Examining Medicare Part D Policies for Extended Supplies of Medication
In response to the ongoing coronavirus pandemic, current recommendations are for older adults to stay home and away from others. To prepare for extended stays at home, the Centers for Disease Control and Prevention (CDC) recommends gathering extra supplies, including prescription medicines. Some patients may encounter difficulty in doing so, however, as a result of their health plan’s ‘refill too soon’ restrictions, which block coverage for a prescription that is being refilled early. For example, a plan may have a policy of not allowing refills of 30-day prescriptions until at least three weeks after the prescription was last filled.
In light of the coronavirus pandemic, the Coronavirus Aid, Relief, and Economic Security (CARES) Act requires Medicare Part D plans to provide up to a 90-day (3 month) supply of covered Part D drugs to enrollees who request it. Part D plans currently provide drug coverage to more than 46 million older adults and people with disabilities. Prior to this requirement, Part D plans had the option to relax their ‘refill too soon’ restrictions to ensure enrollees had access to a sufficient extended supply of medications, and some plans stated they would temporarily lifted these restrictions, but plans were not required to do so. The change in law is designed to ensure that all Part D enrollees can obtain an extended supply of medications if they request it during the COVID-19 public health emergency.
This analysis examines the share of Part D enrollees who have access to extended supplies of generic, brand-name, and specialty-tier drugs covered by their plan in 2020, under policies that applied prior to the change in law, and that will apply after the COVID-19 emergency declaration ends, when Part D plans will no longer be required by law to issue extended supplies for all Part D drugs they cover.
Findings
Under Part D plan policies on extended supplies that were in effect at the start of the 2020 plan year and will be in effect after the COVID-19 emergency declaration ends:
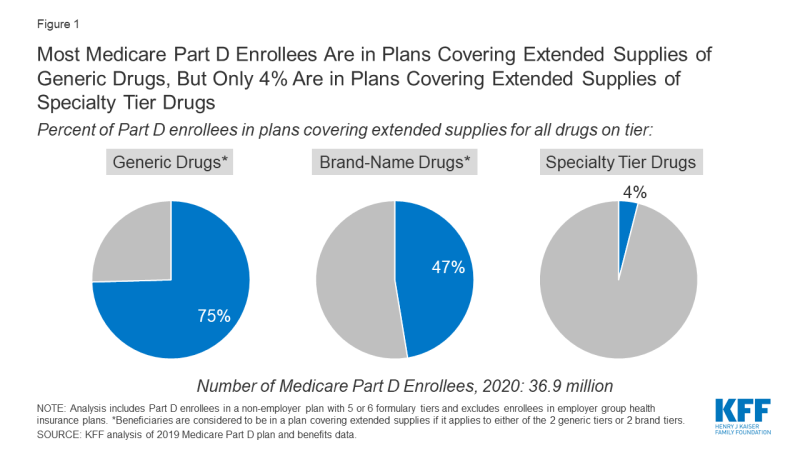
- Three-quarters of Medicare Part D enrollees (27.5 million enrollees) are in a plan that covers extended supplies of all drugs on at least one of the plan’s two tiers for generic drugs (Figure 1).
- Nearly half of all Part D enrollees (47%, or 17.5 million enrollees) are in a plan that covers extended supplies of all drugs on at least one of the plan’s two tiers for brand-name drugs.
- Only 4 percent of Part D enrollees (1.5 million) are in a plan that covers extended supplies of all specialty tier medicines. Specialty tier medicines are defined by Medicare as medicines that cost more than $670 per month and include drugs to manage conditions such as cancer, hepatitis C, multiple sclerosis, and rheumatoid arthritis.
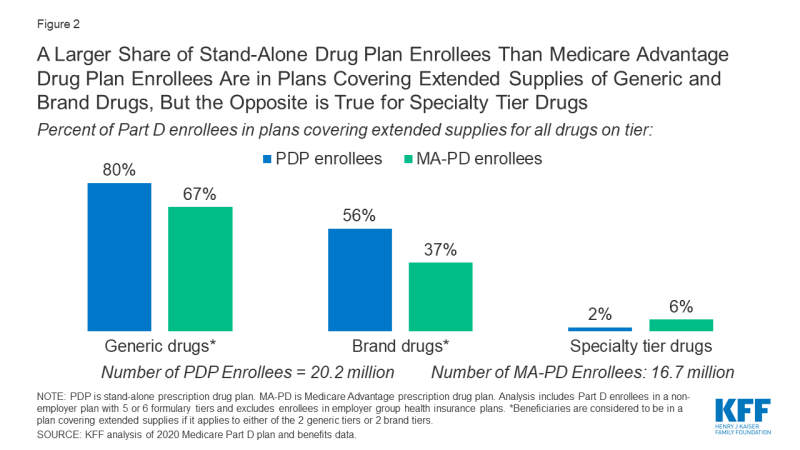
- A larger share of stand-alone drug plan enrollees than Medicare Advantage drug plan enrollees are in plans covering extended supplies of generic drugs (80% vs. 67%, respectively) and brand drugs in 2020 (56% vs. 37%, respectively), but the opposite is true for specialty tier drugs (2% vs. 6%, respectively) (Figure 2).
Discussion
This analysis shows that most Medicare Part D enrollees are in plans covering extended supplies of relatively low-cost generic drugs in 2020, but just under half are in plans that cover extended supplies of brands and only a small share of enrollees are in plans that cover extended supplies of more expensive specialty-tier medications. These coverage policies will be in effect after the COVID-19 emergency declaration ends, when plans will no longer be required by law to issue extended supplies for all Part D drugs they cover.
In light of the CDC recommendations for older adults and people with serious chronic medical conditions to take actions to reduce the risk of becoming infected with the new coronavirus, including staying home and having extra supplies of necessary medications, the requirement that all Part D plans provide up to a 3-month supply of medications to enrollees who request it will help Medicare beneficiaries avoid trips to the pharmacy when there is increased risk of spread of coronavirus in their communities.
Juliette Cubanski and Karyn Schwartz are with KFF. Anthony Damico is an independent consultant.
| Data and Methods |
| This analysis is based on 2020 Medicare Part D plan enrollment and benefit data. The analysis focuses on 36.9 million Part D enrollees who are in a non-employer Part D plan (including both stand-alone prescription drug plans and Medicare Advantage drug plans) with five or six formulary tiers in 2020 (93% of all non-employer Part D enrollees). The analysis excludes 7.0 million enrollees in employer group health insurance plans that offer Part D coverage because details on their plan benefits are not available. |