Leveraging Medicaid in a Multi-Payer Medical Home Program: Spotlight on Rhode Island’s Chronic Care Sustainability Initiative
This last of three case studies examining key operational aspects of coordinated care initiatives in Medicaid focuses on Rhode Island’s Chronic Care Sustainability Initiative (CSI), a multi-payer patient-centered medical home program in which the one Medicaid health plan and all commercial health plans in the state participate. Hallmarks of the initiative are the engaged leadership of the health insurance commissioner and key stakeholders; mandatory participation by commercial insurers, but participatory governance; a common developmental contract used by all payers; and investments in health information technology and other support for practice transformation. Medicaid’s large role as a payer makes it a key source of leverage in multi-payer initiatives, and Medicaid plan and provider experience serving populations with complex needs can also benefit such endeavors. Alignment of goals, performance metrics, practice transformation resources, and incentives across payers sends practices and providers coherent policy and financial signals regarding desired models and outcomes of health care delivery, and increases their potential impact.
Executive Summary
This last of three case studies examining key operational aspects of coordinated care initiatives in Medicaid focuses on Rhode Island’s Chronic Care Sustainability Initiative (CSI). This multi-payer, patient-centered medical home (PCMH) initiative includes the one Medicaid health plan in the state and the commercial health plans, one of the largest of which has many Medicaid as well as commercial enrollees. These payers provide practices that participate in the CSI with financial incentives and practice transformation resources to develop a sustainable model of patient-centered chronic care for adults. The payers use a common contract with the practices that specifies uniform requirements and performance metrics, and they pay practices a uniform monthly per capita care management fee to support nurse care managers, who are integral to Rhode Island’s model. These fees and other investments in practice transformation also help finance data infrastructure at the practice level that is necessary to support a PCMH. CSI policy development and practices are guided by a multi-stakeholder group in a governance structure shaped by the consensus-oriented style and leadership of Rhode Island’s health insurance commissioner. The Office of the Health Insurance Commissioner (OHIC) and the Executive Office of Health and Human Services (EOHHS), where the Medicaid program resides, convene the project jointly.
KEY THEMES
The common contract is central to the multi-payer system. When multiple payers use a common contract, practices face uniform metrics, requirements, and incentives, and can invest in practice improvements that benefit all patients. In the CSI, common contract specifications were developed through a consensus process that included plans and providers. Because an OHIC representative was present at the meetings, antitrust restrictions that would otherwise have barred this process could be waived.
Medicaid participation in a multi-payer initiative presents opportunities and challenges. Because Medicaid is a large purchaser, leveraging its impact matters. Medicaid plan and provider experience in serving high-need populations has benefited the initiative. At the same time, plans and practices with sizeable Medicaid patient panels face challenges, as performance metrics are not risk-adjusted. However, the CSI rewards safety-net practices if they get “half-way to the goal.”
Combining a collaborative model with a mandate is useful. Multi-payer initiatives require buy-in. Even beginning as a voluntary pilot, the CSI might have been hard to launch without the health insurance commissioner’s leadership. Plans acknowledged that the subsequent mandate to participate probably helped move the PCMH effort forward statewide, but, importantly, consensus-style governance has lent acceptability to the mandate. Because the mandate operates through the OHIC, it covers commercial insurers, but it does not extend to self-insured employers or public purchasers. However, the Medicaid plan has always participated, and commercial plans must now pay practices care management fees for their Medicaid as well as their commercial members.
Collaboration requires time, effort, and leadership. The operation of a multi-payer initiative requires plans, practices, and purchasers to make significant commitments of time, focus, and effort on an ongoing basis. Active stakeholder leadership and engagement are necessary to build trust among parties and confidence that aligned action can advance shared goals for patient care and delivery system performance.
Multi-payer initiatives and practice transformation require infrastructure and entail new costs. Convening meetings, collecting data centrally to aggregate across payers, and other activities required to manage a multi-payer initiative all cost money. In addition to the overhead and infrastructure costs to manage the system are significant costs for developing infrastructure at the practice level for data collection and analytics, and for other changes, such as integration of nurse care managers. Care management payments to practices provide critical financing to support such transformation. With the expiration of federal grant funds to support health information technology, maintaining adequate funding is challenging.
Maintaining payer support may require evidence of savings. Health plans’ willingness to provide practices with additional support may ultimately depend on a demonstrated return on investment – evidence that investing in primary care is not only improving patient care, but also generating savings somewhere in the system. Some payers wondered whether payment to practices should be more strongly tied to their performance on clinical process and outcome metrics.
Practice transformation is the beginning, not the end, of system change. The CSI has focused mainly on what goes on in primary care practices, but, ultimately, performance should be measured not just at the practice level, but at the system level, using metrics like aggregate rates of hospitalization and emergency department use. At this writing, hospitals were not yet at the CSI table, but, more recently, the state has been engaging hospitals and has added performance measures on hospital use that are tied to payment.
LOOKING AHEAD
Rhode Island has been successful in engaging plans, providers, and purchasers in a broad medical home initiative. A multi-payer system, including Medicaid in this case and several others nationwide, translates into important advantages for practices and providers, giving them a common, aligned set of goals, performance metrics, practice transformation resources, and incentives. Rhode Island’s ability to implement the CSI was enhanced by engaged leadership, a mixed regulatory-collaborative approach, the state’s small size, and the small number of major payers. Even under these conducive conditions, the organizational commitment, investment, and resources required to develop and implement a multi-payer PCMH initiative have been extensive, and mustering the necessary financing is a formidable, ongoing challenge. While the CSI model may not be feasible in other states, or may need adaptation, it illustrates the potential to leverage Medicaid’s role as a payer to transform health care delivery. Ultimately, to succeed most fully in improving care and reducing costs, multi-payer initiatives will need to extend beyond the sphere of primary care to engage specialists, hospitals, and others in the medical neighborhood. As the ACA expansion of coverage takes effect, and states and other entities seek to improve care delivery and orient payment toward performance, both the scale and momentum of multi-payer initiatives like the CSI can be expected to grow.
Issue Brief: Introduction
In recent years, a growing number of states have undertaken major delivery system reforms in Medicaid, seeking to improve care coordination and health outcomes for Medicaid beneficiaries, and to reduce spending growth in the program. To help inform the development of such initiatives in other places, the Kaiser Commission on Medicaid and the Uninsured worked with Mathematica Policy Research to examine key operational features of coordinated care initiatives in Medicaid in three states – Colorado, North Carolina, and Rhode Island. This issue brief focuses on Rhode Island’s Chronic Care Sustainability Initiative (CSI), a multi-payer, statewide patient-centered medical home (PCMH) initiative. Because Medicaid is the largest health care purchaser in the state, the program’s participation in Rhode Island’s initiative is one crucial source of its leverage.
The information and perspectives presented here are based on a review of CSI program documents and on telephone interviews with the program managers, two large participating health plans, and two participating practices with Medicaid patients — a community health center, and an office-based practice with both commercially-insured and Medicaid patients.
Issue Brief: Program Overview
The CSI, which launched in 2008, had its origins in Rhode Island’s participation in a 2006 foundation-funded initiative that aimed to align public purchasers, private purchasers, and health plans in regional partnerships to more effectively leverage improvements in care for people with chronic conditions.1 Rhode Island has used this multi-payer strategy to support the PCMH model statewide.2 With strong leadership from the state’s health insurance commissioner, a multi-stakeholder group determined that the pilot program should align quality improvement and financial incentives among purchasers, health plans, and providers; improve chronic care in primary care settings; and make primary care a more attractive and viable specialty in Rhode Island.3 The idea was to use the leverage of the state’s large capitated health plans and Medicaid’s major role as a purchaser to drive the desired improvements.
Participating payers
Since the beginning, the CSI has included the two largest commercial health plans in the state – Blue Cross & Blue Shield of Rhode Island (BCBS) and UnitedHealth Care (UHC) – and the state’s one Medicaid health plan, Neighborhood Health Plan of Rhode Island (NHP). (UHC has many Medicaid as well as commercial members.) These payers provide practices that participate in the CSI with financial incentives and practice transformation resources to develop a sustainable model of patient-centered chronic care for adults.
Originally a voluntary pilot, the CSI was formalized in 2011 by state legislation, sponsored by the health insurance commissioner, mandating that all state-regulated (i.e., commercial) health plans participate. In 2012, Rhode Island required all commercial plans with Medicaid contracts to participate in the CSI. As a result, these plans are now required to pay supplemental care management fees to participating practices not just for their commercial enrollees, but also for their Medicaid enrollees if the practice serves at least 200 of them. Medicare began to participate in the initiative when CMS selected Rhode Island for the Multi-Payer Advanced Primary Care Practice (MAPCP) demonstration in July 2011. Therefore, participating practices now receive supplemental payments for Medicare beneficiaries, Medicaid beneficiaries in managed care (about 60% of the total Medicaid population), and privately insured patients. Because the CSI does not include Medicaid patients who are enrolled in the state’s fee-for-service primary care case management (PCCM) program, the PCCM program was outside the scope of this study. However, we were told that, like CSI practices, primary care providers in the PCCM program receive supplemental fees to support nurse care managers, and that the state uses the same performance metrics in both programs. In addition, the Executive Office of Health and Human Services (EOHHS), where the Medicaid program resides organizationally, is a co-convener of the project with the Office of the Health Insurance Commissioner (OHIC) and has taken a more active role in the initiative in recent years. State Medicaid officials attend CSI meetings and the program provides non-financial support for the initiative.
Participating practices
Practices must be selected for the CSI in order to receive supplemental payments from plans. Initially, in 2008, five primary care practices identified as “champions” were selected to participate. Eight more practices were added in 2010, three were added in 2012, and consistent with the state’s strategic plan, 20 practices were added in 2013, including several multi-site practices. The initiative now includes 36 practices, 48 practice sites, and 297 physicians serving an estimated 250,000 Rhode Islanders, approximately 25% of the state’s total population. Under the strategic plan, another 20 practices will be added in each of the next four years and the initiative is slated to serve more than 500,000 patients. At the end of 2012, Medicaid managed care enrollees accounted for about 25% of patients in CSI practices, commercial enrollees constituted 51%, Medicare Advantage enrollees made up 9%, and Medicare fee-for-service beneficiaries made up 15%.4
Core features
The following elements are central to the multi-payer medical home initiative:
A common developmental contract, which all health plans use with participating practices.5 Appendix 1 outlines key elements of the developmental contract: supplemental payments, required practice improvements, performance metrics, and staging of the contract provisions as practices come on line.
A uniform per member per month (PMPM) fee for care coordination, which all plans pay participating practices, and which help finance the practice infrastructure needed to support a PCMH. Practices can also earn additional performance incentive payments.
Practice transformation investments, to support the addition of a nurse care manager, in particular. These investments also support the development and use of electronic health record (EHR)-based performance metrics, and participation in learning collaboratives.
A multi-stakeholder leadership group, which guides CSI policy development and practice transformation.
Governance, authority, and operational management
The health insurance commissioner’s leadership and Rhode Island’s small size and long history of collaboration among major stakeholders have had a defining influence on the CSI’s development and structure. All those interviewed considered the health insurance commissioner’s leadership to have been instrumental in engaging commercial insurers in the initiative and enabling them to develop a common contract. The fact that many of the key actors in the CSI go back years together has also been helpful. The medical directors from several health plans trained together, the health insurance commissioner was formerly the director of NHP, and the current Medicaid medical director was the original CSI project staff person.
Governance. Governance of the CSI was structured to be collaborative and participatory.6 A large Steering Committee and a smaller Executive Committee set strategic direction for the CSI and are responsible for its overall governance; they include representation from the three major stakeholder groups – providers, payers, and purchasers (i.e., employers and Medicaid). The Steering Committee develops consensus on major issues, such as chronic conditions to be targeted, metrics, and payment strategies. While not required to do so, the Executive Committee also operates by consensus. Appendix 2 shows the governance structure, which, besides the Steering Committee and an Executive Committee, includes Working Committees on data and evaluation; practice training support and transformation; practice reporting; payment reform/contracting; and service expansion and integration. The purpose and scope of these Working Committees are outlined in Appendix 3.
The governance structure has remained largely unchanged, although it is now being refined and more formally constituted. In 2013, a Patient Advisory Subcommittee is being introduced to serve as the voice of patients and families and provide advice and input to the Steering and Executive Committees.7 In addition, a new Marketing and Communications Subcommittee is charged with increasing awareness of PCMH among employers and labor unions, increasing patient participation in PCMH practices; supporting the Patient Advisory Subcommittee, and conducting liaison with other community agencies.
Authority. A broader goal of the health insurance commissioner’s is to increase the role of primary care in health care delivery. Operationally, his strategy is to shift Rhode Island’s “primary care spend” from 8% of total health care spending currently, to 30%. To move in this direction, he has required state-regulated insurers to increase the share of their premiums spent on primary care by 1 percentage point per year over the period 2010-2014. Insurer investments in the CSI (e.g., their supplemental payments to participating practices) count toward this required annual increase. The health insurance commissioner has also interpreted his authority to allow him to require plans to contribute to the overhead costs of the data and related infrastructure for the CSI; these costs have grown recently because the federal Beacon Community Program, which provided grants for health information technology and other infrastructure, has ended. Insurer expenditures on these costs also count toward the primary care spend goal.
Operational management. The OHIC, with the support of a staff person then at the state’s Quality Improvement Organization (and now the state’s Medicaid medical director), was responsible for appointing the original Steering Committee and managing CSI’s day-to-day operations. At that time, staffing for the initiative was minimal— just two full-time staff funded by a foundation grant and the health plans. The Rhode Island Foundation, the state’s only community foundation, later served as a vehicle for accepting and handling external funding support for the CSI, and also provided office space for the program. When the original staff left in 2011, the state issued a competitive solicitation for project direction and project management support, and the contract was awarded to Commonwealth Medicine, the medical school at the University of Massachusetts.
Infrastructure. Substantial infrastructure is needed for the CSI to work. Essential components include:
- Support (staff and facilities) for governance, coordination, and convening;
- Technical support to assist practices in constructing all-payer, EHR-based clinical metrics and using them to improve performance;
- Development of interim all-payer, claims-based metrics (e.g., all-cause hospitalizations; ED use) until a permanent, consistent data base that integrates EHR clinical data can be developed;
- Coaching in practice transformation, particularly for practices newly entering the PCMH; and
- An annual Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey of patients in CSI practices.
For part of the CSI’s history, the Beacon grant provided crucial financing to the Rhode Island Quality Institute (RIQI) for some of these infrastructure costs (except for the first item).8 9 With Beacon’s expiration, the costs are now being transferred to the CSI itself and payers are being asked to cover more of them. (The RIQI will continue to do portions of the work related to data collection and analysis, but practice transformation services are no longer procured through the RIQI.) As the CSI expands to include more practices, the needs for infrastructure development and funding will grow. In 2013, the annual cost of administering CSI will be $2.2 million, up from about $0.5 million for its first contract, which started in December 2011.10 About half of the total budget will go to organizations providing support to the RIQI for work previously funded under the Beacon grant.11 In early 2013, Rhode Island received a federal grant for up to $1.6 million under the Center for Medicare and Medicaid Innovation (CMMI) State Innovation Models (SIM) initiative, which is designed to foster state-based models for multi-payer payment and health care delivery system transformation.12 Interviewees expressed hope that the award will allow the CSI to develop a more permanent operating model suitable to a broad-based permanent program.
Issue Brief: Key Themes
The common contract is central to the multi-payer model. The common developmental contract was not easily developed, but its use is central to the CSI. The consistency across all payers of a core set of required metrics, and fixed supplemental payments to practices tied to performance expectations, align the incentives and goals that practices face, and encourage practices to pool the supplemental revenues from all their payers to invest in improvements that benefit all their patients. Interviewees representing practices favored having common metrics over different metrics for four or five different payers, and they pointed out that common metrics also reduce overhead costs for practices.
The common requirements were developed through a consensus process involving participating stakeholders (largely plans and providers). Plans had to be willing to modify their existing contract requirements, at least to some extent. For example, a plan might have to give up “home-grown” requirements of its own in favor of the common contract’s emphasis on NCQA accreditation. Similarly, national firms with common requirements across their health plans had to be willing to make exceptions for a plan operating in Rhode Island if the firm’s and the CSI’s requirements differed. Because of anti-trust laws that limit health plans’ ability to discuss pricing with each other, the deliberations that produced consensus on certain requirements of the common contract would not have been feasible except for the health insurance commissioner’s central convening authority. Specifically, the common developmental contract requires health plans to make a uniform contribution to practices to finance infrastructure-building. Such payments are legally considered to be pricing-related, but the discussion could take place as long as it was convened by OHIC.
Medicaid participation in a multi-payer system presents opportunities and challenges.
Leverage and experience. Because Medicaid is such a large purchaser in Rhode Island – it accounts for a substantial share of health care costs in the state – the ability to leverage the program is integral to the CSI’s impact. Although the majority of adults in Rhode Island are commercially insured, Medicaid is the dominant source of coverage in some CSI practices and covers a substantial share of patients in others. As Medicaid plan officials see it, an important gain from the CSI is that, with all payers at the table, Medicaid and commercial plans can learn from each another. Small plans get what one interviewee described as “a brain trust of medical directors committed to improving quality and re-engineering change in office-based care.” CSI principals say that the initiative has benefited significantly from the experience of plans and safety-net providers serving Medicaid patients, as they have been leaders in quality improvement and have a greater understanding of what it takes to coordinate care, often among many providers, for populations with complex needs for health services and other supports. The CSI provides a framework and environment for consultation and sharing of knowledge and ideas, and helps to avoid the problem of “reengineering a system that works for only one-third of [a] health plan’s members.”
Patient mix differences and fair payment. CSI plans and practices with a sizeable share of Medicaid patients face some unique challenges. Performance metrics are not currently risk-adjusted, possibly because of delays in data acquisition and a lack of resources and expertise to develop a methodology. The RIQI is now taking on the methodological work for risk-adjustment through a subcontract with Research Triangle Institute. Compared with the privately insured, Medicaid patients are more likely to have mental health co-morbidities as well as socioeconomic hardships that contribute to poorer health outcomes. In addition, a substantial share of the patients served by community health centers participating in the CSI are uninsured, making management of their care more challenging and performance benchmarks harder to achieve. (Health centers generally include the uninsured in their performance metrics because they operate on a philosophy that all patients are treated the same and that performance metrics need to be practice-wide, not payer-specific.) Recognizing the potentially higher risk profile of Medicaid and uninsured patients, and seeking to be fair to practices, the CSI established a “half-way to the goal line” approach that rewards practices with incentive payments if they get half-way to the performance benchmark relative to where they started. Stakeholders speaking from a Medicaid perspective praised this measure as a constructive compromise that rewards practices and providers in the safety-net space for their progress toward CSI goals. They expressed concern that plans not view the practices to which this policy applies as “slackers,” but highlighted that the consensus-oriented governance of the CSI provides a structure for discussing and resolving issues that have different implications for different stakeholders.
Combining a collaborative model with a mandate is useful.
Consensus helps legitimate authority. Getting multiple payers to work together on a unified strategy requires a lot of buy-in. Having the CSI pilot begin on a voluntary basis almost certainly helped foster willingness to participate. But even the voluntary initiative might well have been harder to achieve without Rhode Island’s long history of collaboration and what stakeholders describe as the talented leadership of the health insurance commissioner. The health plan representatives who were interviewed do not like the requirement to participate, but acknowledged that the mandate was probably valuable to the effort to extend the chronic care initiative to all adults statewide. By pairing a mandate for commercial insurer participation with a consensus-oriented approach to governance, the state is able to exert leverage that is needed to direct health plans to do some things differently and to spend money in ways that, except for the primary care spend requirement, they would not. It is likely that one reason private insurers have accepted the mandate is that, while their participation is required, they are also part of the consensus process that determines the specific requirements of the initiative.
The locus of authority determines its reach. Because the mandate to participate in the CSI operates through the OHIC, it does not reach all plans or purchasers in the state. The OHIC’s authority covers commercial insurers, but does not extend to self-insured employers or to public purchasers. Although the legislative mandate does not apply to the Medicaid plan, this plan has participated voluntarily in the CSI from the beginning, and, since 2012, the state has required all health plans with Medicaid contracts to pay the supplemental care management fees to practices on behalf of their Medicaid as well as their commercial enrollees, if the practice serves at least 200 of their Medicaid members. The CSI mandate does not apply to the Medicare program, but Medicare participates under the aegis of the Multi-payer Advanced Primary Care Practice (MAPCP) demonstration.
Collaboration requires time and effort and leadership.
Stakeholder commitment. The development and operation of a governance process that is based on consensus decision-making require heavy investments of time by many parties, and a strong commitment to work together to hammer out common goals and objectives and implement the initiative. Ongoing operation of the CSI succeeds because its key stakeholders — plans, practices, and purchasers — continually commit significant time, focus, and effort to the enterprise. To illustrate, the administrator of one participating family medicine practice with eight providers reported that she routinely attends five different CSI-related meetings monthly, as well as ad hoc meetings. Collectively, two or three other individuals in the practice attend another five to six meetings each month on data, reporting, care management, and other topics.
Engaged leadership. Leadership from all the stakeholder groups has been critical to the CSI’s success. Even in a state with a collaborative tradition, there exist competing interests, gaps in trust, and other sources of tension between parties that must be addressed. Individual stakeholders with different perspectives must, through dialogue and other interaction, gain confidence in the other participants and the fairness of the project to perceive an alignment between their own goals and interests and the initiative’s aims. The CSI management team highlighted plan and provider engagement in the initiative as a key to building increased trust between these two groups. Conversations facilitated by the learning collaboratives helped to give plans confidence in providers’ commitment to practice transformation and the use of metrics to drive change, and to give providers confidence that plans are paying them fairly and giving them the data they need to improve care management.
Broad-scale initiatives and practice transformation both require infrastructure.
Overhead costs. Convening meetings, collecting and reporting data centrally for aggregation across payers, and providing assistance to help practices change, are all overhead costs that require funding. Perhaps because the CSI started out as a small pilot, such costs were underestimated initially. Also, because administrative and staff support for the initiative was limited early on, development of a formal organizational structure (e.g., by-laws) was delayed. Funding constraints also led the CSI to rely on different financing approaches for learning collaboratives at different times, rather than on an established and stable means of support.
The timing of the Beacon grant to Rhode Island was fortunate. The overlap between the needs of the CSI and the purposes of the grant – to link development of EHRs to clinical practice improvement and enhanced outcomes – gave the state access early on to substantial support to build infrastructure. However, such grants are not routine and they are typically time-limited. With the Beacon grant’s termination, the CSI health plans are providing additional funding for infrastructure (over and above their care management payments to practices) for at least one year, but there is concern about their ability and willingness to maintain this support over time, particularly if the amount required of them grows. Some expressed the view that, because more work on the data infrastructure was not accomplished earlier, progress was delayed and opportunities were lost, adding to health plans’ and practices’ current costs. For example, if the infrastructure for the exchange of clinical data had been more developed, CSI would not have to invest as much now in claims-based “work-arounds” to analyze costs across all payers.
Costs of practice-level infrastructure-building. Like other efforts to develop patient-centered models of primary care, the CSI generates new needs for spending – to manage the multi-payer effort, collect data, create metrics and reporting processes, and support practice transformation. Primary care practices need to set up systems to track data relevant to the metrics they must report and integrate these metrics into their performance improvement programs. The supplemental payments to participating practices provide critical additional funding to support other required practice changes as well, such as expanded use of nurse care managers who can spend more clinical time with patients. One practice manager reported that the supplemental payments have allowed her to fund a nurse care manager, hire a full-time quality assistant who can do “deeper dives” into the data (e.g., to understand outliers), and keep the practice open longer hours. Some practices had already made some of the needed investments before the supplemental payments became available, but even for these practices that are farther along, the care management fees help finance intensified efforts and additional staff time to participate in learning collaboratives with other practices.
At least some of the CSI practices are finding the supplemental payments insufficient to cover all the costs involved in participating. They explained that they continue to participate for the good of their patients, whom they see getting better care because of the practice changes spurred by the initiative. Consensus is lacking on what level of support participating practices require. Sponsors of similar initiatives elsewhere can also anticipate debate about the appropriate levels of payment to support the practice-level infrastructure needed to support patient-centered care.
Maintaining payer support for CSI may require evidence of savings.
Those we interviewed noted that the health care environment is very fluid in Rhode Island, as it is elsewhere in the nation. The practices that participated in the CSI from the outset were early adopters of change who were philosophically committed to its success; the practices joining now may not be as committed to doing what is necessary internally to develop clinical data and use them to improve performance, although they should be able to benefit from the experience of the established practices. Health plans say that their willingness to provide practices with additional support ultimately depends on a demonstrated return on investment. In today’s payment reform environment, they say, they need evidence that investing in primary care is not only improving patient care and patient experience, but also generating savings somewhere in the system. Some payers wondered aloud whether practices should have more “skin in the game” – that is, whether their payment should be more strongly tied to their performance on clinical process and outcome metrics. It could be that the ability to maintain support for these kinds of initiatives will require settling the return-on-investment question, challenging though that may be.
Practice transformation is the beginning, not the end, of system change.
There was agreement that, ultimately, performance should be measured not just at the level of individual practices, but also at the system level, using metrics like aggregate ED, hospitalization, and readmission rates. Clearly, hospitals are integral to true systemic change. At this writing, hospitals were not yet at the CSI table, and stakeholders reported that they were still relatively traditional, with a primary focus on filling beds; they added that ACO development and hospital acquisition of practices remained limited in the state. As a consequence, the CSI has been focused mainly on what goes on in primary care practices. More recently, however, the state says it has been engaging hospitals, and has added performance measures on hospitalization and ED use that are tied to payment. One interviewee placed the CSI in the broader context of system transformation this way: “I think we’re working towards a system that is more integrated and will address the whole triple aim. Has that been proved yet? I don’t know. I think we’re still walking down the road. We certainly can’t continue in this [current] system. I think this (medical home model) has more optimism around it than other types of approaches. But…we’re not there yet. This is new territory.”
Issue Brief: Looking Ahead
Rhode Island has been successful in engaging health plans, providers, and purchasers in a multi-payer collaboration to support PCMHs, with the goal of improving chronic care for all Rhode Island adults. The leverage exerted by a multi-payer strategy, including Medicaid in this case and several others nationwide, translates into important advantages for practices, giving them a common, aligned set of goals, metrics and performance benchmarks, practice transformation resources, and incentives, across payers and purchasers, to support practice changes that will benefit all their patients.
Rhode Island’s ability to implement the CSI was enhanced by a number of factors. The distinctive leadership of the health insurance commissioner, and his preference for collaboration around policy goals rather than a purely regulatory approach, were crucial. In a different state context, mandating payer participation and the “primary care spend” could be more challenging. The small number of major payers in the state also helped, and the fact that many stakeholders knew each other and understood each other’s goals made it easier for them to “get on same page.” In addition, many Rhode Island practices and providers serve patients with a mix of health insurance, and may be receptive to participating in an initiative that standardizes the requirements and incentives they face from different payers.
But while Rhode Island has some distinctive attributes, the state has confronted some challenges and issues that are likely to be common to states pursuing multi-payer initiatives. Rhode Island’s need to identify new resources for implementation, and the finding that buy-in is important to maintain support for the initiative, are lessons useful to states broadly. The kinds of tensions between plans, practices, and providers that have required negotiation in Rhode Island are pretty universal; other states may wish to consider whether the inclusive and consensus-oriented approach to development and governance that Rhode Island adopted might help bridge differences and build trust among the stakeholders in their environments.
The reality that system-level health improvements and cost savings require change beyond the sphere of primary care is also not unique to Rhode Island, and states generally can benefit from CSI leadership’s observation that specialists, hospitals, and others in the medical neighborhood must also be engaged for multi-payer medical home initiatives to succeed most fully. While the CSI model may not be feasible in other states, or may warrant adaptation, it demonstrates how Medicaid’s role as a major payer can be leveraged to transform health care delivery and payment. As the ACA expansion of coverage brings more Americans into the health care system, and states and other entities seek to improve care delivery and orient payment toward performance, both the scale and momentum of multi-payer efforts like the CSI can be expected to grow.
This Kaiser Commission on Medicaid and the Uninsured (KCMU) issue brief was prepared by Marsha Gold and Winnie Wang of Mathematica Policy Research and Julia Paradise of the Kaiser Family Foundation.
The authors express their appreciation to David Bourassa, Renee Bromley, Deidre Gifford, Debra Hurwitz, Mack Johnston, David Keller, and Renee Rulin, whose expertise and insights were invaluable to this project.
Appendices
Appendix 1: CSI Common Developmental Contract, April 2012
Performance Targets
Target 1: Structural Improvements (Practice Metric): Hire a nurse care manager; establish a compact with four specialists including a hospitalist; establish a plan/policy for after-hours care; have an electronic medical record and achieve Level 1 meaningful use; comply with the Quality Partners of Rhode Island Hospital and community physician best practices; demonstrate best practices for outpatient transitions of care; demonstrate use of evidence-based care; submit quality data
Target 2: Clinical Process Measures (Provider Metric): Achieve benchmark goals on specified CAHPS survey items; meet benchmark goal or achieve 50 percent improvement on at least four of seven metrics: Diabetes HbA1C <8, Diabetes BP<140/90,Diabetes LDL <100,Hypertension <140/90,Tobacco Cessation, Adult BMI (18-64), Adult BMI (65+)
Target 3: Outcome Measures (Provider Metric): CSI practices, in aggregate, to reduce emergency department and all-cause inpatient hospital admission rates by 7.5% and 5% respectively, relative to a comparison group
Staging
- Start-up Year
- Payments support transformation and measure development
- $4.50 PMPM to practices who attain NCQA Level 1 PCMH recognition, report common quality metrics, and achieve a number of process requirements.
- Practices are required to participate in project governance, evaluation and CSI learning collaborative.
- Transition Year
- Payment commits practices to use data measurement to drive performance
- $5.50 PMPM for demonstrating evidence of data-driven performance and attaining NCQA Level 2 recognition
- Performance Year 1
- Pay practices based on performance
- $5.00 PMPM if 0-1 performance targets are met
- $5.50 PMPM if 2 performance targets are met
- $6.00 PMPM if all 3 performance targets are met
- Practices agree to attain NCQA Level 3 PCMH recognition by end of performance year 2
- Performance Year 2
- Pay practices based on performance
- $5.00 PMPM if 0-1 performance target is met
- $5.50 if two performance targets are met
- $6.00 if all three performance targets are met
- Practices must attain NCQA Level 3 PCMH recognition by end of year
Appendix 2: CSI Governance Structure
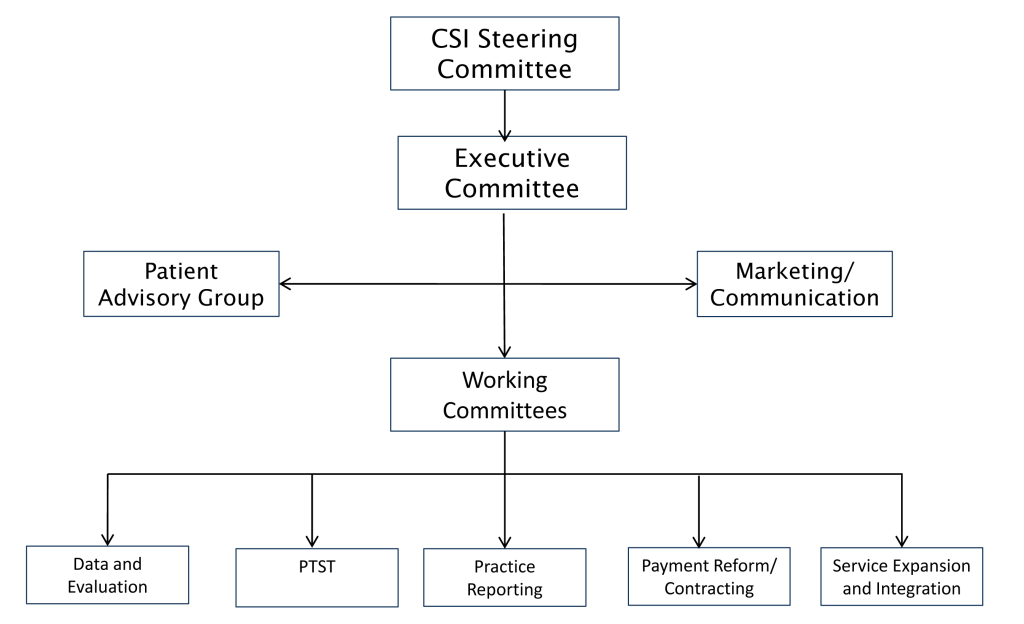
Source: CSI-RI: Strategic Planning, Final Plan, February 21, 2013. http://www.pcmhri.org/files/uploads/CSI_Strategic_Plan_Summary%20March%202013.pdf
Appendix 3: CSI Working Committees: Purpose and Scope
- Data and Evaluation– performance improvement; measure selection; measurement definition/harmonization; goals and benchmarks; evaluation; research; and liaison with other committees
- Practice Training Support and Transformation– conferences, learning collaboratives, coaching, and other forms of assistance
- Practice Reporting– review of quarterly practice data, data validation and public reporting, support for practice improvement and data sharing, support with EHR/IT issues
- Payment Reform/Contracting– contract development, patient attribution, alternative payment models, issues associated with PCMH as part of a delivery system
- Service Expansion and Integration– develop additional service capabilities (e.g., behavioral health, transitional care, oral health) and expand to additional populations (e.g., dual eligibles, children)
Source: CSI-RI: Strategic Planning, Final Plan, February 21, 2013. http://www.pcmhri.org/files/uploads/CSI_Strategic_Plan_Summary%20March%202013.pdf
Endnotes
- Regional Quality Improvement Initiative, Center for Health Care Strategies. Available at http://www.chcs.org/info-url_nocat3961/info-url_nocat_show.htm?doc_id=377021 ↩︎
- Case Study: Rhode Island Pilots Innovative, Cross-Payer Patient-Centered Medical Home Model, Center for Health Care Strategies, July 2009. Available at http://www.chcs.org/publications3960/publications_show.htm?doc_id=985380 ↩︎
- Ibid. ↩︎
- Quarterly MAPCP report on Rhode Island (quarter ending December 31, 2012). Provided to authors by CSI management staff. ↩︎
- The mechanism is actually a common contract amendment that all payers incorporate into their existing contracts with practices. ↩︎
- Rhode Island Chronic Care Sustainability Initiative (CSI-RI) Governing Structure, December 2006. Available at http://www.chcs.org/publications3960/publications_show.htm?doc_id=534883 ↩︎
- CSI-RI: Strategic Planning, Final Plan, February 21, 2013. Available at http://www.pcmhri.org/files/uploads/CSI_Strategic_Plan_Summary%20March%202013.pdf ↩︎
- Rhode Island Beacon Community Program: 2012 Annual Report, Rhode Island Quality Institute, December 5, 2012. Available at http://www.pcmhri.org/files/uploads/Rhode%20Island%20Beacon%20Community%20Program%20Annual%20Report_FINAL12-21-12.pdf ↩︎
- Rhode Island Quality Institute (Fact Sheet, last updated November 29, 2012), Office of the National Coordinator for Health Information Technology. Available at http://www.healthit.gov/sites/default/files/beacon-factsheet-ri.pdf ↩︎
- University of Massachusetts program office communication. ↩︎
- Under a major subcontract to the University of Massachusetts, the Rhode Island Quality Institute will continue quality measurement and reporting tasks, utilization measurement (working with Research Triangle Institute), and administration of an annual Consumer Assessment of HealthCare Providers and Systems (CAHPS) survey. The University of Massachusetts will develop additional subcontracts, the largest of which will involve support for training and technical support for practices. Another will allow the program to develop and pilot two community health teams to help small practices become PCMHs. Others will support evaluation, grants management, marketing, and similar specialized needs. The remainder of the funds will be used to support the current staff at the University of Massachusetts and expand staff to handle the selection and training of new practices sites and increased needs for coordination. ↩︎
- http://innovation.cms.gov/initiatives/State-Innovations-Model-Design/ ↩︎