A View from the States: Key Medicaid Policy Changes: Results from a 50-State Medicaid Budget Survey for State Fiscal Years 2019 and 2020
Delivery Systems
| Key Section Findings |
| As of July 1, 2019, among the 40 states with comprehensive risk-based managed care organizations (MCOs), 33 states reported that 75% or more of their Medicaid beneficiaries were enrolled in MCOs. States continue to carve-in behavioral health services to MCO contracts and nearly all states have managed care quality initiatives in place such as pay for performance or capitation withholds. Medicaid programs have been expanding their use of other service delivery and payment reform models to achieve better outcomes and lower costs. Forty-four states had one or more delivery system or payment reform initiatives in place in FY 2019 (most often patient centered medical homes or ACA Health Homes) with 14 states adding or expanding delivery system reforms in FY 2020.
What to watch:
Tables 2 through 5 include more detail on the populations covered under managed care (Tables 2 and 3), behavioral health services covered under MCOs (Table 4), and managed care quality initiatives (Table 5). Table 6 contains more detailed information on emerging delivery system and payment reform initiatives in place in FY 2019 and new or expanded initiatives in FY 2020. |
Managed Care
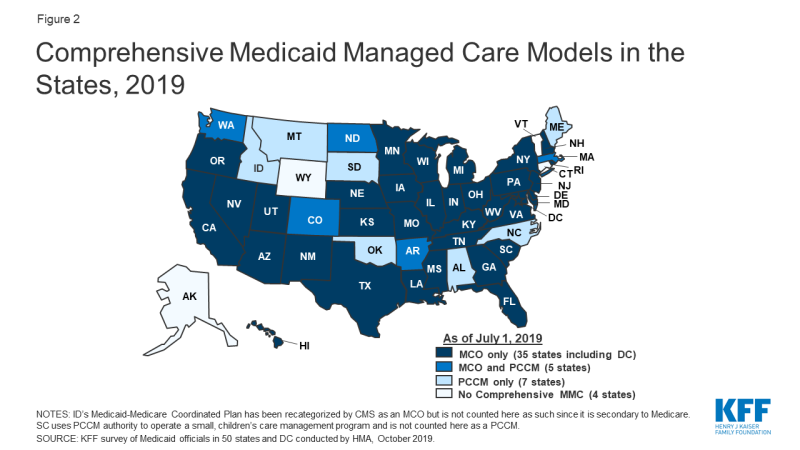
Capitated managed care remains the predominant delivery system for Medicaid in most states. As of July 2019, all states except four – Alaska, Connecticut,1 Vermont,2 and Wyoming – had some form of managed care (comprehensive risk-based managed care organizations (MCOs) and/or primary care case management (PCCM)) in place. As of July 2019, 40 states were contracting with MCOs, up from 39 states last year. Twelve states reported operating a PCCM program, down two states from last year. PCCM is a managed FFS based system in which beneficiaries are enrolled with a primary care provider who is paid a small monthly fee to provide case management services in addition to primary care. For purposes of this report, states contracting with “PCCM entities”3 are also counted as offering a PCCM program.
Of the 47 states that operate some form of managed care, five operate both MCOs and a PCCM program while 35 states operate MCOs only and seven states operate PCCM programs only4 (Figure 2 and Table 2). In total, 28 states contracted with one or more limited benefit prepaid health plans (PHPs) (unchanged from 2018) to provide Medicaid benefits including, behavioral health care, dental care, vision care, non-emergency medical transportation (NEMT), or long-term services and supports (LTSS).
Populations Covered by Risk-Based Managed Care
Among the 40 states with MCOs, 33 states reported that 75% or more of their Medicaid beneficiaries were enrolled in MCOs as of July 1, 2019. This is unchanged from last year’s survey and includes nine of the ten states with the largest total Medicaid enrollment. These nine states (California, New York, Florida, Texas, Pennsylvania, Illinois, Ohio, Michigan, and Washington) account for over half of all Medicaid beneficiaries across the country (Figure 3 and Table 2).5
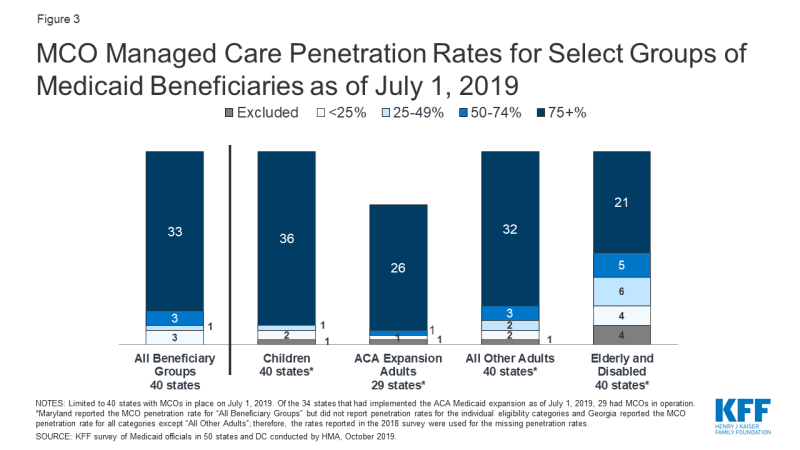
Figure 3: MCO Managed Care Penetration Rates for Select Groups of Medicaid Beneficiaries as of July 1, 2019
Children and adults, particularly those enrolled through the ACA Medicaid expansion, are much more likely to be enrolled in an MCO than elderly Medicaid beneficiaries or persons with disabilities. Thirty-six6 of the 40 MCO states reported covering 75% or more of all children through MCOs. Of the 34 states that had implemented the ACA Medicaid expansion as of July 1, 2019, 29 were using MCOs to cover newly eligible adults.7 The large majority of these states (26 states) covered more than 75% of beneficiaries in this group through capitated managed care, including New Hampshire that ended its Section 1115 premium assistance waiver at the end of CY 2018 and transitioned its Qualified Health Plan-enrolled members to MCOs.8 Thirty-two of the 40 MCO states reported covering 75% or more of low-income adults in pre-ACA expansion groups (e.g., parents, pregnant women) through MCOs. In contrast, the elderly and people with disabilities were the group least likely to be covered through managed care contracts, with only 21 of the 40 MCO states reporting coverage of 75% or more such enrollees through MCOs (Figure 3).
Of the five states with both MCOs and PCCM programs, PCCM programs cover a larger share of beneficiaries than MCOs in three of these states. As of July 1, 2019, Arkansas’ recently implemented MCO program (described further below) covered only 5% of Medicaid beneficiaries with the rest of the Medicaid population divided between PCCM (45%) and fee-for-service (50%); over 90% of Colorado’s enrollees remained in the PCCM program, which is the foundation of the state’s “Accountable Care Collaboratives;” and North Dakota covered 44% of its Medicaid enrollees in its PCCM program compared to 23% of enrollees (all ACA expansion adults) under an MCO contract. In contrast, Massachusetts reported greater MCO enrollment (42%) compared to PCCM (26%) and Washington reported only minimal PCCM enrollment (1%) compared to MCO enrollment (93%).
Arkansas reported implementing an MCO program for the first time in FY 2019 and North Carolina reported plans to implement an MCO program for the first time in FY 2020. In March 2019, Arkansas began making actuarially sound “global payments” to “Provider-led Arkansas Shared Savings Entities” (PASSEs) that serve Medicaid beneficiaries who have complex behavioral health and intellectual and developmental disabilities (I/DD) service needs. In FY 2020, North Carolina will launch new MCO “Standard Plans” with mandatory enrollment for most population groups (about 1.6 million enrollees). Conversely, Alaska reported that it had halted its previous plan to implement an MCO arrangement in FY 2020 to serve one geographic area (Anchorage and the Mat-Su Valley). Only one state reported a policy change that reduces the state’s reliance on the MCO model of managed care: Indiana reported that presumptively eligible members are now initially covered under FFS rather than being enrolled in MCOs.
Populations with Special Needs
For geographic areas where MCOs operate, this year’s survey asked MCO states whether, as of July 1, 2019, certain subpopulations with special needs – excluding those dually eligible for Medicaid and Medicare or receiving long-term services and supports – were enrolled in MCOs for their acute care services on a mandatory or voluntary basis or were always excluded (Exhibit 5 and Table 3).
Consistent with results from past surveys, pregnant women were most likely to be enrolled on a mandatory basis while persons with I/DD were among the least likely to be enrolled on mandatory basis. As a group, seniors were most likely to be excluded (although a number of states noted that non-dual, non-LTSS seniors constitute a relatively small subpopulation). Foster children were most likely to be enrolled on a voluntary basis, although they were enrolled on a mandatory basis in a larger number of states.
| Exhibit 5: MCO Enrollment of Populations with Special Needs, July 1, 2019 (# of States) |
|||||||
| Non-Dual/Non-LTSS: | |||||||
| Pregnant women | Medically Fragile/ Technology Dependent Children | Foster Children | Persons with SMI/SED | Persons with I/DD | Persons w/ physical disabilities | Seniors | |
| Always mandatory | 34 | 20 | 22 | 26 | 19 | 24 | 23 |
| Always voluntary | 2 | 7 | 8 | 5 | 6 | 4 | 3 |
| Varies | 3 | 8 | 7 | 7 | 8 | 8 | 5 |
| Always excluded | 1 | 5 | 3 | 2 | 7 | 4 | 9 |
| Notes: “SMI/SED” – persons with serious mental illness or serious emotional disturbance, “I/DD” – persons with intellectual and developmental disabilities. | |||||||
This year’s survey also asked MCO states to comment on their acute care MCO enrollment policies for dual eligibles and persons receiving LTSS. Because these two characteristics often overlap, all state responses could not be sorted into discrete categories. At least 11 states, however, reported that both dual eligibles and persons receiving LTSS had their Medicaid acute care services covered on a mandatory basis under an MCO arrangement (Arizona, Delaware, Hawaii, Iowa, Kansas, Nebraska, New Hampshire, New Jersey, New Mexico, Tennessee, and Virginia). Conversely, nine states reported that both dual eligibles and persons receiving LTSS were always excluded from acute care MCO coverage (Georgia, Indiana, Louisiana, Missouri, Mississippi, North Dakota, Nevada, Wisconsin, and West Virginia). Also, states with Financial Alignment Initiatives for dual eligibles in addition to other managed care programs often cited varying enrollment criteria for dual eligibles.
Acute Care Managed Care Population Changes
In both FY 2019 and FY 2020, a few states reported actions to increase enrollment in acute care managed care, reflecting full or nearly full MCO saturation in most MCO states. As described above, Arkansas and North Carolina reported implementing, or plans to implement, an MCO program for the first time in FY 2019, and FY 2020, respectively. Of the 40 states with MCOs already in place as of July 1, 2019, six states in FY 2019 and eight states in FY 2020 indicated that they made specific policy changes to increase the number of enrollees in MCOs through voluntary or mandatory enrollment of new groups into MCOs, or mandatory enrollment of specific eligibility groups that were formerly enrolled on a voluntary basis (Exhibit 6). Thirty-eight states reported that acute care MCOs were operating statewide as of July 2019. The remaining two MCO states without statewide programs (Colorado and Nevada) did not report a geographic expansion planned for FY 2020.
| Exhibit 6: Medicaid Acute Care Managed Care Population Expansions, FY 2019 and FY 2020 | ||
| FY 2019 | FY 2020 | |
| Geographic Expansions | — | — |
| New Population Groups Added | DE, MS, NH, OH, PA, VA | DE, IL, NY, OH, PA, TN, WV |
| Voluntary to Mandatory Enrollment | — | NE, NY |
| Implementing an MCO program for the first time | AR | NC |
In FY 2019 and FY 2020, states expanded MCO enrollment (either voluntary or mandatory) to other groups including persons with ID/DD (Delaware and New York), special needs children, children with SED, or SSI children (Illinois, Mississippi, Tennessee), expansion adults transitioning from the state’s premium assistance program to MCO coverage (New Hampshire), children in foster care (New York and West Virginia), workers with disabilities, persons receiving Specialized Recovery Services, and persons meeting the nursing facility level of care criteria (Ohio), and persons with third party liability coverage (Virginia). Also, Pennsylvania reported the addition of full benefit dual eligibles and individuals receiving LTSS to acute care managed care by continuing the geographic phase-in of its Community HealthChoices (CHC) MCO program that combines both acute care and LTSS.
Only two states made enrollment mandatory for a specific eligibility group that was formerly enrolled on a voluntary basis: in FY 2020, Nebraska is making enrollment mandatory for refugee resettlement and state disability assistance enrollees, and New York is making enrollment mandatory for participants in its 1915(c) HCBS Children’s waiver (unless eligible for another enrollment exception).
Services Covered Under MCO Contracts
Behavioral Health Services Covered Under MCO Contracts
Although MCOs are at risk financially for providing a comprehensive set of acute care services, nearly all states exclude or “carve-out” certain services from their MCO contracts, frequently behavioral health services. States with acute care MCOs were asked to indicate whether specialty outpatient mental health (MH) services, inpatient mental health services, and outpatient and inpatient substance use disorder (SUD) services are always carved-in (i.e., virtually all services are covered by the MCO), always carved-out (to PHP or FFS), or the carve-in status varies by geographic or other factors. Consistent with results from last year’s survey, more than half of the 40 MCO states reported that specific behavioral health service types were carved into their MCO contracts, with specialty outpatient mental health services somewhat less likely to be carved in (Exhibit 7 and Table 4).
| Exhibit 7: MCO Coverage of Behavioral Health, July 1, 2019 (# of States) |
||||
| Specialty Outpatient MH* | Inpatient MH | Outpatient SUD | Inpatient SUD | |
| Always carved-in | 23 | 28 | 29 | 29 |
| Always carved-out | 10 | 7 | 7 | 6 |
| Varies | 7 | 5 | 4 | 5 |
| *“Specialty outpatient mental health” services mean services used by adults with Serious Mental Illness (SMI) and/or youth with serious emotional disturbance (SED), commonly provided by specialty providers such as community mental health centers. | ||||
Eight states in FY 2019 and nine states in FY 2020 reported changes in how behavioral health benefits are delivered under MCO contracts:
- Four states in FY 2019 (Mississippi, New Jersey, New York, and Virginia) and one state in FY 2020 (New Jersey) reported actions to carve certain behavioral health services into their MCO contracts. Ohio reported a full carve-in of behavioral health services as of July 1, 2018.
- Four other states (Kentucky, Nebraska, West Virginia, and Wisconsin) reported plans to add SUD waiver services to their MCO contracts in FY 2020. South Carolina added “in lieu of” SUD IMD (“Institutions for Mental Disease”) services to its MCO contracts in FY 2019 and other SUD services in FY 2020.
- Arizona and Washington reported implementing, or plans to implement, additional integrated MCO contracts in both FY 2019 and FY 2020.
- Mississippi added “in lieu of” free standing psychiatric hospital services to its MCO contracts in FY 2019.
- North Carolina’s “Standard” MCO plans implemented in FY 2020 will cover some behavioral health services, other than certain high intensity services that will continue to be provided by the state’s current behavioral health plans.
Managed Care (Acute and LTSS) Quality, Contract Requirements, and Administration
Quality Initiatives
Over time, the expansion of comprehensive risk-based managed care in Medicaid has been accompanied by greater attention to measuring quality and plan performance and, increasingly, to measuring health outcomes. After years of comprehensive risk-based managed care experience within the Medicaid program, states have become more sophisticated in incorporating quality metrics into the ongoing monitoring of MCOs, and many states now incorporate quality into the procurement process.9
States procure MCO contracts using different approaches; however, most states use competitive bidding, in part because the dollar value is so large. Under these procurements, states can specify requirements and criteria that go beyond price and may expect plans to compete on the basis of value-based payment arrangements with network providers, specific policy priorities such as improving birth outcomes, strategies to address social determinants of health, and/or other specific performance and quality criteria.
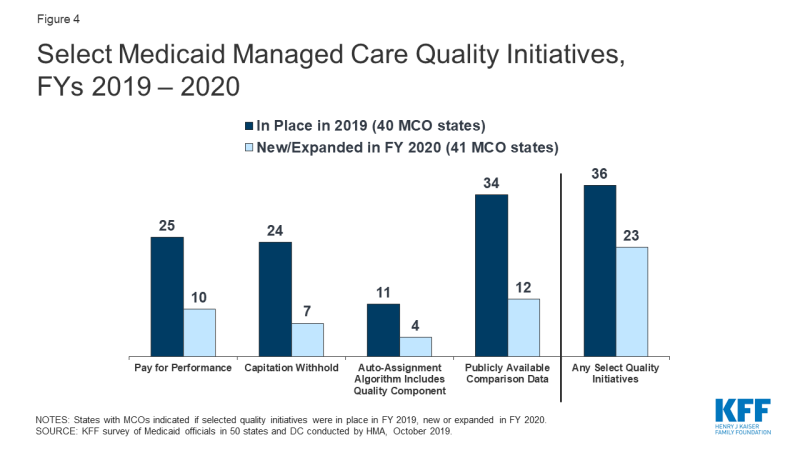
Nearly all MCO states (36 of 40 states) reported using at least one select Medicaid managed care quality initiative in FY 2019 (Figure 4 and Table 5). Two additional states not reporting quality initiatives in 2019 indicated that they had implemented new quality initiatives in FY 2020, bringing the total number to 38 states with at least one of these managed care quality strategies in place. States were asked to indicate whether they had specific managed care quality strategies (acute and/or MLTSS) in place in FY 2019 and to identify newly added or expanded initiatives for FY 2020. The overwhelming majority of states (34 out of 40) reported they made MCO comparison data publicly available in FY 2019. More than half of MCO states reported pay for performance incentives and/or capitation withhold arrangements in place in FY 2019. Fewer states reported use of an auto-assignment algorithm that includes quality performance measures.
In FY 2020, more than half of MCO states (23 states) expect to implement new or expanded quality initiatives (Figure 4). The majority of the actions states plan for FY 2020 represent enhancements or expansions to current quality strategies, rather than implementation of a new strategy. However, five states reported new initiatives in FY 2020. Three states reported implementing a pay for performance strategy (California, Illinois, and New Hampshire) and two states reported implementing a capitation withhold (Mississippi and New Hampshire) for the first time. Utah plans to make acute care MCO comparison data available in FY 2020 through the creation of a public-facing dashboard. Ohio reports transitioning from a pay for performance to a capitation withhold strategy in its acute care programs.10
PERFORMANCE MEASURE FOCUS AREAS
States that employed a pay for performance bonus or penalty, a capitation withhold and/or an auto-assignment quality factor (discussed above) were asked to identify performance measure focus areas linked to these quality incentives (Exhibit 8). Over three quarters of MCO states (31 states) reported using chronic disease management metrics when rewarding or penalizing plan performance. More than half of MCO states reported linking these quality initiatives to perinatal/birth outcome measures (26 states) or mental health measures (24 states). These focus areas are not surprising given the chronic physical health and behavioral health needs of the Medicaid population, as well as the significant share of the nation’s births funded by Medicaid. Over half of MCO states (22 states) tie quality incentives to potentially preventable events (PPEs) and nearly half (17 states) link incentives to value-based purchasing metrics, which is a growing area of focus for states (discussed in more detail below). Twelve states listed “other” focus areas including LTSS-related metrics (e.g., documentation of care goals and interaction with the care team in a dual eligible Financial Alignment Initiative (California)) and HCBS rebalancing (Hawaii). Other states reported incentives or penalties linked to operational metrics such as claims processing timelines and submission of encounter data.
| Exhibit 8: Performance Measure Focus Areas for MCO Incentives | ||
| Performance Area | # of States |
States |
| Chronic Disease Management | 31 | AZ, CA, CO, DC, DE, FL, GA, HI, IA, IL, IN, KS, LA, MA, MI, MN, MO, MS, NE, NJ, NM, NV, NY, OH, OR, PA, RI, SC, TX, WA, WI |
| Perinatal/Birth Outcome | 26 | CA, CO, DC, DE, FL, HI, IL, IN, KS, LA, MI, MO, MS, NE, NH, NJ, NM, NV, OH, OR, PA, RI, SC, TX, VA, WI |
| Mental Health | 24 | CA, CO, FL, GA, HI, IA, IL, IN, KS, LA, MA, MN, MO, NH, NM, NY, OH, OR, PA, RI, SC, TX, WA, WI |
| Potentially Preventable Events | 22 | AZ, CA, DC, DE, FL, GA, IA, LA, MA, MI, MN, MO, NE, NH, NJ, OH, PA, RI, SC, TX, VA, WI |
| Substance Use Disorder | 19 | CO, FL, HI, IL, IN, KS, LA, MA, NH, NM, OH, OR, PA, RI, SC, TX, VA, WA, WI |
| Value-Based Purchasing | 17 | AZ, CA, DE, GA, KS, LA, MI, MN, NH, NM, OH, PA, RI, SC, TN, TX, WA |
| Dental | 13 | AZ, CA, GA, IN, KS, MI, MN, MO, NY, OR, PA, TX, WI |
| Member Satisfaction | 12 | DC, GA, HI, LA, MA, MI, NH, NY, OH, OR, SC, TX |
| Health Info Exchange | 4 | CA, MI, OH, WI |
| Health Disparities | 2 | CA, MI |
| Telehealth | 1 | NY |
| Other | 12 | CA, DE, HI, IA, IL, IN, MA, MI, NE, NV, TN, WI |
| *MD did not report. | ||
State-Mandated Performance Improvement Projects (PIPs)
For contracts starting on or after July 1, 2017, federal regulations mandate that states require each MCO or PHP to establish and implement an ongoing comprehensive quality assessment and performance improvement (QAPI) program for Medicaid services that includes Performance Improvement Projects (PIPs). PIPs may be designated by CMS, by states, or developed by health plans, but must be designed to achieve significant, sustainable improvement in health outcomes and enrollee satisfaction. In this year’s survey, states were asked to indicate whether they mandate MCO PIPs in a particular focus area. Thirty MCO states reported mandating certain PIPs in their MCO and PHP contracts in FY 2019 and four additional states indicated they were adding PIP requirements in FY 2020. The mandated PIP focus areas reported covered a wide range of programmatic topics, including child and adolescent wellness, perinatal/birth outcomes, behavioral health, dental health, chronic disease management, and long-term care, among other areas. Unlike the performance-based incentive initiatives mentioned above, a mandated PIP may not be directly tied to incentives or penalties, but nevertheless represents a performance area of particular importance to the state. Priority areas frequently reported include:
- Maternal and Child Health. Michigan reports requiring an MCO PIP to address racial disparities in the timeliness of prenatal care. Florida’s new MCO contracts require PIPs in the areas of reducing adverse birth outcomes, as well as reducing potentially preventable hospital events, transportation, and mental health or integrating mental health and primary care. In addition to a PIP related to consumer satisfaction, Iowa mandates an MCO PIP related to well child visits for children between 3 and 6 years of age.
- Chronic Care Disease Management. In addition to a PIP related to maternal health, DC also mandates a PIP related to comprehensive diabetes care. With a focus on efforts to reduce health disparities, Ohio reports requiring a PIP related to hypertension control in addition to a PIP on reducing preterm birth/infant mortality.
- Behavioral Health. Massachusetts mandates PIPs that correspond with two quality domains: Behavioral Health – prevention, assessment, and treatment of mental illness, including substance use and other dependencies; and Community Needs Assessment/ Risk Stratification – identifying and assessing priority populations for health conditions and social determinants of health and developing appropriate and timely interventions. In addition to a clinical PIP in the area of either child or perinatal health, Tennessee requires MCOs to implement a behavioral health PIP related to bipolar disorder, major depression, and schizophrenia.
- Long-Term Services and Supports. Pennsylvania MLTSS PIPs include a focus on transitioning beneficiaries from nursing facilities to home and community-based settings and strengthening care coordination. New Jersey MLTSS PIPs include initiatives to reduce falls and address gaps in care. Delaware mandates a PIP related to oral health of LTSS beneficiaries and at least one other MCO-defined PIP related to this population among five required PIPs in its MCO contracts.
MCO Contract Requirements
Alternative [Provider] Payment Models Within MCO Contracts
Value-based purchasing (VBP) strategies are important tools for states pursuing improved quality and outcomes and reduced costs of care within Medicaid and across payers. Generally speaking, VBP strategies include activities that hold a provider or MCO accountable for cost and quality of care.11 This often includes efforts to implement alternative payment models (APMs) which replace FFS/volume-driven provider payments with payment models that incentivize quality, coordination, and value (e.g., shared savings/shared risk arrangements and episode-based payments). Many states included a focus on adopting and promoting APMs as part of their federally-supported State Innovation Model (SIM) projects and as part of delivery system reform efforts approved under Section 1115 Medicaid waivers.12 A number of states are now encouraging or requiring MCOs to adopt APMs to advance VBP in Medicaid; our survey asked about requirements in MCO contracts.
More than half of MCO states (21 states) identified a specific target in their MCO contracts for the percentage of provider payments or plan members that MCOs must cover via APMs in FY 2019 (Exhibit 9). Three additional states plan to add a target percentage in FY 2020. States with targets linked to expenditures reported a wide range of currently required APM percentage targets ranging from a high of 80% (Hawaii) and 75% (Washington) to a low of 10% (Missouri and Wisconsin). Eleven states (Arizona, California, Louisiana, New Hampshire, New Mexico, North Carolina, Oregon, Pennsylvania, South Carolina, Texas, and Washington) reported that their APM targets were linked to the Health Care Payment Learning & Action Network’s (LAN’s) APM Framework that categorizes APMs in tiers.13
In addition, fourteen states reported that their MCO contracts included incentives or penalties for meeting or failing to meet APM targets in FY 2019 (Exhibit 9). Three states reported plans to add penalties or incentives in FY 2020 (DC, New Hampshire, and Oregon).
| Exhibit 9: States that Require MCOs to Meet a Target % for Provider APMs | ||
| # of States | States | |
| In Place FY 2019 | 21 | AZ*, CA, DE*, HI, IA*, LA*, MA, MO*, NE, NH, NM*, NY*, OH*, PA*, RI*, SC*, TN*, TX*, WA*, WI, WV |
| Plan to Begin in FY 2020 | 3 | DC, NC, OR |
| States with an * reported MCO contracts include incentives or penalties for meeting or failing to meet APM targets in FY 2019. While MI did not report an APM target, it did report that a performance incentive related to APM requirements was in place in FY 2019. | ||
In FY 2019, eight states had contracts that required MCOs to participate in a state-directed VBP initiative (e.g., state—administered or directed episode of care or ACO initiative) and seven states planned to do so in FY 2020 (Exhibit 10). For example: California requires MCOs to make payments to Designated Public Hospitals on performance measures in four strategic categories; Illinois plans to require MCOs to participate in its new Integrated Health Home initiative; Ohio requires MCOs to participate in its SIM payment innovation efforts, episode-based payment model, and Comprehensive Primary Care program; Tennessee mandates that MCOs participate in the state’s episodes of care, patient-centered medical home and behavioral health home initiatives; and Virginia is planning to implement bundled payments for maternity and asthma that MCOs will be required to implement.
Further, 12 states in FY 2019 required MCOs to develop a VBP strategy within state-specified guidelines and five states planned to do so in FY 2020 (Exhibit 10). For example: Arizona requires its MCOs to develop strategies within the LAN-APM categories 2B and above; Kansas requires MCOs to implement VBP models that expand service coordination, increase employment, and provide better outcomes for foster children; Oregon requires its MCOs to develop new or expanded VBP efforts in specified care delivery focus areas; and Utah will require MCOs to adopt a VBP strategy to address hypertension.
| Exhibit 10: State Requirements for MCO VBP Initiatives | |||||
| Require MCOs to: | FY 2019 | FY 2020 | |||
| Participate in a state-directed VBP initiative | 8 States | CA, FL, GA, IA, MN, OH, RI, TN | 7 States | IL, KS, LA, MO, MS, PA, VA | |
| Develop a VBP strategy within state-specified guidelines | 12 States | AZ, DE, GA, HI, IA, KS, LA, MI, MN, NM, NY, RI, | 5 States | MO, NH, OR, PA, UT | |
Administrative Policies
Minimum Medical Loss Ratios
The Medical Loss Ratio (MLR) reflects the proportion of total capitation payments received by an MCO spent on clinical services and quality improvement. CMS published a final rule in 2016 that requires states to develop capitation rates for Medicaid to achieve an MLR of at least 85% in the rate year, for rating periods and contracts starting on or after July 1, 2019. Also, contracts taking effect on or after July 1, 2017 must include a requirement for plans to calculate and report an MLR.14 The 85% minimum MLR is the same standard that applies to Medicare Advantage and private large group plans. There is no federal requirement for Medicaid plans to pay remittances to the state if they fail to meet the MLR standard, but states have discretion to require remittances.
States were asked whether they require MCOs that do not meet the minimum MLR requirement to pay remittances. Twenty-four states reported that they always require MCOs to pay remittances, while six states indicated they sometimes require MCOs to pay remittances (Exhibit 11). States reporting that they sometimes require remittances often limit this requirement to certain MCO contracts – for example, MCO contracts for the adult expansion population. One state (South Carolina) reported allowing an exception to the remittance requirement if an MCO achieved a high National Committee for Quality Assurance (NCQA) health insurance plan rating.15
| Exhibit 11: Medicaid MCO Minimum Medical Loss Ratio (MLR) Remittance Requirements as of July 1, 2019 | ||
| # of States | States | |
| State always requiring remittance | 24 | CO, DE, IA, IL, IN, KY, LA, MD, MI, MN, MO, MS, NE, NH, NJ, NM, NV, OR, PA, RI, UT, VA, WA, WV |
| State sometimes requiring remittance | 6 | AR, CA, MA, NY, OH, SC |
PCCM and PHP Program Changes
Primary Care Case Management (PCCM) Program Changes
Of the 12 states with PCCM programs, three reported enacting policies to increase PCCM enrollment in FY 2019 or FY 2020. Colorado reported growth in its PCCM-based Accountable Care Collaboratives in FY 2019 when it implemented a mandatory enrollment policy and Idaho reported that implementation of the ACA Medicaid expansion in January 2020 would increase PCCM enrollment. Also, Alabama reported implementing two new PCCM programs that rely on contracts with PCCM entities:
- In FY 2019, Alabama implemented the “Integrated Care Network” (ICN) program that provides enhanced case management, education, and outreach services to most LTSS recipients in both HCBS and institutional settings.
- In FY 2020, Alabama reported plans to replace its current PCCM program (Patient 1st) and Maternity PHP program with a new PCCM entity program (the Alabama Coordinated Health Network) that will cover care coordination services.
Three states (California, North Carolina, and Vermont) reported actions to decrease enrollment in a PCCM program in FY 2019 or FY 2020. California and Vermont ended their PCCM programs in FY 2019 and North Carolina will be transitioning many PCCM enrollees to its new MCO program in FY 2020.
Limited-Benefit Prepaid Health Plans (PHP) Changes
Over half of states (28 states) reported contracting with at least one PHP as of July 1, 2019. In this year’s survey, the 28 states were asked to indicate whether certain services (listed in Exhibit 12 below) were provided under these arrangements. The most frequently cited services provided (of those included in the question) were dental services (15 states), followed by outpatient mental health services (14 states), and inpatient mental health, outpatient SUD treatment services, and NEMT (13 states each).
| Exhibit 12: Services Covered Under PHP Contracts, July 1, 2019 | ||
| # of States | States16 | |
| Dental | 15 | AR, CA, FL, IA, ID, LA, MI, NE, NV, OR, RI, TN*, TX, UT, WI |
| Outpatient Mental Health | 14 | CA, CO, HI, ID, LA, MA, MI, NC, OR, PA, TN*, UT, WA, WI |
| Inpatient Mental Health | 13 | CA, CO, HI, LA, MA, MI, NC, OR, PA, TN*, UT, WA, WI |
| Outpatient SUD Treatment | 13 | CA, CO, ID, LA, MA, MI, NC, OR, PA, TN*, UT, WA, WI |
| Non-Emergency Medical Transportation (NEMT) | 13 | AR, FL, IN, KY, ME, MI, NJ, OK, RI, TN*, TX, UT, WI |
| Inpatient SUD Treatment | 11 | CA, LA, MA, MI, NC, OR, PA, TN*, UT, WA, WI |
| Long-Term Services and Supports | 6 | ID, MI, NC, NY, TN*, WI |
| Vision | 2 | TN*, WI |
| * In addition to separate dental and vision PHPs, TN contracts with a non-risk PHP to provide comprehensive benefits (physical health, behavioral health and LTSS) to children who are in foster care, receive Supplemental Security Income (SSI), or receive care in certain institutional settings. | ||
Four states reported implementing policies to increase PHP enrollment in FY 2019 or FY 2020. Three states (Florida, Utah, and Rhode Island) reported new or expanded dental PHPs in FY 2019 or planned for FY 2020 and Idaho reported that implementation of the ACA Medicaid expansion in FY 2020 would increase PHP enrollment.
Eight states also reported actions that decreased PHP enrollment in FY 2019 or FY 2020. Alabama reported plans to end its maternity care PHP (when its new PCCM-entity program is implemented); Hawaii reported that as of July 1, 2018, its behavioral health PHP contract includes stricter requirements for contacting hard to engage members which is expected to slightly reduce PHP enrollment; Kentucky reported that it is planning to eliminate methadone treatment-related NEMT coverage for most adults (excluding pregnant women and former foster care youth); North Carolina reported that many members will shift to integrated Standard Plans when they are implemented in FY 2020, reducing enrollment in the state’s behavioral health PHPs; Oregon reported that one behavioral health PHP was ending its state contract in FY 2020; Tennessee reported that in FY 2020, SSI children will be assigned to an MCO rather than its non-risk PHP that provides comprehensive benefits; Texas reported plans to transition from a NEMT brokerage model to an MCO carve-in model; Washington reported that enrollment in its behavioral health PHPs is decreasing as the state converts behavioral health PHPs to fully integrated MCO contracts in additional geographic areas.
In this year’s survey, states with PHPs were also asked to briefly describe PHP contract quality strategies in place in FY 2019 or planned for FY 2020. Nearly two-thirds of states with PHPs reported a variety of quality strategies including tracking of HEDIS and/or other measures; requiring PIPs; incentive payments; withholds tied to performance measures; public reporting of performance results (e.g., report cards or dashboards); imposition of penalties or liquidated damages; and use of APMs.
Social Determinants of Health
Social determinants of health are the conditions in which people are born, grow, live, work, and age that shape health.17 Addressing social determinants of health is important for improving health and reducing longstanding disparities in health and health care. Social determinants of health include but are not limited to housing, food, education, employment, healthy behaviors, transportation, and personal safety.
In April 2017, the CMS Center for Medicare and Medicaid Innovation (CMMI) launched the “Accountable Health Communities” (AHC) Model to implement and test different approaches to support local communities in addressing the health-related social needs of Medicare and Medicaid beneficiaries. The model aims to bridge the gap between clinical and community service providers and is the first CMS innovation model that focuses on social determinants of health.18 As part of this effort, CMS has developed an AHC Health-Related Social Needs Screening Tool.19 There are currently 30 organizations participating in the program, and the release of the first evaluation is anticipated in 2020.20
There has also been increased attention to social determinants of health at the state level, with many states developing strategies to identify and address a range of these issues both within MCO contracts and more broadly outside of managed care.
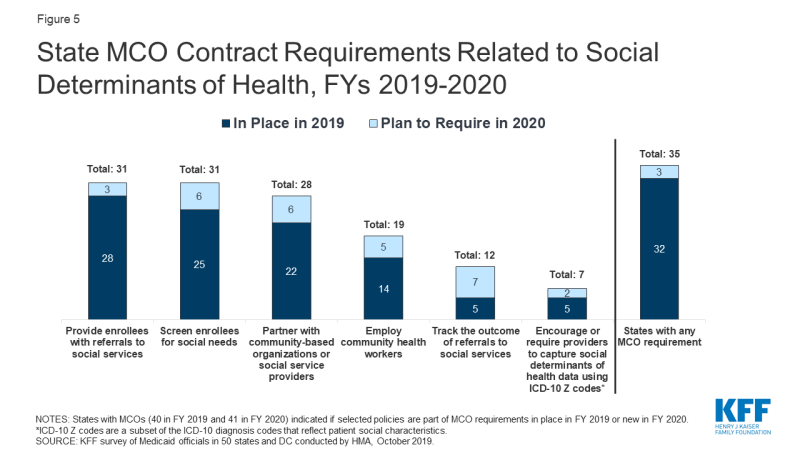
With Medicaid managed care delivery systems operating in 41 states as of FY 2020, many states are leveraging MCO contracts to promote strategies to address social determinants of health. In this year’s survey, MCO states were asked about MCO contract requirements related to social determinants of health in place in FY 2019 or planned for implementation in FY 2020. Over three-quarters of the 41 MCO states as of FY 2020 (35) are leveraging Medicaid MCO contracts to promote at least one strategy to address social determinants of health (Figure 5). As of FY 2020, about three-quarters of MCO states will require MCOs to: screen enrollees for social needs (31 states); provide enrollees with referrals to social services (31 states); or partner with community-based organizations (28 states) (Figure 5). 21 Almost half of MCO states will require MCOs to employ community health workers (CHWs) or other non-traditional health workers (19 states). Approximately a third of MCO states reported that they will require MCOs to track the outcomes of social services referrals (12 states) and fewer states reported that they will require MCOs to encourage/require their providers to capture member social determinants of health data using ICD-10 Z codes22 (7 states) (ICD-10 Z codes are a subset of the ICD-10 diagnosis codes that reflect patient social characteristics).
The following are examples of state MCO initiatives related to social determinants of health:
- Colorado is working with its MCOs to develop a reporting mechanism to track referrals to social services, with the goal of establishing a future performance metric that could be tied to payment.
- Michigan establishes a minimum ratio of CHWs to members and requires MCOs to provide or arrange for CHW services as part of the state’s comprehensive population health management strategy.23
- West Virginia’s enrollment broker collects social determinants of health data for beneficiaries enrolling in managed care and shares this data with MCOs. The MCOs use the data to identify and engage members in need of non-medical supports and refer those members to community services.
| North Carolina: Transitioning to Managed Care with a Focus on Social Determinants of Health |
In FY 2020, North Carolina will implement risk-based, capitated managed care contracts that will eventually cover approximately 1.6 million of its 2 million enrollees. MCOs will be required to:
|
In addition to initiatives through MCOs, many states have strategies outside of their MCO programs (in FFS programs) to address social determinants of health. This year’s survey asked all states about non-MCO initiatives in place in FY 2019 or planned for implementation in FY 2020 related to social determinants of health. About half of all states indicated having non-MCO initiatives in place in FY 2019 related to screening enrollees for social needs, providing enrollees with referrals to social services, or partnering with community-based organizations. Fewer states indicated having non-MCO initiatives in place in FY 2019 to track the outcome of social services referrals, employ community health workers, or encourage/require providers to capture social determinants of health data using ICD-10 Z codes.
The following are state examples of non-MCO initiatives related to social determinants of health:
- Connecticut requires participating practices of its PCMH+ program (an upside-only shared savings initiative) to demonstrate formal agreements with community partners (e.g., housing entities, food pantries). The state also encourages providers to capture ICD-10 Z codes on claims to help identify beneficiaries who may need assistance and connect them to community resources and supports.
- Montana’s Medicaid program will reimburse for services provided by Tribal Community Health Aides, as directed by House Bill 599.26
- Vermont’s Chronic Care Initiative (VCCI) has a licensed case management team that screens members that are engaged with VCCI for SDOH needs. Screening areas include housing, transportation, food security, and utility payments. VCCI employs two outreach coordinators whose primary role is to reach out to all newly enrolled adult members, screen them, and provide brief intervention and navigation to services.
In addition to the MCO and non-MCO social determinants initiatives discussed above, states also highlighted other social determinants of health activity currently underway, including:
- Three states (Arizona, District of Columbia, and Oregon) indicated they are exploring ways to leverage health information exchange (HIE) systems to support a “closed loop” referral process.
- In addition to North Carolina, at least three other states (Connecticut, Ohio, and Pennsylvania) have developed or are in the process of developing standardized screening and assessment tools that include domains related to social determinants of health. Additionally, Indiana’s Medicaid eligibility application includes screening questions related to social determinants of health.
- South Carolina has a statewide pediatric ambulatory care quality improvement collaborative (called Quality Through Technology and Innovation in Pediatrics), funded by the South Carolina Department of Health and Human Services (SCDHHS) and involving over 30 pediatric offices in South Carolina, that promotes social and emotional development, positive parenting, and the promotion of the parent-child bond and parental mental health. The program includes social determinants of health screenings and community resource ideas for practices to screen and refer for non-medical needs.
- Washington’s Section 1115 Medicaid Transformation Project leverages Accountable Communities of Health (ACH) as lead entities to align priorities, partners from the traditional and non-traditional sectors, resources, and action to transform the Medicaid delivery system. While performance outcomes are largely clinical, the design of the effort is based on the premise that social health, public health, and community-based organizations must play a role with the clinical delivery system in order to achieve these outcomes. ACHs in several regions are implementing the Pathways Community Hub model27 for care coordination, which uses template screening and referral systems for social services and CHWs to screen, refer, and complete interventions for select social service needs.
Criminal Justice-Involved Populations
Improving continuity of care for individuals released from correctional facilities into the community is important to ensure that individuals with complex or chronic health conditions, including behavioral health needs, have an effective transition to treatment in the community. It can also help address the opioid epidemic by mitigating the risk of overdose in the period following incarceration.28 In FY 2019, five states required MCOs to provide care coordination services to at least some enrollees prior to release from incarceration, and three additional states reported plans to require care coordination in FY 2020 (Exhibit 13). Several states also reported providing or plans to provide FFS care coordination services to incarcerated persons prior to release.
| Exhibit 13: Providing Care Coordination Services to Enrollees Prior to Release from Incarceration29 | ||||
| FY 2019 | FY 2020 | |||
| MCO Requirement | 5 States | AZ, CO, LA, OH, WA | 3 States | DE, HI, VA |
| FFS Initiative | 8 States | CA, CO, CT, KS, MI, PA, RI, SC | 3 States | DC, DE, VA |
| MCO requirement not reported: GA, MD, MI, NH; FFS initiative not reported: GA, MD | ||||
The following are state examples of MCO pre-release care coordination initiatives:
- Louisiana Department of Corrections staff identify “high-need” beneficiaries for pre-release case management through MCOs, including the provision of at least one “in-reach” appointment prior to release and the scheduling of needed appointments following release.
- Ohio’s Medicaid Pre-Release Enrollment program facilitates direct enrollment of incarcerated individuals into an MCO. Beneficiaries with complex needs are assigned an MCO care manager prior to release who develops a transition plan and helps connect the member to needed community services and supports.
- Washington requires MCOs to provide care coordination for enrollees transitioning into or out of a correctional facility. This includes establishing a data sharing process to support the sharing of health information between the MCO and the correctional facility. As part of the care coordination program, MCOs must also arrange transportation, schedule appointments, and provide housing and employment assistance services.
While not an MCO initiative, Connecticut outstations Medicaid eligibility staff at correctional facilities to support transitions into the community, including enrollment in Medicaid, the provision of medication vouchers, and connecting the individual to the state’s contracted Medicaid medical administrative services organization to facilitate care coordination. Additionally, New York is pursuing a Section 1115 waiver amendment to provide the following covered Medicaid services beginning 30 days prior to release from a correctional facility for Medicaid beneficiaries with certain serious health conditions: care management services, including “in-reach” engagement; needs assessment; discharge care plan; referrals and appointment scheduling; linkages to social services and peer supports; clinical consultation services to support continuity of care; and a medication management program.
Emerging Delivery System and Payment Reforms
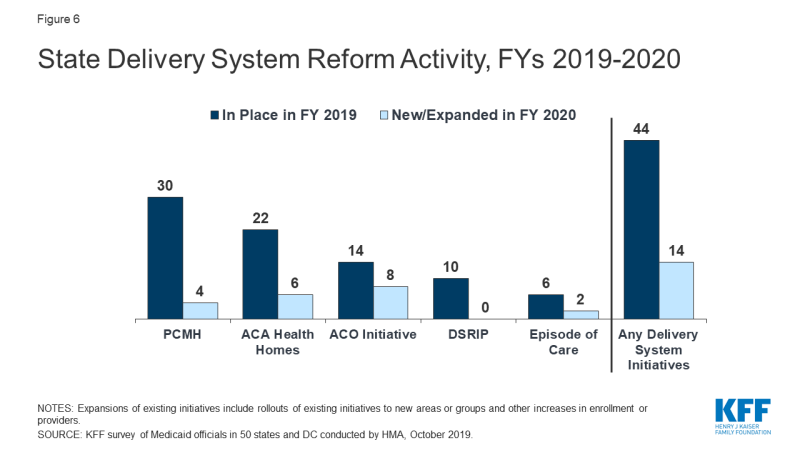
Over three-quarters of all state Medicaid programs (44 states) had at least one of the specified delivery system or payment reform models in place in FY 2019, continuing the upward trend of state-led reforms that aim to address quality and costs (Figure 6 and Table 6). This year’s survey asked states whether certain delivery system and payment reform models (defined in the box below) were in place in FY 2019, and whether they planned to adopt or enhance these models in FY 2020. For FY 2020, 14 states reported plans to adopt or expand one or more of the models to reward quality and encourage integrated care. Key initiatives include patient-centered medical homes (PCMHs), ACA Health Homes, and Accountable Care Organizations (ACOs).
| Delivery System Reform Initiatives Defined |
|
PCMH and Health Home initiatives were the most common delivery system reform initiatives in place in states in FY 2019 (Table 6). PCMH initiatives operated in over half (30 states) of Medicaid programs in FY 2019 and four states reported plans to expand or enhance their existing PCMH programs in FY 2020, often citing increased provider participation. Over one-third of states (22 states) had at least one Health Home initiative in place in FY 2019. Four states reported plans to adopt and two states reported plans to expand Health Homes in FY 2020. Additionally, one state (Ohio) reported plans to request to extend the ACA enhanced match rate for two additional quarters (i.e., for a total of 10 quarters) for SUD Health Homes approved on or after October 1, 2018, as permitted under the SUPPORT Act.
Two states reported eliminations or restrictions to their programs coming in FY 2020. One state (Alabama) reported that both its PCMH and Health Home programs would end in FY 2020 when its new PCCM-entity program is implemented, and New York reported that its PCMH program would be restricted in FY 2020 due to budget caps being applied to PMPM payments.
About a quarter of states had ACO initiatives in place and fewer states have episode of care initiatives in place in FY 2019 (Table 6). Fourteen states reported having an ACO initiative in place for at least some of their Medicaid beneficiaries in FY 2019.35 In some cases, states reported contracting directly with ACOs while other states reported encouraging or requiring their MCOs to contract with ACOs. Two states reported new initiatives and six states reported plans to expand an existing initiative in FY 2020. Six states reported that they had episode-of-care payment initiatives in place in FY 2019, unchanged from 2018 although Pennsylvania will implement a new initiative in 2020 and Ohio will expand its existing initiative in 2020. One state (Arkansas) reported plans to delink its program from reimbursement incentives while retaining as an informational quality benchmark.
| State Delivery System Reform Examples |
|
Ten states reported DSRIP initiatives in place in FY 2019, unchanged from FY 2018 (Table 6) with three states (Kansas, New Jersey, New Mexico) ending their programs in 2020 and one state (Texas) indicating a funding decrease. DSRIP initiatives, which emerged under the Obama administration, have provided states with significant federal funding to support hospitals and other providers in changing how they provide care to Medicaid beneficiaries. No states reported expansions or enhancements to existing initiatives or reported new DSRIP initiatives planned for FY 2020. These initiatives were not intended to be permanent and the Trump administration has not signaled an intent to promote these initiatives going forward.
All-payer claims database (APCD) systems are large-scale databases that systematically collect medical claims, pharmacy claims, dental claims (typically, but not always), and eligibility and provider files from both private and public payers. APCDs can be used to help identify areas to focus reform efforts and for other purposes. Eighteen states reported having an APCD in place. Two states (Connecticut and New York) reported that their APCD would be expanded in FY 2020 and one state (Hawaii) reported plans for a new APCD in FY 2020 (data not shown). California and Delaware also reported that they were in the early stages of development for an APCD in FY 2020.
In addition to the initiatives discussed above, states mentioned a variety of other delivery system and payment reform initiatives. These are not counted in the totals for Figure 6 and Table 6, including value-based purchasing initiatives, pay for performance payments, or other incentive arrangements targeted at hospitals, nursing facilities, federally qualified health centers (FQHCs), or other provider types. Examples of other initiatives reported include the following: in FY 2019, Arizona implemented an APM for FQHCs; in FY 2020, Georgia will expand its school nurse administrative claiming program to include services to students who do not have an Individualized Education Plan (IEP); Maryland reported seeking Section 1115 waiver authority to implement a “Collaborative Care” model pilot that integrates physical and behavioral health services in primary care settings, and Pennsylvania implemented MCO directed payments to Opioid Use Disorder Centers of Excellence (COEs) for care management services in January 2019.
States with significant populations and/or services delivered outside of contracted MCO arrangements also reported on a wide range of non-MCO quality activities. These activities include collection of HEDIS data and other performance measures, conducting beneficiary satisfaction (CAHPS37) surveys, collecting LTSS measures, conducting performance improvement projects, and publicly reporting quality data. One state (Alabama) that is implementing a comprehensive quality strategy for its new PCCM-entity program is highlighted below.
| Alabama Coordinated Health Network Quality Activities |
| In FY 2020, Alabama will contract with one PCCM-entity in each of the state’s seven predefined regions to provide care coordination services for the majority of its Medicaid members. Each PCCM-entity will be held accountable for improving health outcomes based on HEDIS and CMS Quality Measures and will be eligible for a 10% quality bonus based on their performance on those measures. Each PCCM-entity must also implement three Quality Improvement Projects focused on prevention of childhood obesity, reduction in infant mortality, and substance use disorder. |
State strategies to improve maternal health
The rates of maternal mortality (typically defined as death within one year of pregnancy) in the U.S. have been steadily rising over the past several decades, with significantly higher mortality rates among people of color.38 Medicaid plays a pivotal role in providing prenatal and maternity-related services to pregnant women in the U.S. and pays for nearly half of all births.39 Reflecting that the Medicaid program covers a high need, low-income population, women with Medicaid coverage are more likely to have chronic conditions, preterm births, and low-birthweight babies.40
This year’s survey asked states to briefly describe initiatives implemented in FY 2019 or planned for FY 2020 to improve birth outcomes and/or address maternal mortality challenges. About two-thirds of the states reported new or expanded Medicaid initiatives with over a quarter of states focused on pregnant women with SUD. The most frequently mentioned strategies were MCO-related initiatives including Performance Improvement Projects (PIPs), incentives tied to improvement on performance measures related to birth outcomes or maternal health, and state encouraged MCO value-added benefits for pregnant women. More states reported expanding benefits (both statewide and pilot programs) and eligibility for pregnant and postpartum women compared to the 2017 and 2018 survey (see Benefits and Cost-sharing section for more information on benefit changes and Eligibility and Premiums section for more information on eligibility changes).
The following are other examples of strategies states are using to improve maternal health:
- At least 11 states41 reported applying for the Maternal Opioid Misuse (MOM) Model CMMI grant initiative. The MOM model is intended to address fragmentation in the care of pregnant and postpartum Medicaid beneficiaries with opioid use disorder (OUD) through delivery system transformation. CMMI will distribute a maximum of $64.6 million across a maximum of 12 states, whose Medicaid agencies will implement the model with one or more “care-delivery partners” in their communities. Award notices are anticipated in the fall of 2019.
- Seven states (Arizona, Florida, Maine, Missouri, New York, Pennsylvania, and Virginia) reported initiating some type of statewide initiative or task force that aims to collect information and address issues related to maternal health.
- Six states added or expanded one or more statewide or pilot-based benefits that include doula care services (New Jersey, and New York), home visiting programs (Illinois and New Mexico), group prenatal care services (Georgia and New Jersey), and midwife services (Wyoming).42
- Seven states reported eligibility changes for women that include extending postpartum coverage from 60 days to one year (Illinois, South Carolina, and Missouri [only for pregnant women with SUD] ), increasing the income limit for eligibility (North Dakota and West Virginia), and restoring retroactive coverage for pregnant women (Delaware and Oklahoma).
- Four states reported on other value-based purchasing strategies (Colorado, Connecticut, New Jersey, and Texas) that include incentives to providers to increase health outcomes around deliveries and perinatal care.
- Two states reported delivery system reforms to increase the use of risk screening tools by providers (Montana and Texas). Also, Ohio reported plans to submit a SPA to implement SUD “Mom and Baby Dyad” care, linking it to other SUD waiver activities such as intensive care coordination, and developing a residential treatment provider type to provide treatment for mom and baby as needed.
Table 2: Share of the Medicaid Population Covered Under Different Delivery Systems in all 50 States and DC, as of July 1, 2019
| States | Type(s) of Managed Care In Place | Share of Medicaid Population in Different Delivery Systems | ||
| MCO | PCCM | FFS / Other | ||
| Alabama | PCCM | — | 85.0% | 15.0% |
| Alaska | FFS | — | — | 100.0% |
| Arizona | MCO | 94.0% | — | 6.0% |
| Arkansas* | PCCM and MCO | 5.0% | 45.0% | 50.0% |
| California | MCO | 81.1% | — | 18.9% |
| Colorado | MCO and PCCM* | 9.5% | 90.5% | 0.0% |
| Connecticut | FFS* | — | — | 100.0% |
| Delaware | MCO | 97.0% | — | 3.0% |
| DC | MCO | 75.0% | — | 25.0% |
| Florida | MCO | 90.0% | — | 10.0% |
| Georgia | MCO | 75.0% | — | 25.0% |
| Hawaii | MCO | 99.9% | — | 0.1% |
| Idaho* | PCCM | — | 83.9% | 16.1% |
| Illinois | MCO | 81.4% | — | 18.6% |
| Indiana | MCO | 78.0% | — | 22.0% |
| Iowa | MCO | 94.3% | — | 5.8% |
| Kansas | MCO | 99.4% | — | 0.6% |
| Kentucky | MCO | 91.0% | — | 9.0% |
| Louisiana | MCO | 90.1% | — | 9.9% |
| Maine | PCCM | — | 60.0% | 40.0% |
| Maryland | MCO | 85.7% | — | 14.3% |
| Massachusetts | MCO and PCCM | 42.0% | 26.0% | 32.0% |
| Michigan | MCO | 76.5% | — | 23.5% |
| Minnesota | MCO | 82.9% | — | 17.1% |
| Mississippi | MCO | 65.0% | — | 35.0% |
| Missouri | MCO | 73.0% | — | 27.0% |
| Montana | PCCM | — | 87.0% | 13.0% |
| Nebraska | MCO | 99.9% | — | 0.1% |
| Nevada | MCO | 74.0% | — | 26.0% |
| New Hampshire | MCO | 97.7% | — | 2.3% |
| New Jersey | MCO | 95.0% | — | 5.0% |
| New Mexico | MCO | 80.7% | — | 19.3% |
| New York | MCO | 76.6% | — | 23.4% |
| North Carolina | PCCM | — | 90.0% | 10.0% |
| North Dakota | MCO and PCCM | 23.0% | 43.5% | 33.5% |
| Ohio | MCO | 93.7% | — | 6.3% |
| Oklahoma | PCCM | — | 74.5% | 25.5% |
| Oregon | MCO* | 91.0% | — | 9.0% |
| Pennsylvania | MCO | 89.3% | — | 10.7% |
| Rhode Island | MCO | 90.0% | — | 10.0% |
| South Carolina | MCO* | 77.0% | — | 23.0% |
| South Dakota | PCCM | — | 80.0% | 20.0% |
| Tennessee | MCO | 100.0% | — | 0.0% |
| Texas | MCO | 94.0% | — | 6.0% |
| Utah | MCO | 75.3% | — | 24.7% |
| Vermont | FFS | — | — | 100.0% |
| Virginia | MCO | 98.0% | — | 2.0% |
| Washington | MCO and PCCM | 93.0% | 1.0% | 6.0% |
| West Virginia | MCO | 77.0% | — | 23.0% |
| Wisconsin | MCO | 78.3% | — | 21.7% |
| Wyoming | FFS | — | — | 100.0% |
| NOTES: MCO refers to risk-based managed care; PCCM refers to Primary Care Case Management. FFS/Other refers to Medicaid beneficiaries who are not in MCOs or PCCM programs. *AR – Most expansion adults served by Qualified Health Plans through “Arkansas Works” premium assistance waiver. *CO – PCCM enrollees are part of the state’s Accountable Care Collaboratives (ACCs). *CT – Terminated its MCO contracts in 2012 and now operates its program on a fee-for-service basis using three ASO entities. *ID – The Medicaid-Medicare Coordinated Plan (MMCP) has been recategorized by CMS as an MCO but is not counted here as such since it is secondary to Medicare. *OR – MCO enrollees include those enrolled in the state’s Coordinated Care Organizations. *SC – Uses PCCM authority to provide care management services to medically complex children.
SOURCE: Kaiser Family Foundation Survey of Medicaid Officials in 50 states and DC conducted by Health Management Associates, October 2019. |
||||
| States | Non-Dual, Non-LTSS Populations | ||||||
| Pregnant Women | Medically Fragile/Tech Dependent Children | Foster Children | Persons with SMI/SED | Persons with ID/DD | Persons with Physical Disabilities | Seniors | |
| Alabama | — | — | — | — | — | — | — |
| Alaska | — | — | — | — | — | — | — |
| Arizona | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory |
| Arkansas | Varies | Excluded | Varies | Mandatory | Mandatory | Excluded | Varies |
| California | Mandatory | Mandatory | Varies | Mandatory | Mandatory | Mandatory | Mandatory |
| Colorado | Voluntary | Voluntary | Voluntary | Voluntary | Voluntary | Voluntary | Voluntary |
| Connecticut | — | — | — | — | — | — | — |
| Delaware | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory |
| DC | Mandatory | Voluntary | Varies | Varies | Excluded | Varies | Excluded |
| Florida | Mandatory | Mandatory | Mandatory | Mandatory | Voluntary | Mandatory | Mandatory |
| Georgia | Varies | Excluded | Mandatory | Excluded | Excluded | Excluded | Excluded |
| Hawaii | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory |
| Idaho | — | — | — | — | — | — | — |
| Illinois | Mandatory | Excluded | Excluded | Mandatory | Mandatory | Mandatory | Mandatory |
| Indiana | Mandatory | Varies | Voluntary | Varies | Varies | Varies | Mandatory |
| Iowa | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory |
| Kansas | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory |
| Kentucky | Mandatory | Varies | Mandatory | Varies | Varies | Varies | Varies |
| Louisiana | Mandatory | Varies | Mandatory | Varies | Varies | Varies | Varies |
| Maine | — | — | — | — | — | — | — |
| Maryland | Mandatory | Excluded | Mandatory | Varies | Varies | Varies | Excluded |
| Massachusetts | Voluntary | Voluntary | Voluntary | Voluntary | Voluntary | Voluntary | Voluntary |
| Michigan | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Varies | Mandatory |
| Minnesota | Varies | Voluntary | Voluntary | Voluntary | Voluntary | Voluntary | Varies |
| Mississippi | Mandatory | Voluntary | Voluntary | Varies | Excluded | Mandatory | Excluded |
| Missouri | Mandatory | Voluntary | Mandatory | Voluntary | Excluded | Voluntary | Excluded |
| Montana | — | — | — | — | — | — | — |
| Nebraska | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory |
| Nevada | Mandatory | Voluntary | Voluntary | Voluntary | Excluded | Excluded | Excluded |
| New Hampshire | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory |
| New Jersey* | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory |
| New Mexico | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory |
| New York | Mandatory | Mandatory | Varies | Mandatory | Voluntary | Mandatory | Mandatory |
| North Carolina | — | — | — | — | — | — | — |
| North Dakota | Excluded | Excluded | Excluded | Excluded | Excluded | Excluded | Excluded |
| Ohio | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory |
| Oklahoma | — | — | — | — | — | — | — |
| Oregon | Mandatory | Mandatory | Varies | Mandatory | Varies | Mandatory | Mandatory |
| Pennsylvania | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory |
| Rhode Island | Mandatory | Varies | Mandatory | Mandatory | Mandatory | Mandatory | Excluded |
| South Carolina | Mandatory | Varies | Voluntary | Mandatory | Varies | Varies | Voluntary |
| South Dakota | — | — | — | — | — | — | — |
| Tennessee | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory |
| Texas | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory |
| Utah | Mandatory | Varies | Varies | Mandatory | Varies | Varies | Mandatory |
| Vermont | — | — | — | — | — | — | — |
| Virginia | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory | Mandatory |
| Washington | Mandatory | Varies | Voluntary | Mandatory | Varies | Mandatory | Mandatory |
| West Virginia | Mandatory | Mandatory | Excluded | Mandatory | Excluded | Mandatory | Excluded |
| Wisconsin | Mandatory | Varies | Varies | Varies | Voluntary | Mandatory | Varies |
| Wyoming | — | — | — | — | — | — | — |
| Mandatory | 34 | 20 | 22 | 26 | 19 | 24 | 23 |
| Voluntary | 2 | 7 | 8 | 5 | 6 | 4 | 3 |
| Varies | 3 | 8 | 7 | 7 | 8 | 8 | 5 |
| Excluded | 1 | 5 | 3 | 2 | 7 | 4 | 9 |
| NOTES: “–” indicates there were no MCOs operating in that state’s Medicaid program as of July 1, 2019. I/DD – intellectual and developmental disabilities, SMI – Serious Mental Illness, SED – Serious Emotional Disturbance. States were asked to indicate for each group if enrollment in MCOs is “Mandatory,” “Voluntary,” “Varies,” or if the group is “Excluded” from MCOs as of July 1, 2019. *NJ: Nursing facility residents as of July 1, 2014 were grandfathered and remain excluded from MCO enrollment unless they experience a change in eligibility status or are discharged from the nursing facility.
SOURCE: Kaiser Family Foundation Survey of Medicaid Officials in 50 states and DC conducted by Health Management Associates, October 2019. |
|||||||
Table 4: Behavioral Health Services Covered Under Acute Care MCO Contracts in all 50 States and DC, as of July 1, 2019
| States | Specialty OP Mental Health | Inpatient Mental Health | Outpatient SUD | Inpatient SUD |
| Alabama | — | — | — | — |
| Alaska | — | — | — | — |
| Arizona* | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Arkansas | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| California | Always Carved-out | Always Carved-out | Always Carved-out | Always Carved-out |
| Colorado | Always Carved-out | Always Carved-out | Always Carved-out | Always Carved-out |
| Connecticut | — | — | — | — |
| Delaware | Varies | Varies | Varies | Varies |
| DC | Always Carved-out | Always Carved-in | Always Carved-out | Always Carved-in |
| Florida | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Georgia | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Hawaii | Always Carved-out | Always Carved-out | Always Carved-in | Always Carved-in |
| Idaho | — | — | — | — |
| Illinois | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Indiana | Varies | Always Carved-in | Always Carved-in | Always Carved-in |
| Iowa | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Kansas | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Kentucky | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Louisiana | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Maine | — | — | — | — |
| Maryland | Always Carved-out | Always Carved-out | Always Carved-out | Always Carved-out |
| Massachusetts | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Michigan | Always Carved-out | Always Carved-out | Always Carved-out | Always Carved-out |
| Minnesota | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Mississippi | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Missouri | Always Carved-out | Varies | Varies | Varies |
| Montana | — | — | — | — |
| Nebraska | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Nevada | Always Carved-in | Varies | Always Carved-in | Always Carved-in |
| New Hampshire | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| New Jersey | Varies | Always Carved-in | Varies | Always Carved-in |
| New Mexico | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| New York | Varies | Always Carved-in | Always Carved-in | Always Carved-in |
| North Carolina | — | — | — | — |
| North Dakota | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Ohio | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Oklahoma | — | — | — | — |
| Oregon | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Pennsylvania | Always Carved-out | Always Carved-out | Always Carved-out | Always Carved-out |
| Rhode Island | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| South Carolina | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| South Dakota | — | — | — | — |
| Tennessee | Always Carved-in | Always Carved-in | Always Carved-in | Always Carved-in |
| Texas | Varies | Always Carved-in | Always Carved-in | Always Carved-in |
| Utah | Always Carved-out | Always Carved-out | Always Carved-out | Always Carved-out |
| Vermont | — | — | — | — |
| Virginia | Always Carved-out | Varies | Always Carved-in | Varies |
| Washington | Varies | Varies | Varies | Varies |
| West Virginia | Always Carved-in | Always Carved-in | Always Carved-in | Varies |
| Wisconsin | Varies | Always Carved-in | Always Carved-in | Always Carved-in |
| Wyoming | — | — | — | — |
| Always Carved-in | 23 | 28 | 29 | 29 |
| Always Carved-out | 10 | 7 | 7 | 6 |
| Varies | 7 | 5 | 4 | 5 |
| NOTES: OP – Outpatient. SUD – Substance Use Disorder. “–” indicates there were no MCOs operating in that state’s Medicaid program in July 2019. For beneficiaries enrolled in an MCO for acute care benefits, states were asked to indicate whether these benefits are always carved-in (meaning virtually all services are covered by the MCO), always carved-out (to PHP or FFS), or whether the carve-in varies (by geography or other factor). “Specialty outpatient mental health” refers to services utilized by adults with Serious Mental Illness (SMI) and/or youth with serious emotional disturbance (SED) commonly provided by specialty providers such as community mental health centers. *AZ: Foster care children have separate MCOs for Acute and Behavioral Health, all other populations are in an integrated MCO.
SOURCE: Kaiser Family Foundation Survey of Medicaid Officials in 50 states and DC conducted by Health Management Associates, October 2019. |
||||
Table 5: Select Medicaid Managed Care Quality Initiatives in all 50 States and DC, In Place in FY 2019 and Actions Taken in FY 2020
|
States |
Pay for Performance/ |
Capitation Withhold |
Auto-Assignment Algorithm Includes Quality Performance Measures |
Publicly Available Comparison Data About MCOs |
Any Select Quality Initiatives |
|||||
|
|
In |
New or Expanded |
In Place FY 2019 |
New or Expanded |
In |
New or Expanded |
In Place FY 2019 |
New or Expanded |
In |
New or Expanded |
|
Alabama |
— |
— |
— |
— |
— |
— |
— |
— |
— |
— |
|
Alaska |
— |
— |
— |
— |
— |
— |
— |
— |
— |
— |
|
Arizona |
X |
X |
X |
X |
X |
X |
X |
|||
|
Arkansas |
X |
X |
||||||||
|
California |
X* |
X |
X |
X |
X |
X |
X |
|||
|
Colorado |
X |
X |
X |
|||||||
|
Connecticut |
— |
— |
— |
— |
— |
— |
— |
— |
— |
— |
|
Delaware |
X |
X |
X |
X |
X |
X |
||||
|
DC |
X |
X |
||||||||
|
Florida |
X |
X |
X |
X |
X |
X |
||||
|
Georgia |
X |
X |
X |
X |
X |
|||||
|
Hawaii |
X |
X |
X |
X |
X |
X |
X |
|||
|
Idaho |
— |
— |
— |
— |
— |
— |
— |
— |
— |
— |
|
Illinois |
X* |
X |
X |
X |
X |
|||||
|
Indiana |
X |
X |
X |
X |
X |
X |
X |
|||
|
Iowa |
X |
X |
X |
X |
||||||
|
Kansas |
X |
X |
X |
X |
X |
X |
||||
|
Kentucky |
X |
X |
||||||||
|
Louisiana |
X |
X |
X |
X |
X |
X |
||||
|
Maine |
— |
— |
— |
— |
— |
— |
— |
— |
— |
— |
|
Maryland |
X |
X |
X |
X |
||||||
|
Massachusetts |
X |
X |
X |
X |
||||||
|
Michigan |
X |
X |
X |
X |
X |
X |
X |
X |
X |
|
|
Minnesota |
X |
X |
X |
|||||||
|
Mississippi |
X* |
X |
||||||||
|
Missouri |
X |
X |
X |
X |
X |
X |
||||
|
Montana |
— |
— |
— |
— |
— |
— |
— |
— |
— |
— |
|
Nebraska |
X |
X |
X |
X |
X |
|||||
|
Nevada |
X |
X |
X |
X |
||||||
|
New Hampshire |
X* |
X* |
X* |
X |
X |
X |
||||
|
New Jersey |
X |
X |
X |
|||||||
|
New Mexico |
X |
X |
X** |
X |
X |
|||||
|
New York |
X |
X |
X |
|||||||
|
North Carolina |
— |
— |
— |
— |
— |
|||||
|
North Dakota |
||||||||||
|
Ohio |
X |
X |
X |
X |
X |
X |
X |
X |
||
|
Oklahoma |
— |
— |
— |
— |
— |
— |
— |
— |
— |
— |
|
Oregon |
X |
X |
X |
X |
X |
X |
||||
|
Pennsylvania |
X |
X |
X |
X |
X |
X |
||||
|
Rhode Island |
X |
X |
X |
X |
X |
X |
||||
|
South Carolina |
X |
X |
X |
X |
X |
|||||
|
South Dakota |
— |
— |
— |
— |
— |
— |
— |
— |
— |
— |
|
Tennessee |
X |
X |
||||||||
|
Texas |
X |
X |
X |
X |
X |
X |
||||
|
Utah |
X* |
X |
||||||||
|
Vermont |
— |
— |
— |
— |
— |
— |
— |
— |
— |
— |
|
Virginia |
X |
X |
X |
X |
X |
X |
||||
|
Washington |
X |
X |
X |
X |
X |
X |
||||
|
West Virginia |
||||||||||
|
Wisconsin |
X |
X |
X |
X |
||||||
|
Wyoming |
— |
— |
— |
— |
— |
— |
— |
— |
— |
— |
|
Totals |
25 |
10 |
24 |
7 |
11 |
4 |
34 |
12 |
36 |
23 |
|
NOTES: States with MCO contracts were asked to report if select quality initiatives were included in contracts in FY 2019, or are new or expanded in FY 2020. The table above does not reflect all quality initiatives states have included as part of MCO contracts. “*” indicates that a policy was newly adopted in FY 2020, meaning that the state did not have any policy in that category/column in place in FY 2019. “**” New Mexico reported eliminating the use of quality metrics in its auto-assignment algorithm at end of CY 2018. SOURCE: Kaiser Family Foundation Survey of Medicaid Officials in 50 states and DC conducted by Health Management Associates, October 2019. |
||||||||||
Table 6: Select Delivery System and Payment Reform Initiatives in all 50 States and DC, In Place in FY 2019 and Actions Taken in FY 2020
|
States |
Patient-Centered Medical Homes |
ACA Health Homes |
Accountable Care Organizations (ACO) |
Episode of Care Payments |
Delivery System Reform Incentive Payment Program |
Any Delivery System or Payment Reform Initiatives |
||||||
|
In Place FY 2019 |
New/ Expand FY 2020 |
In Place FY 2019 |
New/ Expand FY 2020 |
In Place FY 2019 |
New/ Expand FY 2020 |
In Place FY 2019 |
New/ Expand FY 2020 |
In |
New/ Expand FY 2020 |
In |
New/ Expand FY 2020 |
|
|
Alabama |
X |
X |
X |
|||||||||
|
Alaska |
X |
X* |
X |
X |
||||||||
|
Arizona |
X |
X |
||||||||||
|
Arkansas |
X |
X |
X |
|||||||||
|
California |
X |
X |
X |
X |
X |
|||||||
|
Colorado |
X |
X |
X |
|||||||||
|
Connecticut |
X |
X |
X |
X |
X |
X |
X |
|||||
|
Delaware |
X |
X |
||||||||||
|
DC |
X |
X |
||||||||||
|
Florida |
X |
X |
||||||||||
|
Georgia |
X |
X |
||||||||||
|
Hawaii |
X* |
X |
||||||||||
|
Idaho |
X |
X* |
X |
X |
||||||||
|
Illinois |
X |
X* |
X |
X |
||||||||
|
Indiana |
||||||||||||
|
Iowa |
X |
X |
X |
|||||||||
|
Kansas |
X* |
X |
X |
X |
||||||||
|
Kentucky |
||||||||||||
|
Louisiana |
X |
X |
X |
X |
X |
|||||||
|
Maine |
X |
X |
X |
X |
X |
|||||||
|
Maryland |
X |
X |
||||||||||
|
Massachusetts |
X |
X |
X |
|||||||||
|
Michigan |
X |
X |
X |
|||||||||
|
Minnesota |
X |
X |
X |
X |
||||||||
|
Mississippi |
||||||||||||
|
Missouri |
X |
X |
X |
X |
||||||||
|
Montana |
X |
X |
||||||||||
|
Nebraska |
X |
X |
X |
|||||||||
|
Nevada |
||||||||||||
|
New Hampshire |
X |
X |
||||||||||
|
New Jersey |
X |
X |
X |
X |
X |
|||||||
|
New Mexico |
X |
X |
X |
X |
X |
|||||||
|
New York |
X |
X |
X |
X |
X |
X |
X |
X |
X |
|||
|
North Carolina |
X |
X |
||||||||||
|
North Dakota |
||||||||||||
|
Ohio |
X |
X |
X* |
X |
X |
X |
X |
|||||
|
Oklahoma |
X |
X |
X |
|||||||||
|
Oregon |
X |
X |
||||||||||
|
Pennsylvania |
X |
X |
X |
X |
X* |
X |
X |
|||||
|
Rhode Island |
X |
X |
X |
X |
||||||||
|
South Carolina |
X |
X |
||||||||||
|
South Dakota |
X |
X |
||||||||||
|
Tennessee |
X |
X |
X |
X |
||||||||
|
Texas |
X |
X |
X |
|||||||||
|
Utah |
||||||||||||
|
Vermont |
X |
X |
X |
X |
X |
X |
X |
|||||
|
Virginia |
X |
X |
||||||||||
|
Washington |
X |
X |
X |
|||||||||
|
West Virginia |
X |
X |
||||||||||
|
Wisconsin |
X |
X |
||||||||||
|
Wyoming |
X |
X |
X |
X |
||||||||
|
Totals |
30 |
4 |
22 |
6 |
14 |
8 |
6 |
2 |
10 |
0 |
44 |
14 |
|
NOTES: Expansions of existing initiatives include rollouts of existing initiatives to new areas or groups and significant increases in enrollment or providers. “*” indicates that a policy was newly adopted in FY 2020, meaning that the state did not have any policy in that category/column in place in FY 2019. SOURCE: Kaiser Family Foundation Survey of Medicaid Officials in 50 states and DC conducted by Health Management Associates, October 2019. |
||||||||||||