California’s Previously Uninsured After The ACA’s Second Open Enrollment Period
Executive Summary
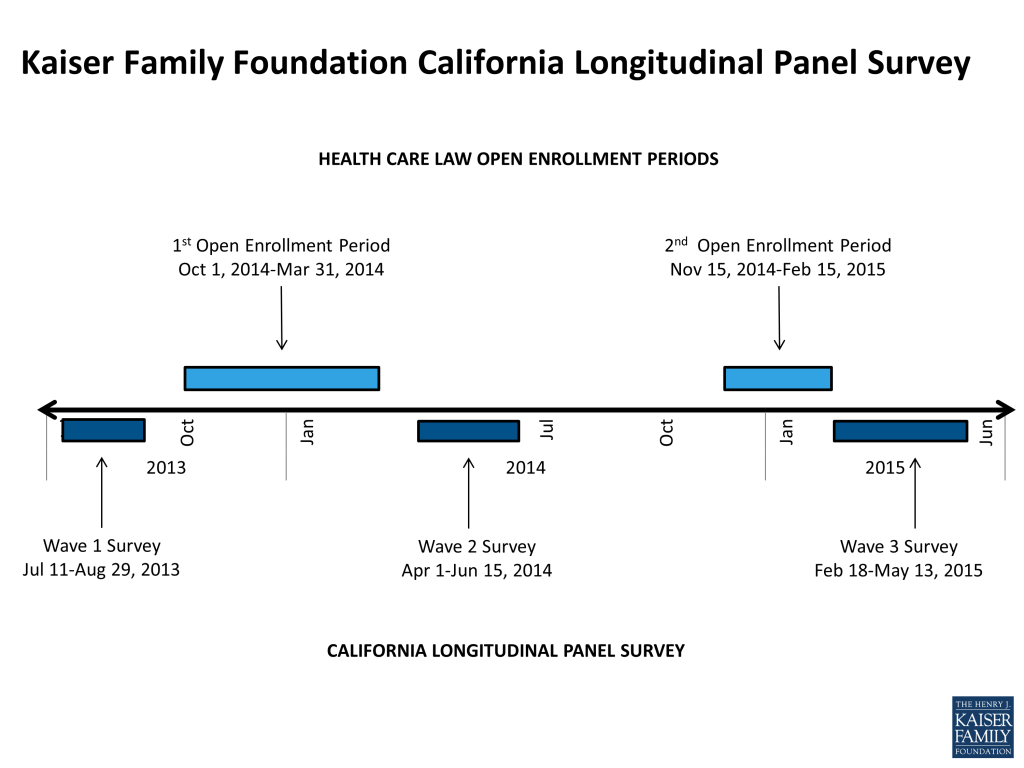
The Kaiser Family Foundation California Longitudinal Panel Survey is a series of surveys that, over time, tracks the experiences and views of a representative, randomly selected sample of Californians who were uninsured prior to the major coverage expansions under the Affordable Care Act (ACA). The initial baseline survey was conducted with a representative sample of 2,001 nonelderly uninsured Californian adults in summer 2013, prior to the ACA’s initial open enrollment period. After the first open enrollment period concluded in spring 2014, the second survey in the series followed up with the same group of previously uninsured Californians who participated in the baseline (a longitudinal panel survey). The third in the series, and the focus of this report, followed up with them again after the second open enrollment period in spring 2015 to find out whether more have gained coverage, lost coverage, or remained uninsured, what barriers to coverage remain, how those who now have insurance view their coverage, and to assess the impacts that gaining health insurance may have had on financial security and access to care. A fourth survey in the series will keep tracking these individuals as the expansions and changes in California continue under the ACA. The surveys are designed and analyzed by researchers at KFF and the fieldwork costs associated with the spring 2014 and spring 2015 surveys were paid for by The California Endowment.
This longitudinal panel study allows us to follow a large group of randomly selected uninsured Californians and assess how their insurance status changes over time to learn more about why those changes did or did not occurr, and what gaining health insurance means for their daily lives without having to rely on respondents ability to report and recall details from months or years ago. By tracking a scientifically representative panel, we can quantify how widespread or limited certain problems or changes that may have been reported anecdotally actually were. Statistically representative narratives and stories from individual’s actual experiences can then be drawn from the sample to illuminate more accurately how the uninsured fare as the law is implemented in California.
Key Findings
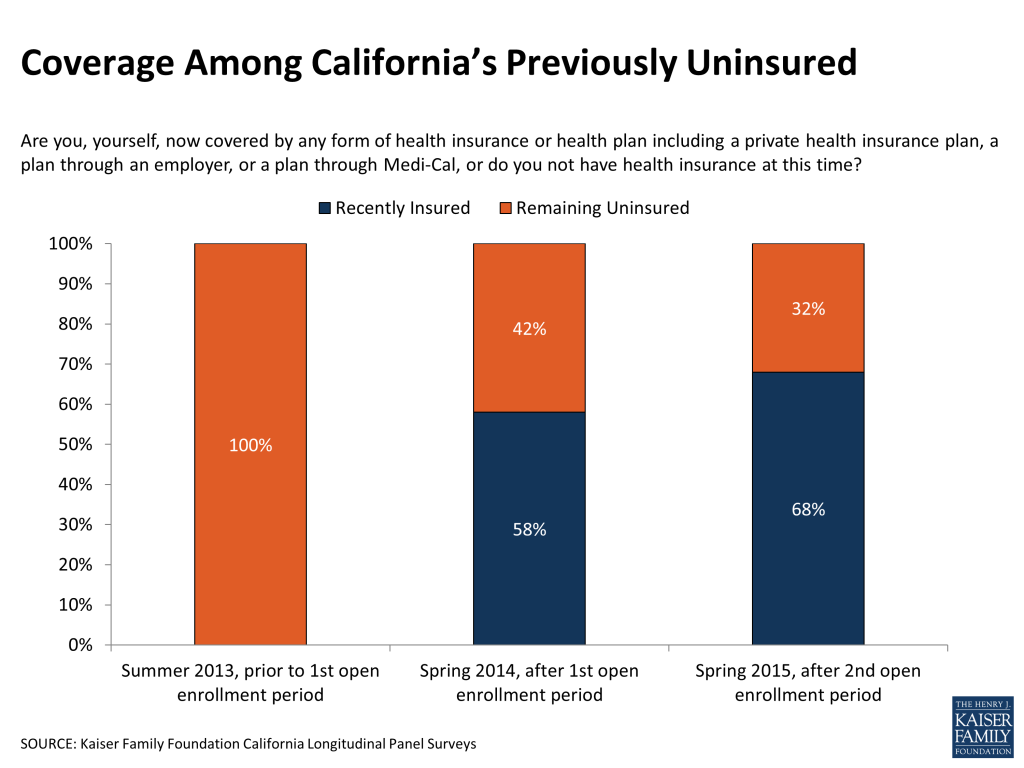
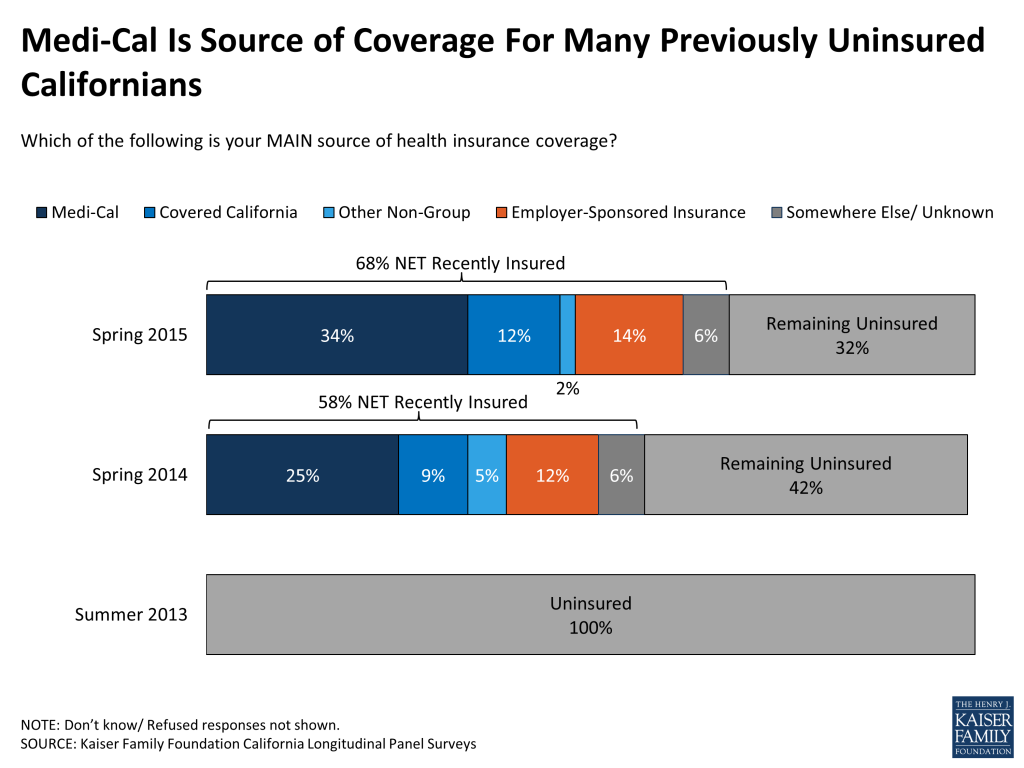
After two rounds of open enrollment under the Affordable Care Act, 68 percent of Californians who were uninsured prior to the first open enrollment period now report that they have health insurance, referred to in this report as the “recently insured.” This share is up from 58 percent after the first open enrollment period in the spring of 2014. The largest share of California’s previously uninsured, a third (34 percent), say they have coverage thought the state’s Medicaid program, Medi-Cal, up from 25 percent after the first open enrollment period. In addition, 14 percent say they are insured through an employer, 12 percent say they have a plan through Covered California, the state’s health insurance marketplace where people can shop for and compare health insurance plans and access federal subsidies for coverage, and another 7 percent say they have other non-group coverage or insurance through some other source. About a third (32 percent) report being currently uninsured, referred to in this report as the “remaining uninsured.” Because the same group of previously uninsured people has been followed over time, the survey is also able to explore the dynamics of health insurance and track how many people have moved in to or back out of coverage since the baseline survey in 2013.
Coverage Among Key Groups
Enrollment rates for whites and Hispanics are similar (79 percent for whites and 74 percent for eligible Hispanics) when excluding those Hispanics who are likely to be ineligible for financial assistance through Covered California or Medi-Cal due to their immigration status. In addition, just over half (53 percent) of those who say they’ve spent their lifetime without insurance now report having coverage, significantly lower than the more than 7 in 10 who said they had insurance at some point in the past who report gaining coverage since the health care law was implemented. Still, the gains in coverage among those who report never having coverage are notable.
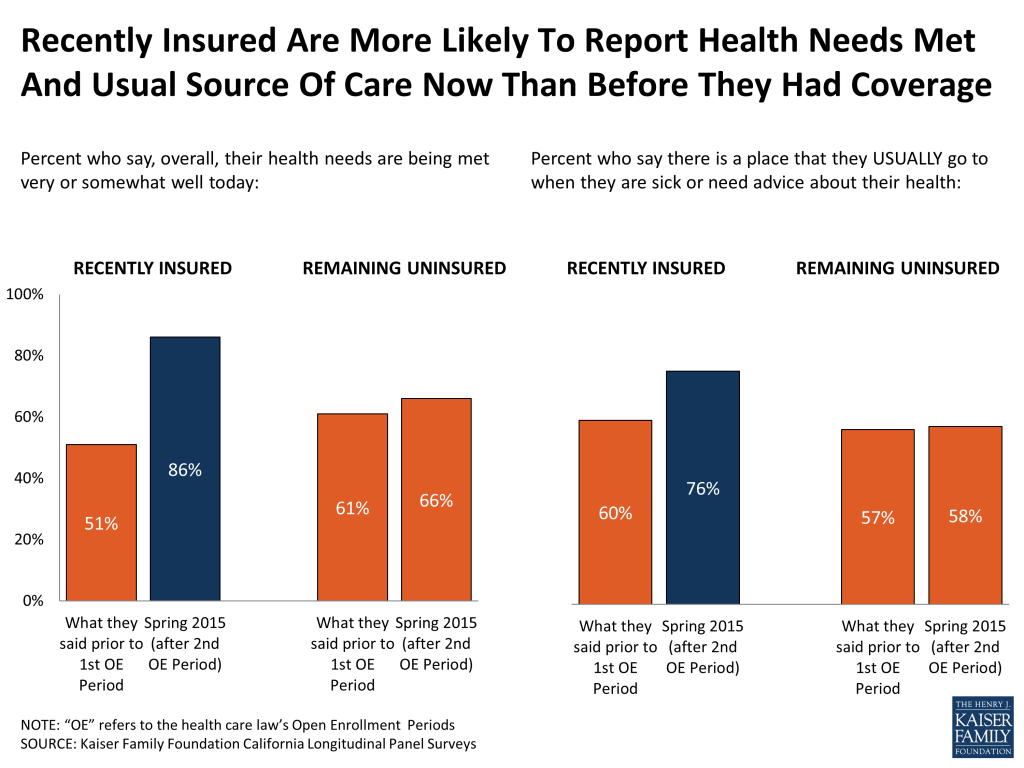
Gains In Financial Security And Health Needs Being Met For Recently Insured
The survey finds significant improvements in perceptions of health care affordability and access to care for the recently insured, but that affordability and access issues remain even for those who gained coverage. Those who have gained insurance are much less likely than they were in the baseline survey to report problems paying for medical bills in the past 12 months (23 percent now, compared to 45 percent in 2013) or difficulty affording health care (49 percent now, compared to 86 percent in 2013). They also are more likely to now report that their health needs are being met (86 percent now, compared to 51 percent in 2013) and that they now have a usual source of care to go to when they are sick or need medical advice (76 percent now, compared to 60 percent in 2013). For those who have remained uninsured, they report having difficulty affording care, problems paying for medical bills, their health needs being met, or having a usual source of care at similar rates as they did in the baseline survey.
Most Rate Plan Favorably, But Some Report Access Challenges
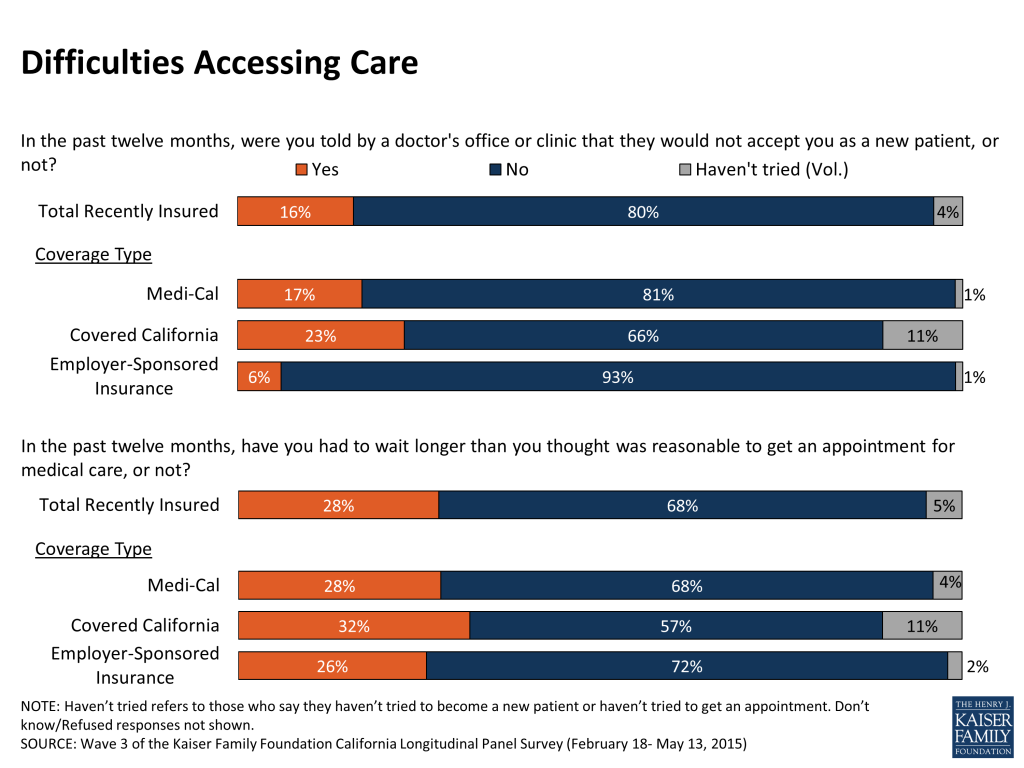
While most of California’s recently insured (76 percent) report positive experiences with their current plan and say they are satisfied with their plan’s choice of primary care doctors (79 percent), hospitals (75 percent), and specialists (67 percent), some say they have experienced problems accessing care in the past year. For example, 16 percent of the recently insured say they have been told by a doctor’s office in the past year that they would not accept them as a new patient and 28 percent say that within the past year they have had to wait longer than they thought was reasonable for a medical appointment.
Remaining Uninsured Are Largely Long-Term Uninsured Or Ineligible For ACA Coverage
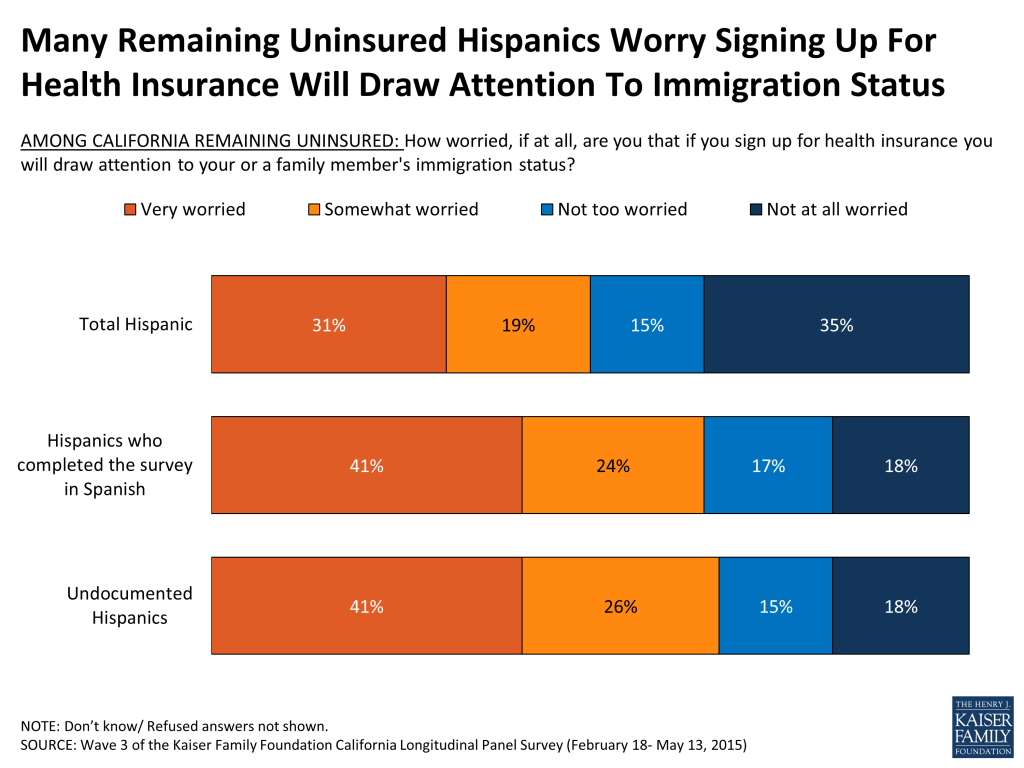
Many of California’s remaining uninsured have had little interaction with the health insurance system in the years prior to the ACA implementation. Four in 10 (41 percent) of the remaining uninsured are undocumented immigrants who are not eligible for Medi-Cal or assistance through Covered California and 43 percent are likely eligible for coverage but had been without coverage for two years or more or never had insurance as of the baseline survey. In addition, 70 percent of the remaining uninsured are Hispanic, including 41 percent who are Hispanic undocumented immigrants and 29 percent who are Hispanics likely eligible for coverage under the ACA. Immigration concerns may be a barrier for some Hispanics to enroll in coverage; half of remaining uninsured Hispanics report being worried that if they sign up for health insurance they will draw attention to their immigration status or that of a family member.
Key Findings: Introduction
This report is the latest in the California Longitudinal Panel Survey series examining how previously uninsured Californians navigate the health care system as the Affordable Care Act (ACA) goes into effect. Prior to the enactment of the health care law, California had the largest non-elderly uninsured adult population in the nation, at nearly 6 million.1 The state eagerly adopted options under the ACA to expand coverage to more low- and moderate-income people, primarily through the development of Covered California, the state’s marketplace where people can shop for and compare health plans and access financial help to purchase insurance, and by expanding eligibility for Medi-Cal, the state’s Medicaid program, to include parents and adults without dependent children earning 138% of the federal poverty level (FPL) or less (about $33,465 annually for a family of 4 in 2015). As an early adopter with large numbers of uninsured, California is a particularly valuable place to track how the rollout of the health care law has impacted the state’s uninsured, and its progress and challenges can help inform future enrollment efforts state-wide and nationally.
To track the experiences and perceptions of California’s uninsured as the ACA is implemented, the Kaiser Family Foundation is conducting the California Longitudinal Panel Survey series, following the same group of randomly selected Californians over time who were uninsured prior to the major coverage expansions under the ACA. The initial baseline survey was conducted with a representative sample of 2,001 nonelderly uninsured Californian adults in summer 2013, prior to the ACA’s initial open enrollment period.2 It found that most of the state’s uninsured said they wanted insurance but that most didn’t think they could afford it, as the vast majority reported family incomes under 400% FPL (about $94,000 a year for a family of 4 in 2013). At that time, the first open enrollment period under the ACA was just a couple months away and many of California’s uninsured were unaware of the upcoming coverage expansion opportunities and were unsure of how the law would impact them.
After the first open enrollment concluded in spring 2014, the second survey in the series followed up with the same group of previously uninsured Californians to find out whether they gained coverage or remained uninsured, how they felt about and interacted with the new coverage options, and what barriers to getting insurance remained.3 Many (58 percent) of California’s previously uninsured reported having health insurance at the close of the first open enrollment period. Most reported that shopping for coverage went smoothly, however some expressed difficulty affording the cost of coverage. Still, about 4 in 10 remained uninsured, despite the fact that many reported incomes that put them in the group likely eligible for Medi-Cal or for financial assistance through Covered California.
The third survey in the series, and the focus this report, returns to the same group of previously uninsured Californians a year later, after the second open enrollment period, to determine whether more of them had gained coverage, if some had moved out of coverage and back to being uninsured, and what their ongoing experience has been with their health insurance or the health care system more generally.
One additional survey in the series will continue to track these individuals as the expansions and changes in California under the ACA become the status quo as time passes. While the surveys are generally timed around the ACA’s open enrollment periods, it is important to note that eligible individuals are able to enroll in Medi-Cal year round.
California has made considerable strides in enrolling eligible low- and moderate-income people in new coverage options under the ACA. During the first open enrollment period, about 1.6 million people enrolled in Medi-Cal and 1.4 million people enrolled in Covered California.4 During the second open enrollment period, many renewed their coverage and nearly 500,000 new enrollees signed up for plans through Covered California and more than 780,000 signed up for Medi-Cal.5 By following a representative group of Californians who were uninsured prior to the ACA’s coverage expansions, a key target of the ACA, we can better understand how these new coverage opportunities have impacted this group’s ability to access coverage and gain insight into their interactions with these new pathways to coverage.
While the ACA makes it easier for some people to get and keep coverage, other people will move in and out of coverage due to job status changes, shifts in income that change their eligibility for public subsidies or coverage, or missed deadlines for enrollment. While many previously uninsured Californians now have insurance, other Californians who had insurance prior to the ACA’s coverage expansions may now be uninsured, a group whose experiences and movements within the health care system are not captured in this series of surveys. As a result, this survey does not estimate the overall change in the number of uninsured Californians since the start of open enrollment, but instead estimates the share of previously uninsured who gained coverage.
Key Findings: Section 1: Coverage Gains Among The Previously Uninsured
Enrollment
After two rounds of open enrollment under the Affordable Care Act, 68 percent of Californians who were uninsured prior to the first open enrollment period now report that they have health insurance, up from 58 percent after the first open enrollment period in the spring of 2014. About a third (32 percent) report being currently uninsured, a group referred to throughout this report as the “remaining uninsured;” this share is down from 42 percent in the spring of 2014. Excluding those who are likely ineligible for coverage under the ACA due to their immigration status,6 77 percent of California’s eligible remaining uninsured now reports having coverage.
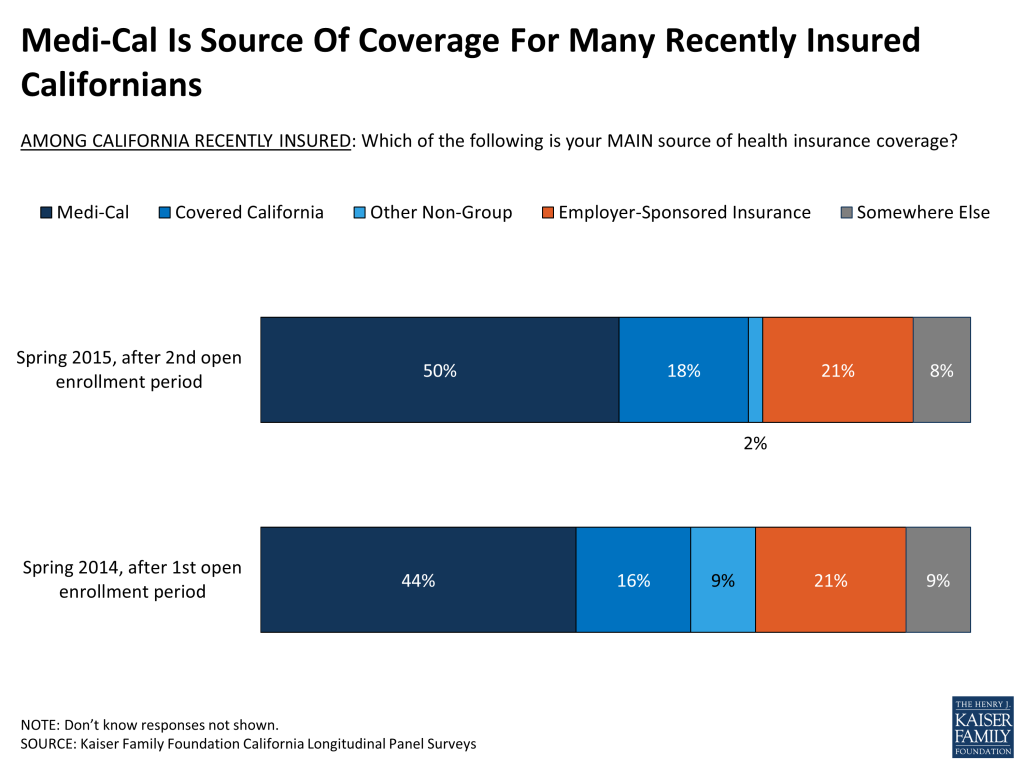
Those previously uninsured Californians who now report after the second open enrollment period that they have health insurance (68 percent), referred to throughout this report as “California’s recently insured,” say they gained coverage from several different sources. The largest share of California’s previously uninsured, a third (34 percent), say they have coverage through the state’s Medicaid program, Medi-Cal, up from 25 percent after the first open enrollment period. In addition, 14 percent currently say they are insured through an employer, 12 percent say they have a plan through Covered California, the state’s health insurance marketplace where people can shop for and compare health insurance plans and access federal subsidies for coverage, and another 7 percent say they have other non-group coverage or insurance through some other source.7
Who Now Has Coverage?
Because Latinos made up over half of the uninsured adult population prior to the ACA’s coverage expansions, particular attention has been paid to enrollment among this group. Currently, roughly 6 in 10 (59 percent) Hispanics who were uninsured prior to the first open enrollment period in summer 2013 report now having coverage, much lower than the 79 percent of previously uninsured whites who say they are insured. However, excluding the 1 in 3 previously uninsured Latinos who are likely to be ineligible for financial assistance through Covered California or Medi-Cal due to their immigration status,8 74 percent of eligible Latinos say they now have coverage, a share nearly equivalent to that for whites.

In addition, similar shares of many other demographic groups now report having coverage, such as men and women, people of different ages and people of different employment status. However, some groups have made particular gains in coverage or lagged somewhat behind. For example, previously uninsured people who report being in good health are more likely to say they have coverage than those who report being in fair or poor health (71 percent vs. 62 percent). In contrast, those who report having a debilitating chronic disease that keeps them from fully participating in work or other activities are more likely to say they have coverage now than those without significant chronic disease (78 percent vs. 66 percent). Just over half (53 percent) of those who say they’ve spent their lifetime without insurance now report having coverage, significantly lower than the more than 7 in 10 who said they had insurance at some point in the past who report gaining coverage since the health care law was implemented. Still, the gains in coverage among those who report never having coverage are notable. (Table 1)
| Table 1: Percentage Of Each Group Of Previously Uninsured Reporting That They Are Recently Insured Or Remain Uninsured | |||||||
| TOTAL RECENTLY INSURED IN 2015 | COVERAGE TYPE IN 2015 | TOTAL REMAINING UNINSURED IN 2015 | |||||
| Medi-Cal | Covered California | Other Non-Group | Employer-Sponsored Insurance | ||||
| TOTAL | 68% | 34% | 12% | 2% | 14% | 32% | |
| AGE | 19-34 | 68% | 32% | 11% | 1% | 20% | 32% |
| 35-49 | 62% | 33% | 11% | 2% | 12% | 38% | |
| 50-64 | 71% | 37% | 17% | 2% | 10% | 28% | |
| RACE | White non-Hispanic | 79% | 29% | 21% | 2% | 20% | 21% |
| Hispanic (NET) | 59% | 31% | 7% | 2% | 13% | 41% | |
| Hispanic, Eligible | 74% | 41% | 10% | 2% | 16% | 25% | |
| GENDER | Male | 65% | 28% | 10% | 2% | 18% | 35% |
| Female | 71% | 40% | 15% | 1% | 11% | 29% | |
| LENGTH OF TIME UNINSURED PRIOR TO ACA | 2mo – <1 year | 75% | 32% | 16% | 2% | 22% | 25% |
| 1 year to <2 years | 74% | 47% | 7% | 1% | 15% | 26% | |
| 2 or more years | 72% | 35% | 15% | 2% | 13% | 27% | |
| Never had insurance | 53% | 26% | 9% | 1% | 13% | 47% | |
| EMPLOYMENT | Employed | 65% | 26% | 15% | 1% | 20% | 34% |
| Unemployed | 74% | 47% | 7% | 3% | 5% | 26% | |
| A student, retired, on disability, or stay at home parent | 70% | 45% | 10% | 2% | 5% | 30% | |
| EDUCATION | High school or less | 61% | 37% | 8% | 1% | 11% | 39% |
| Some college | 75% | 34% | 15% | 1% | 18% | 25% | |
| College or more | 82% | 20% | 28% | 3% | 23% | 18% | |
| HEALTH STATUS | Excellent/ Very good/ Good | 71% | 33% | 15% | 2% | 15% | 29% |
| Fair/ Poor | 62% | 34% | 7% | 1% | 13% | 38% | |
| MARITAL STATUS | Married | 69% | 31% | 13% | 2% | 18% | 30% |
| Not married | 67% | 35% | 12% | 1% | 12% | 33% | |
| FAMILY INCOME | Less than 138% FPL | 65% | 48% | 6% | <1% | 7% | 34% |
| Between 138% – 400% FPL | 71% | 18% | 21% | 3% | 21% | 29% | |
| DEBILITATING CHRONIC CONDITION | Yes | 78% | 43% | 14% | 2% | 11% | 21% |
| No | 66% | 32% | 12% | 1% | 15% | 34% | |
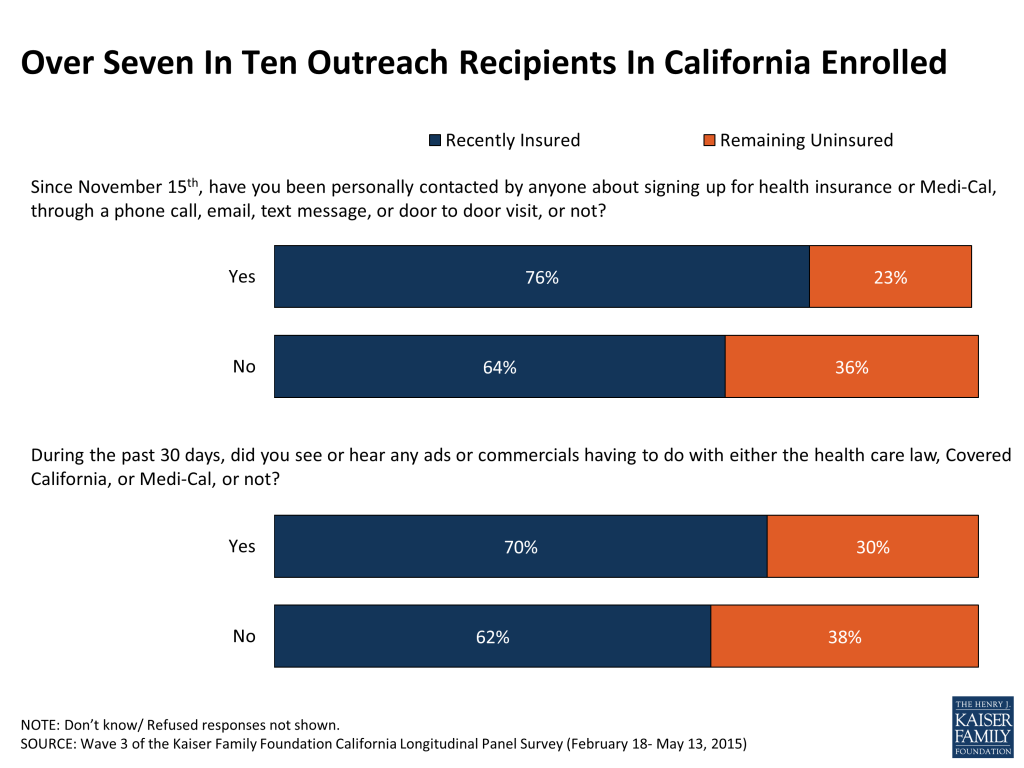
Being contacted by phone, email or a door-to-door visit about signing up for health insurance appears to have played a role in some of California’s previously uninsured gaining or keeping coverage. Three-quarters (76 percent) of those who say they were personally contacted since November 15th say they now have coverage, compared to 64 percent of those who report that they were not contacted. At the same time, there is no statistical difference in gains in coverage for those who report seeing commercials in the past 30 days having to do with the health care law, Covered California or Medi-Cal and those who say they didn’t see such ads (70 percent vs. 62 percent).
Many of these factors tend to be interconnected so in order to isolate which personal elements best predict who of California’s previously uninsured now has coverage, we conducted a regression analysis with demographic factors and outreach indicators. This analysis showed two factors mattered most. Previously uninsured Californians who say they are still uninsured are more likely to be undocumented immigrants or say they never had insurance, even after accounting for a variety of other demographic factors such as age, race/ethnicity, sex, and education.9
Views Of ACA’s Personal Impact Vary By Coverage Status And Type
Previously uninsured Californians vary in their opinion of the ACA’s impact on their lives. Large shares say the law has had no direct impact on them or their families; however, not surprisingly, the remaining uninsured are more likely to hold this view than those who have recently gained insurance in the two years since the law was implemented (66 percent vs. 44 percent). Additionally, those with recent insurance are more likely to say the ACA has helped them (41 percent) than hurt them (14 percent), while those who remain uninsured are more likely to say the law has hurt them rather than helped them (22 percent vs. 8 percent).
Among the recently insured, perceptions of the ACA’s personal impact vary by plan type. Those who report receiving coverage through Covered California and Medi-Cal are more likely to say the law has helped them than those who report having employer-sponsored insurance. About 6 in 10 (62 percent) of those enrolled through Covered California and about 4 in 10 (43 percent) of those with Medi-Cal coverage say the law has helped them. Most with recent coverage through an employer say they have felt no direct impact (59 percent), and for those who have, they are evenly divided on whether they have been helped or hurt (20 percent vs. 21 percent).

Dynamics In Enrollment And Coverage
People tend to move in and out of coverage as their income, employment status and other life factors change, particularly those with lower-incomes or recent experience being uninsured. One of the primary advantages of a longitudinal panel survey is the ability to examine these movements by following the same group of people over time.
Many (50 percent) Californians who reported being uninsured prior to the ACA’s first open enrollment period, reported gaining insurance in the spring 2014, after the first open enrollment period, and also now say they have coverage after the second open enrollment period in spring 2015, referred to here as those “still insured.”10 While these people may have fluctuated in and out of coverage or changed plans over the course of the year, they are not necessarily new to health insurance. Another 19 percent of California’s previously uninsured are more likely to be new to their coverage because they reported being uninsured after the first open enrollment period in the spring of 2014. This group is referred to here as the “newly insured.”11
In addition, 23 percent of people reported being uninsured after both open enrollment periods and another 8 percent said they had coverage after the first open enrollment period but now say they are without health insurance. These groups combined are referred to here as the “remaining uninsured.”

These groups are worth a closer look to better understand who took longer to gain coverage, who went back to being uninsured, who remains without coverage, and who continues to report having coverage. Majorities of the remaining uninsured (69 percent) are Hispanic, compared to 43 percent of those still insured. In addition, the newly insured (59 percent) are more likely to be men than those still insured (44 percent). A striking 40 percent of the remaining uninsured said during the baseline survey prior to the ACA’s first open enrollment period that they have never had insurance, while smaller shares of the newly insured (23 percent) and the still insured (18 percent) say they have never had coverage. Those who are still insured (19 percent) are more likely to say they have a debilitating chronic condition than the newly insured (10 percent) or remaining uninsured (9 percent). (Table 2)
| Table 2: Demographics Of Each Group Of Previously Uninsured Californians* | ||||
| NEWLY INSURED IN 2015 (19%) | STILL INSURED IN 2015 (50%) | REMAINING UNINSURED IN 2015 (31%) | ||
| AGE | 19-34 | 32% | 39% | 34% |
| 35-49 | 34% | 26% | 40% | |
| 50-64 | 30% | 31% | 24% | |
| 65+ | 4% | 4% | 1% | |
| RACE | White non-Hispanic | 34% | 34% | 20% |
| Black non-Hispanic | 9% | 6% | 3% | |
| Other non-Hispanic | 2% | 16% | 7% | |
| Hispanic | 53% | 43% | 69% | |
| Hispanic, eligible | 42% | 37% | 26% | |
| Hispanic, undocumented | 11% | 6% | 41% | |
| GENDER | Male | 59% | 44% | 53% |
| Female | 41% | 56% | 47% | |
| LENGTH OF TIME UNINSURED PRIOR TO ACA | 2 months to less than a year | 8% | 18% | 9% |
| 1 year to less than 2 years | 15% | 18% | 11% | |
| 2 years or more | 53% | 46% | 41% | |
| Never had insurance | 23% | 18% | 40% | |
| EMPLOYMENT | Employed | 68% | 56% | 63% |
| Unemployed | 13% | 15% | 14% | |
| A student, retired, on disability, or stay at home parent | 19% | 29% | 23% | |
| EDUCATION | High school or less | 53% | 47% | 70% |
| Some college | 37% | 33% | 23% | |
| College or more | 10% | 19% | 6% | |
| HEALTH STATUS | Excellent/ Very good/ Good | 59% | 69% | 61% |
| Fair/ Poor | 41% | 31% | 39% | |
| MARITAL STATUS | Married | 41% | 38% | 37% |
| Not married | 59% | 62% | 62% | |
| FAMILY INCOME | Less than 138% FPL | 56% | 54% | 61% |
| Between 138% – 400% FPL | 40% | 39% | 34% | |
| Over 400% FPL | 4% | 6% | 5% | |
| DEBILITATING CHRONIC CONDITION | Yes | 10% | 19% | 9% |
| No | 90% | 79% | 90% | |
| SAW OR HEARD ANY ADS | Yes, saw or heard ads | 70% | 70% | 61% |
| No, did not see or hear ads | 30% | 30% | 39% | |
| PERSONALLY CONTACTED | Yes, been contacted | 26% | 34% | 19% |
| No, have not been contacted | 74% | 66% | 81% | |
| *Based on those who completed the survey in spring 2014 and spring 2015, after each open enrollment period. | ||||
Key Findings: Section 2: Financial Security, Access To Care, And Health Insurance
Problems Paying Bills And Affording Care
Having health insurance appears to have eased some of the financial burden for previously uninsured Californians. About half (49 percent) of those who report now having coverage after the second open enrollment period say it is difficult to afford health care, while 86 percent of them said the same thing when they were uninsured in summer 2013, prior to the first open enrollment period. For those who have remained uninsured, there has been no substantial change in the large majority who say they have a difficult time affording care (85 percent vs. 81 percent in summer 2013). Additionally, those who report having health insurance now are about half as likely to say they have had problems paying medical bills in the past year than they did when they were uninsured in summer 2013 (23 percent vs. 45 percent) and that these bills have had a major financial impact (11 percent vs. 27 percent).

For those who report currently having health insurance in spring 2015 after the second open enrollment period, affording health care falls among one of several household expenses people say they have difficulty affording. But, for those who remain uninsured, health care is the most frequently cited burdensome household expense, with over 8 in 10 (85 percent) saying it is at least somewhat difficult to afford.

Even with some saying coverage is difficult to afford, overall, about half (53 percent) of previously uninsured Californians who have recently gained coverage say that having health insurance makes them feel more financially secure. Just over a third (36 percent) say it doesn’t make much of a difference, and a smaller share (10 percent) say it makes them feel less financially secure. In addition, most (62 percent) of those now with insurance say they feel well-protected by their health insurance, but a third say they feel vulnerable to medical bills.

While many who have recently gained insurance report feeling more financially secure as a result of their coverage, a quarter of the recently insured report forgoing needed medical care in the past year due to cost, similar to the share of those remaining without insurance (31 percent). These shares may be similar due to the fact that most of California’s previously uninsured are lower income and face general affordability challenges. Further, some recently insured say they don’t understand the health care services their plan provides or what they have to pay to use services. Those recently insured who report not understanding their health insurance are more likely to report forgoing care than those who say they understand their health insurance at least somewhat well.
| Table 3: Understanding Of Health Insurance And Likelihood Of Forgoing Medical Care | ||||||||
| REMAINING UNINSURED | RECENTLY INSURED | |||||||
| Total Recently Insured | Understand Coverage Somewhat/ Very Well (64%) | Understand Coverage Not Too/ Not At All Well (35%) | Understand Cost Somewhat/ Very Well (71%) | Understand Cost Not Too/ Not At All Well (27%) | ||||
| Was there a time over the past twelve months when you needed medical care, but did not get it because of the cost, or not? | ||||||||
| Yes | 31% | 25% | 18% | 37% | 19% | 40% | ||
| No | 69% | 75% | 82% | 63% | 81% | 60% | ||
Changes In Reports Of Health Needs Being Met Or Having A Usual Source Of Care
In addition to feeling less financial burden from health costs, those who say they have gained insurance recently are also more likely to report that their health needs are being met now that they have insurance compared to when they were uninsured – nearly 9 in 10 (86 percent) now versus about half (51 percent) in the baseline survey in the summer of 2013 prior to the first open enrollment period. Among those without coverage, there has been no statistical change in reports of how well their health needs are being met.
Those who recently gained insurance are also now more likely to say they have a usual source of care than before they had coverage (76 percent, compared to 60 percent in summer 2013).
Key Findings: Section 3: Previously Uninsured Now With Coverage
Source of Coverage
Like last year, the primary source of coverage for California’s previously uninsured who now have insurance continues to be Medi-Cal, with half reporting they have coverage through the state’s Medicaid program. About 2 in 10 (21 percent) of those now with insurance say they are enrolled in a plan through an employer or through Covered California (18 percent). The combined enrollment in Medi-Cal and Covered California shows that at the end of the second enrollment period about two-thirds (68 percent) of California’s recently insured have coverage through these ACA-related coverage options.
Gaps In Coverage And Plan Changes
As noted above, although people report having health insurance at a point in time, they may experience gaps in coverage during periods of transitions such as gaining or losing coverage through an employer or during changes in income and eligibility. Nearly 6 in 10 (58 percent) of the recently insured say they had health insurance for all of the last 12 months, but about 4 in 10 (42 percent) say they went without coverage at some point in the past year.
People also may move from one type of insurance or health plan to another over the course of the year as their access to coverage through an employer changes or their eligibility changes as their income fluctuates. About 6 in 10 (63 percent) of the recently insured say they stayed with the same plan they had in 2014, while about a fifth (17 percent) say they changed to a different plan. Another 20 percent say they didn’t have coverage last year.
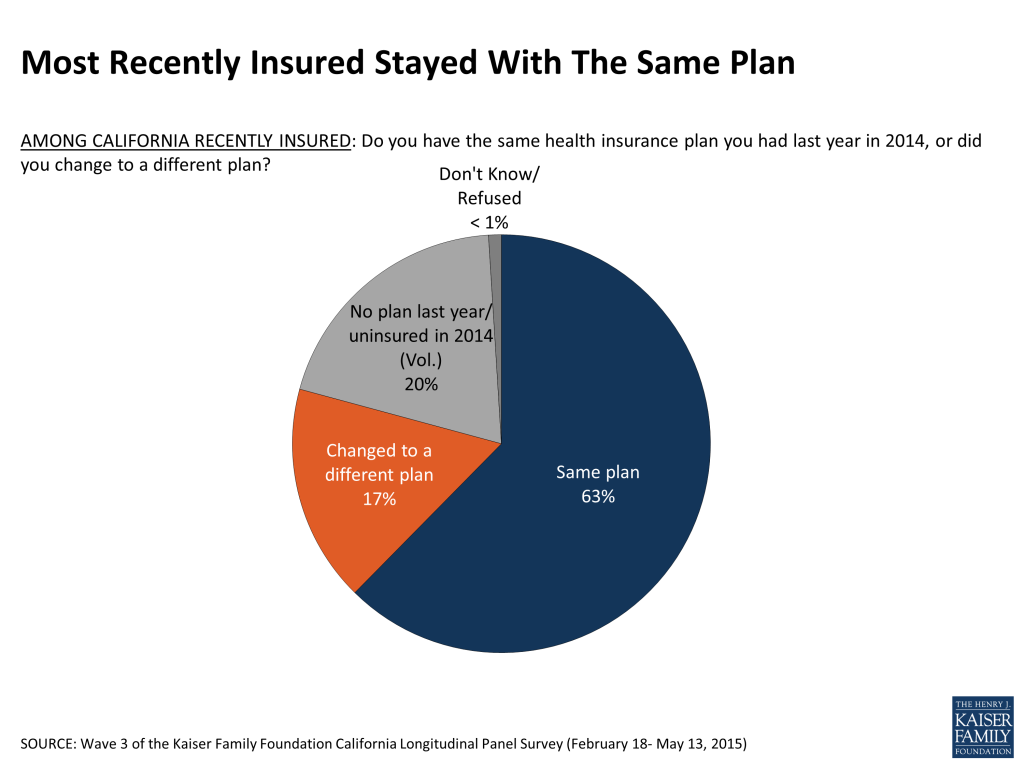
Most of the recently insured who changed plans said it was easy to do (75 percent, or 12 percent of those with insurance). People report changing plans for a number of reasons, such as a change in income (8 percent), wanting a plan with more choice of providers or a plan that covered a specific provider (7 percent), and a change in personal or family health needs (5 percent).

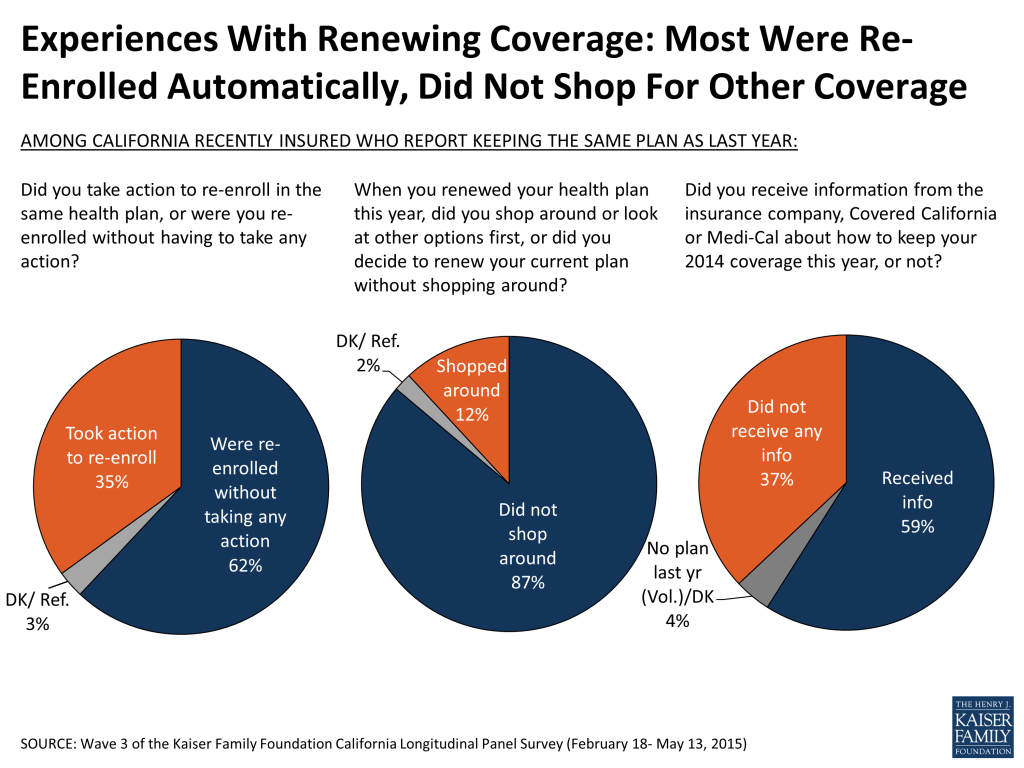
For those recently insured who report staying with the same plan this year (63 percent), most say they were re-enrolled without having to take any action (62 percent, or 39 percent of the insured overall). About a third of those who report staying with the same plan (35 percent, 22 percent of the insured overall) took action to re-enroll. A large majority of those who stayed with the same plan (87 percent, or 54 percent of the insured overall) say they didn’t shop around for other options before keeping their same insurance plan, but a few say they did (12 percent, or 7 percent of the insured overall). In addition, 6 in 10 of those who say they kept the same plan (59 percent, 36 percent of the insured overall) say they received information from an insurance company, Covered California or Medi-Cal about how to keep their plan.
Plan Costs And Affordability
About half (49 percent) of the recently insured say their plan cost about what they expected. Roughly a third (32 percent) of those with Medi-Cal coverage and about a quarter (27 percent) of those with a Covered California plan say their plan cost less than expected, while 13 percent of those with employer-sponsored coverage say the same.

Many previously uninsured Californians have incomes that qualify them for financial assistance from the government to help pay for insurance. Nine in 10 of previously uninsured people who say they have coverage through Covered California (91 percent) report that they are getting financial assistance or that their premium is based on income. The vast majority (88 percent) of those receiving financial assistance say they would not be able to afford insurance without it. Still, about half (52 percent) of the previously uninsured now with a Covered California plan say that it is at least somewhat difficult to afford the cost of health insurance each month; a share similar to those now with coverage through an employer (58 percent).
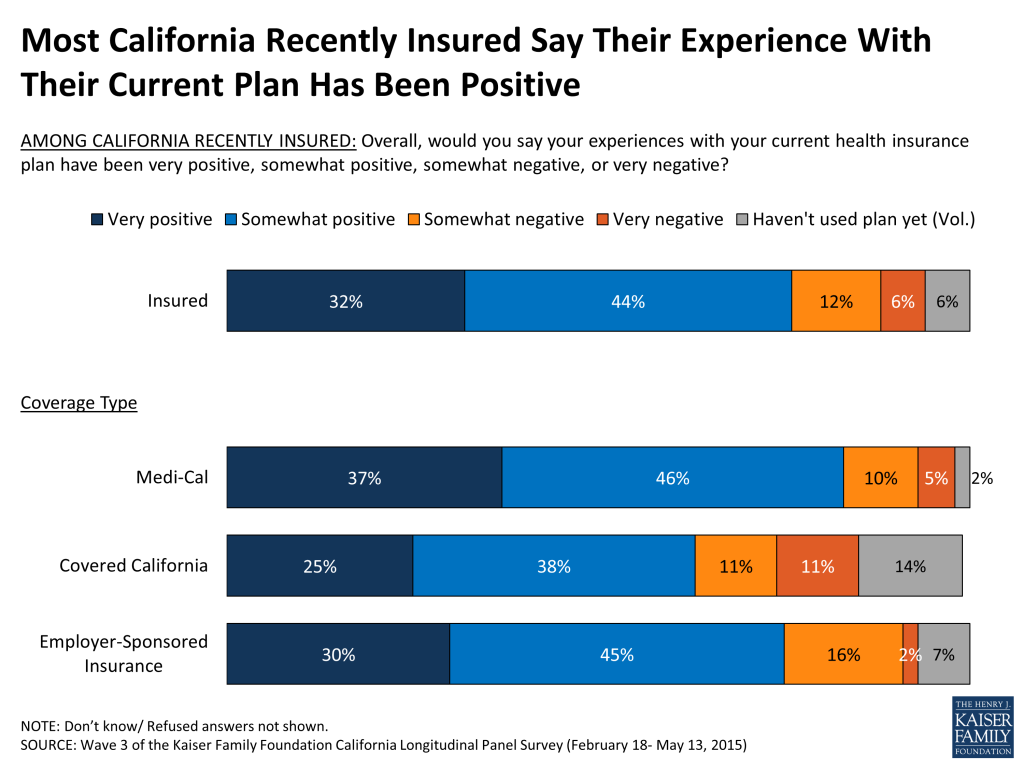
Perceptions Of Current Plan
Large majorities of those who report having insurance after the second open enrollment period say their experiences with their current health plan have been positive, including about 8 in 10 (83 percent) Medi-Cal enrollees and about 6 in 10 (63 percent) Covered California enrollees.
The recently insured are largely satisfied with their plan’s choice of primary care doctors (79 percent), hospitals (75 percent), and specialists (67 percent), a finding that is consistent across plan types; however some say that they have experienced problems accessing care in the past 12 months. For example, 16 percent of the recently insured say they have been told by a doctor’s office in the past 12 months that they would not accept them as a new patient. Higher shares of those with Medi-Cal (17 percent) or plans through Covered California (23 percent) say they’ve been turned away by a doctor’s office or clinic than those with employer coverage (6 percent). About 3 in 10 (28 percent) of the recently insured say they have had to wait longer than they thought was reasonable for an appointment for medical care. It is possible that some experienced these issues prior to enrolling in their current coverage. Still, the majority of the recently insured (72 percent) say they have visited a doctor in the past 12 months, significantly higher than the 4 in 10 (40 percent) who are uninsured.
Key Findings: Section 4: The Remaining Uninsured
Who Is Remaining Uninsured?
Although many previously uninsured Californians gained coverage in the nearly two years since the health care law went into effect, 32 percent report that they do not currently have health insurance. Many of these remaining uninsured had little interaction with the health insurance system in the years prior to the ACA implementation. Nearly 4 in 10 of the remaining uninsured reported in the baseline survey that they had been without health insurance for two or more years (38 percent), and an additional 4 in 10 (40 percent) said they have never had insurance. Hispanics make up 70 percent of the remaining uninsured and over half of them (41 percent) report being undocumented immigrants who are not eligible for Medi-Cal or assistance through Covered California, although state lawmakers are considering expanding eligibility to this group. Many report a family income that makes them likely eligible for Medi-Cal (26 percent) or for financial assistance through Covered California (25 percent), while 41 percent report being undocumented and therefore are ineligible.12

Why Don’t They Have Insurance?
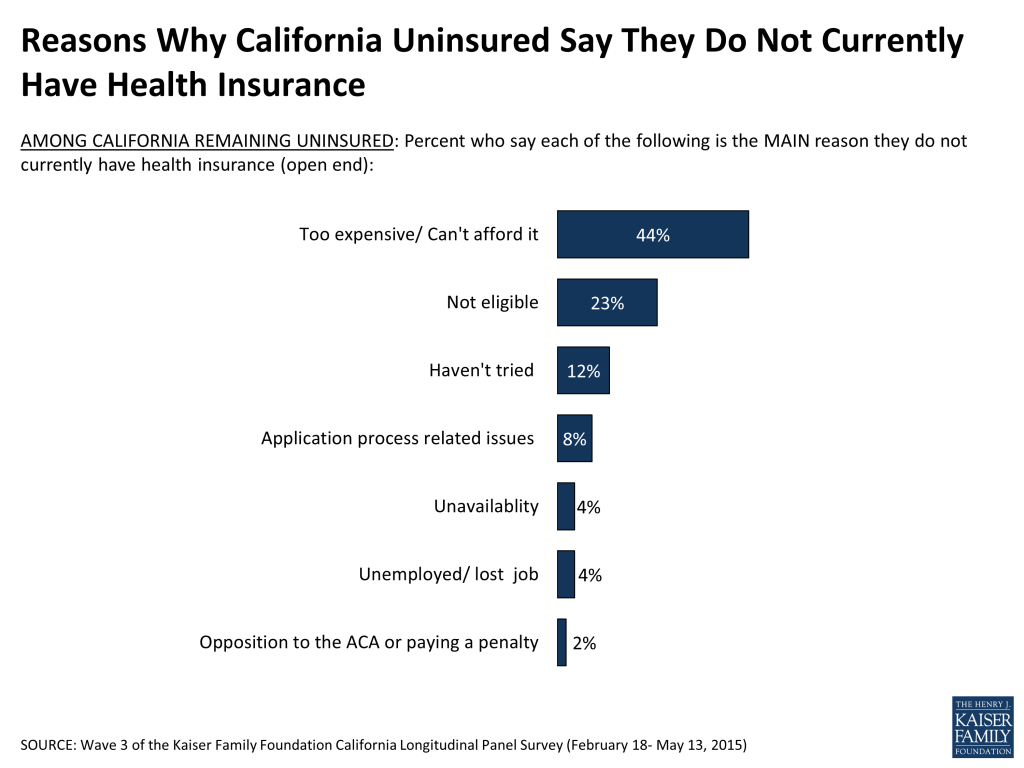
When asked to say in their own words the main reason why they do not currently have health insurance, 44 percent of California’s remaining uninsured say it is because health insurance is too expensive and they can’t afford it. Affordability is by far the most common reason named for lacking health insurance, followed by eligibility reasons (23 percent), such as immigration concerns (15 percent) or the fact that they are ineligible for Medi-Cal or government help (7 percent). About 1 in 10 (12 percent) say they haven’t tried, they don’t need insurance, or they just haven’t gotten around to it, and fewer than 1 in 10 (8 percent) name application process related issues as the main reason. Small shares say other reasons such as unavailability (4 percent), including that their employer doesn’t offer coverage (1 percent) or their plan was cancelled (3 percent), unemployment (4 percent), and opposition to the health care law (2 percent). The shares naming these reasons for not currently having health insurance are similar to those for the remaining uninsured last spring, after the first open enrollment period.
Did They Try To Get Insurance?
Just over a third (37 percent) of California’s remaining uninsured say they tried to get health insurance in the past 6 months. Two in 10 of them (20 percent) say they attempted to get coverage from Covered California and the same share report attempting to get coverage through Medi-Cal. Fewer say they attempted to get coverage through a broker (11 percent), directly from a private insurance company (10 percent), or through an employer (7 percent).

Those who tried but did not gain health insurance point to cost as a main reason they were unsuccessful. A quarter (26 percent) of California’s remaining uninsured say they tried but didn’t get insurance because it was too expensive, including 14 percent who say they shopped for health insurance and 12 percent who say they didn’t bother shopping because they didn’t think they could afford it. Another 13 percent say they weren’t eligible for coverage, and 1 in 10 (9 percent) say they were not able to complete the application process.

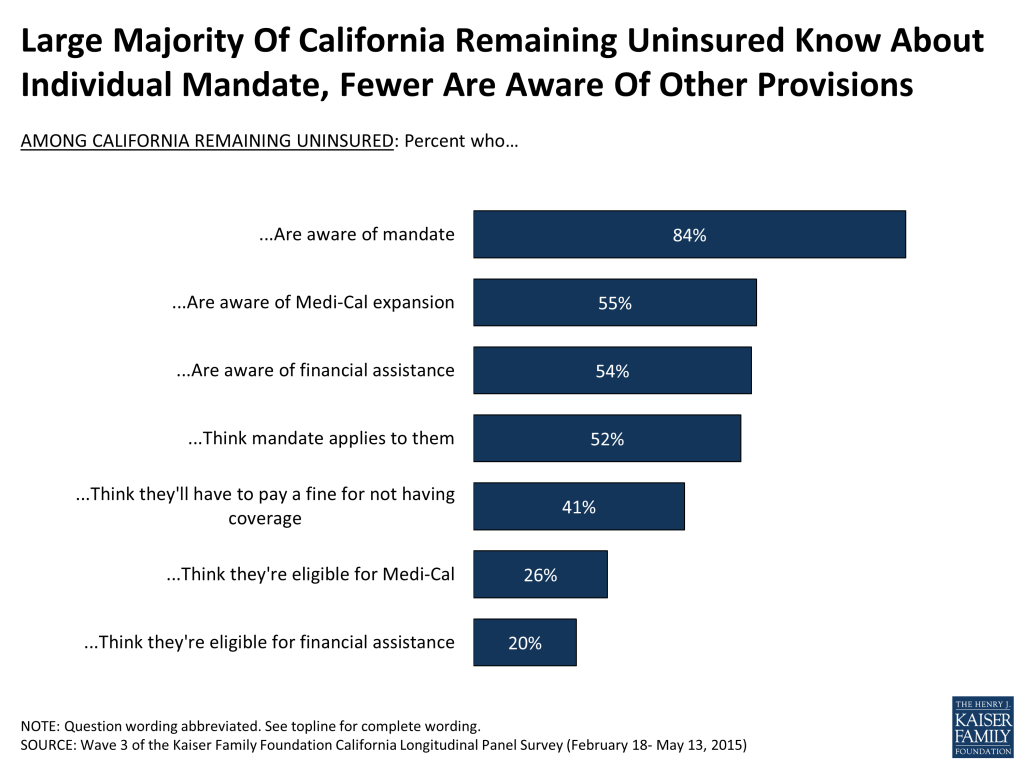
Knowledge About Health Care Law Provisions That Could Benefit Them
A large share (84 percent) of the remaining uninsured in California are aware of the health care law’s requirement that most Americans have health insurance or pay a fine, and most (52 percent) think that the requirement applies to them. Although about 4 in 10 (41 percent) say they think they will have to pay a fine for not having coverage this year, 47 percent do not think they will have to pay a fine and 11 percent are unsure. It is important to note that many may in fact be exempt from the requirement due to financial hardship or other exceptions under the law. Over half (55 percent) say that if they found out they had to pay a fine for not having coverage last year in 2014 they would be likely to sign up for coverage this year.
Smaller shares of the remaining uninsured are aware of provisions of the health care law, beyond the requirement to have coverage, intended to expand coverage to the uninsured and those with lower-incomes. Just over half know that the law allowed for the expansion of the Medi-Cal program to cover more low-income Californians (55 percent) or that the law provides financial help to low- and moderate-income people to help them purchase health insurance coverage (54 percent).
California’s Remaining Uninsured Hispanics
The Hispanic population is particularly important in California because Latinos make up the largest racial or ethnic group in the state, accounting for 38 percent of the population,13 and 7 in 10 of the remaining uninsured are Hispanic (70 percent). However, 58 percent of California’s remaining uninsured Hispanics (41 percent of the remaining uninsured overall) may not be eligible for coverage because of their immigration status, which leaves 40 percent of California’s remaining uninsured Hispanics likely eligible for, but without health insurance coverage (29 percent of the remaining uninsured overall).
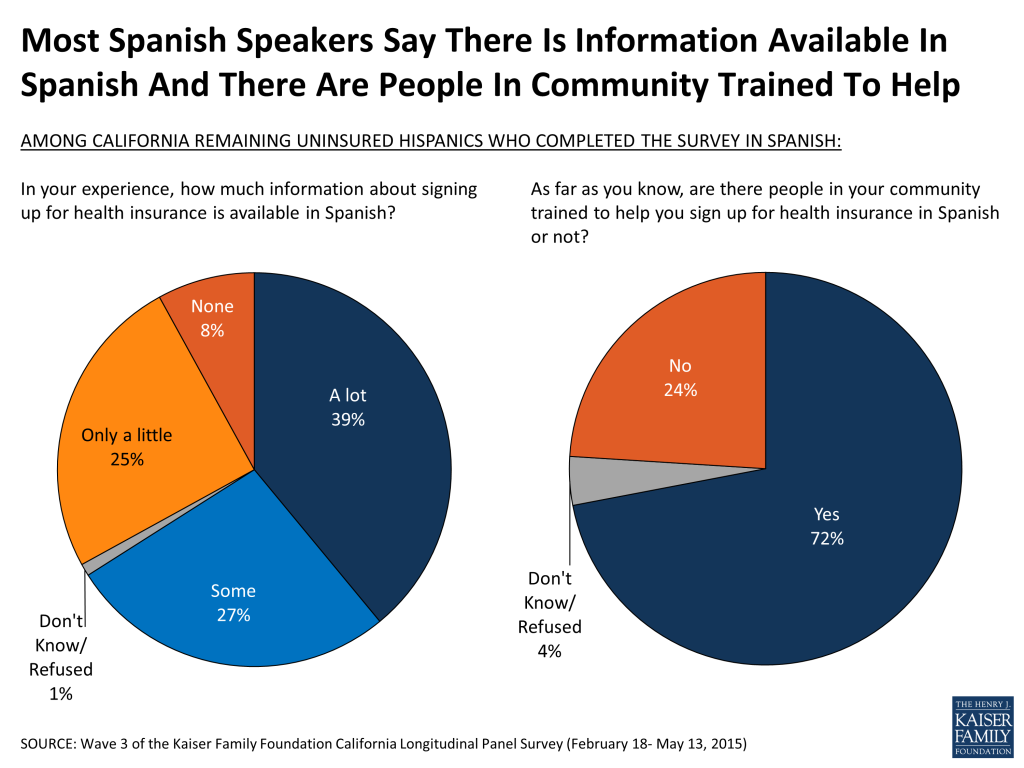
Navigating health insurance options and health care jargon can be confusing, and adding language differences to the equation has the potential to be an even bigger barrier to enrollment. However, Californians currently without health insurance who prefer to communicate in Spanish give largely positive feedback when asked how much information is available in Spanish and whether there are people in their community trained to help them sign up for insurance in Spanish. Most (66 percent) remaining uninsured Spanish speakers say that, in their experience, there is at least some information about signing up for insurance available in Spanish – about 4 in 10 (39 percent) say there is a lot of information available and another 27 percent say there is some information available. There is still room for improvement though, as a third of Spanish-speaking remaining uninsured Californians report that there is only a little information available in Spanish (25 percent) or say that there is none available at all (8 percent). A majority (72 percent) of Spanish-speaking uninsured also report there are people in their community trained to help them sign up, while a quarter (24 percent) say that there are not people in their community trained to help and 4 percent say they do not know.
Half of uninsured Hispanics say they are worried that if they sign up for health insurance it will draw attention to their immigration status or that of a family member, and this share is even higher among undocumented uninsured (67 percent). Additionally, slightly more than half of undocumented Hispanics (54 percent) say they worry about being deported or that a family member could face deportation if they sign up for health insurance.
Key Findings: Section 5: A Closer Look At Previously Uninsured With Medi-cal And Covered California Coverage
Because California was an early adopter of the health care law and led the way by expanding Medi-Cal and creating its own health insurance marketplace, the lessons learned from the experiences of previously uninsured Californians as they navigate the state’s new health insurance options provide insight both at the state level and nation-wide.
Shopping For Coverage
There continues to be large variation in enrollment method depending on type of coverage. Nearly half (48 percent) of California’s previously uninsured who enrolled in Covered California say they bought their policy online, compared to just 13 percent of Medi-Cal recipients. Large shares of Medi-Cal enrollees (40 percent) instead say they signed up in-person, while only 14 percent of Covered California enrollees say the same. More than 2 in 10 in each group say they signed up over the phone.

Over 4 in 10 (44 percent) recently insured Californians say that someone helped them enroll or renew their coverage, fewer than the roughly 6 in 10 (63 percent) who reported getting assistance last year, in part reflecting that some were automatically renewed in coverage. Community health workers were one of the primary helpers for those enrolling in Medi-Cal while most who enrolled in plans through Covered California say they got help from a Covered California representative.
| Table 4: Assistance Enrolling | ||
| Did someone help you enroll in health insurance/renew your health plan or did you complete the enrollment/renewal process on your own? | Covered California | Medi-Cal |
| Someone helped me/ did the whole thing for me (Vol.) | 50% | 42% |
| Family member or friend | 6 | 8 |
| Covered California representative | 32 | 9 |
| Health insurance broker or agent | 9 | 2 |
| Community or county health worker | <1 | 15 |
| A health plan representative | <1 | 3 |
| Someone else | 2 | 5 |
| Automatically renewed (Vol.) | 8 | 7 |
| Completed it alone | 41 | 50 |
| Note: Don’t know/Refused responses not shown. | ||
Majorities of the recently insured say shopping for coverage was easy. For example, 77 percent of those with Medi-Cal and 66 percent of those with coverage through Covered California say it was easy to figure out if their income qualified them for financial assistance. Similar shares of the recently insured overall also say it was easy to compare the monthly cost of coverage (74 percent), the services covered under the plans (65 percent), and the cost sharing requirements (64 percent).

While the Medi-Cal program experienced a significant backlog in 2014 as it dealt with large numbers of applicants, most (58 percent) of California’s previously uninsured who say they are now covered by the program say it took less than a month to find out whether they were eligible for Medi-Cal. However, 19 percent say it took between one and two months and 1 in 5 (20 percent) say it took more than two months.
About 4 in 10 (38 percent) who have recently gained insurance through Covered California or reported they had it last year say they got a Health Insurance Marketplace Statement from Covered California containing information about their health insurance coverage for their 2014 taxes, and 27 percent say that the form showed they received a premium tax credit in 2014. However, it is possible that if an individual’s income or family size changes over the course of the year, they may end up owing money to the government. This may come as a surprise to some, as about half (49 percent) of those who say they currently have coverage through Covered California are unaware of this, and many (40 percent) who currently have a Covered California plan say their monthly income changed over the course of 2014, including 24 percent who say they had a big change in income.
The Remaining Uninsured’s Experience With Covered California Website And Phone Center
Small percentages of California’s remaining uninsured report that they have contacted Covered California via web or phone; just 14 percent say they have visited the Covered California website and 7 percent say they have called the 1-800 number since November 15, 2014. This is a substantial change from last year, when about twice as many uninsured reported visiting the website (30 percent) or calling the 1-800 number (15 percent).

Conclusion: Conclusion
After two open enrollment cycles under the ACA, 68 percent of California’s previously uninsured report having health insurance, up from the share (58 percent) who said they had coverage after the first open enrollment period. The largest share reports having coverage through Medi-Cal (34 percent) and 12 percent say they have coverage through Covered California, similar to the 14 percent who say they have coverage through an employer. There have been considerable gains in access and affordability among those who have gained insurance compared to what they said in the baseline survey, while those who remain uninsured report difficulty affording care and that their health needs are being met at similar rates as they did nearly two years ago. Most of California’s previously uninsured who reported having coverage after the first open enrollment period continued to report having coverage, but some have since become uninsured, while some others who reported being uninsured after the first open enrollment period, now report having coverage. These dynamics indicate the potential challenges of getting and keeping coverage for the previously uninsured as well as potential opportunities for new enrollment gains among those who have potentially missed chances to enroll in the past. Future gains in coverage may be moderate, however, as the third (32 percent) of California’s previously uninsured who remain without coverage consists largely of harder to reach groups; those who are undocumented immigrants and therefore ineligible for coverage through the ACA and those who reported as of the baseline survey that they had been without coverage for two or more years or had never had health insurance. A fourth wave of the Kaiser Family Foundation California Longitudinal Panel Survey will continue to track this same, representative group of previously uninsured Californians to see how they are faring several years into the ACA’s implementation.
Conclusion: About The Terms Used In This Report
This report primarily uses the following definitions for key groups examined in the survey:
The overall group of Californians who were uninsured prior to the ACA’s first open enrollment period, most often referred to as “California’s previously uninsured.”
1) The subgroup of previously uninsured Californians who currently report that they are uninsured, referred to as “California’s remaining uninsured.” This group includes some who reported having coverage in 2014, some who reported not having coverage in 2014, and some whose 2014 coverage status is unknown because they were unable to be contacted in 2014.
2) The subgroup of previously uninsured Californians who now report that they have health insurance, referred to as “California’s recently insured.” Two subgroups within California’s recently insured are:
a) Those who reported that they were uninsured in the summer of 2013 and either said in spring 2014 that they did not have coverage or were unable to be contacted, but now report having health insurance, referred to as “California’s newly insured,” and
b) Those who reported that they were uninsured in the summer of 2013, reported gaining insurance in the spring of 2014 and say they still have coverage in spring 2015, referred to as “California’s still insured.”
And, as noted in the Survey Methodology Section, only those uninsured for at least two months were included in the baseline survey. Other terms used occasionally throughout the report are defined below.
- Eligible Previously Uninsured Californians: Because the coverage expansions under the ACA do not extend to undocumented immigrants, some of the analyses focuses on those who reported being U.S. citizens or permanent residents in the baseline survey, described in shorthand as those who are ‘eligible’ for the ACA’s coverage expansions.
- Undocumented Previously Uninsured Californians: For the purposes of this report, undocumented immigrants are defined as those who reported in the baseline survey that a) they were not born in the United States or Puerto Rico, b) they came to this country without a green card, and c) they have not received a green card or become a permanent resident since arriving. There are several ways that this definition, while workable for the purposes of a broad analysis of this sort, falls short of the complexity of real life. First, it relies on self-reporting, and since respondents have an incentive not to reveal unlawful immigration status, it is undoubtedly a somewhat imperfect measure. Second, those that did not answer all three in the series of immigration status items in the baseline survey were not able to be categorized. Third, by necessity of time and efficiency, the survey did not allow for a full exploration of the many nuances inherent in the U.S. immigration system. For example, this category may actually include a small number of individuals in California as refugees, asylees or other humanitarian immigrants who might better be placed among the ‘eligible uninsured’. The survey, unfortunately, does not allow this level of detailed sorting. Since estimated immigration status is based on individuals’ responses to the baseline survey, it is possible that some small share of those thought to be undocumented immigrants have now become permanent residents or received a green card.
- Income categories: Because eligibility for two of the law’s main components – the Medi-Cal expansion and the tax credits being made available to purchase insurance on the new exchanges – is based on an individual’s family income relative to the federal poverty level (FPL), in some cases we report survey results by FPL categories. Eligible previously uninsured Californians with incomes 138% FPL or less (roughly $33,000 a year for a family of 4 in 2014) are eligible for Medi-Cal coverage, while those with incomes greater than 138% and up to 400% FPL (roughly $33,000-$95,000 for a family of 4 in 2014), are eligible for subsidies to purchase insurance through Covered California Marketplace. Those with incomes above 400% FPL are allowed to buy insurance through Covered California, but are not eligible for subsidy assistance. For convenience, we sometimes refer to the eligible group with incomes 138% FPL or less as the “Medi-Cal target group”, and those greater than 138% and up to 400% FPL as the “exchange subsidy target group”. These obviously are approximations that do not allow for every real world exception to be taken into account. For example, lawfully present immigrants may remain subject to a five year wait before they may enroll in Medi-Cal, but for the purposes of this analysis they are included in the Medi-Cal target group if they meet the income criteria. Similarly, some of those in the exchange subsidy target group may not be eligible for marketplace subsidies if they have access to affordable employer coverage, a situation difficult to ascertain in a phone survey.
Methodology
This is the third in a series of surveys by the Kaiser Family Foundation (KFF) tracking the views and experiences of a group of Californians who were uninsured in the summer of 2013, prior to implementation of the ACA’s insurance market reforms and coverage expansions through Covered California and Medi-Cal. The first survey (Wave 1) was conducted from July 11-August 29, 2013, with a randomly selected group of individuals who were uninsured at the time of the interview, and was paid for entirely by KFF. The second survey (Wave 2) was conducted from April 1-June 15, 2014 and the current survey (Wave 3) was conducted from February 18-May 13, 2015, with the same longitudinal panel of respondents, whether they obtained coverage or remained uninsured. All three surveys were designed and analyzed by researchers at KFF. Social Science Research Solutions collaborated with KFF researchers on sample design, weighting, and supervised fieldwork. Fieldwork costs associated with Waves 2 and 3 of the survey were paid for by The California Endowment.
The Wave 1 survey was conducted among a representative random sample of 2,001 adults ages 19-64 living in California who reported having been without health insurance for at least two months at the time of the interview14 (NOTE: persons without a telephone could not be included in the random selection process). Computer-assisted telephone interviews conducted by landline (990) and cell phone (1,011, including 660 who had no landline telephone) were carried out in English and Spanish by SSRS. To increase efficiency in reaching this low-incidence, hard-to-reach group, both the landline and cell phone sampling frames oversampled areas with a lower-income population (since being uninsured is negatively correlated with income). The landline sample frame also oversampled households whose phone numbers were matched with directory listings indicating the presence of at least one person age 19-64 and a household income of less than $25,000. Additionally, 230 interviews (130 landline, 100 cell phone) were conducted with respondents who previously completed recent national SSRS omnibus surveys of the general public and indicated they were ages 19-64 and uninsured. These previous surveys were conducted with nationally representative, random-digit-dial landline and cell phone samples. Waves 2 and 3 also consisted of computer-assisted telephone interviews conducted in English and Spanish by landline and cell phone, including those who had no landline phone.
| Total | Landline | Cell phone(no landline) | Web | |
| Wave 1 (July 11-August 29, 2013) | 2,001 | 990 | 1,011 (660) | Not applicable |
| Wave 2 (April 1-June 15, 2014) | 1,219 | 623 | 545 (327) | 51 |
| Wave 3 (February 18-May 13, 2015) | 1,105 | 555 | 463 (317) | 87 |
In order to re-connect with respondents who may be more willing to complete the survey online, an abbreviated web version was introduced on for Waves 2 and 3 after attempts had been made to reach respondents by phone. The online questionnaire was offered in English and Spanish and was limited to key questions about insurance status, type of coverage, and reasons for obtaining coverage or remaining uninsured. A total of 51 respondents in Wave 2 and 87 respondents in Wave 3 completed the online version of the survey.
Screening for Waves 2 and 3 involved verifying that the respondent had participated in Wave 1. Multiple attempts were made to reach every respondent from Wave 1 and encourage participation in later waves. Efforts included multiple dialing at various times of day and throughout the week, mailings and emails to those who provided such contact information, repeated dialing of non-working numbers, and attempts to find alternative phone numbers for non-working numbers.
A multi-stage weighting design was applied to ensure accurate representation of California’s nonelderly adult uninsured population prior to the ACA’s coverage expansions. The weighting process for Waves 2 and 3 involved corrections for sample design, as well as sample weighting to match the weighted Wave 2 sample and the weighted Wave 3 sample to Wave 1 responses along demographic characteristics. As it did for Wave 1, the base weight for Waves 2 and 3 accounted for the oversamples used in the sample design, as well as the likelihood of non-response for the sample from earlier omnibus surveys, number of eligible household members for the landline sample, and a correction to account for the fact that respondents with both a landline and cell phone have a higher probability of selection. Demographic weighting parameters for Waves 2 and 3 were based on Wave 1 weighted demographics, which were adjusted for age, education, race/ethnicity, nativity (for Hispanics only), Hispanics by gender, presence of own child in household, marital status, California region, poverty level, and phone usage. For more information on weighting and data sources, see the Wave 1 methodology. All differences referred to in the report are statistically significant. Statistical tests of significance account for the effect of weighting, and, for trend analysis, testing takes into account the survey’s panel design.
A unique consideration for panel surveys such as the Kaiser Family Foundation California Longitudinal Panel Survey, is whether those who participate in subsequent waves are different in terms of their attitudes or demographics than those who refuse to participate again or were unable to be re-contacted. Of the total 2,001 respondents who completed Wave 1, 1,219 participated in Wave 2 and 1,105 completed Wave 3. These completion rates are within an expected range given that the uninsured are already an often a difficult to reach population since many are lower income, younger, undocumented immigrants, and members of racial/ethnic minority groups, and may change phone numbers or move more often than the public at large. After data collection was complete, data from Wave 1 and Wave 3 were compared to evaluate the impact of some respondents not completing Wave 3, referred to as attrition. While there are some differences in the unweighted demographics of those who completed Wave 3 and the full Wave 1 sample, these differences are corrected for by weighting. As shown in the table below the total weighted distributions are similar for Wave 1 and Wave 3 for age, gender, race/ethnicity, party identification, education and income. See the Wave 3 Attrition Appendix for more information on attrition.
| Unweighted | Weighted | ||||||||
| Wave 1 (n=2001) | Completed Wave 3 (n=1105) | Completed all 3 Waves (n=923) | Percentage Point Difference (W1 – W3 Total) | Wave 1 | Completed Wave 3 | Completed all 3 Waves | Percentage Point Difference (W1 – W3 Total) | ||
| Gender | |||||||||
| Male | 48% | 44% | 42% | 4 | 54% | 53% | 50% | 1 | |
| Female | 52% | 56% | 58% | -4 | 46% | 47% | 50% | -1 | |
| Race/ ethnicity | |||||||||
| White | 27% | 32% | 35% | -5 | 26% | 27% | 30% | -1 | |
| Black | 7% | 7% | 8% | 0 | 5% | 5% | 6% | 0 | |
| Hispanic | 58% | 54% | 50% | 4 | 56% | 55% | 53% | 1 | |
| Other Race | 8% | 7% | 8% | 1 | 12% | 11% | 11% | 1 | |
| Age | |||||||||
| 18 to 29 | 23% | 18% | 17% | 5 | 33% | 31% | 27% | 2 | |
| 30 to 39 | 21% | 19% | 20% | 2 | 24% | 24% | 25% | 0 | |
| 40 to 49 | 22% | 21% | 21% | 1 | 21% | 21% | 22% | 0 | |
| 50 to 64 | 35% | 41% | 42% | -6 | 22% | 24% | 26% | -2 | |
| Education | |||||||||
| HS or less | 57% | 51% | 50% | 6 | 58% | 56% | 55% | 2 | |
| Some college | 28% | 31% | 32% | -3 | 29% | 30% | 31% | -1 | |
| College Grad+ | 15% | 17% | 17% | -2 | 12% | 13% | 13% | -1 | |
| Phone status | |||||||||
| Landline | 49% | 54% | 55% | -5 | 42% | 45% | 48% | -3 | |
| Cell | 51% | 46% | 45% | 5 | 58% | 55% | 52% | 3 | |
| Marital status | |||||||||
| Married | 33% | 32% | 32% | 1 | 37% | 37% | 38% | 0 | |
| Not Married | 67% | 67% | 68% | 0 | 62% | 63% | 62% | -1 | |
| Family income | |||||||||
| <138% FPL | 60% | 58% | 58% | 2 | 52% | 53% | 54% | -1 | |
| 138%-400% FPL | 30% | 32% | 32% | -2 | 36% | 35% | 34% | 1 | |
| 400%+ FPL | 5% | 6% | 5% | -1 | 7% | 7% | 7% | 0 | |
| Language of interview | |||||||||
| English | 63% | 67% | 69% | -4 | 65% | 66% | 66% | -1 | |
| Spanish | 37% | 33% | 31% | 4 | 35% | 34% | 34% | 1 | |
| Resident Status | |||||||||
| Citizen/ legal immigrant | 79% | 83% | 84% | -4 | 78% | 80% | 81% | -2 | |
| Undocumented immigrant | 20% | 16% | 15% | 4 | 21% | 19% | 18% | 2 | |
| Party Identification | |||||||||
| Republican | 11% | 12% | 13% | -1 | 11% | 12% | 13% | -1 | |
| Democrat | 35% | 36% | 36% | -1 | 32% | 32% | 31% | 0 | |
| Independent | 35% | 35% | 34% | 0 | 37% | 39% | 38% | -2 | |
| Other | 9% | 8% | 8% | 1 | 9% | 8% | 8% | 1 | |
Another consideration for panel surveys is the potential for “sensitization effects,” that is, what effect returning to the same people about the same topics has on their experiences or views. For example, after taking the baseline survey that covered many aspects of the coverage expansions under the ACA, were people more likely to seek out information about health insurance and enroll than they would have been otherwise? While there is no direct way to measure this effect on this survey, other analyses have found that these effects are minimal and short-lived,15 and we do not believe they would have had a substantial impact on results presented here, particularly given all the other media coverage, advertising, and outreach targeted at this population during the fall and winter of 2013 and 2014.
The margin of sampling error including the design effect for the full sample is plus or minus 4 percentage points. For the recently insured, it is plus or minus 5 percentage points and for the remaining uninsured it is plus or minus 8 percentage points. Numbers of respondents and margin of sampling error for key subgroups are shown in the table below.
| Group | N | MOSE |
| Total Wave 3 | 1105 | +/- 4 percentage points |
| Recently Insured | 797 | +/- 5 percentage points |
| Recently insured by Medi-Cal | 411 | +/- 7 percentage points |
| Recently insured by non-group plan | 168 | +/- 11 percentage points |
| Recently insured through Covered California | 147 | +/- 12 percentage points |
| Recently insured through an employer | 143 | +/- 11 percentage points |
| Recently insured Hispanics | 380 | +/- 7 percentage points |
| Remaining Uninsured | 303 | +/- 8 percentage points |
| Remaining uninsured Hispanics | 209 | +/- 9 percentage points |
| Remaining uninsured undocumented immigrants | 110 | +/- 13 percentage points |
For results based on other subgroups, the margin of sampling error may be higher. Sample sizes and margin of sampling errors for other subgroups are available by request. Note that sampling error is only one of many potential sources of error in this or any other public opinion poll.
Some demographic measures referred to in the report were only asked during the baseline survey, such as questions about educational attainment, debilitating chronic condition, length of time uninsured, resident status, and race/ethnicity. For more information on the first and second waves of the Kaiser Family Foundation California Longitudinal Panel Survey visit:
Wave 1: https://www.kff.org/health-reform/report/californias-uninsured-on-the-eve-of-aca-open-enrollment/
Endnotes
- Kaiser Family Foundation analysis of 2013 ASEC Supplement to the Current Population Survey. ↩︎
- Kaiser Family Foundation, California’s Uninsured On The Eve Of ACA Open Enrollment, September 2013, https://modern.kff.org/health-reform/report/californias-uninsured-on-the-eve-of-aca-open-enrollment/. ↩︎
- Kaiser Family Foundation, Where Are California’s Uninsured Now? Wave 2 Of The Kaiser Family Foundation California Longitudinal Panel Survey, July 2014, https://modern.kff.org/health-reform/report/where-are-californias-uninsured-now-wave-2-of-the-kaiser-family-foundation-california-longitudinal-panel-survey/. ↩︎
- DHHS Centers for Medicare & Medicaid Services, “Medicaid & CHIP: May 2014 Monthly Applications, Eligibility Determinations and Enrollment Report,” July 11, 2014 http://medicaid.gov/AffordableCareAct/Medicaid-Moving-Forward-2014/Downloads/May-2014-Enrollment-Report.pdf. DHHS Office of the Assistant Secretary for Planning and Evaluation Issue Brief, “Health Insurance Marketplace: Summary Enrollment Report For The Initial Annual Open Enrollment Period,” May 1, 2014 http://aspe.hhs.gov/health/reports/2014/MarketPlaceEnrollment/Apr2014/ib_2014Apr_enrollment.pdf. The California Department of Health Care Services estimates 1.9 million people have enrolled in Medi-Cal since open enrollment started, http://news.coveredca.com/2014/04/covered-californias-historic-first-open.html. ↩︎
- Covered California 2015 End of Open Enrollment Report, http://www.coveredca.com/PDFs/end-of-open-enrollment-report.pdf ↩︎
- For the purposes of this report, the ‘eligible uninsured’ are California residents who said they had been uninsured for at least two months in the baseline survey and would be eligible for participation in the ACA coverage expansion based on their self-reported status as a citizen, permanent resident, or lawfully present immigrant. See the “About The Terms In This Report” Section for more details. ↩︎
- The total share with non-group coverage, including those in Covered California, remained stable between the spring 2014 survey and the spring 2015 survey. In addition to an actual enrollment increase, there may be other reasons why more report in Wave 3 that they have Covered California specifically. For example, more people may be familiar with “Covered California” and thus better able to self-report their source of coverage. In addition, the follow-up question for those who report purchasing coverage on their own was modified for Wave 3. See topline for more information. ↩︎
- For the purposes of this report, undocumented immigrants are defined as those that reported in the baseline survey that a) they were not born in the United States, and b) they came to this country without a green card, and c) they have not received a green card or become permanent residents since arriving. See the “About The Terms In This Report” Section for more details. ↩︎
- Regression results are available on request. ↩︎
- The analysis of the dynamics of health insurance excludes those who were unable to be contacted in spring 2014 and focuses exclusively on those who completed the survey after both open enrollment periods (roughly 8 in 10 of those who were interviewed in spring 2015). Including all the previously uninsured who participated in the most recent survey after the second open enrollment period, the results are similar. ↩︎
- Examining only those who completed both the spring 2014 and spring 2015 surveys results in a slight discrepancy in the shares recently insured and remaining uninsured – 69% and 31% instead of 68% and 32% when the analysis considers everyone who completed the survey in spring 2015 after the second open enrollment period. This is due to the fact that some previously uninsured adults who completed the survey this year did not complete the survey after the 2014 open enrollment period and therefore we are unable to determine their insurance status at that time and they are excluded from the analysis on the dynamics of health insurance. ↩︎
- See endnote 8 or the “About The Terms In This Report” Section for more details. ↩︎
- US Census Bureau, California State & County QuickFacts http://quickfacts.census.gov/qfd/states/06000.html ↩︎
- Those who had been uninsured for less than two months were excluded from the survey since they may be experiencing a short period of uninsurance (i.e. someone who is between jobs), and the goal of the survey was to capture the experiences and views of those who have been without insurance for a longer period of time and are poised to experience the new coverage provisions of the ACA. ↩︎
- M. Brodie, “Sensitization Effects in a Study of the Impact of a Nationally Broadcast Special on Health Care Reform,” in Doctoral Thesis: Political Institutions, Participation, and Media Evaluations— Influences on Health Care Policy (Boston, Mass.: Harvard University, 1995). ↩︎