 Understanding Medicaid Ex Parte Renewals During the Unwinding
Blog
Understanding Medicaid Ex Parte Renewals During the Unwinding
Blog
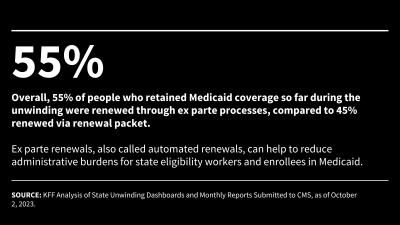
As states unwind the Medicaid continuous enrollment provision, they must comply with federal renewal requirements, including the requirement to conduct ex parte, or automated renewals. This policy watch explains what ex parte renewals are, examines variation in ex parte renewal rates across states, and discusses current issues as well as actions states are taking to increase ex parte rates.