Beyond the Numbers: Access to Reproductive Health Care for Low-Income Women in Five Communities
Crow Tribal Reservation, MT
KFF: Usha Ranji, Michelle Long, and Alina Salganicoff
Health Management Associates: Rebecca Kellenberg, Carrie Rosenzweig, and Sharon Silow-Carroll
Introduction
 The Crow reservation is the geographically largest Native American reservation in Montana, and home to approximately 8,000 members of Crow Nation, about 75% of the total enrolled membership. Located about 60 miles southeast of Billings, the reservation covers most of Big Horn County, but a small portion extends into Yellowstone County. The Crow Tribal Council governs the Nation, and Indian Health Services (IHS) is responsible for providing health services, although other coverage options and providers are also utilized. Montana offers coverage for reproductive health services for low-income women through its Medicaid expansion program1 and its Plan First family planning Medicaid waiver. These programs have had a significant impact in a community with high unemployment and poverty rates (Figure 1) and where stark health disparities between the white and Native American populations persist.
The Crow reservation is the geographically largest Native American reservation in Montana, and home to approximately 8,000 members of Crow Nation, about 75% of the total enrolled membership. Located about 60 miles southeast of Billings, the reservation covers most of Big Horn County, but a small portion extends into Yellowstone County. The Crow Tribal Council governs the Nation, and Indian Health Services (IHS) is responsible for providing health services, although other coverage options and providers are also utilized. Montana offers coverage for reproductive health services for low-income women through its Medicaid expansion program1 and its Plan First family planning Medicaid waiver. These programs have had a significant impact in a community with high unemployment and poverty rates (Figure 1) and where stark health disparities between the white and Native American populations persist.
Although Montana maintains many policies that protect access and coverage for reproductive health services, Crow women living on the reservation face sociodemographic, systemic, and cultural barriers that prevent many from readily accessing services. In many parts of the reservation, the nearest health care provider is an hour drive away; yet, transportation is not readily available in this low-income, rural community, which is federally-designated as medically underserved and as a health professional shortage area. IHS operates a hospital and two health clinics on the reservation, but a legacy of mistrust of IHS, long wait times, and confidentiality concerns prevent some Crow women from using their services. Some of these themes, particularly concerns about confidentiality, are common in small, rural communities across the country, and are not limited to the Crow reservation. While IHS offers a wide range of services including behavioral health, obstetrics and gynecology (Ob-Gyn), dental care, and surgery, pregnant women must transfer to Billings for labor and delivery. Traditional and religious beliefs prevent many Crow women from talking openly about sexual health, which may contribute to high rates of sexually transmitted infections (STIs) and teen pregnancy, and many consider abortion taboo or do not consider it an option when faced with an unplanned or unintended pregnancy.
This case study examines access to reproductive health services for low-income residents of the Crow reservation, Montana. It is based on semi-structured interviews conducted June–July 2019 by staff of KFF and Health Management Associates (HMA) with a range of local safety net clinicians and clinic directors, social service and community-based organizations, researchers, and health care advocates. We also conducted a focus group with low-income women. Interviewees were asked about a wide range of topics that shape access to and use of reproductive health care services in their community, including availability of family planning and maternity services, provider supply and distribution, scope of sex education, abortion restrictions, and the impact of state and federal health financing and coverage policies locally. An Executive Summary and detailed project methodology are available at https://www.kff.org/womens-health-policy/report/beyond-the-numbers-access-to-reproductive-health-care-for-low-income-women-in-five-communities.
| Key Findings from Case Study Interviews and a Focus Groups of Low-income Women |
|
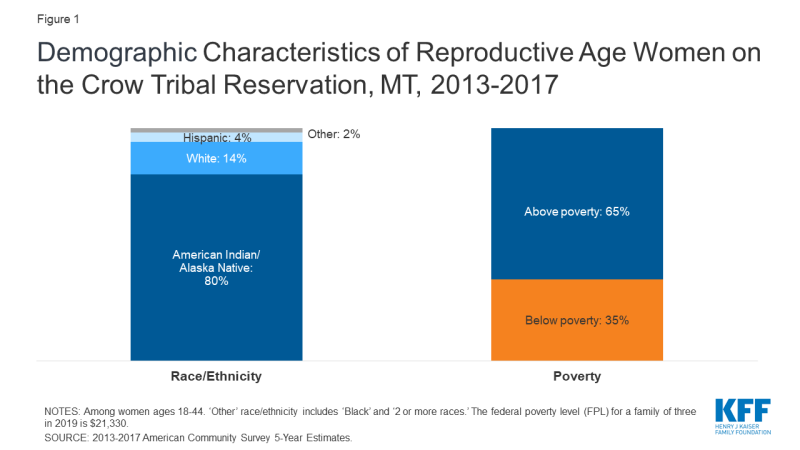
Figure 1: Demographic Characteristics of Reproductive Age Women on the Crow Tribal Reservation, MT, 2013-2017
Indian Health Service and Medicaid Coverage
Medicaid expansion has played a significant role in improving coverage rates for Native Americans in Montana, which has allowed Crow tribal members to access a broader set of services and providers beyond those available at IHS. The additional funding provided through the expansion program has also allowed IHS Service Units to expand their scope of services, a move that is essential to addressing the tremendous disparities in health for native women of reproductive age.
| Table 1: Montana Medicaid Eligibility Policies and Income Limits | |
| Medicaid Expansion | Yes |
| Medicaid Family Planning Program Eligibility | 216% FPL |
| Medicaid Income Eligibility for Adults Without Children, 2019 | 138% FPL |
| Medicaid Income Eligibility for Pregnant Women, 2019 | 162% FPL |
| Medicaid Income Eligibility for Parents, 2019 | 138% FPL |
| NOTE: The federal poverty level for a family of three in 2019 is $21,330. SOURCE: KFF State Health Facts, Medicaid and CHIP Indicators. |
|
The Indian Health Service (IHS) provides health care services to Native Americans, including the Crow tribe, at no-cost. Nationwide, IHS services are administered through 12 area offices and 170 IHS and tribally managed service units, and 41 urban Indian health programs including hospitals, health stations, and clinics. As of April 2019, IHS served 2.56 million Native Americans. The Crow Service Unit has three sites on the reservation: the Crow/Northern Cheyenne Hospital located at the Crow Agency headquarters, the Lodge Grass Health Clinic, and Pryor Health Station. There is also an Urban Indian Health and Wellness Center in Billings. Because IHS-funded services are paid in full by the federal program, focus group participants expressed that out-of-pocket cost is not an issue for them despite high levels of poverty on the reservation. However, IHS staff did discuss that overall funding is often limited.
Medicaid expansion and changes in Purchased/Referred Care reimbursement policy have supported increased access to health care and reproductive health care services. In 2015, the Montana legislature passed the bipartisan Health and Economic Livelihood Partnership (HELP) Act, extending Medicaid coverage (Table 1) to adults with incomes up to 138% of the federal poverty level (FPL). As of 2018, an additional 15,495 Native Americans gained Medicaid coverage through the expansion program in Montana. Expanded Medicaid coverage has allowed Native Americans throughout the state to seek a broader range of services from any provider that accepts Medicaid, allowing them more flexibility and choice in their provider and the care they receive. The increase in Medicaid coverage has also provided a significant influx in funding for Indian Health Service units, which can bill for services provided to Medicaid-enrolled Native Americans with a 100% federal matching rate. Importantly, in addition to the services that IHS facilities and tribal health departments can provide directly, they can also refer patients to additional services at non-tribal providers through the Purchased/Referred Care (PRC) Program. As a result, Native Americans, including Crow tribal members, now have greater access to reproductive health care, including fertility treatment, which is not provided within the IHS system. Approximately 35% of patients at Planned Parenthood of Montana in Billings are covered by Medicaid expansion or the state’s family planning waiver program, Plan First.
“Medicaid expansion has had a large impact for women here.”
–Lucille Other Medicine, Program Assistant, Messengers for Health“With expanded Medicaid, there is a newly liberated set of patients that can choose where they go. We have seen a huge increase in patients coming to our clinic now.”
–Dr. David Mark, CEO, Bighorn Valley Health Center
Provider Distribution
The Crow Agency IHS Service Unit employs one Ob-Gyn and one midwife, who are the only family planning providers in the community. A shortage of providers on the reservation and lack of transportation are barriers to accessing care in a timely manner. Many women seek care at one of the non-IHS clinics off the reservation in nearby Hardin or farther away in Billings.
Provider recruitment and retention is a key challenge both on and off the Crow reservation. Interviewees reported a significant staffing shortage at the Crow Indian Health Service, not only in obstetrics and gynecology, but also in behavioral health and nursing. IHS is in the process of building a housing unit for staff across from the hospital, which they hope will draw more providers to work there. Planned Parenthood in Billings also reported staffing challenges due to competition with other health care providers in the area. Staffing shortages mean the Planned Parenthood clinic must shorten their hours, limiting availability for working women who can often only come in the evening and on the weekends.
Publicly-funded contraceptive services are available on the Crow reservation, but some women experience barriers to obtaining timely services. The Crow-Northern Cheyenne Hospital offers a broad range of services including behavioral health, Ob-Gyn, dental care, and surgery. All three of the IHS locations also provide family planning services, including STI testing and treatment, and on-site insertion of implants and IUDs (at the hospital and Lodge Grass clinic). Sterilization services are not provided, but IHS clinicians said they will refer patients seeking sterilization to providers in Billings. While some providers are able to see patients on the same day the appointment is made, some interviewees noted they double and triple book appointments to account for no-shows. Several focus group participants reported experiencing long waiting room times.
“You can go to IHS for birth control, but you have to show up when it opens to make sure you get an appointment that day.”
–Focus group participant
There are several other key health care providers serving the Crow population. In nearby Hardin (13 miles away), the Bighorn Valley Health Center’s (BVHC) client population is roughly two-thirds Native American, 80% of whom are Crow, and the clinic offers the full range of contraceptive methods and STI testing and treatment. In addition, the Billings Urban Indian Health and Wellness Center, approximately 60 miles away in Billings, operates as part of the federal Urban Indian Health Program as a nonprofit, full-service medical clinic. They provide low- and no-cost health services including oral contraceptives, STI testing and treatment, and free transportation to and from the Crow-Northern Cheyenne Hospital and Pryor Health Station. The Yellowstone County Health Department and multiple primary and specialty care providers are also in Billings, in addition to two Planned Parenthood clinics offering the full range of contraceptive options and abortion services. BVHC and Planned Parenthood were the only clinics in the area receiving federal Title X family planning funds. However, at the time of this site visit, interviewees noted that if the Trump administration’s Title X rule changes take effect, Planned Parenthood will have to leave the program. Subsequent follow up calls with Title X providers found that this requirement has been challenging, and on August 19, 2019, Planned Parenthood formally withdrew from the Title X program nationally following implementation of the rule.
Crow women may go to Crow-Northern Cheyenne Hospital for prenatal care, but the hospital does not offer labor and delivery services. Some Crow women travel to non-IHS providers in Billings for all of their pregnancy care. There is one Ob-Gyn physician at Crow-Northern Cheyenne Hospital. However, the hospital is not approved for labor and delivery services, so women living on the reservation are referred to Billings after 30 weeks gestation, which can be more than an hour drive away. In emergency situations, women have delivered at the emergency room of Big Horn County Memorial Hospital in Hardin. Several focus group participants shared stories of women they knew who had experienced pregnancy loss or preterm births because they were not able to detect a problem with the pregnancy early enough. Although the Crow-Northern Cheyenne Hospital did not have an ultrasound technician at the time of the site visit, they have since hired someone for this position. Historically, midwifery was a common practice within the Crow tribe2, but none of the focus group participants had used a midwife. One interviewee noted that St. Vincent in Billings has an active midwifery clinic and provides prenatal care to many women in the area. IHS is also working to restart their midwifery program at the Crow-Northern Cheyenne Hospital. The hospital employs one female midwife who is available for family planning services and has plans to hire another. Transportation is a significant barrier for women traveling for prenatal or pregnancy-related services. Some focus group participants noted they try to use the Crow Transit bus, but it leaves Crow Agency (the seat of the reservation) once a day at 6:00 am and is reportedly unreliable. In addition, many areas of the reservation are over an hour away from Crow Agency. Medicaid will pay for transportation costs for pregnancy care, but that is of little use if reliable transportation is unavailable. One focus group participant said she has had to hitchhike to and from Billings to get to her health care appointments.
“There is a lack of providers and care continuity – women get confused because they do not see the same provider throughout their pregnancy or for other health services and they do not communicate with each other.”
–Lucille Other Medicine, Program Assistant, Messengers for Health
Several statewide and Crow-specific maternal health programs have existed in the past. The state used to administer the Montana Initiative for the Abatement of Infant Mortality (MIAMI) Project to increase access to prenatal, delivery, and postpartum care for high-risk pregnant women and their infants. Additionally, the Crow Healthy Mothers and Healthy Babies program previously provided outreach and education to pregnant women. Recently, the Montana Healthcare Foundation has supported Native American perinatal behavioral health program development efforts statewide, but it is unknown how this will impact the Crow tribe. BVHC provides fully-integrated care for pregnant women including access to substance use treatment with on-site behavioral health providers.
| Initiative: Crow Indian Health Service Maternal Child Health Coordinator |
| The IHS Crow-Northern Cheyenne Hospital recently hired a Maternal Child Health (MCH) Coordinator to increase utilization of prenatal care and prepare for when the hospital is approved to begin deliveries again. In this role, the MCH Coordinator performs prenatal intake and education, arranges for Medicaid-funded breast pumps, labs, and ultrasounds, and provides case management and postpartum contraception. |
Substance Use Disorder and Pregnancy
Substance use disorder is a serious concern on the Crow reservation, and a recent policy announced by the Big Horn Attorney’s office to “crack down” on pregnant women using drugs or alcohol has made outreach and engagement even more difficult. Interviewees reported high rates of substance use among youth and adults on the reservation. Focus group participants explained that children whose parents have substance use disorders (SUD) are often sent into foster care out of state, and interviewees said that grandmothers often step in to raise young grandchildren in the absence of parents who are dealing with addiction. BVHC has a robust SUD treatment program for pregnant women. The clinic conducts outreach and screening, performs a warm handoff to internal providers for treatment, and offers Medication-Assisted Treatment (MAT) for those with opioid use disorders. Messengers for Health, a health outreach and education program on the Crow reservation, also teaches substance use prevention to youth within the schools. Still, interviewees reported significant stigma around substance use during pregnancy. In January 2018, the Big Horn County Attorney announced he would seek to jail pregnant women found to be using drugs or alcohol. In response to strong backlash, the attorney has backed away from the policy (although has not yet changed it as of October 2019) and has been participating in workgroups about how to provide holistic care to those with SUD. One interviewee noted the attorney’s actions had a noticeable “chilling effect” on women presenting for prenatal, family planning, and postpartum care and made outreach to these women even more challenging than it already was.
Contraceptive Provision, Access, and Use
The full range of contraceptive methods are available at IHS; however, contraception use is reportedly low, particularly among teens, contributing to the Crow tribe having the highest teen pregnancy rate in Montana. Lack of transportation, confidentiality concerns, cultural beliefs, lack of awareness, and historical mistrust of health care providers among the Crow population are barriers to care.
Provider shortages, traditional beliefs, and a lack of health literacy all contribute to the higher rates of teen pregnancy among Crow youth. The overall Montana teen birth rate is 26 births per 1,000. Big Horn County, where Crow reservation is located, is ranked highest in the state for teen births, at 85 births per 1,000. Contraceptive care for low-income women is available at IHS and various providers in Hardin and Billings. However, interviewees explained that babies are viewed as a blessing in many traditional families, even for teens, and given this perspective, family planning is not always prioritized. Low health literacy was also reported as a limitation to contraceptive use.
“Due to our cultural ways and strong values for life, most Crow people may not actively engage in family planning. However, there are some families especially from our younger generations who do family planning, which I feel is wise because of today’s economy.”
–Alma McCormick, Executive Director, Messengers for Health“Health literacy about puberty, menstruation and birth control is a big barrier, and many young women do not know they can be their own advocates.”
–Nona Main, former Health Educator, Planned Parenthood of Montana
A legacy of forced sterilization and experimentation, confidentiality concerns, and turnover at the IHS administration has led to a distrust of IHS and other western providers. Several interviewees discussed the lasting impact the history of nonconsensual research and forced sterilization has had on the Crow tribe. Native American women,3 including Crow women,4,5 were sterilized without their consent by U.S. government employees as recently as 50-60 years ago.
Confidentiality concerns are also a significant barrier to family planning and STI testing services on the reservation, as is common in many small communities. Several interviewees expressed concern that patients’ relatives and friends working at IHS do not always adhere to robust confidentiality standards. In addition, turnover in the service unit director position at IHS and within the tribal administration also serves as a barrier to social service and health education programs such as Messengers for Health, whose leaders must gain each new administration’s buy-in for their existing programs.
St. Vincent is the only religious health system in Billings, and in practice, it has few restrictions on contraception, although it recently stopped performing tubal ligation. There are two major health systems in the area, St. Vincent and Billings Clinic, both of which provide the full range of contraceptive methods including LARC. However, St. Vincent stopped providing tubal ligation in June 2019, and interviewees reported that St. Vincent providers often refer to Planned Parenthood for long-acting reversible contraception (LARC), such as IUDs and implants, because of their own beliefs or they lack experience due to low volume. Several focus group participants noted they typically do not go to St. Vincent for contraception simply because Billings Clinic, the other major hospital in the area, is closer to the reservation.
| Initiative: Messengers for Health’s lay health advisor approach to cancer prevention |
| Messengers for Health started in 1996 as a partnership between members of the Crow Nation and a Montana State University faculty member to address health equity, and in particular, the high rates of cancer among the Crow tribe. According to their website, cancer is the leading cause of death on the Crow reservation, and there are low rates of preventive screening. Using a lay health advisor approach, the organization relies on “messengers” from the community to educate the Crow people about risk factors for cancer and assist them in seeking out preventive screening. Their first program focused on educating Crow women and girls, from 5th to 12th grade, about cervical cancer using a culturally competent curriculum. Messengers for Health also started the Crow Warriors for Health program to increase colorectal, prostate and lung cancer knowledge among men within the community. The program encourages Crow men to lead educational outreach activities using culturally appropriate materials. They also assist Crow men with scheduling appointments, determining eligibility to cover any screening or treatment costs, and transportation or gas vouchers for follow-up visits. In Crow culture, any mention of cancer was considered taboo, but due to the work of Messengers for Health, women and men are now discussing cancer openly and regularly seeking preventive screenings such as pap tests, mammograms, and colorectal screenings. The organization also has a program providing sex education to youth in schools, a stroke prevention campaign, and a chronic illness and self-care management project. |
Sex Education Policy and Provision
Sex education is mostly discussed informally in the home, with intermittent efforts to provide formal education in schools. Education about STIs and HIV is lacking, and there is significant stigma associated with HIV.
Sex education on the Crow reservation is influenced by strong cultural and gender roles within the Crow tribe. As some interviewees described it, Crow families are closely knit, and the tribe has a tradition of matrilineal kinship. Older women, especially, adhere to strong beliefs in modesty and treat topics about sexuality, family planning and abortion as taboo. Crow girls often look to their grandmothers for education on these issues. This is significant given many grandmothers are raising their grandchildren. However, family planning is not typically prioritized, and focus group participants said many girls and young women do not know where to get contraception. Two focus group participants shared they each had friends who became pregnant at 11 and 14 years old, respectively. Abortion was not considered an option for either, and someone else raised the babies for them. “This is common,” said one focus group participant.
“Most sex education is informal and focused more on girls than boys. They’re taught to behave with modesty and ‘keep themselves out of trouble’.”
–Lucille Other Medicine, Program Assistant, Messengers for Health
| Initiative: Planned Parenthood’s online contraceptive app |
| Since October 2018, Planned Parenthood of Montana offers a mobile app to conduct online contraceptive visits for residents of Montana over the age of 18. Using the app, new or existing patients can message a provider to discuss their medical history and get a prescription for oral contraceptives. Pills cost $24 per pack for a one month supply and arrive by mail to the patient within a couple days. However, Medicaid does not currently cover the service, and Planned Parenthood staff said that private plans in the state also do not cover it because they have an existing contracted telehealth provider and do not want to use another one. The service is currently underutilized, perhaps due to a lack of outreach and affordability. |
Outside of the family, several school-based sex education programs exist but are not adopted consistently. Messengers for Health was invited into schools on the reservation by Crow women in the community to educate girls from 5th to 12th grade about sexual risk factors for cervical cancer using a culturally competent curriculum. Topics reflected cultural values and covered self-respect, peer pressure, substance use, and discussions about what students have heard about sex from their families. Over the years, adoption of this program has varied depending on level of support from the Crow administration. Planned Parenthood in Billings employed a Health Educator who is Native American and has worked with several schools in and around the Crow reservation. In several Crow communities on the reservation, she taught the culturally-tailored “Making Proud Choices” curriculum to high school students. In one town, she was only allowed to work with female students due to Crow cultural norms. However, in another community, both boys and girls participated. Interviewees felt the latter community’s remoteness from Crow Agency and overall lack of services led to greater appreciation and acceptance of the education and outreach. Interviewees added that there appears to be more openness to this type of education as staff gets younger and more aware of these issues, particularly as they relate to substance use.
STI and HIV rates are on the rise, and there is significant stigma associated with HIV. Interviewees report that STI rates have increased dramatically in both Big Horn and Yellowstone counties. The STI incidence rate (including chlamydia, gonorrhea, and syphilis) for Big Horn County, where most of the Crow reservation is located, was 5,484.9 per 100,000 in 2017 compared to 551.6 per 100,000 across the entire state of Montana. Due to confidentiality concerns and lack of awareness, many people do not get tested for STIs or HIV. Stigma, particularly related to HIV, is a growing concern as HIV rates increase due to drug use. Several interviewees said HIV patients travel to Billings for their care to avoid confidentiality concerns at IHS. Another interviewee noted that 20 years ago, tribal public health nurses would go out into the community and provide condoms and testing, but that IHS does not currently do any outreach related to STIs or HIV. Focus group participants said the providers they see in Billings do talk with them about STIs and provide information about prevention and testing services.
“I think people are afraid people will find out if they have [HIV] so they don’t go to get tested.”
–Focus group participant
Sexual and Domestic Violence
As in many tribal communities, the Crow tribe has a history of sexual abuse and domestic violence dating back to colonization and boarding schools. In 1871, the U.S. Congress declared Native Americans wards of the U.S. government and began a forced assimilation campaign to integrate children into the dominant white culture. Native American children were taken from their families at the age of 4 or 5 and placed in government and Catholic church-run boarding schools where communication with their families was prohibited. Many suffered physical and sexual abuse. In the absence of healing, the effects on the community continue, and is exacerbated by substance use, limited access to employment, and poverty.
Interviewees noted that sexual and domestic violence remain major problems in current times. The Crow Agency has a domestic violence program that supports women who are victims of abuse. Advocates visit women who are referred by the police to connect them with needed services including a safe house, restraining orders, and health care. However, interviewees and focus group participants noted that women may wait a long time for the police to come if they call from the reservation, so these advocates often encourage women to go to Billings. Issues with law enforcement jurisdiction can also complicate problems. The FBI, county sheriff, and tribal police all have overlapping roles on these issues, which can result in re-traumatizing victims and missteps in investigations. One interviewee shared a story of an FBI agent barging in on a victim’s family planning appointment. Another provider pointed to domestic violence’s impact on women’s reproductive choices in instances where abusers prohibit women from using contraception, causing pregnancy and increased dependency on the abuser. Focus group participants also raised the issue of the disappearance of tribal members as a key concern of their community. Native Americans make up less than 7% of the state’s population but accounted for 26% of all missing person reports between 2016 and 2018, and Native women and girls account for 30-40% of human and sex trafficking victims in Montana. The emergency department at the Crow-Northern Cheyenne Hospital has Sexual Assault Nurse Examiner (SANE)-trained nurses, and all of the hospital staff have been trained in trauma-informed care. Interviewees also discussed the importance of the availability of female providers to reduce barriers for victims seeking family planning and reproductive health care.
Access to Abortion Counseling and Services
Crow families typically do not discuss abortion, and many are opposed to it. The nearest abortion services are located in Billings.
Many Crow women and girls do not consider abortion an option, and often relatives will raise the child. Some Crow women used to practice abortion using plants/herbs. In fact, women from other tribes used to come to Crow communities for this purpose. However, these practices are not common today due to general opposition to abortion. The Christian church is very influential on the Crow reservation, and abortion is considered taboo due to both traditional and religious beliefs. Interviewees explained that babies are considered a blessing among traditional Crow families, regardless of the circumstance of the pregnancy. When needed, relatives will step in and raise the child. A few of the focus group participants noted they knew of a friend who had an abortion, but most were reluctant to discuss it or said they did not believe in abortion, and it had never crossed their mind as an option.
Abortion counseling and services are not available on the reservation, but there are two Planned Parenthood locations in Billings that offer abortion services. Montana does not have any of the state-level abortion restrictions that some other states have, such as waiting periods, mandated parental involvement, or limitations on publicly-funded abortions. However, IHS providers are federal employees, and therefore do not provide abortions. Some providers make abortion referrals to Planned Parenthood in Billings. Under court order, Montana’s Medicaid program is one of 15 state Medicaid programs that uses state funds to pay for abortion beyond the circumstances of rape, incest, and life endangerment permitted by the federal Hyde amendment, and Planned Parenthood reported they have had no issues receiving reimbursement.
Even though Big Horn County is considered “blue in a red state,” as one interviewee put it, there is strong anti-abortion sentiment in Big Horn and Yellowstone Counties. As a result, women who are seeking abortions, and providers who want to refer them, do so with discretion. Despite abortion being highly stigmatized in the area, Planned Parenthood staff reported they do see Crow patients seeking abortion services.
“There is a lot of confusion about what is legal and what is not [regarding abortion], on both the provider and patient side.”
–Dr. David Mark, CEO, Bighorn Valley Health Center
Conclusion
Montana offers broad coverage for reproductive health services through the expanded Medicaid program and family planning waiver. Medicaid expansion has significantly improved the financial health of both IHS and non-tribal providers, leading to increased capacity to meet the overall health care needs of the Crow tribal community. Tribal members can access most methods of contraception at IHS service units on the reservation at no cost. However, there are not enough providers to meet the reproductive health care needs of Crow women on the reservation. Confidentiality concerns, historical mistrust of the health care system, and lack of transportation are barriers to care. Many topics related to contraception, abortion, and STIs are not discussed openly, contributing to the highest teen pregnancy rates in the state and high rates of STIs. However, several organizations, including Messengers for Health and Planned Parenthood of Montana have had success with outreach and education in schools, and continue to look for ways to engage youth. Substance use also influences family roles, particularly in cases where grandmothers step in to raise children when parents are absent due to challenges with substance use. Sexual and domestic violence affects many Crow families; interviewees reported that enhancements to both victims support services and law enforcement systems are needed to address these issues.
Acknowledgements
The authors thank all of the interviewees that participated in the structured interviews for their insights, time, and helpful comments. All interviewees who agreed to be identified are listed below. The authors also thank the focus group participants, who were guaranteed anonymity and thus are not identified by name.
Nona Main, former Health Educator, Native Outreach Project, Planned Parenthood of Montana
David Mark, MD, CEO, Bighorn Valley Health Center
Timothy P. McCleary, Ph.D., Department Head, General Studies Department, Little Big Horn College
Alma McCormick, Executive Director, Messengers for Health, Crow Nation
Lucille Other Medicine, MSW, Program Assistant, Messengers for Health, Crow Nation
