Women and Health Care in the Early Years of the ACA: Key Findings from the 2013 Kaiser Women's Health Survey
Connections to Health Providers
Women have a broad range of health needs that evolve over the course of their lives. In their younger years, health concerns related to reproductive and sexual health are priorities. As they age, management of chronic health problems takes on a larger role. Women’s health needs and connections to providers are major factors in how they use health care. The ACA includes a number of measures that affect the delivery of care, such as incentives to increase the supply of primary care providers, who are often a woman’s main connection to the larger health system. However, in recent years, there has been much concern that the supply of primary care providers is already insufficient and that this problem will be exacerbated by the health care demands of the newly insured. The ACA also prioritizes the development and expansion of health care delivery models, such as medical homes and accountable care organizations, which include financial incentives for providers to work in partnerships. The goal is to provide a strong linkage to a primary care provider and integrate the wide array of clinicians that women may turn to for health care. The expectation is that this will result in better coordination and continuity of care, as well as enhanced access to the full range of services women may need.
Usual Sources of Care
Having a usual site of care and a doctor are markers of women’s access to care and are associated with higher use of recommended preventive care and screening services. Having a regular place or provider helps with care coordination and can promote access and continuity. There is increased attention in the ACA to the concept of a “medical home.” In the case of women, this would be a health care setting where women’s health needs can be addressed and coordinated in a way that can promote the quality of care and reduce duplication in care. This is especially important for women, who are more likely than men to rely on at least two providers for their routine care.
Most women have a place that they go for routine care, but it is less common among young, Hispanic, low-income and uninsured women to have a usual source of care.
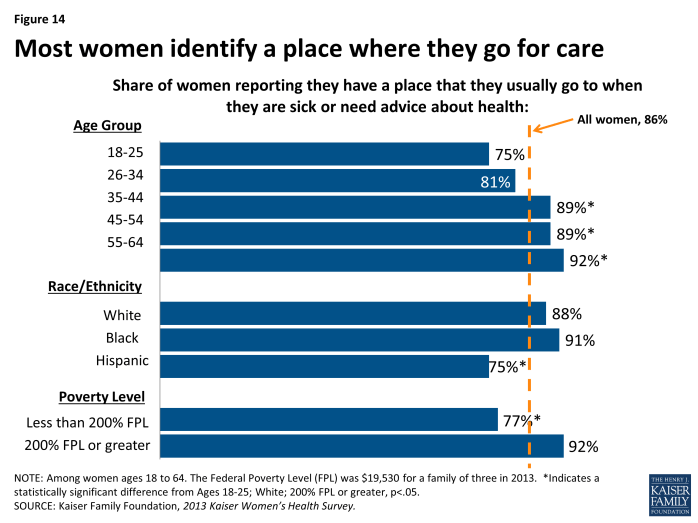
Most women (86%) report they have a place to go for care when they are sick or need advice about their health (Exhibit 4.1). This rate is significantly higher than for men (72%). Among women, however, the rate is lowest among younger women, with 75% of women ages 18 to 25 and 81% of women 26 to 34 reporting they have a usual place to get their care, significantly lower than the rates for women who are older. Fewer Hispanic women (75%), low-income (77%) and uninsured women (69%) report they have a routine place to get their care.
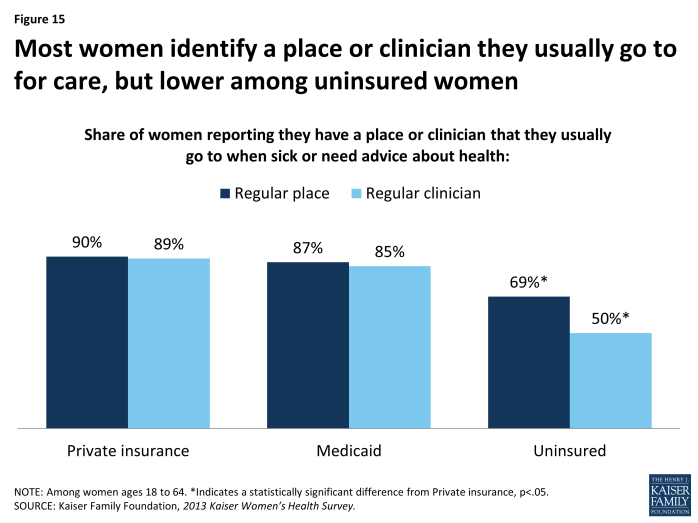
The vast majority of women also report that they have a specific clinician (doctor or other health provider) that they see for their routine care. Overall, more than eight in ten women report that they have a provider (81%) they use when they are sick or need routine care, compared to 68% of men. The rate is similar between privately insured women (89%) and those covered by Medicaid (85%) (Exhibit 4.2). For uninsured women, however, connections with individual providers are the most tenuous. While about two-thirds (69%) say they have a place they get their care, only half report that they have a specific clinician that they see for routine care (50%).
Health care settings
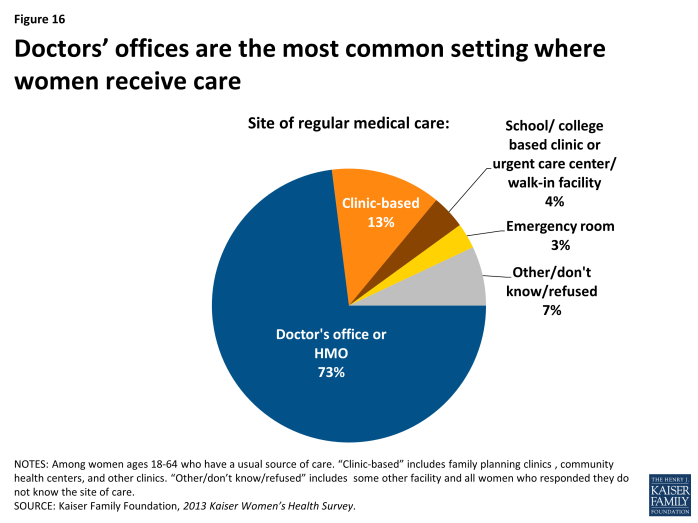
Most women get their routine care from doctor’s offices, but one in ten rely on clinic-based settings.
Among women who identify a routine setting, doctor’s offices and HMOs are the most common site reported (Exhibit 4.3). Almost three in four women (73%) report that this is where they seek care. About one in ten women (13%) rely on a clinic setting and 3% report an emergency room as their routine source of care. A small fraction of women report that they rely on school based clinics or urgent care centers for their routine care. Women who use urgent centers and emergency rooms may be most at risk for receiving expensive, fragmented, and discontinuous care.
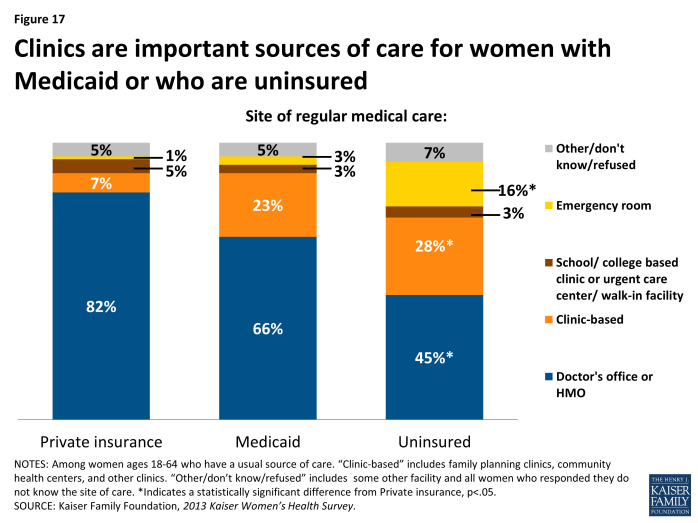
A sizable minority of women covered by Medicaid or who are uninsured rely on clinics for their care. For one in six uninsured women, emergency departments serve as their routine source of care.
Differences in the types of settings that women with various types of insurance coverage rely on are notable (Exhibit 4.4). This variation reflects the networks of providers available to women through their plans and the long-standing role that safety net providers have filled in serving uninsured and low-income patients. While eight in ten women with private insurance (82%) go to a doctor’s office for routine care, this share drops to two-thirds of women with Medicaid coverage (66%) and less than half of uninsured women (45%). There have been historical challenges with physician participation in the Medicaid program, which is due in part to low provider reimbursement rates under the program. Medicaid beneficiaries (23%) an d uninsured women (28%) have much higher use of clinics than privately-insured women (7%). Community health centers and public clinics were established to help care for low-income and underserved populations and play a major role serving these women. Of particular concern though, is that 16% of uninsured women say they usually seek care when they are sick or need medical advice in an emergency room, a rate considerably higher than their counterparts with Medicaid (3%) or private coverage (1%). As more women gain coverage under the ACA, they may also have better access to primary care and it is hoped that reliance on emergency departments for non-urgent care will fall. It is also not clear at this point, however, whether the provider networks under plans offered by state Marketplaces will include traditional safety-net providers, such as community health centers and family planning clinics.
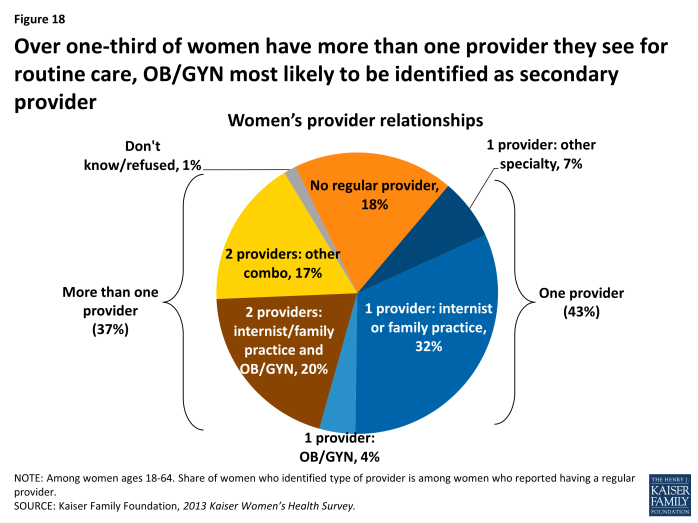
One-third of women report that they see more than more than one clinician for their routine care.
Over four in ten women (43%) report they see one provider regularly and one-third of women (37%) say they have multiple providers to address their basic health needs (compared to 18% of men). Family practitioners and internists are the most common provider types, and among those with multiple providers, Obstetrician-Gynecologists (Ob/Gyns) are the most commonly identified second provider. This is not surprising given women’s reproductive and sexual health needs. Almost one in five women (18%) do not have a regular provider of any type (Exhibit 4.5).
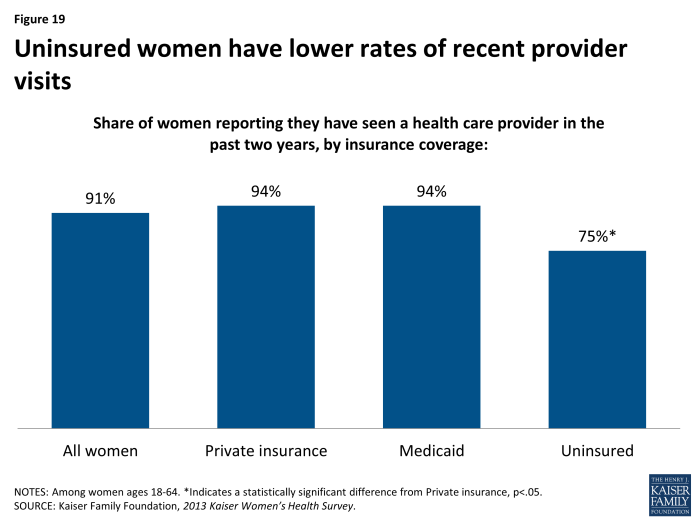
Most women have had a recent health provider visit in the past two years, but uninsured women have the lowest rates.
Nine in ten adult women (91%) have seen a health care provider in the past two years compared to 75% of men. Hispanic women (84%) have a significantly lower rate than Black (91%) or White (93%) women of having a provider visit in the past two years. The largest difference is between women who are uninsured (75%), who have a significantly lower rate than women with private insurance or Medicaid (Exhibit 4.6). Designing a medical home for women is complicated by the traditional division of care that many women experience, with reliance on Ob/Gyns for reproductive care as well as primary care providers for other types of care. Among women with more complex and multiple medical conditions, similar challenges will arise. In designing programs and systems that encourage stable and comprehensive medical homes, the distinct needs of women are important considerations.
Most women use at least one prescription medication on an ongoing basis, and nearly one in ten take six or more medications on a regular basis.
Another important health access issue relates to women’s use of prescription drugs. Over half of women (56%) take at least one prescription medicine on a regular basis compared to just over one-third of men (37%). Three in ten women say they take one or two prescription medications (31%), while nearly one in ten women (9%) report taking at least six different medicines on a regular basis. Use of prescription medications is driven in part by health needs as well as access to care. Use rises with age, partly due to the higher rates of chronic conditions among older women. Six in ten uninsured women report that they do not use a prescription medicine on a regular basis, compared to about four in ten women with private insurance (40%) and Medicaid (42%) (Table 5). This may be in part attributable to poorer access to care, undiagnosed conditions that could be managed with medication, and poorer ability to pay for medications since they do not have insurance. Almost one in five women covered by Medicaid (19%) take at least 6 medications on an ongoing basis, compared to 6% of women with private insurance. This difference may be explained by the poorer health status of women enrolled in Medicaid. Women with Medicaid coverage are disproportionately poor and some may qualify on the basis of their disability as well as their poverty status. Under the ACA, prescription medicines are one of the Essential Health Benefits (EHBs) that all new plans must now cover, but specific medicines and cost sharing requirements vary between plans.
| Table 5: Prescription drug use by women, by age, race/ethnicity and insurance status | |||||||||
| All Women | Age Group | Race/Ethnicity | Insurance Status | ||||||
| Share of women reporting: | Ages 18-44 | Ages 45-64 | White | Black | Hispanic | Private | Medicaid | Uninsured | |
| No Rx Use | 44% | 50% | 37%* | 39% | 45% | 60%* | 40% | 42% | 61%* |
| 1-2 Medicines | 31% | 36% | 25%* | 33% | 28% | 27% | 36% | 20%* | 22%* |
| 3-5 Medicines | 16% | 9% | 23%* | 18% | 16% | 8%* | 17% | 19% | 8%* |
| 6+ Medicines | 9% | 4% | 15%* | 10% | 10% | 5% | 6% | 19%* | 7% |
| NOTE: Among women ages 18-64. *Indicates a statistically significant difference from ages 18-44, White, Private insurance, p<05.SOURCE: Kaiser Family Foundation, 2013 Kaiser Women’s Health Survey. | |||||||||