Women and Health Care in the Early Years of the ACA: Key Findings from the 2013 Kaiser Women's Health Survey
Preventive Services
Clinical preventive care helps identify health problems earlier, allowing conditions to be treated or managed more effectively before they become more serious. The ACA prioritizes and promotes access to clinical preventive services by requiring that new private plans cover recommended clinical preventive services without cost sharing. The specific services that new plans must include are the ones that are recommended by:1
- the US Preventive Services Task Force (USPSTF), an independent body of clinicians and scientists that reviews the evidence of preventive health care services and develops recommendations for primary care providers and health care systems; services with grade A or B are covered under the ACA policy;2
- the Advisory Committee on Immunization Practices (ACIP), a group of medical and public health experts convened by the Centers for Disease Control and Prevention (CDC) that makes recommendations on vaccines for people of all ages;3
- the Health Resources and Services Administration’s (HRSA) Bright Futures project for children, in partnership with the American Academy of Pediatrics provides recommendations to improve health of infants, children and adolescents;4
- the Health Resources and Services Administration, Office of Women’s Health issued federal regulations for eight preventive care services for women based on recommendations from a committee of the Institute of Medicine (IOM).5
The combined roster of services recommended by these groups is extensive and can be classified into a few broad categories, including counseling and screening tests related to cancer, chronic conditions, mental health, health behaviors, and certain sexual and reproductive health services. For women, the law also requires no cost sharing for at least one annual “well woman” visit.
Knowledge and Understanding of the ACA Rules on Preventive Care
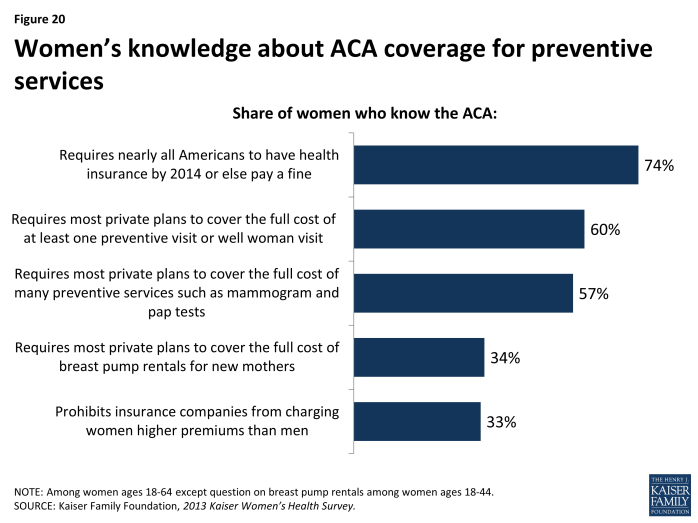
Women’s awareness of the ACA requirements regarding no-cost coverage of preventive care is uneven.
Coverage for preventive services without cost sharing is required in all new private plans, including employer-sponsored plans, individual market plans, and those in the new state marketplaces. While millions of women could potentially reap these benefits, many are unaware of ACA’s coverage for preventive services (Exhibit 5.1). A sizable majority (74%) of women are aware of the ACA’s requirement that individuals carry insurance, but fewer know that at least one preventive visit for women must be covered (60%), or of the no-cost coverage for preventive services such as mammograms (57%). Knowledge is quite low even among subgroups that are most directly affected. For example, only 34% of women of reproductive age (ages 18 to 44) know of the coverage for breastfeeding supports including breast pump rental. Awareness of other benefits of particular relavence to women, such as the prohibition on insurers charging higher premiums for women over men, known as gender rating, is also low.
General Checkups and Provider-Patient Counseling
Provider visits can give women an opportunity to talk with clinicians about a broad range of issues, including preventing illness, the role of lifestyle factors, and management of chronic illnesses. Under the ACA, new plans must cover at least one annual “well woman visit,” which the IOM Committee on Clinical Preventive Services for Women recommended could specifically cover a range of topics, such as assessment of diet and physical activity, history of pregnancy complications, mental health screenings for pregnant and post-partum women, screening for metabolic syndrome, preconception care, prenatal care, and screening for STIs.6
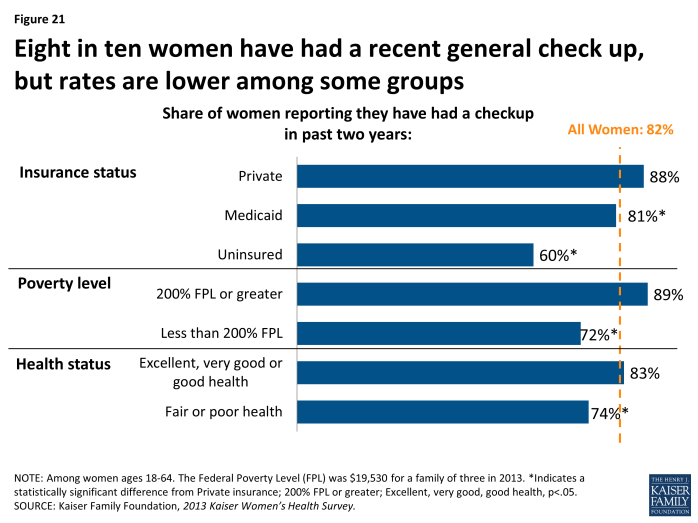
The majority of women have had a recent checkup with a provider.
Eight in ten women (82%) have had a general checkup in the past two years (Exhibit 5.2). However, it is less common among uninsured women (60%), women with incomes less than 200% FPL (72%), and those with poorer health (74%). Rates are similar between women of different racial and ethnic groups, with about eight in ten White (83%), Hispanic (79%), and Black (88%) women reporting they have had a recent well woman visit.
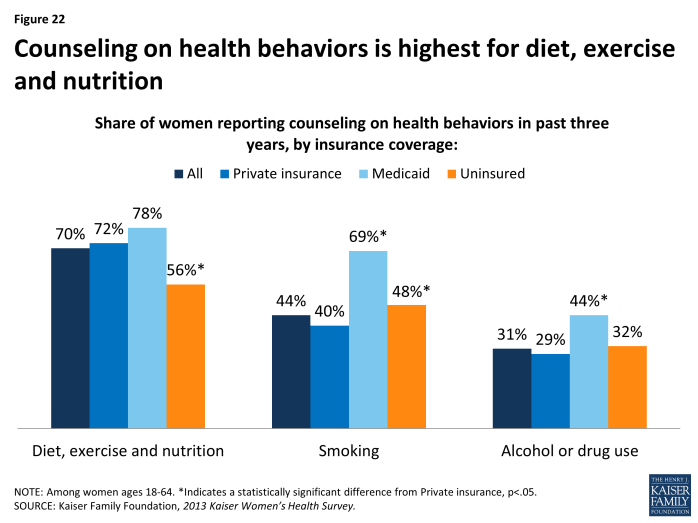
In general, rates of counseling on healthy lifestyles are highest for diet, exercise, and nutrition.
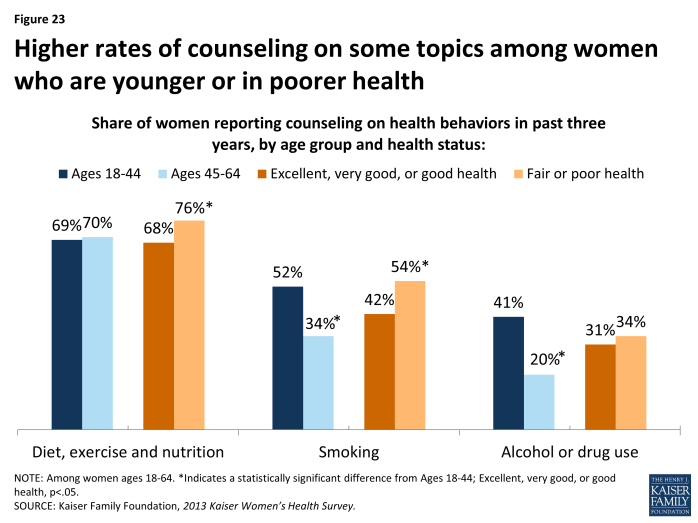
One component of preventive care that is now covered by plans without cost-sharing is provider counseling on health-related behaviors such as diet, smoking, and alcohol use, which have been shown to affect a wide range of health issues including a woman’s risk for chronic diseases. Consistent with other national trends, the highest rate of preventive counseling is on diet and nutrition, which 70% of women have discussed with a provider in the past three years (Exhibit 5.3). However, fewer than half of women have recently talked to a provider about other risk factors for chronic illnesses, such as smoking (44%) and alcohol or drug use (31%). Across the board, women covered by Medicaid have the highest rates of counseling. In addition, younger women and those in poorer health have higher counseling rates compared to their counterparts (Exhibit 5.4).
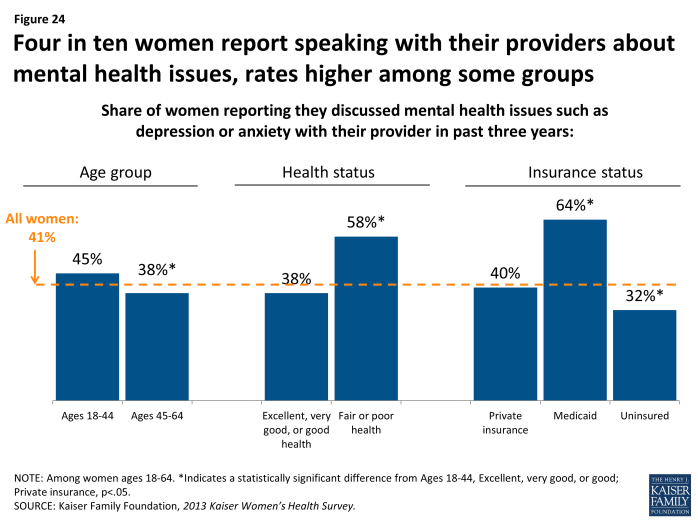
Fewer than half of women have talked recently with a provider about mental health issues.
It is estimated that 21% of adult women are affected by some form of mental illness, such as depression, anxiety, trauma, eating disorders, or dementia.7 Under the ACA, mental health services have been included as one of the ten Essential Health Benefits,8 meaning that all new plans must cover this category, although coverage for specific services varies between plans. Depression and anxiety in particular present challenges to a disproportionate share of women over their lifetimes, and in response, the USPSTF recommends routine screenings. Four in ten (41%) women report having discussed a mental health issue such as anxiety or depression with a provider in the past three years (Exhibit 5.5). Mental health screening rates are similar between women of different racial and ethnic groups, with about four in ten White (42%), Hispanic (42%), and Black (39%) women reporting discussing with a provider. As with other counseling topics, the rate is higher among women who are younger, sicker, or covered by Medicaid.
Screening Tests
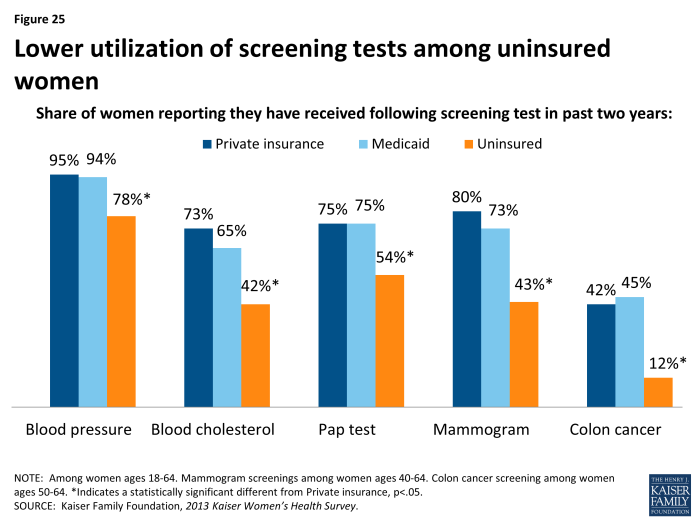
Rates of preventive screening tests are higher among women with insurance.
Use of preventive services can lead to early identification of conditions when they are most responsive to early interventions. This is especially true for some types of cancers and cardiovascular conditions. For example, routine mammograms and pap tests, which are used to identify breast and cervical cancers respectively, are recommended by the USPSTF as necessary preventive services. The USPSTF also recommends regular screenings for elevated blood pressure and cholesterol levels because they are considered markers for cardiovascular conditions, including stroke and heart disease. These services are all now covered by new private plans under the ACA’s preventive services coverage requirements.
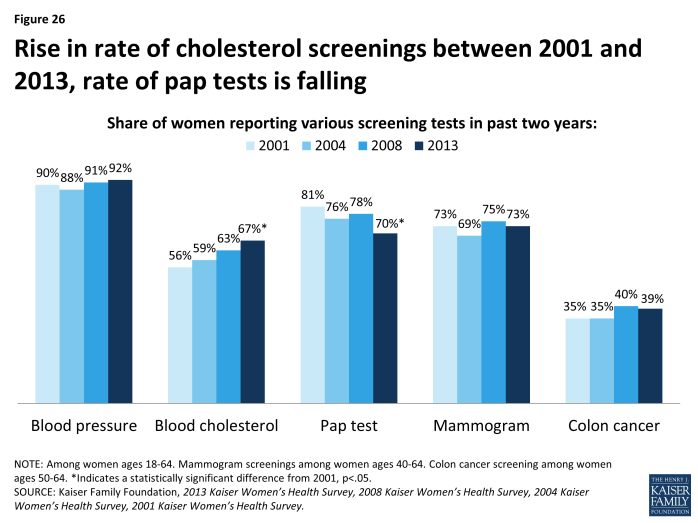
Most women have received cancer and cardiovascular screening tests in the past two years, including mammograms (73%), pap tests (70%), and cholesterol tests (67%), with some variation by age group (Table 6). The rate of blood cholesterol tests varies significantly between younger women (58% for women ages 18 to 44) and older women (78% for women ages 45 to 64). Cholesterol tests are recommended for women older than 20 who are at increased risk for heart disease.9 Rates of screening for colon cancer within the past two years are lower, with about four in ten (39%) women 50 and older reporting a recent colorectal screening. The USPSTF recommends three different methods with different intervals that are equally effective screenings for women between age 50 and 75 years: 1) annual high-sensitivity fecal occult blood testing, 2) sigmoidoscopy every 5 years combined with high-sensitivity fecal occult blood testing every 3 years, and 3) screening colonoscopy at intervals of 10 years.10
| Table 6: Rates of screening tests among women, by age and race/ethnicity | |||||||
| Preventive Screening | USPSTF Recommendation | Share of Women Reporting Screening Test in Past Two Years | |||||
| All Women | Age Group | Race/Ethnicity | |||||
| Ages 18-44 | Ages 45-64 | White | Black | Hispanic | |||
| Blood Pressure (Hypertension) |
Screening for high blood pressure in adults age 18 and older. | 92% | 90% | 94%* | 94% | 93% | 83%* |
| Blood Cholesterol Test (Coronary Heart Disease) | Screening of women ages 20 and older who are at increased risk for coronary heart disease. | 67% | 58% | 78%* | 69% | 66% | 63% |
| Pap Test (Cervical Cancer) |
A pap test every 3 years for women ages 21-65, or a combination of a pap test and HPV test every 5 years for women ages 30-65. | 70% | 72% | 67% | 71% | 76% | 72% |
| Mammogram (Breast Cancer) |
Mammography screenings once every 1 to 2 years for women ages 40 and older. | 73% | N/A | N/A | 74% | 79% | 72% |
| Colonoscopy, Fecal Occult Blood test, Flexible Sigmoidoscopy (Colorectal Cancer) | 1) Annual high-sensitivity fecal occult blood testing or 2) sigmoidoscopy every 5 years with high-sensitivity fecal occult blood testing every 3 years or 3) screening colonoscopy at 10 year intervals for adults ages 50 to 75. | 39% | N/A | N/A | 40% | 35% | 34% |
| NOTES: Among women ages 18-64, except mammogram (ages 40-64), and colorectal cancer (ages 50-64). The ACA requires coverage of mammogram services based on the USPSTF 2002 recommendation on breast cancer screening, which recommended screening every 1-2 years beginning at age 40. *Indicates a statistically significant difference from ages 18-44, White, p<.05. SOURCE: U.S. Preventive Services Task Force, USPSTF A and B Recommendations; Kaiser Family Foundation, 2013 Kaiser Women’s Health Survey. |
|||||||
Women who are uninsured have consistently lower use of all screening tests. While 95% of privately-insured women have had a blood pressure check in the past two years, the rate is 78% among uninsured women (Exhibit 5.6). Just over half of uninsured women have had a recent pap test, compared to three in four women with private insurance or Medicaid. The differences are even larger for mammography, cholesterol and colon cancer screenings, which typically require that patients go to a lab or other facility to have blood drawn or obtain other costly testing procedures. Women with Medicaid coverage receive screening tests on a par with women who are privately insured.
Over the past decade, self-reported rates of screening tests have been fairly level, except for a rise in the rate of cholesterol screenings and a decline in the rate of pap testing between 2001 and 2013 (Exhibit 5.7). The latter may be related to changes in the recommendations and guidelines for cervical cancer screening over that time period, which reduced the frequency and narrowed the age group for testing compared to earlier guidelines.11