Facilitating Access to Mental Health Services: A Look at Medicaid, Private Insurance, and the Uninsured
In 2015, over 43 million adults had a mental illness and nearly 10 million had a serious mental illness, such as depression, bipolar disorder, or schizophrenia. People with mental health conditions often have chronic medical conditions, significant health care services utilization, and barriers to employment, and are frequently involved with the criminal justice system.1,2,3,4 Medicaid plays an important role for individuals with mental health conditions, particularly among those with low incomes. In 2015, Medicaid covered 22% of nonelderly adults with mental illness and 26% of nonelderly adults with serious mental illness. The Medicaid program covers many inpatient and outpatient mental health services, such as psychiatric treatment, counseling, and prescription medications. Medicaid coverage of mental health services is often more comprehensive than private insurance coverage.
As of June 2017, 32 states have expanded Medicaid, with enhanced federal funding, to cover adults up to 138% of the federal poverty level ($16,643/year for an individual in 2017). The Medicaid expansion has enabled many low-income individuals with mental health conditions to obtain coverage and access treatment. The following series of graphics describes individuals with mental health conditions and compares mental health needs and receipt of services among individuals without insurance, with Medicaid, and with private insurance. The data show that utilization of mental health services among people with Medicaid is comparable to and sometimes greater than utilization among people with private insurance, while people who lack insurance often face difficulty obtaining services.
1. 20% of nonelderly adults have a mental illness and 5% have a serious mental illness.
2. Nonelderly adults with mental illness are predominantly white, female, and under 50.
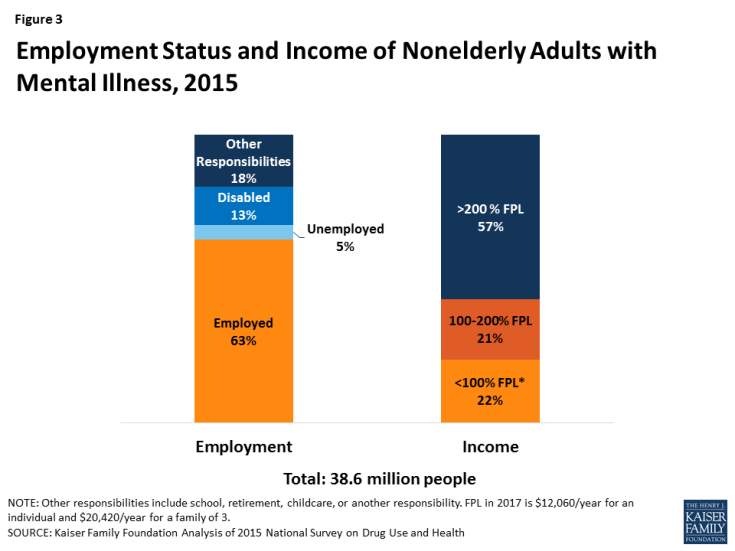
3. Most nonelderly adults with mental illness are employed (63%), but over 4 in 10 have low incomes, including 22% below poverty.
4. Nonelderly adults with mental illness often have co-morbid health conditions.
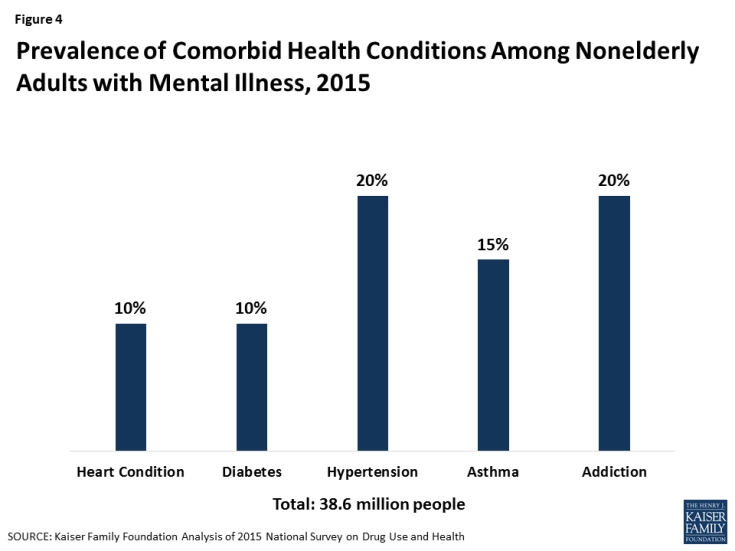
Figure 4: Prevalence of Comorbid Health Conditions Among Nonelderly Adults with Mental Illness, 2015
5. Most nonelderly adults with mental illness and serious mental illness have either Medicaid or private insurance, and Medicaid plays a particularly important role for those with low incomes.
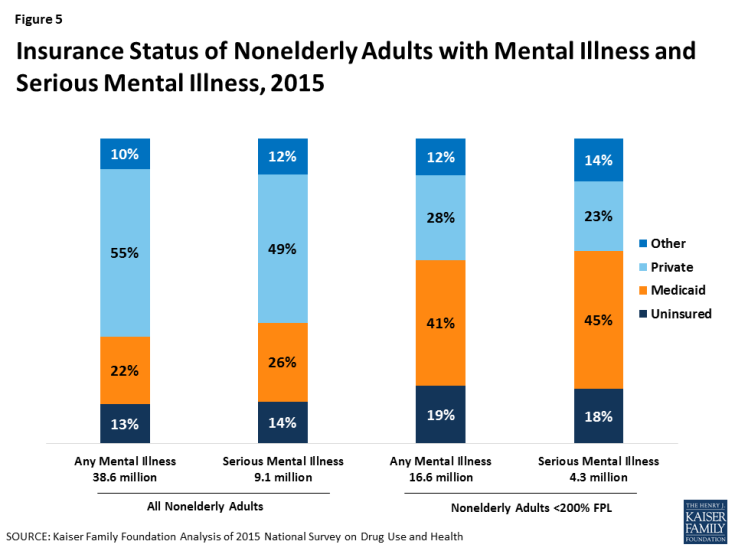
Figure 5: Insurance Status of Nonelderly Adults with Mental Illness and Serious Mental Illness, 2015
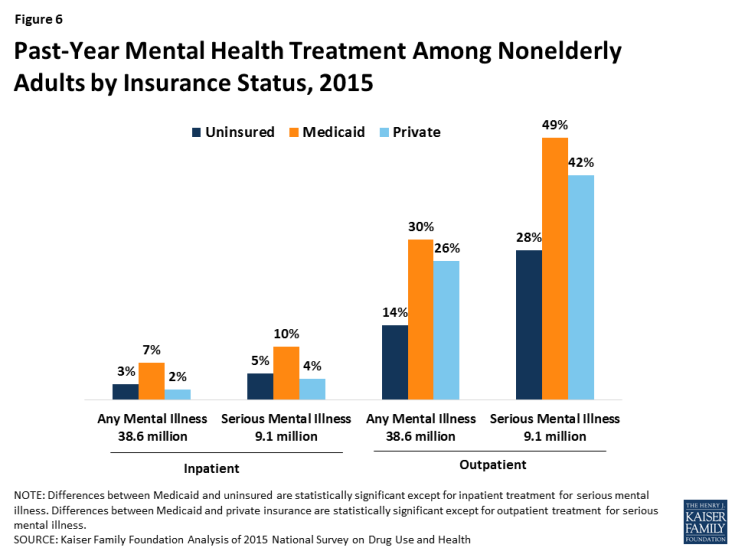
6. Among nonelderly adults with mental illness and serious mental illness, those with Medicaid are more likely than those without insurance or with private insurance to receive treatment.
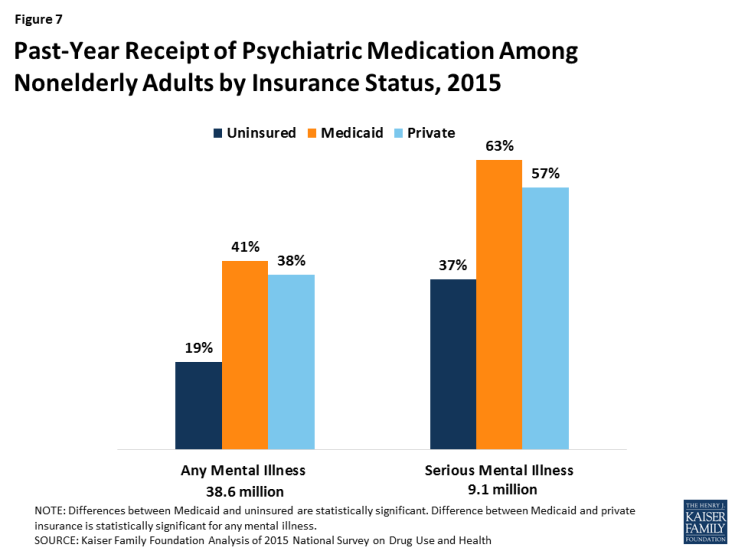
7. Receipt of psychiatric medication is also more common among nonelderly adults with Medicaid compared to those without insurance or with private insurance.
Endnotes
Benjamin G. Druss and Elizabeth Reisinger Walker. Mental disorders and medical comorbidity (Princeton, NJ: Robert Wood Johnson Foundation, February 2011), http://www.integration.samhsa.gov/workforce/mental_disorders_and_medical_comorbidity.pdf
Audrey J. Weiss et al., Trends in Emergency Department Visits Involving Mental and Substance Use Disorders, 2006-2013 (Rockville, MD: Agency for Healthcare Research and Quality, December, 2016), https://www.hcup-us.ahrq.gov/reports/statbriefs/sb216-Mental-Substance-Use-Disorder-ED-Visit-Trends.pdf
Ronald C. Kessler, et al., “Depression in the Workplace: Effects on Short-Term Disability,” Health Affairs, 18, 5(1999):163-71.
Doris J. James and Lauren E. Glaze. Mental Health Problems of Prison and Jail Inmates (Washington, DC: US Department of Justice, December 2006), https://www.bjs.gov/content/pub/pdf/mhppji.pdf