Views and Experiences with End-of-Life Medical Care in Japan, Italy, the United States, and Brazil: A Cross-Country Survey
Liz Hamel, Bryan Wu, and Mollyann Brodie
Published:
Overview
In partnership with The Economist, the Kaiser Family Foundation conducted a cross-country survey of adults in Japan, Italy, the United States, and Brazil about people’s views and experiences related to aging and end-of-life medical care. These four countries are each at a different stage of population aging. On one end of the spectrum, Japan is the world’s oldest country (27 percent are ages 65 and older) and has the longest life expectancy along with a shrinking overall population . Italy is not far behind, with a population that is 21 percent elderly, the largest proportion among European nations . The United States is in the middle of the aging trajectory, with the share of the population ages 65 and older expected to grow from about 15 percent in 2015 to 24 percent by 2060 . At the other end of the spectrum, Brazil has a relatively young population today, but due to recent changes in mortality and fertility, the share of the population that is elderly is expected to double (from 7 percent to 14 percent) by 2031. These four countries also reflect different cultural and institutional considerations when it comes to preparing and providing care for those near the end of life, and both the demographic and cultural differences are reflected in the survey results reported here.
This report summarizes the overall survey results with comparisons across the four countries, and includes sections highlighting particular findings in Japan, Italy, and Brazil. A separate report with more detail on the U.S. results is available here.
Coverage from The Economist
What people want in their final months
What people want at the end of life
Summary
Four-Country Comparison: Five Key Takeaways
- Despite the demographic and cultural differences between these four countries, there are some common themes that emerge from the survey results. For example, in each country surveyed a majority say their government is not well-prepared to deal with the aging population, and residents are more apt to give their health care system a negative rating than a positive one when it comes to providing end-of-life care. In another area of commonality, majorities in all four countries express a preference to die at home, but fewer say they expect to die at home than say that is their wish. Large majorities across countries also feel that doctors should be completely honest with seriously ill patients, regardless of their prognosis.
- When asked about priorities for health care at the end of people’s lives, majorities across three of the four countries (Japan, Italy, and the U.S.) prioritize reducing pain and stress over extending life as long as possible. Similarly, when asked what is important in thinking about their own death, “living as long as possible” ranks last on a list of seven possible factors in these three countries. Brazil stands out as an exception on these measures, with a larger share placing a priority on extending life, both in general and for themselves personally.
- When it comes to discussing and planning for the end of life, majorities across countries say death is a subject that is generally avoided rather than something people feel free to talk about. However, the U.S. stands out from other countries, with higher shares reporting having conversations with loved ones about their end-of-life wishes and having these wishes written down.
- About one in five adults in each country surveyed say they were involved in helping to make medical decisions for a loved one who died in the past five years. Acting as a medical decision-maker for someone who died appears to influence people’s own personal end-of-life preparations; in Japan, the U.S., and Brazil, those who served as a medical decision-maker for someone else are more likely to say they’ve had a serious conversation with a loved one about their own end-of-life wishes, and to have those wishes in a written document.
- While most of those who experienced the death of a loved one report positive experiences overall, some negative reports are not uncommon. Majorities across countries say their loved one’s wishes about medical care were followed, that their spiritual and religious beliefs were respected, and that they died with friends or family present. Still, substantial shares of those who experienced the death of a loved one (particularly in Japan and Brazil) say the person experienced more pain than was necessary (about four in ten in Brazil, about three in ten in Japan, and a quarter in the U.S. and Italy) or that they did not have access to appropriate medical treatments for prolonging life (about four in ten in Japan and Brazil, one-third in Italy, and 18 percent in the U.S.). About one in five of those experiencing the death of a loved one across countries say their loved one received medical care that placed an undue burden on the patient’s family.
Key Findings Across Countries
Perceptions of the Aging Population and Preparedness of Government, Health System, and Families
Across the four countries surveyed, the share of the public perceiving population aging as a major problem corresponds roughly to each country’s place on the aging trajectory. Nine in ten adults in Japan and about six in ten in Italy (the two “older” countries in the survey) see the growing number of older people in their country as a major problem, compared with about four in ten in the “younger” countries of the U.S. and Brazil.
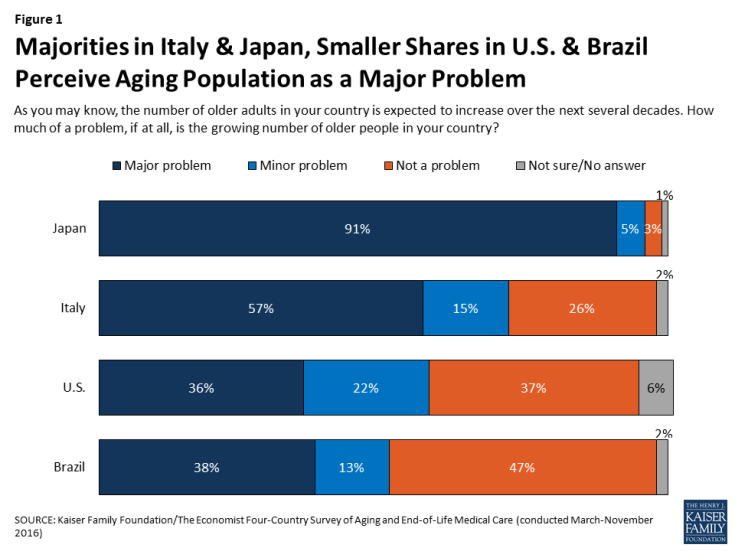
Figure 1: Majorities in Italy & Japan, Smaller Shares in U.S. & Brazil Perceive Aging Population as a Major Problem
Across all four countries surveyed, majorities say the government is “not too prepared” or “not at all prepared” to deal with the aging population. Preparedness ratings are somewhat more mixed when it comes to the country’s health care system and families. In Italy and Brazil, majorities see the health care system as unprepared, while residents of the U.S. and Japan are more evenly divided between thinking the health care system is prepared and not prepared. Asked how prepared families are to deal with the aging population, majorities in Italy, Japan, and Brazil say families are not prepared, while Americans are more evenly split.

Figure 2: Across Countries, Many See Government, Health System, and Families as Unprepared to Deal with Aging Population
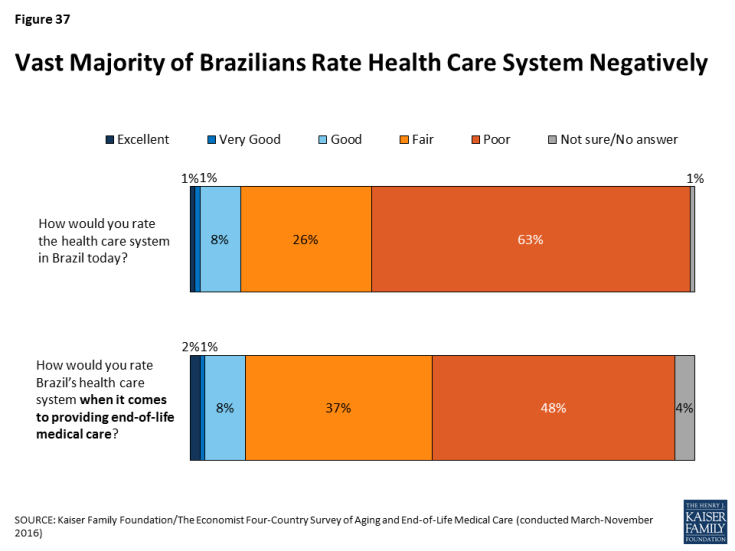
Another similarity across countries is in residents’ relatively negative ratings of their health care systems. In each country, the public is more likely to rate their health care system as “fair” or “poor” than to say it is “excellent” or “very good.” This is true when residents are asked to rate the health care system in general and also when they are asked about end-of-life medical care specifically. Residents of Brazil – a country whose state-run health care system has been plagued by problems – are particularly negative on these measures, with about nine in ten giving a “fair” or “poor” rating.
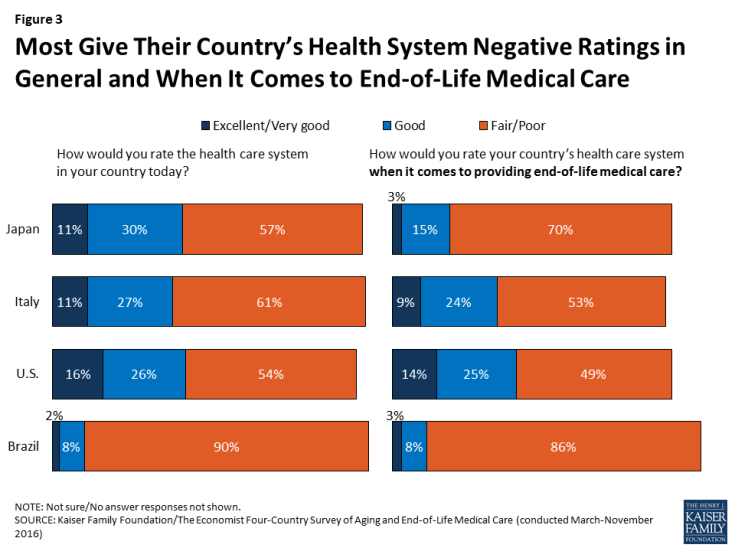
Figure 3: Most Give Their Country’s Health System Negative Ratings in General and When It Comes to End-of-Life Medical Care
Residents of the four countries differ somewhat in their views of who should bear the greatest responsibility for financing care for an aging population. In Italy and Brazil, large majorities of around eight in ten say it’s the government’s responsibility to pay for people’s health and long-term care needs as they age, as do just over half in Japan. Views in the U.S. are more evenly split between those who say the responsibility should fall mostly on individuals and families (44 percent) and those who say it’s the responsibility of the government (42 percent). These views are largely divided by party identification, as views of government responsibility generally are in the U.S., with Democrats more likely to place the responsibility on government and Republicans more likely to place it on families.
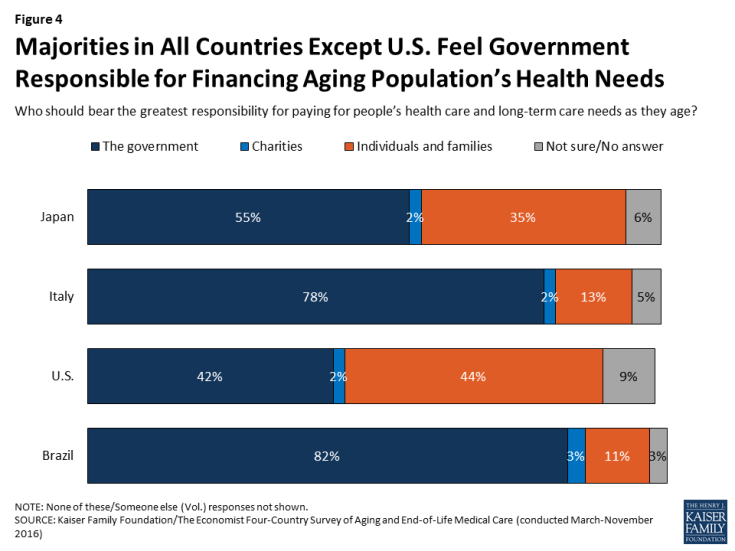
Figure 4: Majorities in All Countries Except U.S. Feel Government Responsible for Financing Aging Population’s Health Needs
Outside of financial responsibility, most people across countries see a large role for families in helping aging family members. Solid majorities say that it is the duty of children to help take care of their parents’ needs as they get older, ranging from 61 percent in Japan to 91 percent in Brazil. With the exception of Italy, in each country older adults themselves are less likely than their younger counterparts to say it is the children’s duty.
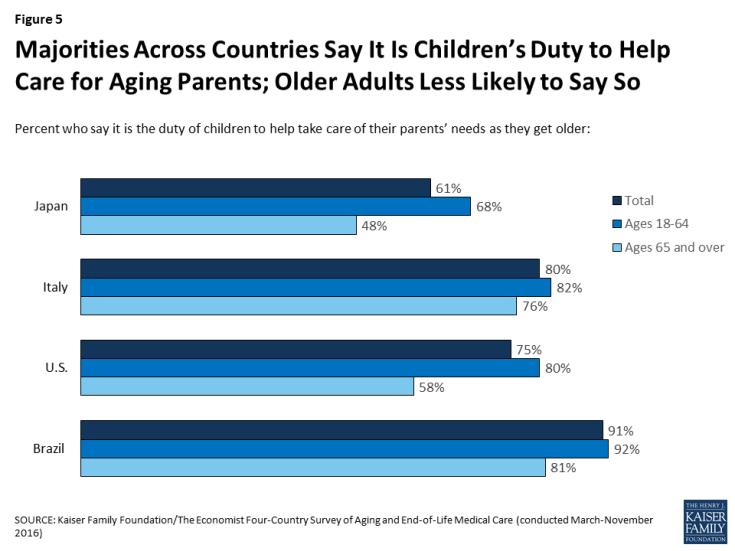
Figure 5: Majorities Across Countries Say It Is Children’s Duty to Help Care for Aging Parents; Older Adults Less Likely to Say So
Priorities at the End of Life
The survey reveals a difference between residents of Brazil and those of the other three countries surveyed when it comes to the relative priority placed on extending life. When asked what should be more important when it comes to health care at the end of people’s lives, half of Brazilians (50 percent) choose “preventing death and extending life as long as possible” while about four in ten (42 percent) choose “helping people die without pain, discomfort, and stress.” This stands in contrast to Japan, Italy, and the U.S., where large majorities – between 68 percent and 82 percent – prioritize reducing pain and stress over extending life.
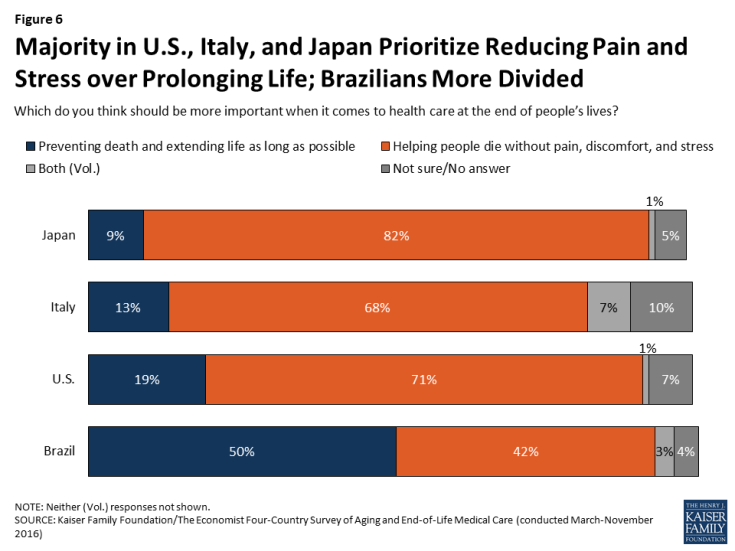
Figure 6: Majority in U.S., Italy, and Japan Prioritize Reducing Pain and Stress over Prolonging Life; Brazilians More Divided
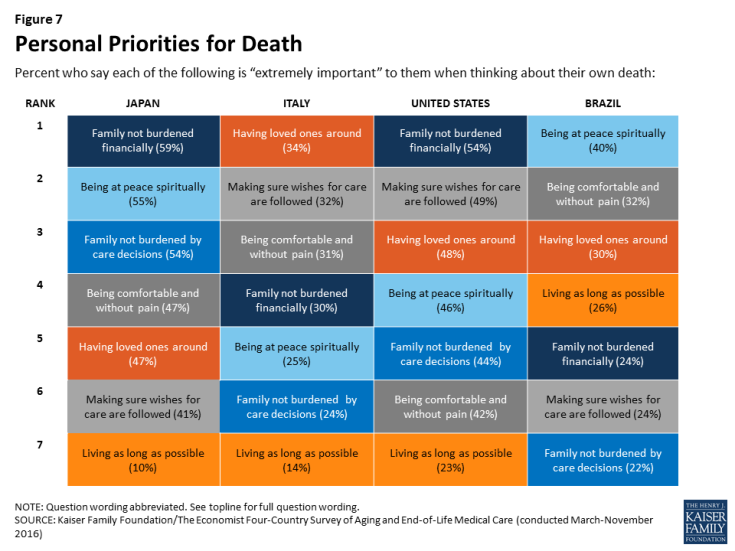
Similarly, when asked what is important in thinking about their own death, Brazilians stand out in the relative importance placed on extending life. In Japan, Italy, and the U.S., “living as long as possible” ranks last on the list of seven possible factors, with a substantially lower share saying it is “extremely important” to them compared with any other factor. By contrast, “living as long as possible” ranks fourth in Brazil, with 26 percent saying it is “extremely important,” similar to the shares who say the same about other priorities like having loved ones around and not burdening one’s family financially. These differences between Brazil and the other countries surveyed may have something to do with Brazil’s relatively younger population; across countries, younger adults are generally more likely than older adults to place greater emphasis on extending life.
In terms of what is most important to people in thinking about their own death, in the U.S. and Japan, where medical care is generally expensive, “making sure your family is not burdened financially by your care” ranks at the top of the list.1 In Italy, the top concern is “having loved ones around you,” followed closely by “making sure your wishes about medical care are followed” and “being comfortable and without pain.” In Brazil, the top concern is “being at peace spiritually.”
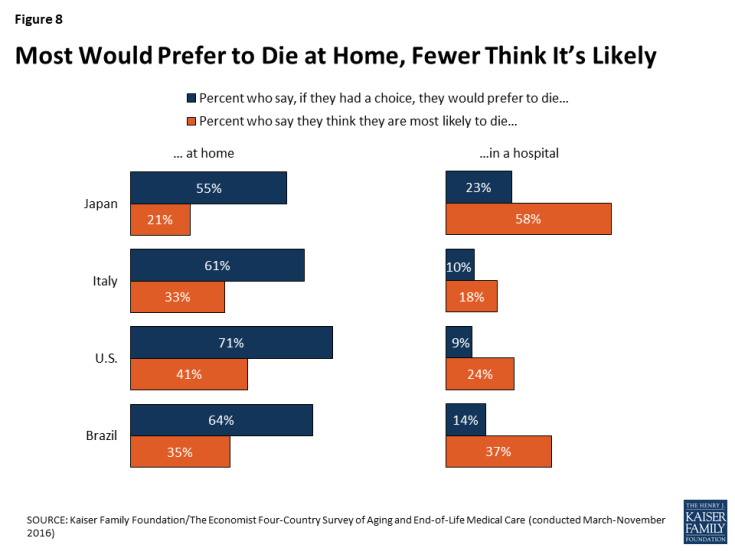
In considering their own death, individuals across countries share the desire to die at home, along with the expectation that this desire is not likely to be fulfilled. Across the four countries surveyed, majorities say if they had the choice, they would prefer to die at home. However, when asked where they think they are most likely to die, a much smaller share in each country say they expect to die at home. This pattern is starkest in Japan – a country with 13.4 hospital beds per 1,000 residents (roughly 4 times as many as any other country surveyed) – where 55 percent say they would prefer to die at home, but 58 percent think they are most likely to die in a hospital.2
Who Should Have Control of Medical Decisions at the End of Life?
There is some variation across the countries surveyed in views of whether doctors or patients and their families should have the greater say in decisions about end-of-life medical treatments. The vast majority of adults in Japan (88 percent) and the U.S. (87 percent) say that patients and their families should have the greater say, while closer to half in Italy (52 percent) and Brazil (47 percent) say the same. By contrast, substantial shares of Brazilians (40 percent) and Italians (30 percent) say that doctors should have the greater say in which medical treatments to pursue for seriously ill patients who are near the end of their lives, compared with about one in ten in Japan and the U.S.
Interestingly, however, the two countries surveyed (Brazil and Italy) where residents are least likely to say patients and their families should have the greater say in end-of-life medical decisions are also the most likely to say people in their own country have too little control over decisions about their own medical care at the end of life (79 percent and 59 percent, respectively). About half (49 percent) of U.S. adults also feel that people have too little control over these decisions. In Japan, about half (49 percent) feel that people in their country have about the right amount of control, while a smaller share (36 percent) say they have too little.
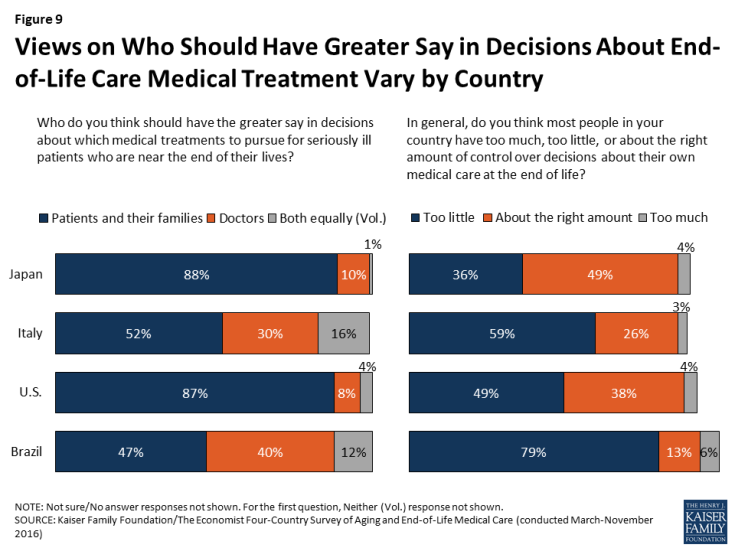
Figure 9: Views on Who Should Have Greater Say in Decisions About End-of-Life Care Medical Treatment Vary by Country
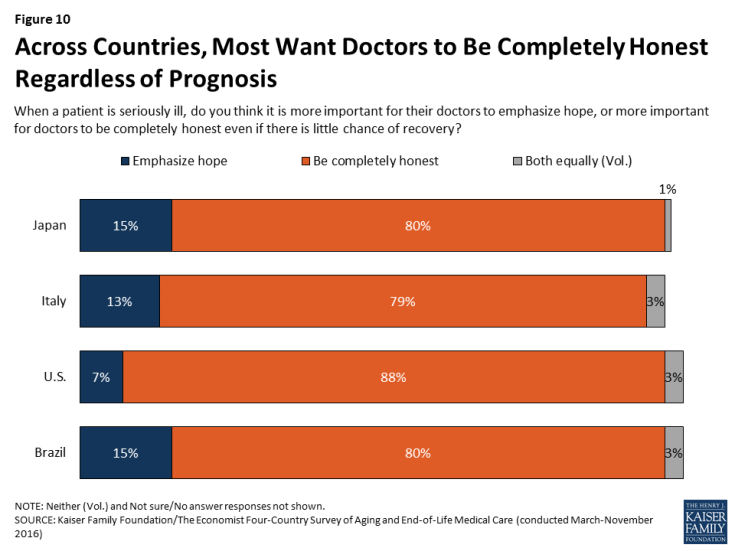
Despite these differences, most people across the countries surveyed agree that doctors should be honest with patients regardless of their prognosis. Large majorities say that when a patient is seriously ill, it is more important for doctors to be completely honest even if there is little chance of recovery, while a small share across countries believe it is more important for doctors to emphasize hope for seriously ill patients.
Talking about Death and Planning Ahead
Across countries, majorities say death is a subject that is generally avoided rather than something people feel free to talk about. However, the U.S. stands out from other countries, with higher shares reporting having conversations with loved ones about end-of-life wishes and having these wishes written down.
When it comes to the subject of death, majorities ranging from 57 percent in Japan to 69 percent in the U.S. say that death is a subject that is generally avoided in their country’s society, while much smaller shares (ranging from 26 percent in the U.S. to 38 percent in Japan) say death is a subject people generally feel free to talk about.
This reluctance to talk about death is reflected in people’s self-reported conversations. Fewer than half of adults (including those ages 65 and over) in Italy, Japan, and Brazil say they’ve had a serious conversation with a loved one about their own wishes for end-of-life medical care. These conversations are somewhat more common in the U.S., with just over half the general population and about three-quarters of Americans ages 65 and over saying they’ve had such a conversation. Having one’s end-of-life medical wishes in a written document is also more common in the U.S.; a quarter of U.S. adults (27 percent) and half of U.S. seniors (51 percent) say they do, compared with fewer than 1 in 6 in other countries.
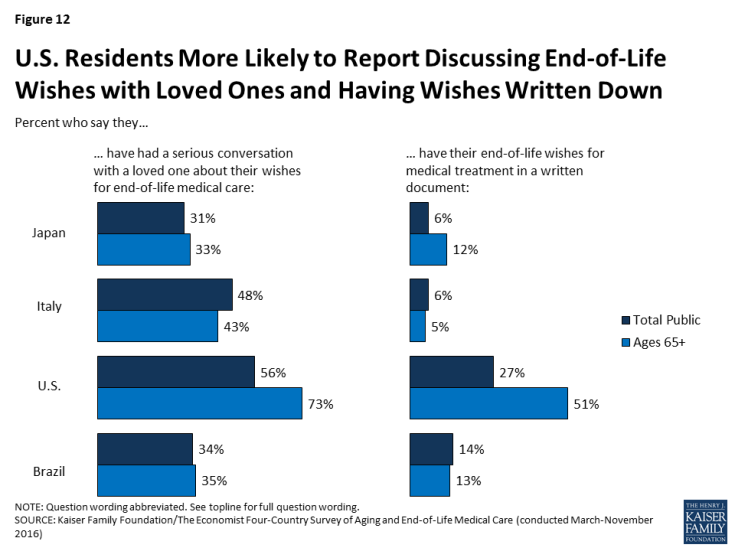
Figure 12: U.S. Residents More Likely to Report Discussing End-of-Life Wishes with Loved Ones and Having Wishes Written Down
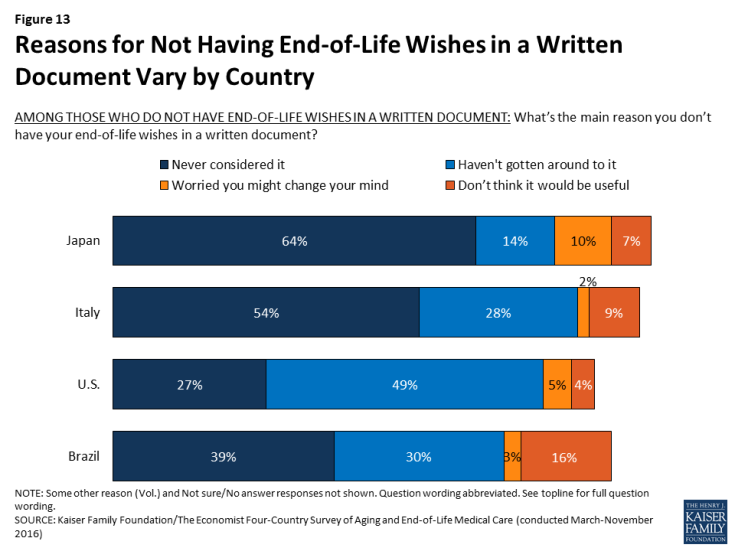
Among those who do not have their wishes written down, the top reason in Italy, Japan, and Brazil is “you never considered it,” suggesting that writing down one’s wishes is not a commonly discussed practice in these countries. By contrast, the top reason in the U.S. is “you just haven’t gotten around to it,” suggesting that Americans are more likely than residents of the other countries surveyed to think of writing down their medical wishes as a common practice and something they expect to do at some point in their lives.
If conversations with loved ones about end-of-life wishes are relatively uncommon, conversations with health care professionals about these issues are even rarer. Just about one in ten in each country say they’ve had a conversation about their wishes for end-of-life medical treatment with a doctor or other health care provider, rising to 22 percent among seniors in the United States. A somewhat larger share – roughly three in ten – in the U.S. and Japan say they’ve participated in a discussion with a health care provider about another family member’s wishes for their care at the end of life, but still the majority say they have not participated in such a conversation.
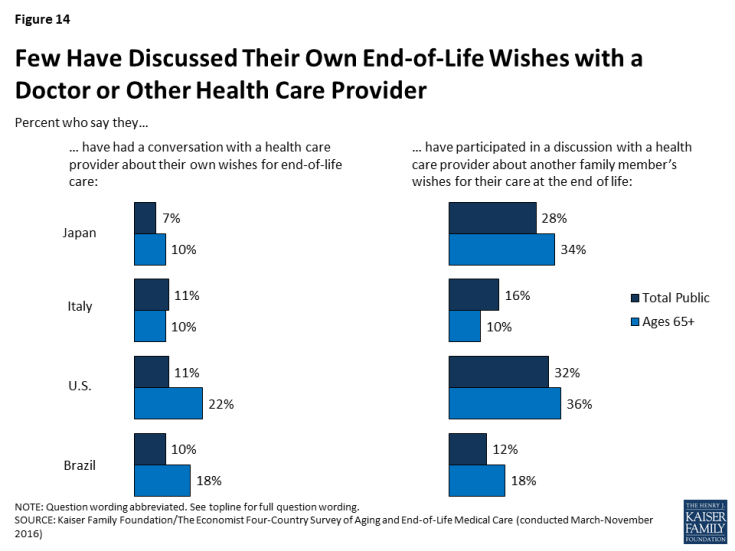
Figure 14: Few Have Discussed Their Own End-of-Life Wishes with a Doctor or Other Health Care Provider
Experiences with Death of a Loved One
At least half of people in each of the four countries surveyed report experiencing the death of someone close to them within the past five years, including substantial minorities who say they helped provide care or helped make medical decisions for the person who died. Overall, about one-fifth in Japan, one-quarter in the U.S. and Italy, and one-third in Brazil say they helped to provide care for a loved one who died in the past five years. About one in five in each country say they were involved in helping to make medical decisions for someone who died in that time frame.
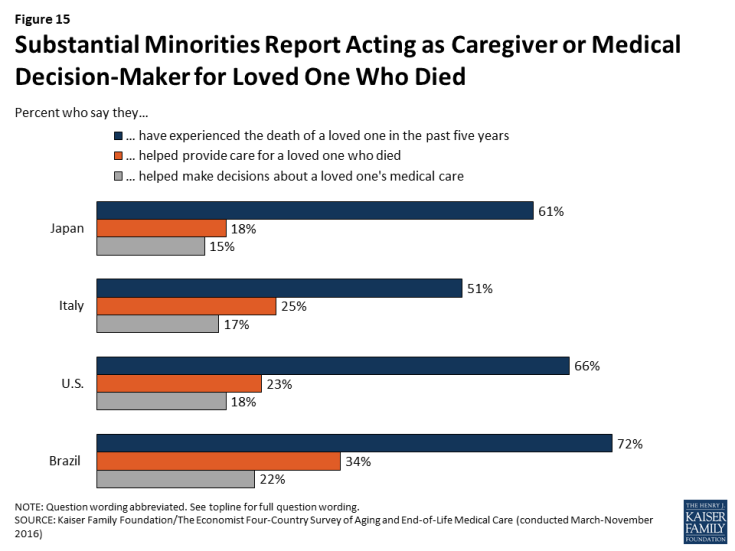
Figure 15: Substantial Minorities Report Acting as Caregiver or Medical Decision-Maker for Loved One Who Died
Among those who say they acted as a medical decision-maker for a loved one who died, residents of the U.S. are more likely than residents of the other countries surveyed to say they had a good idea of their loved one’s end-of-life wishes. A majority of Americans who served as a medical decision-maker for someone who died say they knew exactly what the person wanted (57 percent) or had a pretty good idea (32 percent), while just one in ten say they didn’t really know what their loved one wanted. By contrast, between a third and four in ten in Japan, Italy, and Brazil say they didn’t really know what their loved one’s wishes were before they died. This difference may be related to the finding noted above that Americans are more likely to report having conversations with loved ones about end-of-life wishes.
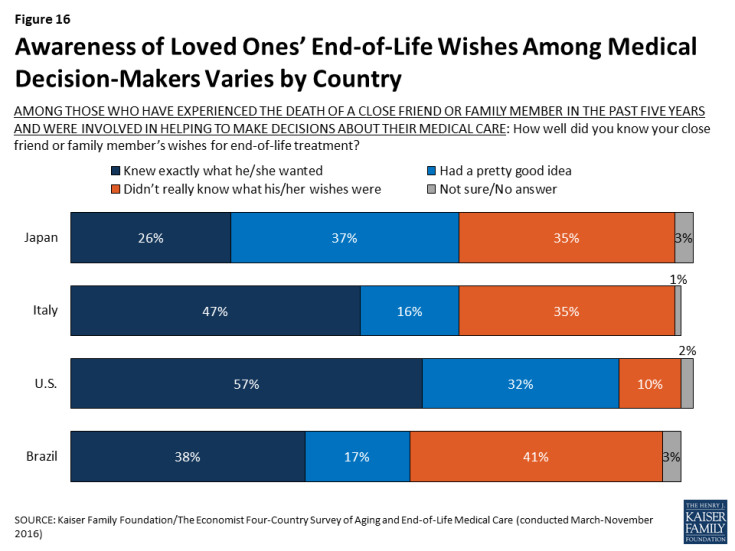
Figure 16: Awareness of Loved Ones’ End-of-Life Wishes Among Medical Decision-Makers Varies by Country
Acting as a medical decision-maker for someone who died also appears to influence people’s own personal end-of-life preparations; in Japan, the U.S., and Brazil, those who served as a medical decision-maker for someone else are significantly more likely to say they’ve had a serious conversation with a loved one about their own end-of-life wishes, and to have those wishes in a written document.
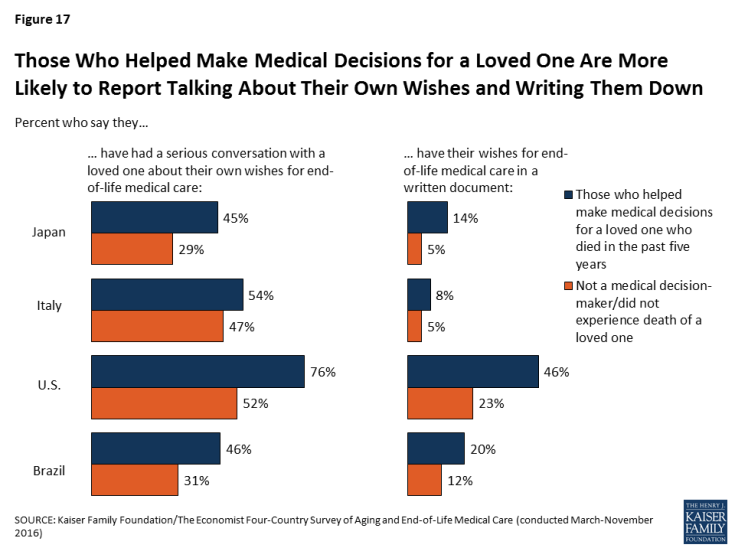
Figure 17: Those Who Helped Make Medical Decisions for a Loved One Are More Likely to Report Talking About Their Own Wishes and Writing Them Down
While most of those who experienced the death of a loved one report positive experiences overall, some negative reports are not uncommon. Among those who experienced the death of someone close to them in the past five years, majorities across countries say their loved one’s wishes about medical care were followed, that their spiritual and religious beliefs were respected, and that they died with friends or family present.
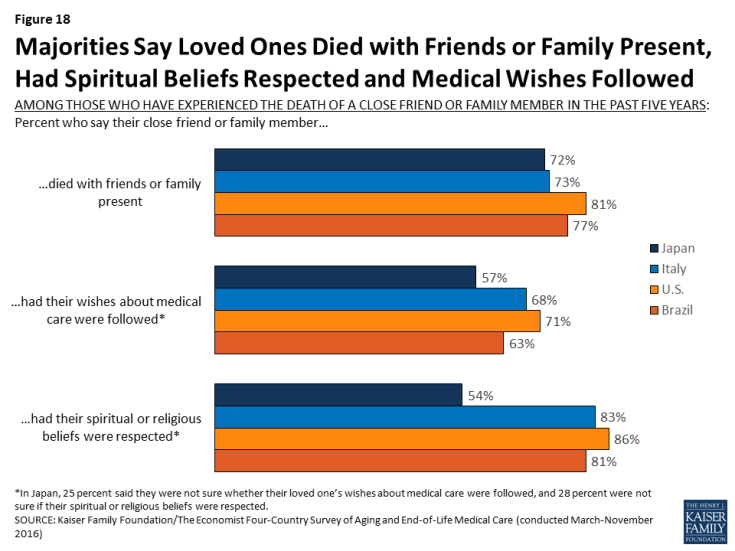
Figure 18: Majorities Say Loved Ones Died with Friends or Family Present, Had Spiritual Beliefs Respected and Medical Wishes Followed
Still, substantial shares of those who experienced the death of a loved one – particularly in Japan and Brazil – say the person experienced more pain than was necessary (about four in ten in Brazil, three in ten in Japan, and a quarter in the U.S. and Italy) or that they did not have access to appropriate medical treatments for prolonging life (about four in ten in Japan and Brazil, one-third in Italy, and 18 percent in the U.S.). About one in five of those experiencing the death of a loved one across countries say their loved one received medical care that placed an undue burden on the patient’s family.
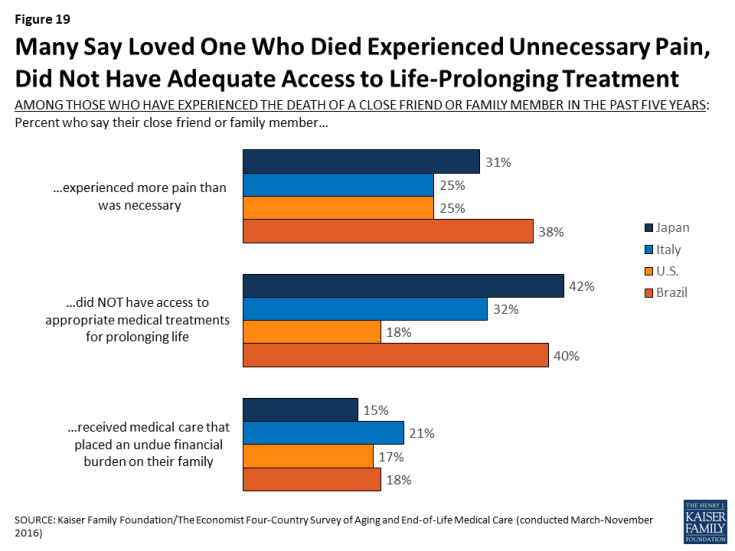
Figure 19: Many Say Loved One Who Died Experienced Unnecessary Pain, Did Not Have Adequate Access to Life-Prolonging Treatment
Awareness and Opinions of Hospice Care
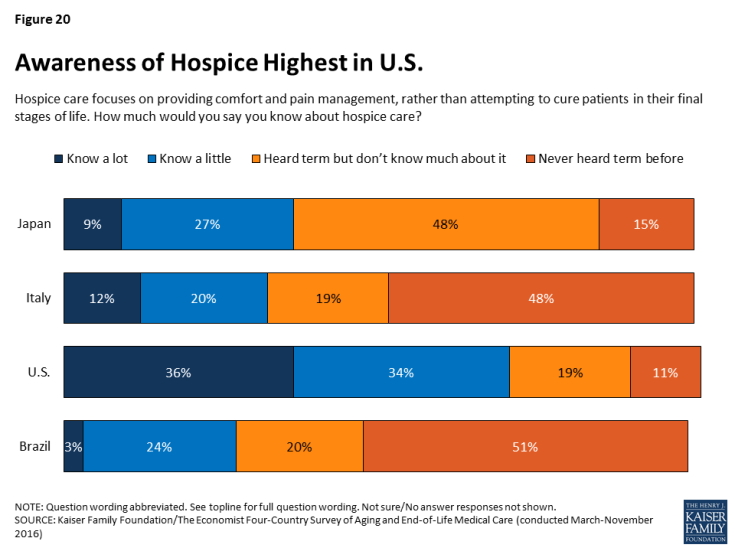
Hospice care is an option for seriously ill patients near the end of life that emphasizes providing comfort and pain management rather than curative treatment. In the U.S., the use of hospice care has increased in recent years, and hospice services are provided in various settings, including hospitals, free-standing hospice centers, and often in the patient’s own home.3 In the other countries surveyed, hospice care is less common and is usually provided in a designated hospice facility. Reflecting these differences, adults in the U.S. are much more likely than those in Japan, Italy, or Brazil to say they know something about hospice. Seven in ten Americans say they know at least a little about hospice care, compared with between about a quarter and a third in the other countries surveyed.
Among those who have heard of it, feelings about hospice care across countries are overwhelmingly positive, with large majorities (between seven and eight in ten) saying they have a positive opinion of hospice.
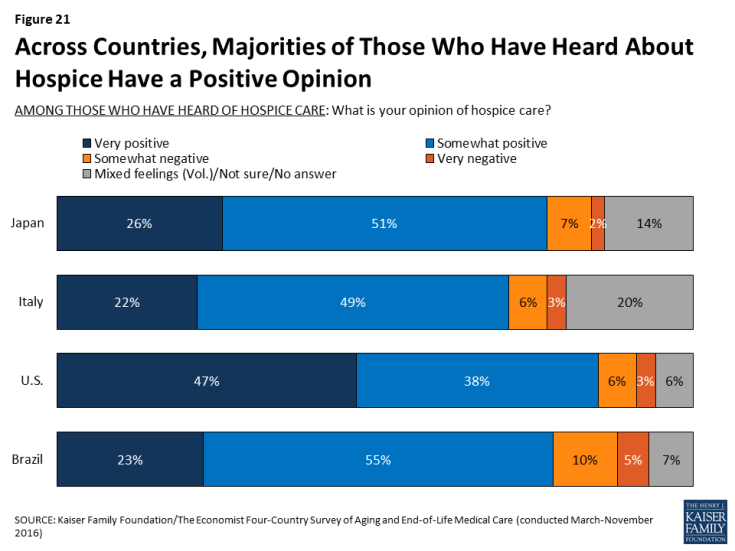
Figure 21: Across Countries, Majorities of Those Who Have Heard About Hospice Have a Positive Opinion
While relatively few of those who experienced the death of a loved one in Japan, Italy, and Brazil say that their loved one died in a hospice facility, roughly half (53 percent) of U.S. adults who experienced a death say their loved one either died in a hospice facility or was receiving hospice services before they died. In the U.S., those whose close friend or family member received hospice services are more likely than those who didn’t receive such services to say their loved one’s spiritual or religious beliefs were respected, that they died with friends or family present, and that their wishes about medical care were followed. Although the aim of hospice is to relieve pain and suffering and not necessarily to extend life, those whose loved ones received hospice services are also more likely than those who didn’t to say the person had access to appropriate treatments for prolonging life. However, there is no significant difference based on receipt of hospice services in the share who say their loved one experienced more pain than necessary or received care that placed an undue financial burden on the family.
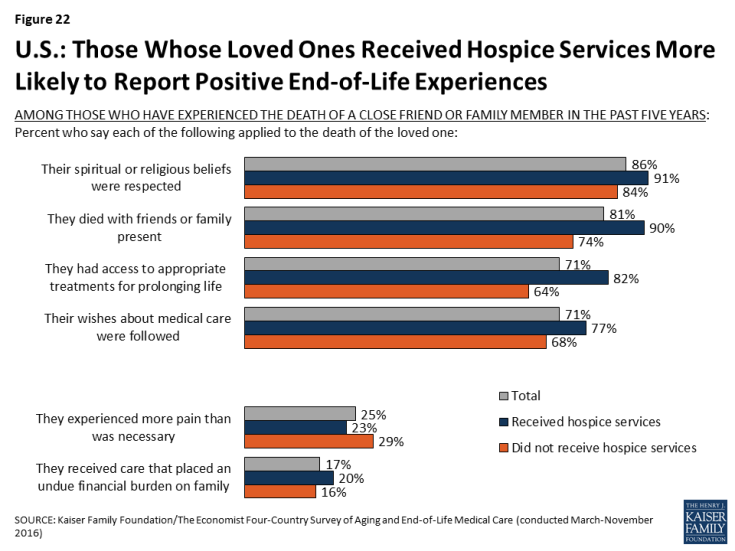
Figure 22: U.S.: Those Whose Loved Ones Received Hospice Services More Likely to Report Positive End-of-Life Experiences
Country Highlights: Japan
As the country in the survey with the oldest population, residents of Japan see the growing number of older adults as a major problem, and rate their health care system poorly on providing end-of-life care.
Nine in ten adults (91 percent) in Japan say the growing number of older people is a major problem for their country, far higher than any of the other countries surveyed. While just over half say it is the government’s responsibility to finance care for this aging population, one-third (35 percent) say the responsibility should fall on individuals and families. Japanese adults are also particularly sour on their health system when it comes to providing end-of-life medical care: seven in ten give it a rating of fair or poor on a 5-point scale.
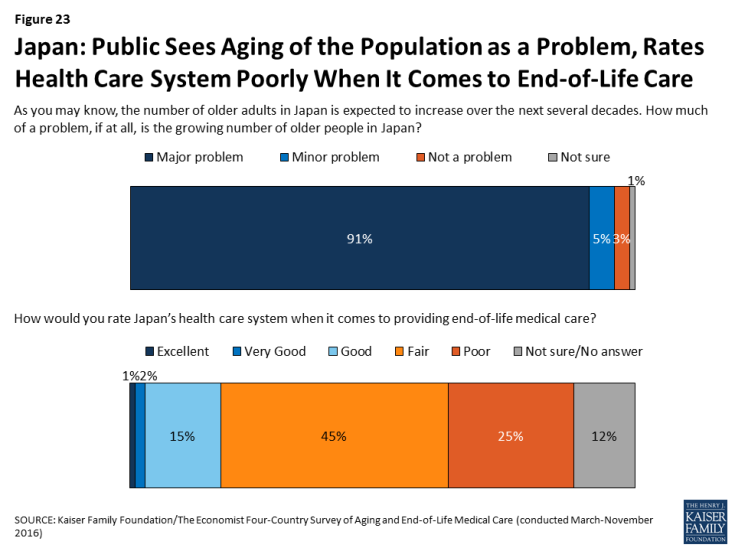
Figure 23: Japan: Public Sees Aging of the Population as a Problem, Rates Health Care System Poorly When It Comes to End-of-Life Care
In Japan, a country with 13.4 hospital beds per 1,000 residents (roughly 4 times as many as any other country surveyed), residents are more likely than those in other countries surveyed to expect to die in a hospital and to say a loved one died in a hospital.
While just over half (55 percent) of Japanese adults say they would prefer to die at home, the majority (58 percent) think they are most likely to die in a hospital, higher than any of the other countries surveyed. Among residents with a loved one who died in the past five years, 69 percent in Japan say their loved one died in a hospital, while just 15 percent say they died at home.
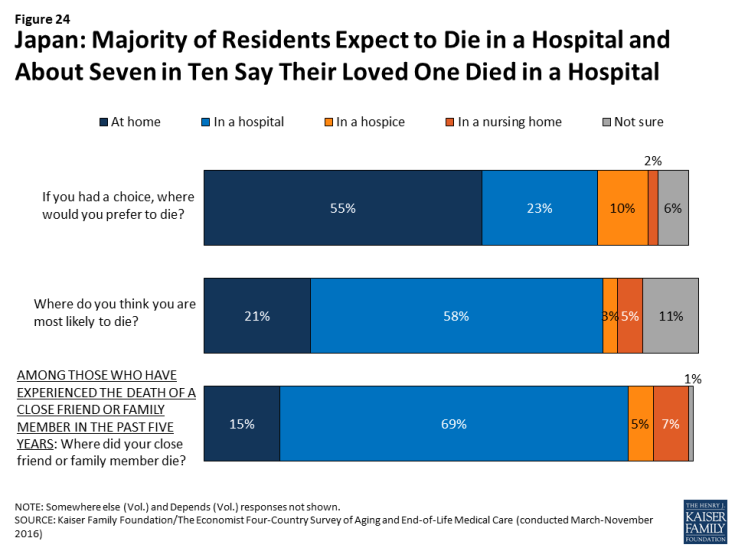
Figure 24: Japan: Majority of Residents Expect to Die in a Hospital and About Seven in Ten Say Their Loved One Died in a Hospital
The top concern for Japanese adults in thinking about their own death is making sure their family is not financially burdened.
Six in ten (59 percent) adults in Japan say that making sure their family is not burdened financially by their care is “extremely important” in thinking about their own death. About half also place this level of importance on being at peace spiritually, not burdening their family with tough decisions about their medical care, having loved ones around, and being comfortable and without pain. By contrast, just 10 percent of Japanese adults say that living as long as possible is extremely important to them, ranking far below any other concern.
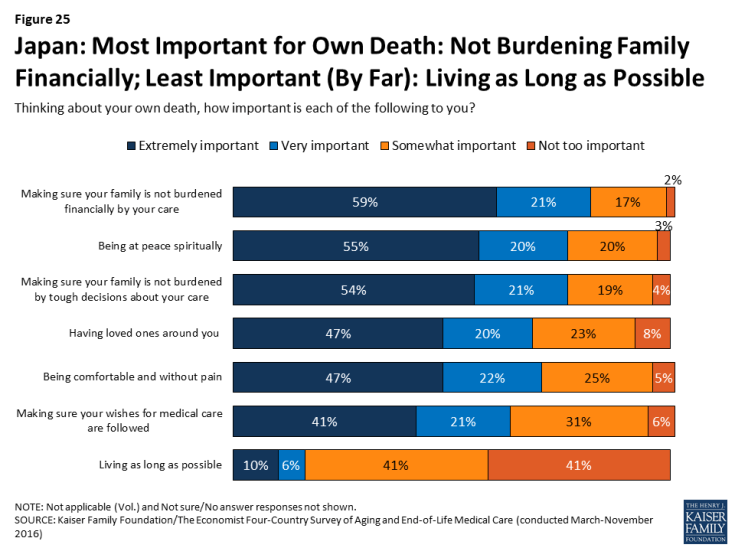
Figure 25: Japan: Most Important for Own Death: Not Burdening Family Financially; Least Important (By Far): Living as Long as Possible
Conversations about end-of-life wishes are uncommon in Japan.
Just 31 percent of Japanese adults (and 33 percent of those ages 65 and over) say they’ve had a serious conversation with a loved one about their own wishes for end-of-life care. Just 7 percent say they’ve had such a conversation with a doctor and 6 percent say they have their wishes written down. Among those who don’t have their wishes in writing, two-thirds (64 percent) say they’ve never considered it, suggesting this is something that is not discussed or done often in Japan.
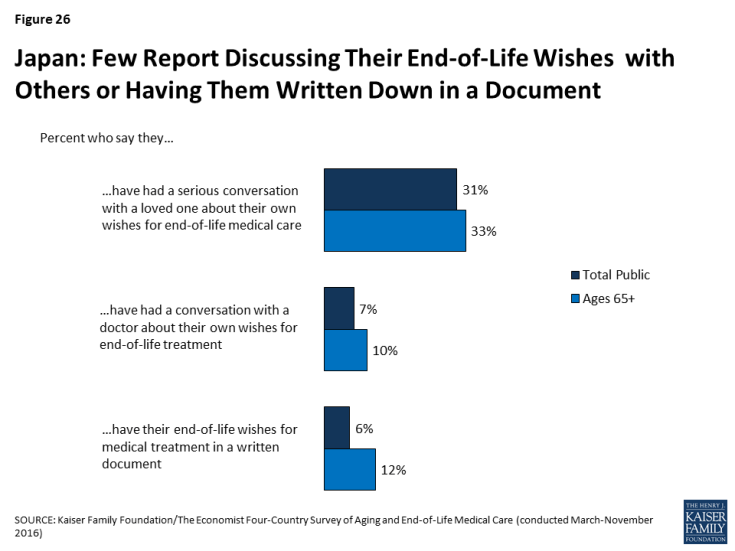
Figure 26: Japan: Few Report Discussing Their End-of-Life Wishes with Others or Having Them Written Down in a Document
Perhaps reflecting this lack of conversation, just 26 percent of adults in Japan who served as a medical decision-maker for someone who died say they knew exactly what their loved one wanted in terms of medical treatment, substantially lower than among decision-makers in the other countries surveyed.
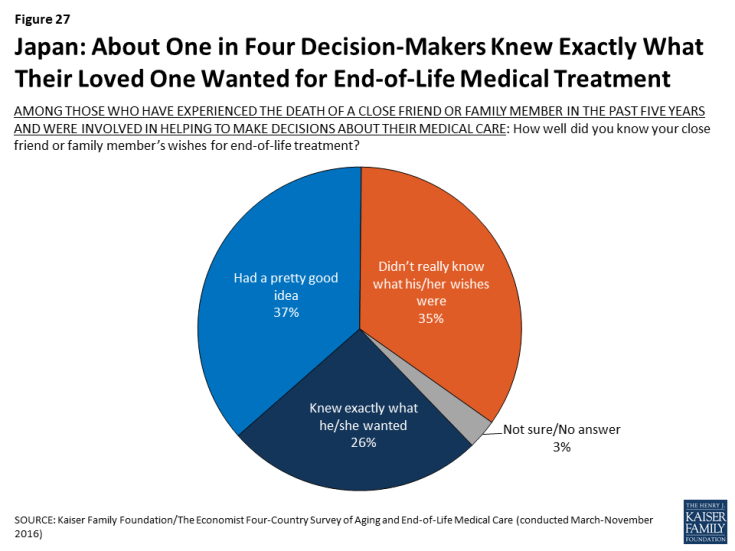
Figure 27: Japan: About One in Four Decision-Makers Knew Exactly What Their Loved One Wanted for End-of-Life Medical Treatment
Some attitudes about end-of-life medical care in Japan differ by education level and gender.
University graduates in Japan are more likely than those with lower levels of education to say the health care system places too much emphasis on extending life and too little emphasis on helping people die without pain and stress. Those with higher levels of education are also more likely to say most people have too little control over decisions about their own medical care at the end of life.
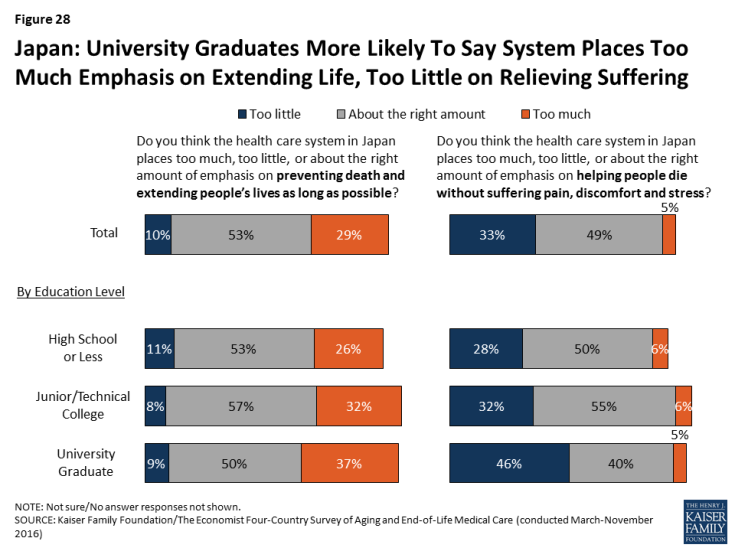
Figure 28: Japan: University Graduates More Likely To Say System Places Too Much Emphasis on Extending Life, Too Little on Relieving Suffering
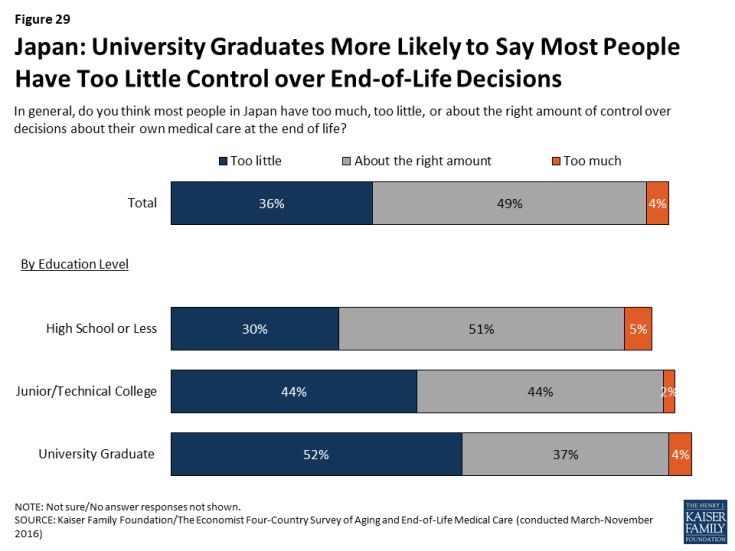
Figure 29: Japan: University Graduates More Likely to Say Most People Have Too Little Control over End-of-Life Decisions
In Japan, women are more likely than men to say they’ve had a conversation with a loved one about their wishes (36 percent vs. 26 percent). By contrast, Japanese men are more likely than women to say they’d prefer to die at home (66 percent vs. 45 percent).
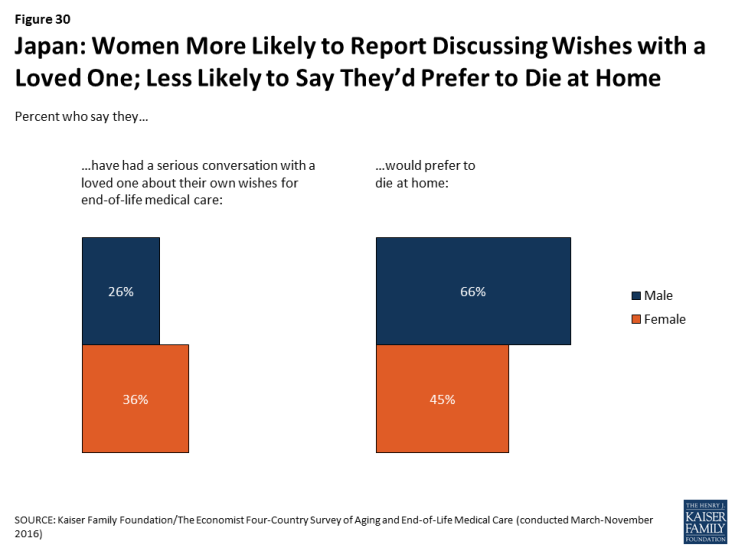
Figure 30: Japan: Women More Likely to Report Discussing Wishes with a Loved One; Less Likely to Say They’d Prefer to Die at Home
Country Highlights: Italy
Italians want their government to take responsibility for the aging population, but most doubt its preparedness to do so.
In Italy, the second-oldest country in our survey, 72 percent see the aging of the population as a problem – including 57 percent who say it’s a major problem – and roughly eight in ten (78 percent) say it should be the responsibility of the government to pay for people’s health and long-term care needs as they age. Yet nearly nine in ten Italians say the government is “not too prepared” (37 percent) or “not at all prepared” (48 percent) to deal with the aging population, and two-thirds (65 percent) say the same about the country’s health care system. Furthermore, six in ten (61 percent) give the country’s health care system a fair or poor rating overall, and half (53 percent) say the same when it comes to end-of-life medical care.
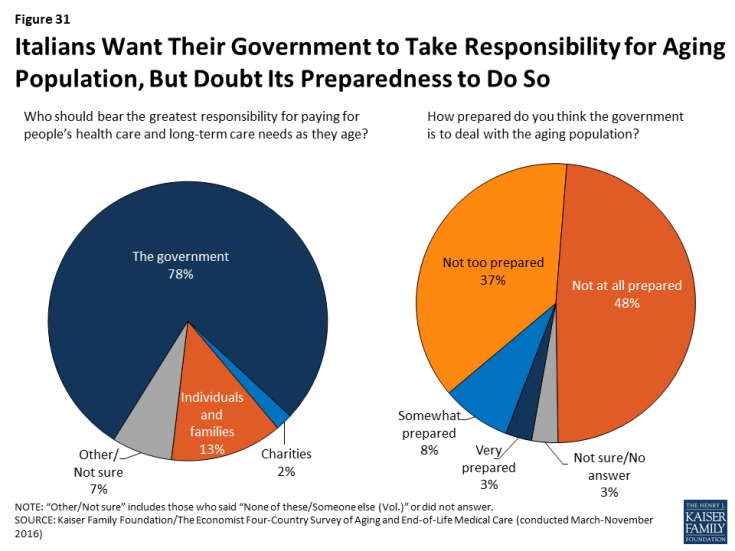
Figure 31: Italians Want Their Government to Take Responsibility for Aging Population, But Doubt Its Preparedness to Do So
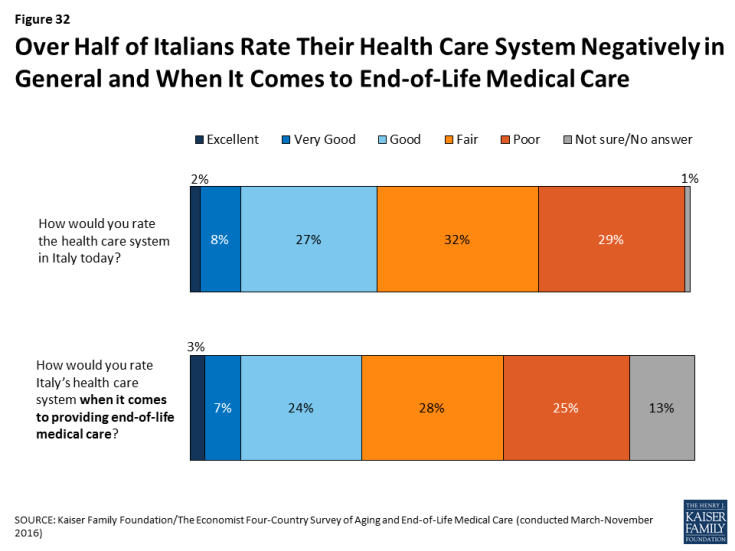
Figure 32: Over Half of Italians Rate Their Health Care System Negatively in General and When It Comes to End-of-Life Medical Care
Italians are more likely than residents of some other countries surveyed to place decisions about end-of-life medical care in the hands of doctors. This is particularly true among Italians with lower incomes and lower levels of education.
While just 11 percent of Italians say they have had a serious conversation with a doctor about their own wishes for end-of-life medical care and just 6 percent say they have these wishes written down, Italians seem somewhat more willing than residents of the U.S. and Japan to place decision-making in the hands of doctors. Three in ten Italians (compared with about one in ten in the U.S. and Japan) say that doctors should have the greater say in which medical treatments to pursue for seriously ill patients who are near the end of their lives, while about half (compared with nearly 9 in 10 in the U.S. and Japan) say patients and their families should have the greater say.
In Italy, those with lower incomes and lower levels of education are more likely than their higher-income, more educated counterparts to say that doctors should have a greater say in these decisions. For example, 37 percent of Italians with less than a high school education say that doctors should have the greater say in medical decisions, compared with just 17 percent of university graduates.
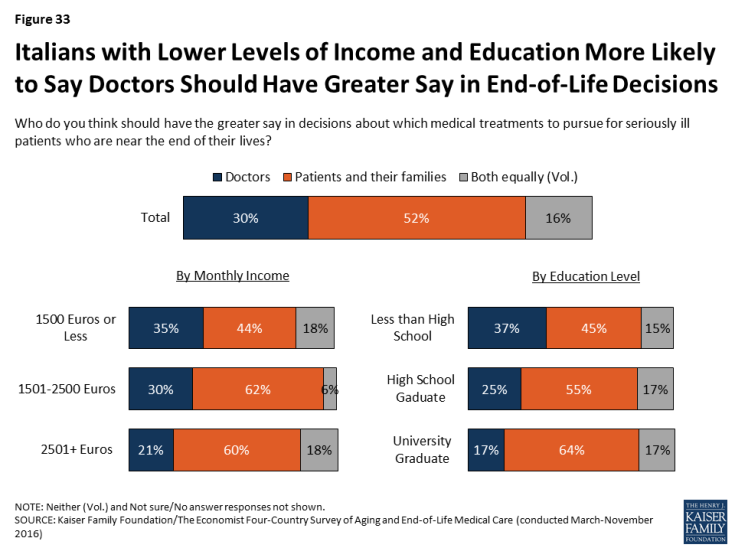
Figure 33: Italians with Lower Levels of Income and Education More Likely to Say Doctors Should Have Greater Say in End-of-Life Decisions
When it comes to priorities for their own death, Italians value the presence of loved ones along with a variety of other factors.
Asked what is important in thinking about their own death, a third (34 percent) of Italians say that having loved ones around is “extremely important.” Similar shares say the same about making sure their wishes for medical care are followed, being comfortable and without pain, and making sure their family is not burdened financially by their care. As in Japan, living as long as possible ranks far behind other factors, with just 14 percent saying it is “extremely important” to them.
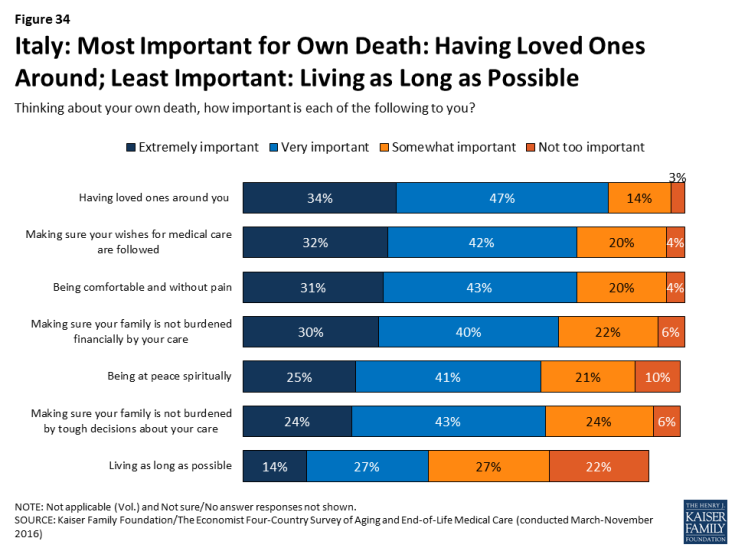
Figure 34: Italy: Most Important for Own Death: Having Loved Ones Around; Least Important: Living as Long as Possible
Some other interesting demographic differences in views of end-of-life care in Italy are worth highlighting.
As in Japan, women in Italy are somewhat more likely than men to report having had a serious conversation with a loved one about their own wishes for end-of-life medical care (53 percent vs. 42 percent).
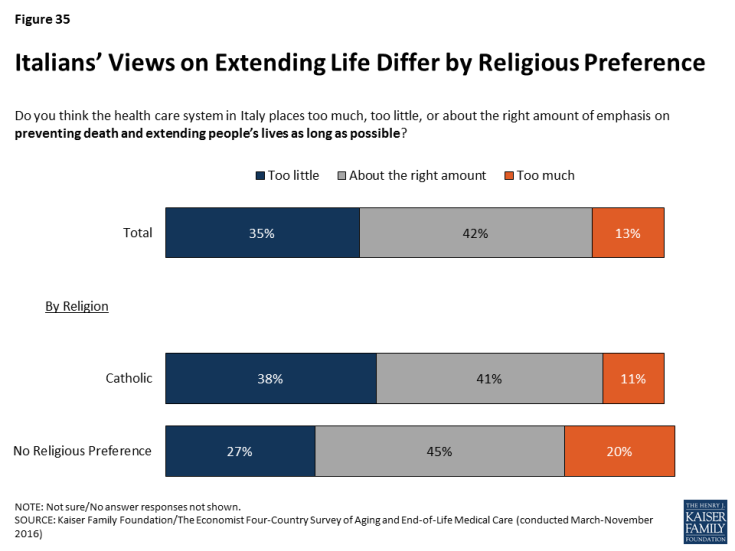
Catholics – who make up 75 percent of adults in Italy – are more likely than those with no religious preferences to say the health care system in Italy places too little emphasis on extending life (38 percent vs. 27 percent). By contrast, those with no religious preference are more likely than Catholics to say the health care system places too much emphasis on extending life (20 percent vs. 11 percent).
Among Italians with a loved one who died in the past five years, those with lower incomes are more likely to say their loved one received medical care that placed an undue financial burden on the family and less likely to say they had access to appropriate life-extending treatments.
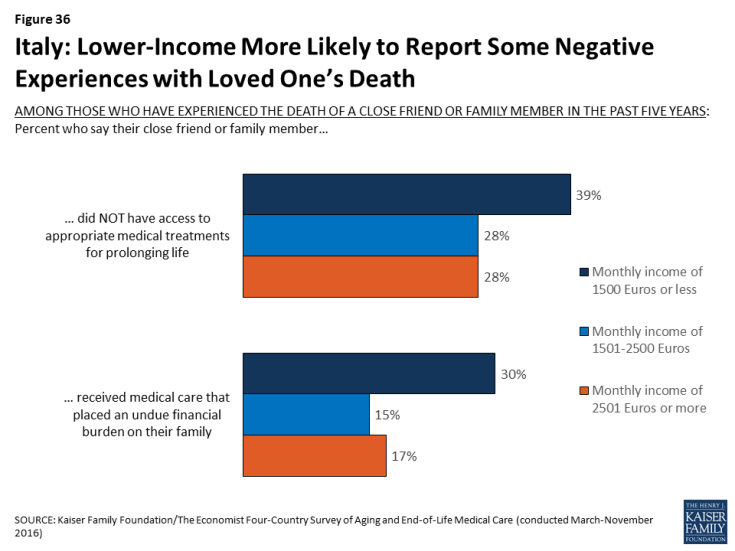
Figure 36: Italy: Lower-Income More Likely to Report Some Negative Experiences with Loved One’s Death
Country Highlights: Brazil
Among the countries surveyed, Brazilians stand out as having the most negative views of their health care system, yet they are the most likely to defer to doctors when it comes to end-of-life decision making.
In Brazil, a country whose state-sponsored health care system has been plagued by problems, nine in ten residents give the health care system a rating of “fair” or “poor” both in general (90 percent) and when it comes to providing end-of-life medical care (86 percent), by far the most negative ratings among the countries surveyed.
Brazilians are also the most likely of any country surveyed to say that most people in their country have too little control over their own medical care at the end of life (79 percent). Despite this sense that people should have more control, Brazilians are more likely than residents of the other countries surveyed to say that doctors should have the greater say in which medical treatments to pursue for seriously ill patients; 4 in 10 say doctors should have the greater say, while about half say patients and their families should have the greater say. And among Brazilians who have not discussed their own end-of-life wishes with a loved one, the main reason given is that they will trust their doctor to make those decisions for them when the time comes.
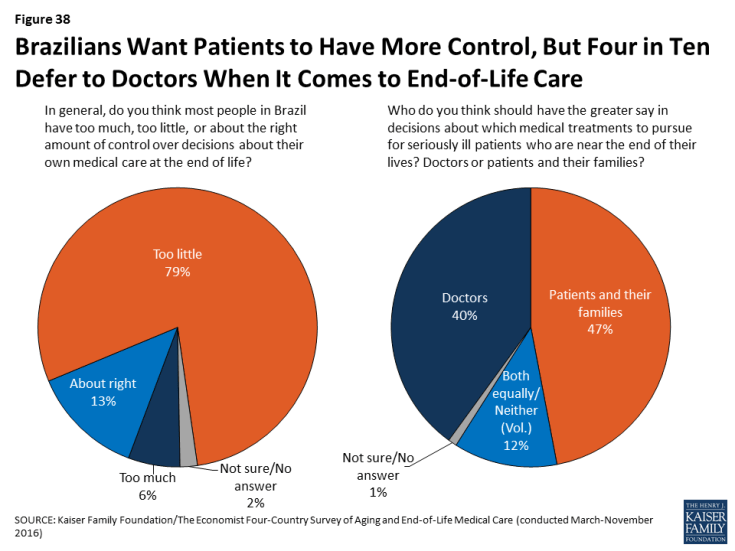
Figure 38: Brazilians Want Patients to Have More Control, But Four in Ten Defer to Doctors When It Comes to End-of-Life Care
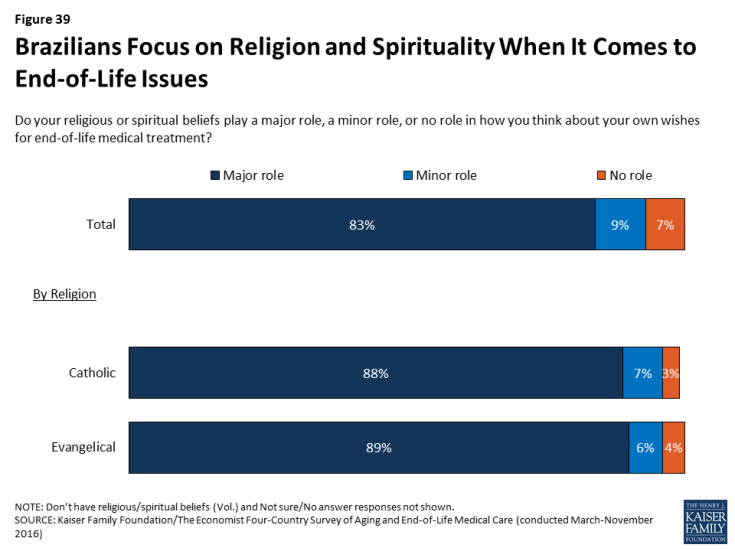
Brazilians stand out as being more likely than residents of other countries surveyed to focus on religion and spirituality when it comes to end-of-life issues.
Eight in ten Brazilians (83 percent) say their religious or spiritual beliefs play a major role in how they think about their own wishes for end-of-life medical treatment, compared to about half of residents in the U.S. and Italy and just 13 percent in Japan. Forty-four percent of adults in Brazil identify as Catholic and three in ten identify as Evangelical; these groups are about equally likely to say their beliefs play a major role in their thinking on these issues.
When asked the importance of various factors in thinking about their own death, “being at peace spiritually” ranks number one in Brazil, with 40 percent saying it is extremely important and another 49 percent saying it is very important. In contrast to the other countries surveyed, a quarter of Brazilians (26 percent) say that living as long as possible is extremely important to them, placing it on par with other concerns like having loved ones around, making sure your family is not burdened financially, and making sure your wishes about medical care are followed.
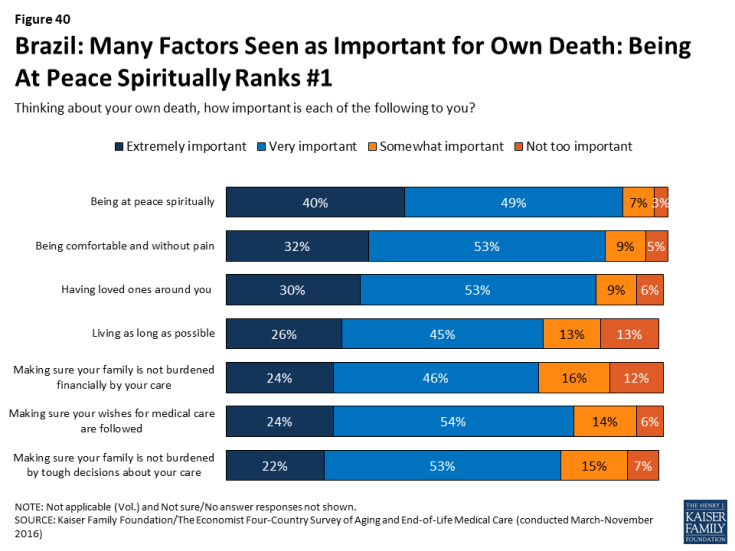
Figure 40: Brazil: Many Factors Seen as Important for Own Death: Being At Peace Spiritually Ranks #1
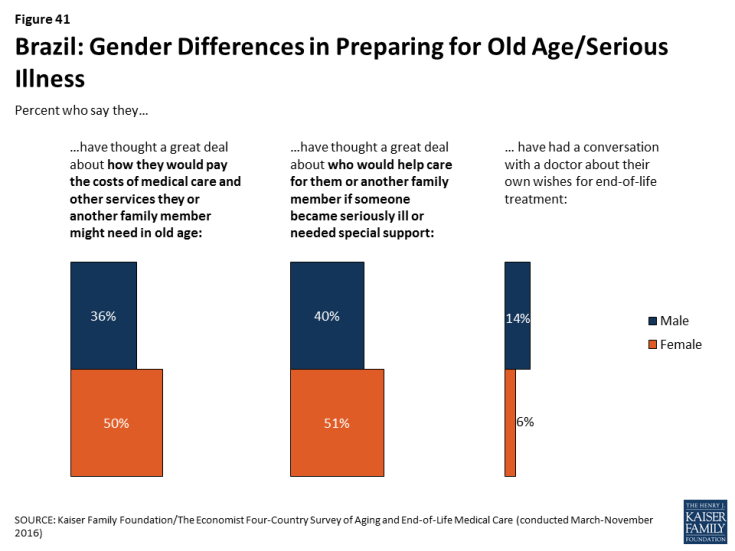
Some attitudes about end-of-life care in Brazil differ by gender and education level.
Among Brazilians, women are more likely than men to say they have thought a great deal about how they would pay for the costs of medical care and other services they or another family member might need in old age (50 percent vs. 36 percent) and who would provide care for them or another family member if someone became seriously ill and needed special support (51 percent vs. 40 percent). However, men are more likely than women to report discussing their own wishes for end-of-life treatment with a health care provider (14 percent versus 6 percent).
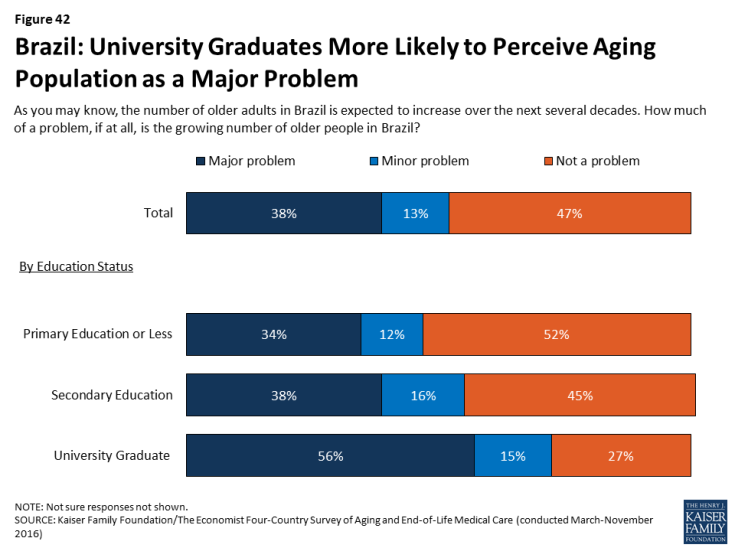
While Brazil is a relatively young country, Brazilians with higher levels of education appear to be more concerned than their less-educated counterparts about the issue of population aging. Nearly six in ten university graduates (56 percent) say the growing number of older adults in Brazil is a major problem, compared with about a third (34 percent) of those with a primary education or less.
There is also a difference based on education level in Brazilians’ attitudes about extending life. While Brazilians overall are more likely to prioritize prolonging life over helping people die without pain, discomfort, and stress, university grads lean in the other direction (58 percent say reducing pain and stress should be more important).
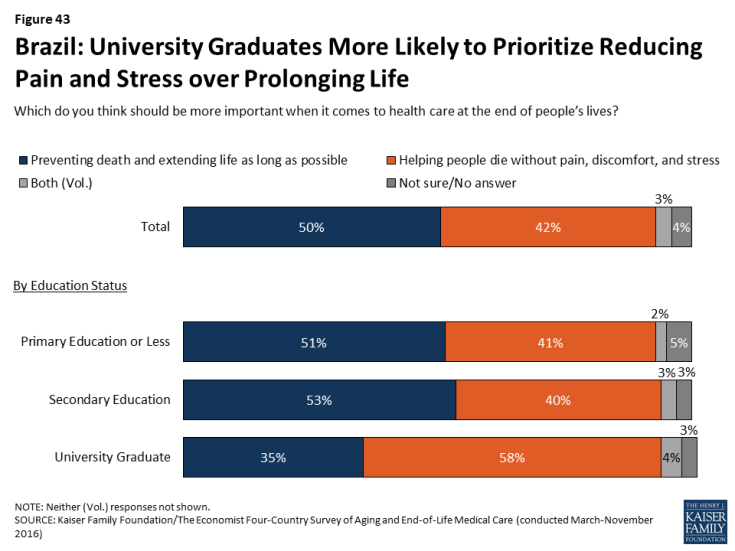
Figure 43: Brazil: University Graduates More Likely to Prioritize Reducing Pain and Stress over Prolonging Life
Methodology
The Kaiser Family Foundation/The Economist Four-Country Survey on Aging and End-of-Life Medical Care was conducted among nationally representative random digit dial (RDD) telephone (landline and cell phone) samples of adults ages 18 and older, living in the United States (including Alaska and Hawaii), Brazil, Italy, and Japan (Note: persons without a telephone could not be included in the random selection process). SSRS carried out the sampling and weighting for all countries, and conducted computer-assisted telephone interviews for the U.S. sample. Interviews in Brazil were carried out by Cido International, and interviews in Japan and Italy were carried out by European Field Group, under the direction of SSRS. RDD landline and cell phone samples were provided by Marketing Systems Group (MSG) for the U.S., Sample Answers for Brazil, and Sample Solutions Europe (SSE) for Japan and Italy. Interview languages, field dates, and sample sizes for each country are shown in the table below. Teams from The Economist and the Kaiser Family Foundation worked together to develop the survey questionnaire and analyze the data. The Kaiser Family Foundation paid for the fieldwork costs associated with the survey. Each organization is responsible for its content.
Due to the multi-national design, the questionnaire was tested and translated in multiple stages. The first step involved a live-interview telephone pretest of the English questionnaire with U.S. respondents. Revisions to the English questionnaire were made following the pretest in order to shorten the survey instrument and improve respondent comprehension of questions. Following the English pretest, the questionnaire was translated into Spanish (for interviewing in the U.S.), Italian, Japanese, and Portuguese. Translations were reviewed by a team of professional translators and by regional experts at The Economist. A second pretest was conducted in Italy, Japan, and Brazil, after which further revisions were made to the non-English versions of the questionnaire.
In each country, to randomly select a household member for the landline samples, respondents were selected by asking for the adult male or female currently at home who had the most recent birthday based on a random rotation. If no one of that gender was available, interviewers asked to speak with the adult of the opposite gender who had the most recent birthday. For the cell phone samples, interviews were conducted with the adult who answered the phone.
Multi-stage weighting processes were applied separately for each country to ensure an accurate representation of each country’s national adult population. The first stage of weighting involved corrections to account for the fact that respondents with both a landline and cell phone have a higher probability of selection. The second weighting stage was designed to make demographic adjustments to the sample to match national population estimates. In the U.S., the sample was balanced to match known adult-population parameters using data from the Census Bureau’s 2015 March supplement of the Current Population Survey (CPS) and phone use parameters from the July-December 2015 early release estimates for the National Health Interview Survey. The weighting parameters used for the U.S. were age, gender, education, race/ethnicity, marital status, census region, and telephone use. In Italy, the sample was balanced using estimates from Instituto Nazionale di Statistica’s population projections based on 2010-2011 Census reports, with weighting parameters for age, education, region, and region by density. In Japan, the sample was balanced to match population parameters from Japan’s Statistical Yearbook 2015, based on age, education, and region by prefecture. In Brazil, the sample was balanced using the 2010 Population Census conducted by Instituto Brasileiro de Geografia de Estatística, based on age, education, region, and rural status. All statistical tests of significance account for the effect of weighting.
At the end of the field period, SSRS completed several data validation processes on the international data that included: internal validity checks, testing for straightlining, and analyzing paradata (interviewer workload, interview length, interview time, and overlap of interviews). The Kaiser Family Foundation, along with SSRS, also conducted a percent-match procedure to identify cases that share a high-percentage of identical responses to a large set of questions. This extra validation measure allows for detection of possible duplicate data, whether as a result of intentional falsification, or due to errors in data-processing.
The margin of sampling error including the design effect for each country sample is plus or minus 4 percentage points. For results based on subgroups, the margin of sampling error will be higher; sample sizes and margins of sampling error for subgroups are available by request. Note that sampling error is only one of many potential sources of error in this or any other public opinion poll. Kaiser Family Foundation public opinion and survey research is a charter member of the Transparency Initiative of the American Association for Public Opinion Research.
| Country | Field dates | Language(s) | Total sample size (unweighted) | Cell phone sample | Landline sample | M.O.S.E |
| U.S | March 30-May 29 | English and Spanish | 1,006 | 739 | 268 | ±4 percentage points |
| Italy | September 15-October 3 | Italian | 1,000 | 600 | 400 | ±4 percentage points |
| Japan | September 10-October 20 | Japanese | 1,000 | 500 | 500 | ±4 percentage points |
| Brazil | August 26-November 12 | Portuguese | 1,233 | 714 | 519 | ±4 percentage points |
Endnotes
Summary
Key Findings Across Countries
Peter G. Peterson Foundation, Per Capita Healthcare Costs – International Comparison, October 2016. http://www.pgpf.org/chart-archive/0006_health-care-oecd
OECD, Health Statistics 2014, 2014. http://www.oecd.org/els/health-systems/Briefing-Note-JAPAN-2014.pdf
National Hospice and Palliative Care Organization, Hospice Care in America, September 2015. http://www.nhpco.org/sites/default/files/public/Statistics_Research/2015_Facts_Figures.pdf