further, while there were well-documented technical problems with initial enrollment efforts, some uninsured adults may face additional challenges in signing up for coverage, as they lack basic tools needed for this process such as internet access or bank accounts. Outreach and enrollment will be crucial to the ultimate success of the ACA in expanding coverage, yet many uninsured adults have limited connection to potential outreach avenues. Past experience demonstrates that both broad and targeted outreach efforts and direct one-on-one enrollment assistance will be key for successful enrollment.20
A majority of uninsured adults who are income eligible for coverage expansions reported knowing little or nothing about Medicaid and Marketplace programs prior to the start of open enrollment.
Despite ongoing media attention to the ACA, most uninsured adults who are likely eligible for coverage under the law21 reported that they knew little about either Medicaid or Marketplaces prior to the start of open enrollment. Seven in ten uninsured adults with incomes in the Medicaid target range (<138% FPL) say they knew nothing at all or only a little about their state’s Medicaid program, and eight in ten uninsured adults in the income range for Marketplace subsidies (139-400% FPL) reported that they knew nothing at all or only a little about the Marketplaces. While these shares are fairly constant across coverage categories (see Appendix Table A6), they point to the need for substantial outreach and education efforts among the target population for coverage expansions. Recent media attention to the challenges faced in initial enrollment efforts likely has increased awareness of coverage options; however, it is not clear to what extent media attention has translated to understanding of what is available and how to enroll, or discouraged attempts to enroll. More recent polling data indicates that 46% of the nonelderly uninsured of all incomes were not aware that the law provides help to low- and moderate-income Americans to help them purchase coverage, and two-thirds (66%) of nonelderly uninsured (all incomes) say they don’t have enough information to understand how the law will impact their families, a share that has been fairly consistent since Fall 2013.22
While most uninsured adults have the necessary tools for enrolling in coverage, some will experience additional logistical issues in signing up.
Under the ACA, online applications through Healthcare.gov or state-specific Marketplace sites are intended to be the primary mode for signing up for coverage in the Marketplace. In addition, all states are required to accept online applications for Medicaid (in addition to paper, phone, and in-person applications), and many people who are eligible for Medicaid may first apply for coverage through the Marketplace web site. Thus, internet access is an important tool in accessing coverage under the law. While the majority of uninsured adults have access to the internet either at home or outside the home (Figure 26), 19% of low-income (<138% FPL) and 14% of moderate income (139-400% FPL) uninsured adults report that they do not have internet access readily available. Further, some people who report having internet access may be using their mobile devices for access, but currently healthcare.gov (and most states) are not configured to allow for application via mobile device. People without internet access via a computer may be able to enroll through other more traditional avenues such as over the phone or in person at county offices or providers, but efforts may be needed to inform people about these other application routes, and some using them may experience a slower enrollment process than they would if they applied online.
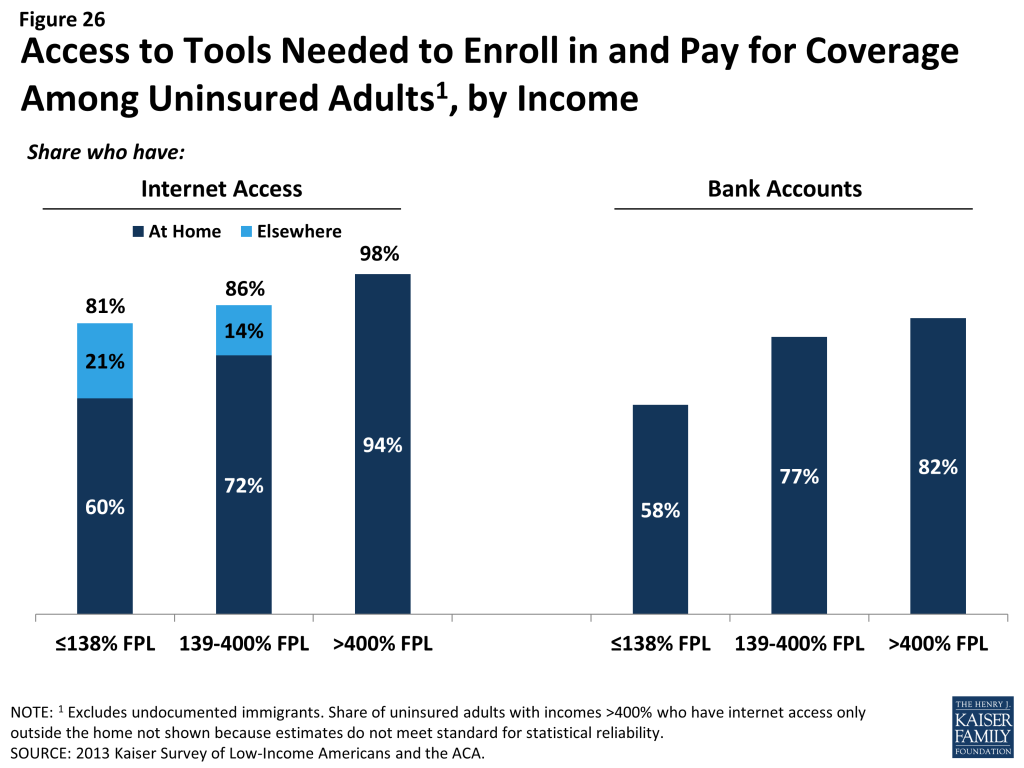
Once people are enrolled in coverage, they will require a means to pay their premiums on a regular basis (if enrolled in Marketplace coverage). While plans must accept various forms of payment,23 direct withdrawal from a checking account is a simple and reliable way to ensure that premiums are paid on time. However, nearly a quarter (23%) of uninsured adults in the income range for Marketplace subsidies (139-400% FPL) and nearly one in five (18%) of uninsured adults who could gain unsubsidized coverage through the Marketplace report that they do not have a checking or savings account (Figure 26). These “unbanked” uninsured adults may face some logistical barriers to paying premiums that those who can use direct withdrawal do not.
Many uninsured adults could be reached through targeted outreach avenues.
Across states, a variety of outreach and enrollment efforts are underway to help connect eligible people to coverage, ranging from broad marketing and media campaigns to direct one-on-one assistance. Moreover, a wide array of groups and individuals are involved in outreach and enrollment, including community-based organizations, providers, health centers, and faith-based groups.24 Some states are also utilizing new “fast track enrollment” opportunities to efficiently enroll large numbers of eligible individuals in their Medicaid programs.25 Specifically, CMS offered states the opportunity to facilitate enrollment of eligible people into Medicaid by using data already available to states through the Supplemental Nutritional Assistance Program (SNAP) and children’s eligibility data for Medicaid and the Children’s Health Insurance Program (CHIP). Experiences in states that have already launched these strategies indicate they can be highly successful in connecting people to coverage, reaching a significant share of adults eligible for the Medicaid expansion while minimizing burdens for both individuals and eligibility staff.26
Many uninsured adults report that they or their family already have a link to a social service program, making fast track enrollment efforts a promising avenue for outreach. Among uninsured adults with incomes in the range for Medicaid eligibility (<138% FPL), over six in ten (62%) report that they or someone in their immediate family receives either SNAP, cash assistance, disability payments, or Medicaid or CHIP (Figure 27). SNAP is the most common connection to social services programs among the low-income uninsured (46%). These programs already have much of the information needed to determine eligibility for Medicaid under the ACA, such as income, residence, and family structure, and could provide an efficient route to enrolling the uninsured in coverage. While lower shares of moderate-income uninsured adults report a connection to a social service program, outreach to this group of uninsured adults could also reach many eligible for coverage.
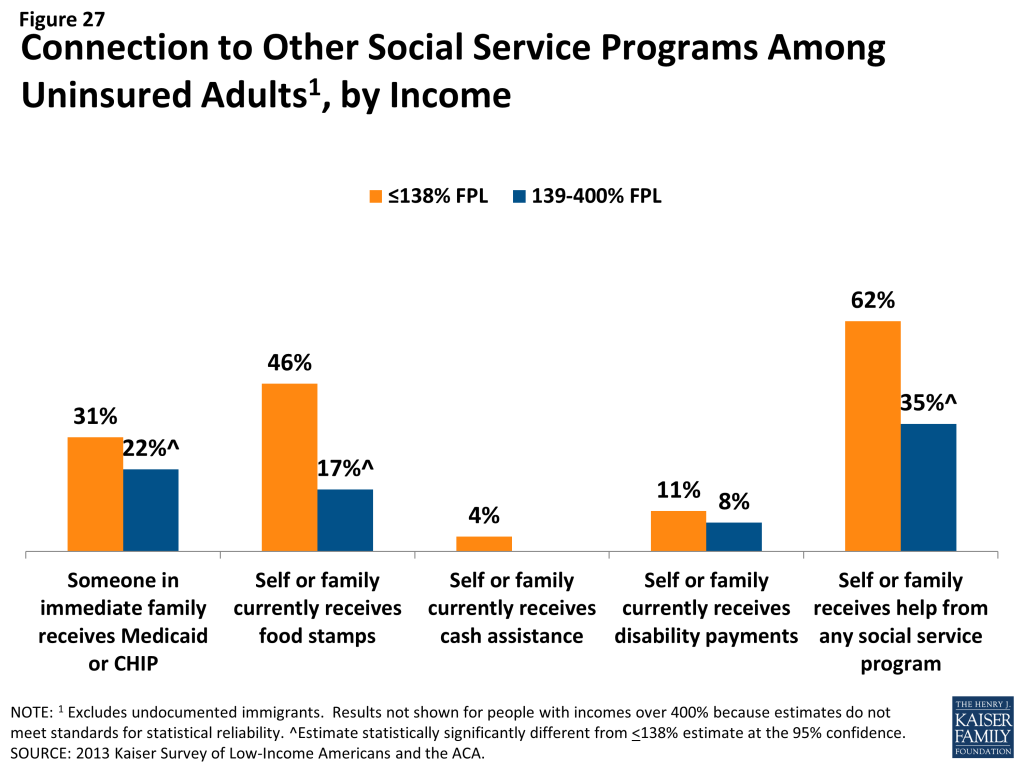
For those without a connection to social services agencies, outreach through providers may be a promising approach. Many community health centers or hospitals and health systems are very involved with outreach and enrollment efforts, sometimes having enrollment workers in-house to help patients with ACA enrollment. Clinics in particular are an important outreach location, as about one in five low- or moderate-income uninsured adults report that they use a clinic or health center as their usual source of care (Figure 28). Hospitals reach many uninsured adults through periodic visits: at least one in five uninsured low- or moderate-income adults report visiting a hospital in the past year for either emergency services or for inpatient or outpatient care. Patients who seek episodic care in emergency rooms or hospitals may be receptive to outreach efforts, as they have a demonstrated need for services and are likely to face high bills if they remain uninsured; however, outreach workers may be challenged to engage individuals in the application process at a time when they are seeking services for an urgent or acute problem.27
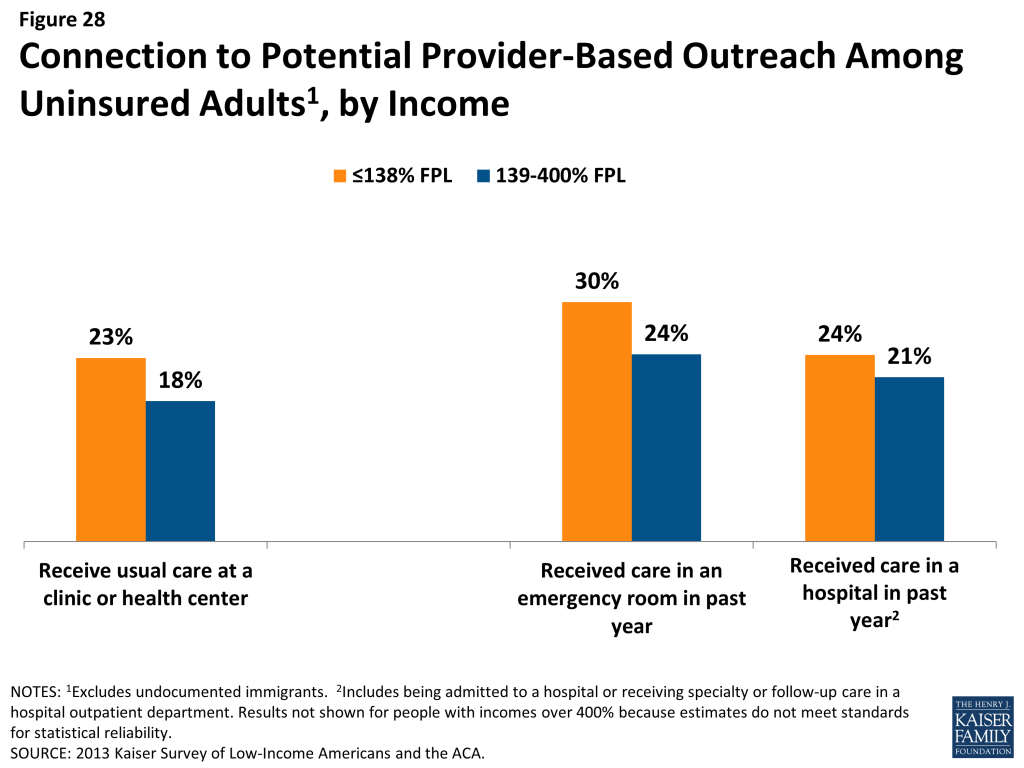
Conclusion And Policy Implications
Conclusion & Policy Implications
The survey findings related to: i) patterns of insurance coverage, ii) the process of enrolling in and choosing health coverage, iii) interactions with the health care system, iv) financial security, and v) readiness for ACA coverage expansions have implications for early implementation of the ACA. Below, we summarize the implications how this pre-ACA baseline data can inform outreach and enrollment, plan selection and scope of coverage, providers and health systems.
Reaching Eligible Uninsured Adults
Outreach and enrollment will be an ongoing process. While there is much focus on the initial push to enroll people in coverage under the ACA, enrollment is not a “one shot” effort that will be completed in the first few months of implementation. The survey findings reveal that millions of people lose and gain coverage throughout the year, either due to job changes, income fluctuations, or problems at renewal. It also demonstrates that low-income individuals are particularly vulnerable to gaps in coverage that can result from such changes. Thus, implementing the ACA will require ongoing efforts to enroll and keep people in coverage.
Some eligible uninsured adults have little or no connection to pre-ACA health or social services systems and may be hard to reach. Many people targeted for coverage expansions are not currently connected to the health care system, have been outside the health insurance system for quite some time, or are not linked to social services programs. The survey shows that nearly half of uninsured adults have lacked coverage for five years or longer, most uninsured do not have a regular source of care, and many uninsured have no health care visits over the course of a year. Further, while many low-income (<138% FPL) uninsured adults have a family connection to a social services program, the majority of moderate-income (139-400% FPL) uninsured adults do not. Public outreach campaigns are likely important avenues for reaching these individuals. In addition, policymakers may pursue new outreach avenues to find and reach out to the “unconnected” uninsured.
Many eligible uninsured have experience with pre-ACA health care, health insurance, or social services systems, but there is great need for continued education of new coverage options. Others targeted for coverage expansions have experience with the health care system and health insurance but may be unaware that eligibility and costs have changed under the ACA. Notable shares reported in the survey that they were unaware of new coverage options at the start of open enrollment, and many report experiences of trying to get coverage and encountering cost or eligibility barriers. It will be important to reach out to people who have tried to apply for coverage in the past to let them know coverage options for them may have changed. While awareness of coverage under the ACA has likely increased in recent months, given heavy media attention to the rollout of health reform, it is important to make sure the information they receive is accurate. In addition, with currently 25 states having not expanded their Medicaid programs, having left millions of low-income adults in a “coverage gap,”28 new coverage options will need to be state-specific. Efforts to reach people through “fast track” enrollment may be particularly fruitful for low-income uninsured in expansion states, as these approaches require limited paperwork and reach people with known eligibility.
Connecting People to Suitable Coverage
In addition to technical issues with websites, it will be important to monitor whether other challenges in enrolling in health coverage that existed prior to the ACA are addressed by ACA simplification provisions. Policymakers have made strides in addressing many of the website glitches that plagued early enrollment efforts under the ACA, and they continue to focus attention on addressing these technical issues. However, there are other challenges to enrolling in coverage and picking a plan that policymakers may need to address. Survey results indicate that, before the ACA, some insured people reported challenges in comparing plan information or in compiling required paperwork. While most Medicaid applicants reported that they found the process to be not difficult, Medicaid enrollees were more likely than adults with other types of coverage to report challenges in selecting a plan. The ACA includes provisions to ease the plan selection process for people purchasing coverage through the Marketplaces and to simplify the application process for Medicaid. It will be important to track implementation of these simplifications to ensure that challenges that some people faced in the past do not carry over to ACA enrollment.
Early assessments of plan choice under the ACA may account for the fact that cost is only one factor in people’s preferences for health coverage. Much focus in early coverage of ACA enrollment has been on the premiums and deductibles that people will face under their new coverage. These features provide concrete measures that people can examine, and certainly costs are a key concern for new enrollees. However, the survey shows that people also value other aspects of their coverage, such as benefits and networks, sometimes even more than low out-of-pocket costs. Evaluations of coverage therefore may consider how well new plans are meeting the full range of priorities and preferences for health coverage, and future changes to plan offerings under the law may consider people’s priorities for their coverage.
Even once people have insurance, they may face issues in scope of coverage for benefits they need. Survey findings reveal that the vast majority of enrollees in various types of coverage report being satisfied with their plan, but notable shares report a problem with their scope of coverage. Many adults on Medicaid report needing coverage for dental services that are not included in their plan, and people with private coverage also report gaps in ancillary services. Future assessments of the impact of the ACA should gauge whether the scope of coverage people have under the law, and early implementation can work to educate people about both what is and what is not included in their coverage.
While the ACA could ameliorate the financial burden of health care for many, affordability of health services may remain a challenge. In addition to the goal of facilitating access to health care services, a goal of coverage expansions is to provide financial protection from medical expenses. As survey findings show, even once people gain insurance, health care costs can be a challenge. Though less likely than their uninsured counterparts to have difficulties with medical costs, low-income insured adults report challenges in paying premiums, copayments, out-of-pocket costs for uncovered services, and other health care expenses. In addition, all low-income families, regardless of insurance coverage, face financial hardship in making ends meet. While affordability provisions in the ACA may address some of the challenges that low-income insured individuals face in affording medical care, it will be important to track ongoing financial barriers and financial instability even among those who have coverage. Further, efforts to “bend the cost curve” in health care may be a promising approach to addressing not only costs to financing sources but also to individuals.
Adapting the Health System and Patterns of Care to Meet New Needs
Based on demonstrated need and barriers to care among the uninsured prior to the ACA, health care providers may see increases in adults seeking care. Ultimately, the goal of coverage expansions under the ACA is to help people access needed health care services. Thus, once people gain coverage, providers and health systems will need to be prepared to serve newly-insured people. Survey findings reinforce conclusions from prior research that gaining health coverage is likely to alter the way that people interact with the health system. Compared to their insured counterparts, uninsured adults face barriers to care, despite many having a demonstrated need. Some uninsured adults have ongoing health conditions yet still are not receiving regular care, and others have postponed preventive or other services, primarily due to cost. These findings indicate that there is likely to be some pent-up demand for health care services among the newly-covered. Outreach and education may be needed to link the newly-insured to a regular provider and help them establish a pattern of regular preventive care.
Changes in insurance coverage may lead people to use new or different providers, but safety net providers will continue to serve many vulnerable populations. Many are concerned about shifting patterns of care under the ACA, as changes where people receive care may alter revenue streams for providers. The effect of changing revenue streams for different types of providers is unclear at this point. Based on the survey findings, the uninsured are likely to have more options for where to receive their care once they obtain coverage under the ACA. Compared to their insured counterparts, prior to the ACA, they were more likely to seek care in clinics, hospitals, or urgent care centers and to report limited options for where to get medical care. As people gain coverage, they may shift their service locations to more closely resemble that of people with private or Medicaid coverage. However, clinics and hospitals may continue to see high levels of the uninsured, particularly in states that do not expand their Medicaid programs. As uncompensated care funds diminish over time, these safety net providers may be strained to meet demand in the face of shrinking resources.
As implementation unfolds, providers may continue to be on the front lines of not only service delivery but also outreach and enrollment. Providers are one avenue that policymakers are using to reach out to uninsured adults who may be eligible for coverage expansions under the ACA. Survey findings indicate that emergency rooms and hospitals may be promising avenues for reaching eligible individuals with episodic interactions with the health system, and community health centers can reach a share of the uninsured who use them for ongoing care.
Moving Forward in ACA Implementation
As enrollment in new coverage options grows and people begin to use their coverage, survey findings point to several issues that can inform ongoing efforts to implement the ACA. Future reports using the 2013 Kaiser Survey of Low-Income Americans and the ACA will continue to delve into these issues and provide state-specific findings, and future surveys can assess whether and how coverage, access, and family finances change under the law.
Methods
This report is based on findings from the 2013 Kaiser Survey of Low-Income Americans and the ACA. This survey, conducted by the Kaiser Family Foundation (KFF) in summer 2013, examines health insurance coverage, health care use and barriers to care, and financial security among insured and uninsured adults across the income spectrum, with a focus on populations targeted for coverage expansions under the Affordable Care Act (ACA). The survey provides a baseline against which future surveys can assess the impact of the ACA on low-and moderate-income adults. The survey includes a national sample as well as three state-specific samples in California (conducted with support from the Blue Shield of California Foundation (BSCF)), Missouri (conducted with support from the Missouri Foundation for Health (MFH)), and Texas.
The survey was designed and analyzed by researchers at KFF, with feedback on the California and Missouri state-specific components from BSCF and MFH, respectively. Social Science Research Solutions (SSRS) collaborated with KFF researchers on sample design and weighting; SSRS also supervised the fieldwork.
The survey was conducted by telephone from July 24 through September 29, 2013, from representative random samples of California, Missouri, and Texas residents between the ages of 19-64, along with respondents from the remaining 47 states and the District of Columbia. In total, 8,762 interviews were completed; of these, 2,558 were with respondents living in California, 1,872 with respondents in Missouri, 1,809 with respondents in Texas, and 2,523 with respondents from other states. Computer-assisted telephone interviews (CATI) conducted by landline (4,529) and cell phone (4,233) were carried out in English and Spanish by SSRS.
Because the study was designed to focus on the low-income population, the sample was designed to over-sample this group. To efficiently reach lower-income respondents, the sample was stratified based on the estimated income level of geographic areas within the nation and within each of the three states with state-specific samples. This process was done separately for the landline and cell phone sampling frames. For the landline sample, strata were defined based on the median income within telephone exchanges; for the cell phone sample, strata were defined based on the household income associated with the billing rate-center to which the cell phone number is linked. The exact criteria for distinguishing between the strata varied from state to state. In addition, 684 interviews (359 on landline and 325 on cell phone) were conducted with respondents who were previously interviewed by SSRS as part of omnibus surveys of the general public and indicated they were ages 19-64, resided in the appropriate geography for the sample (if part of one of the state samples), and reported annual income of less than $25,000. These previous surveys were conducted with nationally representative, random-digit-dial landline and cell phone samples.
Screening for the survey involved verifying that the respondent (or another member of the household for the landline sample) met the criteria of: 1) being 19-64 years old; and 2) providing income information that allowed them to be classified by family income. Respondents were classified by family income as a share of the federal poverty level (FPL) based on their family size and total annual gross income.[endnote 101777-2] Poverty level groups included income < 138% of FPL (the income range for the Medicaid expansion), income of 139-400% FPL (the income range for Marketplace tax credits), and income above 400% of FPL (eligible only for unsubsidized coverage). For the landline sample, if two or more people met the criteria, a respondent was randomly selected by the CATI program. Selected respondents were asked to confirm their state of residence.
A multi-stage weighting approach was applied to ensure an accurate representation of the various income groups ages 19 to 64. The weighting process involved corrections for sample design as well as sample weighting to match known demographics of the target populations in order to correct for systematic non-response along these parameters. The base weight accounted for the oversamples used in the sample design, as well as the likelihood of non-response for the re-contact sample, number of eligible household members for the landline sample, and a correction to account for the fact that respondents with both a landline and cell phone have a higher probability of selection. Demographic weighting parameters were based on population estimates for the 19-64 year old poverty-level population in each state based on the U.S. Census Bureau’s 2011 American Community Survey (ACS). The weighting parameters for each poverty-level group within the three state-specific samples and the remaining national sample were: age, education, race/ethnicity, presence of own child in the household, marital status, region, and phone-status. All statistical tests of significance account for the effect of weighting.
The margin of sampling error (including the design effect) for national estimates, state estimates and state-by-poverty-level estimates are shown in Table A. For the national sample, the margin of sampling error is plus or minus 3.5 percentage points for both the low- and moderate-income groups. For results based on other subgroups, the margin of sampling error may be higher. Sample sizes and margin of sampling errors for other subgroups are available by request. In reporting results, any estimate with a relative standard error (standard error divided by the point estimate) greater than 30 percent or based on a cell size less than 50 is considered unreliable and not reported. Note that sampling error is only one of many potential sources of error in this or any other survey.
| Table A: Number of Respondents and Margin of Sampling Error for National and State-Specific Samples | ||
| N | Margin of Sampling Error | |
| U.S. Total | 8,762 | +/- 2% |
| U.S. < 138% FPL | 3,536 | +/- 4% |
| U.S. 139%-400% FPL | 3,570 | +/- 4% |
| U.S. >400% | 1,656 | +/- 5% |
| California Total | 2,558 | +/- 3% |
| CA < 138% FPL | 1,020 | +/- 5% |
| CA 139% – 400% FPL | 1,007 | +/- 5% |
| CA >400% | 531 | +/- 6% |
| Missouri Total | 1,872 | +/- 4% |
| MO < 138% FPL | 760 | +/- 5% |
| MO 139% – 400% FPL | 791 | +/- 5% |
| MO >400% | 321 | +/- 8% |
| Texas Total | 1,809 | +/- 4% |
| TX <138% FPL | 754 | +/- 6% |
| TX 139% – 400% FPL | 753 | +/- 5% |
| TX >400% | 302 | +/- 8% |
In analyzing results, we group respondents into mutually exclusive insurance categories of: Uninsured (report that they are not covered by health insurance), Employer Coverage (report that they have a plan through their own employer, a spouse’s employer, or a parent’s employer), Nongroup Coverage (report that they purchase their coverage themselves, and Medicaid (including people who are dually eligible for Medicare coverage). In capturing Medicaid coverage, state-specific program names were used. A small number of people report that they are covered by other sources, including Medicare (<3%), a government program besides Medicaid or Medicare (<3%), or some other source such as the VA, school-based coverage, or an unnamed source (<1%). We do not report results for people covered by these other coverage categories, as cell sizes were generally too small for reliable estimates.
Because eligibility for two of the law’s main coverage provisions– the Medicaid expansion and tax credits to purchase insurance on the Marketplaces– is based on an individual’s family income relative to the federal poverty level (FPL), in most cases we report survey results by FPL categories that match eligibility levels under the ACA. These categories are 1) those with incomes 138% FPL or less (roughly $32,000 a year for a family of 4), the income range for the Medicaid expansion; 2) those with incomes of 139 to 400% FPL (roughly $32,000-$94,000 for a family of 4), the income range for tax credits in the Marketplace; and 3) those with incomes above 400% FPL, who are not be eligible for financial assistance in gaining coverage. This classification is not intended to fully capture eligibility, as not everyone in these income ranges will be eligible for coverage under the ACA. For example, as of January 2014, 23 states were not planning to expand their Medicaid programs, and 2 states were planning on implementing their Medicaid expansion after January 2014.29 Further, undocumented immigrants are ineligible for coverage under the ACA, and recent legal immigrants cannot receive Medicaid coverage (though they can purchase subsidized coverage in the Marketplace). Last, some people may be ineligible for Marketplaces subsidies because they have access to affordable employer coverage. However, the income categories provide a picture of the population targeted by various expansions, rather than a picture of the specific population eligible under the law.
For results that examine the uninsured population’s readiness for the ACA (Section V), we exclude individuals who are undocumented immigrants, as this group is ineligible for any coverage under the ACA. In other sections, which aim to describe the experience of the entire uninsured population, we include undocumented immigrants in the results. We define undocumented immigrants as those who reported 1) they were born outside the United States, 2) are not a citizen, 3) did not have a green card when they arrived in the United States, and 4) have not received a green card or become a permanent resident since arriving. This measure may be subject to error in several ways. First, it relies on self-reporting, and respondents have an incentive not to reveal unlawful immigration status. Second, those that did not answer all questions in the series of immigration status items (75 respondents) were not able to be categorized as undocumented and were therefore included; if they are in fact undocumented, then the results may differ slightly. Third, a small number of people may have a legal status besides permanent residency or green card (such as refugees, asylees or other humanitarian immigrants). Unfortunately, due to time constraints, the survey was not able to fully explore all of these immigration pathways.
This report includes analysis of findings from the survey that may inform early challenges in implementing health reform. It does not include a full reporting of all the findings from the survey. Future reports will provide additional analysis of other survey findings. Survey toplines with overall frequencies for all items in the questionnaire are available upon request.
Appendix: Additional Tables
Additional Tables
| Table A1: Demographics of Adults, by Insurance Coverage | ||||
| Uninsured | Insured | |||
| Employer | Nongroup | Medicaid | ||
| Income | ||||
| < 138% FPL | 53% | 11%* | 14%* | 78%* |
| 139-399% FPL | 39% | 36% | 44% | 20%* |
| >400% FPL | 8% | 53%* | 42%* | — |
| Family Work Status | ||||
| Working Family | 66% | 91%* | 79%* | 30%* |
| Non-Working Family | 34% | 9%* | 21%* | 70%* |
| Age | ||||
| 19-25 | 17% | 14% | — | 14% |
| 26-34 | 27% | 19%* | 18% | 26% |
| 35-44 | 24% | 23% | 13%* | 16%* |
| 45-64 | 33% | 44%* | 58%* | 44%* |
| Health Status | ||||
| Ongoing Health Condition | 30% | 32% | 32% | 60%* |
| No Ongoing Health Condition | 69% | 67% | 67% | 39%* |
| Fair or Poor Health Status | ||||
| Excellent/Very Good/Good | 68% | 88%* | 86%* | 54%* |
| Fair or Poor | 32% | 12%* | 14%* | 45%* |
| Race | ||||
| White, Non Hispanic | 49% | 70%* | 75%* | 52% |
| Hispanic | 30% | 11%* | 9%* | 18%* |
| Black, Non-Hispanic | 12% | 10% | — | 20%* |
| Asian/Pacific Islander | 2% | 4% | — | — |
| American Indian Alaska Native | — | 1% | — | — |
| Other/DK, Non-Hispanic | 6% | 5% | — | 5% |
| Citizenship | ||||
| Citizen | 81% | 96%* | 97%* | 93%* |
| Non-Citizen | 19% | 4%* | — | 7%* |
| Notes: Don’t Know and Refused responses not shown. Excludes people covered by other sources, such as Medicare, VA/CHAMPUS, or other state programs. NA: Not applicable”–“: Estimates with relative standard errors greater than 30% or cell sizes below 50 are not provided.* Estimate statistically significantly different from uninsured estimate at the 95% confidence level.Source: 2013 Kaiser Survey of Low-Income Americans and the ACA. | ||||
| Table A2: History of Uninsurance and Attempts to Gain Coverage Among Currently Uninsured Adults, by Income | |||||
| All | By Income | ||||
| <138% FPL | 139-400% FPL | >400% FPL | |||
| Length of Time Uninsured | |||||
| < 3 months | 9% | 7% | 9% | — | |
| 3 Months to Less than a Year | 10% | 9% | 13% | — | |
| 1 Year to 5 years | 34% | 33% | 35% | — | |
| 5 Years or More | 29% | 31% | 27% | — | |
| Have Never Had Coverage | 18% | 20% | 16% | — | |
| Attempts to Gain Coverage | |||||
| Applied for Medicaid in past 5 years | 31% | 38% | 27%^ | — | |
| Applied for Medicaid but did not enroll | 22% | 27% | 18%^ | — | |
| Applied for Medicaid but told ineligible | 19% | 25% | 15%^ | — | |
| Tried to purchase nongroup coverage in past 5 years | 22% | 20% | 22% | — | |
| Tried to purchase nongroup coverage but did not purchase policy | 17% | 15% | 17% | — | |
| Tried to purchase nongroup coverage but too expensive | 13% | 14% | 13% | — | |
| Notes: Don’t Know and Refused responses not shown. Excludes people covered by other sources, such as Medicare, VA/CHAMPUS, or other state programs. NA: Not applicable”–“: Estimates with relative standard errors greater than 30% or cell sizes below 50 are not provided.^ Estimate statistically significantly different from <138% FPL estimate at the 95% confidence level.Source: 2013 Kaiser Survey of Low-Income Americans and the ACA. | |||||
| Table A3: Ease of Applying for Medicaid, Among Adults who Have Applied, by Income | |||||
| All | By Income | ||||
| <138% FPL | 139-400% FPL | >400% FPL | |||
| Share reporting step was somewhat or very easy: | |||||
| Finding out how to apply | 75% | 76% | 74% | — | |
| Filling in requested information | 74% | 74% | 74% | — | |
| Assembling the required paperwork | 62% | 63% | 59% | — | |
| Submitting the application | 78% | 78% | 78% | — | |
| Share reporting all steps were somewhat or very easy | 50% | 49% | 51% | — | |
| Note: Includes adults who either are currently covered by Medicaid or report that they have applied for the program within the past 5 years.”–“: Estimates with relative standard errors greater than 30% or cell sizes below 50 are not provided.Source: 2013 Kaiser Survey of Low-Income Americans and the ACA. | |||||
| Table A4: Reasons for and Problems with Choosing Health Plan, Among Adults who Had and Made a Choice, by Income | |||||
| All | By Income | ||||
| <138% FPL | 139-400% FPL | >400% FPL | |||
| Share who chose plan primarily because: | |||||
| Your costs under the plan were low | 29% | 21% | 30%^ | 31%^ | |
| The selection of health care providers was broad or included your doctor | 22% | 27% | 20% | 21% | |
| The plan covered a wide range of benefits or a specific benefit that you need | 32% | 31% | 30% | 34% | |
| Friends or family recommended the plan | 6% | 7% | 8% | — | |
| Other members of your family were already enrolled in this plan | 4% | 5% | 3% | — | |
| Some other reason | 6% | 7% | 8% | 5% | |
| Share of Insured Adults Reporting: | |||||
| Difficulty comparing services covered under each plan | 24% | 29% | 28% | 19%^ | |
| Difficulty comparing what costs would be under each plan | 17% | 17% | 20% | 16% | |
| Difficulty comparing the doctors, hospitals, and other health care providers you could see under each plan | 24% | 25% | 24% | 24% | |
| At least one aspect of plan choice to be difficult | 36% | 41% | 40% | 32% | |
| Note: Includes insured adults who had a choice of plans and reported that they made the choice themselves. Excludes those who responded Don’t Know or Refused.”–“: Estimates with relative standard errors greater than 30% or cell sizes below 50 are not provided.^ Estimate statistically significantly different from <138% FPL estimate at the 95% confidence level.Source: 2013 Kaiser Survey of Low-Income Americans and the ACA. | |||||
| Table A5: Problems with Health Coverage among Insured Adults, by Income and Coverage | |||
| Insured | |||
| Employer | Nongroup | Medicaid | |
| Rate Health Coverage as “Not so good” or “Poor” | |||
| All | 11% | 26%* | 16%* |
| By Income | |||
| <138% FPL | 16% | — | 16% |
| 139-400% FPL | 11% | 18% | — |
| >400% FPL | 9% | — | — |
| Needed Service Not Covered by Plan | |||
| All | 13% | 27%* | 26%* |
| By Income | |||
| <138% FPL | 18% | — | 26% |
| 139-400% FPL | 16% | 27% | 25% |
| >400% FPL | 11% | — | — |
| Plan Would Not Pay for Service You Thought Was Covered | |||
| All | 21% | 34%* | 34%* |
| By Income | |||
| <138% FPL | 29% | — | 32% |
| 139-400% FPL | 24% | 32% | 39% |
| >400% FPL | 18% | — | — |
| Costs You Had to Pay for a Service Were Higher Than Expected | |||
| All | 38% | 48%* | 22%* |
| By Income | |||
| <138% FPL | 36% | — | 21%* |
| 139-400% FPL | 38% | 48% | — |
| >400% FPL | 38% | 54%* | — |
| Notes: Excludes people covered by other sources, such as Medicare, VA/CHAMPUS, or other state programs.”–“: Estimates with relative standard errors greater than 30% or cell sizes below 50 are not provided.* Estimate statistically significantly different from employer estimate at the 95% confidence level.Source: 2013 Kaiser Survey of Low-Income Americans and the ACA. | |||
| Table A6: Knowledge of Coverage Pathways available under the ACA, by Income and Coverage | ||||||
| Uninsured^ | Insured | |||||
| Employer | Nongroup | Medicaid | ||||
| Know “only a little” or “nothing at all” about their state’s Medicaid program | ||||||
| All | 70% | 69% | 73%* | 46%* | ||
| By Income | ||||||
| <138% FPL | 70% | 64% | 65% | 46%* | ||
| 139-400% FPL | 67% | 71% | 75% | 47%* | ||
| >400% FPL | 84% | 68%* | 73% | — | ||
| Know “only a little” or “nothing at all” about the new Marketplaces | ||||||
| All | 82% | 63%* | 70%* | 79% | ||
| By Income | ||||||
| <138% FPL | 86% | 77%* | 69%* | 78% | ||
| 139-400% FPL | 80% | 71%* | 78% | 84% | ||
| >400% FPL | 73% | 55% | 62% | — | ||
| Notes: Excludes people covered by other sources, such as Medicare, VA/CHAMPUS, or other state programs.^ Uninsured excludes undocumented immigrants.”–“: Estimates with relative standard errors greater than 30% or cell sizes below 50 are not provided.* Estimate statistically significantly different from uninsured estimate at the 95% confidence level. Source: 2013 Kaiser Survey of Low-Income Americans and the ACA. | ||||||
Endnotes
- Kaiser Commission on Medicaid and the Uninsured. The Uninsured: A Primer- Key Facts about Health Insurance on the Eve of Coverage Expansions (Washington, DC: Kaiser Family Foundation), October 23, 2013. Available at: https://modern.kff.org/uninsured/report/the-uninsured-a-primer-key-facts-about-health-insurance-on-the-eve-of-coverage-expansions/ ↩︎
- Ibid. ↩︎
- Care without Coverage: Too Little, Too Late, Committee on the Consequences of Uninsurance, Board on Health Care Services, Institute of Medicine, National Academy Press, 2002 ↩︎
- J. Hadley, J. Holahan, T. Coughlin, and D. Miller, 2008 “Covering The Uninsured In 2008: Current Costs, Sources Of Payment, And Incremental Costs” Health Affairs 27 (5) w399 (published online 25 August 2008). ↩︎
- G. Anderson, 2007, “From ‘Soak The Rich’ To ‘Soak The Poor’: Recent Trends In Hospital Pricing.” Health Affairs 26(4): 780-789. ↩︎
- D. Himmelstein et al., 2009. “Medical bankruptcy in the United States, 2007: results of a national study.” Am J Med. 122(8): 741-6. Available at: http://www.pnhp.org/new_bankruptcy_study/Bankruptcy-2009.pdf ↩︎
- Some states had expanded coverage to parents at higher income levels or provided coverage to adults without children. See http://modern.kff.org/medicaid/fact-sheet/medicaid-eligibility-for-adults-as-of-january-1-2014/ for more detail on pre- and post-ACA Medicaid eligibility for adults. ↩︎
- Samantha Artiga and Jessica Stephens, Kaiser Commission on Medicaid and the Uninsured, Martha Heberlein, Tricia Brooks, and Joan Alker, Georgetown Center for Children and Families, Getting into Gear for 2014: Findings from a 50-State Survey of Eligibility, Enrollment, Renewal, and Cost-Sharing Policies in Medicaid and CHIP, 2012-2013, (Washington, DC: Kaiser Family Foundation), January 2013. Available at: http://modern.kff.org/medicaid/report/getting-into-gear-for-2014-findings-from-a-50-state-survey-of-eligibility-enrollment-renewal-and-cost-sharing-policies-in-medicaid-and-chip-2012-2013/ ↩︎
- Collins S, et al. 2012. “Gaps in Health Insurance: Why So Many Americans Experience Breaks in Coverage and How the Affordable Care Act Will Help.” The Commonwealth Fund. Available at: http://www.commonwealthfund.org/~/media/Files/Publications/Issue%20Brief/2012/Apr/1594_collins_gaps_in_hlt_ins_tracking_brief_v2.pdf; Cassedy A, Fairbrother G, and Newacheck PW. 2008. “The Impact of Insurance Instability on Children’s Access, Utilization, and Satisfaction with Health Care. Ambulatory Pediatrics. 8(5):321-8. ↩︎
- Artiga and Stephens, Getting into Gear. ↩︎
- Ibid. See http://modern.kff.org/medicaid/report/getting-into-gear-for-2014-shifting-new-medicaid-eligibility-and-enrollment-policies-into-drive/ for more detail. ↩︎
- Zhou, C. and Zhang, Y. (2012). The vast majority of Medicare Part D beneficiaries still don’t choose the cheapest plans that meet their medication needs. Health Affairs, 31: 2259-2264; McLaughlin, C.G., Chernew, M., & Taylor, E.F. (2002). Medigap premiums and Medicare HMO enrollment. Health Services Research 37: 1445-1468. ↩︎
- Kaiser Commission on Medicaid and the Uninsured. Oral Health and Low-Income Nonelderly Adults: A Review of Coverage and Access (Washington, DC: Kaiser Family Foundation), June 2012. Available at: http://modern.kff.org/medicaid/issue-brief/access-to-affordable-dental-care-gaps-for/ ↩︎
- Care without Coverage: Too Little, Too Late, Committee on the Consequences of Uninsurance, Board on Health Care Services, Institute of Medicine, National Academy Press, 2002. ↩︎
- Coverage Matters: Insurance and Health Care, Committee on the Consequences of Uninsurance, Board on Health Care Services, Institute of Medicine, National Academy Press, 2001. ↩︎
- Julia Paradise and Rachel Garfield, What is Medicaid’s Impact on Access to Care, Health Outcomes, and Quality of Care? Setting the Record Straight on Evidence (Washington, DC: Kaiser Commission on Medicaid and the Uninsured), August 2, 2013. Available at: https://modern.kff.org/medicaid/issue-brief/what-is-medicaids-impact-on-access-to-care-health-outcomes-and-quality-of-care-setting-the-record-straight-on-the-evidence. ↩︎
- Wilper AP, Woolhandler S, Lasser KE, McComick D, Bor DH, Himmelstein DU. Hypertension, diabetes, and elevated cholesterol among insured and uninsured US adults. Health Affairs. 2009;28(6):w1151-9. ↩︎
- Kaiser Commission on Medicaid and the Uninsured. Community Health Centers in an Era of Health Reform: An Overview and Key Challenges to Health Center Growth (Washington, DC: Kaiser Family Foundation), March 1, 2013. Available at: https://modern.kff.org/health-reform/issue-brief/community-health-centers-in-an-era-of-health-reform-overview/ ↩︎
- Kaiser Commission on Medicaid and the Uninsured. The Medicaid Medically Needy Program: Spending and Enrollment Update (Washington, DC: Kaiser Family Foundation), December 30, 2012. Available at: http://modern.kff.org/medicaid/issue-brief/the-medicaid-medically-needy-program-spending-and/ ↩︎
- Kaiser Commission on Medicaid and the Uninsured. Key Lessons from Medicaid and CHIP Outreach and Enrollment Under the Affordable Care Act (Washington, DC: Kaiser Family Foundation), June 2013. Available at: https://modern.kff.org/medicaid/issue-brief/key-lessons-from-medicaid-and-chip-for-outreach-and-enrollment-under-the-affordable-care-act/ ↩︎
- In this section, we exclude uninsured adults who are undocumented immigrants, as this group is ineligible for coverage under the law. See Methods for more detail on determining immigration status based on survey responses. ↩︎
- Kaiser Family Foundation Health Tracking Poll (conducted January 14-21, 2014); available at https://modern.kff.org/health-reform/poll-finding/kaiser-health-tracking-poll-january-2014/ ↩︎
- 45 C.F.R. § 156.1240 ↩︎
- “Health Centers to Help Uninsured Americans Gain Affordable Health Coverage,” Health and Human Services, July 10, 2013. Available at: http://www.hhs.gov/news/press/2013pres/07/20130710a.html ↩︎
- Kaiser Commission on Medicaid and the Uninsured. Fast Track to Coverage: Facilitating Enrollment of Eligible People into the Medicaid Expansion (Washington, DC: Kaiser Family Foundation), November 19, 2013. Available at: http://modern.kff.org/medicaid/issue-brief/fast-track-to-coverage-facilitating-enrollment-of-eligible-people-into-the-medicaid-expansion/ ↩︎
- Ibid. ↩︎
- Varney, Sarah. “Emergency Rooms Are Front Line For Enrolling New Obamacare Customers.” Kaiser Health News/NPR, January 14, 2014; available at: http://www.kffhealthnews.org/stories/2014/january/14/signing-up-for-obamacare-in-the-er.aspx. ↩︎
- Kaiser Commission on Medicaid and the Uninsured, The Coverage Gap: Uninsured Poor Adults in States that Do not Expand Medicaid (Washington, DC: Kaiser Family Foundation), October 23, 2013. Available at: https://modern.kff.org/health-reform/issue-brief/the-coverage-gap-uninsured-poor-adults-in-states-that-do-not-expand-medicaid/ ↩︎
- “Status of State Action on Medicaid Expansion Decision, 2014,” Kaiser Family Foundation State Health Facts. Retrieved January 29, 2014: http://modern.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/ ↩︎